Health and Behavior Assessment Intervention A New Paradigm

Health and Behavior Assessment & Intervention: A New Paradigm for Professional Psychology VPA 2004
Virginia Psychological Association Richmond, VA October 22, 2004 Antonio E. Puente, Ph. D. Department of Psychology University of North Carolina at Wilmington, NC 28403 VPA 2004
Contact Information n Websites n n n E-mail n n n Univ = www. uncw. edu/people/puente Practice = www. clinicalneuropsychology. us University = Puente@uncw. edu Practice = Puente@clinicalneuropsychology. us Telephone n n University = 910. 962. 3812 Practice = 910. 509. 9371 VPA 2004
Acknowledgments q q q q q Department of Psychology, UNC-Wilmington NCPA Board of Directors, Practice Division, & Staff National Academy of Neuropsychology Division 40 of APA Practice Directorate of the American Psychological Association American Medical Association’s CPT Staff CMS Medical Policy Staff Inter-Divisional Health Care Committee; APA Selected Individuals (e. g. , Jim Georgoulakis) VPA 2004
Background (1988 – present) North Carolina Psychological Association (e) q APA’s Policy & Planning Board; Div. 40 (e) q American Medical Association’s Current Procedural Terminology Committee (IV/V) (a) q Health Care Finance Administration’s Working Group for Mental Health Policy (a) q Center for Medicare/Medicaid Services’ Medicare Coverage Advisory Committee (fa) q Consultant with the North Carolina Medicaid Office; North Carolina Blue Cross/Blue Shield (a) q NAN’s Professional Affairs & Information Office (a) (legend; a = appointment, fa = federal appointment, e = elected) q VPA 2004
Purpose of Presentation n n Increase Reimbursement Increase Range, Type & Quality of Services Decrease Fraud & Abuse Provide Guidelines for Professional Services Increase Professional Stature in Health Care, in general VPA 2004
Outline of Presentation n n n Medicare Current Procedural Terminology Relative Value Units Health & Behavior Codes Current Problems & Possible Solutions Resources Predictions for the Future VPA 2004
Medicare: Overview n n n Why Focus on Medicare The Medicare Program Local Medical Review (policy & panels) VPA 2004
Medicare: Why n The Standard Coding n Value n Documentation n Auditing n VPA 2004
Medicare: Overview n n Centers for Medicare and Medicaid Services Benefits Part A (Hospital) n Part B (Supplementary) n Part C (Medicare+ Choice) n VPA 2004
Medicare: Local Review n Local Medical Review Policy LMRP vs National Policy n Location of LMRPs n n Carrier Medical Director n n A Physician-based Model Policy Panels Lack of Understanding of Their Roles n Lack of Representation on Such Panels n VPA 2004
Medicare Payment (since 1993) n Surgical n n Higher Reimbursement than Cognitive Physician Cognitive Work n Supporting Equipment & Staff n VPA 2004
Current Procedural Terminology: Overview n n n n Background Codes & Coding Existing Codes Model System X Type of Problem Medical Necessity Documenting Time VPA 2004
CPT: Background n American Medical Association Developed by Surgeons (& Physicians) in 1966 for Billing Purposes n 7, 500+ Discrete Codes n n CMS AMA Under License with CMS n CMS Now Provides Active Input into CPT n VPA 2004
CPT: Background/Direction n n Current System = CPT 5 Categories I= Standard Coding for Professional Services n II = Performance Measurement n III = Emerging Technology n VPA 2004
CPT: Applicable Codes n n n Total Possible Codes = Approximately 7, 500 Possible Codes for Psychology = Approximately 40 to 60 Sections = Five Separate Sections n n n Psychiatry Biofeedback Central Nervous Assessment Physical Medicine & Rehabilitation Health & Behavior Assessment & Management VPA 2004
CPT: Development of a Code n Initial n n Health Care Advisory Committee (non-MDs) Primary CPT Work Group n CPT Panel n n Time Frame n 3 -5 to over a decade VPA 2004
