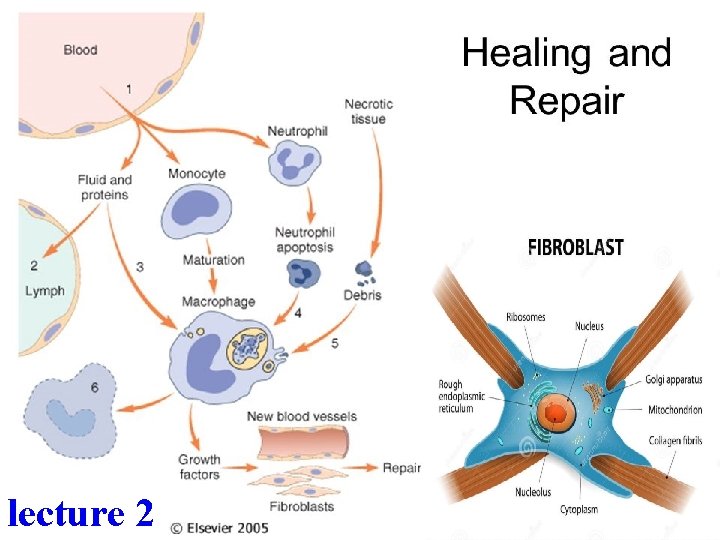
Healing and repair lecture 2 Wound healing Healing




- Slides: 42
• • Healing and repair lecture 2
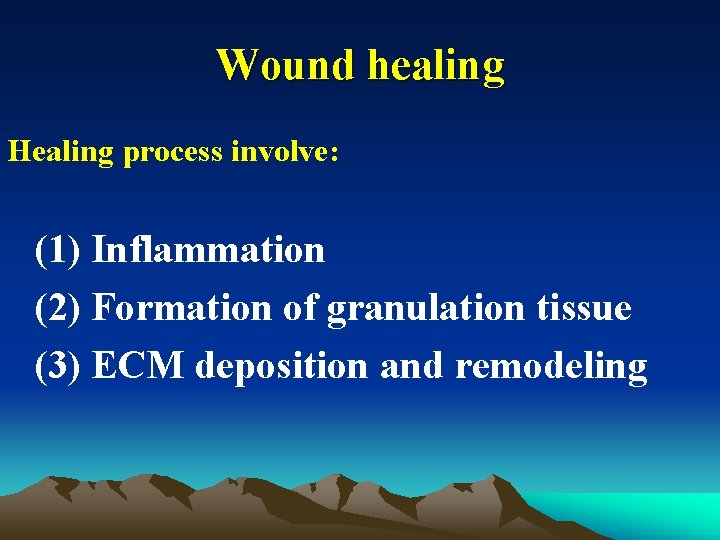
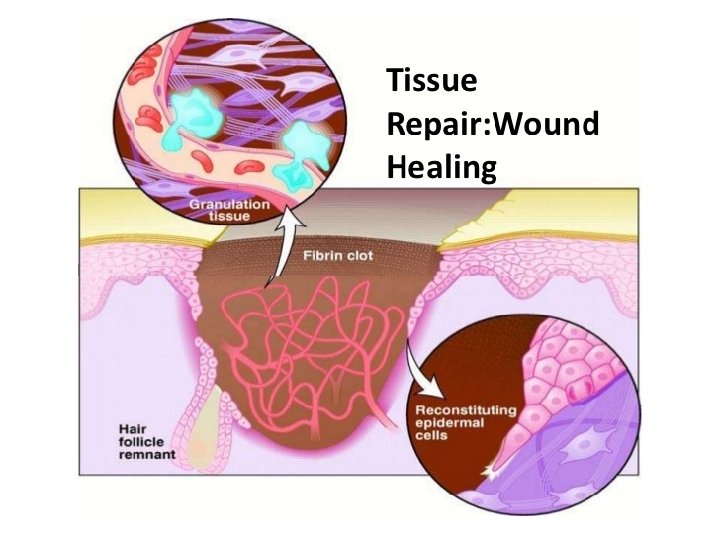
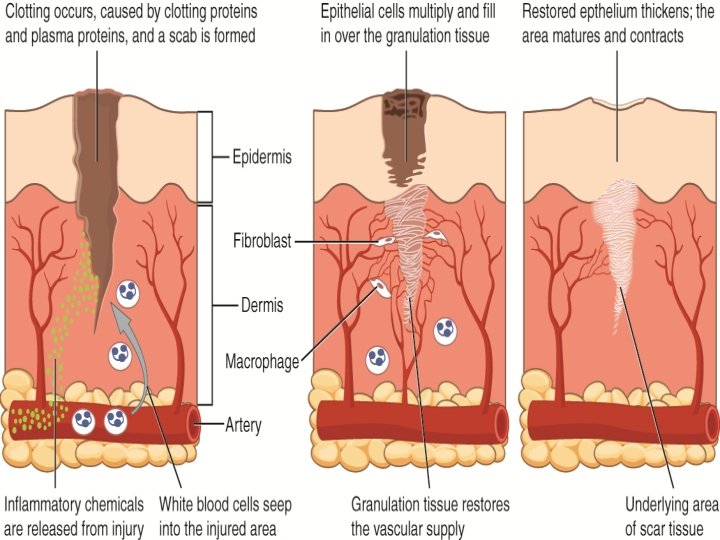
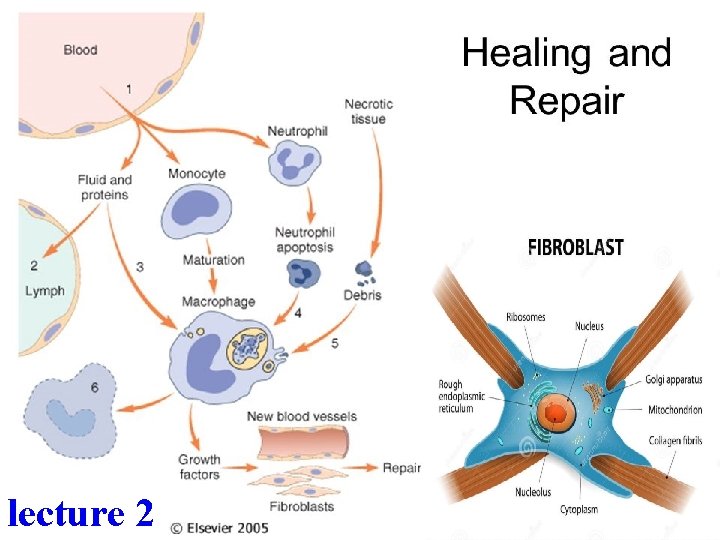
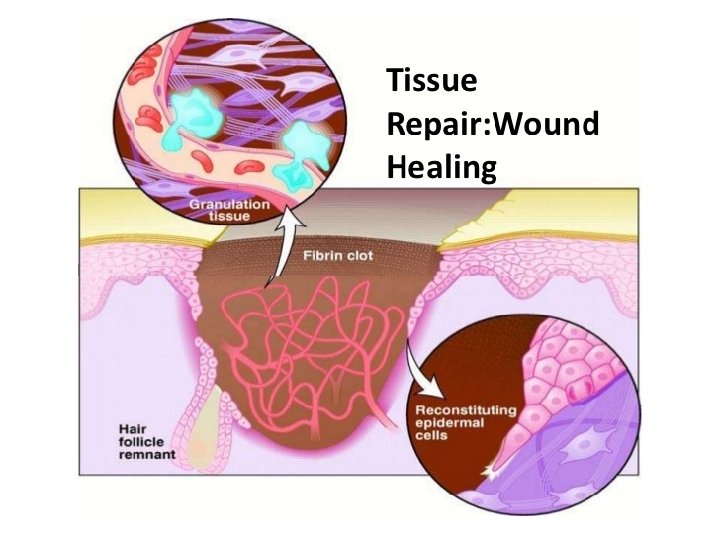
Wound healing Healing process involve: (1) Inflammation (2) Formation of granulation tissue (3) ECM deposition and remodeling

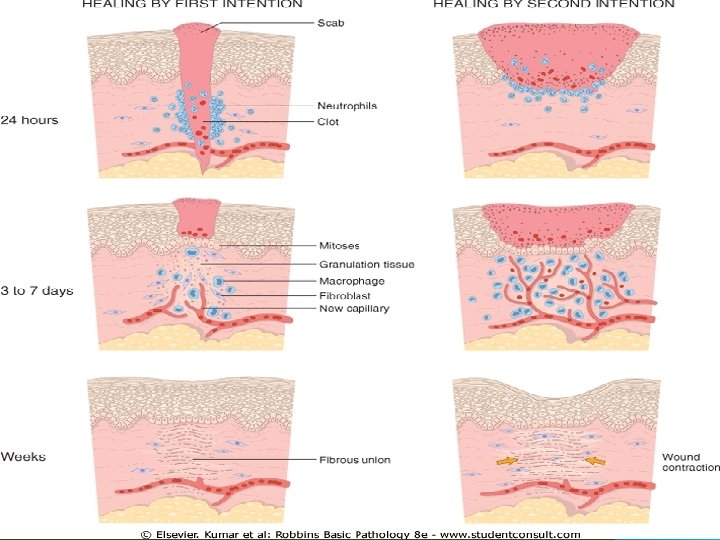
Wound healing Healing of any wound can occur by one of two type of repair: 1. Healing by First Intention (primary union). 2. Healing by Second Intention (secondary union).
Two facts 1. Healing of tissue wounds occurs by: Organization : Granulation tissue formation & scarring. 2. The difference between primary and secondary union are quantitative, not qualitative i. e. the same elements are involved but their proportions are different.
