Healthcare Failure Mode and Effect Analysis SM Edward
- Slides: 14
Healthcare Failure Mode and Effect Analysis. SM Edward J. Dunn, MD, MPH VA National Center for Patient Safety edward. dunn@med. va. gov www. patientsafety. gov
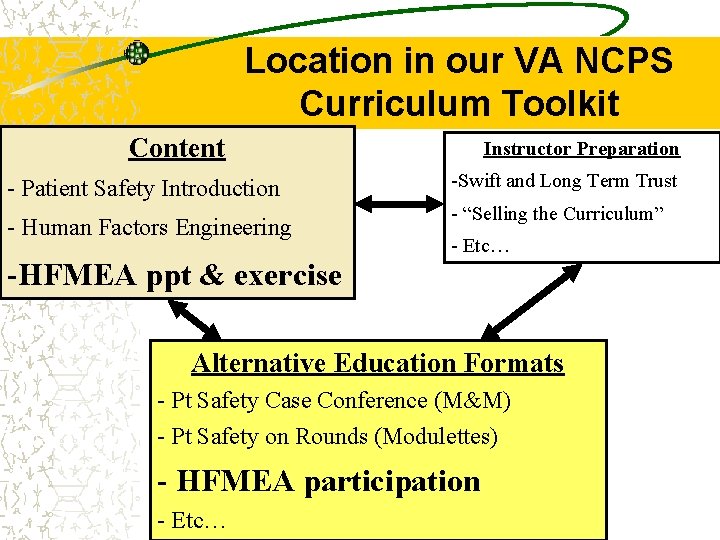
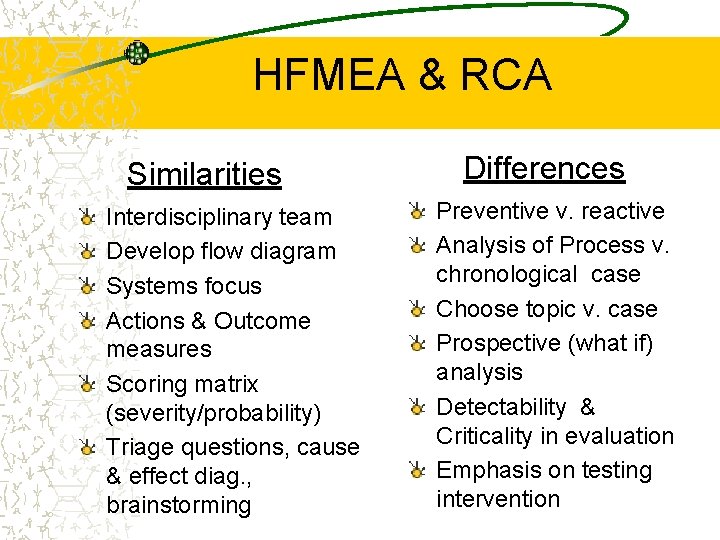
Location in our VA NCPS Curriculum Toolkit Content - Patient Safety Introduction - Human Factors Engineering -HFMEA ppt & exercise Instructor Preparation -Swift and Long Term Trust - “Selling the Curriculum” - Etc… Alternative Education Formats - Pt Safety Case Conference (M&M) - Pt Safety on Rounds (Modulettes) - HFMEA participation - Etc…
