Health Impact Assessment Screening Webinar Friday March 4

Health Impact Assessment Screening Webinar Friday March 4, 2011 1
Introductions & Facilitators Participant Introductions Webinar Facilitator Kim Gilhuly, M. P. H. Project Director Human Impact Partners kim@humanimpact. org 510 -740 -0142 2
Agenda HIA Introduction HIA Collaboration HIA Project Examples Screening Description & Key Points Screening Criteria Additional Q&A, Discussion 3
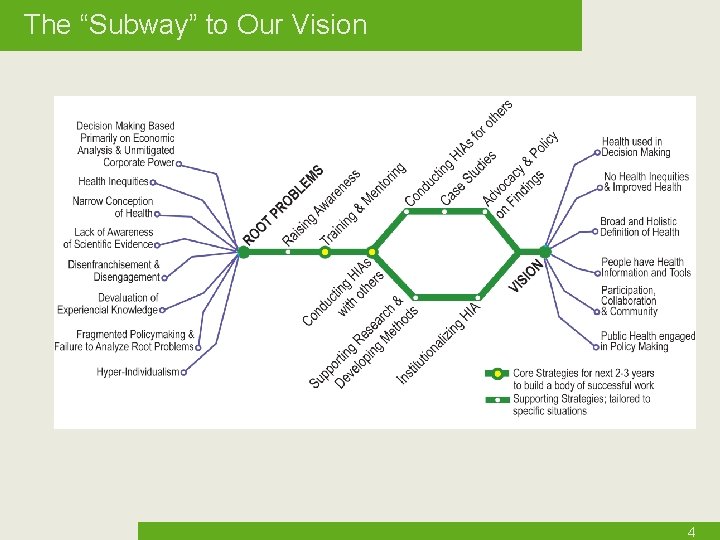
The “Subway” to Our Vision 4
Learning Objectives Participants will: Understand the purpose & process of HIA Review examples of completed HIA projects Understand the role & process of HIA Screening potential policies, regulations, or ordinances to assess in the HIA 5
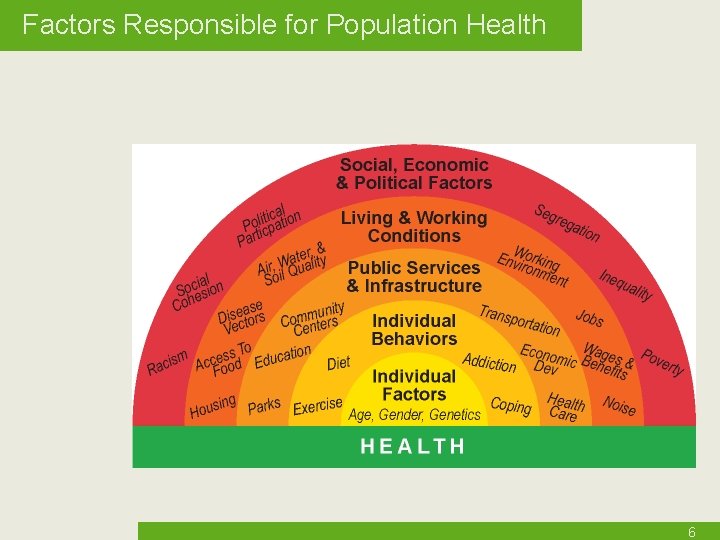
Factors Responsible for Population Health 6
Introduction to Health Impact Assessment Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity. 7

Incorporating Health into Decision-Making The world would look different Development Farm Policy Incarceration Immigration Ports Education 8
Why Health? Limitations to economics-based decision-making Externalities Disparities A health frame can be persuasive People understand health personally Health is an indicator of quality of life and well-being Health is a shared value People are morally outraged by health inequities 9
HIA Definition Health Impact Assessment A combination of procedures, methods and tools that systematically judges the potential, and sometimes unintended, effects of a policy, plan, program or project on the health of a population and the distribution of those effects within the population. HIA identifies appropriate actions to manage those effects. International Association for Impact Assessment, 2006 10
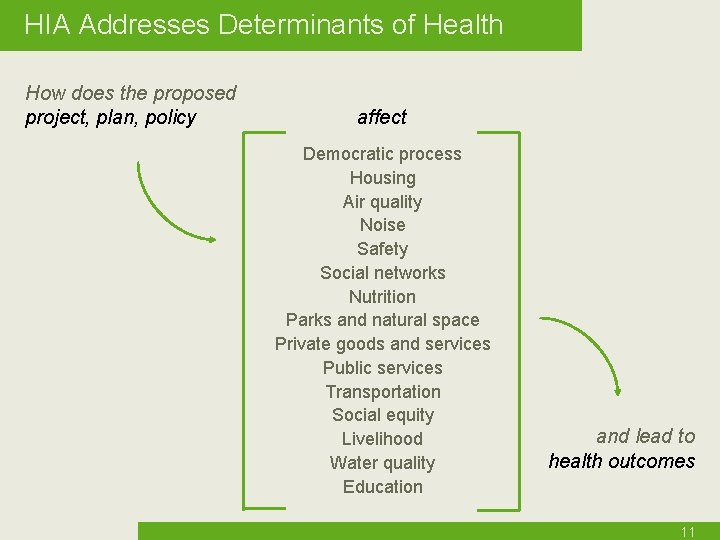
HIA Addresses Determinants of Health How does the proposed project, plan, policy affect Democratic process Housing Air quality Noise Safety Social networks Nutrition Parks and natural space Private goods and services Public services Transportation Social equity Livelihood Water quality Education and lead to health outcomes 11
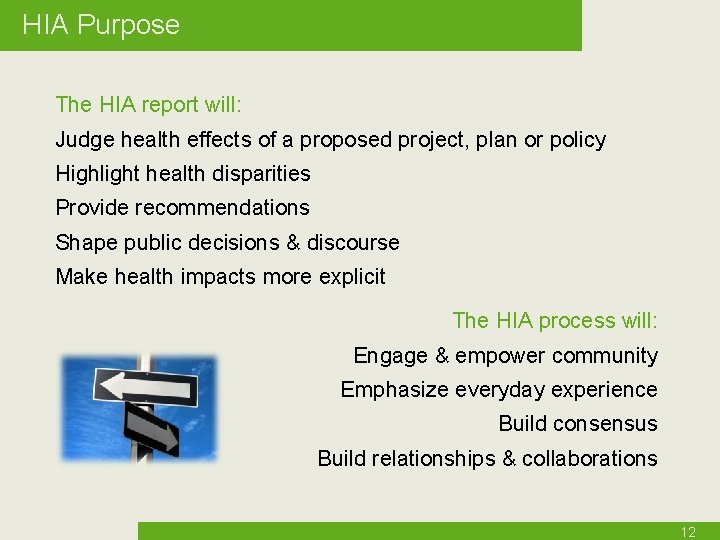
HIA Purpose The HIA report will: Judge health effects of a proposed project, plan or policy Highlight health disparities Provide recommendations Shape public decisions & discourse Make health impacts more explicit The HIA process will: Engage & empower community Emphasize everyday experience Build consensus Build relationships & collaborations 12
