Health Family Welfare Department Gandhinagar Gujarat Sickle Cell



- Slides: 29
Health & Family Welfare Department Gandhinagar, Gujarat Sickle Cell Anemia Control Program (A Major Tribal Health Program of Gujarat) Presentation by : Anju Sharma IAS Mission Director (NRHM) Government of Gujarat
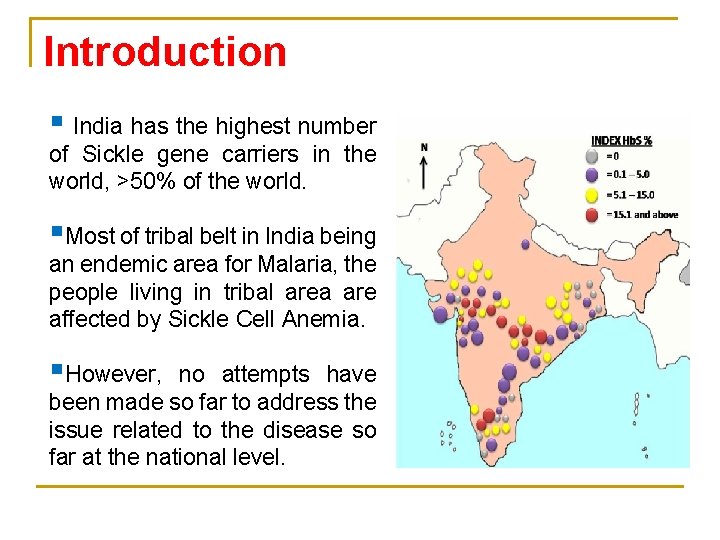
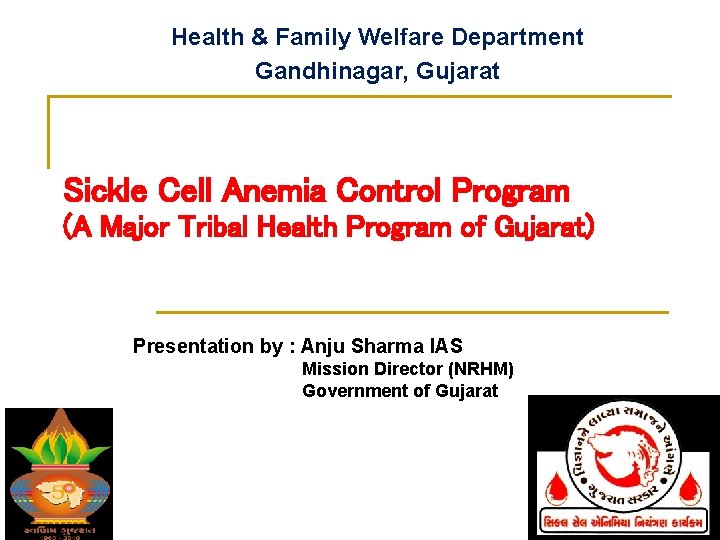
Introduction § India has the highest number of Sickle gene carriers in the world, >50% of the world. §Most of tribal belt in India being an endemic area for Malaria, the people living in tribal area are affected by Sickle Cell Anemia. §However, no attempts have been made so far to address the issue related to the disease so far at the national level.
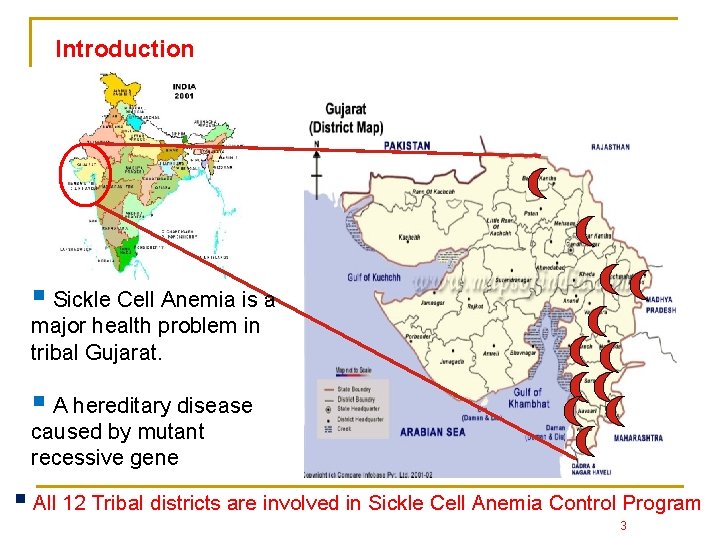
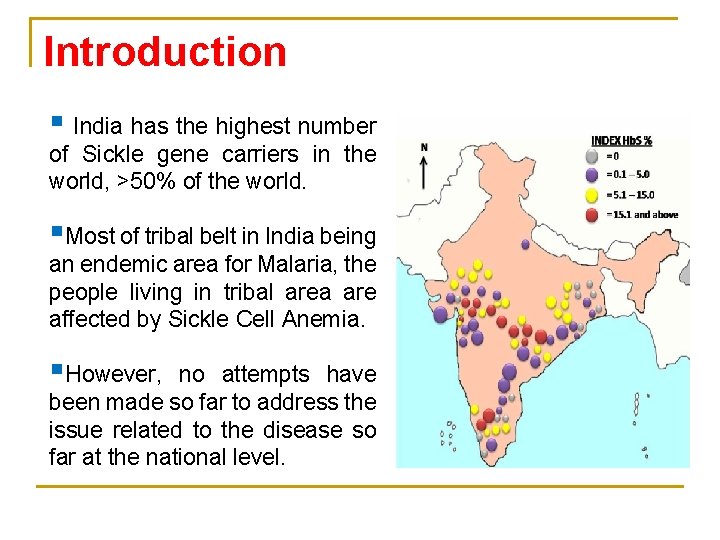
Introduction § Sickle Cell Anemia is a major health problem in tribal Gujarat. § A hereditary disease caused by mutant recessive gene § All 12 Tribal districts are involved in Sickle Cell Anemia Control Program 3
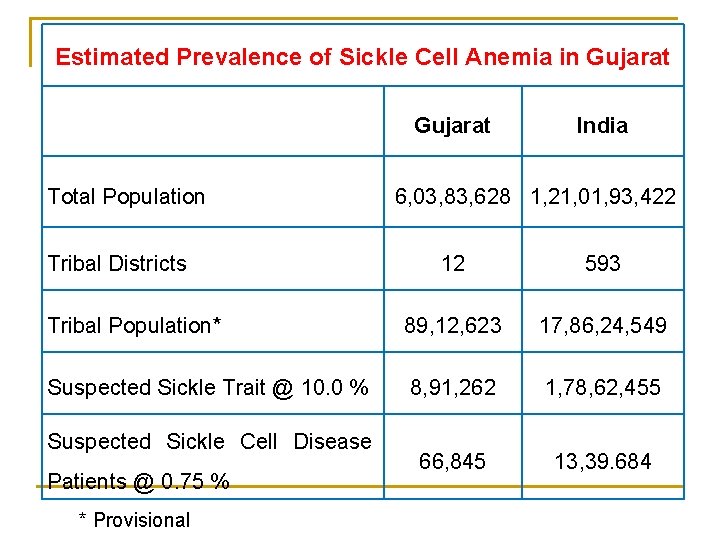
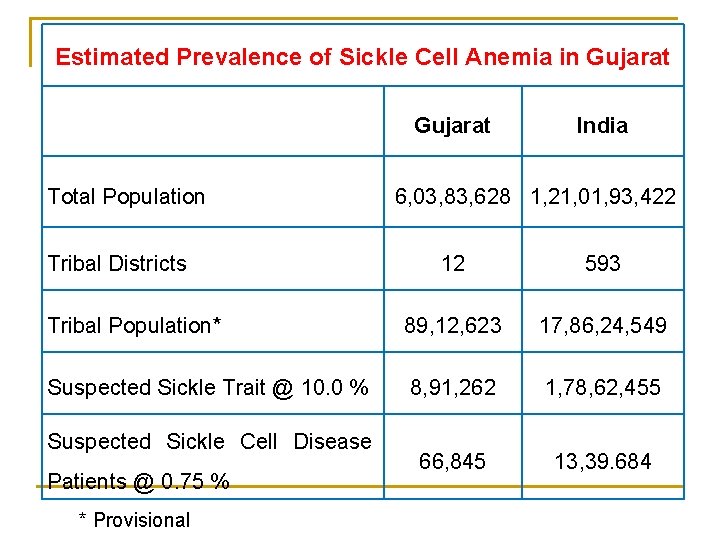