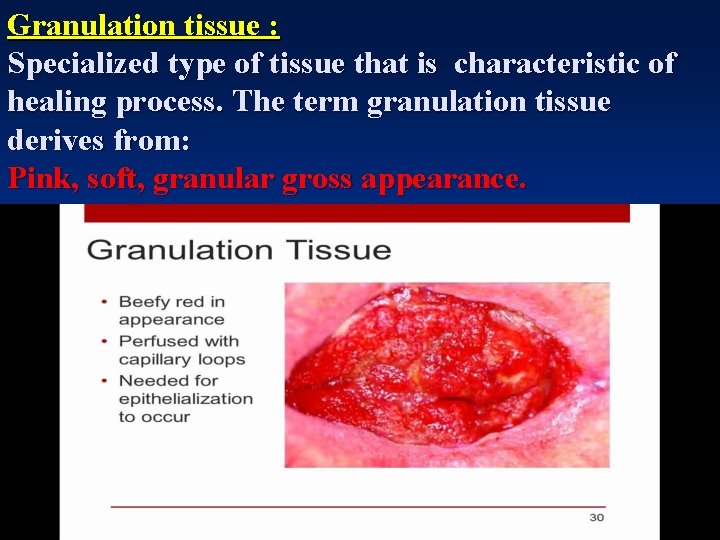
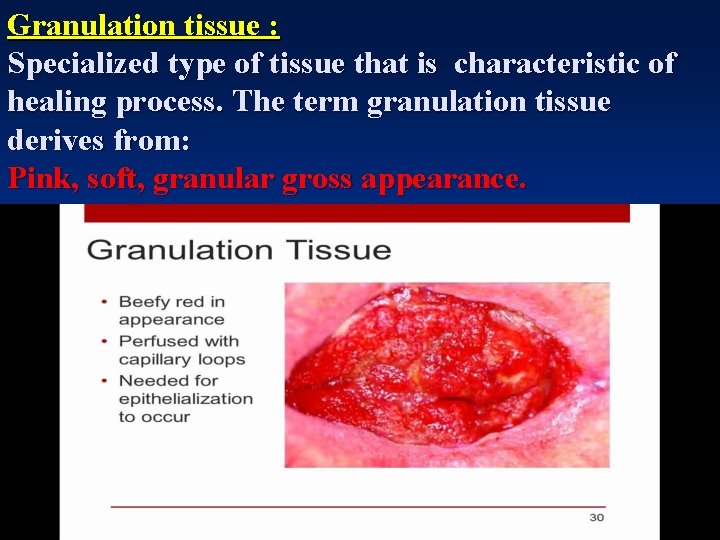
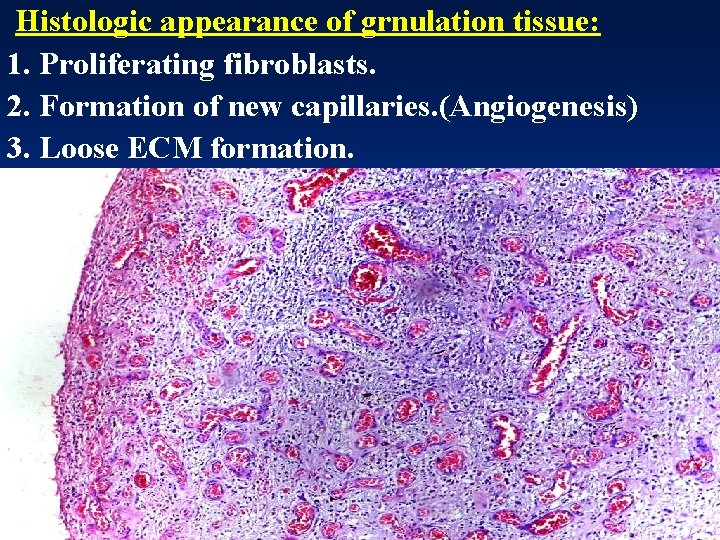
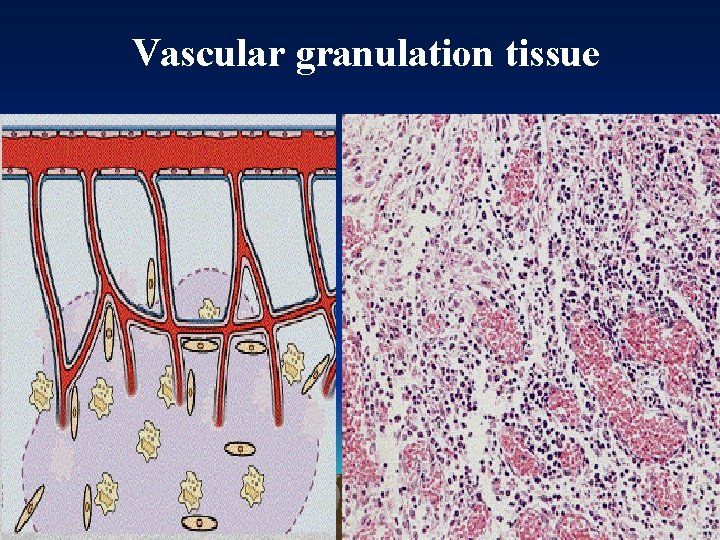
Granulation tissue : Specialized type of tissue that is characteristic of healing process. The term granulation tissue derives from: Pink, soft, granular gross appearance.
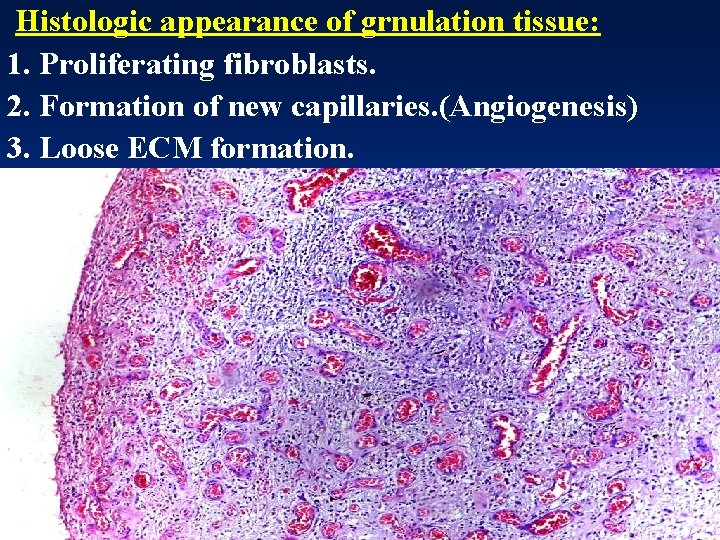
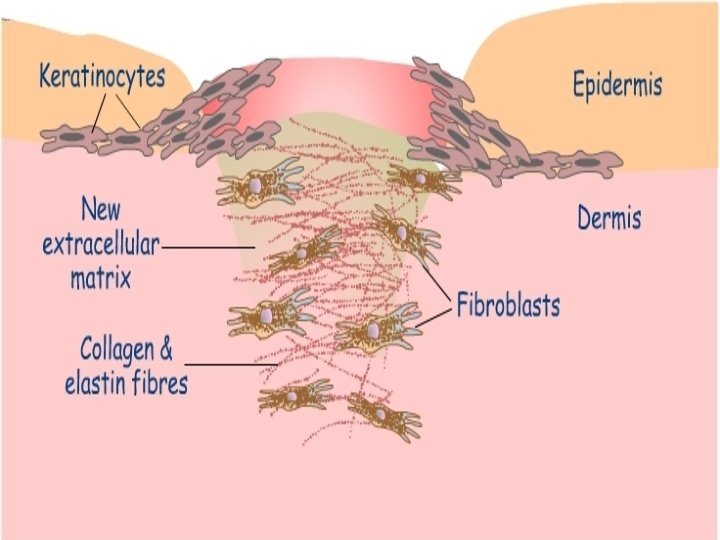
Histologic appearance of grnulation tissue: 1. Proliferating fibroblasts. 2. Formation of new capillaries. (Angiogenesis) 3. Loose ECM formation.
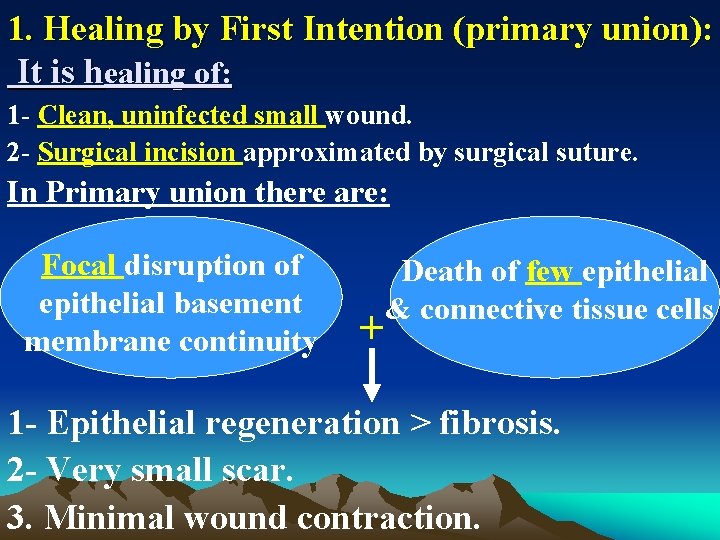
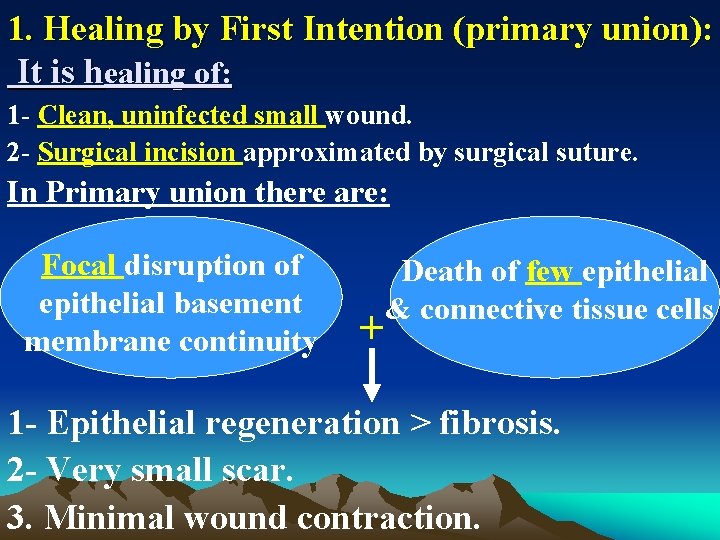
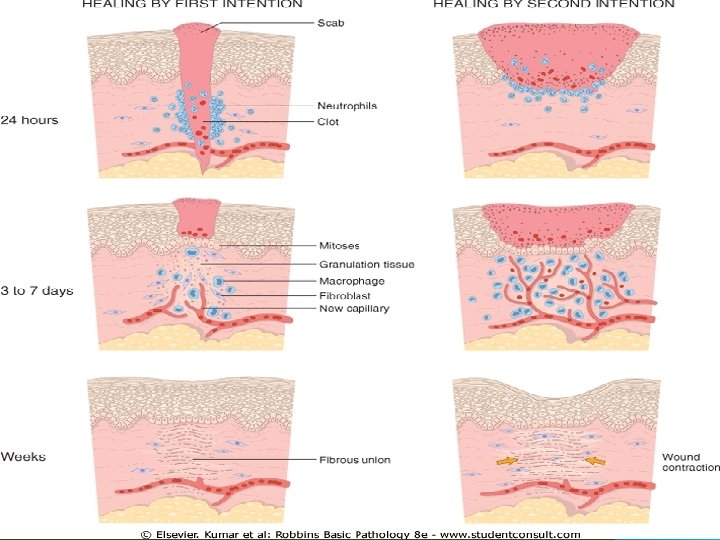
1. Healing by First Intention (primary union): It is healing of: 1 - Clean, uninfected small wound. 2 - Surgical incision approximated by surgical suture. In Primary union there are: Focal disruption of epithelial basement membrane continuity + Death of few epithelial & connective tissue cells 1 - Epithelial regeneration > fibrosis. 2 - Very small scar. 3. Minimal wound contraction.
