Headaches Ioanna Zimianiti https www icsmmeded com 44



- Slides: 89

Headaches Ioanna Zimianiti https: //www. icsmmeded. com/ 44 35 22
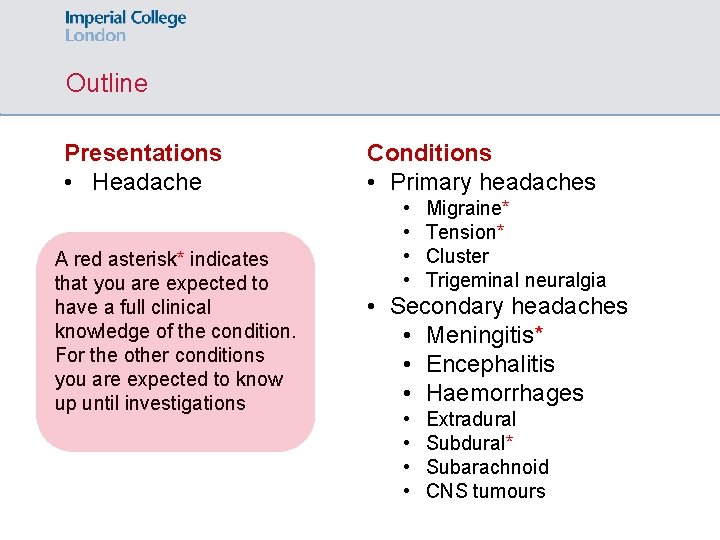
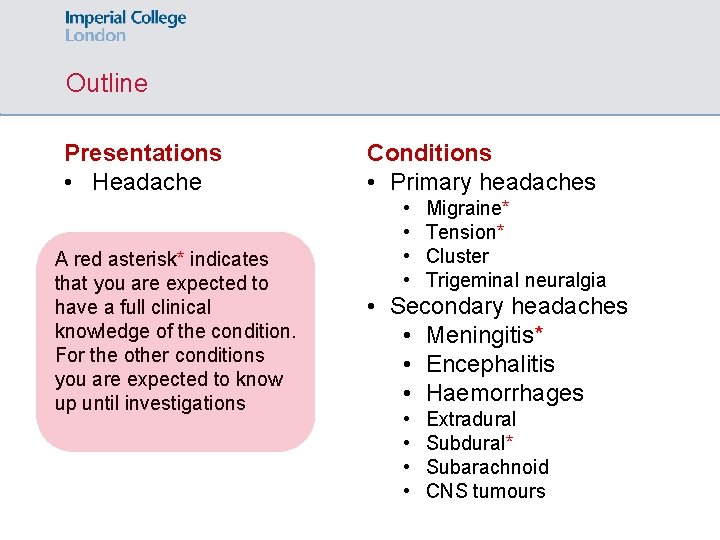
Outline Presentations • Headache A red asterisk* indicates that you are expected to have a full clinical knowledge of the condition. For the other conditions you are expected to know up until investigations Conditions • Primary headaches • • Migraine* Tension* Cluster Trigeminal neuralgia • Secondary headaches • Meningitis* • Encephalitis • Haemorrhages • • Extradural Subdural* Subarachnoid CNS tumours
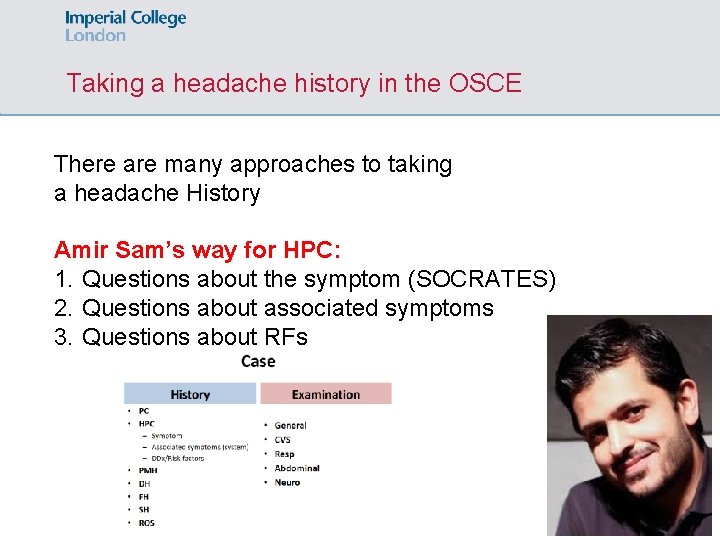
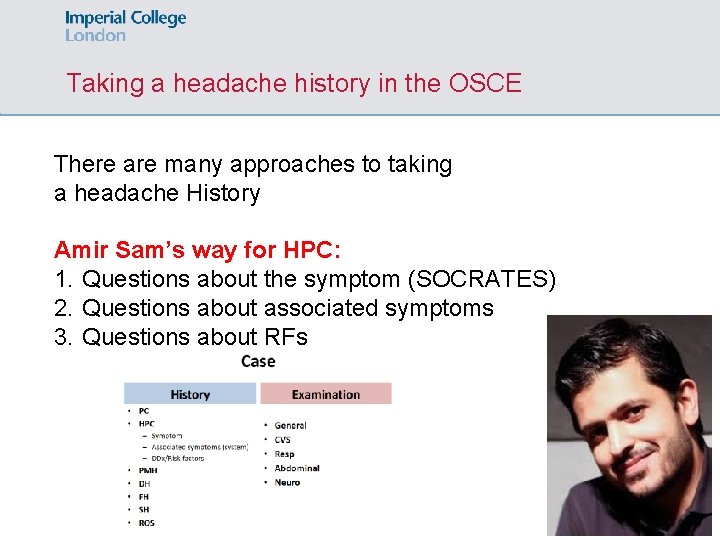
Taking a headache history in the OSCE There are many approaches to taking a headache History Amir Sam’s way for HPC: 1. Questions about the symptom (SOCRATES) 2. Questions about associated symptoms 3. Questions about RFs
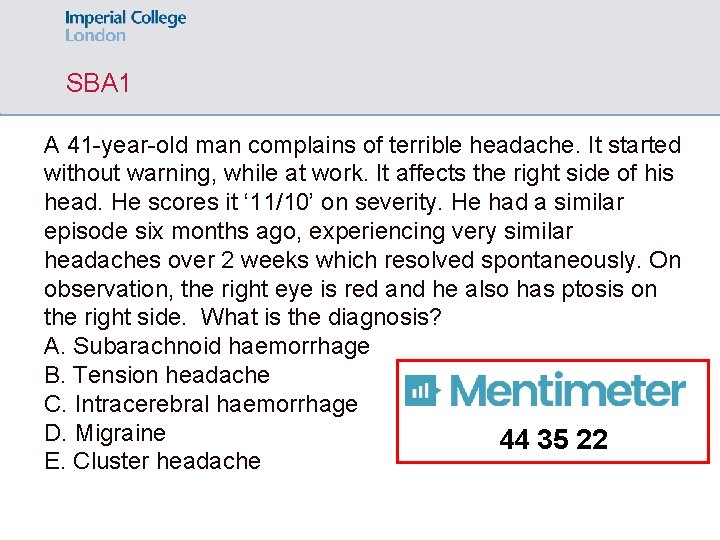
SBA 1 A 41 -year-old man complains of terrible headache. It started without warning, while at work. It affects the right side of his head. He scores it ‘ 11/10’ on severity. He had a similar episode six months ago, experiencing very similar headaches over 2 weeks which resolved spontaneously. On observation, the right eye is red and he also has ptosis on the right side. What is the diagnosis? A. Subarachnoid haemorrhage B. Tension headache C. Intracerebral haemorrhage D. Migraine 44 35 22 E. Cluster headache
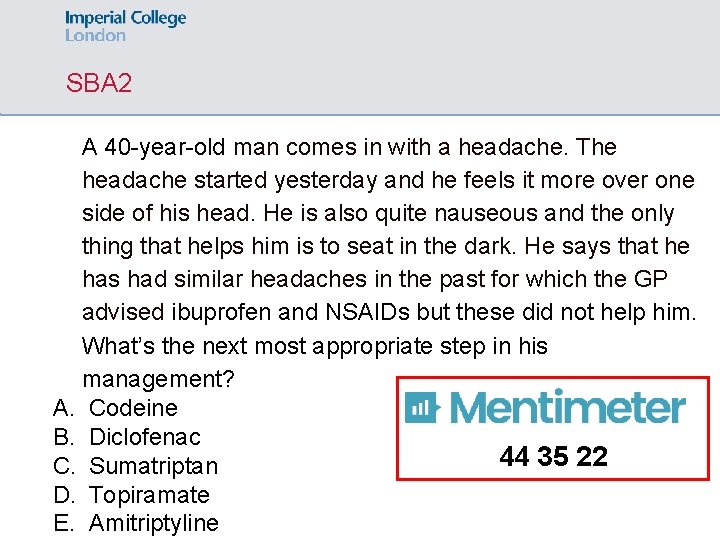
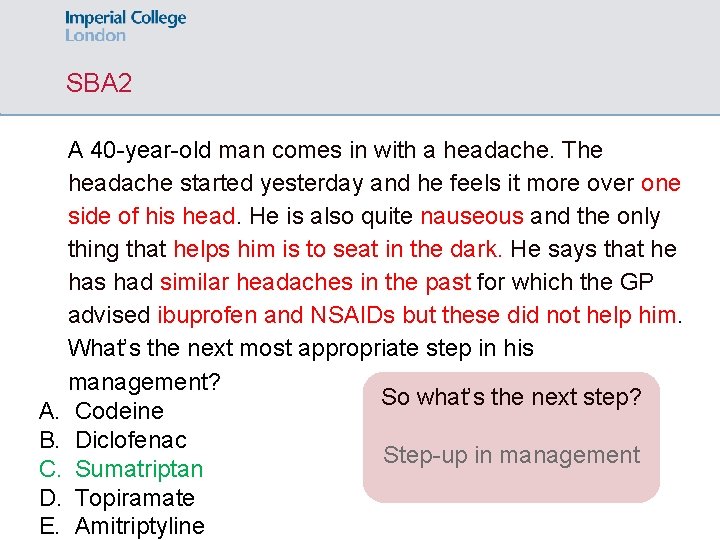
SBA 2 A 40 -year-old man comes in with a headache. The headache started yesterday and he feels it more over one side of his head. He is also quite nauseous and the only thing that helps him is to seat in the dark. He says that he has had similar headaches in the past for which the GP advised ibuprofen and NSAIDs but these did not help him. What’s the next most appropriate step in his management? A. Codeine B. Diclofenac 44 35 22 C. Sumatriptan D. Topiramate E. Amitriptyline
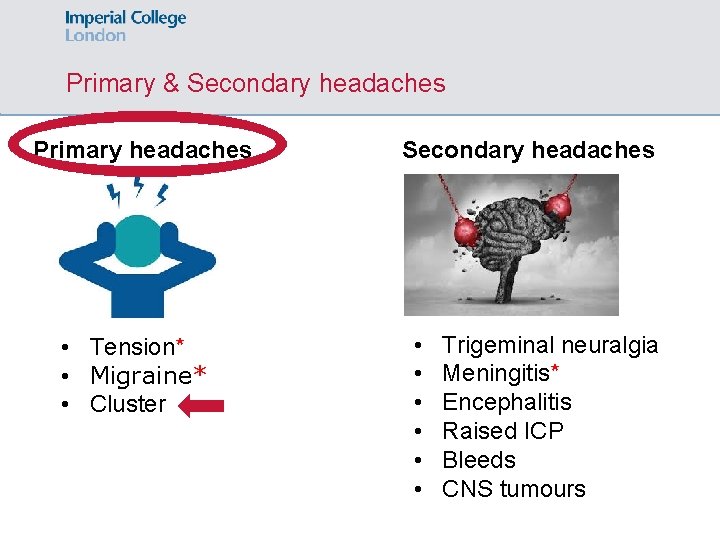
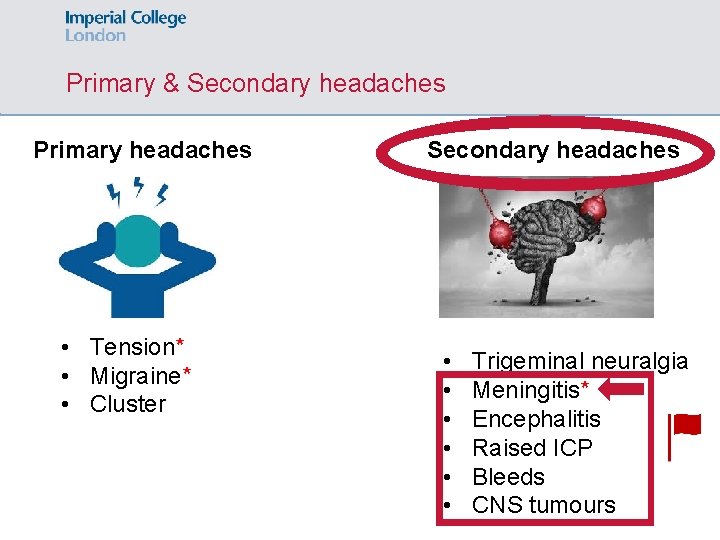
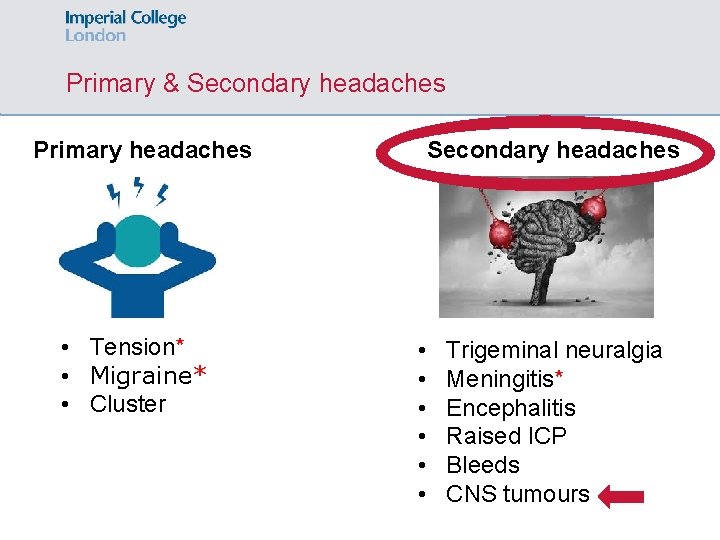
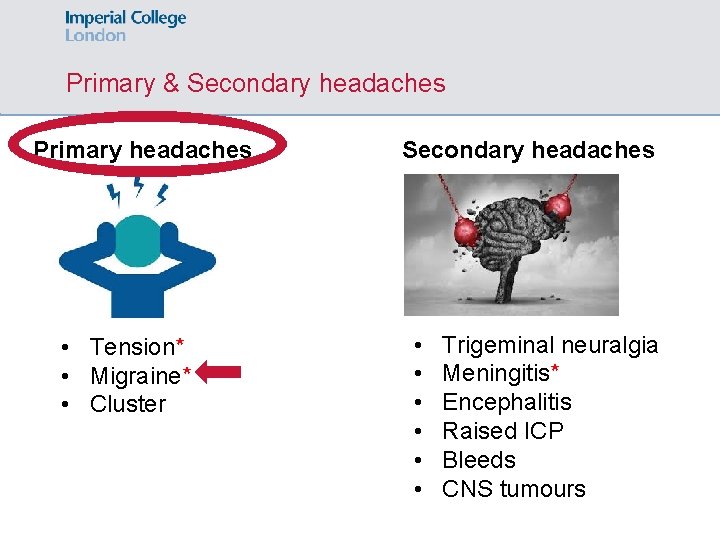
Primary & Secondary headaches Primary headaches • Tension* • Migraine* • Cluster Secondary headaches • • • Trigeminal neuralgia Meningitis* Encephalitis Raised ICP Bleeds CNS tumours
Tension headache*: Definition, Aetiology & Epidemiology Definition: the most common type of headache, which is considered a normal, everyday headache. Aetiology: muscle contraction? Epidemiology: , young
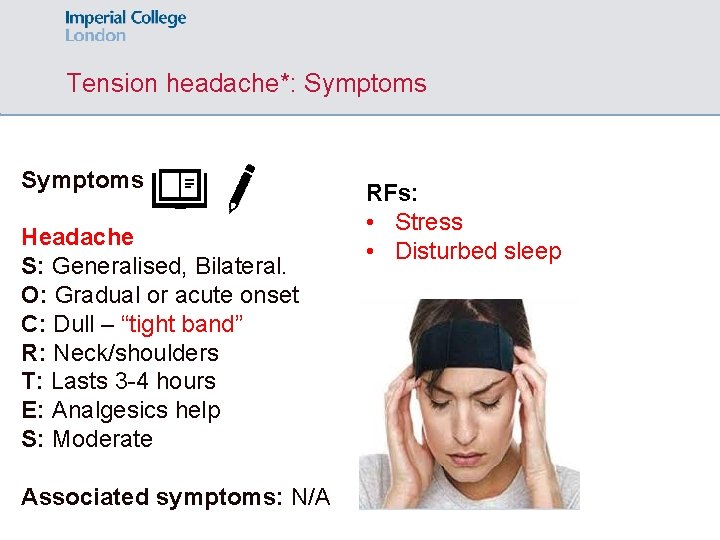
Tension headache*: Symptoms Headache S: Generalised, Bilateral. O: Gradual or acute onset C: Dull – “tight band” R: Neck/shoulders T: Lasts 3 -4 hours E: Analgesics help S: Moderate Associated symptoms: N/A RFs: • Stress • Disturbed sleep