Estimated Prevalence of Sickle Cell Anemia in Gujarat Total Population Tribal Districts India 6, 03, 83, 628 1, 21, 01, 93, 422 12 593 Tribal Population* 89, 12, 623 17, 86, 24, 549 Suspected Sickle Trait @ 10. 0 % 8, 91, 262 1, 78, 62, 455 66, 845 13, 39. 684 Suspected Sickle Cell Disease Patients @ 0. 75 % * Provisional
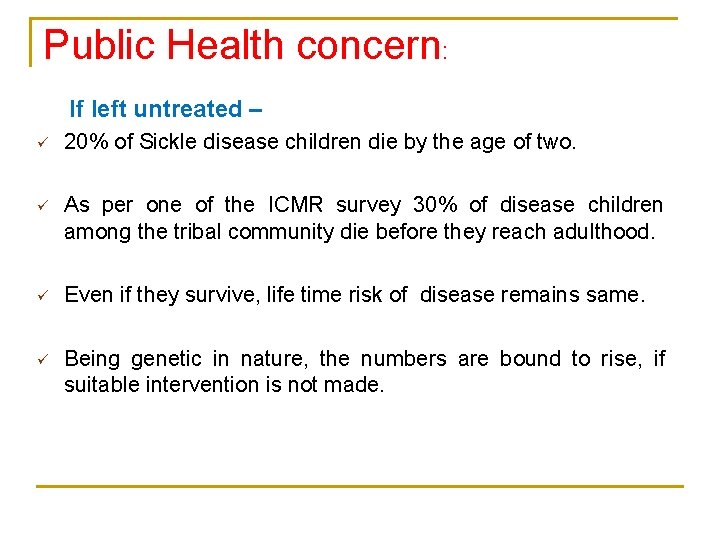
Public Health concern: If left untreated – ü 20% of Sickle disease children die by the age of two. ü As per one of the ICMR survey 30% of disease children among the tribal community die before they reach adulthood. ü Even if they survive, life time risk of disease remains same. ü Being genetic in nature, the numbers are bound to rise, if suitable intervention is not made.
Sickle Cell Anemia Control Program – Gujarat Initiative: In the year 2006, the Department of Health & Family Welfare, Government of Gujarat initiated a Public Private Partnership - Sickle Cell Anemia Control Program in 5 districts of south Gujarat. Now by 2010 -11, it has been extended to all 12 tribal districts of Gujarat and Gujarat Sickle Cell Anemia Control Society has been formed under society registration act 21 of 1860. 6
GOALS: § No Sickle Cell Disease childbirth by 2020. § Prevention of death from Sickle Cell Crisis. § To improve health status and quality of life of Sickle Cell Anemia patients.