CPT: Psychiatry n Sections n n n Interview (90801) vs. Intervention 9 e. g. , 908. 06) Office vs. Inpatient Regular vs. Evaluation & Management Other Types of Interventions n Insight, Behavior Modifying, and/or Supportive vs. Interactive VPA 2004
CPT: CNS Assessment n Interview n n 96115 Testing Psychological = 96100; 96110/11 n Neuropsychological = 96117 n Other = 96105, 96110/111 n VPA 2004
CPT: Physical Medicine & Rehabilitation n n 97770 now 97532 Note: 15 minute increments VPA 2004
CPT: Health & Behavior Assessment & Management n n Purpose: Medical Diagnosis Time: 15 Minute Increments Assessment Intervention VPA 2004
Rationale: General n n Acute or chronic (health) illness may not meet the criteria for a psychiatric diagnosis Avoids inappropriate labeling of a patient as having a mental health disorder Increases the accuracy of correct coding of professional services Increase range of services VPA 2004
Rationale: Specific Examples n n n Patient Adherence to Medical Treatment Symptom Management & Expression Health-promoting Behaviors Health-related Risk-taking Behaviors Overall Adjustment to Medical Illness VPA 2004
Overview of Codes n n New Subsection Six New Codes Assessment n Intervention n Established Medical Illness or Diagnosis Focus on Biopsychosocial Factors VPA 2004
Assessment Explanation n Identification of psychological, behavioral, emotional, cognitive, and social factors In the prevention, treatment, and/or management of physical health problems Focus on biopsychosocial factors (not mental health) VPA 2004
Assessment (continued) n May include (examples); health-focused clinical interview n behavioral observations n psychophysiological monitoring n health-oriented questionnaires n and, assessment/interpretation of the aforementioned n VPA 2004
Intervention Explanation n Modification of psychological, behavioral, emotional, cognitive, and/or social factors Affecting physiological functioning, disease status, health, and/or well being Focus = improvement of health with cognitive, behavioral, social, and/or psychophysiological procedures VPA 2004
Intervention (continued) n May include the following procedures (examples); Cognitive n Behavioral n Social n Psychophysiological n VPA 2004
Diagnosis Match n n n Associated with acute or chronic illness Prevention of a physical illness or disability Not meeting criteria for a psychiatric diagnosis or representing a preventative medicine service VPA 2004
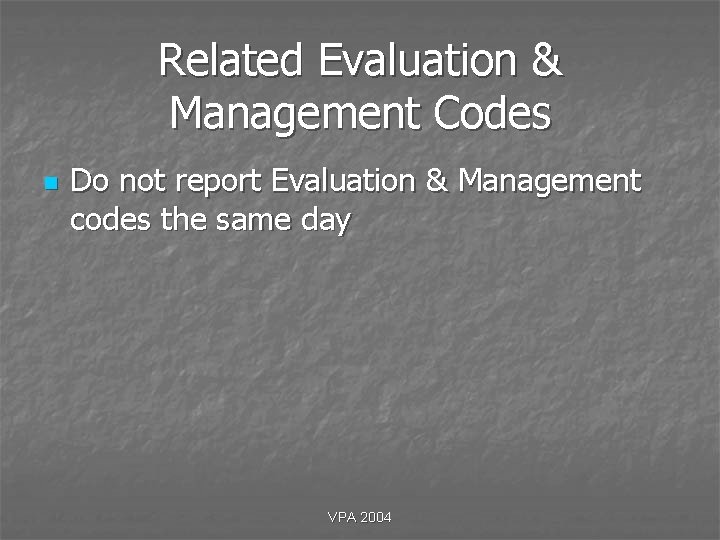
Related Psychiatric Codes n n If psychiatric services are required (9080190899) along with these, report predominant service Do not report psychiatric and these codes on the same day VPA 2004
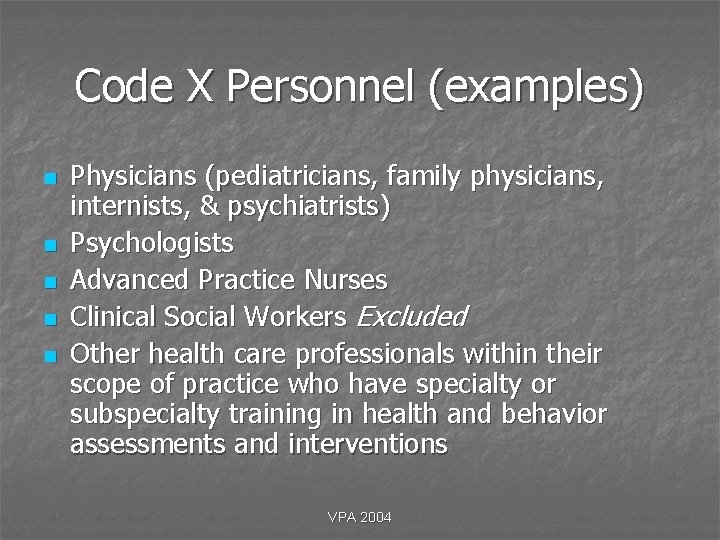
Related Evaluation & Management Codes n Do not report Evaluation & Management codes the same day VPA 2004
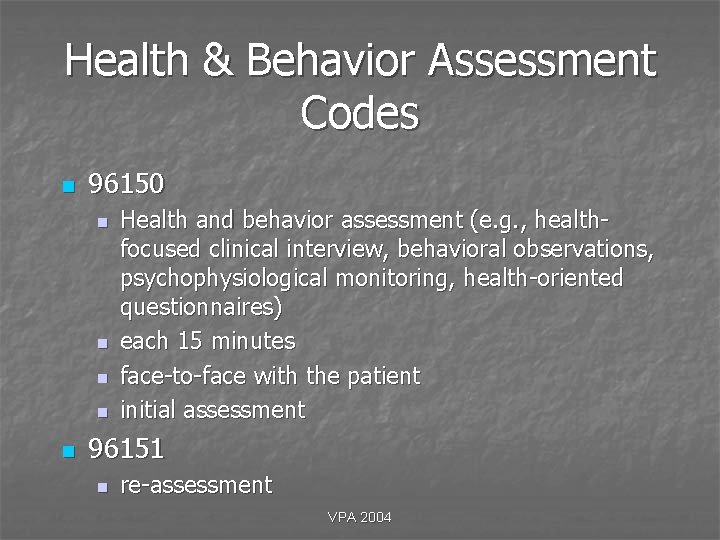
Code X Personnel (examples) n n n Physicians (pediatricians, family physicians, internists, & psychiatrists) Psychologists Advanced Practice Nurses Clinical Social Workers Excluded Other health care professionals within their scope of practice who have specialty or subspecialty training in health and behavior assessments and interventions VPA 2004
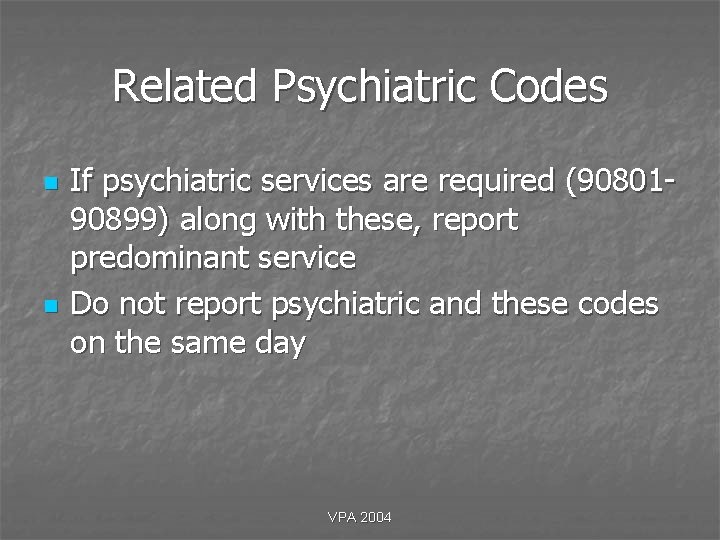
Health & Behavior Assessment Codes n 96150 n n n Health and behavior assessment (e. g. , healthfocused clinical interview, behavioral observations, psychophysiological monitoring, health-oriented questionnaires) each 15 minutes face-to-face with the patient initial assessment 96151 n re-assessment VPA 2004
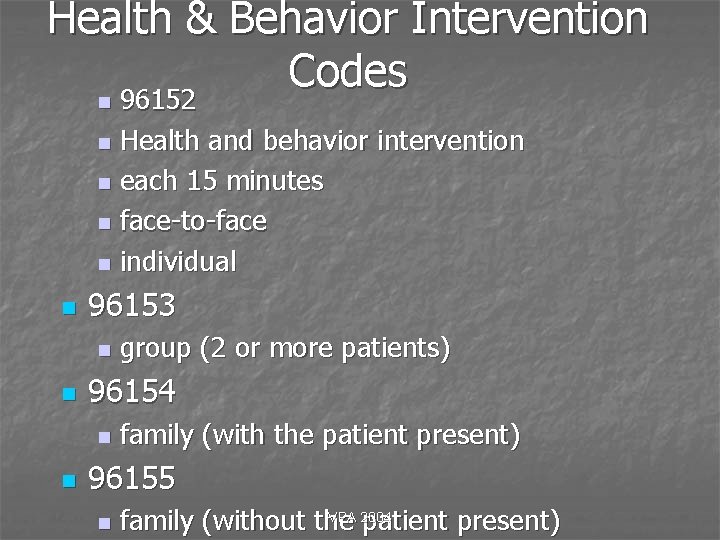
Health & Behavior Intervention Codes n 96152 n Health and behavior intervention n each 15 minutes n face-to-face n individual n n 96153 n n 96154 n n group (2 or more patients) family (with the patient present) 96155 n VPA 2004 family (without the patient present)
