Health care is complex its issues are complicated

- Slides: 28

Health care is complex: its issues are complicated and solutions in some cases are not clear — as the 2012 election nears, health reform takes center stage Dr. Paul Keckley, Executive Director for the Deloitte Center for Health Solutions shares ten myths about the health reform debate
1 Most Americans like our current system. They want the current system protected at all costs. Facts: • The majority of Americans think the current system is inefficient, expensive, and wasteful • The public is increasingly concerned about its costs • Our polls say the public wants to see the system fixed using technologies that increase efficiency, reduce error, and expand the role of nurses and pharmacists in the delivery of care Source: 2012 Deloitte Survey of U. S. Health Care Consumers Copyright © 2012 Deloitte Development LLC. All rights reserved.
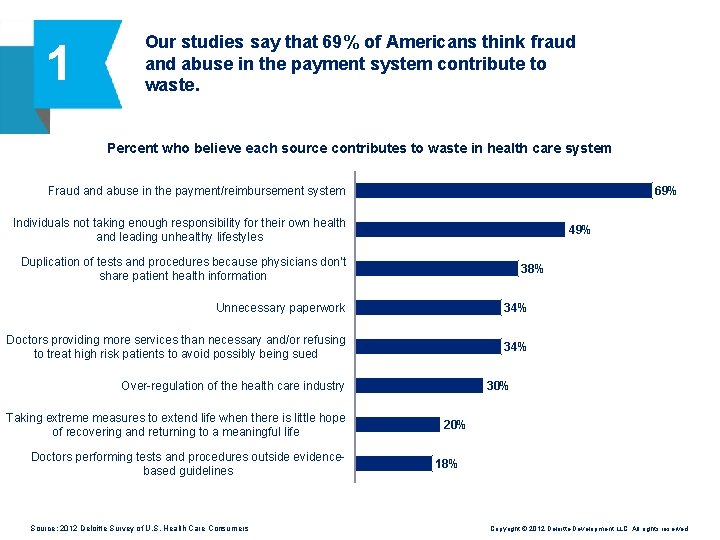
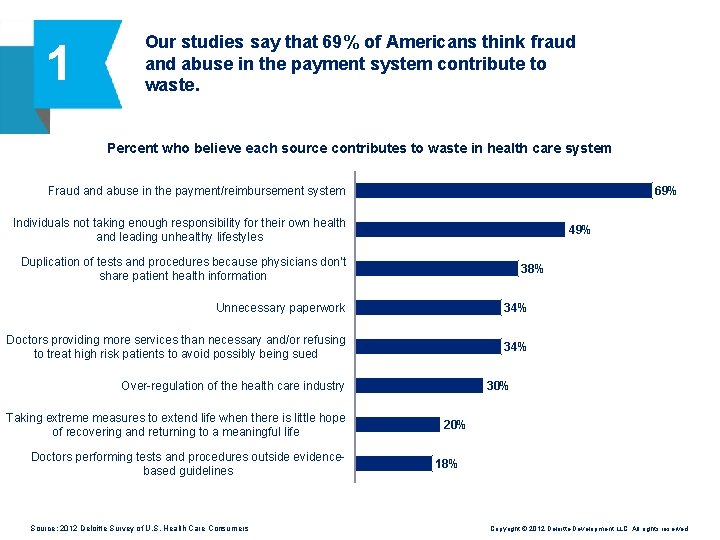
1 Our studies say that 69% of Americans think fraud and abuse in the payment system contribute to waste. Percent who believe each source contributes to waste in health care system Fraud and abuse in the payment/reimbursement system 69% Individuals not taking enough responsibility for their own health and leading unhealthy lifestyles 49% Duplication of tests and procedures because physicians don’t share patient health information 38% Unnecessary paperwork 34% Doctors providing more services than necessary and/or refusing to treat high risk patients to avoid possibly being sued 34% 30% Over-regulation of the health care industry Taking extreme measures to extend life when there is little hope of recovering and returning to a meaningful life Doctors performing tests and procedures outside evidencebased guidelines Source: 2012 Deloitte Survey of U. S. Health Care Consumers 20% 18% Copyright © 2012 Deloitte Development LLC. All rights reserved.
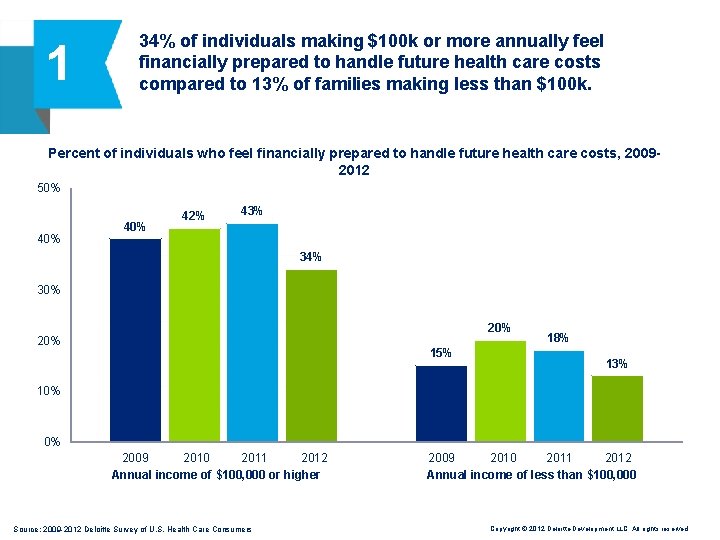
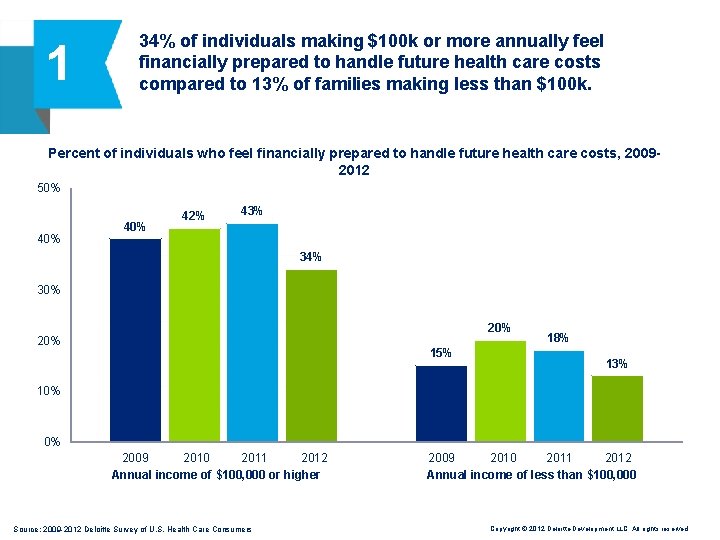
1 34% of individuals making $100 k or more annually feel financially prepared to handle future health care costs compared to 13% of families making less than $100 k. Percent of individuals who feel financially prepared to handle future health care costs, 20092012 50% 40% 42% 43% 34% 30% 20% 15% 18% 13% 10% 0% 2011 2012 2009 2010 Annual income of $100, 000 or higher Source: 2009 -2012 Deloitte Survey of U. S. Health Care Consumers 2009 2010 2011 2012 Annual income of less than $100, 000 Copyright © 2012 Deloitte Development LLC. All rights reserved.