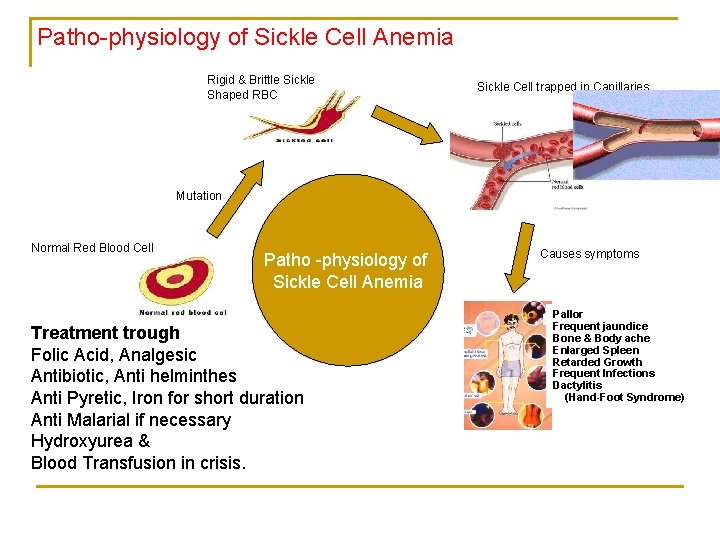
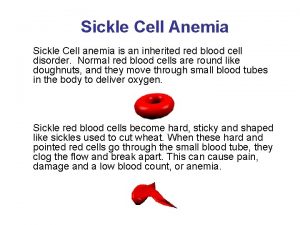
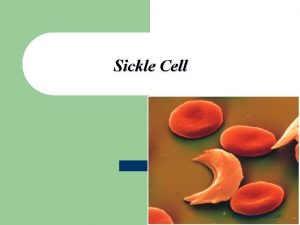
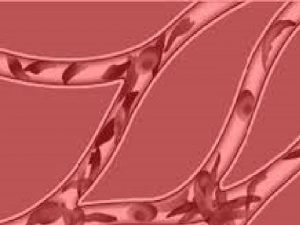
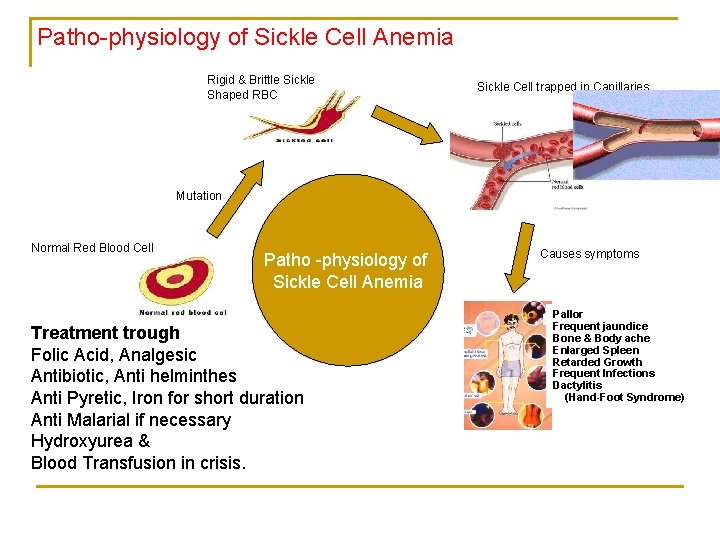
Patho-physiology of Sickle Cell Anemia Rigid & Brittle Sickle Shaped RBC Sickle Cell trapped in Capillaries Mutation Normal Red Blood Cell Patho -physiology of Sickle Cell Anemia Treatment trough Folic Acid, Analgesic Antibiotic, Anti helminthes Anti Pyretic, Iron for short duration Anti Malarial if necessary Hydroxyurea & Blood Transfusion in crisis. Causes symptoms Pallor Frequent jaundice Sickle Cell Anemia, Bone & Body ache Hemolytic Jaundice, Enlarged Spleen Joint Pain, etc. Retarded Growth Frequent Infections Dactylitis (Hand-Foot Syndrome)
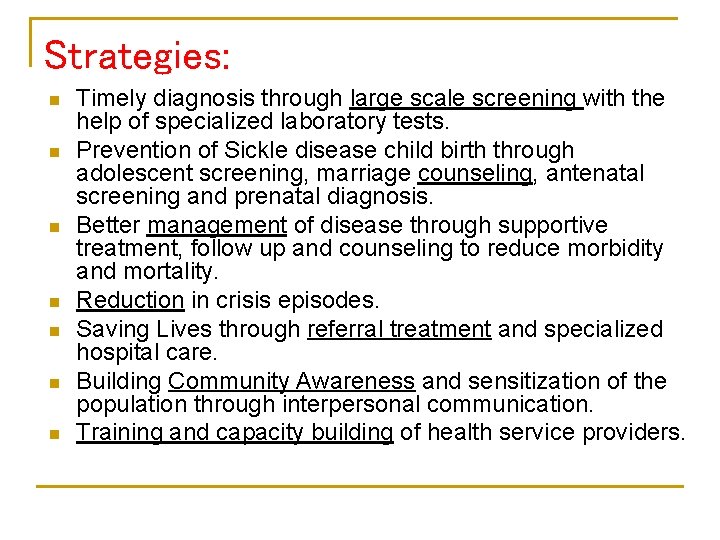
Strategies: n n n n Timely diagnosis through large scale screening with the help of specialized laboratory tests. Prevention of Sickle disease child birth through adolescent screening, marriage counseling, antenatal screening and prenatal diagnosis. Better management of disease through supportive treatment, follow up and counseling to reduce