Why use prospective analysis? § Aimed at prevention of adverse events § Doesn’t require previous bad experience (patient harm) § Makes system more robust § JCAHO requirement
JCAHO Standard LD. 5. 2 Effective July 2001 Leaders ensure that an ongoing, proactive program for identifying risks to patient safety and reducing medical/health care errors is defined and implemented. § § Identify and prioritize high-risk processes Annually, select at least one high-risk process Identify potential “failure modes” For each “failure mode, ” identify the possible effects § For the most critical effects, conduct a root cause analysis
Who uses failure mode effect analysis? § Engineers worldwide in: Ø Aviation Ø Nuclear power Ø Aerospace Ø Chemical process industries Ø Automotive industries § Has been around for over 40 years § Goal has been, and remains, to prevent accidents from occurring
Healthcare Version - HFMEASM Combines: – Traditional Failure Mode Effect Analysis – Hazard Analysis and Critical Control Point – VA Root Cause Analysis Adapted and Tested in Healthcare Settings – 163 VA hospitals (with some success) – Still a complex process/time commitment (see NIH)
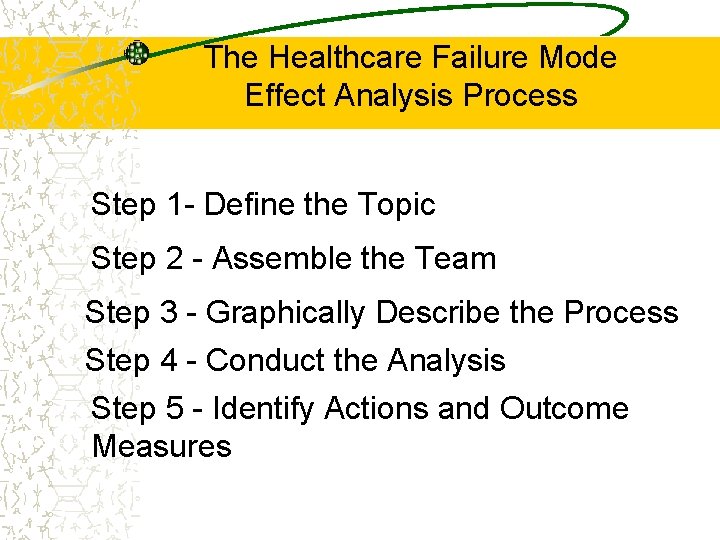
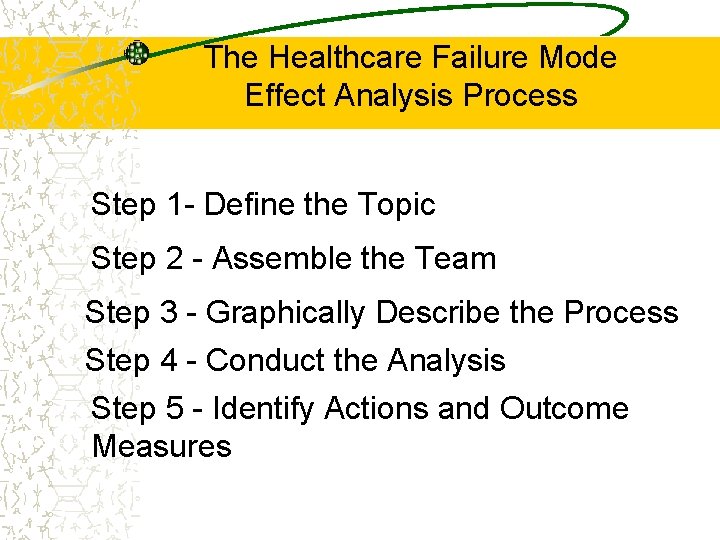
The Healthcare Failure Mode Effect Analysis Process Step 1 - Define the Topic Step 2 - Assemble the Team Step 3 - Graphically Describe the Process Step 4 - Conduct the Analysis Step 5 - Identify Actions and Outcome Measures
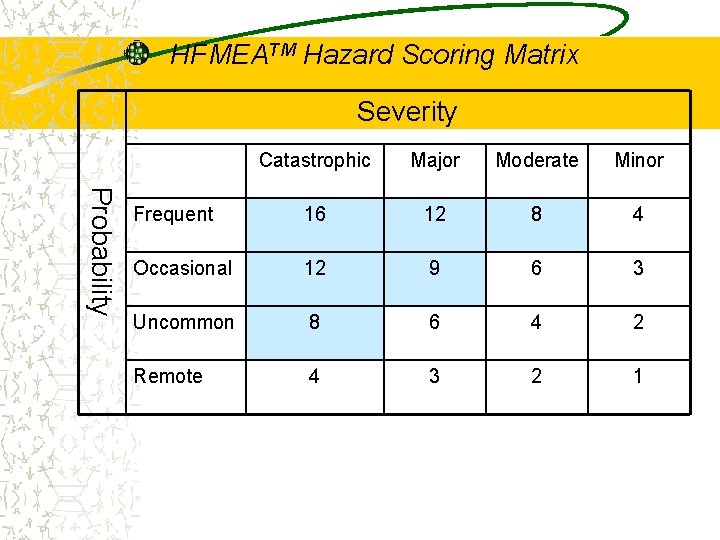
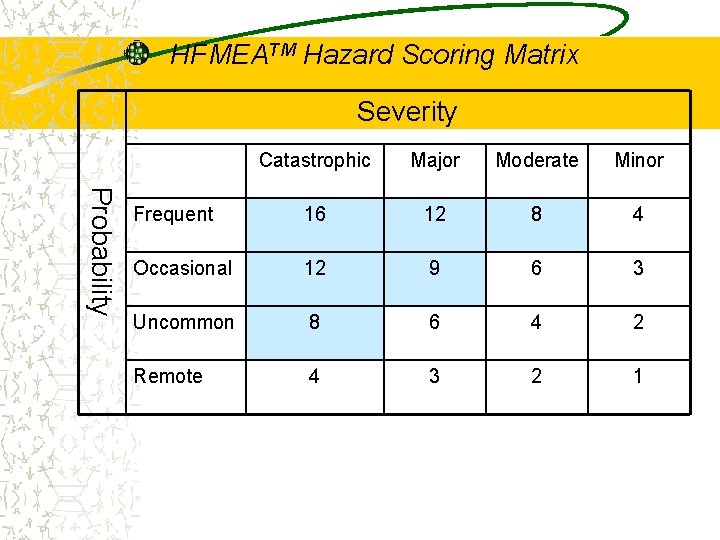
HFMEATM Hazard Scoring Matrix Severity Probability Catastrophic Major Moderate Minor Frequent 16 12 8 4 Occasional 12 9 6 3 Uncommon 8 6 4 2 Remote 4 3 2 1
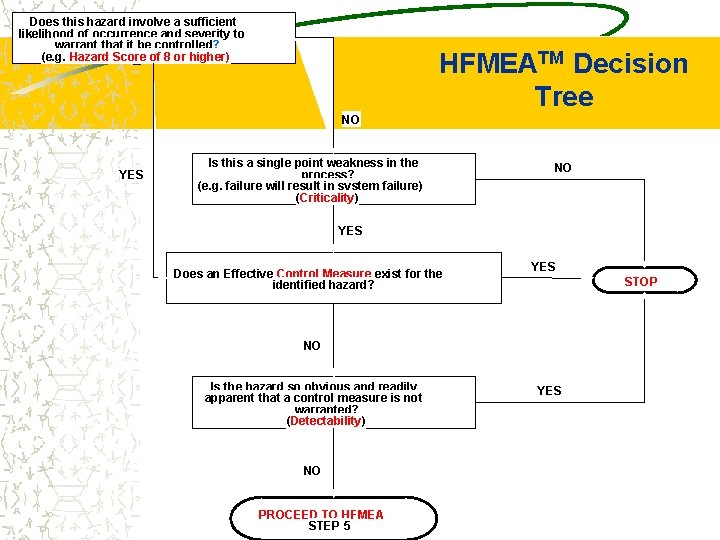
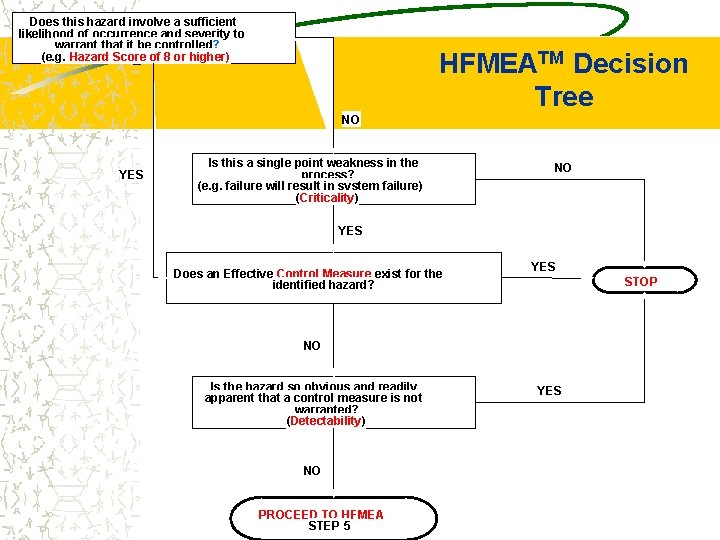