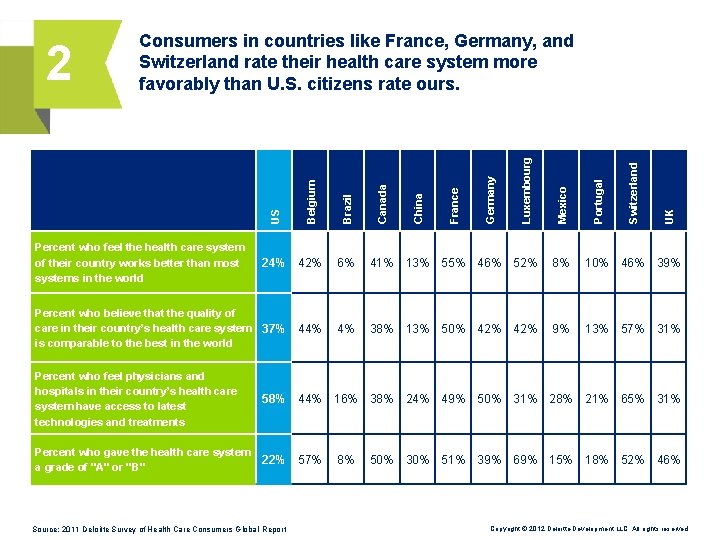
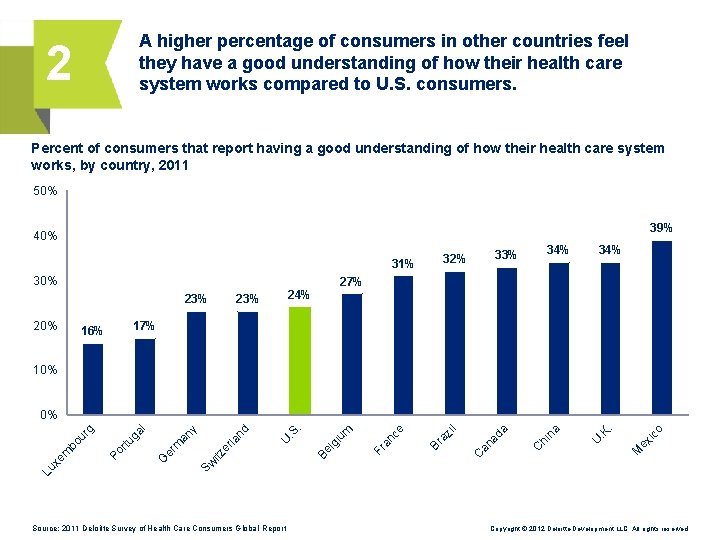
2 Most Americans understand the U. S. system and think it’s better than others. Facts: • Most Americans do not understand are rarely exposed to the complex, “under-the-hood” aspects of our system • It’s more likely that they understand the parts of the system they connect with directly: doctors, hospitals, insurance plans, and the public and private health programs they use in their local communities • Only a handful of consumers have direct knowledge of systems in other countries • Notably, our polls of consumers in countries like France, Germany, Switzerland, and others reveal their constituents understand their systems more and rate their system more favorably than U. S. citizens rate our health care system Copyright © 2012 Deloitte Development LLC. All rights reserved.
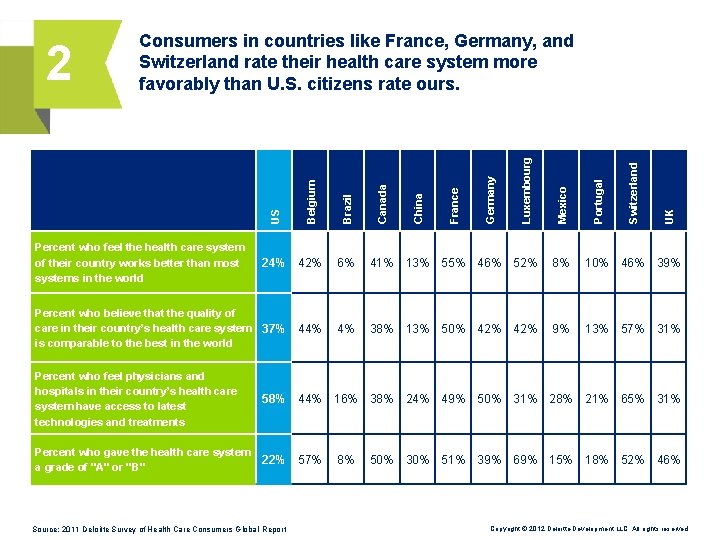
Percent who feel the health care system of their country works better than most systems in the world 24% 42% Percent who believe that the quality of care in their country’s health care system 37% is comparable to the best in the world 44% UK Switzerland Portugal Mexico Luxembourg Germany France China Canada Brazil Belgium US 2 Consumers in countries like France, Germany, and Switzerland rate their health care system more favorably than U. S. citizens rate ours. 6% 41% 13% 55% 46% 52% 8% 10% 46% 39% 4% 38% 13% 50% 42% 9% 13% 57% 31% Percent who feel physicians and hospitals in their country’s health care system have access to latest technologies and treatments 58% 44% 16% 38% 24% 49% 50% 31% 28% 21% 65% 31% Percent who gave the health care system a grade of "A" or "B" 22% 57% Source: 2011 Deloitte Survey of Health Care Consumers Global Report 8% 50% 30% 51% 39% 69% 15% 18% 52% 46% Copyright © 2012 Deloitte Development LLC. All rights reserved.
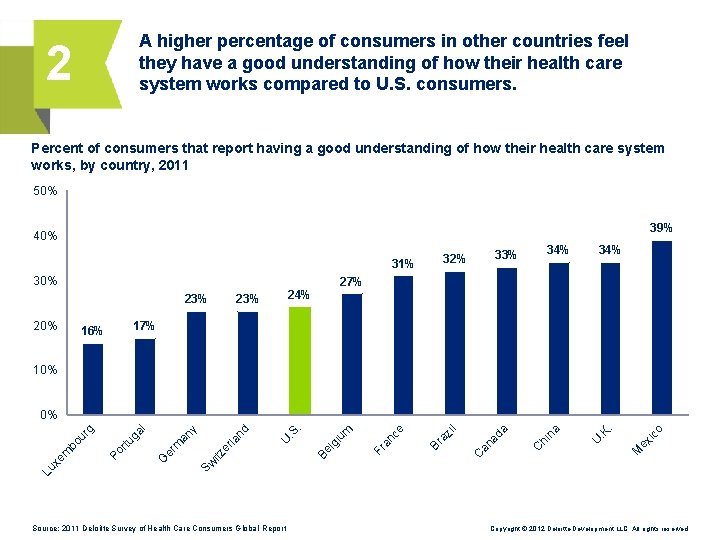
A higher percentage of consumers in other countries feel they have a good understanding of how their health care system works compared to U. S. consumers. 2 Percent of consumers that report having a good understanding of how their health care system works, by country, 2011 50% 39% 40% 31% 30% 34% 33% 32% 34% 27% 23% 20% 24% 23% 17% 16% 10% o . M ex ic . K U a hi n C ad a C an az il Br an ce Fr gi um Be l . . S U la nd er itz er m an y ga l rtu Po G Sw Lu xe m bo ur g 0% Source: 2011 Deloitte Survey of Health Care Consumers Global Report Copyright © 2012 Deloitte Development LLC. All rights reserved.