morbidity and mortality. Reduction in crisis episodes. Saving Lives through referral treatment and specialized hospital care. Building Community Awareness and sensitization of the population through interpersonal communication. Training and capacity building of health service providers.
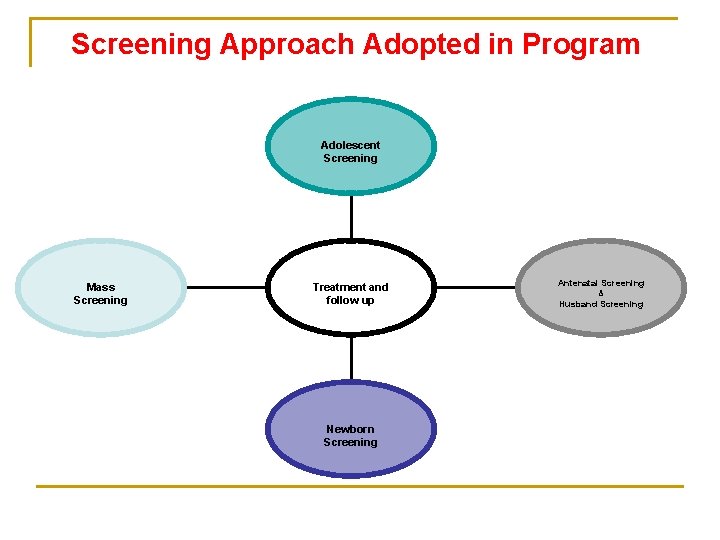
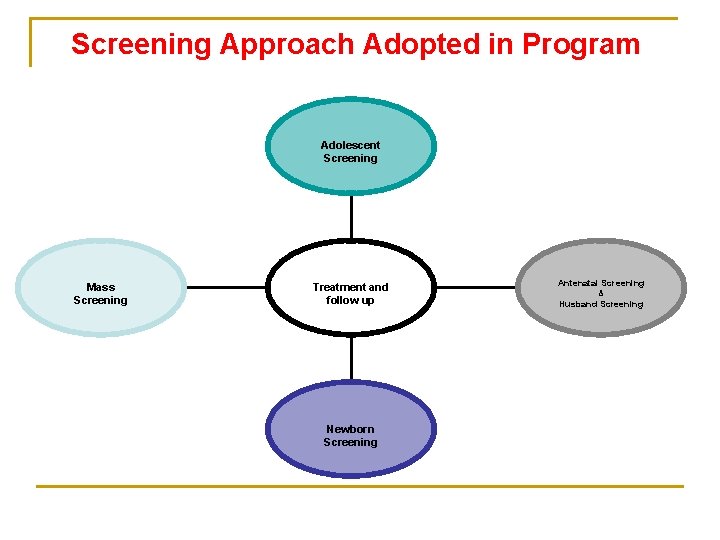
Screening Approach Adopted in Program Adolescent Screening Mass Screening Treatment and follow up Newborn Screening Antenatal Screening & Husband Screening

Institutions involved in the program No. Institutions Year 2006 -07 Year 2011 1 Medical College 1 2 2 General Hospital 3 12 3 PHC 44 333 4 CHC 29 70 5 NGO 1 2 78 419 Total 11
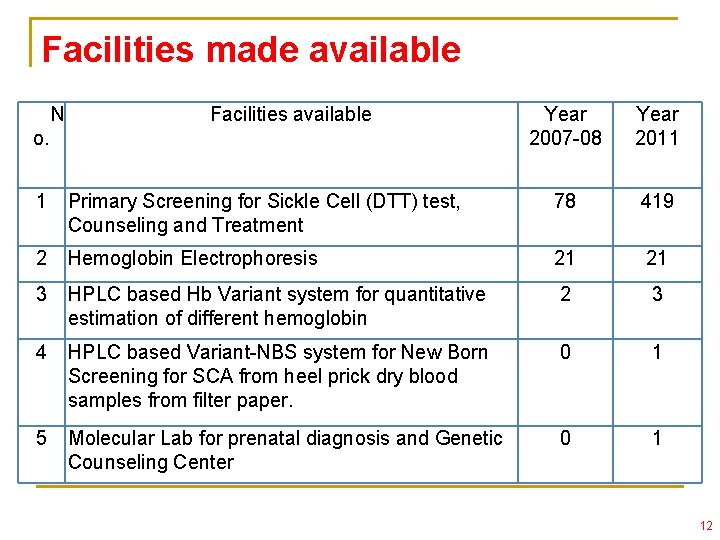
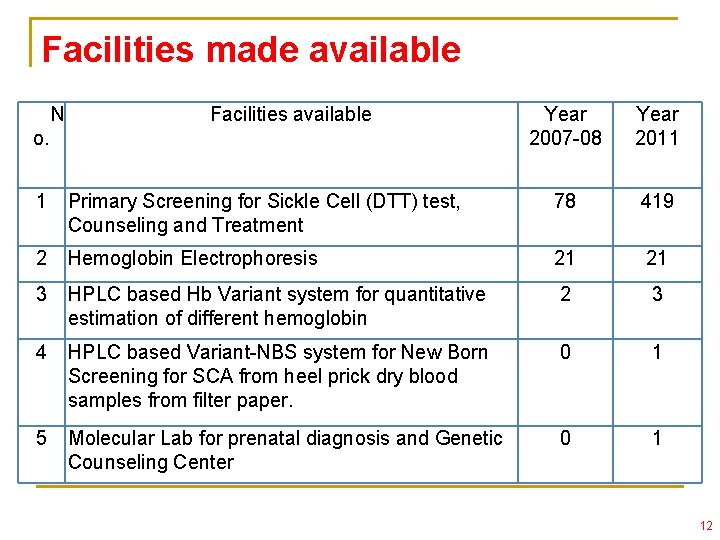
Facilities made available N Facilities available o. Year 2007 -08 Year 2011 1 Primary Screening for Sickle Cell (DTT) test, Counseling and Treatment 78 419 2 Hemoglobin Electrophoresis 21 21 3 HPLC based Hb Variant system for quantitative estimation of different hemoglobin 2 3 4 HPLC based Variant-NBS system for New Born Screening for SCA from heel prick dry blood samples from filter paper. 0 1 5 Molecular Lab for prenatal diagnosis and Genetic Counseling Center 0 1 12