Tension headache: Examination - Management Examination: Normal Investigations: N/A Management: • Conservative: Headache diaries (avoid triggers, relaxation) Medical: Simple analgesia (paracetamol, ibuprofen) IMPORTANT: Beware of medication-overuse headaches
Primary & Secondary headaches Primary headaches • Tension* • Migraine* • Cluster Secondary headaches • • • Trigeminal neuralgia Meningitis* Encephalitis Raised ICP Bleeds CNS tumours
Migraine*: Definition & Aetiology Definition: Migraine is a chronic condition that causes attacks of headaches Aetiology: Inflammation of the trigeminal nerve changes the way that the brain process stimuli
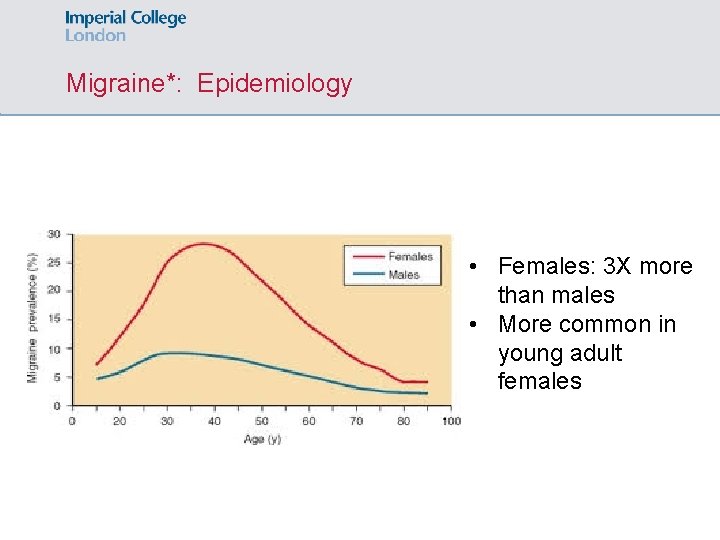
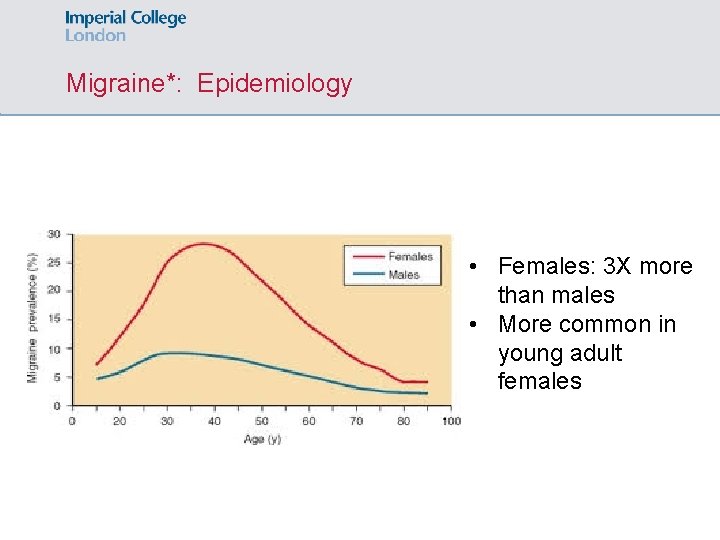
Migraine*: Epidemiology • Females: 3 X more than males • More common in young adult females
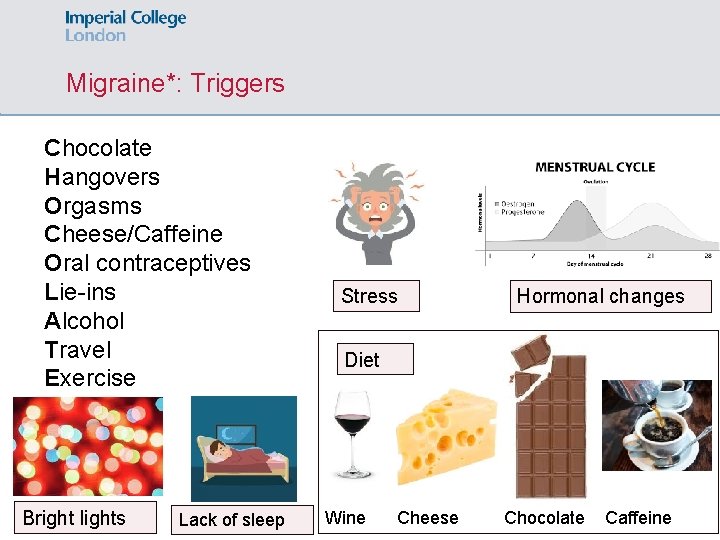
Migraine*: Triggers
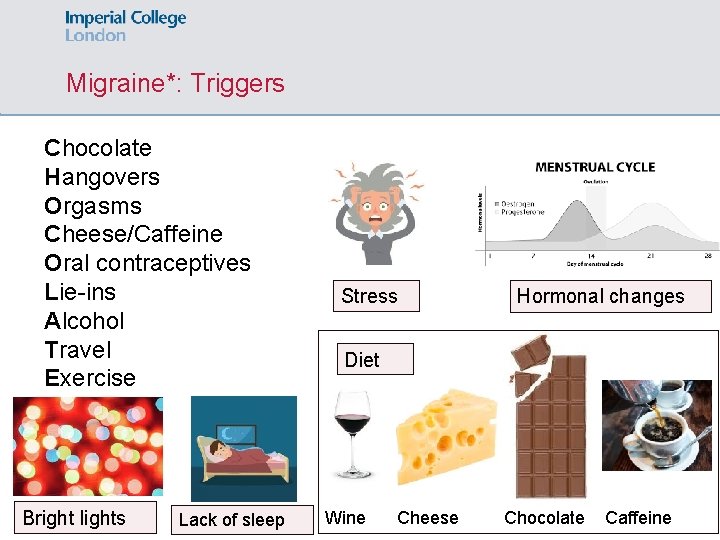
Migraine*: Triggers Chocolate Hangovers Orgasms Cheese/Caffeine Oral contraceptives Lie-ins Alcohol Travel Exercise Bright lights Lack of sleep Stress Hormonal changes Diet Wine Cheese Chocolate Caffeine
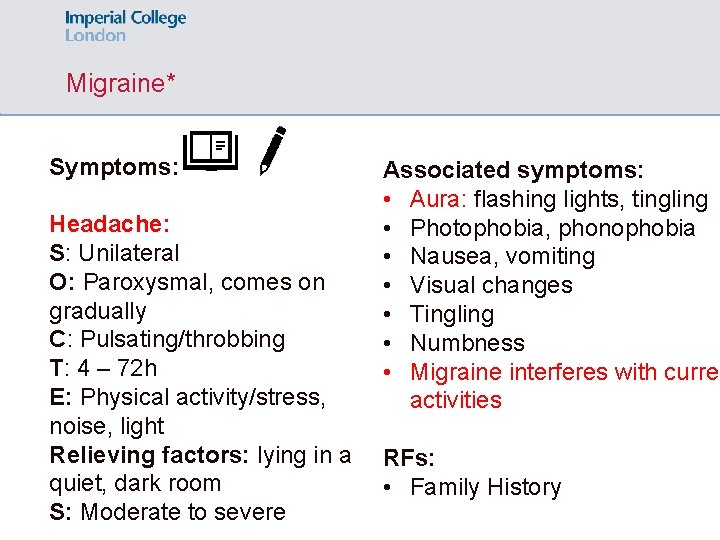
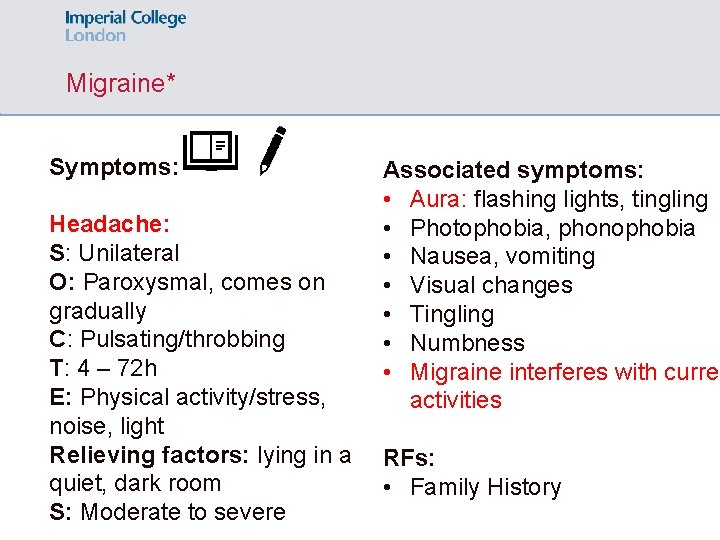
Migraine* Symptoms: Headache: S: Unilateral O: Paroxysmal, comes on gradually C: Pulsating/throbbing T: 4 – 72 h E: Physical activity/stress, noise, light Relieving factors: lying in a quiet, dark room S: Moderate to severe Associated symptoms: • Aura: flashing lights, tingling • Photophobia, phonophobia • Nausea, vomiting • Visual changes • Tingling • Numbness • Migraine interferes with curren activities RFs: • Family History
Migraine*: Investigations Migraine is a CLINICAL diagnosis Investigations only to exclude sinister causes

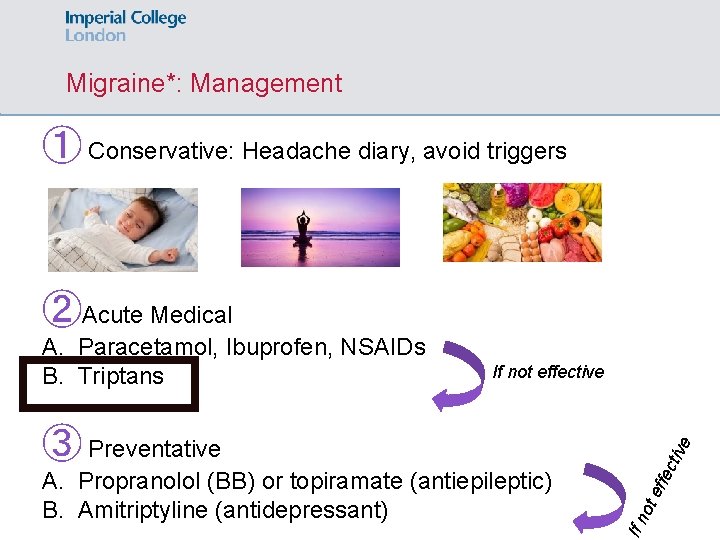
Migraine*: Management ① Conservative: Headache diary, avoid triggers ②Acute Medical A. Paracetamol, Ibuprofen, NSAIDs B. Triptans If not effective ctiv ffe ot e If n A. Propranolol (BB) or topiramate (antiepileptic) B. Amitriptyline (antidepressant) e ③ Preventative
SBA 2 A 40 -year-old man comes in with a headache. The headache started yesterday and he feels it more over one side of his head. He is also quite nauseous and the only thing that helps him is to seat in the dark. He says that he has had similar headaches in the past for which the GP advised ibuprofen and NSAIDs but these did not help him. What’s the next most appropriate step in his management? What’s the diagnosis? A. Codeine B. Diclofenac Migraine C. Sumatriptan D. Topiramate E. Amitriptyline
SBA 2 A 40 -year-old man comes in with a headache. The headache started yesterday and he feels it more over one side of his head. He is also quite nauseous and the only thing that helps him is to seat in the dark. He says that he has had similar headaches in the past for which the GP advised ibuprofen and NSAIDs but these did not help him. What’s the next most appropriate step in his management? So what’s the next step? A. Codeine B. Diclofenac Step-up in management C. Sumatriptan D. Topiramate E. Amitriptyline