Does this hazard involve a sufficient likelihood of occurrence and severity to warrant that it be controlled? (e. g. Hazard Score of 8 or higher) HFMEATM Decision Tree NO YES Is this a single point weakness in the process? (e. g. failure will result in system failure) (Criticality) NO YES Does an Effective Control Measure exist for the identified hazard? YES STOP NO Is the hazard so obvious and readily apparent that a control measure is not warranted? (Detectability) NO PROCEED TO HFMEA STEP 5 YES
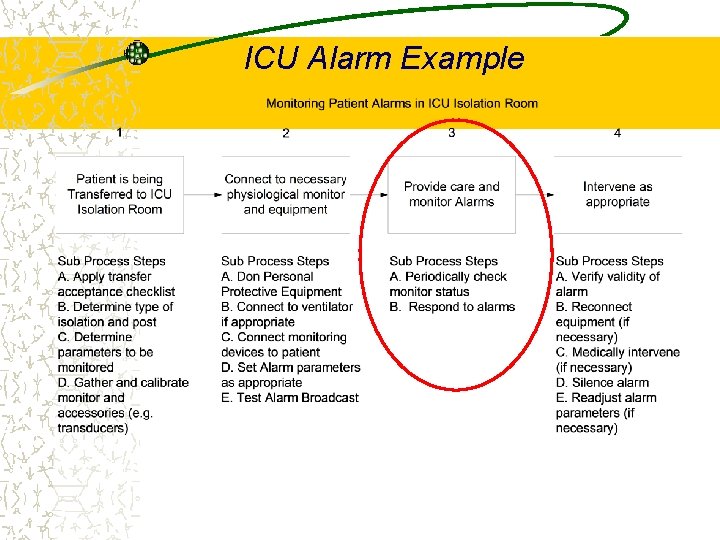
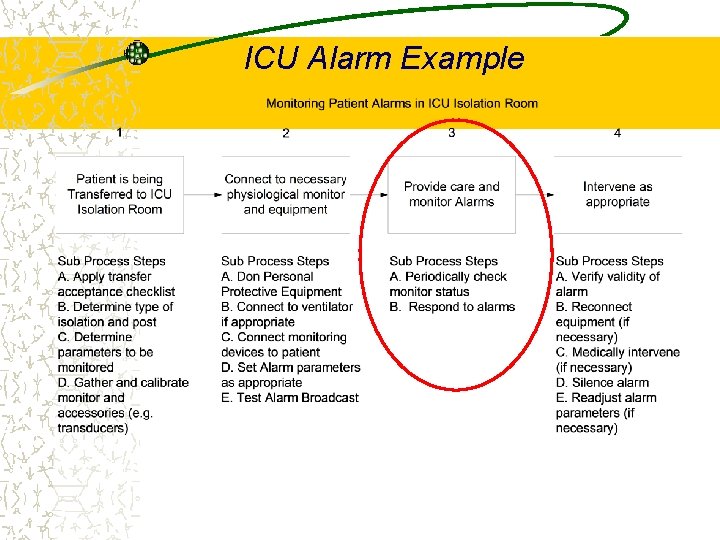