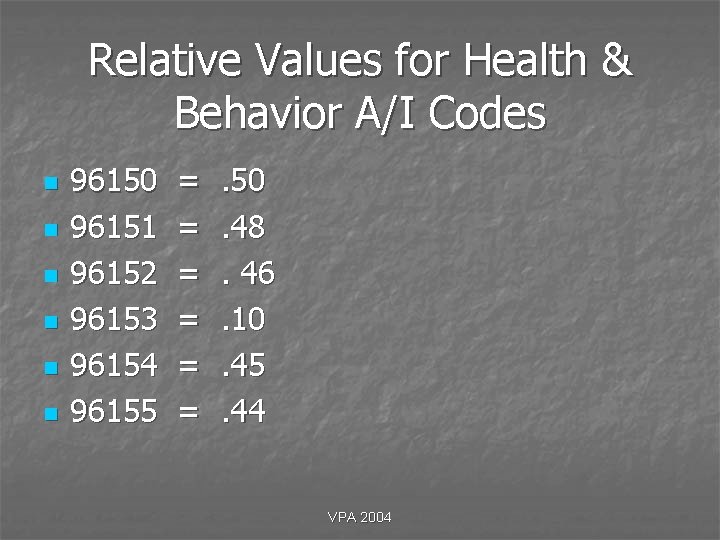
Relative Values for Health & Behavior A/I Codes n n n 96150 96151 96152 96153 96154 96155 = = = . 50. 48. 46. 10. 45. 44 VPA 2004
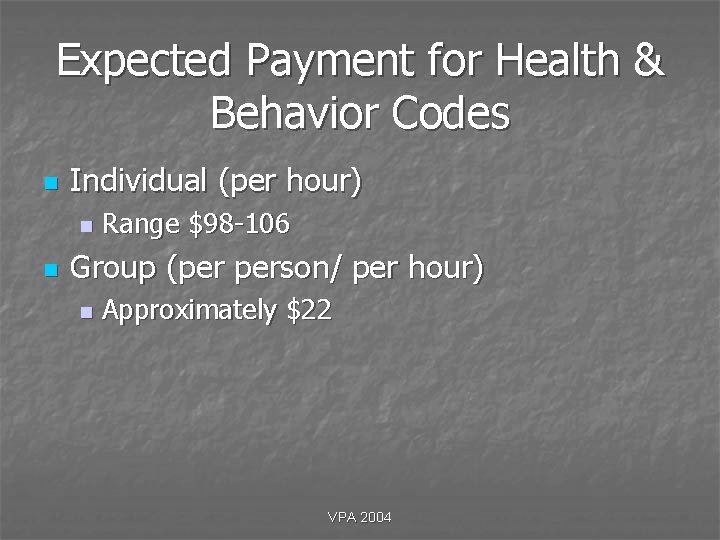
Expected Payment for Health & Behavior Codes n Individual (per hour) n n Range $98 -106 Group (per person/ per hour) n Approximately $22 VPA 2004
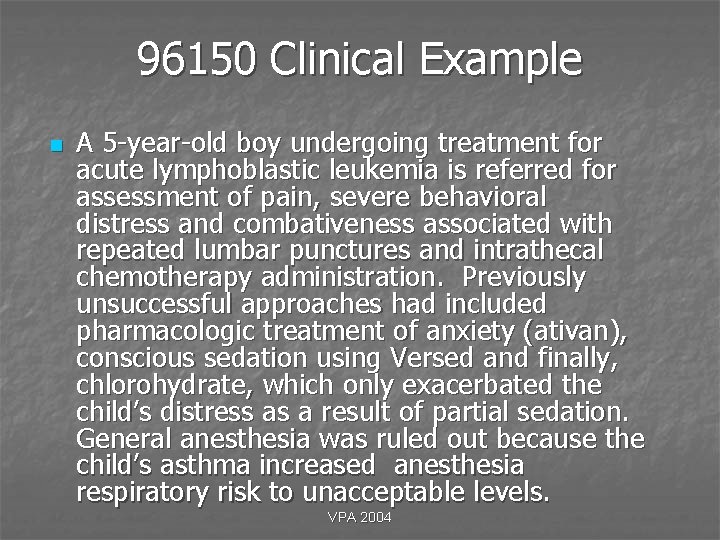
96150 Clinical Example n A 5 -year-old boy undergoing treatment for acute lymphoblastic leukemia is referred for assessment of pain, severe behavioral distress and combativeness associated with repeated lumbar punctures and intrathecal chemotherapy administration. Previously unsuccessful approaches had included pharmacologic treatment of anxiety (ativan), conscious sedation using Versed and finally, chlorohydrate, which only exacerbated the child’s distress as a result of partial sedation. General anesthesia was ruled out because the child’s asthma increased anesthesia respiratory risk to unacceptable levels. VPA 2004
96150 Description of Procedure n n The patient was assessed using standardized tests and questionnaires (e. g. , the Information-seeking scale, Pediatric Pain Questionnaire, Coping Strategies Inventory) which, in view of the child’s age, were administered in a structured format. The medical staff and child’s parents were also interviewed. On the day of a scheduled medical procedure, the child completed a self-report distress questionnaire. Behavioral observations were also made during the procedure using the CAMPIS-R, a structured observation scale that quantifies child, parent, and medical staff behavior. An assessment of the patient’s condition was performed through the administration of various health and behavior instruments. VPA 2004
96151 Clinical Example n A 35 -year-old female, diagnosed with chronic asthma, hypertension and panic attacks was originally seen ten months ago for assessment and follow-up treatment. Original assessment included extensive interview regarding patient’s emotional, social, and medical history, including her ability to manage problems related to the chronic asthma, hospitalizations, and treatments. Test results from original assessment provided information for treatment planning which included health and behavior interventions using a combination of behavioral cognitive therapy, relaxation response training and visualization. After four months of treatment interventions, the patient’s hypertension and anxiety were significantly reduced and thus the patient was discharged. Now six months following discharge, the patient has injured her knee and has undergone arthroscopic surgery with follow-up therapy VPA 2004
96151 Description of Procedure n n Patient was seen to reassess and evaluate psychophysiological responses to these new health stressors. A review of the records from the initial assessment, including testing and treatment intervention, as well as current medical records was made. Patient’s affective and physiological status, compliance disposition, and perceptions of efficacy of relaxation and visualization practices utilized during previous treatment intervention are examined. Administration of anxiety inventory/questionnaire (e. g. , Burns Anxiety Inventory) is used to quantify patient’s current level of response to present health stressors and compared to original assessment levels. Need for further treatment is evaluated. A reassessment of the patients condition was performed through the use of interview and behavioral health instruments. VPA 2004