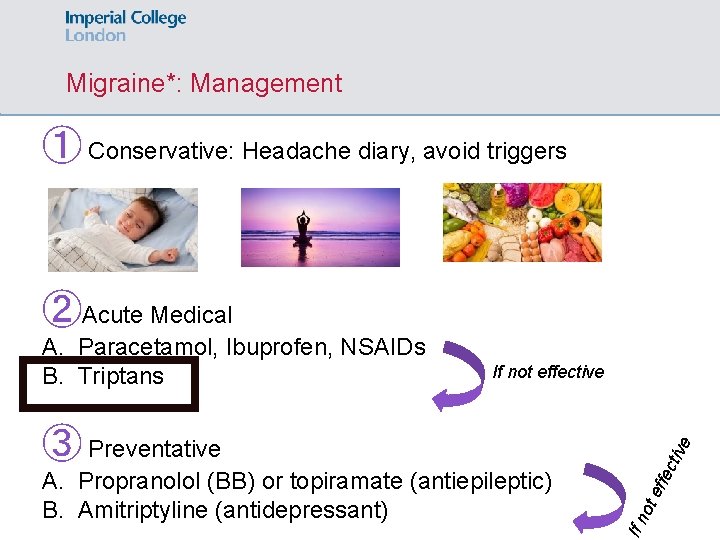
Migraine*: Management ① Conservative: Headache diary, avoid triggers ②Acute Medical A. Paracetamol, Ibuprofen, NSAIDs B. Triptans If not effective ctiv ffe ot e If n A. Propranolol (BB) or topiramate (antiepileptic) B. Amitriptyline (antidepressant) e ③ Preventative
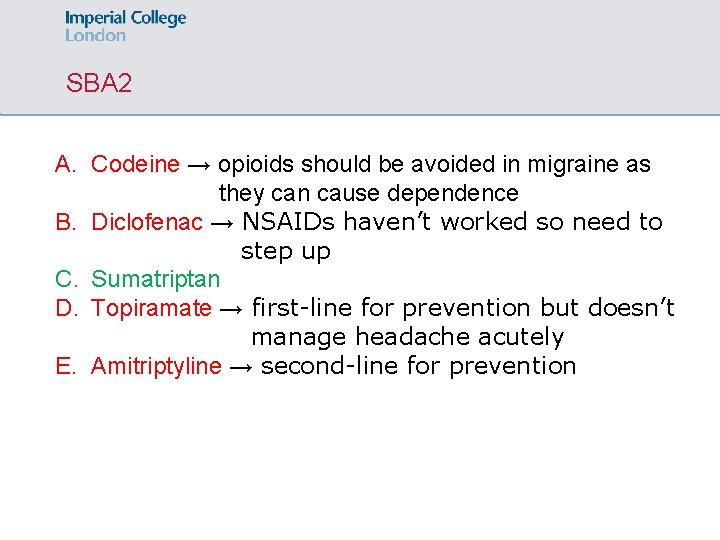
SBA 2 A. Codeine → opioids should be avoided in migraine as they can cause dependence B. Diclofenac → NSAIDs haven’t worked so need to step up C. Sumatriptan D. Topiramate → first-line for prevention but doesn’t manage headache acutely E. Amitriptyline → second-line for prevention
Primary & Secondary headaches Primary headaches • Tension* • Migraine* • Cluster Secondary headaches • • • Trigeminal neuralgia Meningitis* Encephalitis Raised ICP Bleeds CNS tumours
Cluster headache: Definition & Epidemiology Definition: A neurological disorder characterized by recurrent, severe headaches on one side of the head, which occur at a cyclical pattern Epidemiology: , 20 -40 years old
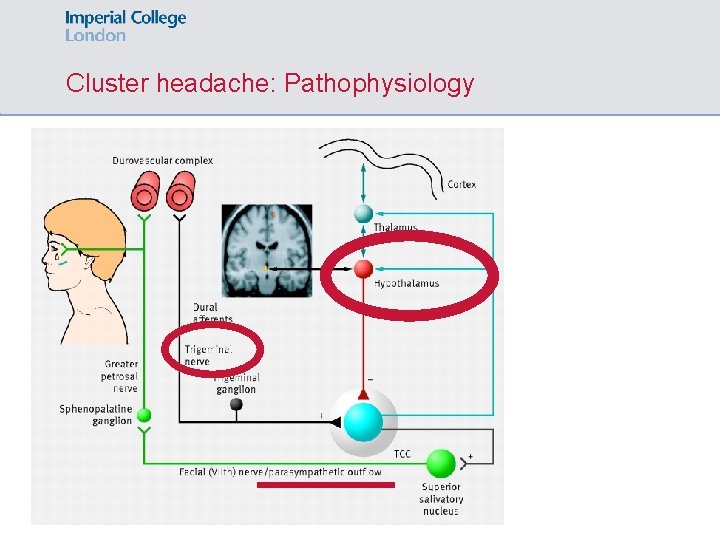
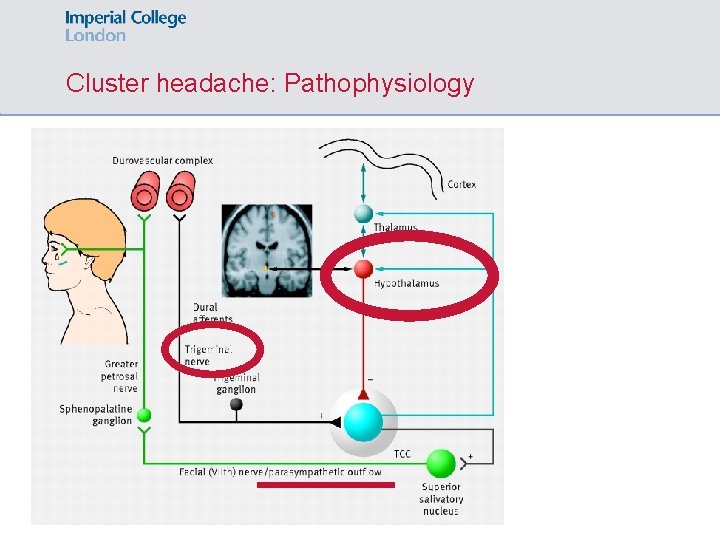
Cluster headache: Pathophysiology
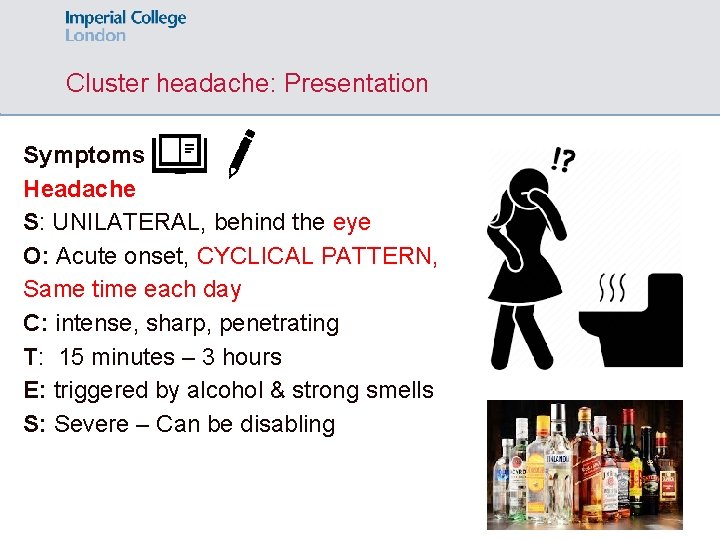
Cluster headache: Presentation Symptoms Headache S: UNILATERAL, behind the eye O: Acute onset, CYCLICAL PATTERN, Same time each day C: intense, sharp, penetrating T: 15 minutes – 3 hours E: triggered by alcohol & strong smells S: Severe – Can be disabling
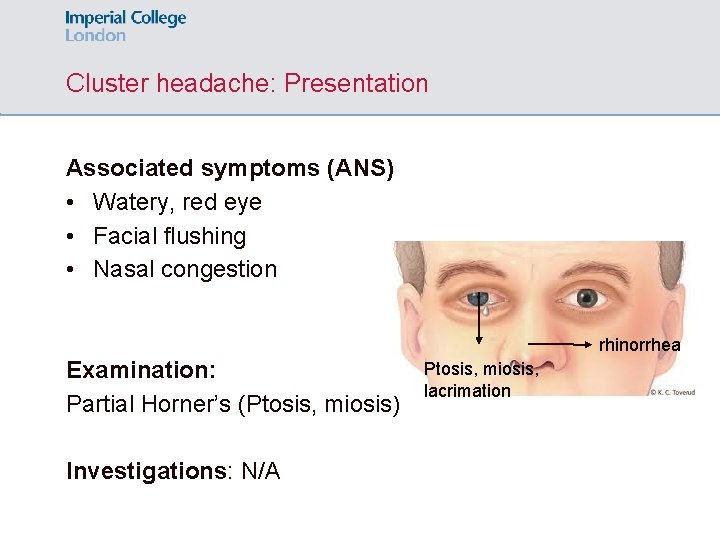
Cluster headache: Presentation Associated symptoms (ANS) • Watery, red eye • Facial flushing • Nasal congestion rhinorrhea Examination: Partial Horner’s (Ptosis, miosis) Investigations: N/A Ptosis, miosis, lacrimation
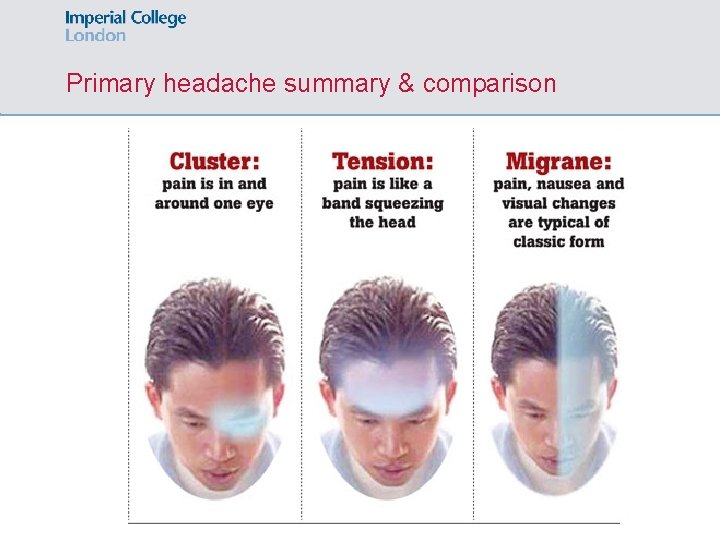
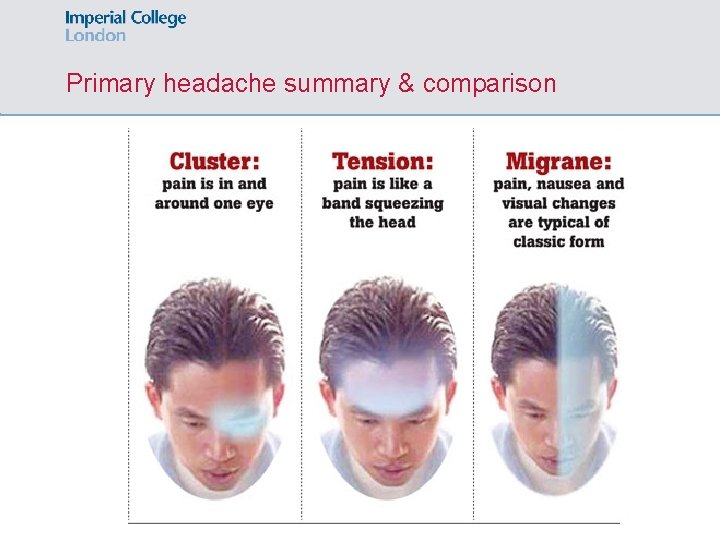
Primary headache summary & comparison
SBA 1 A 41 -year-old man complains of terrible headache. It started without warning, while at work. It affects the right side of his head. He scores it ‘ 11/10’ in severity. He had a similar episode six months ago, experiencing very similar headaches over 2 weeks which resolved spontaneously. On observation, he right side is red and he also has ptosis on the right side. What is the diagnosis? A. Subarachnoid haemorrhage B. Tension headache C. Intracerebral haemorrhage D. Migraine E. Cluster headache
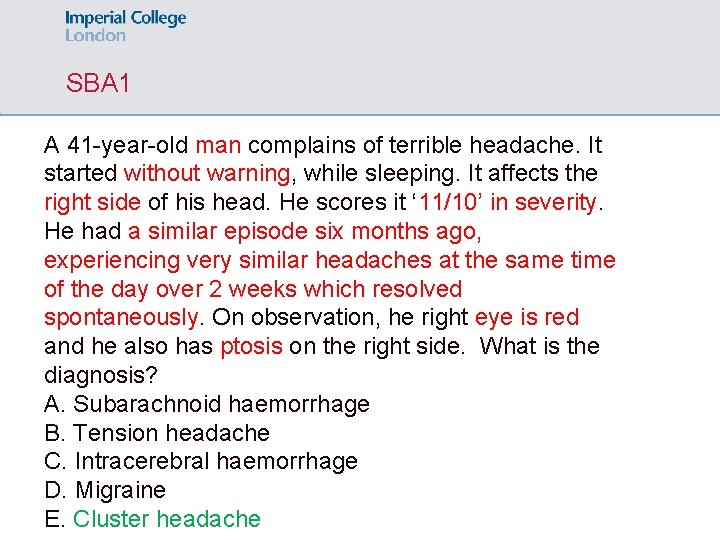
SBA 1 A 41 -year-old man complains of terrible headache. It started without warning, while sleeping. It affects the right side of his head. He scores it ‘ 11/10’ in severity. He had a similar episode six months ago, experiencing very similar headaches at the same time of the day over 2 weeks which resolved spontaneously. On observation, he right eye is red and he also has ptosis on the right side. What is the diagnosis? A. Subarachnoid haemorrhage B. Tension headache C. Intracerebral haemorrhage D. Migraine E. Cluster headache