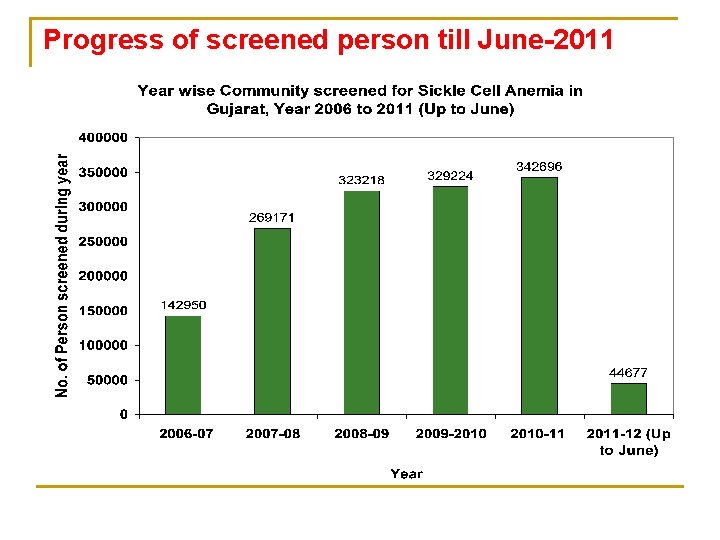
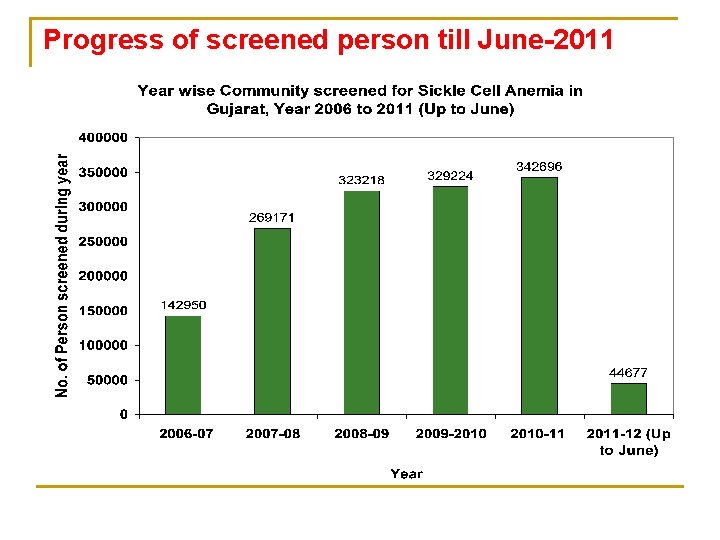
Progress of screened person till June-2011
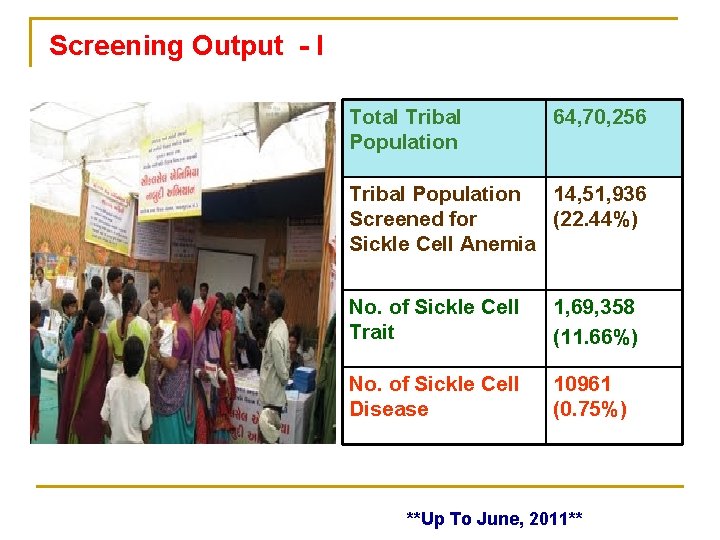
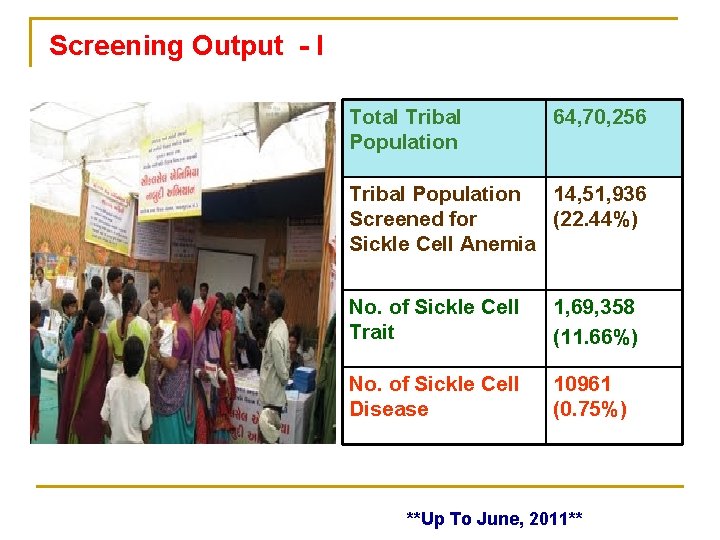
Screening Output - I Total Tribal Population 64, 70, 256 Tribal Population 14, 51, 936 Screened for (22. 44%) Sickle Cell Anemia No. of Sickle Cell Trait 1, 69, 358 (11. 66%) No. of Sickle Cell Disease 10961 (0. 75%) **Up To June, 2011**
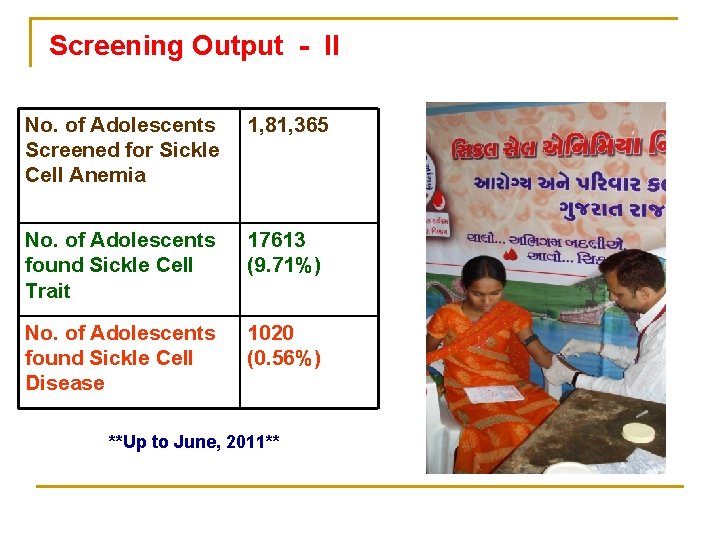
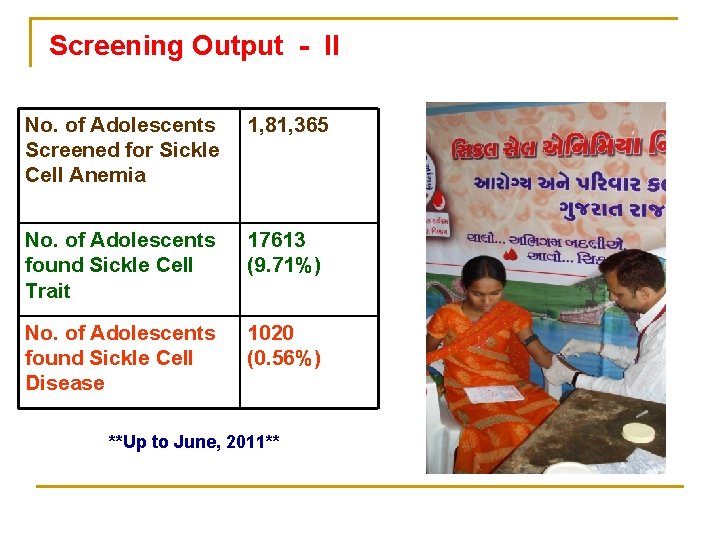
Screening Output - II No. of Adolescents Screened for Sickle Cell Anemia 1, 81, 365 No. of Adolescents found Sickle Cell Trait 17613 (9. 71%) No. of Adolescents found Sickle Cell Disease 1020 (0. 56%) **Up to June, 2011**
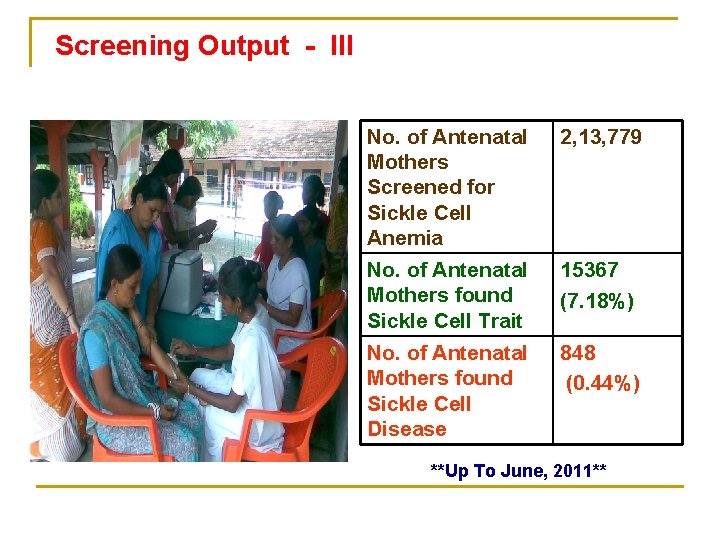
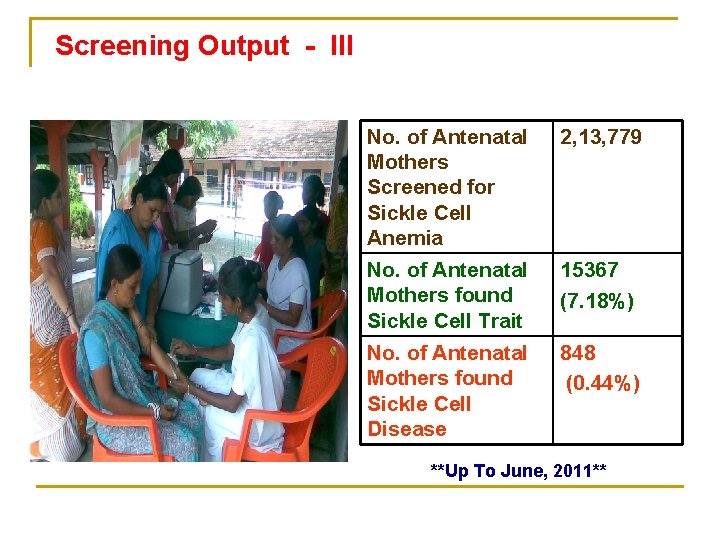
Screening Output - III No. of Antenatal Mothers Screened for Sickle Cell Anemia 2, 13, 779 No. of Antenatal Mothers found Sickle Cell Trait 15367 (7. 18%) No. of Antenatal Mothers found Sickle Cell Disease 848 (0. 44%) **Up To June, 2011**