96152 Clinical Example n A 55 -year-old executive has a history of cardiac arrest, high blood pressure and cholesterol, and a family history of cardiac problems. He is 30 lbs. overweight, travels extensively for work, and reports to be a moderate social drinker. He currently smokes one-half pack of cigarettes a day, although he had periodically attempted to quit smoking for up to five weeks at a time. The patient is considered by his physician to be a “Type A” personality and at high risk for cardiac complications. He experiences angina pains one or two times per month. The patient is seen by a behavior medicine specialist. Results from the health and behavior assessment are used to develop a treatment plan, taking into account the patient’s coping skills and lifestyle. VPA 2004
96152 Description of Procedure n Weekly intervention sessions focus on psychoeducational factors impacting his awareness and knowledge about his disease process, and the use of relaxation and guided imagery techniques that directly impact his blood pressure and heart rate. Cognitive and behavioral approaches for cessation of smoking and initiation of an appropriate physician-prescribed diet and exercise regimen are also employed. VPA 2004
96153 Clinical Example n A 45 -year-old female is referred for smoking cessation secondary to chronic bronchitis, with a strong family history of emphysema. She smokes two packs per day. The health and behavior assessment reveals that the patient uses smoking as a primary way of coping with stress. Social Influences contributing to her continued smoking include several friends and family members who also smoke. The patient has made multiple previous attempts to quit “on her own”. When treatment options are reviewed, she is receptive to the recommendation of an eightsession group cessation program. VPA 2004
96153 Description of Procedure n The program components include educational information (e. g. , health risks, nicotine addiction), cognitive-behavioral treatment (e. g. , self-monitoring, relaxation training, and behavioral substitution), and social support (e. g. , group discussion, social skills training). Participants taper intake over four weeks to a quit date and then attend three more sessions for relapse prevention. Each group sessions lasts 1. 5 hrs. VPA 2004
96154 Clinical Example n Tara is a 9 -year-old girl, diagnosed with insulin dependent diabetes two years ago. Her mother reports great difficulty with morning and evening insulin injections and blood glucose testing. Tara whines and cries, delaying the procedures for 30 minutes or more. She refused to give her own injections or conduct her own blood glucose tests, claiming they “hurt”. Her mother spends many minutes pleading for her cooperation. Tara’s father refuses to participate, saying he is “afraid” of her needles. Both parents have not been able to go to a movie or dinner alone, because they know of no one who can care for Tara’s ten year old sister claims she never has any time with her mother, since her mother is always occupied with Tara’s illness. Tara and her sister have a very poor relationship and are always quarreling. Tara’s parents frequently argue; her mother complains that she gets no help from her husband. Tara’s father complains that his wife has no time for anyone except Tara. VPA 2004
96154 Description of Procedure n A family-based approach is used to address the multiple components of Tara’s problem behaviors. Relaxation and exposure techniques are used to address Tara’s father’s fear of injections, which he has inadvertently has been modeling for Tara is taught relaxation and distraction techniques to reduce the tension she experiences with finger sticks and injections. Both parents are taught to shape Tara’s behavior, praising and rewarding successful diabetes management behaviors, and ignoring delay tactics. Her parents are also taught judicious use of time-out and response cost procedures. Family roles and responsibilities are clarified. Clear communication, conflict-resolution, and problem-solving skills are taught. Family members practice applying these skills to a variety of problems so that they will know how to successfully address new problems that may arise in the future. VPA 2004