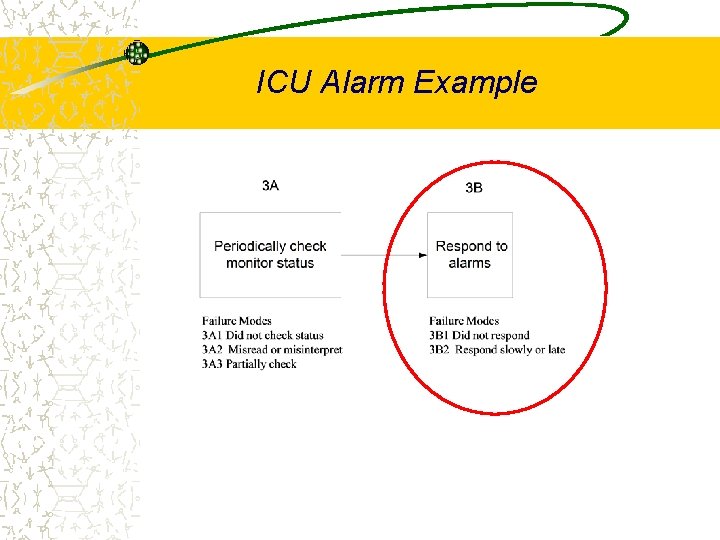
ICU Alarm Example
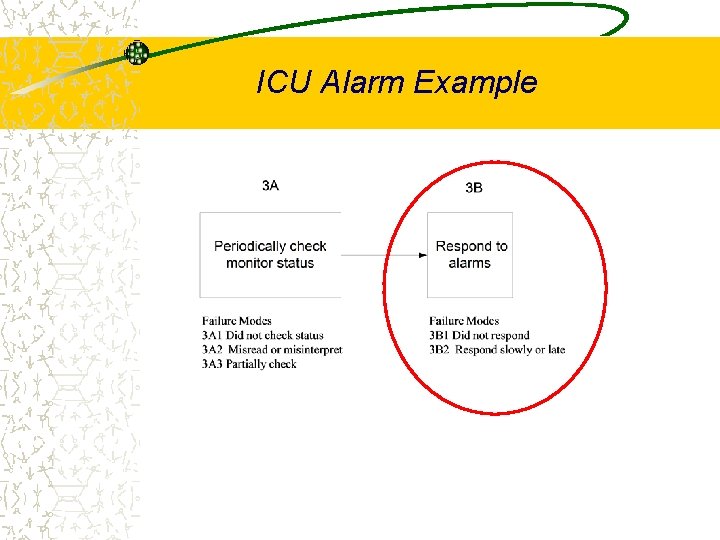
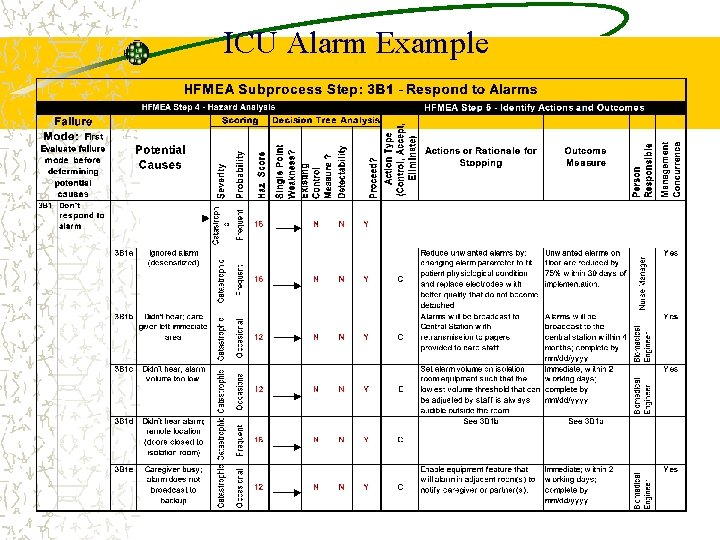
ICU Alarm Example
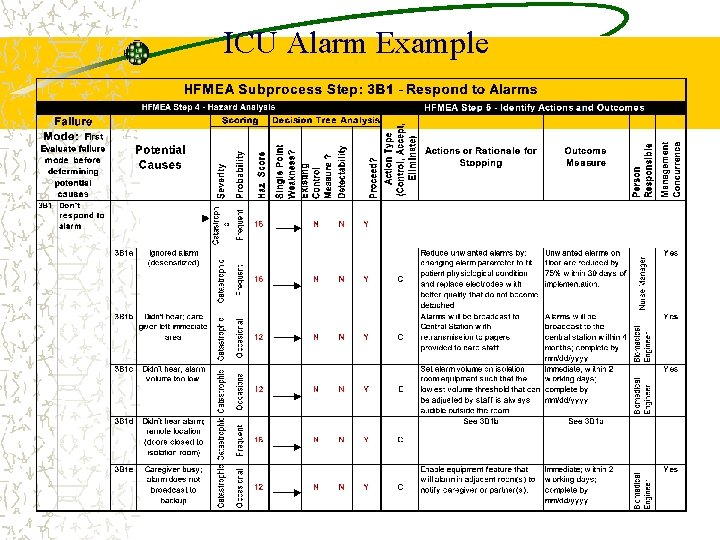
ICU Alarm Example
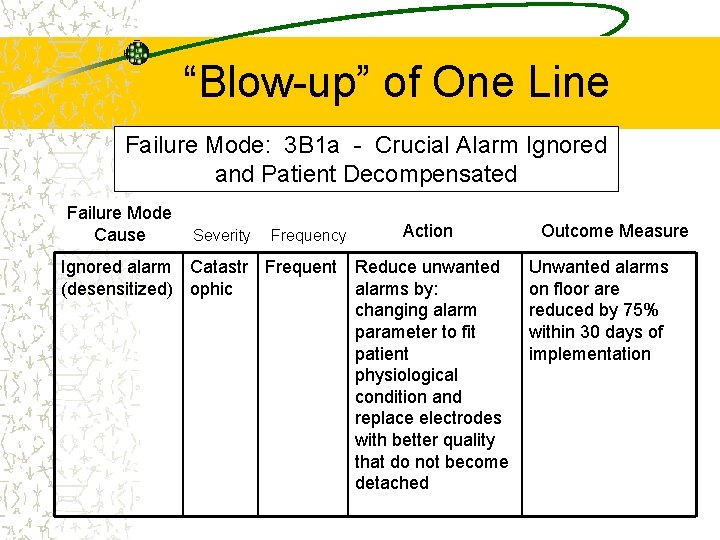
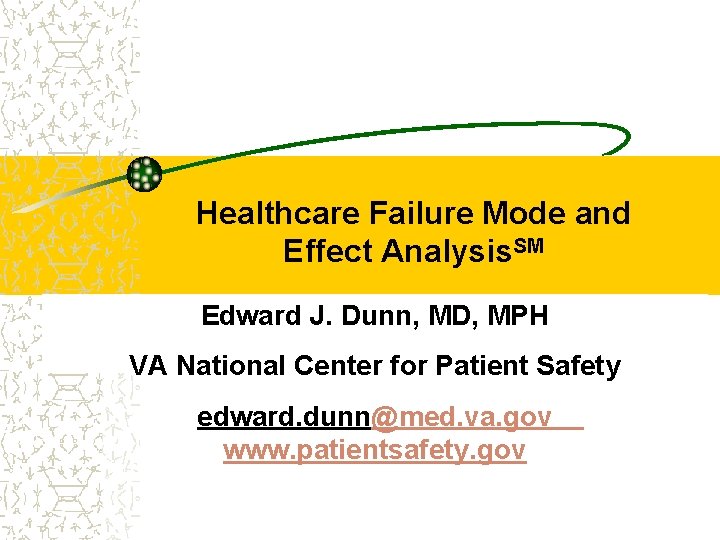
“Blow-up” of One Line Failure Mode: 3 B 1 a - Crucial Alarm Ignored and Patient Decompensated Failure Mode Cause Severity Frequency Ignored alarm Catastr Frequent (desensitized) ophic Action Reduce unwanted alarms by: changing alarm parameter to fit patient physiological condition and replace electrodes with better quality