SBA 1 A. Subarachnoid haemorrhage → not recurrent, no ANS symptoms B. Tension headache → no ANS symptoms C. Intracerebral haemorrhage not recurrent, no ANS symptoms D. Migraine → no ANS symptoms E. Cluster headache
Primary & Secondary headaches Primary headaches • Tension* • Migraine* • Cluster Secondary headaches • • • Trigeminal neuralgia Meningitis* Encephalitis Raised ICP Bleeds CNS tumours
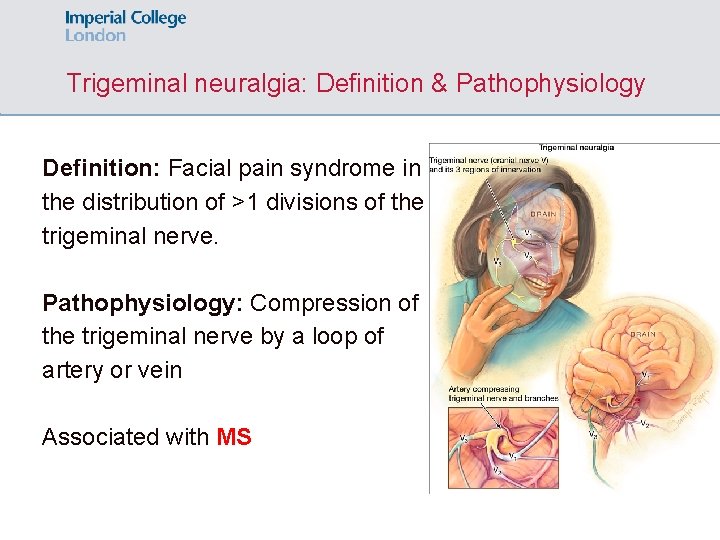
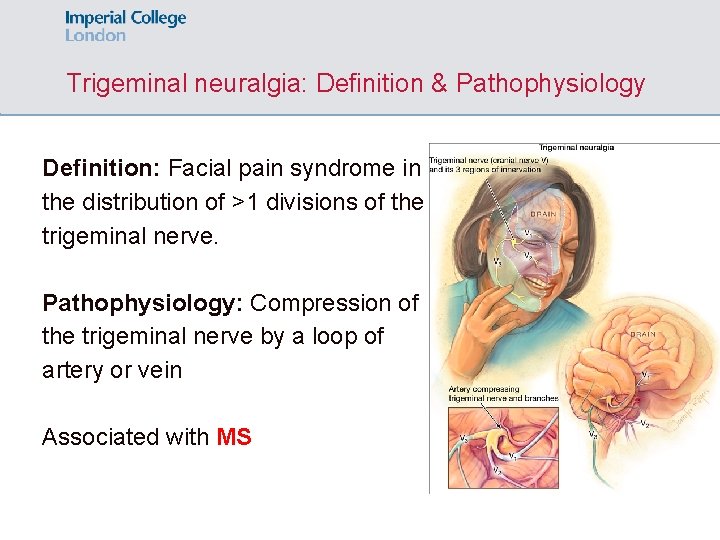
Trigeminal neuralgia: Definition & Pathophysiology Definition: Facial pain syndrome in the distribution of >1 divisions of the trigeminal nerve. Pathophysiology: Compression of the trigeminal nerve by a loop of artery or vein Associated with MS
Trigeminal neuralgia: Triggers

Trigeminal neuralgia: Triggers
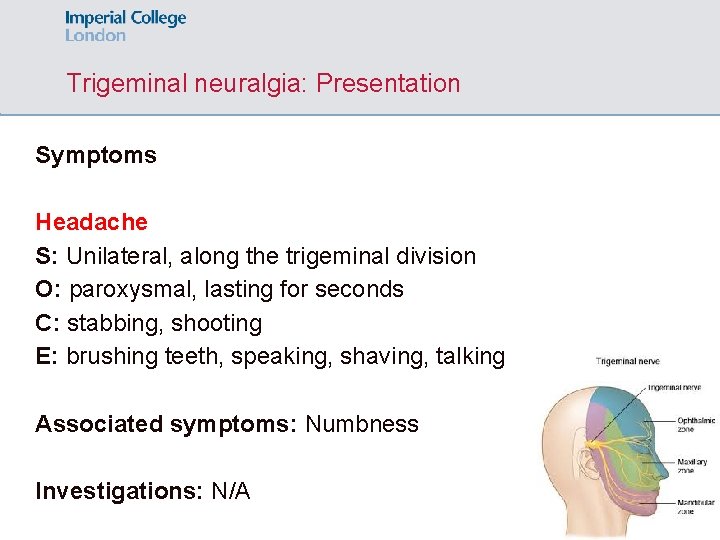
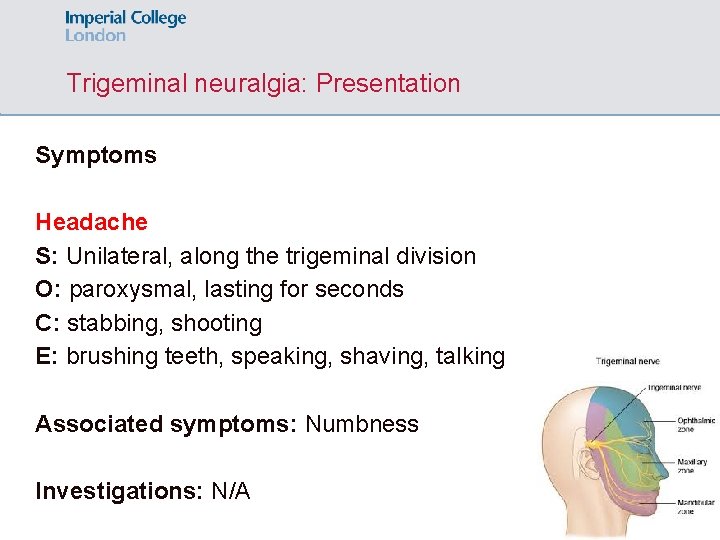
Trigeminal neuralgia: Presentation Symptoms Headache S: Unilateral, along the trigeminal division O: paroxysmal, lasting for seconds C: stabbing, shooting E: brushing teeth, speaking, shaving, talking Associated symptoms: Numbness Investigations: N/A
Primary & Secondary headaches Primary headaches • Tension* • Migraine* • Cluster Secondary headaches • • • Trigeminal neuralgia Meningitis* Encephalitis Raised ICP Bleeds CNS tumours
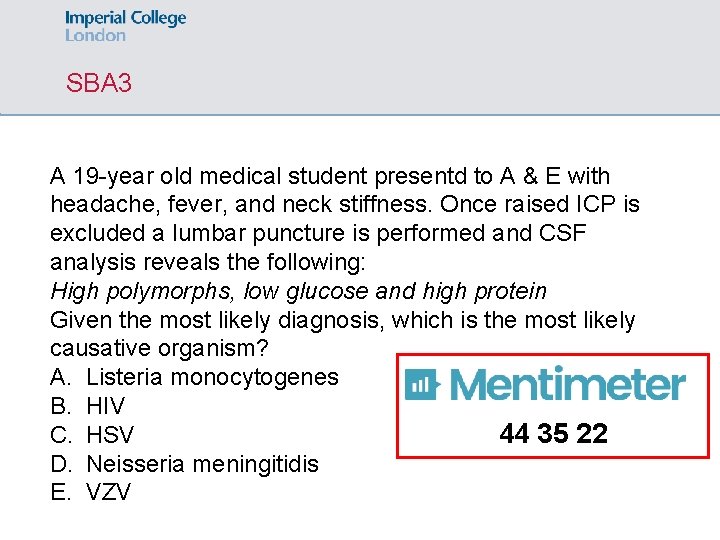
SBA 3 A 19 -year old medical student presentd to A & E with headache, fever, and neck stiffness. Once raised ICP is excluded a lumbar puncture is performed and CSF analysis reveals the following: High polymorphs, low glucose and high protein Given the most likely diagnosis, which is the most likely causative organism? A. Listeria monocytogenes B. HIV C. HSV 44 35 22 D. Neisseria meningitidis E. VZV
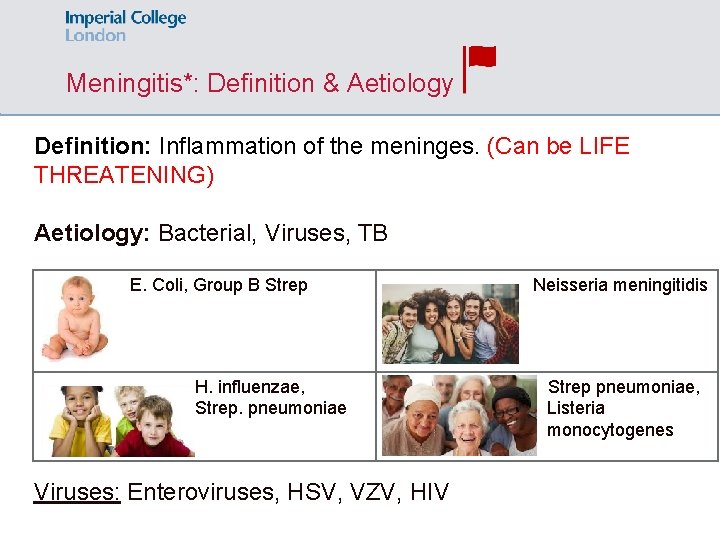
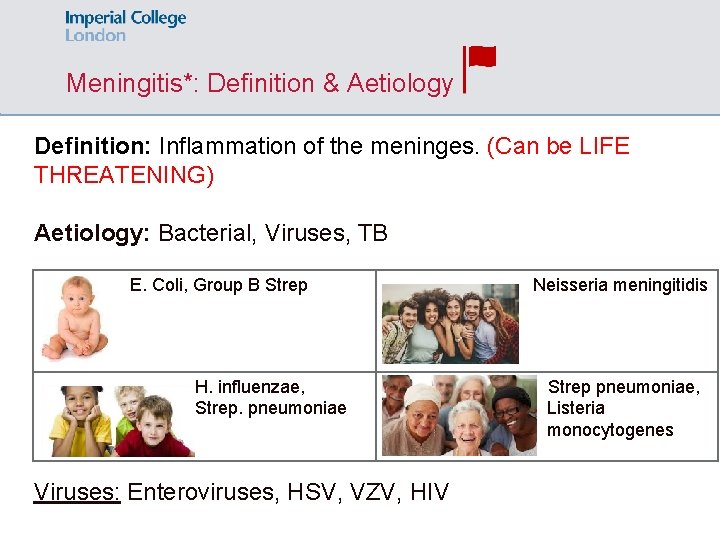
Meningitis*: Definition & Aetiology Definition: Inflammation of the meninges. (Can be LIFE THREATENING) Aetiology: Bacterial, Viruses, TB E. Coli, Group B Strep H. influenzae, Strep. pneumoniae Viruses: Enteroviruses, HSV, VZV, HIV Neisseria meningitidis Strep pneumoniae, Listeria monocytogenes
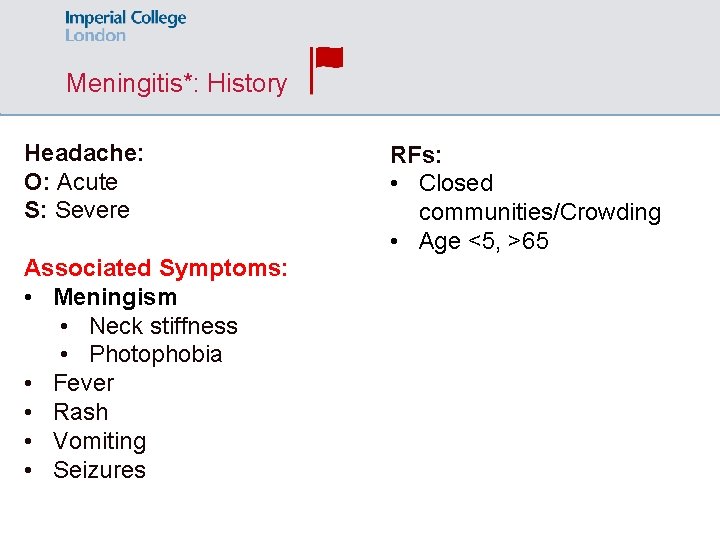
Meningitis*: History Headache: O: Acute S: Severe Associated Symptoms: • Meningism • Neck stiffness • Photophobia • Fever • Rash • Vomiting • Seizures RFs: • Closed communities/Crowding • Age <5, >65
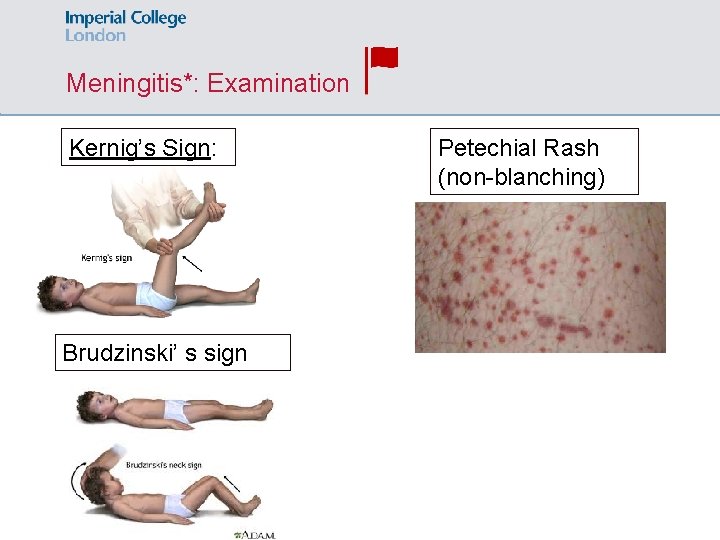
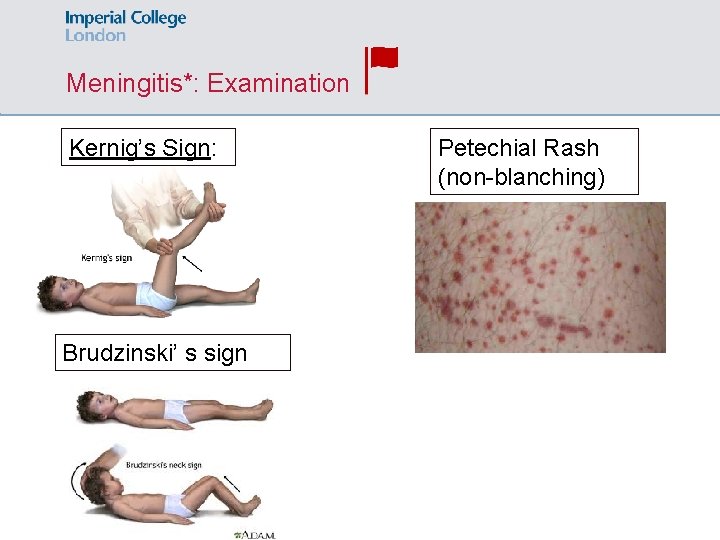
Meningitis*: Examination Kernig’s Sign: Brudzinski’ s sign Petechial Rash (non-blanching)
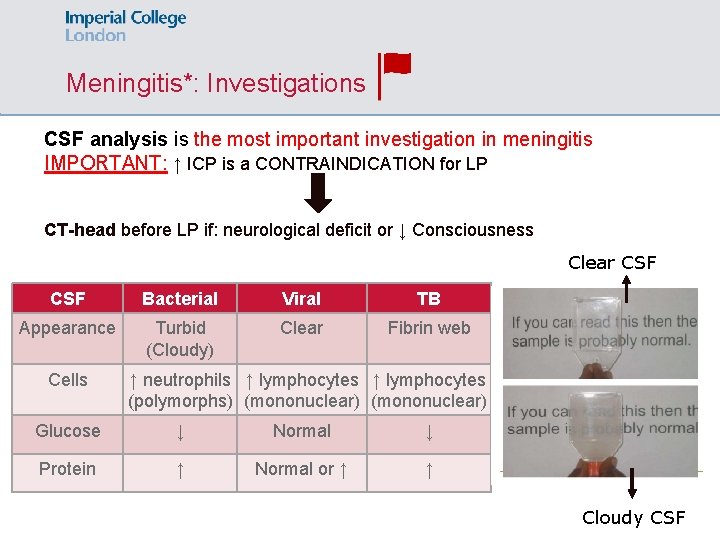
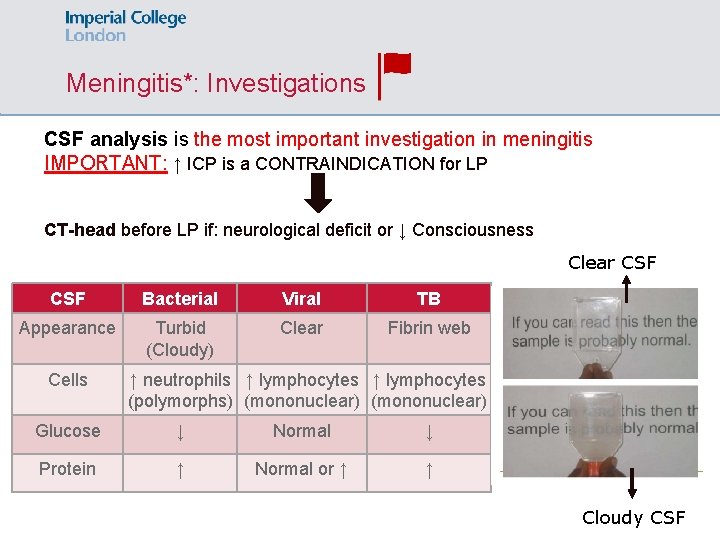
Meningitis*: Investigations CSF analysis is the most important investigation in meningitis IMPORTANT: ↑ ICP is a CONTRAINDICATION for LP CT-head before LP if: neurological deficit or ↓ Consciousness Clear CSF Bacterial Viral TB Appearance Turbid (Cloudy) Clear Fibrin web Cells ↑ neutrophils ↑ lymphocytes (polymorphs) (mononuclear) Glucose ↓ Normal ↓ Protein ↑ Normal or ↑ ↑ Cloudy CSF