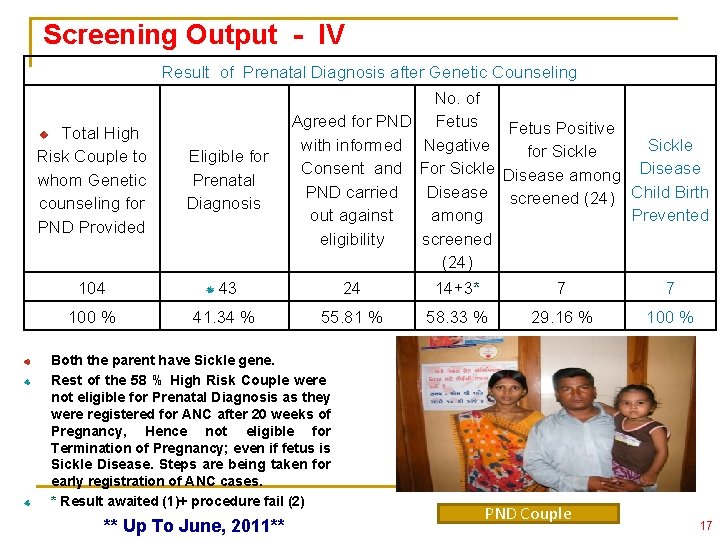
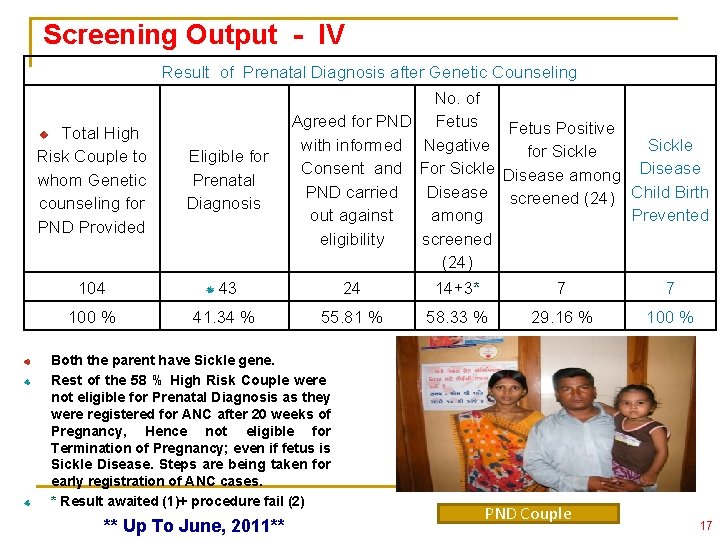
Screening Output - IV Result of Prenatal Diagnosis after Genetic Counseling No. of Agreed for PND Fetus Positive with informed Negative Sickle for Sickle Consent and For Sickle Disease among Disease PND carried Disease screened (24) Child Birth out against Prevented among eligibility screened (24) Total High Risk Couple to whom Genetic counseling for PND Provided Eligible for Prenatal Diagnosis 104 43 24 14+3* 7 7 100 % 41. 34 % 55. 81 % 58. 33 % 29. 16 % 100 % Both the parent have Sickle gene. Rest of the 58 % High Risk Couple were not eligible for Prenatal Diagnosis as they were registered for ANC after 20 weeks of Pregnancy, Hence not eligible for Termination of Pregnancy; even if fetus is Sickle Disease. Steps are being taken for early registration of ANC cases. * Result awaited (1)+ procedure fail (2) ** Up To June, 2011** PND Couple 17
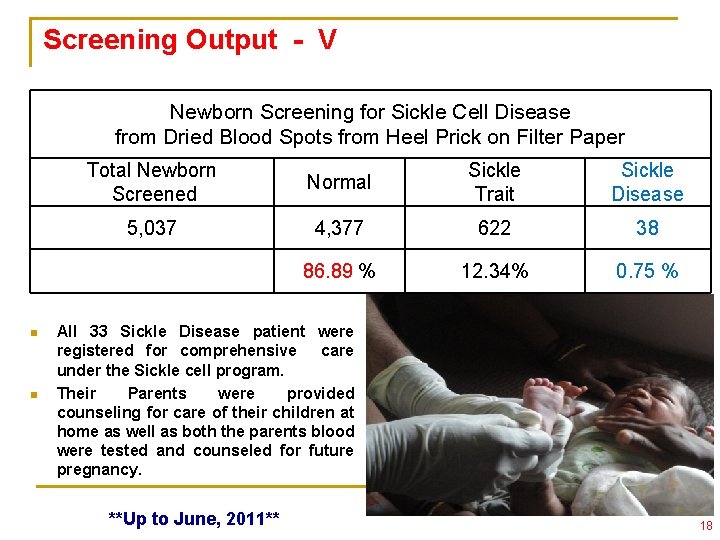
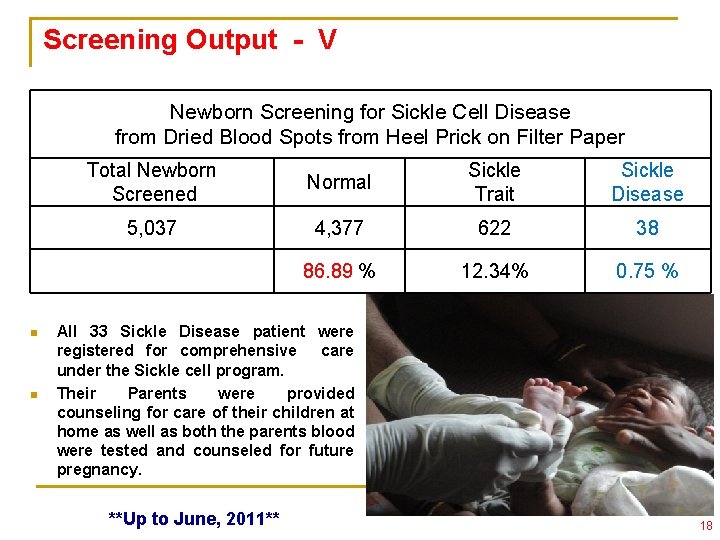