that do not become detached Outcome Measure Unwanted alarms on floor are reduced by 75% within 30 days of implementation
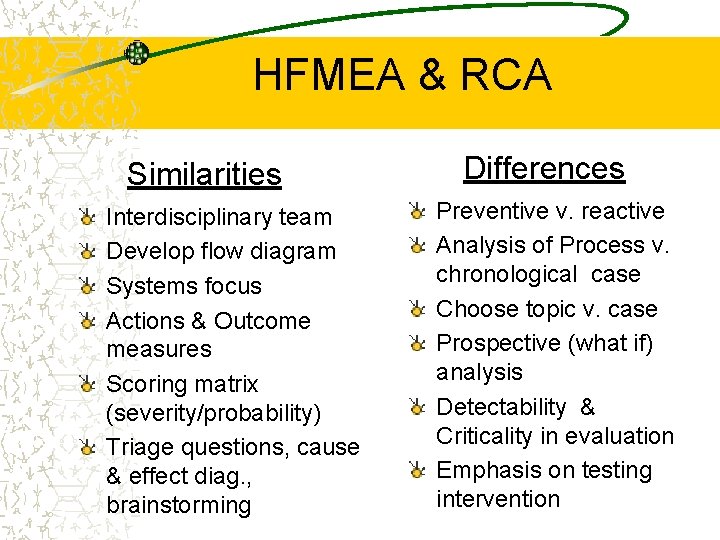
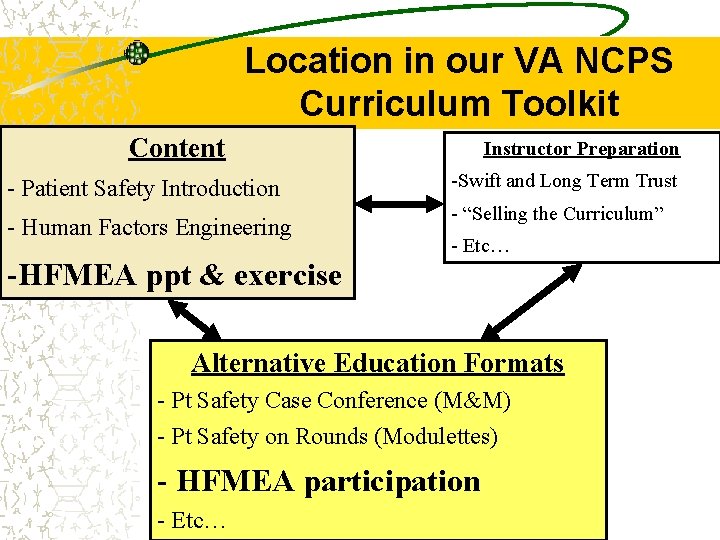
HFMEA & RCA Similarities Interdisciplinary team Develop flow diagram Systems focus Actions & Outcome measures Scoring matrix (severity/probability) Triage questions, cause & effect diag. , brainstorming Differences Preventive v. reactive Analysis of Process v. chronological case Choose topic v. case Prospective (what if) analysis Detectability & Criticality in evaluation Emphasis on testing intervention