Meningitis*: Management & Complications Management at GP: benzylpenicillin IM & URGENT REFERAL TO THE HOSPITAL at A & E: Broad spectrum antibiotics (ceftriaxone IV, benzylpenicillin IM, acyclovir if viral) • Targeted antibiotic Tx depending on sensitivities. • Consider IV dexamethasone Complications: • Hearing loss (most common) • Sepsis • Impaired mental status
Primary & Secondary headaches Primary headaches • Tension* • Migraine* • Cluster Secondary headaches • • • Trigeminal neuralgia Meningitis* Encephalitis Raised ICP Bleeds CNS tumours
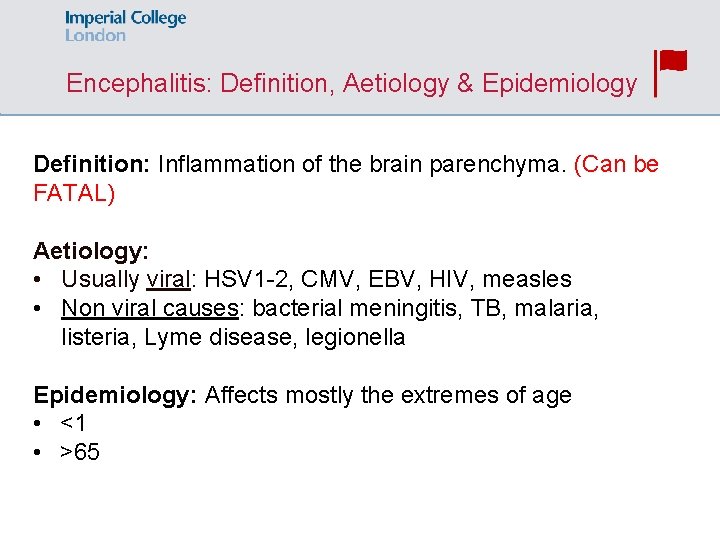
Encephalitis: Definition, Aetiology & Epidemiology Definition: Inflammation of the brain parenchyma. (Can be FATAL) Aetiology: • Usually viral: HSV 1 -2, CMV, EBV, HIV, measles • Non viral causes: bacterial meningitis, TB, malaria, listeria, Lyme disease, legionella Epidemiology: Affects mostly the extremes of age • <1 • >65
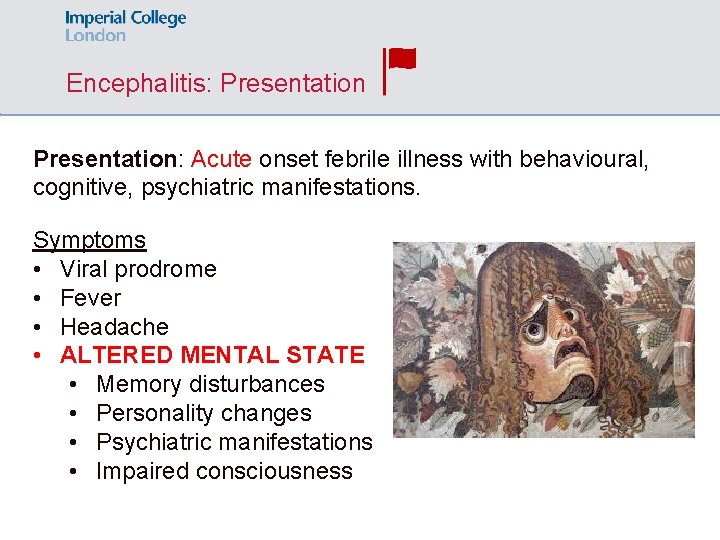
Encephalitis: Presentation: Acute onset febrile illness with behavioural, cognitive, psychiatric manifestations. Symptoms • Viral prodrome • Fever • Headache • ALTERED MENTAL STATE • Memory disturbances • Personality changes • Psychiatric manifestations • Impaired consciousness
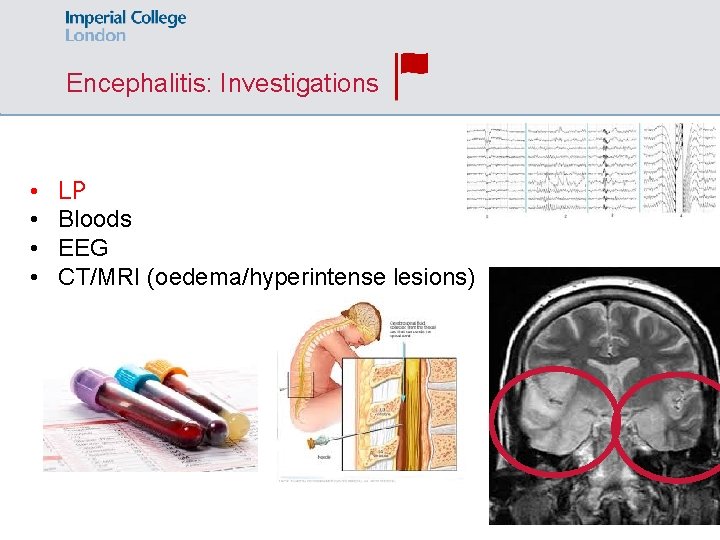
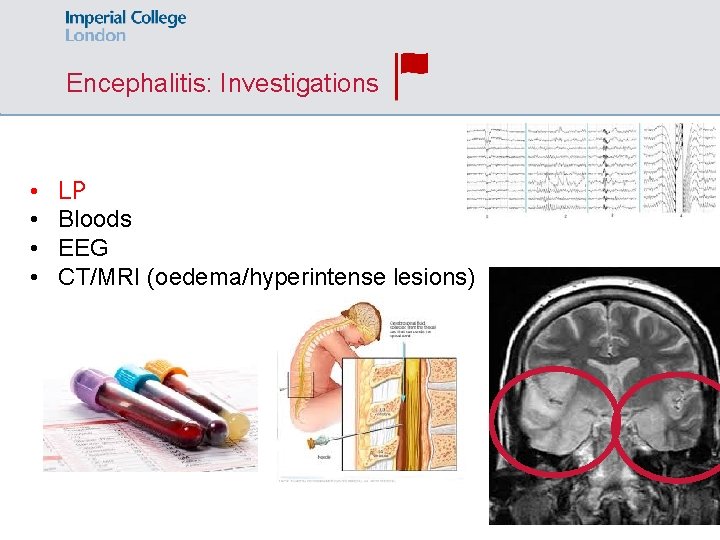
Encephalitis: Investigations • • LP Bloods EEG CT/MRI (oedema/hyperintense lesions)
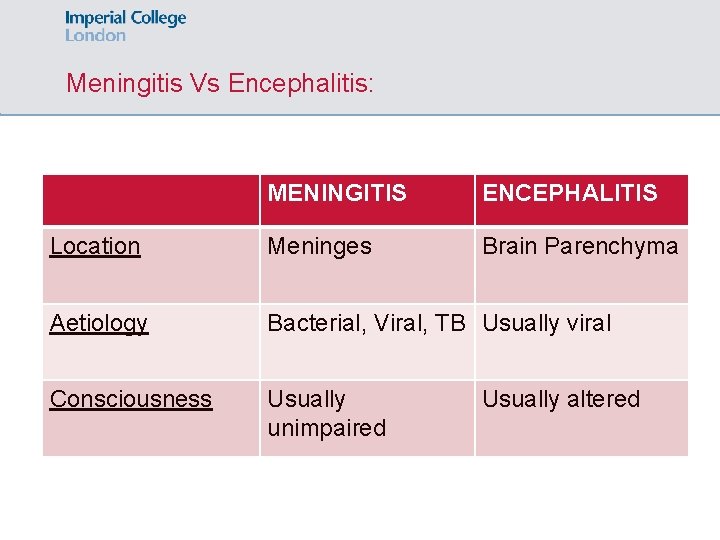
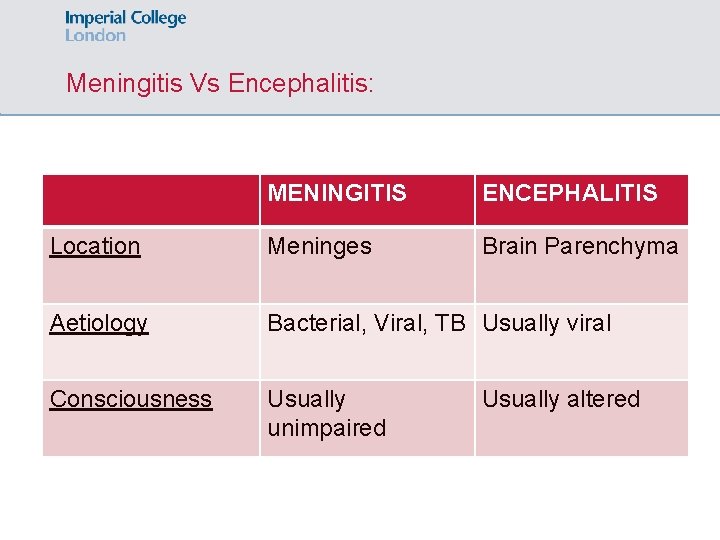
Meningitis Vs Encephalitis: MENINGITIS ENCEPHALITIS Location Meninges Brain Parenchyma Aetiology Bacterial, Viral, TB Usually viral Consciousness Usually unimpaired Usually altered
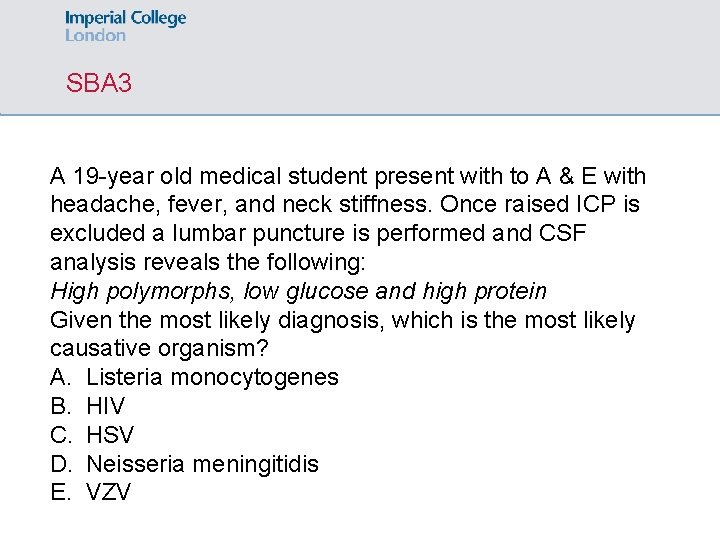
SBA 3 A 19 -year old medical student present with to A & E with headache, fever, and neck stiffness. Once raised ICP is excluded a lumbar puncture is performed and CSF analysis reveals the following: High polymorphs, low glucose and high protein Given the most likely diagnosis, which is the most likely causative organism? A. Listeria monocytogenes B. HIV C. HSV D. Neisseria meningitidis E. VZV
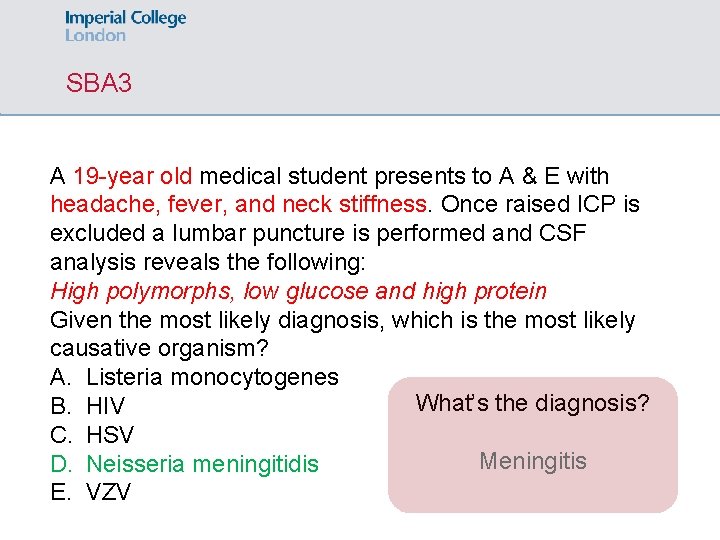
SBA 3 A 19 -year old medical student presents to A & E with headache, fever, and neck stiffness. Once raised ICP is excluded a lumbar puncture is performed and CSF analysis reveals the following: High polymorphs, low glucose and high protein Given the most likely diagnosis, which is the most likely causative organism? A. Listeria monocytogenes What’s the diagnosis? B. HIV C. HSV Meningitis D. Neisseria meningitidis E. VZV
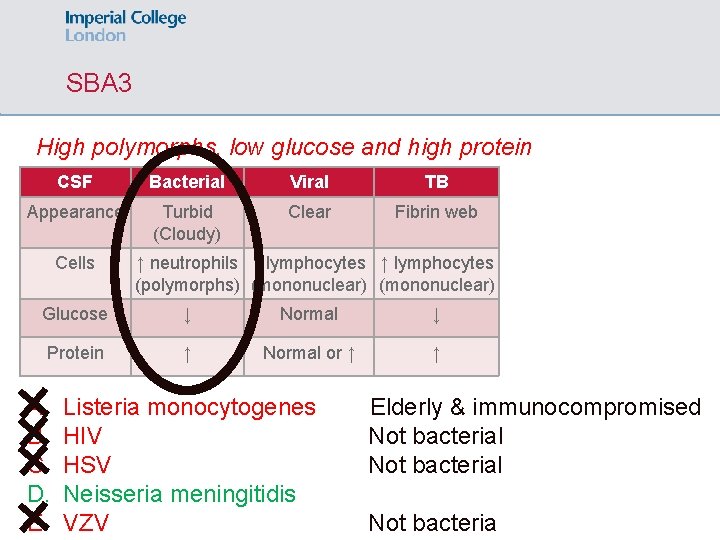
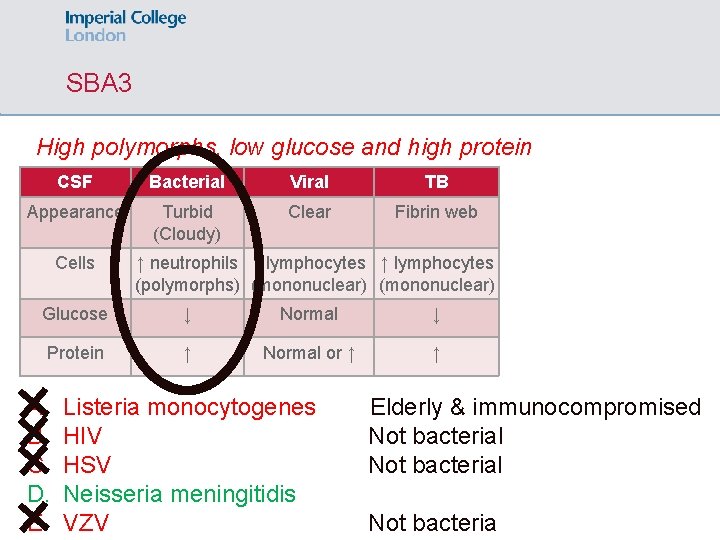
SBA 3 High polymorphs, low glucose and high protein CSF Bacterial Viral TB Appearance Turbid (Cloudy) Clear Fibrin web Cells ↑ neutrophils ↑ lymphocytes (polymorphs) (mononuclear) Glucose ↓ Normal ↓ Protein ↑ Normal or ↑ ↑ A. B. C. D. E. Listeria monocytogenes HIV HSV Neisseria meningitidis VZV Elderly & immunocompromised Not bacterial Not bacteria