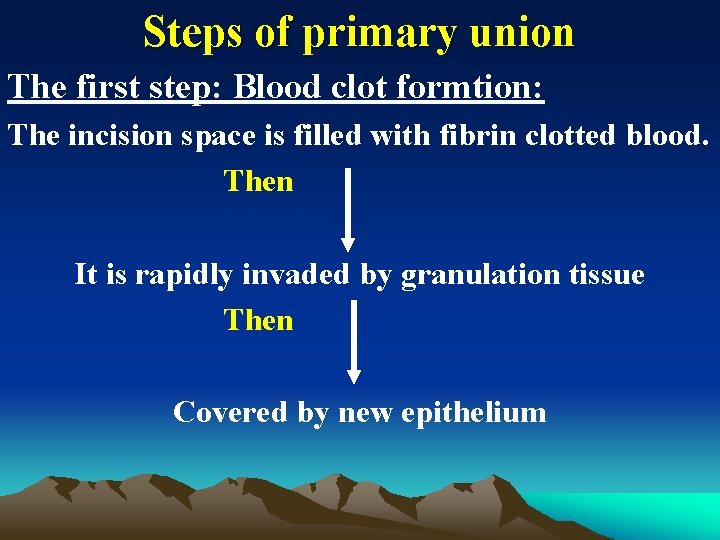
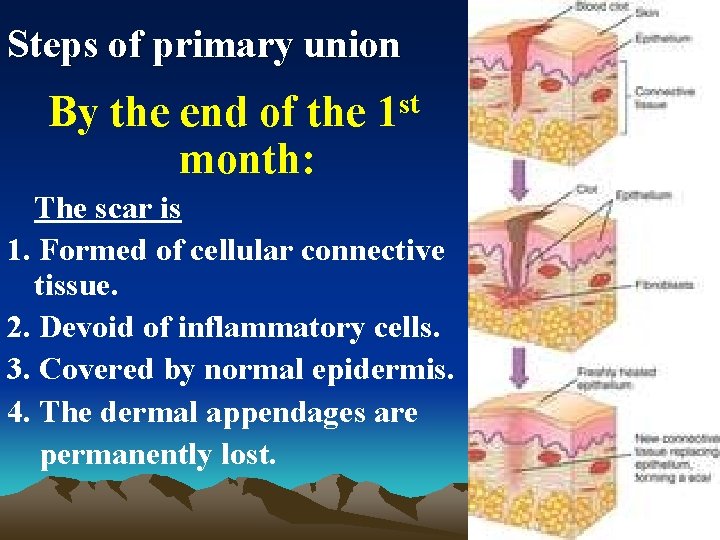
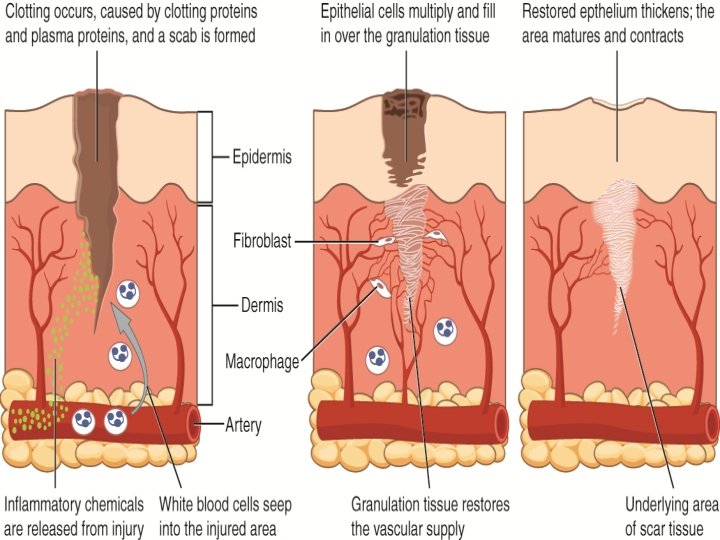
Steps of primary union The first step: Blood clot formtion: The incision space is filled with fibrin clotted blood. Then It is rapidly invaded by granulation tissue Then Covered by new epithelium
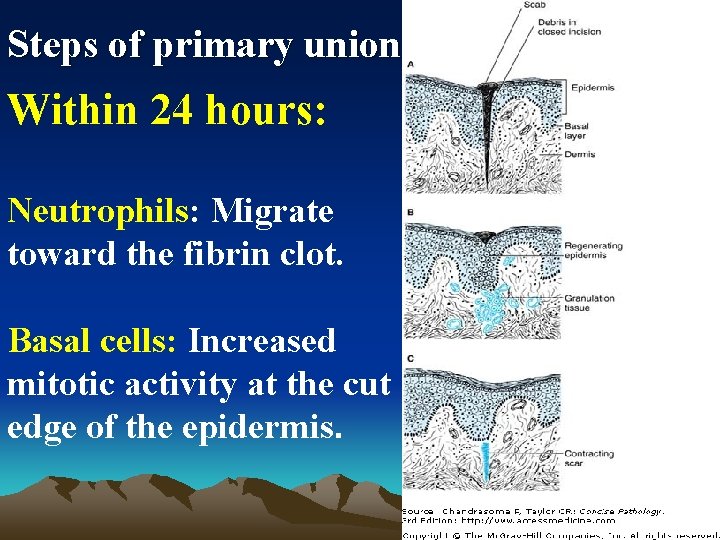
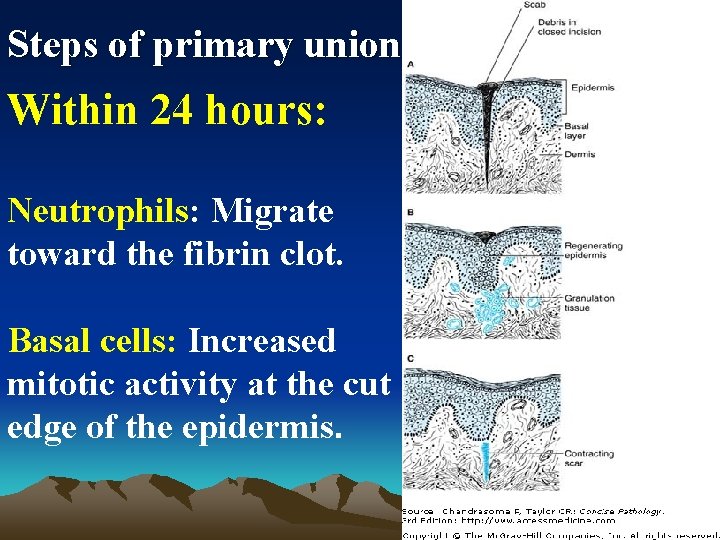
Steps of primary union Within 24 hours: Neutrophils: Migrate toward the fibrin clot. Basal cells: Increased mitotic activity at the cut edge of the epidermis.
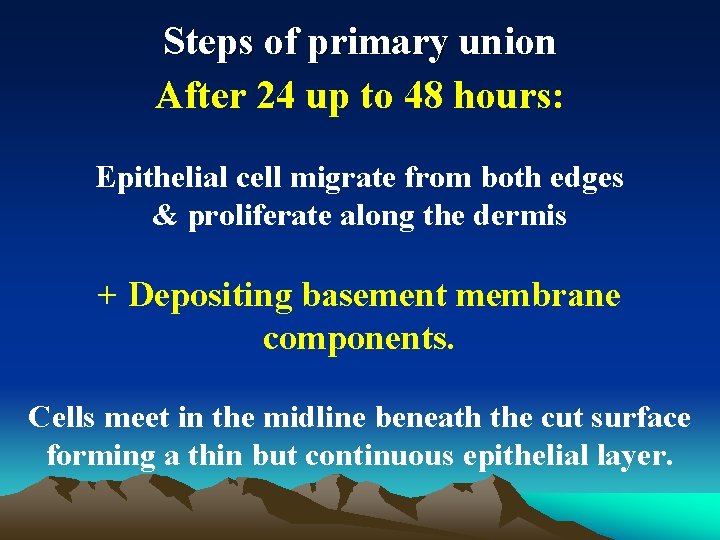
Steps of primary union After 24 up to 48 hours: Epithelial cell migrate from both edges & proliferate along the dermis + Depositing basement membrane components. Cells meet in the midline beneath the cut surface forming a thin but continuous epithelial layer.
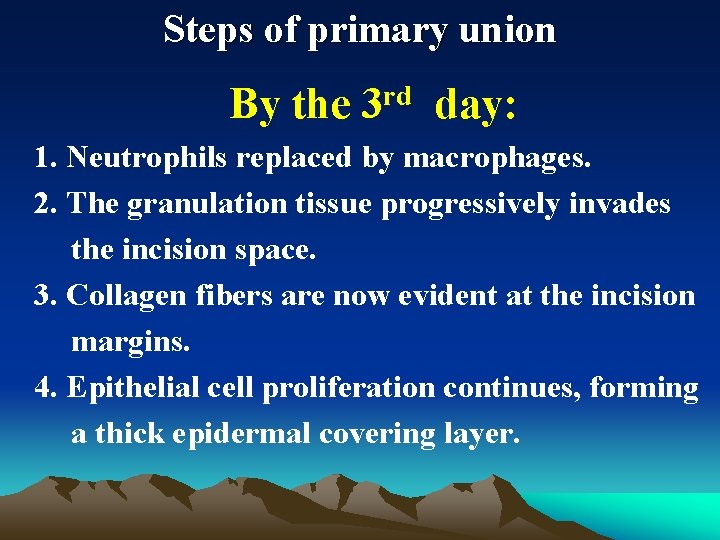
Steps of primary union By the 3 rd day: 1. Neutrophils replaced by macrophages. 2. The granulation tissue progressively invades the incision space. 3. Collagen fibers are now evident at the incision margins. 4. Epithelial cell proliferation continues, forming a thick epidermal covering layer.