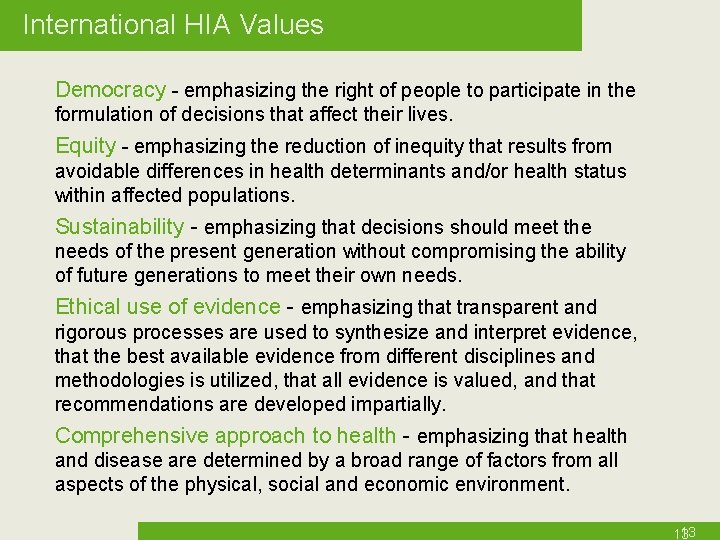
International HIA Values Democracy - emphasizing the right of people to participate in the formulation of decisions that affect their lives. Equity - emphasizing the reduction of inequity that results from avoidable differences in health determinants and/or health status within affected populations. Sustainability - emphasizing that decisions should meet the needs of the present generation without compromising the ability of future generations to meet their own needs. Ethical use of evidence - emphasizing that transparent and rigorous processes are used to synthesize and interpret evidence, that the best available evidence from different disciplines and methodologies is utilized, that all evidence is valued, and that recommendations are developed impartially. Comprehensive approach to health - emphasizing that health and disease are determined by a broad range of factors from all aspects of the physical, social and economic environment. 13 13
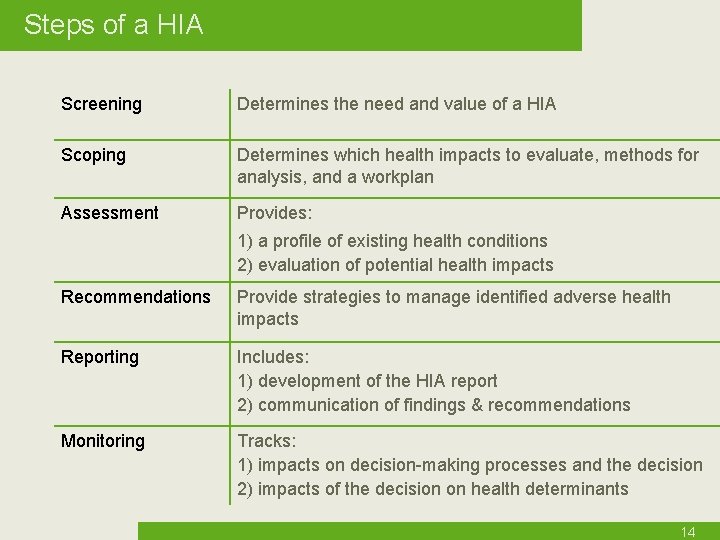
Steps of a HIA Screening Determines the need and value of a HIA Scoping Determines which health impacts to evaluate, methods for analysis, and a workplan Assessment Provides: 1) a profile of existing health conditions 2) evaluation of potential health impacts Recommendations Provide strategies to manage identified adverse health impacts Reporting Includes: 1) development of the HIA report 2) communication of findings & recommendations Monitoring Tracks: 1) impacts on decision-making processes and the decision 2) impacts of the decision on health determinants 14
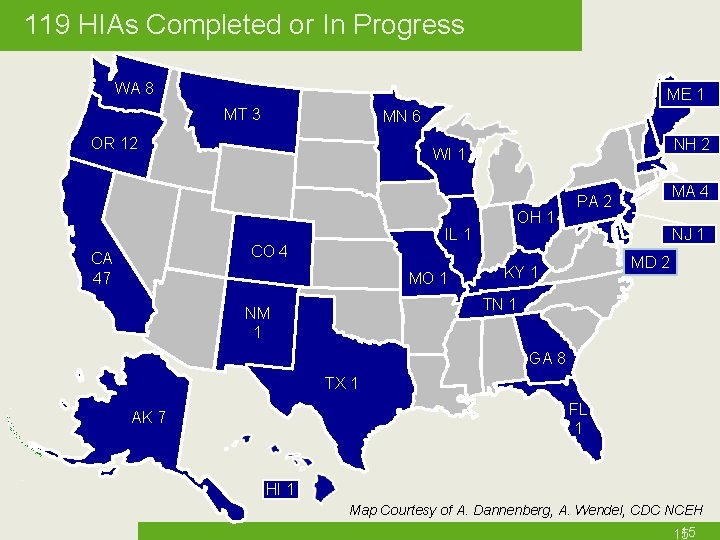
119 HIAs Completed or In Progress WA 8 ME 1 MT 3 MN 6 OR 12 IL 1 CO 4 CA 47 NH 2 WI 1 MO 1 OH 1 MA 4 PA 2 NJ 1 MD 2 KY 1 TN 1 NM 1 GA 8 TX 1 FL 1 AK 7 HI 1 Map Courtesy of A. Dannenberg, A. Wendel, CDC NCEH 15 15
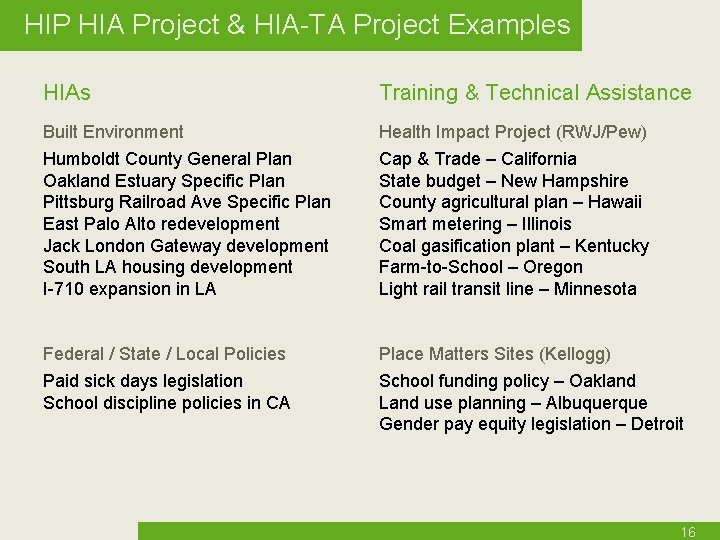
HIP HIA Project & HIA-TA Project Examples HIAs Training & Technical Assistance Built Environment Health Impact Project (RWJ/Pew) Humboldt County General Plan Oakland Estuary Specific Plan Pittsburg Railroad Ave Specific Plan East Palo Alto redevelopment Jack London Gateway development South LA housing development I-710 expansion in LA Cap & Trade – California State budget – New Hampshire County agricultural plan – Hawaii Smart metering – Illinois Coal gasification plant – Kentucky Farm-to-School – Oregon Light rail transit line – Minnesota Federal / State / Local Policies Place Matters Sites (Kellogg) Paid sick days legislation School discipline policies in CA School funding policy – Oakland Land use planning – Albuquerque Gender pay equity legislation – Detroit 16