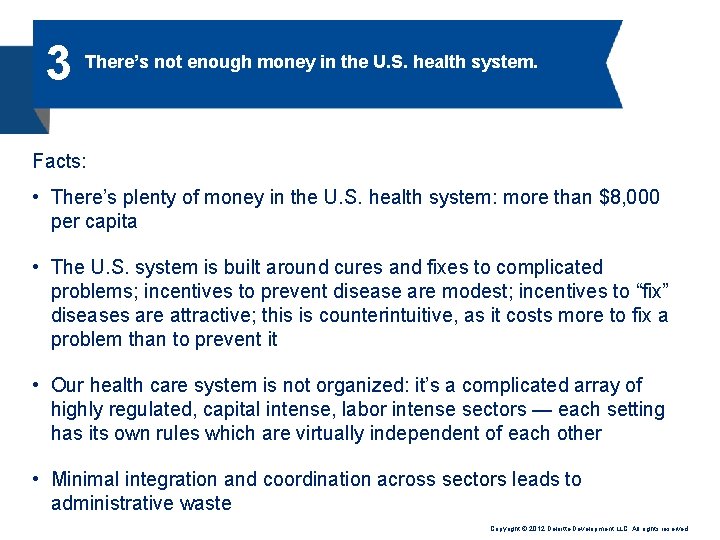
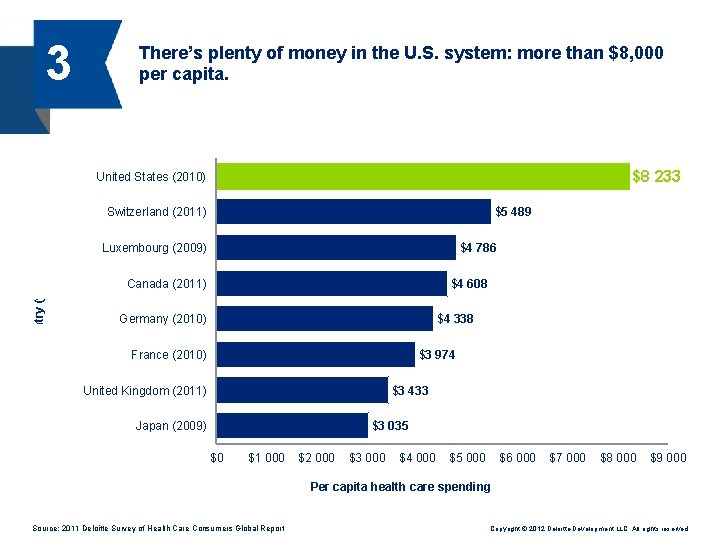
3 There’s not enough money in the U. S. health system. Facts: • There’s plenty of money in the U. S. health system: more than $8, 000 per capita • The U. S. system is built around cures and fixes to complicated problems; incentives to prevent disease are modest; incentives to “fix” diseases are attractive; this is counterintuitive, as it costs more to fix a problem than to prevent it • Our health care system is not organized: it’s a complicated array of highly regulated, capital intense, labor intense sectors — each setting has its own rules which are virtually independent of each other • Minimal integration and coordination across sectors leads to administrative waste Copyright © 2012 Deloitte Development LLC. All rights reserved.
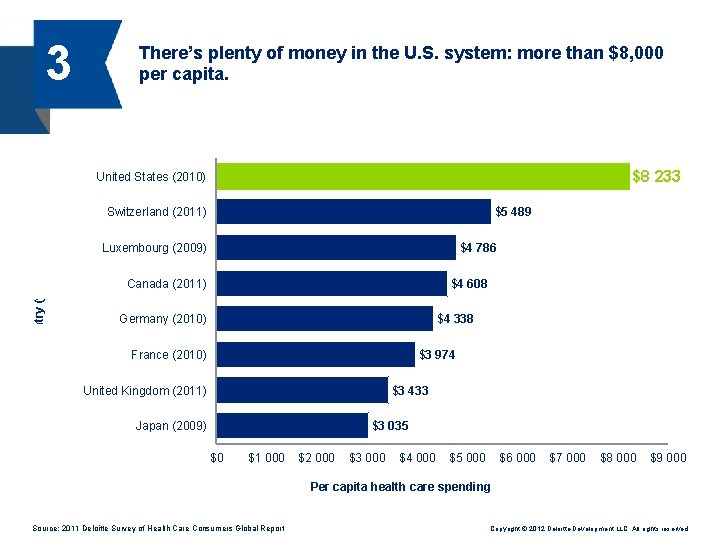
3 There’s plenty of money in the U. S. system: more than $8, 000 per capita. $8 233 United States (2010) Switzerland (2011) $5 489 $4 786 Country (year) Luxembourg (2009) Canada (2011) $4 608 Germany (2010) $4 338 France (2010) $3 974 $3 433 United Kingdom (2011) Japan (2009) $3 035 $0 $1 000 $2 000 $3 000 $4 000 $5 000 $6 000 $7 000 $8 000 $9 000 Per capita health care spending Source: 2011 Deloitte Survey of Health Care Consumers Global Report Copyright © 2012 Deloitte Development LLC. All rights reserved.
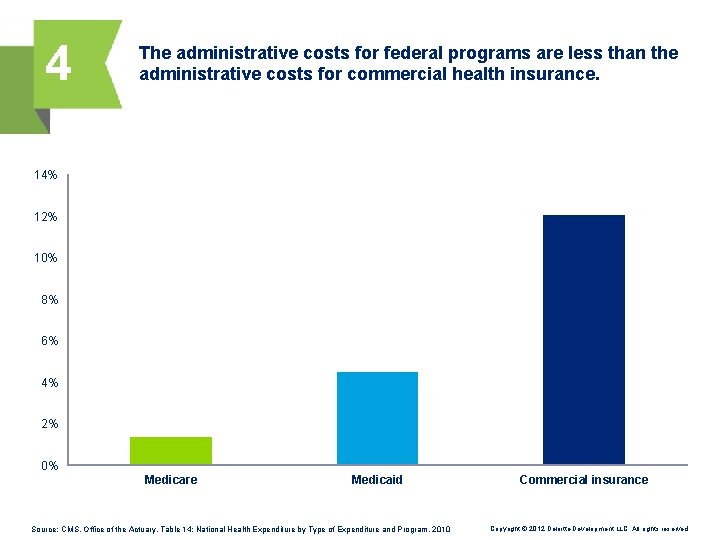
4 Government health care programs — Medicare and Medicaid — are poorly managed and need overhaul. Facts: • Federal and state administrative costs associated with Medicare and Medicaid are less than those associated with commercial health insurance: less than 2% and 5% versus 12%, respectively • Costs of these programs are soaring due to increased enrollment and rising costs of health care utilization • Overhaul of these programs is necessary due to the realities of demand medical inflation, not necessarily the ineptitude of administrators Copyright © 2012 Deloitte Development LLC. All rights reserved.
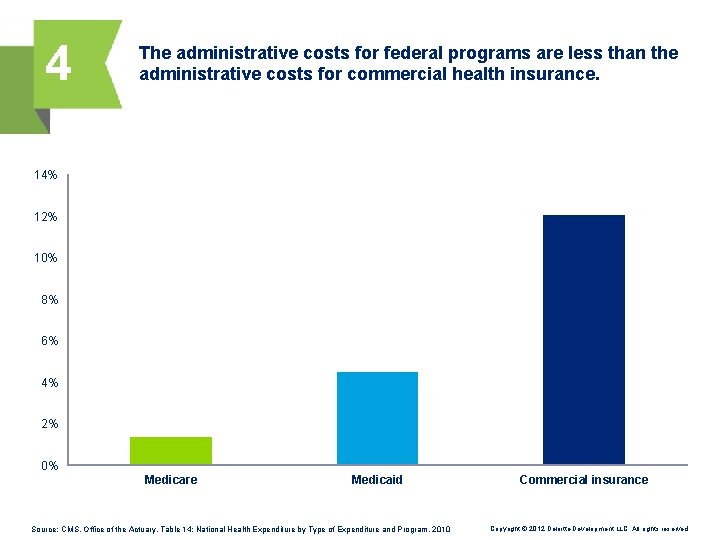
4 The administrative costs for federal programs are less than the administrative costs for commercial health insurance. 14% 12% 10% 8% 6% 4% 2% 0% Medicare Medicaid Source: CMS, Office of the Actuary, Table 14: National Health Expenditure by Type of Expenditure and Program, 2010 Commercial insurance Copyright © 2012 Deloitte Development LLC. All rights reserved.