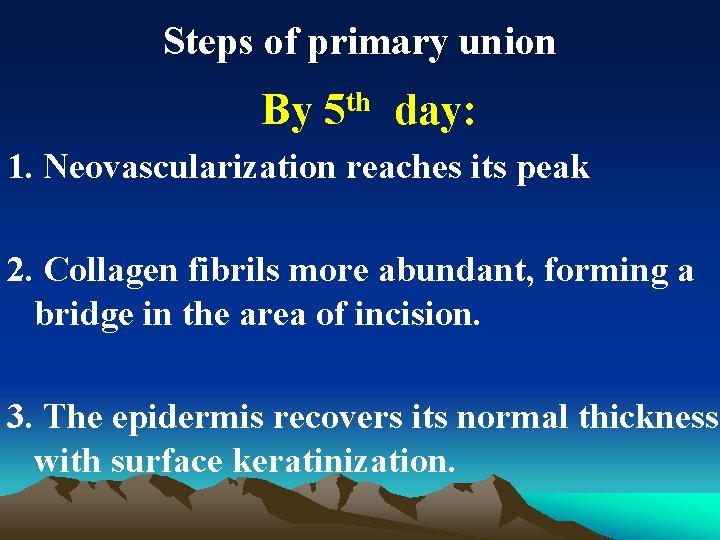
Steps of primary union By th 5 day: 1. Neovascularization reaches its peak 2. Collagen fibrils more abundant, forming a bridge in the area of incision. 3. The epidermis recovers its normal thickness with surface keratinization.
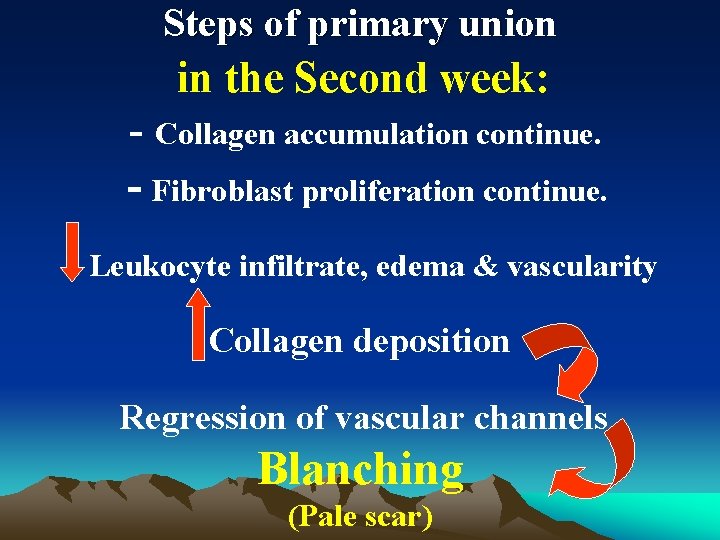
Steps of primary union in the Second week: - Collagen accumulation continue. - Fibroblast proliferation continue. Leukocyte infiltrate, edema & vascularity Collagen deposition Regression of vascular channels Blanching (Pale scar)
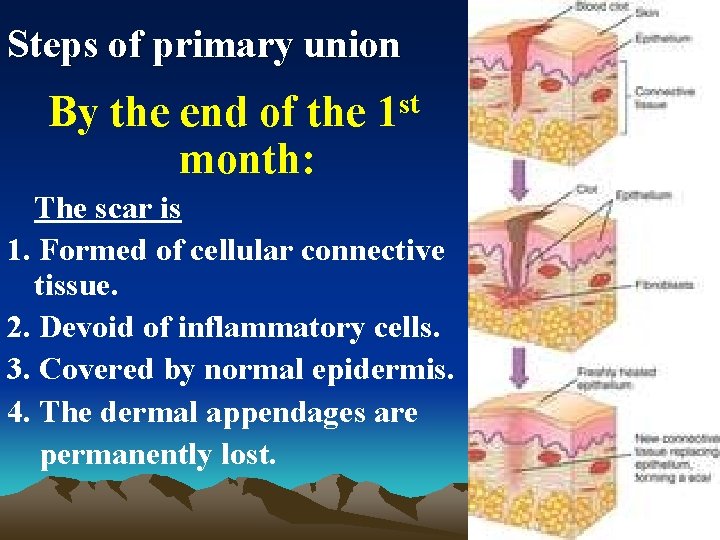
Steps of primary union By the end of the 1 st month: The scar is 1. Formed of cellular connective tissue. 2. Devoid of inflammatory cells. 3. Covered by normal epidermis. 4. The dermal appendages are permanently lost.
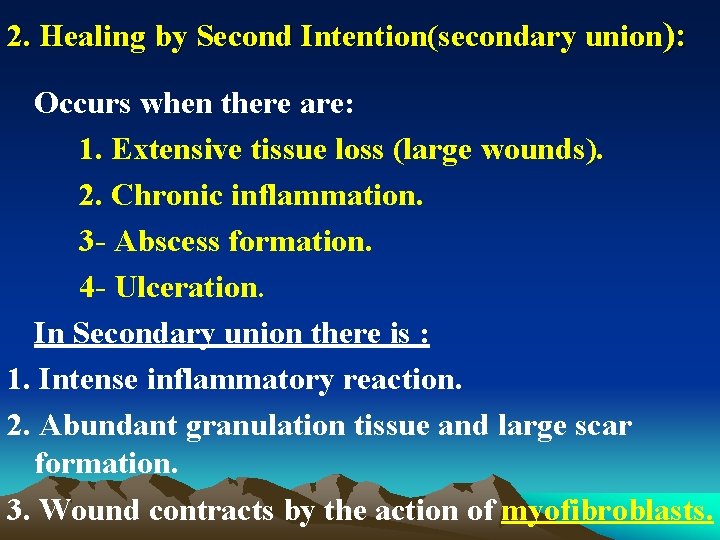
2. Healing by Second Intention(secondary union): Occurs when there are: 1. Extensive tissue loss (large wounds). 2. Chronic inflammation. 3 - Abscess formation. 4 - Ulceration. In Secondary union there is : 1. Intense inflammatory reaction. 2. Abundant granulation tissue and large scar formation. 3. Wound contracts by the action of myofibroblasts.
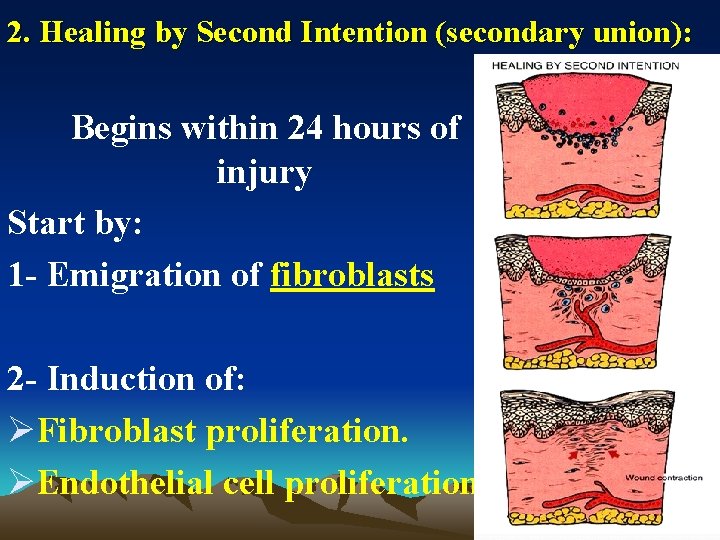
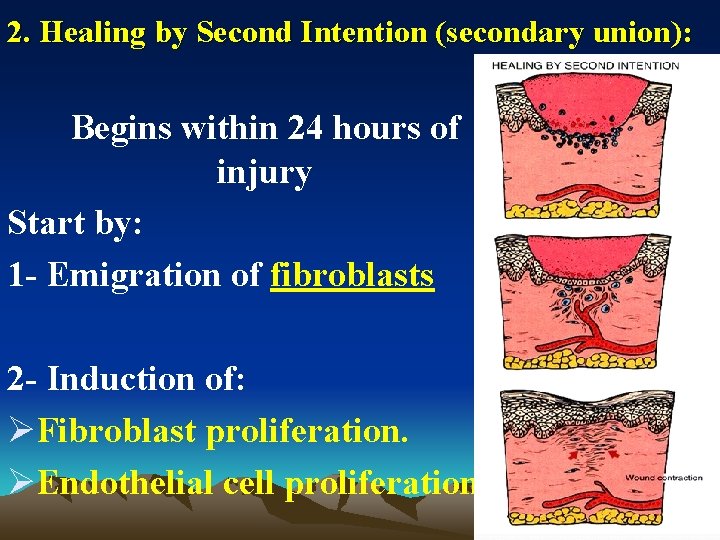
2. Healing by Second Intention (secondary union): Begins within 24 hours of injury Start by: 1 - Emigration of fibroblasts 2 - Induction of: ØFibroblast proliferation. ØEndothelial cell proliferation
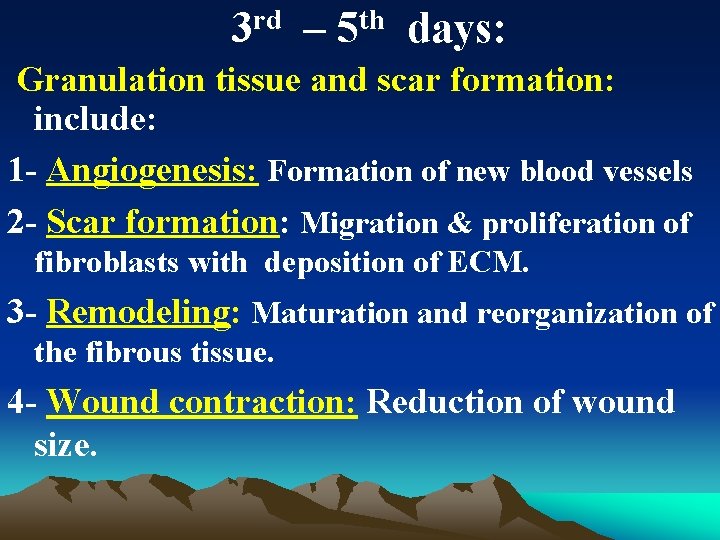
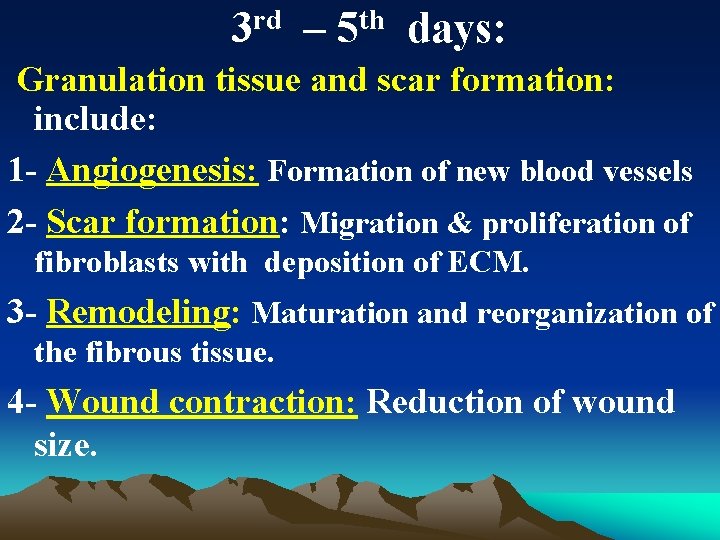
3 rd – 5 th days: Granulation tissue and scar formation: include: 1 - Angiogenesis: Formation of new blood vessels 2 - Scar formation: Migration & proliferation of fibroblasts with deposition of ECM. 3 - Remodeling: Maturation and reorganization of the fibrous tissue. 4 - Wound contraction: Reduction of wound size.