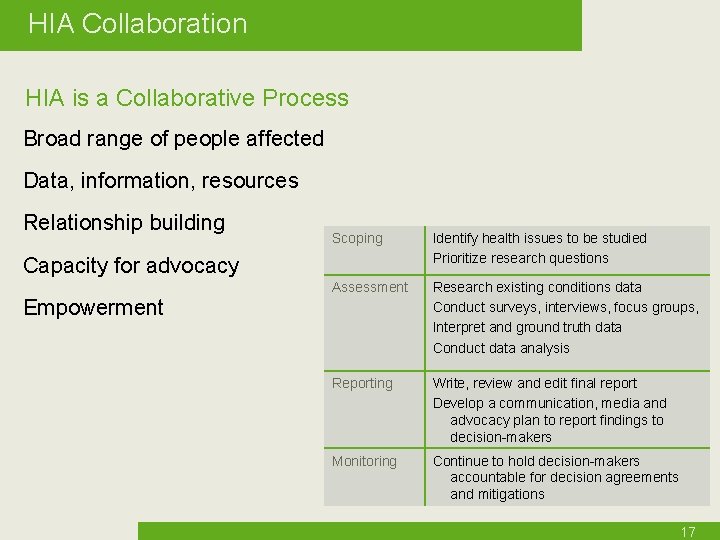
HIA Collaboration HIA is a Collaborative Process Broad range of people affected Data, information, resources Relationship building Scoping Identify health issues to be studied Prioritize research questions Assessment Research existing conditions data Conduct surveys, interviews, focus groups, Interpret and ground truth data Conduct data analysis Reporting Write, review and edit final report Develop a communication, media and advocacy plan to report findings to decision-makers Monitoring Continue to hold decision-makers accountable for decision agreements and mitigations Capacity for advocacy Empowerment 17
Project Example 1 A Health Impact Assessment of the Humboldt County General Plan Update 18
Humboldt Background Proposal Update Humboldt County’s General Plan, including development scenarios to accommodate future growth in the county Collaborators Board of Supervisors Public Health Branch County Planning Department The California Endowment Human Impact Partners Hum. PAL (community organization) 19
Proposed Alternatives Alternative A “Focused growth” All new units built in areas with existing infrastructure 6, 000 units over 25 years Alternative B Build primarily in areas with existing infrastructure Some expansion to areas outside city centers 12, 000 units (6, 000 urban/6, 000 non-urban) Alternative C Requires expansion of infrastructure Allows new housing in outlying areas 18, 000 units (6, 000 urban/12, 000 non-urban) 20
Humboldt Screening Clearly defined decision to be made Decision will impact health Public health involvement invited Resources available Variety of stakeholders interested 21
Humboldt Scoping Process Led by Public Health, Hum. PAL, and HIP Conducted three focus groups with ~50 participants 35 community health indicators used to assess 3 alternatives Healthy housing Safe and sustainable transportation Environmental stewardship Public infrastructure Public safety/Social cohesion Healthy economy 22
Humboldt Assessment For each of the 35 indicators Literature review Collection of existing conditions data Analysis of how 3 alternatives would impact indicators, including vulnerable populations GIS mapping Potential mitigations 23