96155 Clinical Example n Greg is a 42 -year-old male diagnosed with cancer of the pancreas. He is currently undergoing both aggressive chemotherapy and radiation treatments. However, his prognosis is guarded. At present, he is not in the endstage disease process and therefore does not qualify for Hospice care. The patient is seen initially to address issues of pain management via imagery, breathing exercises, and otherapeutic interventions to assess quality of life issues, treatment options, and death and dying issues. VPA 2004
96155 Description of Procedure n Due to the medical protocol and the patient’s inability to travel to additional sessions between hospitalizations, a plan is developed for extending treatment at home via the patient’s wife, who is his primary home caregiver. The patient’s wife is seen by the healthcare provider to train the wife in how to assist the patient in objectively monitoring his pain and in applying exercises learned via his treatment sessions to manage pain. Issues of the patient’s quality of life, as well as death and dying concerns, are also addressed with assistance given to the wife as to how to make appropriate home interventions between sessions. Effective communication techniques with her husband’s physician and other members of his treatment team regarding his treatment protocols are facilitated. VPA 2004
CPT: Model System n n Psychiatric Neurological Non-Neurological Medical Possibly, Evaluation & Management VPA 2004
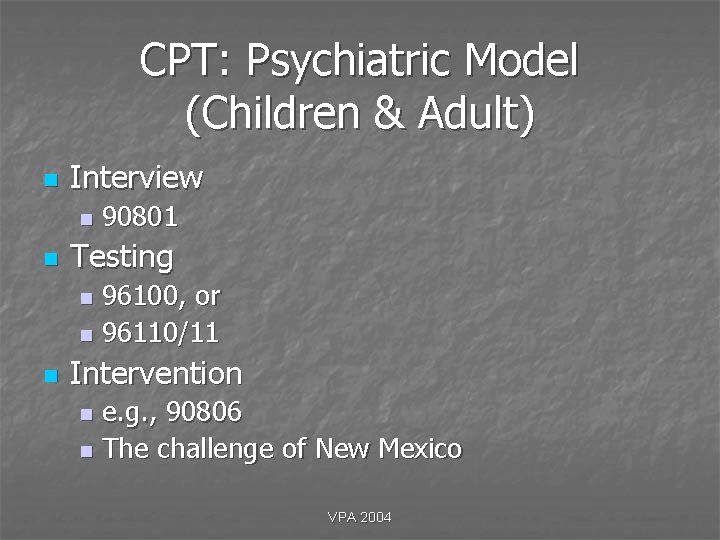
CPT: Psychiatric Model (Children & Adult) n Interview n n 90801 Testing 96100, or n 96110/11 n n Intervention e. g. , 90806 n The challenge of New Mexico n VPA 2004
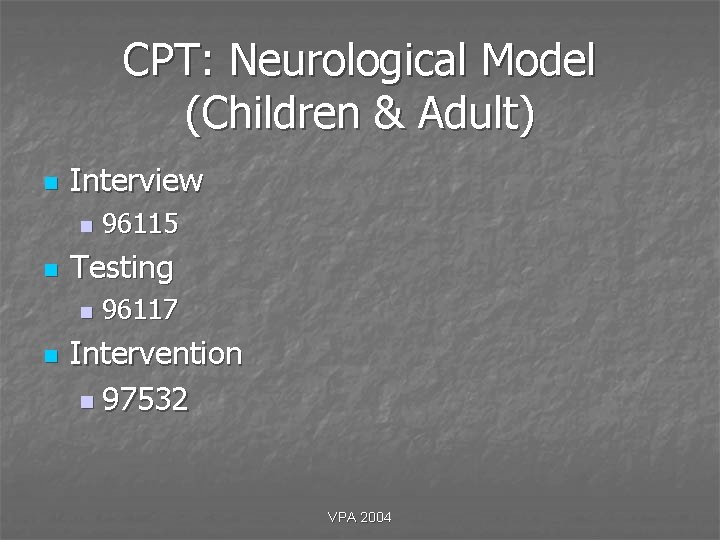
CPT: Neurological Model (Children & Adult) n Interview n n Testing n n 96115 96117 Intervention n 97532 VPA 2004
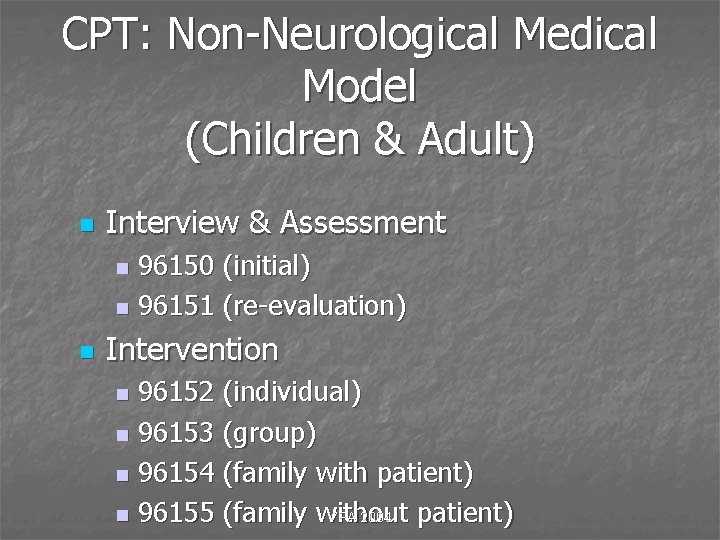
CPT: Non-Neurological Medical Model (Children & Adult) n Interview & Assessment 96150 (initial) n 96151 (re-evaluation) n n Intervention 96152 (individual) n 96153 (group) n 96154 (family with patient) n 96155 (family without patient) VPA 2004 n
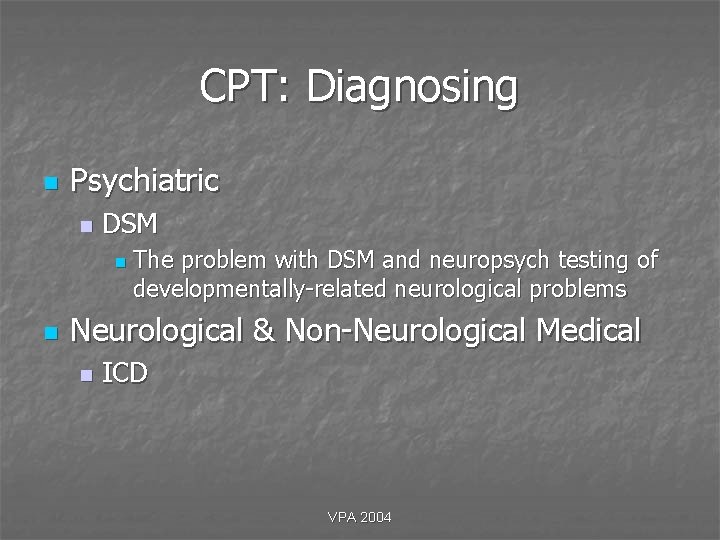
CPT: Diagnosing n Psychiatric n DSM n n The problem with DSM and neuropsych testing of developmentally-related neurological problems Neurological & Non-Neurological Medical n ICD VPA 2004
CPT: Medical Necessity n n n n Scientific & Clinical Necessity Local Medical Review or Carrier Definitions of Necessity = CPT x DX Necessity Dictates Type and Level of Service Necessity Can Only be Proven with Documentation Screening or Regularly Scheduled Evals Do Not Meet Criteria for Necessity Will Results Affect Outcome of Patient Will New Information Be Obtained VPA 2004
CPT: Documenting n n n Purpose Payer Requirements General Principles History Examination Decision Making VPA 2004
Documentation: Purpose n n n Medical Necessity Evaluate and Plan for Treatment Communication and Continuity of Care Claims Review and Payment Research and Education VPA 2004
Documentation: Payer Requirements n n n Site of Service Medical Necessity for Service Provided Appropriate Reporting of Activity VPA 2004
Documentation: General Principles n n n n Rationale for Service Complete and Legible Reason/Rationale for Service Assessment, Progress, Impression, or Diagnosis Plan for Care Date and Identity of Observe Timely Confidential VPA 2004
Documentation: Basic Information Across All Codes n n n n n Date Time, if applicable Identify of Observer (technician ? ) Reason for Service Status Procedure Results/Finding Impression/Diagnoses Disposition Stand Alone VPA 2004