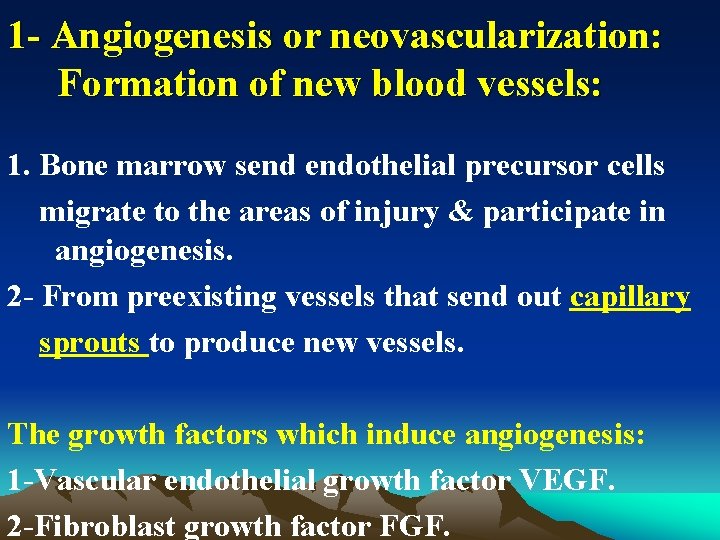
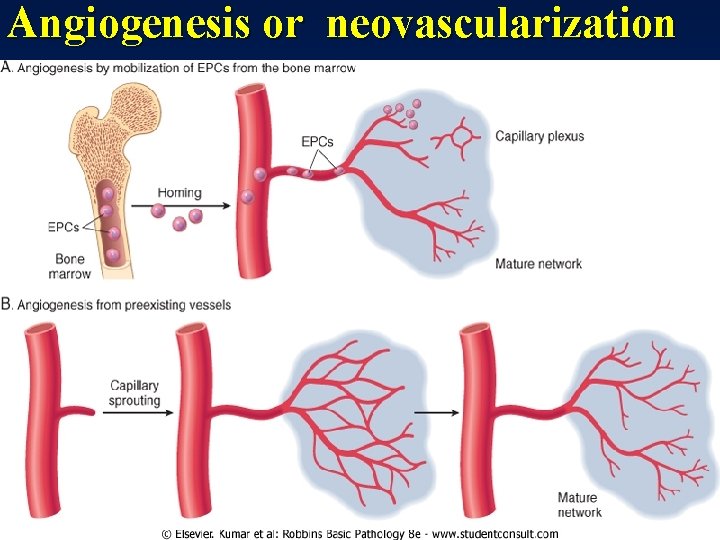
1 - Angiogenesis or neovascularization: Formation of new blood vessels: 1. Bone marrow send endothelial precursor cells migrate to the areas of injury & participate in angiogenesis. 2 - From preexisting vessels that send out capillary sprouts to produce new vessels. The growth factors which induce angiogenesis: 1 -Vascular endothelial growth factor VEGF. 2 -Fibroblast growth factor FGF.
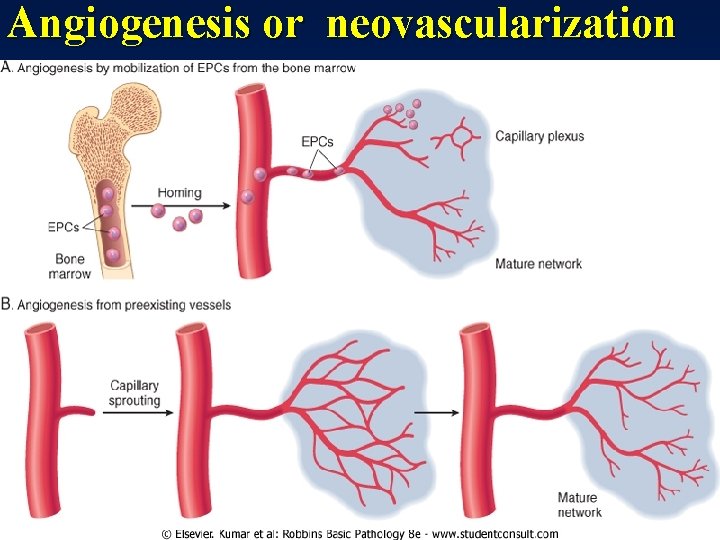
Angiogenesis or neovascularization
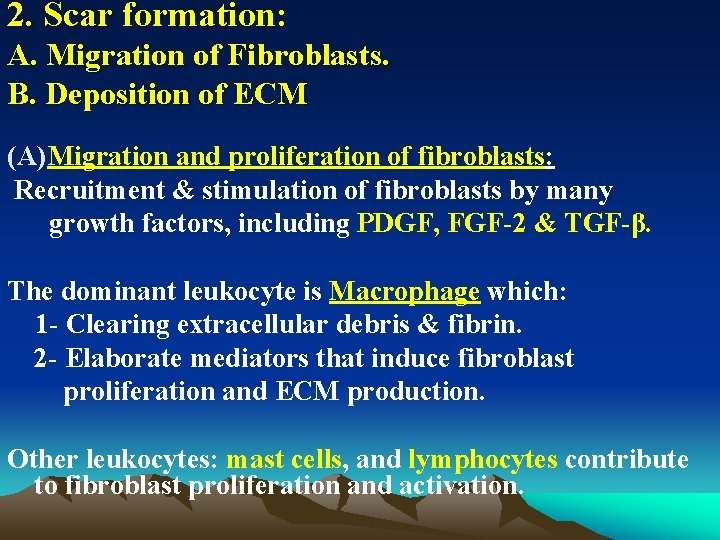
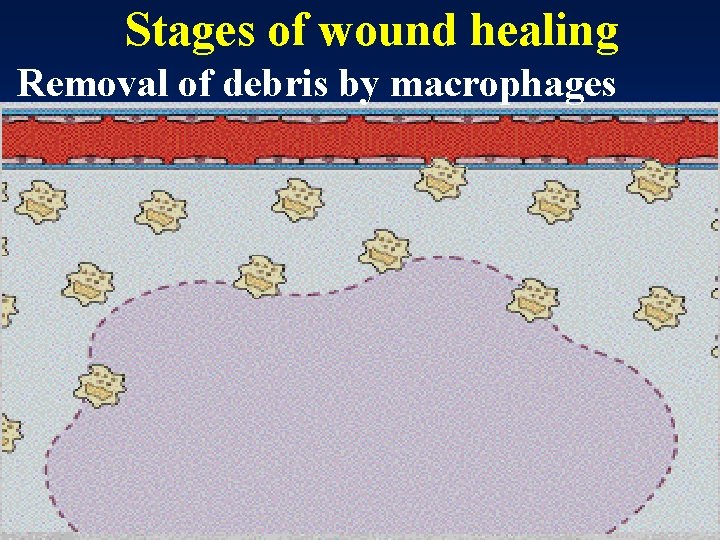
2. Scar formation: A. Migration of Fibroblasts. B. Deposition of ECM (A) Migration and proliferation of fibroblasts: Recruitment & stimulation of fibroblasts by many growth factors, including PDGF, FGF-2 & TGF-β. The dominant leukocyte is Macrophage which: 1 - Clearing extracellular debris & fibrin. 2 - Elaborate mediators that induce fibroblast proliferation and ECM production. Other leukocytes: mast cells, and lymphocytes contribute to fibroblast proliferation and activation.