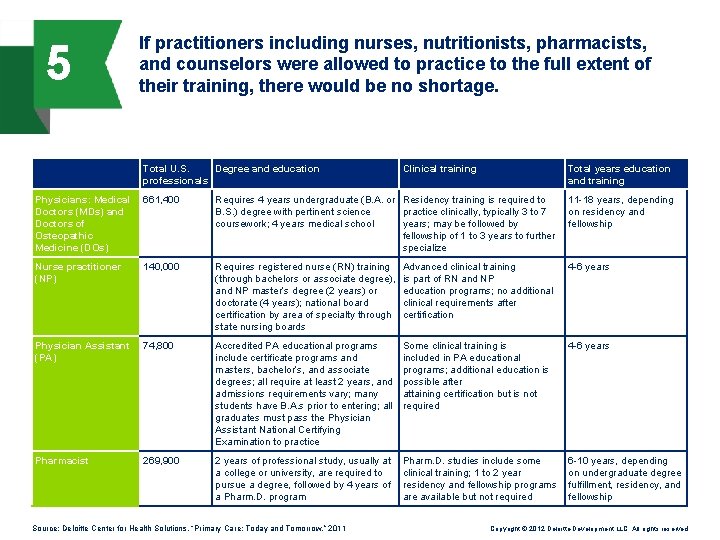
5 There is a shortage of primary care physicians. Facts: • If the presumption is that ONLY MDs/DOs are capable of providing primary care to patients and incentives continue to be based on visits, not results, then the statement is accurate • If new incentives for managing health existed, technologies to enable self-care were accessible, and all practitioners were allowed to practice to the full extent of their training, there might not be a shortage • The myth presumes a reformed system where sick-care and well-care not appropriately balanced and funded Copyright © 2012 Deloitte Development LLC. All rights reserved.
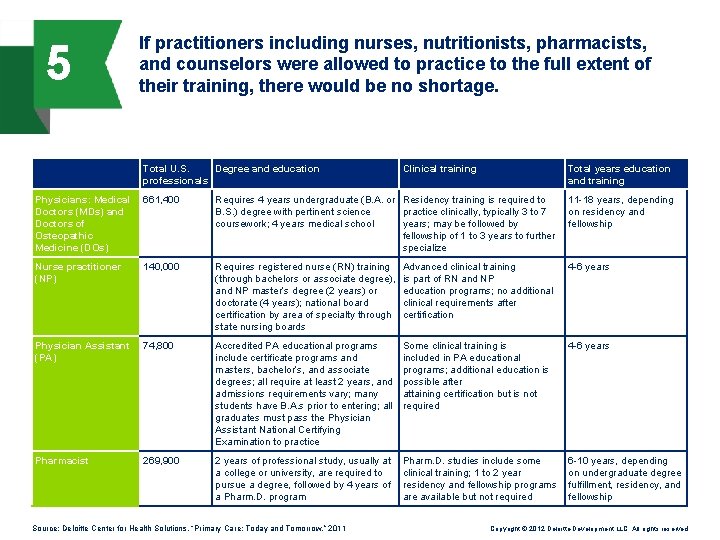
5 If practitioners including nurses, nutritionists, pharmacists, and counselors were allowed to practice to the full extent of their training, there would be no shortage. Total U. S. Degree and education professionals Clinical training Total years education and training Physicians: Medical Doctors (MDs) and Doctors of Osteopathic Medicine (DOs) 661, 400 Requires 4 years undergraduate (B. A. or Residency training is required to B. S. ) degree with pertinent science practice clinically, typically 3 to 7 coursework; 4 years medical school years; may be followed by fellowship of 1 to 3 years to further specialize 11 -18 years, depending on residency and fellowship Nurse practitioner (NP) 140, 000 Requires registered nurse (RN) training (through bachelors or associate degree), and NP master’s degree (2 years) or doctorate (4 years); national board certification by area of specialty through state nursing boards Advanced clinical training is part of RN and NP education programs; no additional clinical requirements after certification 4 -6 years Physician Assistant (PA) 74, 800 Accredited PA educational programs include certificate programs and masters, bachelor’s, and associate degrees; all require at least 2 years, and admissions requirements vary; many students have B. A. s prior to entering; all graduates must pass the Physician Assistant National Certifying Examination to practice Some clinical training is included in PA educational programs; additional education is possible after attaining certification but is not required 4 -6 years Pharmacist 269, 900 2 years of professional study, usually at a college or university, are required to pursue a degree, followed by 4 years of a Pharm. D. program Pharm. D. studies include some clinical training; 1 to 2 year residency and fellowship programs are available but not required 6 -10 years, depending on undergraduate degree fulfillment, residency, and fellowship Source: Deloitte Center for Health Solutions, “Primary Care: Today and Tomorrow, ” 2011 Copyright © 2012 Deloitte Development LLC. All rights reserved.
6 The major driver of health costs is unhealthy lifestyles, and the Affordable Care Act (ACA) doesn’t address this at all. Facts: • Cost associated with chronic diseases and lifestyle choices is only one factor • Other cost drivers include: financial rather than clinical incentives to do more tests and procedures, and the underlying cost of technologies and regulatory compliance • The ACA has a number of provisions that address lifestyle and chronic disease management; beginning in 2014, most health plans will be required to cover preventive wellness and chronic disease management services Copyright © 2012 Deloitte Development LLC. All rights reserved.