Data Contributors Humboldt County Public Works Humboldt County Community Development Services California Department of Forestry Humboldt State University UC Davis Agricultural Extension Service First Five Commission Area 1 Agency on Aging Jacoby Creek Land Trust Childcare Planning Council North Coast Unified Air Quality Management District North Coast Emergency Medical Services Humboldt Partnership for Active Living Redwood Community Action Agency Housing and Homeless Coalition Humboldt County Association of Governments Workforce Investment Board California Water Resources Board (North Coast Watershed Assessment Program) City of Arcata Eureka City Schools Assembly member Patty Berg’s office Humboldt Del Norte County Medical Society Northcoast Environmental Center Fisheries Biologists Natural Resources Conservation Service Arcata Soil Survey Office PG&E Department of Health & Human Services 24

Assessment - VMT Example Existing Conditions In Humboldt County, VMT = 27 miles/person/day (2006) California VMT = 24 miles/person/day VMT affects health Collisions, walking/biking, proximity to goods and services, social cohesion, stress, global warming Disparities Seniors may be unable/unwilling to drive Low-income people may not have access to cars or may need to spend large percent of income on driving VMT: Average vehicle miles traveled person per day 25
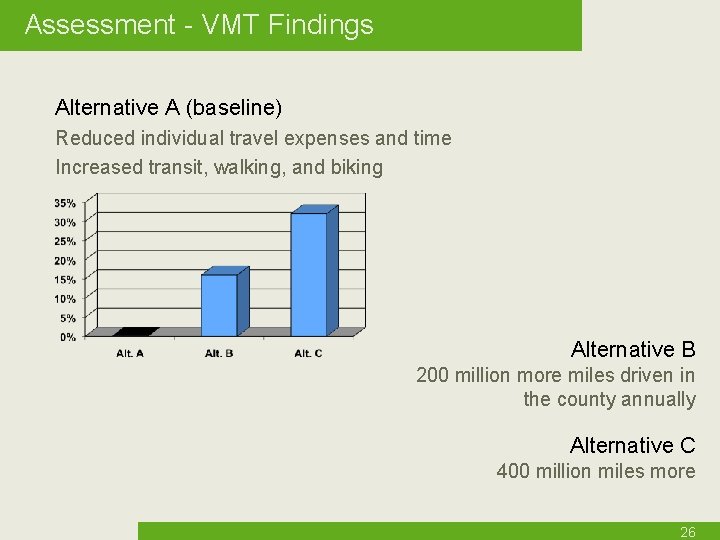
Assessment - VMT Findings Alternative A (baseline) Reduced individual travel expenses and time Increased transit, walking, and biking Alternative B 200 million more miles driven in the county annually Alternative C 400 million miles more 26
Assessment: Transportation Other indicators used for Transportation: • • Average vehicle miles traveled by residents per day Average minutes traveled to work by zip code Proportion of commute trips made by public transit Proportion of households with 1/4 -mile access to local bus Proportion of average income spent on transportation expense Ratio of miles of bike lanes/ pedestrian facilities to road miles Proportion of commute trips and trips to school made by walking or biking Number and rate of bicycle/pedestrian injury collisions Proportion of population living on residential streets with <35 mph speed limits Percent of population who have access to pedestrian facilities 27