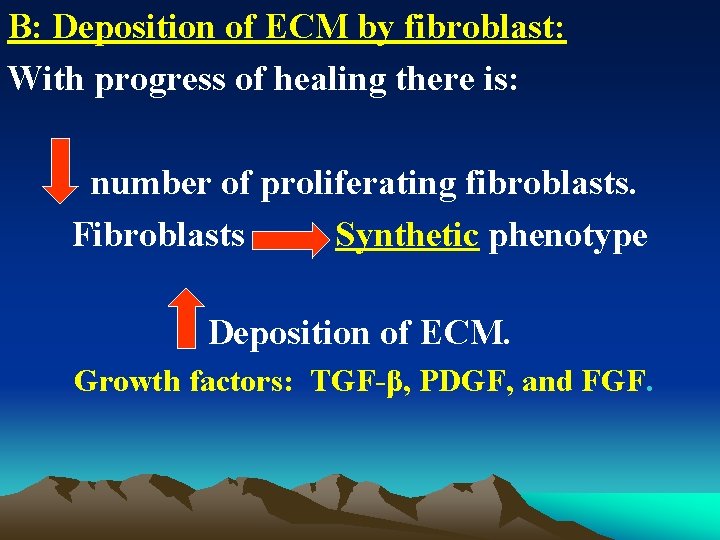
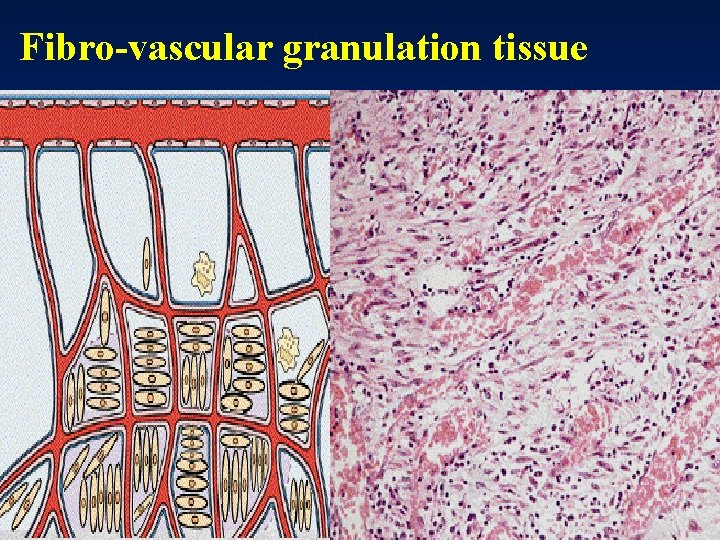
B: Deposition of ECM by fibroblast: With progress of healing there is: number of proliferating fibroblasts. Fibroblasts Synthetic phenotype Deposition of ECM. Growth factors: TGF-β, PDGF, and FGF.
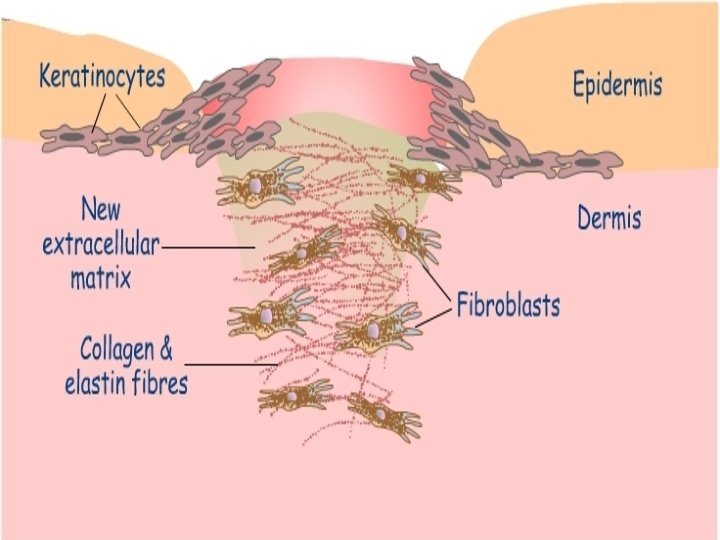
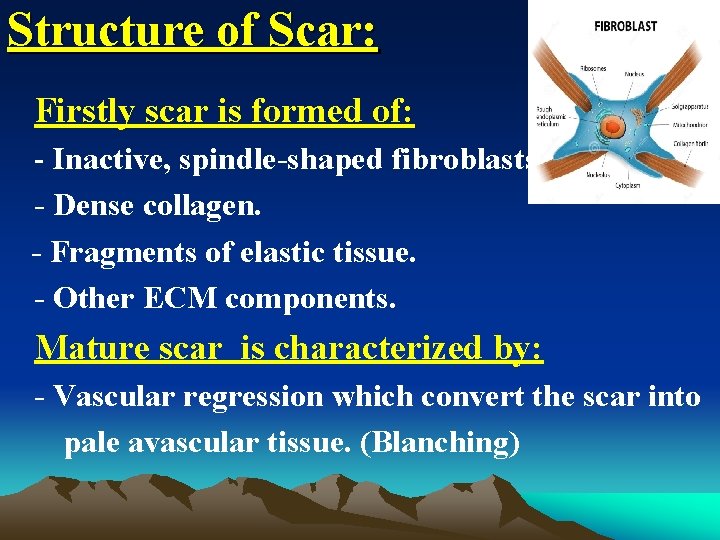
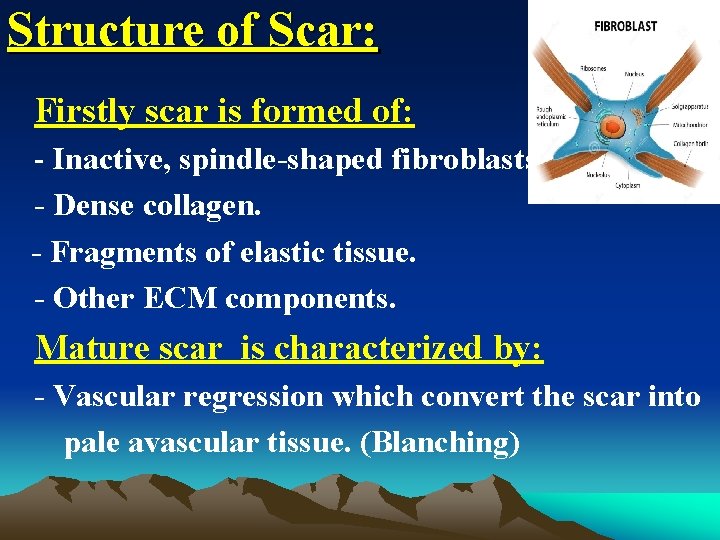
Structure of Scar: Firstly scar is formed of: - Inactive, spindle-shaped fibroblasts. - Dense collagen. - Fragments of elastic tissue. - Other ECM components. Mature scar is characterized by: - Vascular regression which convert the scar into pale avascular tissue. (Blanching)
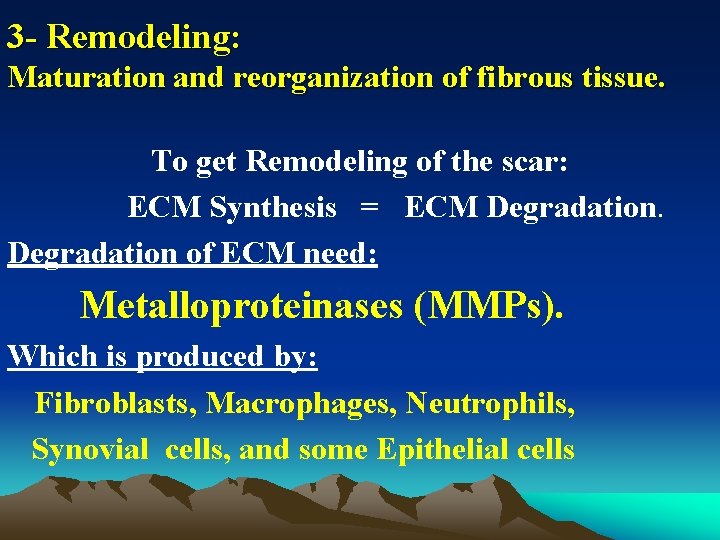
3 - Remodeling: Maturation and reorganization of fibrous tissue. To get Remodeling of the scar: ECM Synthesis = ECM Degradation of ECM need: Metalloproteinases (MMPs). Which is produced by: Fibroblasts, Macrophages, Neutrophils, Synovial cells, and some Epithelial cells
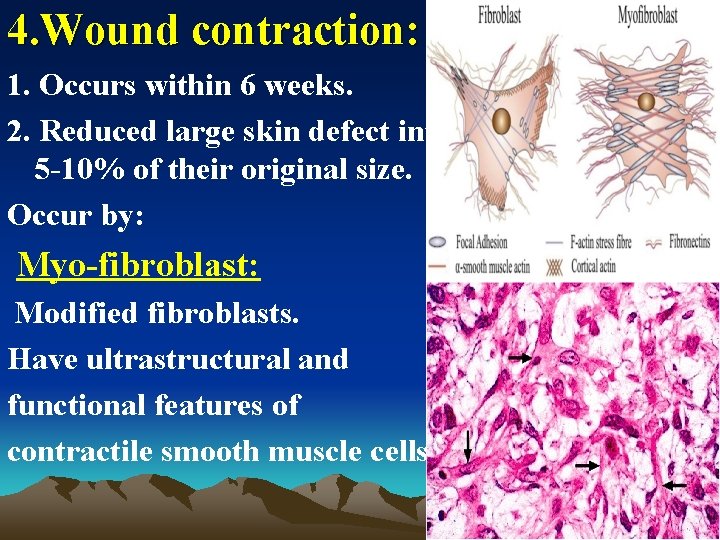
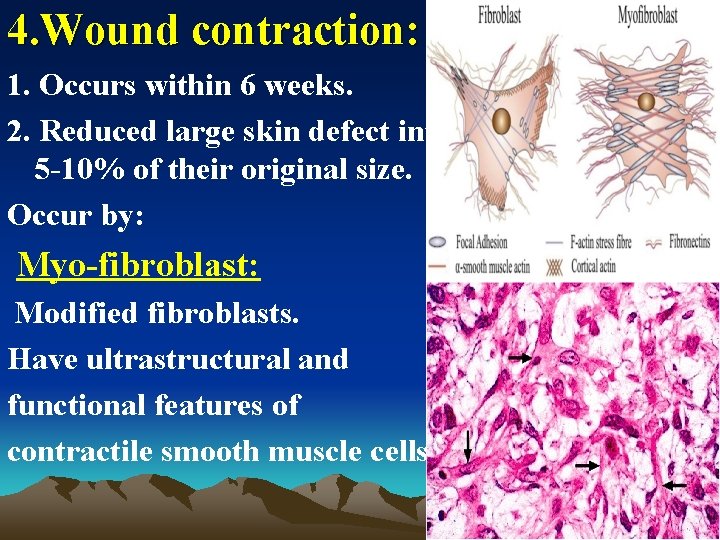
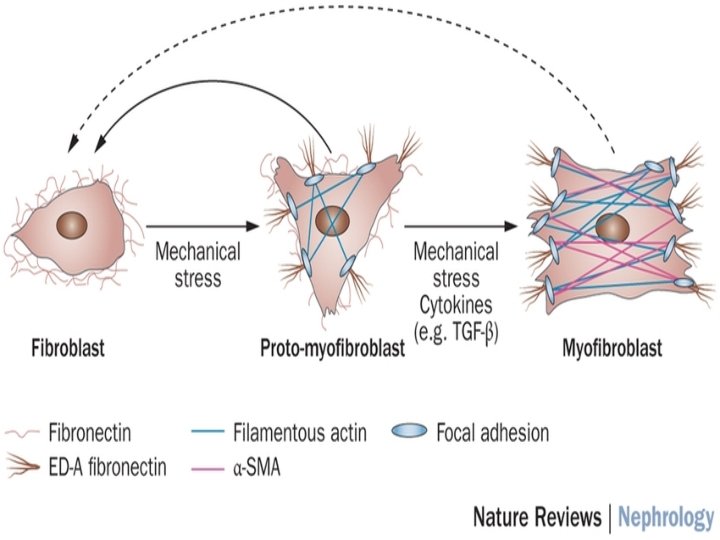
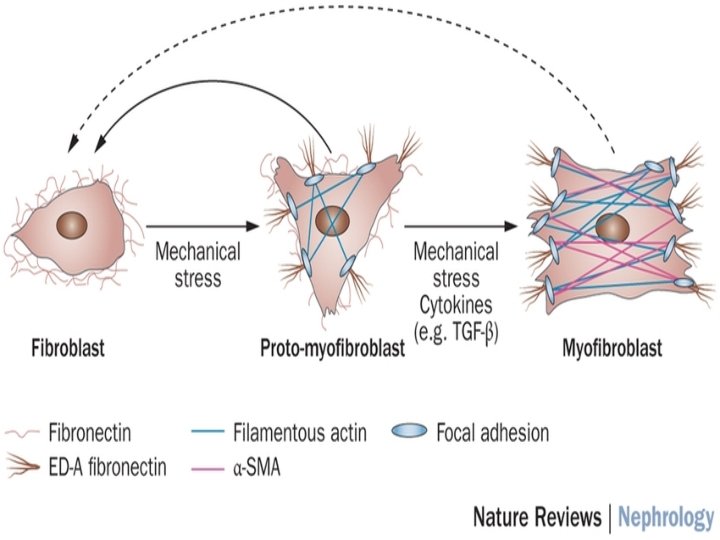
4. Wound contraction: 1. Occurs within 6 weeks. 2. Reduced large skin defect into 5 -10% of their original size. Occur by: Myo-fibroblast: Modified fibroblasts. Have ultrastructural and functional features of contractile smooth muscle cells.