Screening Output - V Newborn Screening for Sickle Cell Disease from Dried Blood Spots from Heel Prick on Filter Paper n n Total Newborn Screened Normal Sickle Trait Sickle Disease 5, 037 4, 377 622 38 86. 89 % 12. 34% 0. 75 % All 33 Sickle Disease patient were registered for comprehensive care under the Sickle cell program. Their Parents were provided counseling for care of their children at home as well as both the parents blood were tested and counseled for future pregnancy. **Up to June, 2011** 18
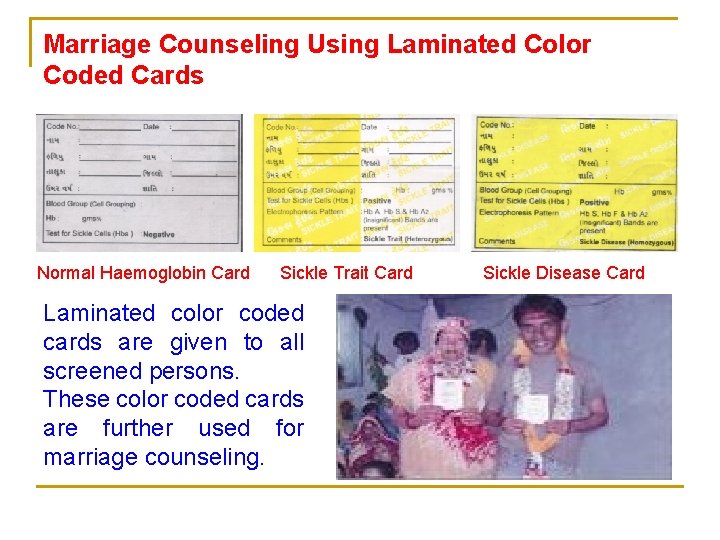
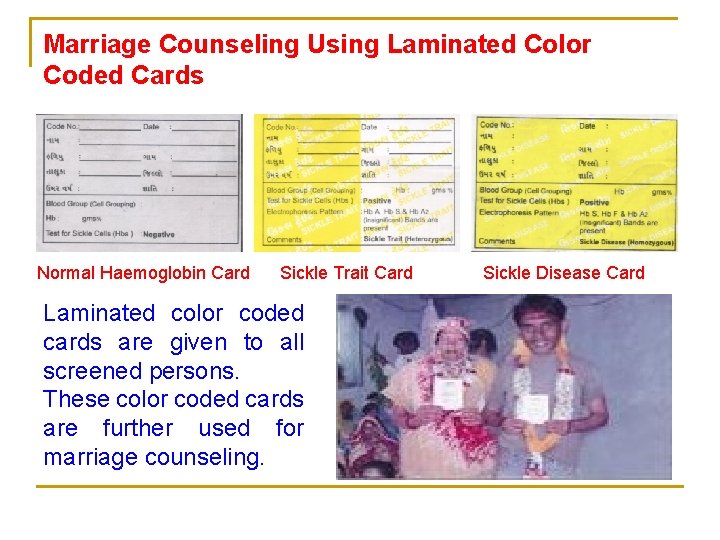
Marriage Counseling Using Laminated Color Coded Cards Normal Haemoglobin Card Sickle Trait Card Laminated color coded cards are given to all screened persons. These color coded cards are further used for marriage counseling. Sickle Disease Card
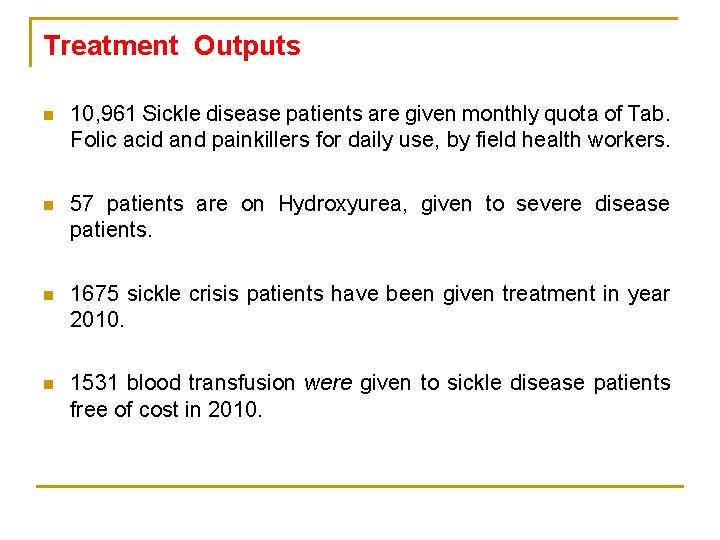
Treatment Outputs n 10, 961 Sickle disease patients are given monthly quota of Tab. Folic acid and painkillers for daily use, by field health workers. n 57 patients are on Hydroxyurea, given to severe disease patients. n 1675 sickle crisis patients have been given treatment in year 2010. n 1531 blood transfusion were given to sickle disease patients free of cost in 2010.