SBA 4 An older man with a longstanding history of AF on anticoagulation with warfarin is brought into A & E by his carer, who is concerned about the patient's confusion at home. The carer describes frequent falls over the last several months. On examination, he has a right-sided pronator drift and is weaker on his right side. His mental status testing reveals poor concentration. What is the most likely cause of his symptoms? A. Stroke B. Subdural haemorrhage 44 35 22 C. Alzheimer’s disease D. Encephalitis E. Parkinson’s disease
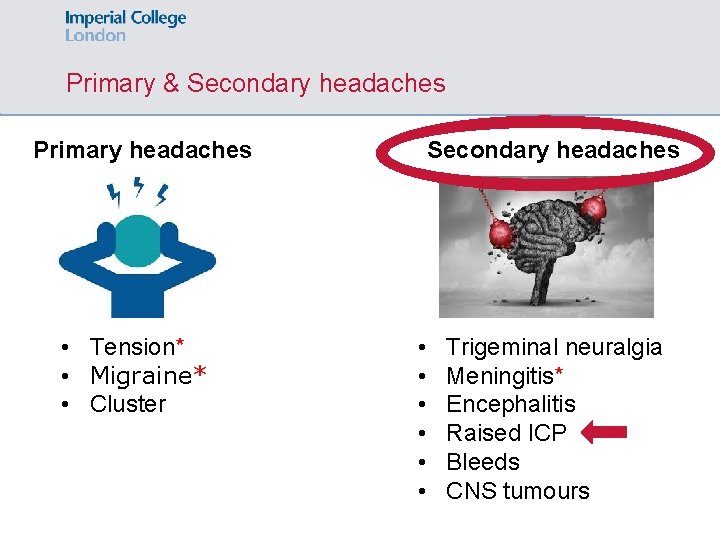
Primary & Secondary headaches Primary headaches • Tension* • Migraine* • Cluster Secondary headaches • • • Trigeminal neuralgia Meningitis* Encephalitis Raised ICP Bleeds CNS tumours
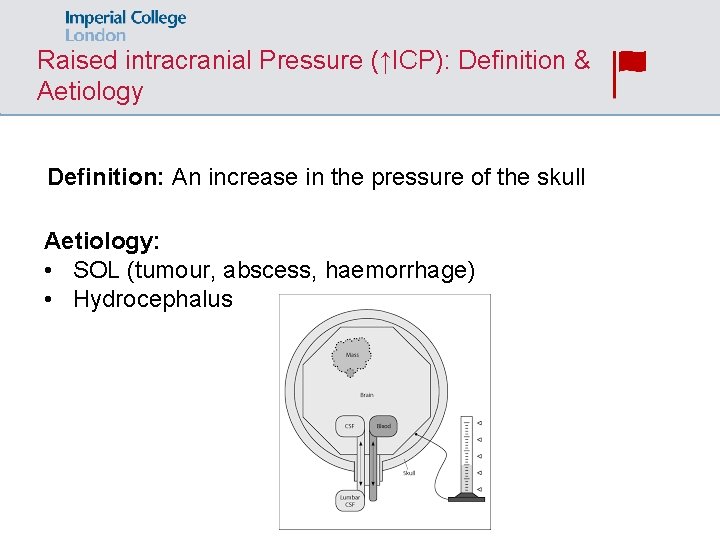
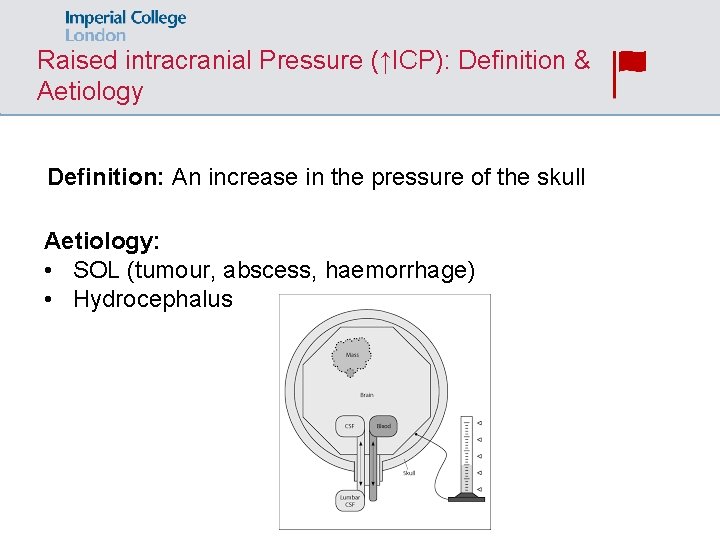
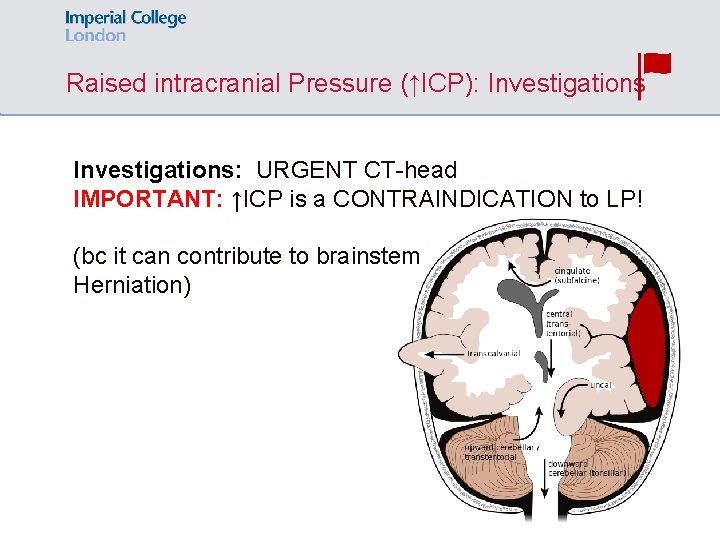
Raised intracranial Pressure (↑ICP): Definition & Aetiology Definition: An increase in the pressure of the skull Aetiology: • SOL (tumour, abscess, haemorrhage) • Hydrocephalus
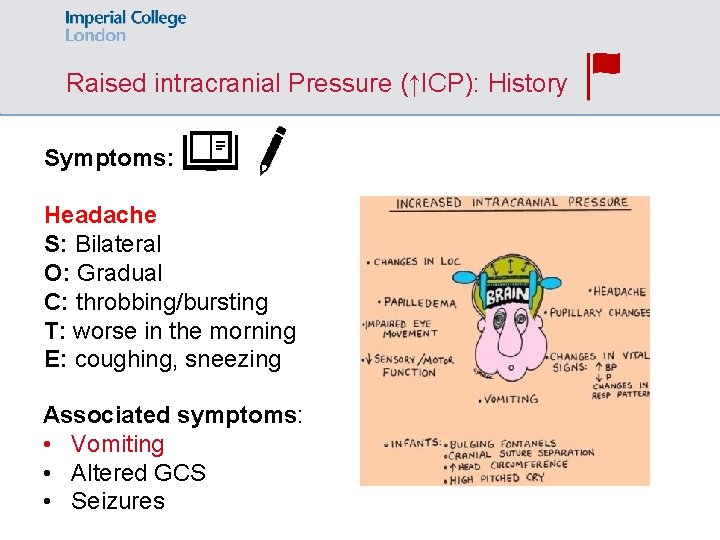
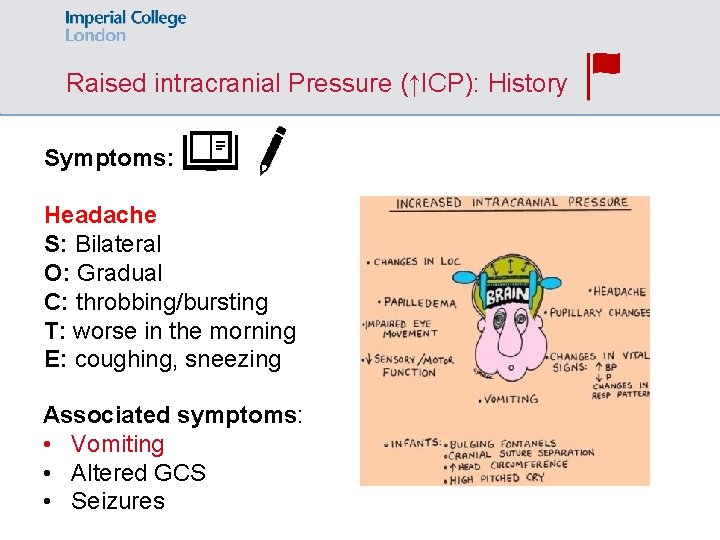
Raised intracranial Pressure (↑ICP): History Symptoms: Headache S: Bilateral O: Gradual C: throbbing/bursting T: worse in the morning E: coughing, sneezing Associated symptoms: • Vomiting • Altered GCS • Seizures
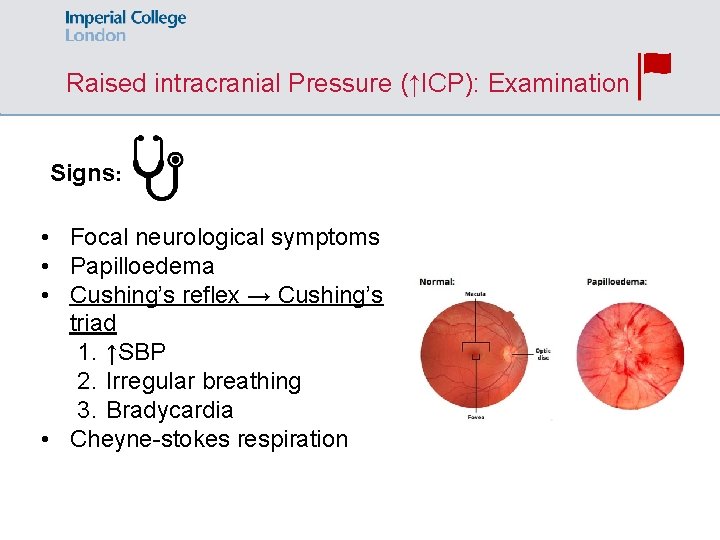
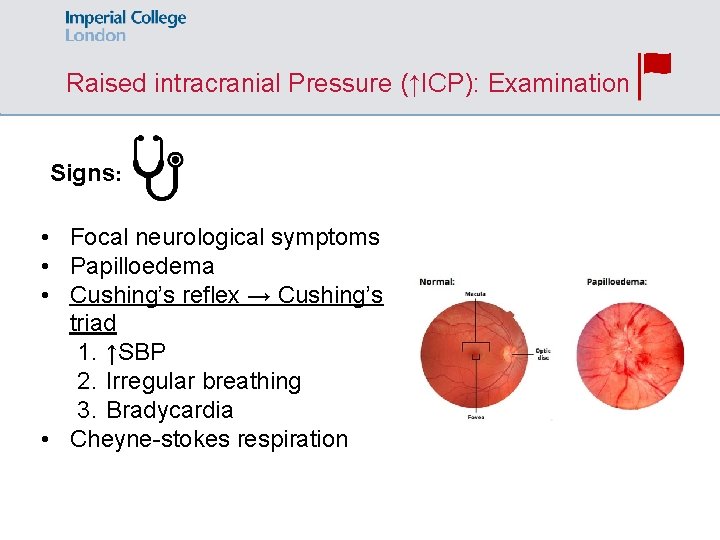
Raised intracranial Pressure (↑ICP): Examination Signs: • Focal neurological symptoms • Papilloedema • Cushing’s reflex → Cushing’s triad 1. ↑SBP 2. Irregular breathing 3. Bradycardia • Cheyne-stokes respiration
Raised intracranial Pressure (↑ICP): Investigations: URGENT CT-head IMPORTANT: ↑ICP is a CONTRAINDICATION to LP! (bc it can contribute to brainstem Herniation)
Primary & Secondary headaches Primary headaches • Tension* • Migraine* • Cluster Secondary headaches • • • Trigeminal neuralgia Meningitis* Encephalitis Raised ICP Bleeds CNS tumours
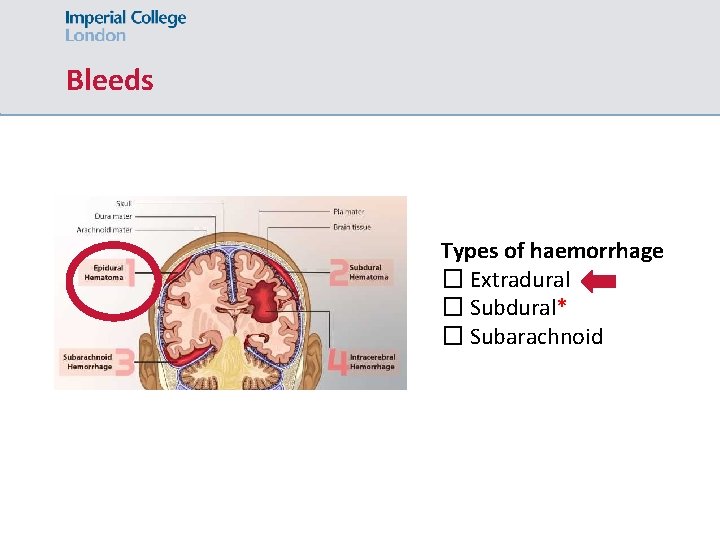
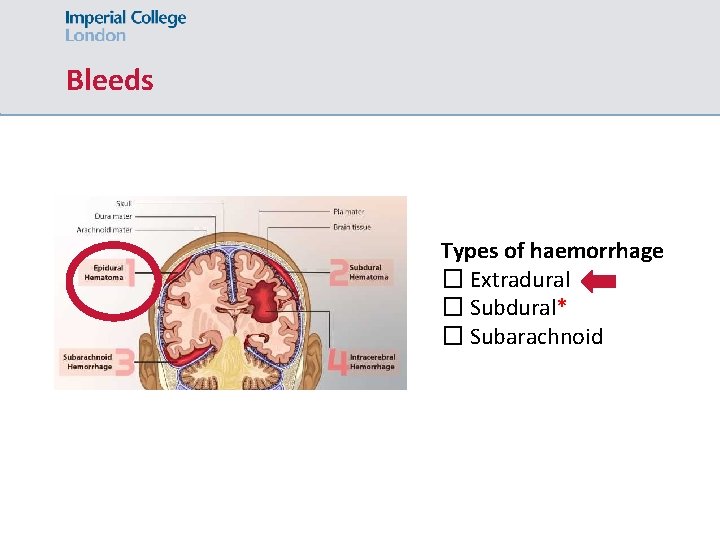
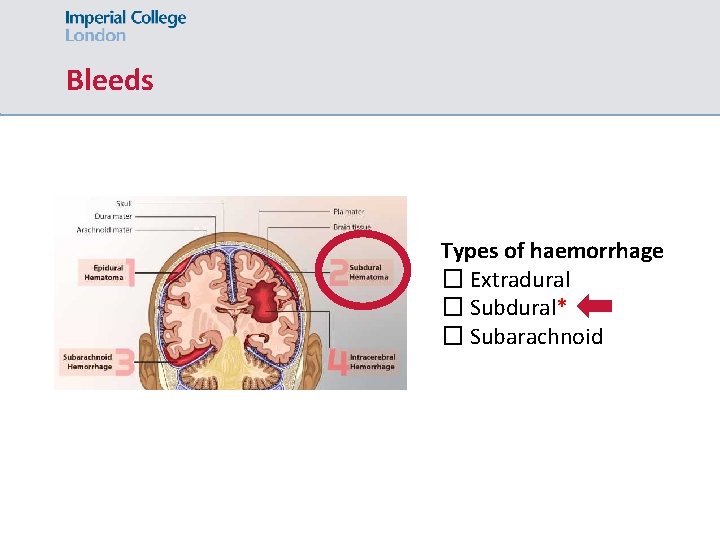
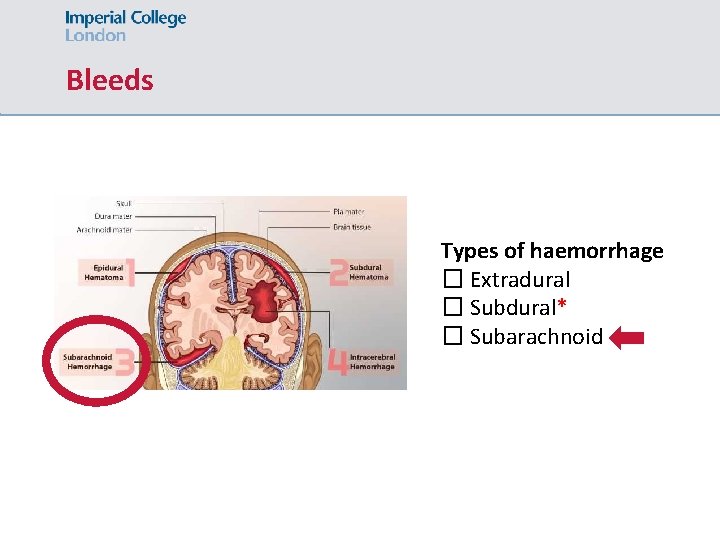
Bleeds Types of haemorrhage � Extradural � Subdural* � Subarachnoid
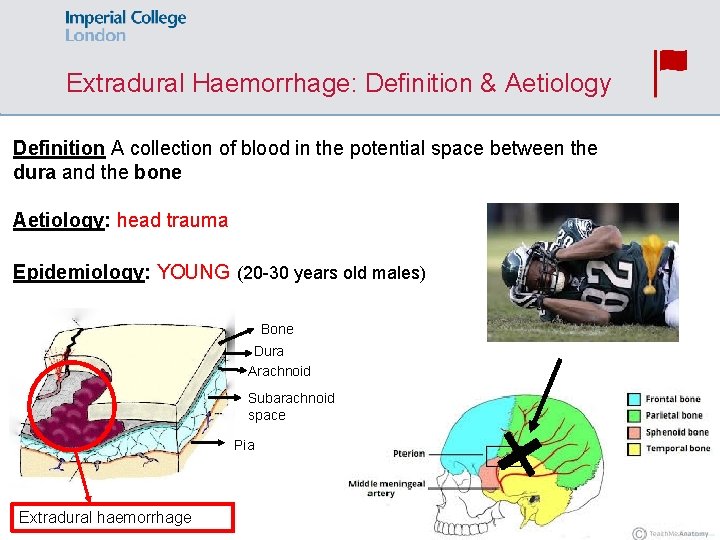
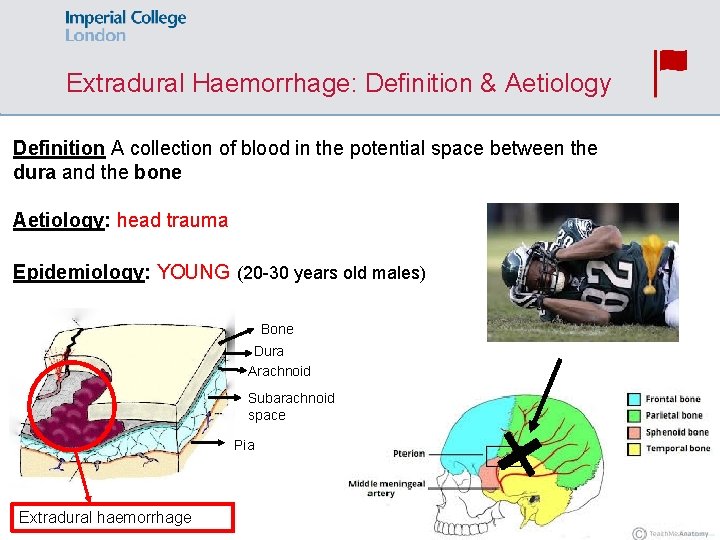
Extradural Haemorrhage: Definition & Aetiology Definition A collection of blood in the potential space between the dura and the bone Aetiology: head trauma Epidemiology: YOUNG (20 -30 years old males) Bone Dura Arachnoid Subarachnoid space Pia Extradural haemorrhage
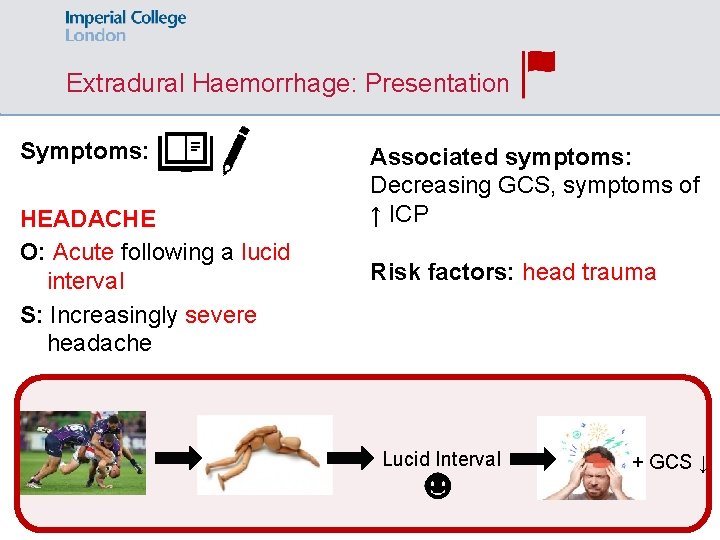
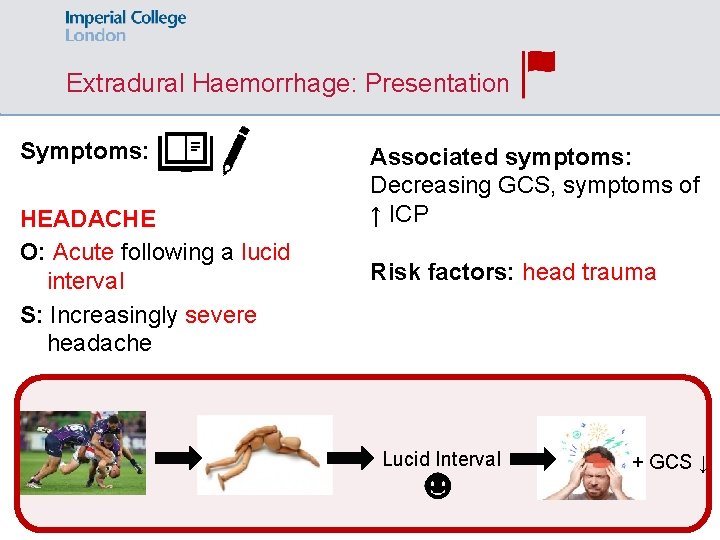
Extradural Haemorrhage: Presentation Symptoms: HEADACHE O: Acute following a lucid interval S: Increasingly severe headache Associated symptoms: Decreasing GCS, symptoms of ↑ ICP Risk factors: head trauma Lucid Interval + GCS ↓
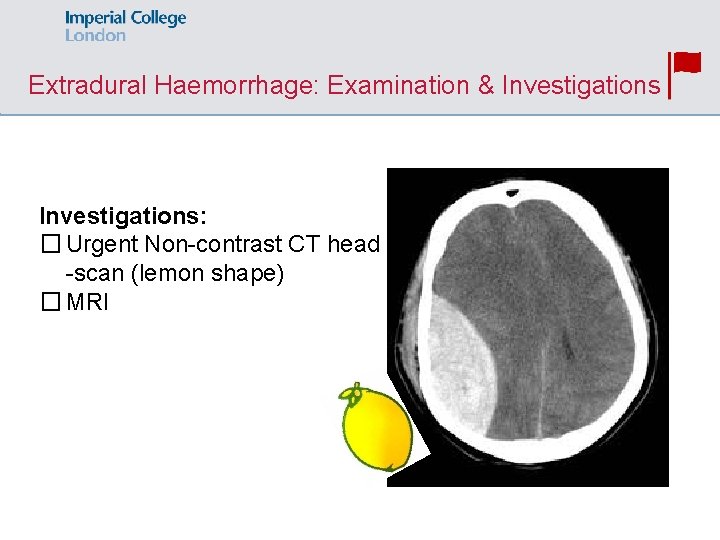