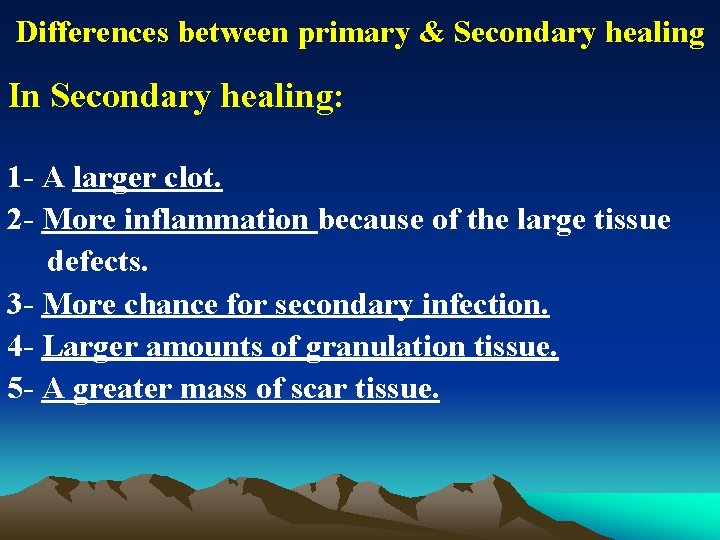
Differences between primary & Secondary healing In Secondary healing: 1 - A larger clot. 2 - More inflammation because of the large tissue defects. 3 - More chance for secondary infection. 4 - Larger amounts of granulation tissue. 5 - A greater mass of scar tissue.
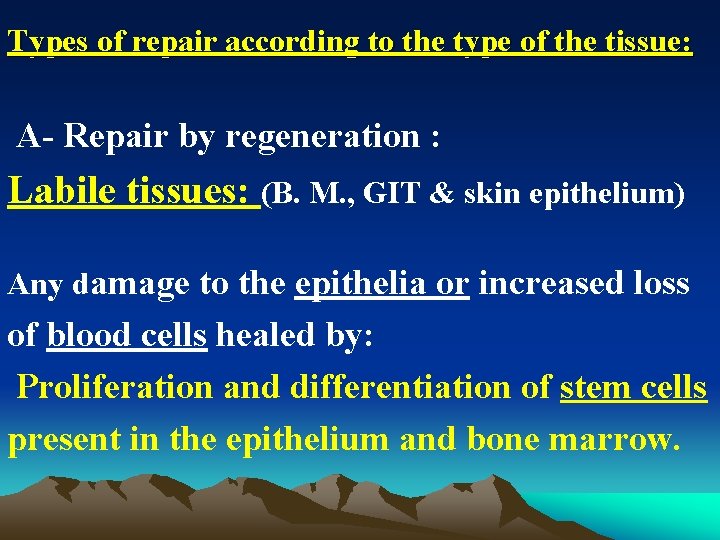
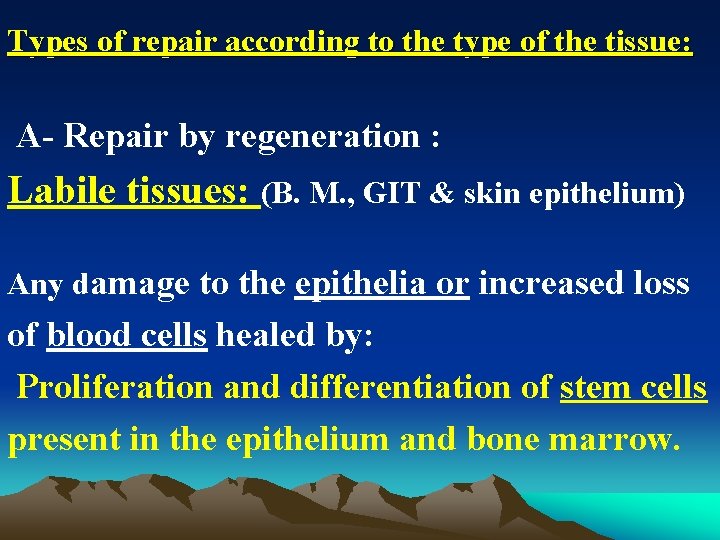
Types of repair according to the type of the tissue: A- Repair by regeneration : Labile tissues: (B. M. , GIT & skin epithelium) Any damage to the epithelia or increased loss of blood cells healed by: Proliferation and differentiation of stem cells present in the epithelium and bone marrow.
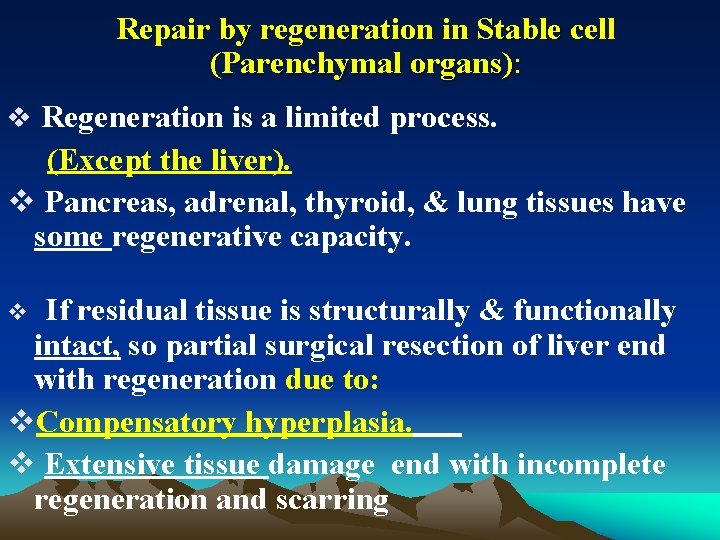
Repair by regeneration in Stable cell (Parenchymal organs): v Regeneration is a limited process. (Except the liver). v Pancreas, adrenal, thyroid, & lung tissues have some regenerative capacity. If residual tissue is structurally & functionally intact, so partial surgical resection of liver end with regeneration due to: v. Compensatory hyperplasia. v Extensive tissue damage end with incomplete regeneration and scarring v
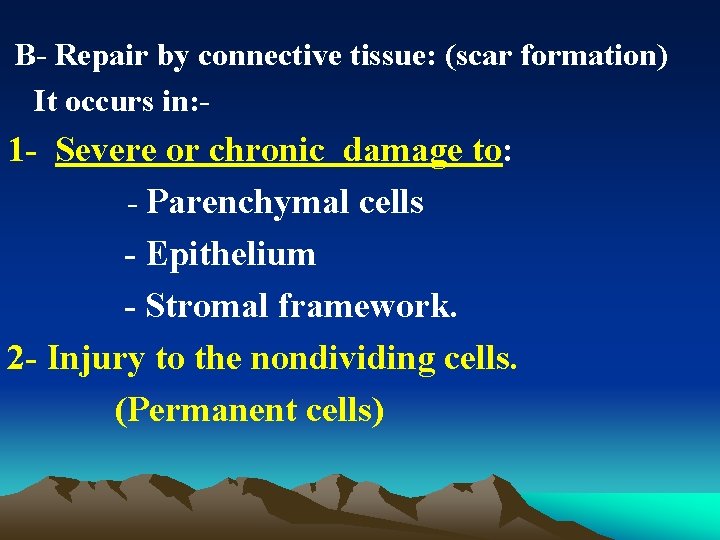
B- Repair by connective tissue: (scar formation) It occurs in: - 1 - Severe or chronic damage to: - Parenchymal cells - Epithelium - Stromal framework. 2 - Injury to the nondividing cells. (Permanent cells)