Documentation: Chief Complaint n n n Concise Statement Describing the Symptom, Problem, Condition, & Diagnosis Foundation for Medical Necessity Must be Complete & Exhaustive VPA 2004
Documentation: Present Illness n Symptoms n n Location, Quality, Severity, Duration, timing, Context, Modifying Factors Associated Signs Follow-up Changes in Condition n Compliance n VPA 2004
Documentation: History n n Past Family Social Medical/Psychological VPA 2004
Documentation: Intervention n n n Reason for Service Status Intervention Results Impression Disposition Time VPA 2004
Documentation: Assessment n n n Reason for Service Dates (time? ) Tests and Protocols (included editions) Narrative of Results Impression Disposition VPA 2004
Documentation: Suggestions n n n Avoid Handwritten Notes Do Not Use Red Ink Avoid Color Paper Document On and After Every Encounter, Every Procedure, Every Patient Review Changes Whenever Applicable Avoid Standard Phrases & Protocols VPA 2004
Time n Defining n Professional (not patient) Time Including: n n Interview & Assessment Codes n n pre, intra & post-clinical service activities Use 15 minute increments Intervention Codes n Use 15 minute increments VPA 2004
Time: Definition n n AMA Definition of Time Physicians also spend time during work, before, or after the face-to-face time with the patient, performing such tasks as reviewing records & tests, arranging for services & communicating further with other professionals & the patient through written reports & telephone contact. VPA 2004
Time (continued) n n n Communicating further with others Follow-up with patient, family, and/or others Arranging for ancillary and/or other services VPA 2004
Time: Testing n Quantifying Time n n Round up or down to nearest increment Time Does Not Include n n n Patient completing tests, forms, etc. Waiting time by patient Typing of reports Non-Professional (e. g. , clerical) time Literature searches, learning new techniques, etc. VPA 2004
Reimbursement History n n n Cost Plus Prospective Payment System (PPS) Diagnostic Related Groups (DRGs) Customary, Prevailing & Reasonable (CPR) Resource Based Relative Value System (RBRVS) VPA 2004
Relative Value Units: Overview n n Components Units Values Current Problems VPA 2004
RVU: Components n n n Physician Work Resource Value Practice Expense Resource Value Malpractice Geographic Conversion Factor (approx. $34) VPA 2004
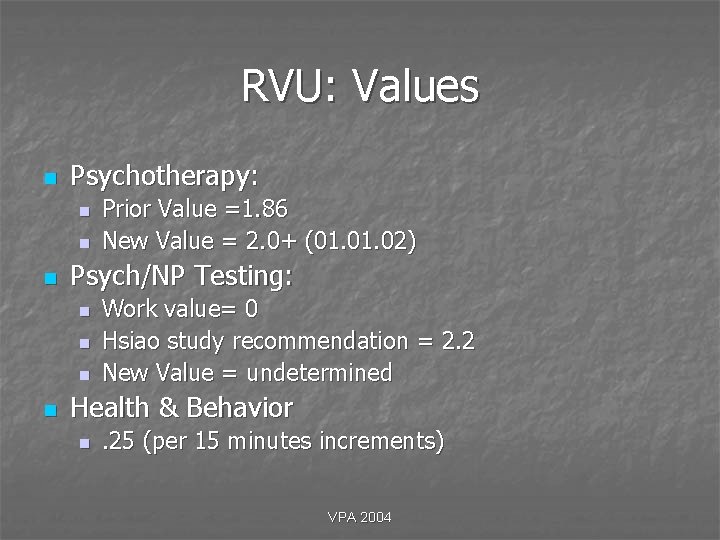
RVU: Values n Psychotherapy: n n n Psych/NP Testing: n n Prior Value =1. 86 New Value = 2. 0+ (01. 02) Work value= 0 Hsiao study recommendation = 2. 2 New Value = undetermined Health & Behavior n . 25 (per 15 minutes increments) VPA 2004
RVU: Acceptance n n n Medicare Blue Cross/Blue Shield 87% Managed Care 69% Medicaid 55% Other 44% New Trends: n n RVUs as a Model for All Insurance Companies RVUs as a Basis for Compensation Formulas VPA 2004
CPT x RVU VPA 2004
Current Problems n n n n n Definition of Physician Incident to Supervision Face-to-Face Time RVUs Work Values Practice Expense & Testing Survey Payment Focus for Fraud & Abuse VPA 2004
Problem: Defining Physician n Definition of a Physician Social Security Practice Act of 1980 n Definition of a Physician n Need for Congressional Act n Likelihood of Congressional Act n The Value of Technical Services of a Psychologist is $. 83/hour (second highest after physicist) n Consequence of the preceding; grouping with 2004 non-doctoral level VPA allied health providers n
Problem: Incident to n Rationale for Incident to n n Definition of Physician Extender n n n How Limitations Definition of In vs. Outpatient n n Congress intended to provide coverage for services not typically covered elsewhere Geographic Vs Financial Why No Incident to (DRG) Solution Available for Some Training Programs Probably no Future to Incident to VPA 2004