Findings: Impacts to Health Higher VMT relates to higher risk of obesity, motor vehicle collision, musculoskeletal pain, and stress, less physical activity and participation with family, friends and in civic life Limited access to goods and services decreases access to health care, contributes to poor diet, and increased transportation expenses Proximity to public transportation predicts use of public transportation. Use of public transportation results in higher levels of physical activity and lower greenhouse gas emissions from automobiles. Urban areas where people use cars less show higher rates of walking and lower rates of obesity and hypertension. Access to safe bike and pedestrian facilities (e. g. sidewalks and wide shoulders on non-urban roads) encourages physical activity. 28
Findings: Transportation Health would be improved most by accommodating future population in areas where residents can most easily access jobs, goods, services, social and cultural events by forms of transportation other than cars, i. e. , in the urban areas where there is an existing infrastructure for these root determinants of health. Plan Alternative A best exemplifies this and is the best option for reducing the ill health effects of excess reliance on cars. 29
Humboldt Recommendations Examples of Transportation-related Recommendations Encourage employer-based incentives for transit Increase public education about public transit Raise priority of non-motorized modes of transport Collect data about pedestrian and bicycle use Establish pedestrian and bicycle routes to schools 30
Humboldt Findings & Outcomes Alternative A: most positive health impacts overall and requires fewest health-related mitigations No decision yet on General Plan Update Recommendations included in Circulation and Housing Elements HIA included as appendix to EIS Built collaboration between planning & public health agencies Built awareness about health and land use among elected officials, general public, planners, community groups Other counties interested in using the approach 31
Project Example 2 A Health Impact Assessment of the 29 th Street Housing Development in South Los Angeles, CA Food Retail Assessment 32
Scope Example: Access to Food Retail Existing Conditions • 37% of area population obese, compared to 21% county-wide • Only 38% of residents surveyed eat fresh fruits and vegetables daily • Studies found less than 75% of markets in South LA sold fresh fruits or vegetables compared to over 90% of stores in more affluent communities, and food quality in S. LA to be inferior • Of over 90 farmers markets in the County, none are in walking distance from project area • Overabundance of fast food and convenience/liquor stores 33