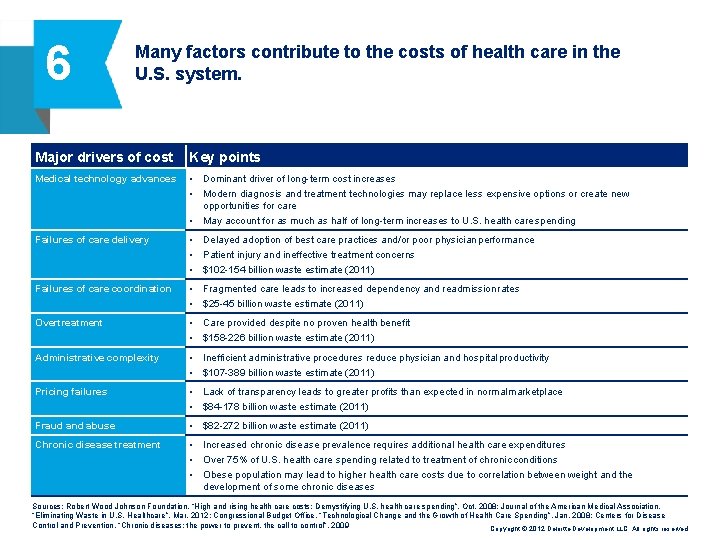
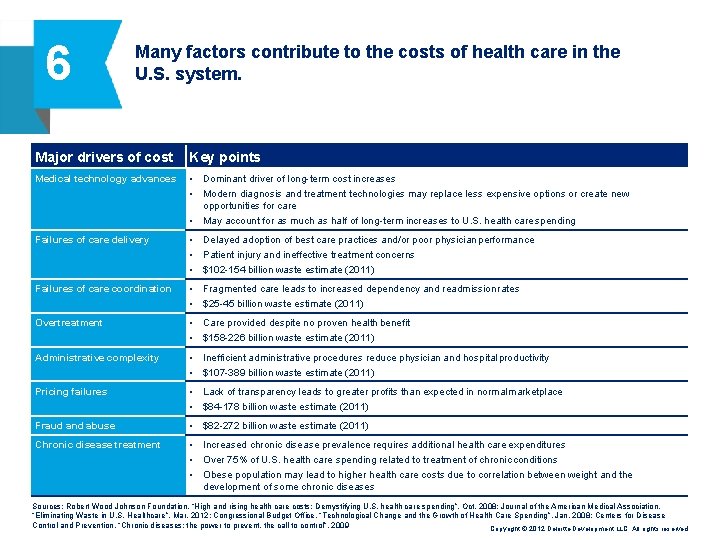
6 Many factors contribute to the costs of health care in the U. S. system. Major drivers of cost Key points Medical technology advances • Dominant driver of long-term cost increases • Modern diagnosis and treatment technologies may replace less expensive options or create new opportunities for care • May account for as much as half of long-term increases to U. S. health care spending Failures of care delivery • Delayed adoption of best care practices and/or poor physician performance • Patient injury and ineffective treatment concerns • $102 -154 billion waste estimate (2011) Failures of care coordination • Fragmented care leads to increased dependency and readmission rates • $25 -45 billion waste estimate (2011) Overtreatment • Care provided despite no proven health benefit • $158 -226 billion waste estimate (2011) Administrative complexity • Inefficient administrative procedures reduce physician and hospital productivity • $107 -389 billion waste estimate (2011) Pricing failures • Lack of transparency leads to greater profits than expected in normal marketplace • $84 -178 billion waste estimate (2011) Fraud and abuse • $82 -272 billion waste estimate (2011) Chronic disease treatment • Increased chronic disease prevalence requires additional health care expenditures • Over 75% of U. S. health care spending related to treatment of chronic conditions • Obese population may lead to higher health care costs due to correlation between weight and the development of some chronic diseases Sources: Robert Wood Johnson Foundation, “High and rising health care costs: Demystifying U. S. health care spending”, Oct. 2008; Journal of the American Medical Association, “Eliminating Waste in U. S. Healthcare”, Mar. 2012; Congressional Budget Office, “Technological Change and the Growth of Health Care Spending”, Jan. 2008; Centers for Disease Control and Prevention, “Chronic diseases: the power to prevent, the call to control”, 2009 Copyright © 2012 Deloitte Development LLC. All rights reserved.
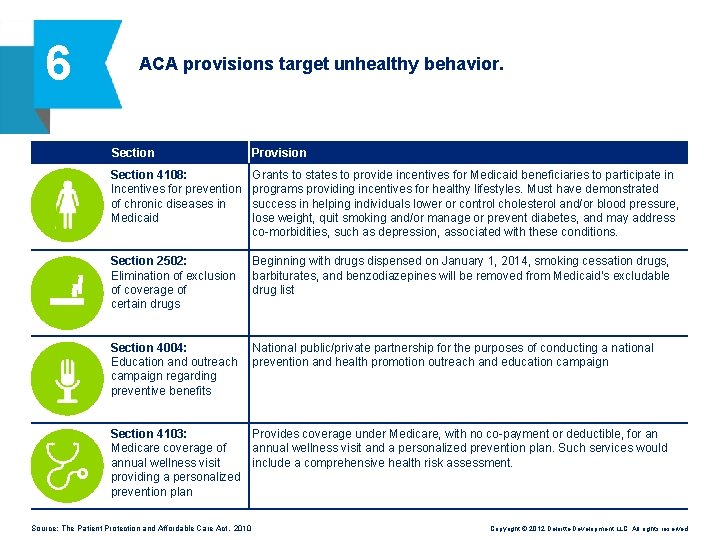
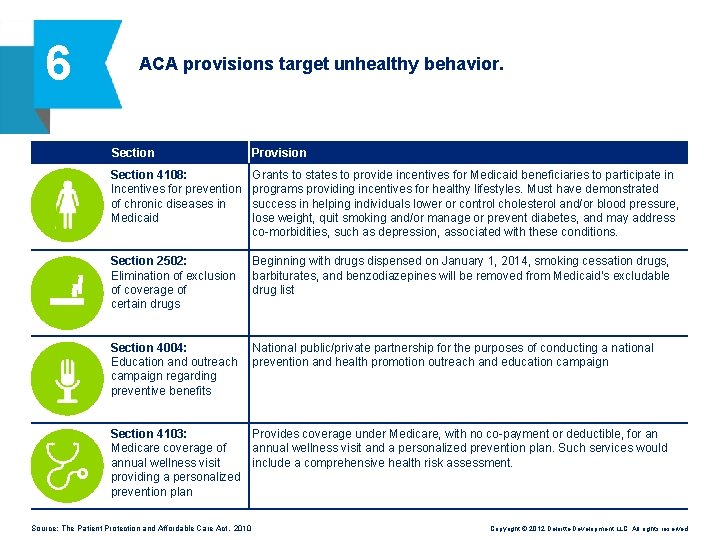
6 ACA provisions target unhealthy behavior. Section Provision Section 4108: Incentives for prevention of chronic diseases in Medicaid Grants to states to provide incentives for Medicaid beneficiaries to participate in programs providing incentives for healthy lifestyles. Must have demonstrated success in helping individuals lower or control cholesterol and/or blood pressure, lose weight, quit smoking and/or manage or prevent diabetes, and may address co-morbidities, such as depression, associated with these conditions. Section 2502: Elimination of exclusion of coverage of certain drugs Beginning with drugs dispensed on January 1, 2014, smoking cessation drugs, barbiturates, and benzodiazepines will be removed from Medicaid’s excludable drug list Section 4004: Education and outreach campaign regarding preventive benefits National public/private partnership for the purposes of conducting a national prevention and health promotion outreach and education campaign Section 4103: Provides coverage under Medicare, with no co-payment or deductible, for an Medicare coverage of annual wellness visit and a personalized prevention plan. Such services would annual wellness visit include a comprehensive health risk assessment. providing a personalized prevention plan Source: The Patient Protection and Affordable Care Act, 2010 Copyright © 2012 Deloitte Development LLC. All rights reserved.