Problem: More Incident to n When is “Incident to” Acceptable: n n Testing Cognitive Rehabilitation; Biofeedback Psychotherapy Definition n n Commonly furnished service Integral, though incidental to psychologist Performed under the supervision Either furnished without charge or as part of the psychologist’s charge VPA 2004
Problem: Incident to & Site of Service n Outpatient vs. Inpatient Geographical Location n Corporate Relationship n Billing Service n Chart Information & Location n VPA 2004
Problem: Incident to versus Independent Service n When Does Incident to Become Independent Service Appearance of No Supervision n Clinical Decisions are Made by Staff n Ratio of Physician to Staff Time Becomes Disproportionate n Distance Difficulties n Supervision Difficulties n VPA 2004
Problems: Recent Difficulties with Incident to n Who Bills Incident to n n Treating Physician Bills not the Supervising Physician Then, Who is the Responsible Party The Physician Must Treat the Patient First Physician Bonuses Must Tied to a Groups’ Overall Pool of Income (e. g. , not referral or possibly individual productivity) VPA 2004
Problem: Supervision n Supervision 1. General = overall direction n 2. Direct = present in office suite n 3. Personal = in actual room n 4. Psychological = when supervised by a psychologist n VPA 2004
Problem: Face-to-Face n n Implications Technical versus Professional Services Surgery is the Foundation for CPT (and most work is face-to-face) Hard to Document & Trace Non-Face-to. Face Work VPA 2004
Problem: RVUs n Bad News n n n 2000 = 5. 5% increase 2001 = 4. 5% increase 2002 = 5. 4% decrease 2003 = 4. 4 to 5. 7% decrease ($34. 14) Really Bad News n n Bush Administration not supportive of changing the conversion formula Change Continued to Probably 2005 Depending on Such Factors as the Stock Market (e. g. , 5000) VPA 2004
Problem: Work Value n n Physician Activities (e. g. , Psychotherapy) Result in Work Values Psychological Based Activities (i. e. , Testing) Have no Work Values RVUs are Heavily Based on Practice Expenses (which are being reduced) Net Result = Maybe Up to a Half Lower VPA 2004
Problem: An Artificial Practice Expense n n n Five Year Reviews Prior Methodology Current Value = approximately 1. 5 of 1. 75 is practice Deadline for New Practice Expense = 2002 n n Currently in Check Due to the Ongoing Survey Expected Value = closer to 50% of total value at best VPA 2004
Problem: Work Value of Testing n n n First Round Second Round Current Round VPA 2004
Problem: Qualification of Technician n What is the Minimum Level of Training Required for a Technician? Bachelor’s vs. Masters n Intern vs. Postdoctoral n VPA 2004
Problem: Payment n Origins of the Problem Balanced Budget Act of 1997 n Employer’s Cost for Health Care in 2002 = $5, 000 per employee n n What Should Your Code Be Payed at? n n www. webstore. ama-assn. org- State Legislation n www. insure. com/health/lawtool. cfm VPA 2004
Problem: Payment Problems n Refilling n n n 51% require refilling of original forms But, up to 60% do not follow up Errors n n n 54% = plan administrator 17% = provider 29% = member VPA 2004
Problem: Payment n Use of HMOs & Third Party n n Shift in Practice Patterns by Psychiatry (14% increase) Exclusion of MSW, etc. Worst Hit Are Psychologists (2% decrease) Compensation n n Gross Charges Adjusted Charges RVUs Receivables VPA 2004
Problem: Payment of Health & Behavior Codes n n Medicare Almost all Resolved Non-Medicare Resolving VPA 2004
Problem: Expenditures & Fraud n Projections n Current n n By 2011; n n 14% 17% ($2. 8 trillion) Examples n Nadolni Billing Service (Memphis) n n $5 million in claims to CIGNA for psychological services $250, 000 fine (& tax evasion); July 12 th VPA 2004
Defining Fraud n Fraud Intentional n Pattern n n Error Clerical n Dates n VPA 2004