Access to Food Retail: Literature What the literature says The local environment has a direct influence on the type of food options that are available to households and individuals Lack of access to healthy food is one of the barriers, particularly for low-income communities, to healthy eating. Diet-related disease is one of the top sources of preventable deaths among Americans, with the burden of overweight and obesity falling disproportionately on populations with the highest poverty rates • USDHHS. 2001. Surgeon General’s Call to Action to Prevent and Decrease Overweight and Obesity. US Dept of Health and Human Services • Carlson SJ, Andres MS, Bickel GW. 1999. Measuring food insecurity and hunger in the United States: development of a national benchmark and prevalence estimates. J Nutr 129: 510 S-6 S. 34
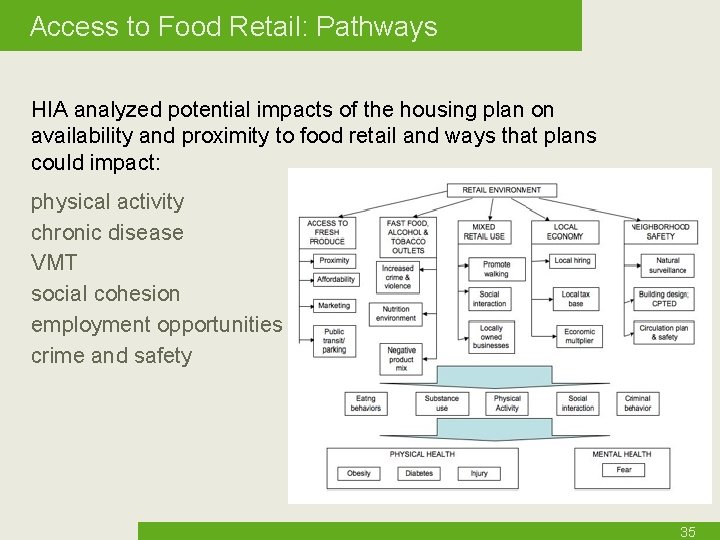
Access to Food Retail: Pathways HIA analyzed potential impacts of the housing plan on availability and proximity to food retail and ways that plans could impact: physical activity chronic disease VMT social cohesion employment opportunities crime and safety 35
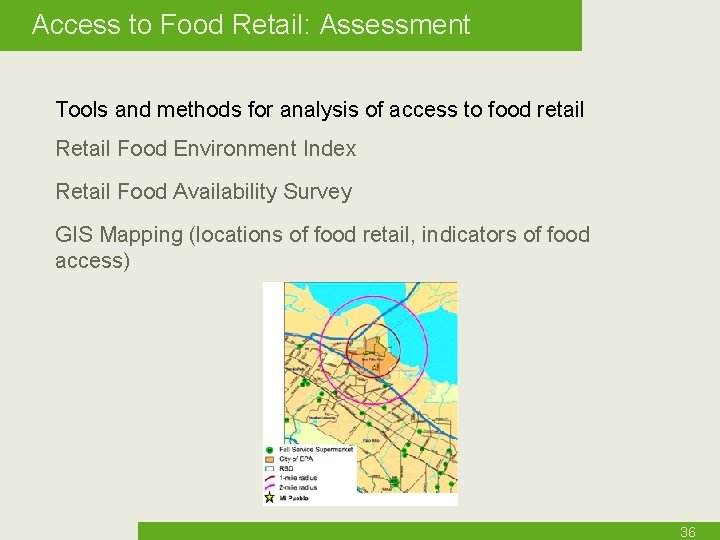
Access to Food Retail: Assessment Tools and methods for analysis of access to food retail Retail Food Environment Index Retail Food Availability Survey GIS Mapping (locations of food retail, indicators of food access) 36

Access to Food Retail: Recommendations Designate space for a small grocery store that sells healthy foods, including fresh produce Consider using multi-purpose space, retail space or the local school to host a farmer’s market Offer a transportation service for residents to access farmers markets and grocery stores where healthy food options are available Advocate for municipal support that promotes store transformations to increases capacity to offer fresh, wholesome foods 37

Massachusetts HIAs Boston Medical Legal Partnership: Child HIA– Rental Voucher Program Child HIA– Low Income Home Energy Assistance Program MA Dept. of Public Health, Environmental Health: HIA of biomass burning facility in Springfield Currently in place: Law stating that transportation projects must include an HIA Local Resources: MA DPH Boston Medical Legal Partnership Northeastern University Institute for Urban Studies 38
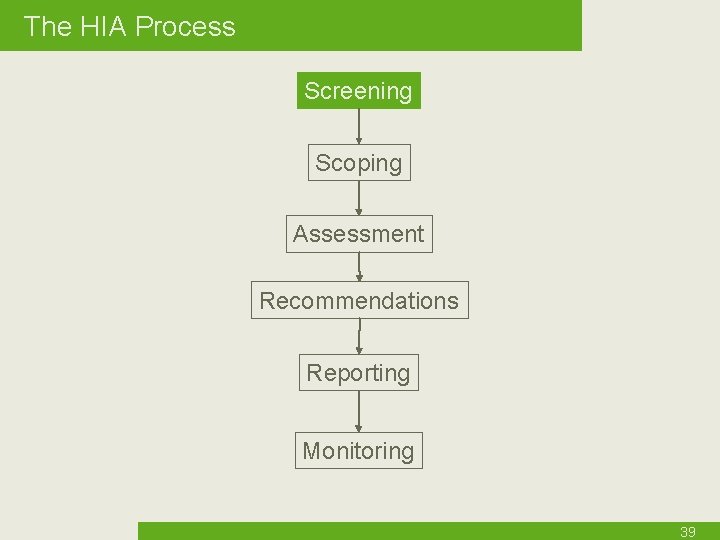
The HIA Process Screening Scoping Assessment Recommendations Reporting Monitoring 39