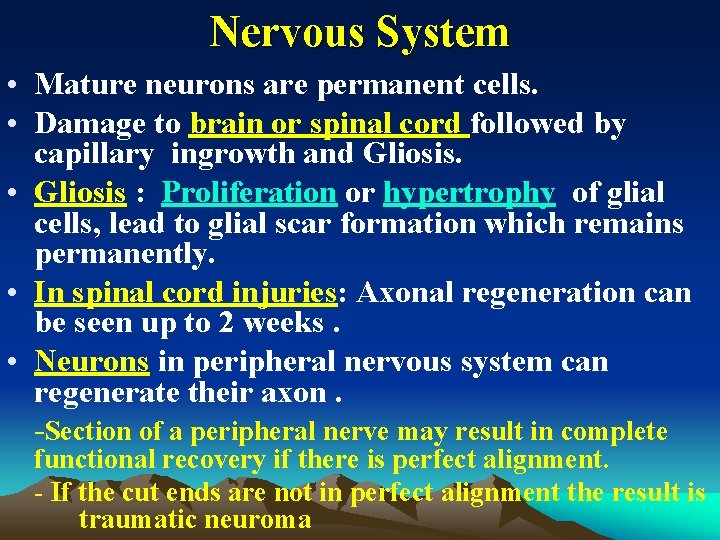
Nervous System • Mature neurons are permanent cells. • Damage to brain or spinal cord followed by capillary ingrowth and Gliosis. • Gliosis : Proliferation or hypertrophy of glial cells, lead to glial scar formation which remains permanently. • In spinal cord injuries: Axonal regeneration can be seen up to 2 weeks. • Neurons in peripheral nervous system can regenerate their axon. -Section of a peripheral nerve may result in complete functional recovery if there is perfect alignment. - If the cut ends are not in perfect alignment the result is traumatic neuroma
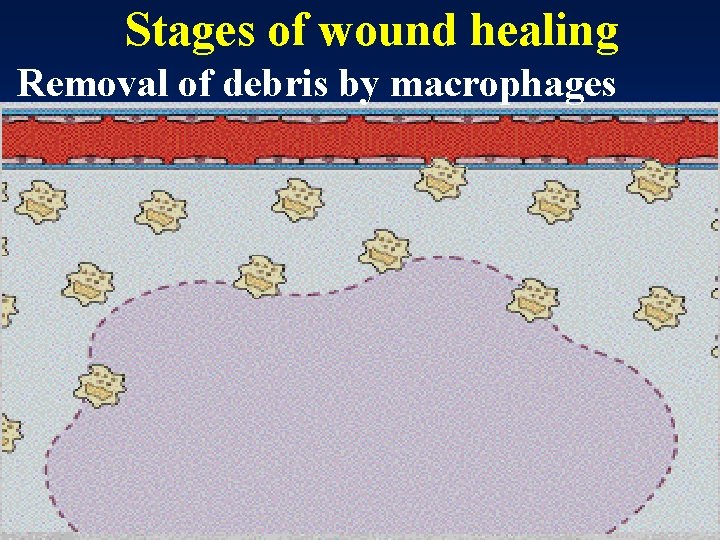
Stages of wound healing Removal of debris by macrophages
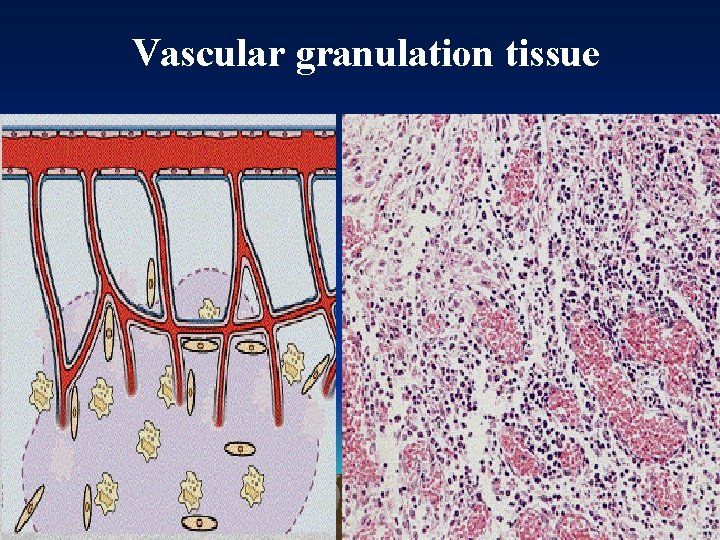
Vascular granulation tissue
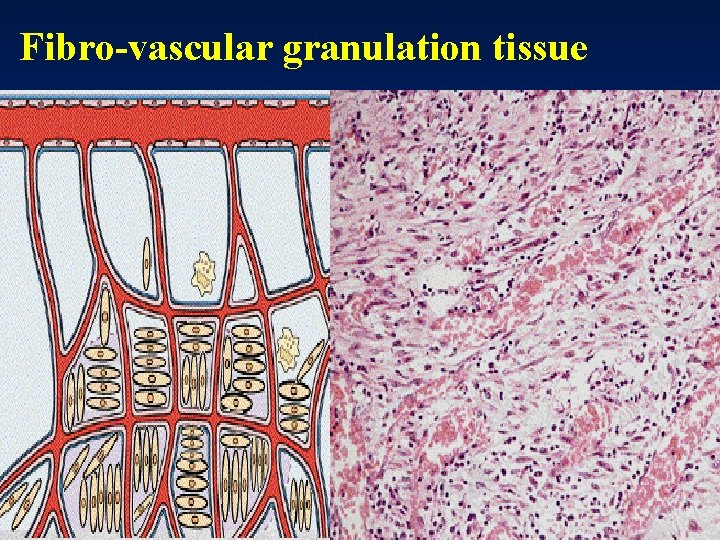
Fibro-vascular granulation tissue
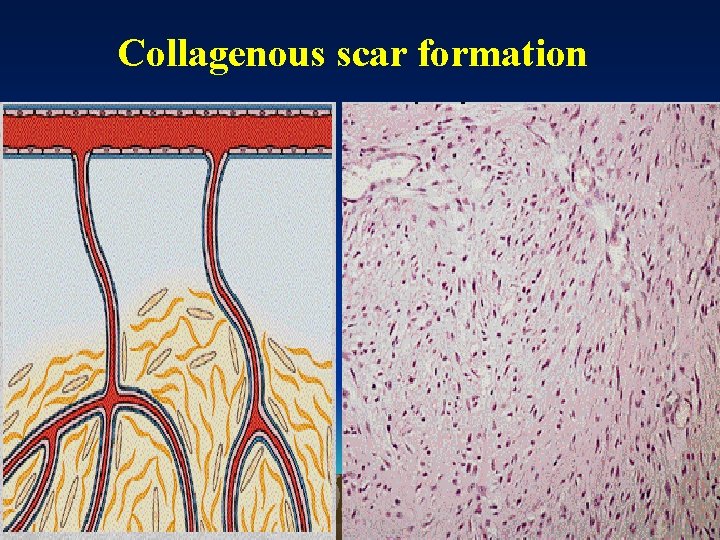
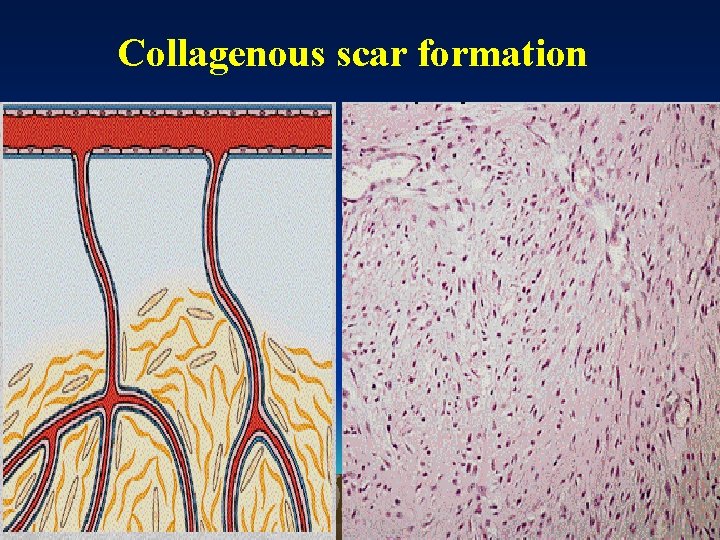
Collagenous scar formation
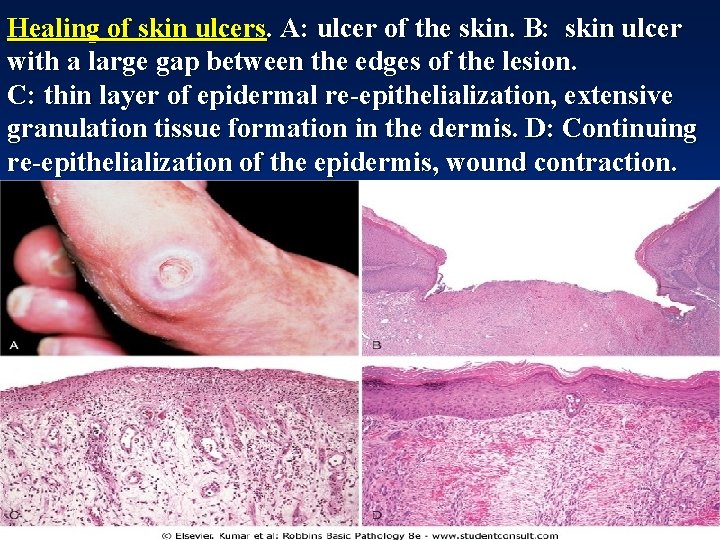
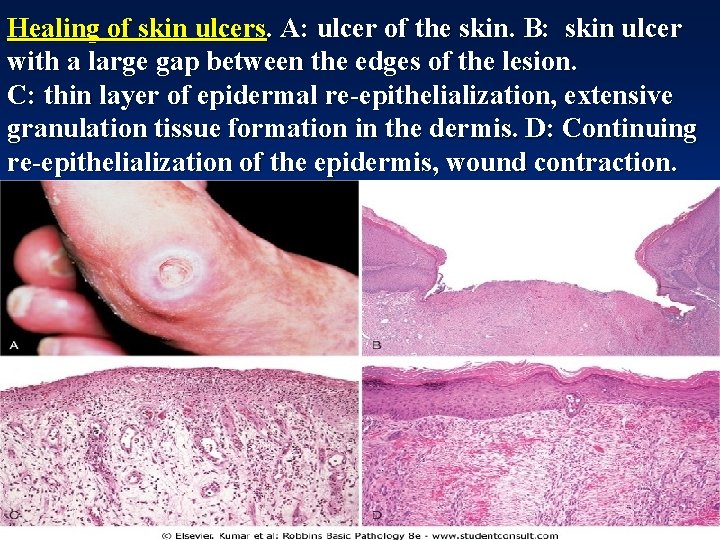
Healing of skin ulcers. A: ulcer of the skin. B: skin ulcer with a large gap between the edges of the lesion. C: thin layer of epidermal re-epithelialization, extensive granulation tissue formation in the dermis. D: Continuing re-epithelialization of the epidermis, wound contraction.

Healing scar in skin


Thank you