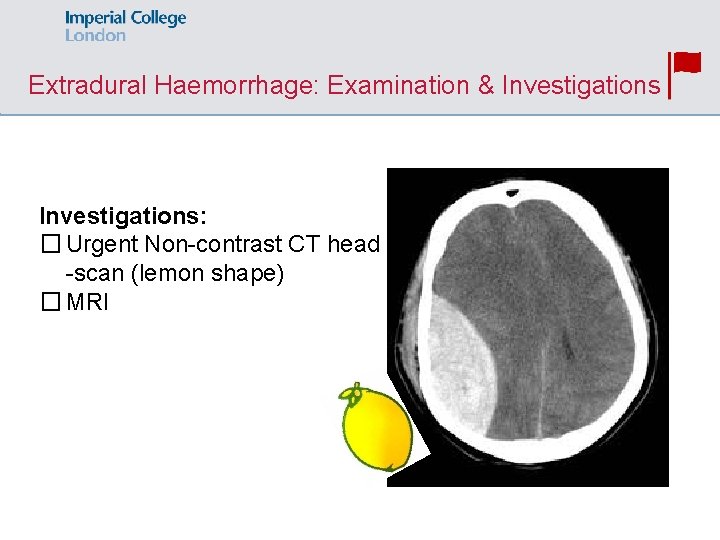
Extradural Haemorrhage: Examination & Investigations: � Urgent Non-contrast CT head -scan (lemon shape) � MRI
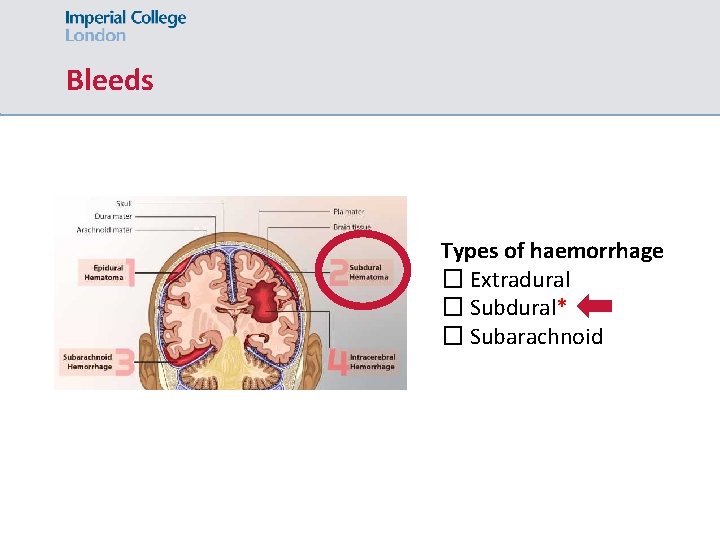
Bleeds Types of haemorrhage � Extradural � Subdural* � Subarachnoid
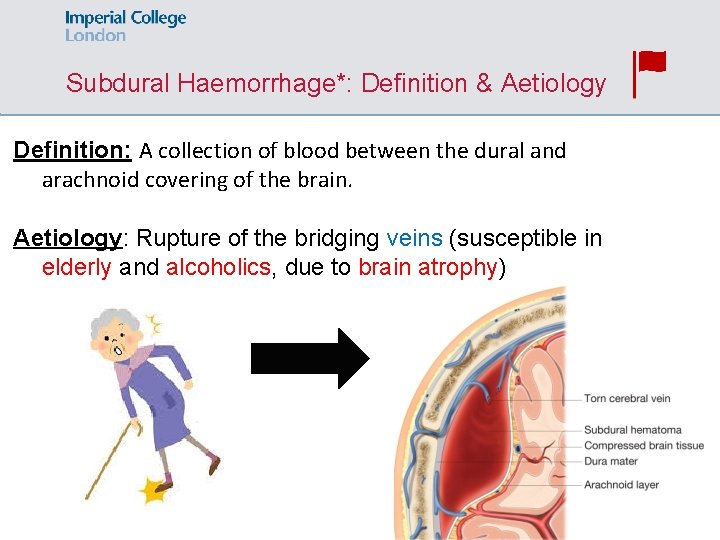
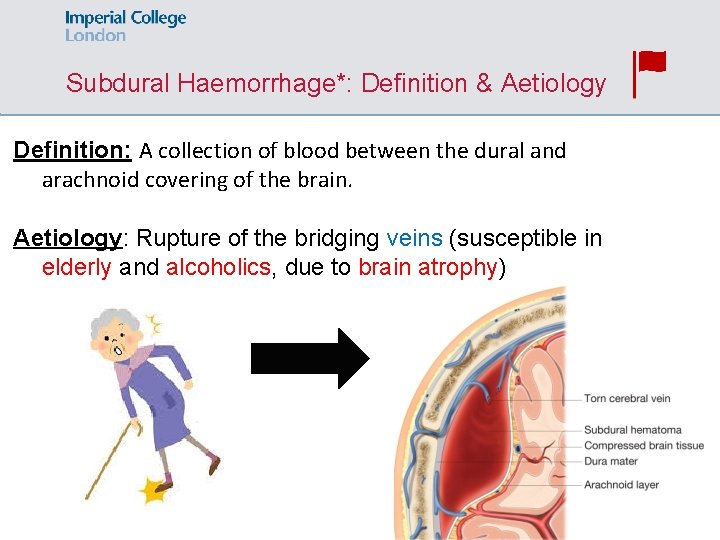
Subdural Haemorrhage*: Definition & Aetiology Definition: A collection of blood between the dural and arachnoid covering of the brain. Aetiology: Rupture of the bridging veins (susceptible in elderly and alcoholics, due to brain atrophy)
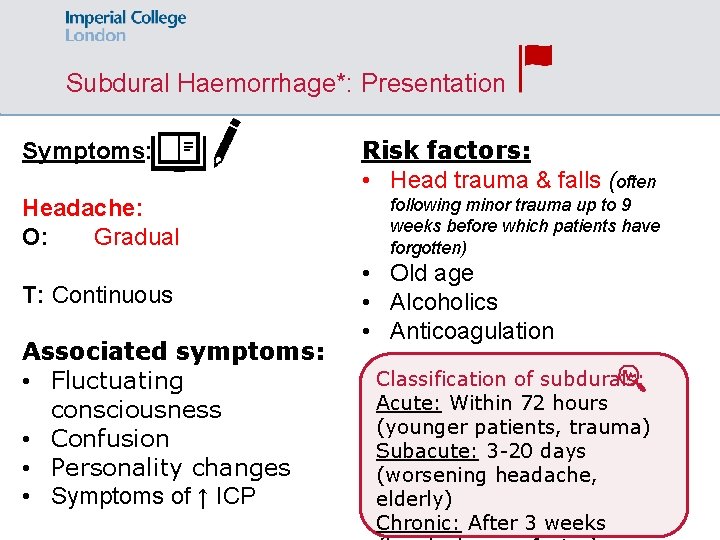
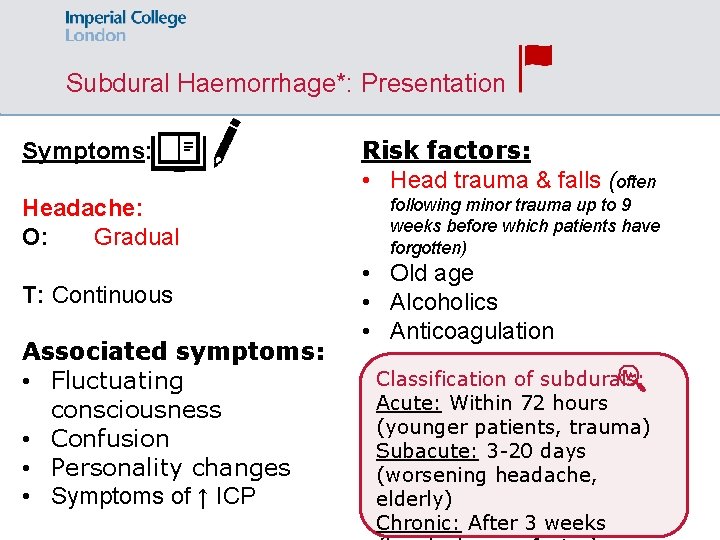
Subdural Haemorrhage*: Presentation Symptoms: Headache: O: Gradual T: Continuous Associated symptoms: • Fluctuating consciousness • Confusion • Personality changes • Symptoms of ↑ ICP Risk factors: • Head trauma & falls (often following minor trauma up to 9 weeks before which patients have forgotten) • Old age • Alcoholics • Anticoagulation Classification of subdurals: Acute: Within 72 hours (younger patients, trauma) Subacute: 3 -20 days (worsening headache, elderly) Chronic: After 3 weeks
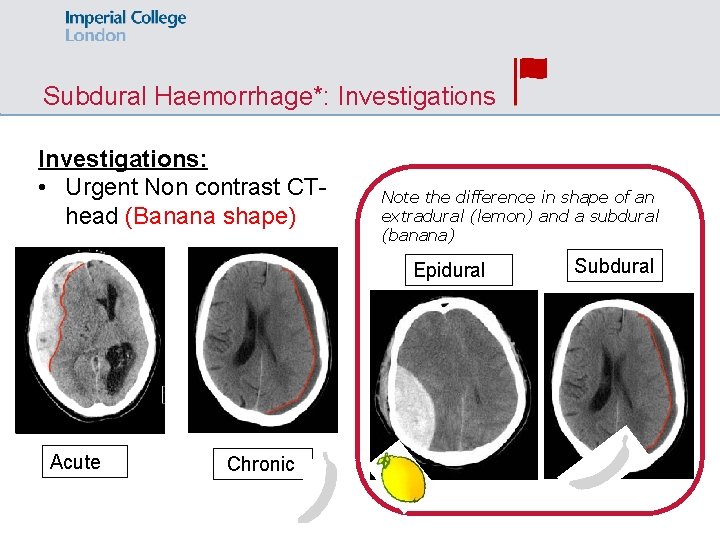
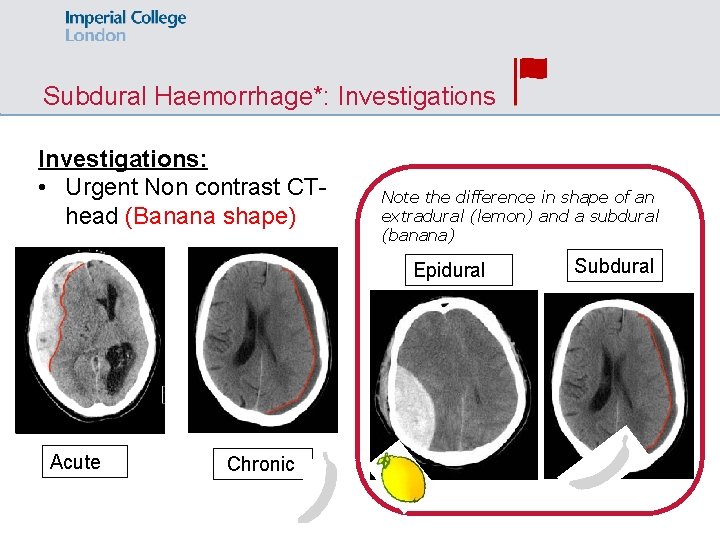
Subdural Haemorrhage*: Investigations: • Urgent Non contrast CThead (Banana shape) Note the difference in shape of an extradural (lemon) and a subdural (banana) Epidural Acute Chronic Subdural
Subdural Haemorrhage*: Management ABCDE & NEUROSURGERY REFERAL Depends on size & presentation • If small (<10 mm) and no significant neurological dysfunction: observe • If large or significant neurological dysfunction: Burr hole or craniotomy
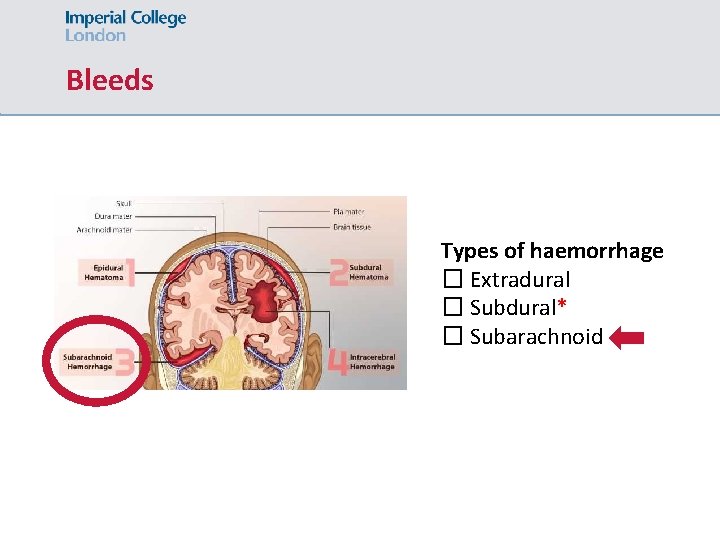
Bleeds Types of haemorrhage � Extradural � Subdural* � Subarachnoid
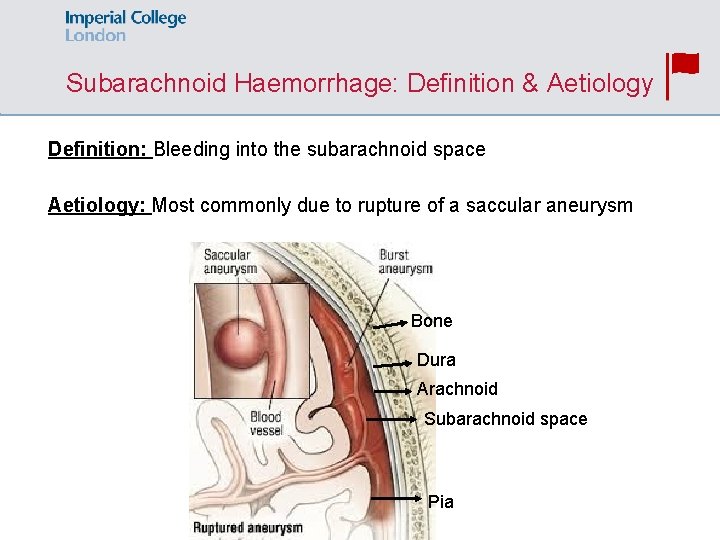
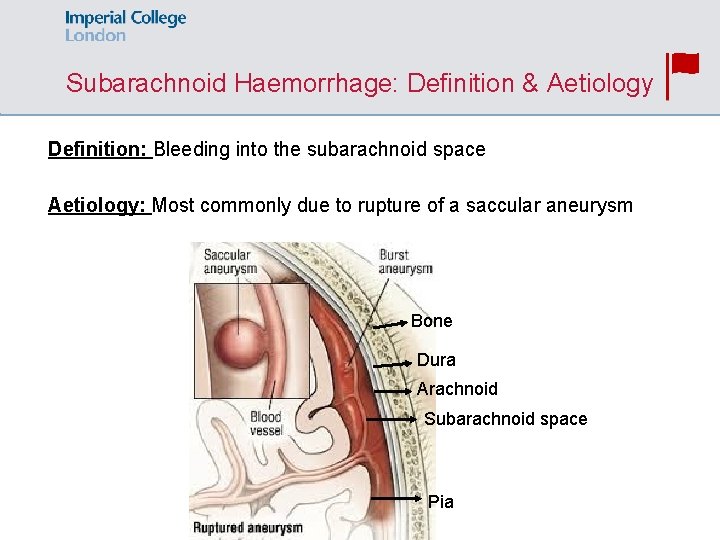
Subarachnoid Haemorrhage: Definition & Aetiology Definition: Bleeding into the subarachnoid space Aetiology: Most commonly due to rupture of a saccular aneurysm Bone Dura Arachnoid Subarachnoid space Pia
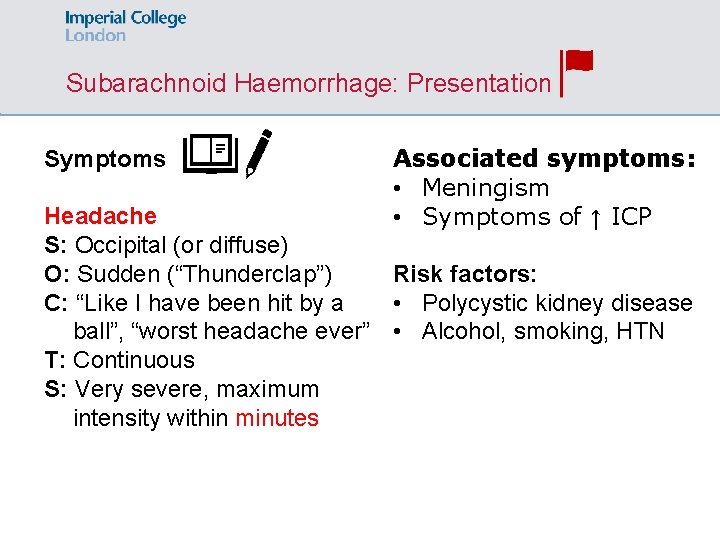
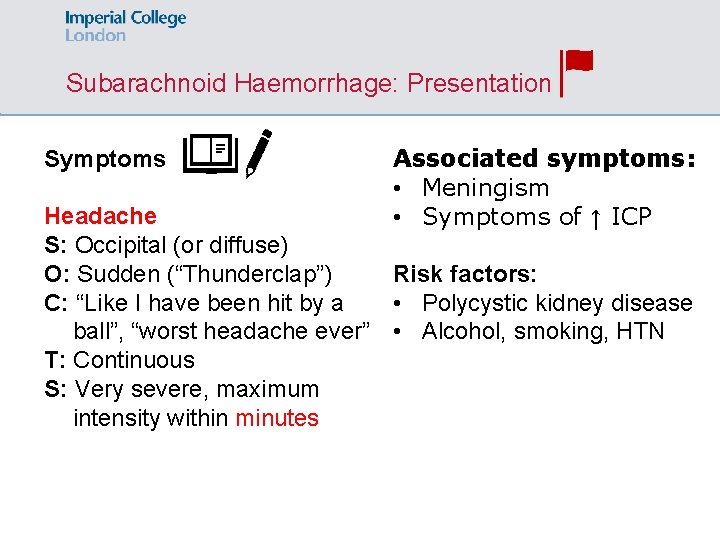
Subarachnoid Haemorrhage: Presentation Symptoms Associated symptoms: • Meningism • Symptoms of ↑ ICP Headache S: Occipital (or diffuse) Risk factors: O: Sudden (“Thunderclap”) • Polycystic kidney disease C: “Like I have been hit by a ball”, “worst headache ever” • Alcohol, smoking, HTN T: Continuous S: Very severe, maximum intensity within minutes
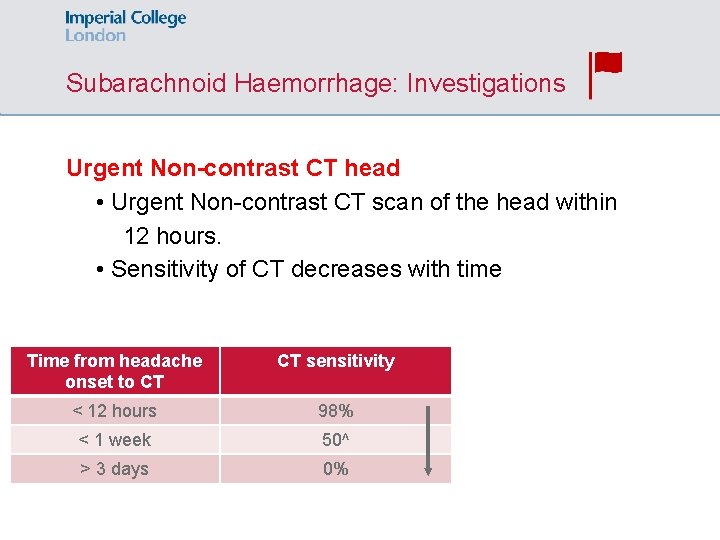
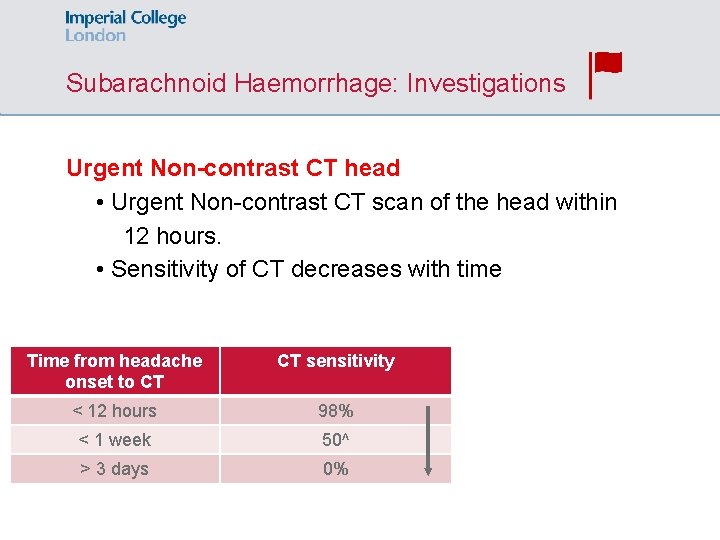
Subarachnoid Haemorrhage: Investigations Urgent Non-contrast CT head • Urgent Non-contrast CT scan of the head within 12 hours. • Sensitivity of CT decreases with time Time from headache onset to CT CT sensitivity < 12 hours 98% < 1 week 50^ > 3 days 0%
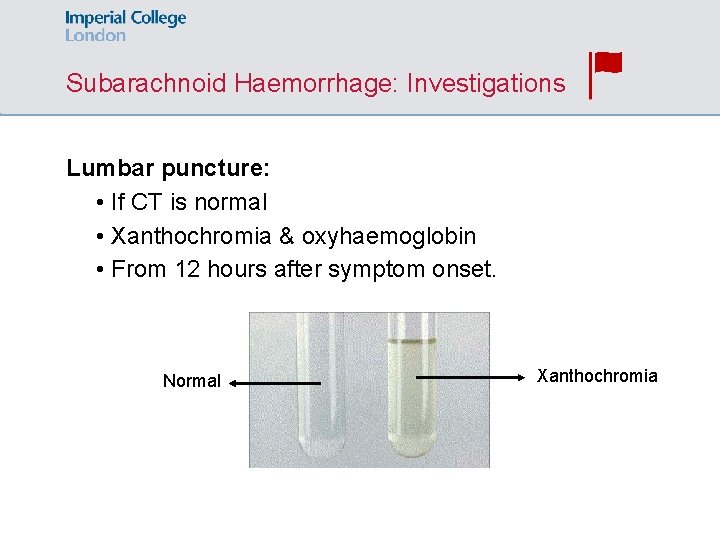
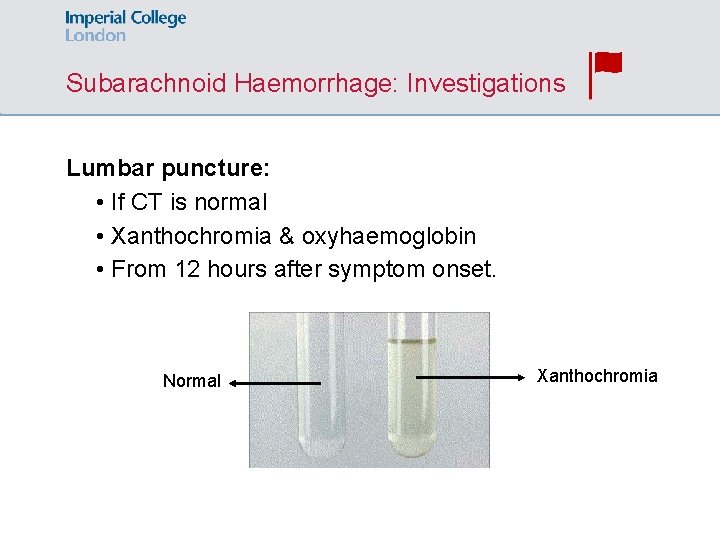