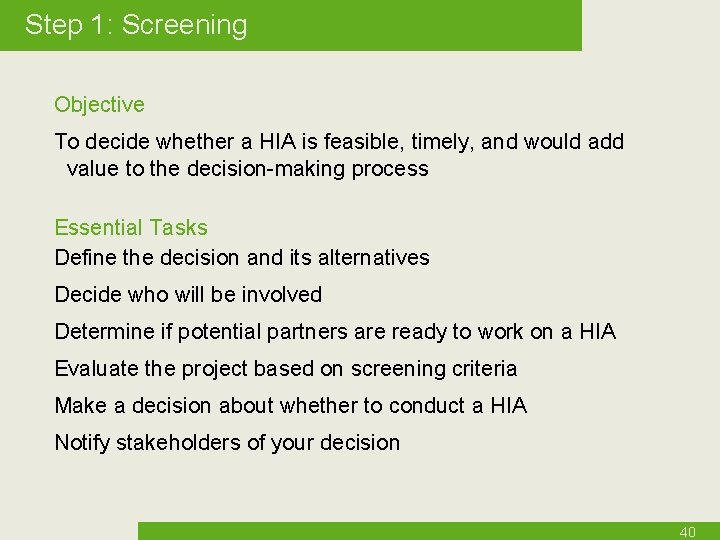
Step 1: Screening Objective To decide whether a HIA is feasible, timely, and would add value to the decision-making process Essential Tasks Define the decision and its alternatives Decide who will be involved Determine if potential partners are ready to work on a HIA Evaluate the project based on screening criteria Make a decision about whether to conduct a HIA Notify stakeholders of your decision 40
Screening Key Points HIA is used to assess a defined project, plan or policy Purpose is to inform decision-makers before they make a decision - as such, HIA is most often carried out prospectively Establish the value of HIA Assess feasibility Understand timing Evaluate decision openness Be inclusive Avoid redundancy 41

Why NOT do a HIA? Example 1 A plan to improve walkability in Chula Vista, CA Plan was already considering health Little opportunity to develop useful recommendations Health advocates involved in design Resources better focused elsewhere 42
Why NOT do a HIA? Example 2 Proposed Wal. Mart distribution center, Merced, CA Idea for the HIA came just before final EIA was released Elected officials not open to considering health Health advocates recommendations were being ignored Resources better used to explore legal options and support the election of more health focused officials 43
Potential HIA Projects to Screen What are some of the local policies related to access to healthy food that you are considering for an HIA? 44
Using Screening Criteria Considering local HIA project ideas, let’s go through some screening criteria 1. The project, plan or policy has been proposed, a final decision about whether to adopt the proposal has not been made, and there is sufficient time to conduct an analysis before the decision is made. 45
Screening Criteria 2. Does the decision have the potential to affect, positively or negatively, environmental or social determinants of health that impact health outcomes of a population? Would health inequities be impacted? In what ways? What are the most important health concerns that could be addressed by a HIA? Would those health impacts be considered without a HIA? 46
Screening Criteria 3. Is the proposal too closely, or too distantly related to health? If applied, would HIA findings and recommendations potentially improve the impact that the project, plan, or policy has on health? 47