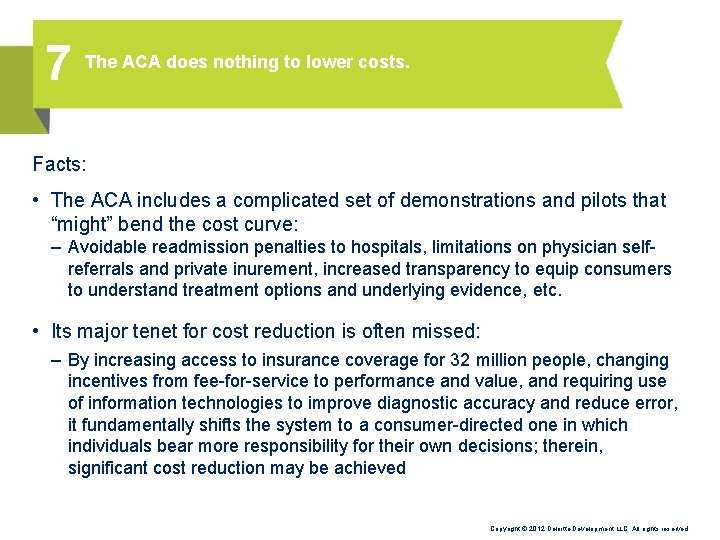
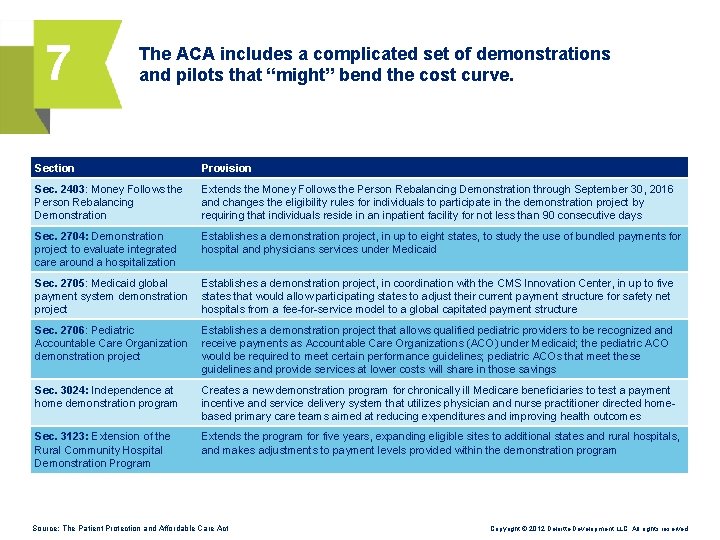
7 The ACA does nothing to lower costs. Facts: • The ACA includes a complicated set of demonstrations and pilots that “might” bend the cost curve: – Avoidable readmission penalties to hospitals, limitations on physician selfreferrals and private inurement, increased transparency to equip consumers to understand treatment options and underlying evidence, etc. • Its major tenet for cost reduction is often missed: – By increasing access to insurance coverage for 32 million people, changing incentives from fee-for-service to performance and value, and requiring use of information technologies to improve diagnostic accuracy and reduce error, it fundamentally shifts the system to a consumer-directed one in which individuals bear more responsibility for their own decisions; therein, significant cost reduction may be achieved Copyright © 2012 Deloitte Development LLC. All rights reserved.
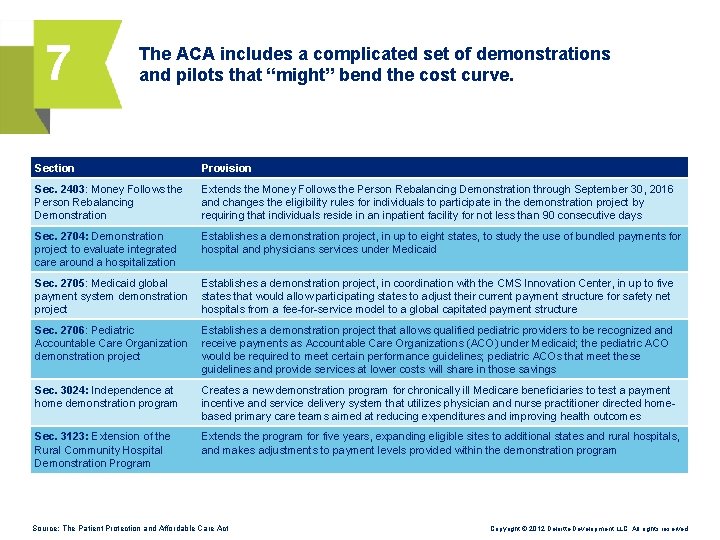
7 The ACA includes a complicated set of demonstrations and pilots that “might” bend the cost curve. Section Provision Sec. 2403: Money Follows the Person Rebalancing Demonstration Extends the Money Follows the Person Rebalancing Demonstration through September 30, 2016 and changes the eligibility rules for individuals to participate in the demonstration project by requiring that individuals reside in an inpatient facility for not less than 90 consecutive days Sec. 2704: Demonstration project to evaluate integrated care around a hospitalization Establishes a demonstration project, in up to eight states, to study the use of bundled payments for hospital and physicians services under Medicaid Sec. 2705: Medicaid global payment system demonstration project Establishes a demonstration project, in coordination with the CMS Innovation Center, in up to five states that would allow participating states to adjust their current payment structure for safety net hospitals from a fee-for-service model to a global capitated payment structure Sec. 2706: Pediatric Accountable Care Organization demonstration project Establishes a demonstration project that allows qualified pediatric providers to be recognized and receive payments as Accountable Care Organizations (ACO) under Medicaid; the pediatric ACO would be required to meet certain performance guidelines; pediatric ACOs that meet these guidelines and provide services at lower costs will share in those savings Sec. 3024: Independence at home demonstration program Creates a new demonstration program for chronically ill Medicare beneficiaries to test a payment incentive and service delivery system that utilizes physician and nurse practitioner directed homebased primary care teams aimed at reducing expenditures and improving health outcomes Sec. 3123: Extension of the Rural Community Hospital Demonstration Program Extends the program for five years, expanding eligible sites to additional states and rural hospitals, and makes adjustments to payment levels provided within the demonstration program Source: The Patient Protection and Affordable Care Act Copyright © 2012 Deloitte Development LLC. All rights reserved.
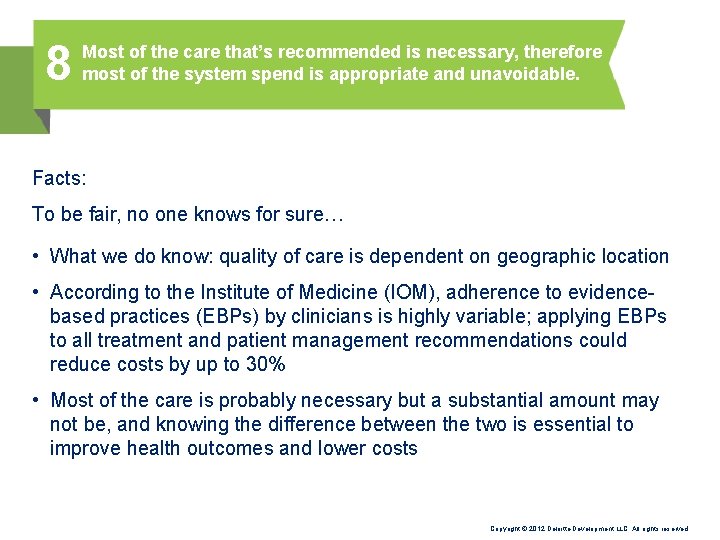
8 Most of the care that’s recommended is necessary, therefore most of the system spend is appropriate and unavoidable. Facts: To be fair, no one knows for sure… • What we do know: quality of care is dependent on geographic location • According to the Institute of Medicine (IOM), adherence to evidencebased practices (EBPs) by clinicians is highly variable; applying EBPs to all treatment and patient management recommendations could reduce costs by up to 30% • Most of the care is probably necessary but a substantial amount may not be, and knowing the difference between the two is essential to improve health outcomes and lower costs Copyright © 2012 Deloitte Development LLC. All rights reserved.