Problem: Fraud & Abuse n n 26 Different Kinds of Fraud Types Mental Health Profiled Estimates of Less Than 10% Recovered Psychotherapy Estimates/Day = 9. 67 hours n n Review Likely if Over 12 Hours Per Day Problems with Fraud Methodology Primarily in how the research was done n Also, in the application of sampling n VPA 2004
Problem: Fraud Office of Inspector General n Primary Problems n n n Psychotherapy (oig. hhs/gov/reports/region 5/50100068) n n n Medical Necessity (approximately $5 billion) Documentation Individual Group # of Hours Who Does the Therapy Psychological Testing n n # of Hours Documentation VPA 2004
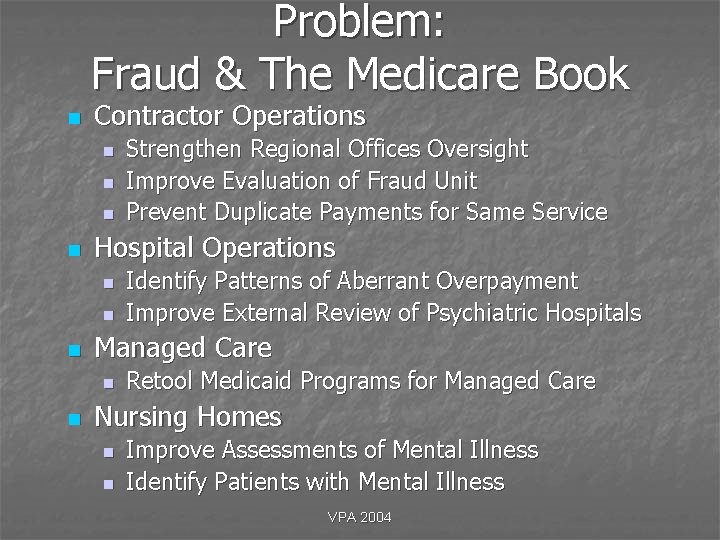
Problem: Fraud & The Medicare Book n Contractor Operations n n Hospital Operations n n n Identify Patterns of Aberrant Overpayment Improve External Review of Psychiatric Hospitals Managed Care n n Strengthen Regional Offices Oversight Improve Evaluation of Fraud Unit Prevent Duplicate Payments for Same Service Retool Medicaid Programs for Managed Care Nursing Homes n n Improve Assessments of Mental Illness Identify Patients with Mental Illness VPA 2004
Problem: The Medicare Book (continued) n Physicians/Allied Health Professionals Improve Oversight of Rural Health Clinics n Eliminate Inappropriate Payments for Mental Health Services n Yet, Improve Medicaid Mental Health Programs n VPA 2004
Problem: Fraud (cont. ) n Nursing Homes n n Identification Overuse of Services Children Experience n n California; Texas Corporation Audit Company Audit Personal Audit VPA 2004
Problem: Fraud (cont. ) n Estimated Pattern of Fraud Analysis For-profit Medical Centers n For-profit Medical Clinics n Non-profit Medical Centers n Non-profit Medical Clinics n Nursing Homes n Group Practices n Individual Practices n VPA 2004
Problem: Mental vs. Physical n Historical vs. Traditional vs. Recent Diagnostic Trends Recent Insurance Interpretations of Dxs Limitations of the DSM The Endless Loop of Mental vs. Physical n NOTE: Important to realize that LMRP is almost n n n always more restrictive than national guidelines VPA 2004
Possible Solutions: General Approaches n n n n Better Understanding & Application of CPT More Involvement in Billing Comprehensive Understanding of LMRP More Representation/Involvement with AMA, CMS & Local Medical Review Panels Meetings with CMS Presentation of New Testing Codes Increased Staff & Relationship Practice Staff and with CAPP VPA 2004
Possible Solutions: Resources n General Web Sites n n n n n www. nanonline. org/paio www. cms. org (medicare/medicaid) www. hhs. org (health & human services) www. oig. hhs. gov (inspector general) www. ahrq. gov (agency for healthcare research) www. medpac. gov (medical payment advisory comm. ) www. whitehouse. gov/fsbr/health (statistics) www. div 40. org (clinical neuropsychology div of apa) www. healthcare. group. com (staff salaries) VPA 2004
Resources (continued) n LMRP Reconsideration Process n n Coding Web Sites n n n www. cms. gov/manuals/pm_trans/R 28 PIM. pdf www. aapcnatl. org (academy of coders) www. ntis. gov/product/correct-coding (coding edits) Compliance Web Sites n n n www. apa. org (psychologists & hipaa) www. cms. hhs. gov/hipaa. (hipaa) www. hcca-info. org (health care compliance assoc. ) VPA 2004
Future Perspectives n Income Steadier due to decreased changes n Probable incremental declines, up to 1020% if traditional practice is pursued n If Medicaid dependent (25% or more), then declines could be even higher n Possible “final” stabilization by 2005 n n Results of election, economy, & new codes VPA 2004
Future Perspectives (continued) n Paradigms Industrial vs. Boutique/Niche n Clinical vs. Forensic n Mental Health vs. Health n Existing vs. Developing n VPA 2004
Future Perspectives n n Evolving Paradigm = Continued and Significant Change Success = Predict, Embrace and Shape Change VPA 2004
- Slides: 108