Screening Criteria 4. Who are the stakeholders and interest groups involved in the decision-making process? Do they seem to have the interest and the capacity to participate in an HIA? Would stakeholders use the HIA to inform or influence the decision-making process? How? 48
Screening Criteria 5. What are some of the challenges (and by what stakeholders) to change that you might anticipate? 49
Additional Screening Criteria 6. Is the decision-making process open to HIA and/or recommendations for changes to design, mitigations and alternatives? 7. Are there decision alternatives that are more or less advantageous to public health? Would one scenario affect vulnerable populations more than another? 8. Have public concerns about the health impacts of the decision been documented (even if these concerns have not explicitly been stated as health concerns)? 9. Are the proposal’s impacts to health significant in terms of the number of people impacted, the magnitude, breadth and immediacy of impacts? 10. Do data and research methods exist to analyze health impacts of concern associated with this decision? 11. Is it feasible to analyze the health impacts of the decision in the decision-making time frame? What are some barriers to timely completion that you might anticipate? 12. Could the HIA help lead to institutional and/or systemic change? 13. What additional information do you need to decide on the overall value of an HIA in this context? 50

Screening Resources Human Impact Partners. 2009. Considerations for the Selection of Appropriate Policies, Plans, or Projects for Analysis using Health Impact Assessment. www. humanimpact. org/HIA_Screening_White. Paper. pdf Human Impact Partners. HIA Readiness Questions. www. humanimpact. org/HIA_Readiness. Questions_1109. doc Taylor L, Gowman N, Quigley R. Deciding if a Health Impact Assessment Is Required (Screening for HIA). NHS Health Development Agency, 2003. Health Impact Assessment: A Screening Tool for the Greater London Authority. www. londonshealth. gov. uk Merseyside Guidelines for Health Impact Assessment. www. ihia. org. uk 51
Next Steps 1. Policy scan - done prior to today 2. Policy selection process – partially done today 3. Preliminary scoping done by Noho DPH and Noho Planning Dept. 4. Scoping workday – steering committee (Date: ? ) 5. Data collection and analysis done by Noho DPH and Noho Planning Dept. 6. Draft HIA report written 7. Draft HIA report comments from steering committee due: 8. Final HIA released: Date ? 52

Next Steps 53
Questions & Discussion 54
- Slides: 54