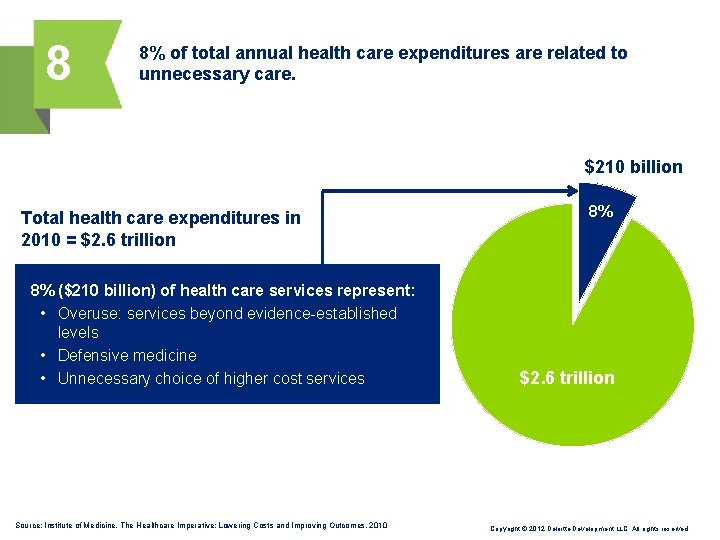
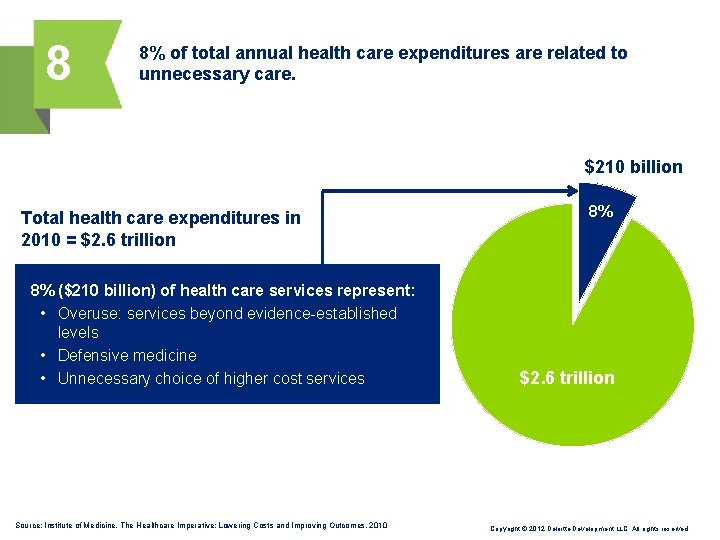
8 8% of total annual health care expenditures are related to unnecessary care. $210 billion Total health care expenditures in 2010 = $2. 6 trillion 8% ($210 billion) of health care services represent: • Overuse: services beyond evidence-established levels • Defensive medicine • Unnecessary choice of higher cost services Source: Institute of Medicine, The Healthcare Imperative: Lowering Costs and Improving Outcomes, 2010 8% $2. 6 trillion Copyright © 2012 Deloitte Development LLC. All rights reserved.
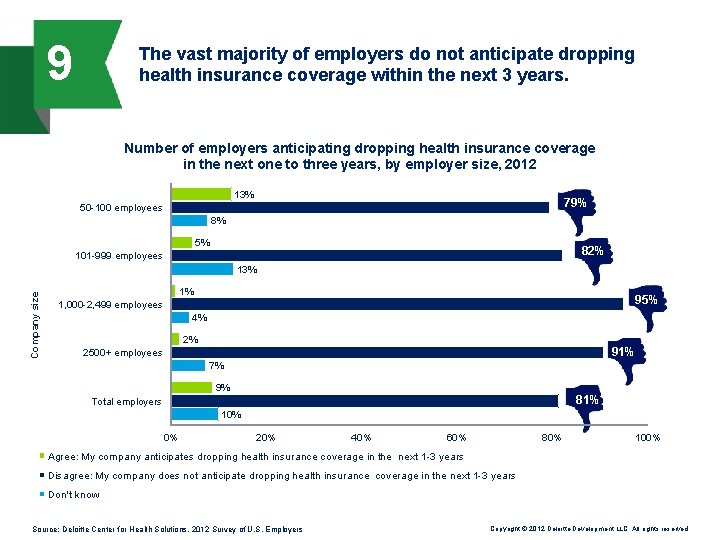
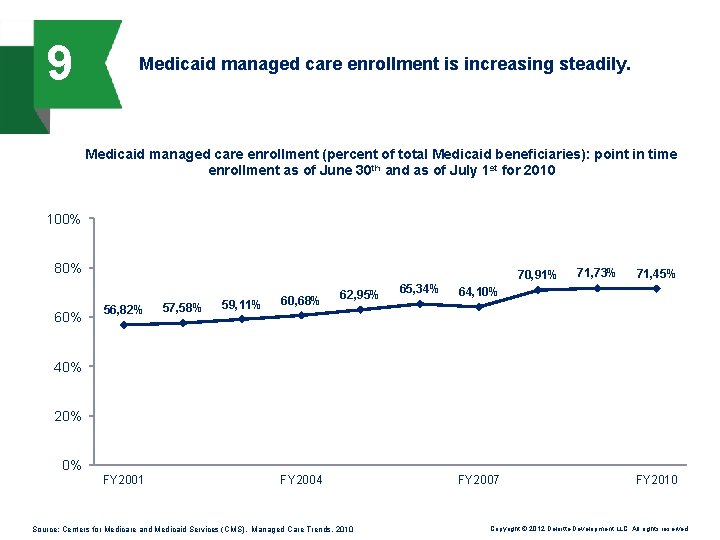
9 The health insurance industry is the problem, and its fate uncertain. Facts: • The problem with the health care system is not the fault of one sector; the entire system is fragmented and expensive • There are two reasons insurance as an industry will thrive in coming years: 1. Employers and consumers value the financial security they gain from insurance coverage: they want to keep coverage 2. Enrollment in managed care will increase: state and federal programs such as Medicare and Medicaid will increasingly embrace managed care in their program designs to lower costs and coordinate care Copyright © 2012 Deloitte Development LLC. All rights reserved.
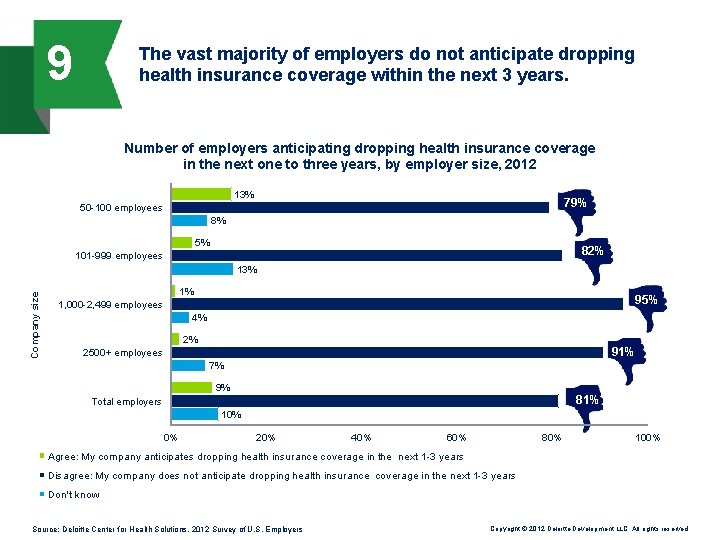
9 The vast majority of employers do not anticipate dropping health insurance coverage within the next 3 years. Number of employers anticipating dropping health insurance coverage in the next one to three years, by employer size, 2012 13% 79% 50 -100 employees 8% 5% 82% 101 -999 employees Company size 13% 1% 95% 1, 000 -2, 499 employees 4% 2% 91% 2500+ employees 7% 9% 81% Total employers 10% 0% 20% 40% 60% 80% 100% Agree: My company anticipates dropping health insurance coverage in the next 1 -3 years Disagree: My company does not anticipate dropping health insurance coverage in the next 1 -3 years Don't know Source: Deloitte Center for Health Solutions, 2012 Survey of U. S. Employers Copyright © 2012 Deloitte Development LLC. All rights reserved.