Other Activities v v v v Established network of counseling centers in tribal blocks. Established mechanism for referral and management of Sickle cell crisis patients. Capacity building and training of MPHWs, ANMs, Village Health and Sanitation Committees and PRI representatives. Targeted IEC and BCC Creation of database and regular reporting and monitoring Logistics and inventory management of drugs. Teacher counselling- Students having Sickle Cell Disease have been exempted from physical training and allowed to go to urinals frequently without asking permission.

Outcomes n Many Sickle cell patients are now able to lead normal lives. Mortality and morbidity due to the disease has reduced. n As per survey in 500 sickle cell disease patients, number of crisis has decreased from 2 -3 per year to 1 per year in tribal districts. n Counseling of 17, 613 sickle positive adolescents and for marriage and future pregnancy. Thousands of marriages between sicklers have been avoided in the Tribal Community. Prevented birth of many sickle Cell Diseased children including 7 through PNDT. n Mass Awareness about the disease.
Socio Economic Impact Before Sickle Cell Disease was in books and academic research papers. NOW The Common Tribal People are most benefited. Today they get regular free medicine at their door step, hence there is marked reduction in crisis. Today they have better Life Span & Functional Status than before. The Fruits of the Program have reached to the door step of Underserved– The Tribal People. 24
Impact on Medical Services Before The Medical Practitioners were not aware of sickle phenomena existing among local public. Most of Sickle Disease patients were misdiagnosed and mistreated. Even if Sickle cell was diagnosed, they believed that this is a genetic disease, there is no cure & nothing can be done. Now Awareness among Medical Practitioners has increased dramatically in respect to Diagnosis & Treatment. Marriage counseling, Antenatal Screening and Prenatal Diagnosis are being advised by medical doctors. 25
Extraordinary Features of the program n n n n Reached to the doorstep of most vulnerable tribal population 14, 51, 936. Reduction in the hardship and arresting productivity loss of tribals. Lifecycle approach. Active involvement of NGOs. Community involvement. Capacity building of both Government and NGO staff. Utilization of National and International expertise (ICMR & SCDIO)-Knowledge Sharing, Technical support Application of modern techniques and research in the field situations - Stem cell research etc.
Sustainability: n n n Though the program initially started with NGO participation, it has been now been integrated with the general health services through training and capacity building of the government service providers. Program approach gives wider reach and long term focus. Demand generation from the community due to their sensitization and awareness building. Training and capacity building of private service providers. Mass support to the program.
Replication of the Program at National level n n Taking up a National Program for Sickle Cell Anemia Control. Components: q q q q Population screening for tribal areas through a life cycle approach Color Coded Laminated Cards to all the screened beneficiaries. Training & Capacity building of service providers in screening, disease management and supportive care Free treatment including blood transfusion to all the sicklers. Genetic counseling, patient counseling and sensitisation of the community, family, etc. Community awareness through Mass based campaigns. Involvement of community & NGOs for better community reach. Medical education & research in Sickle Cell Anemia.

Our Indian Sicklers are Born with Pain Live with Pain & Die with Pain. They hardly Complain. Thank you very much for paying attention to our SICKLERS. 29
 Gujarat general administration department
Gujarat general administration department District integrated health and family welfare society
District integrated health and family welfare society Genotypic ratio of monohybrid cross
Genotypic ratio of monohybrid cross Chapter 14 the human genome making karyotypes answer key
Chapter 14 the human genome making karyotypes answer key Life expectancy of sickle cell patients
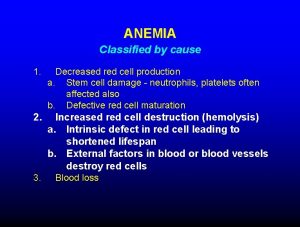
Life expectancy of sickle cell patients Anemia structure
Anemia structure Difference between sickle cell anaemia and thalassemia
Difference between sickle cell anaemia and thalassemia Aplastic crisis
Aplastic crisis Does tiki barber have sickle cell
Does tiki barber have sickle cell Protein synthesis and mutations
Protein synthesis and mutations Pethidine in sickle cell
Pethidine in sickle cell Sickle cell karyotype
Sickle cell karyotype Pedigree key
Pedigree key Sickle cell hemoglobin structure
Sickle cell hemoglobin structure Types of sickle cell disease
Types of sickle cell disease Sickle cell punnett square
Sickle cell punnett square Gene therapy for sickle cell disease
Gene therapy for sickle cell disease Is sickle cell anemia codominant
Is sickle cell anemia codominant Sickle cell osteomyelitis
Sickle cell osteomyelitis Blood
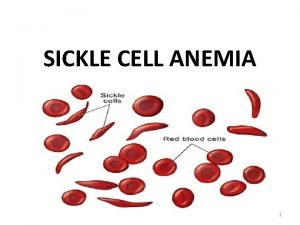
Blood Sickle blood cell
Sickle blood cell Sickle cell anemia
Sickle cell anemia Is sickle cell incomplete dominance
Is sickle cell incomplete dominance Sickle cell anaemia is
Sickle cell anaemia is Old world flycatchers
Old world flycatchers Nata sickle cell
Nata sickle cell Sickle cell anemia
Sickle cell anemia Sickle cell pain
Sickle cell pain Sickle cell anemia symptoms
Sickle cell anemia symptoms Anemia
Anemia