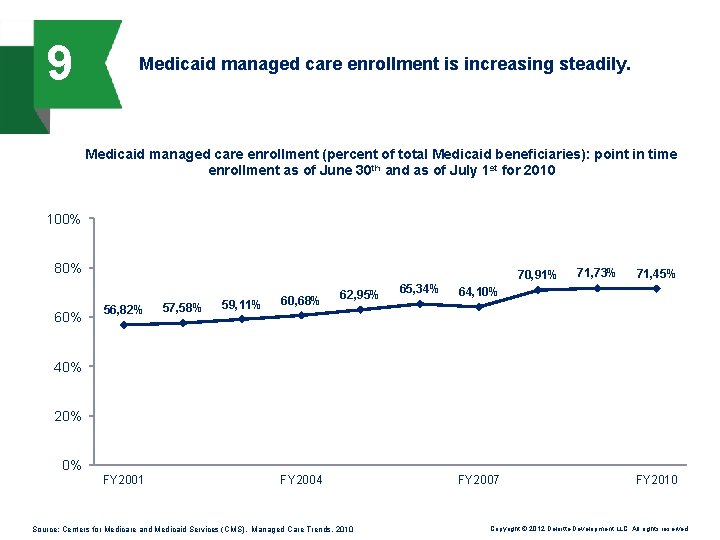
9 Medicaid managed care enrollment is increasing steadily. Medicaid managed care enrollment (percent of total Medicaid beneficiaries): point in time enrollment as of June 30 th and as of July 1 st for 2010 100% 80% 60% 70, 91% 56, 82% 57, 58% 59, 11% 60, 68% 62, 95% 65, 34% 71, 73% 71, 45% 64, 10% 40% 20% 0% FY 2001 FY 2004 Source: Centers for Medicare and Medicaid Services (CMS), Managed Care Trends, 2010 FY 2007 FY 2010 Copyright © 2012 Deloitte Development LLC. All rights reserved.
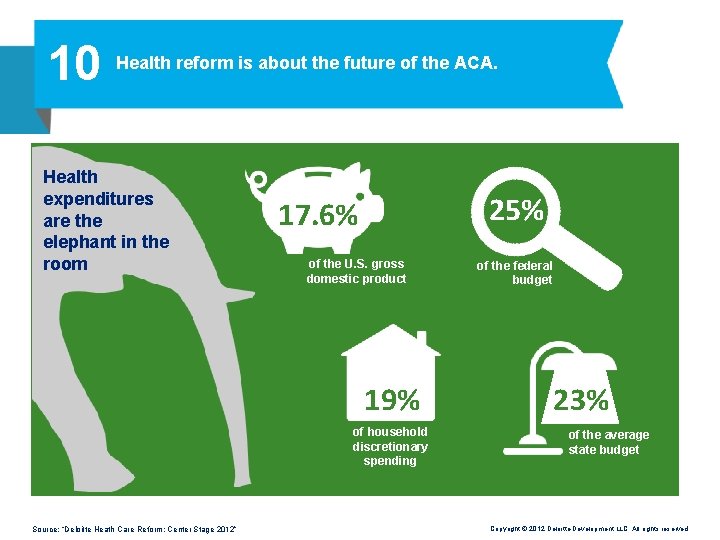
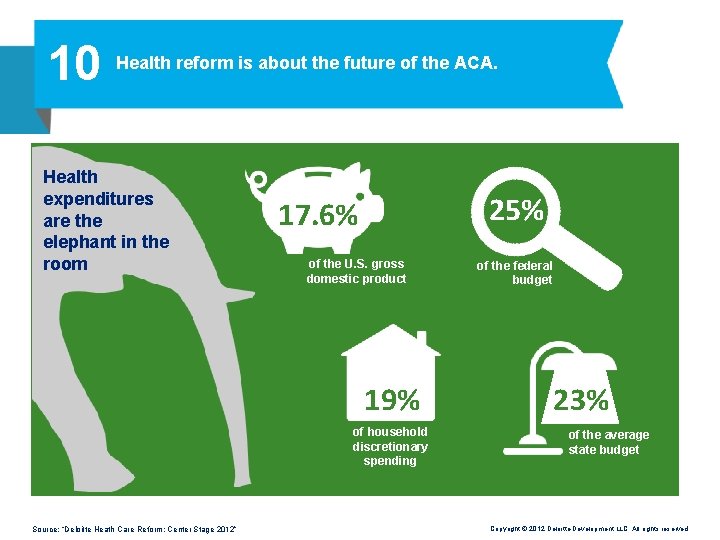
10 Health reform is about the future of the ACA. Health expenditures are the elephant in the room 25% 17. 6% of the U. S. gross domestic product 19% of household discretionary spending Source: “Deloitte Heath Care Reform: Center Stage 2012” of the federal budget 23% of the average state budget Copyright © 2012 Deloitte Development LLC. All rights reserved.
10 Health reform is about the future of the ACA. Facts: • Regardless of the election outcome, policymakers and the industry must grapple with the system’s costs; it should take priority • The big question in health reform is this: Is our system performing at a level that’s commensurate with the value it adds in communities, companies, and households, and if not, how can the value gap be bridged? • It’s about cost vs. results, perception vs. reality, platitude vs. pragmatics, theory vs. practice, and wants vs. needs; it’s the national discussion we have to have regardless of the ACA Copyright © 2012 Deloitte Development LLC. All rights reserved.
Contacts Paul H. Keckley, Ph. D Executive Director Deloitte Center for Health Solutions Deloitte LLP pkeckley@deloitte. com Ama Ocran Health Policy Specialist Deloitte Center for Health Solutions Deloitte LLP aocran@deloitte. com Sophie Stern Health Policy Specialist Deloitte Center for Health Solutions Deloitte LLP sostern@deloitte. com Copyright © 2012 Deloitte Development LLC. All rights reserved.
To learn more about the Deloitte Center for Health Solutions, its projects and events, please visit: www. deloitte. com/centerforhealthsolutions. Deloitte Center for Health Solutions 1001 G Street N. W. Washington, DC 20001 -4545 Phone 202 220 2177 Fax 202 220 2178 Toll free 888 233 6169 Email healthsolutions@deloitte. com Web http: //www. deloitte. com/centerforhealthsolutions This publication contains general information only and Deloitte is not, by means of this publication, rendering accounting, business, financial, investment, legal, tax, or other professional advice or services. This publication is not a substitute for such professional advice or services, nor should it be used as a basis for any decision or action that may affect your business. Before making any decision or taking any action that may affect your business, you should consult a qualified professional advisor. Deloitte shall not be responsible for any loss sustained by any person who relies on this publication. About Deloitte refers to one or more of Deloitte Touche Tohmatsu Limited, a UK private company limited by guarantee, and its network of member firms, each of which is a legally separate and independent entity. Please see www. deloitte. com/about for a detailed description of the legal structure of Deloitte Touche Tohmatsu Limited and its member firms. Please see www. deloitte. com/us/about for a detailed description of the legal structure of Deloitte LLP and its subsidiaries. Certain services may not be available to attest clients under the rules and regulations of public accounting. About the Center The Deloitte Center for Health Solutions (DCHS) is the health services research arm of Deloitte LLP. Our goal is to inform all stakeholders in the health care system about emerging trends, challenges and opportunities using rigorous research. Through our research, roundtables and other forms of engagement, we seek to be a trusted source for relevant, timely and reliable insights. Copyright © 2012 Deloitte Development LLC. All rights reserved. Member of Deloitte Touche Tohmatsu Limited Copyright © 2012 Deloitte Development LLC. All rights reserved.
About Deloitte refers to one or more of Deloitte Touche Tohmatsu Limited, a UK private company limited by guarantee, and its network of member firms, each of which is a legally separate and independent entity. Please see www. deloitte. com/about for a detailed description of the legal structure of Deloitte Touche Tohmatsu Limited and its member firms. Please see www. deloitte. com/us/about for a detailed description of the legal structure of Deloitte LLP and its subsidiaries. Certain services may not be available to attest clients under the rules and regulations of public accounting. Copyright © 2012 Deloitte Development LLC. All rights reserved. Member of Deloitte Touche Tohmatsu Limited