Subarachnoid Haemorrhage: Investigations Lumbar puncture: • If CT is normal • Xanthochromia & oxyhaemoglobin • From 12 hours after symptom onset. Normal Xanthochromia
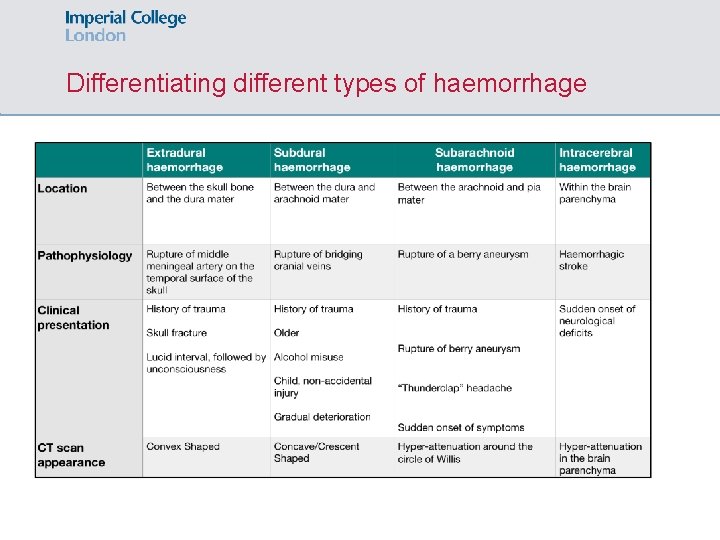
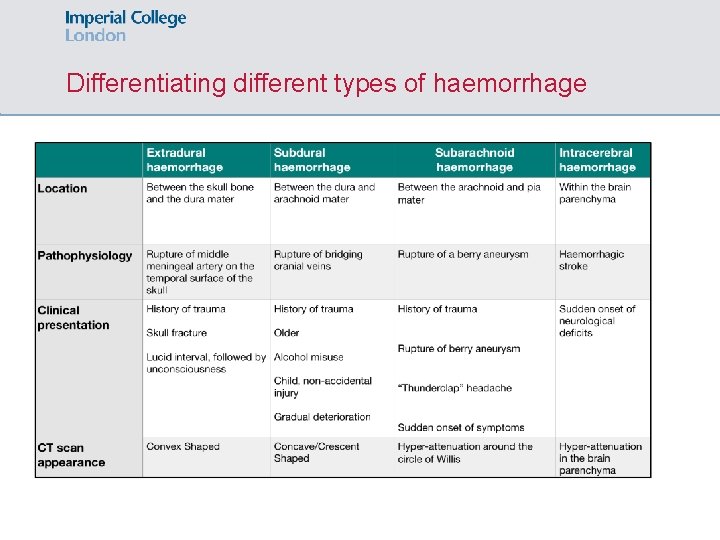
Differentiating different types of haemorrhage
SBA 4 An older man with a longstanding history of AF on anticoagulation with warfarin is brought into A & E by his carer, who is concerned about the patient's confusion at home. The carer describes frequent falls over the last several months. On examination, he has a right-sided pronator drift and is weaker on his right side. His mental status testing reveals poor concentration. What is the most likely cause of his symptoms? A. Stroke B. Subdural haemorrhage C. Alzheimer’s disease D. Encephalitis E. Parkinson’s disease
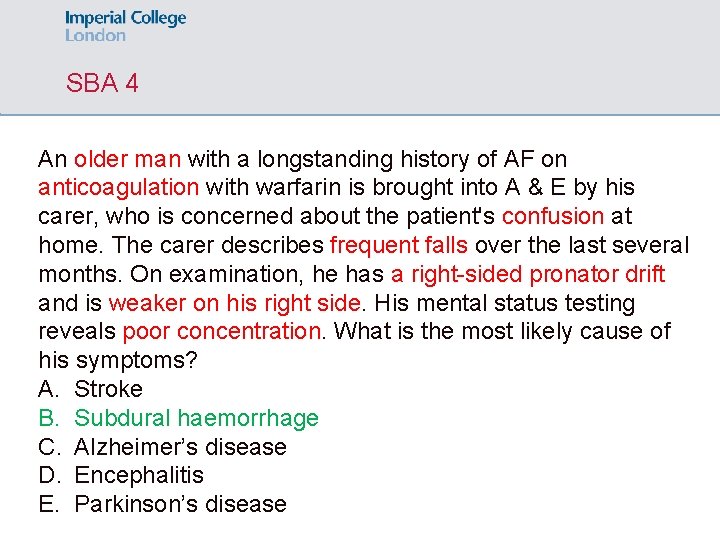
SBA 4 An older man with a longstanding history of AF on anticoagulation with warfarin is brought into A & E by his carer, who is concerned about the patient's confusion at home. The carer describes frequent falls over the last several months. On examination, he has a right-sided pronator drift and is weaker on his right side. His mental status testing reveals poor concentration. What is the most likely cause of his symptoms? A. Stroke B. Subdural haemorrhage C. Alzheimer’s disease D. Encephalitis E. Parkinson’s disease
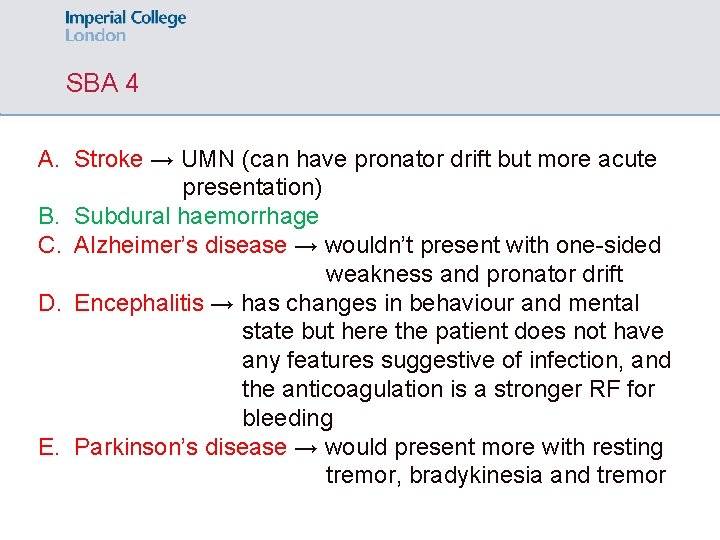
SBA 4 A. Stroke → UMN (can have pronator drift but more acute presentation) B. Subdural haemorrhage C. Alzheimer’s disease → wouldn’t present with one-sided weakness and pronator drift D. Encephalitis → has changes in behaviour and mental state but here the patient does not have any features suggestive of infection, and the anticoagulation is a stronger RF for bleeding E. Parkinson’s disease → would present more with resting tremor, bradykinesia and tremor
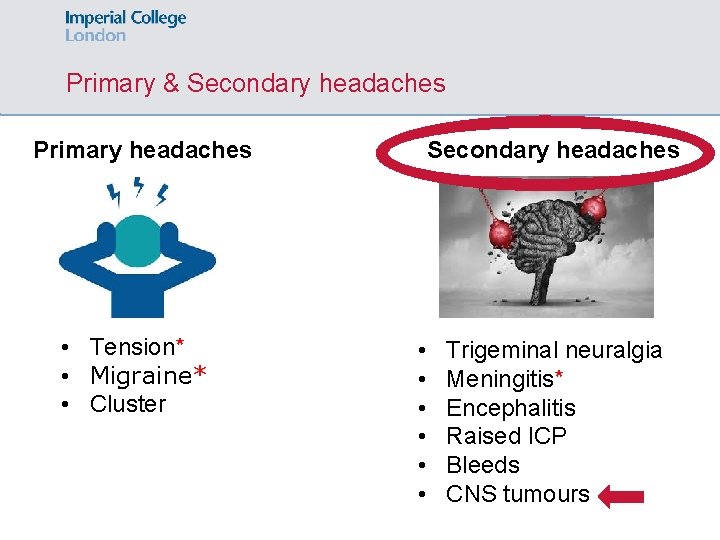
Primary & Secondary headaches Primary headaches • Tension* • Migraine* • Cluster Secondary headaches • • • Trigeminal neuralgia Meningitis* Encephalitis Raised ICP Bleeds CNS tumours
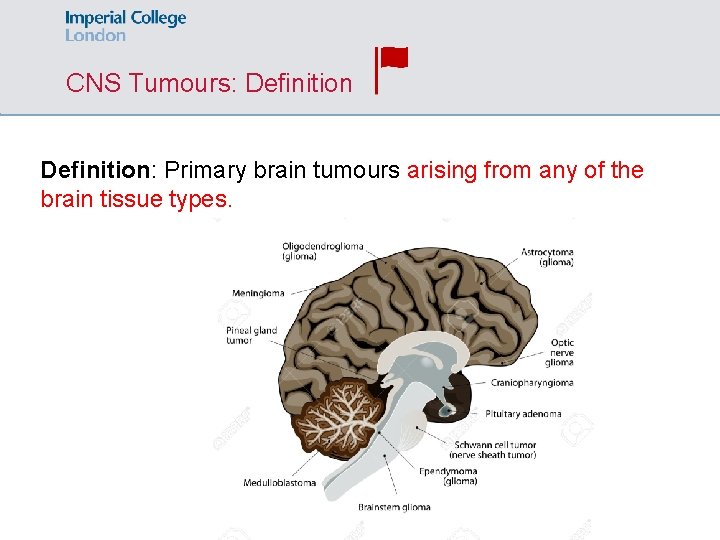
CNS Tumours: Definition: Primary brain tumours arising from any of the brain tissue types.
CNS Tumours: Definition: Primary brain tumours arising from any of the brain tissue types.
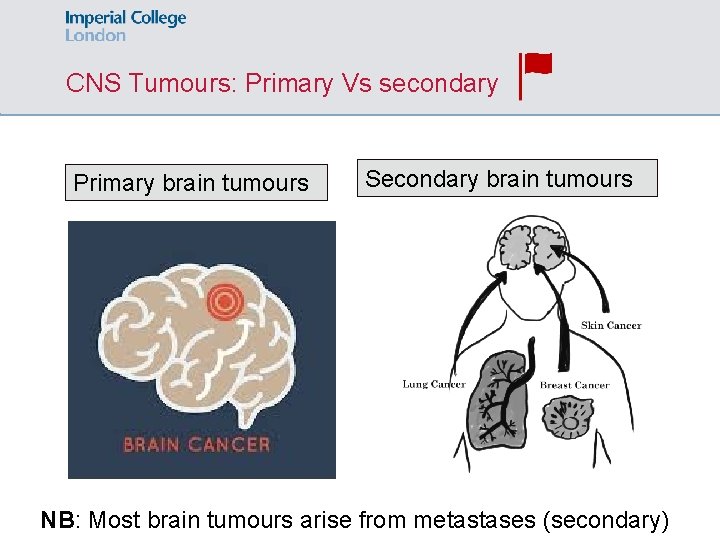
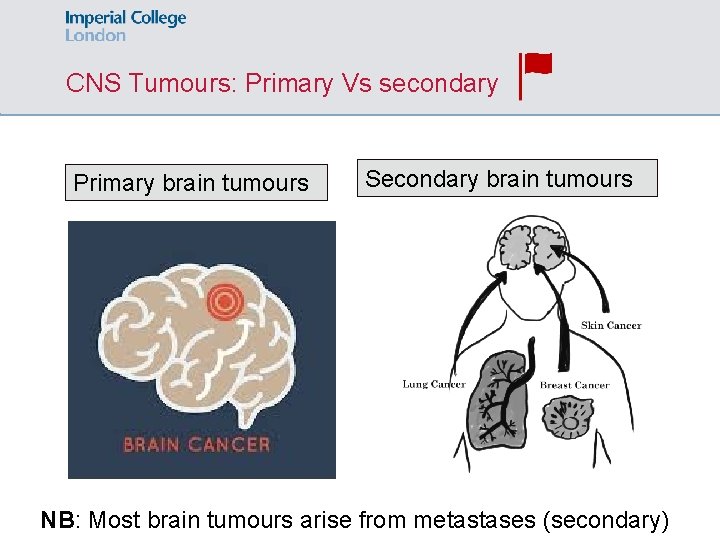
CNS Tumours: Primary Vs secondary Primary brain tumours Secondary brain tumours NB: Most brain tumours arise from metastases (secondary)
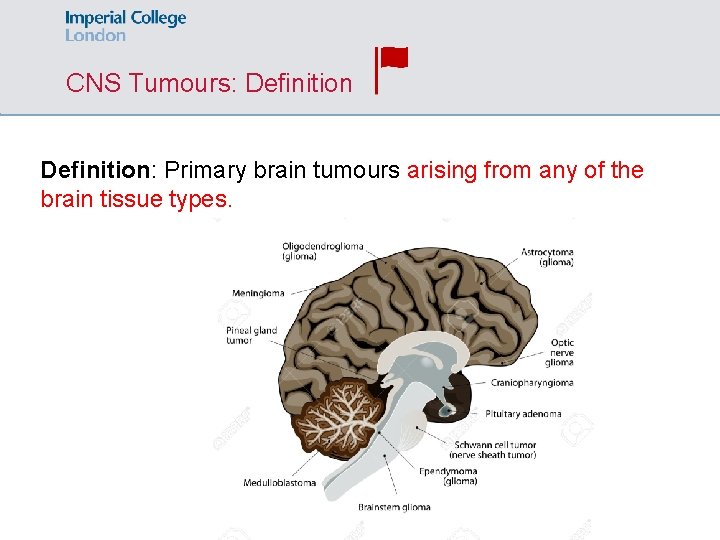
CNS Tumours: Definition: Primary brain tumours arising from any of the brain tissue types.
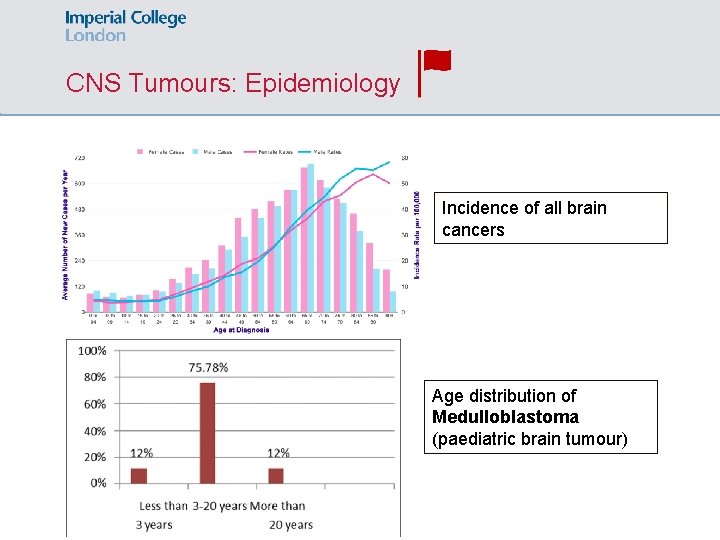
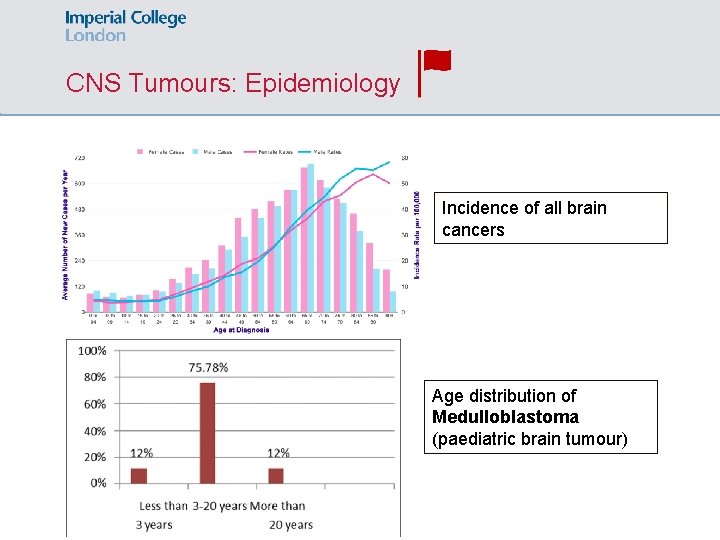
CNS Tumours: Epidemiology Incidence of all brain cancers Age distribution of Medulloblastoma (paediatric brain tumour)
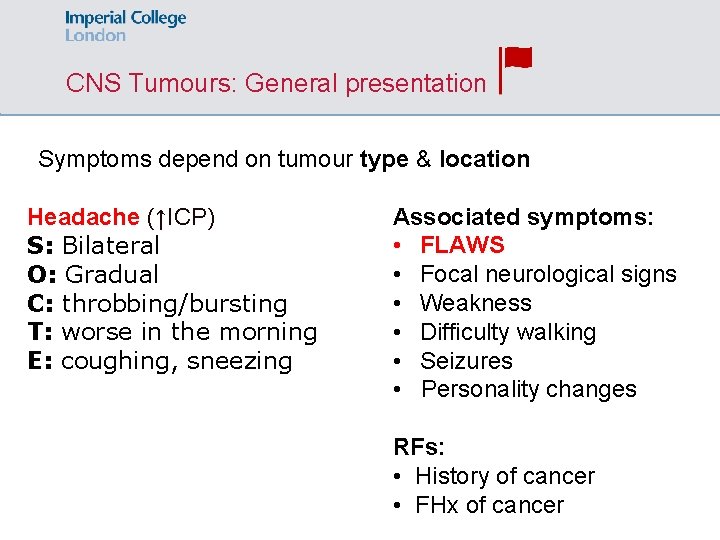
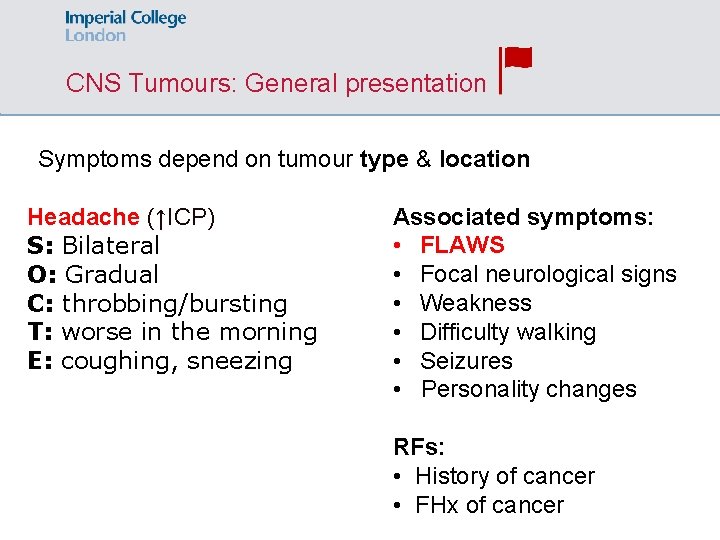
CNS Tumours: General presentation Symptoms depend on tumour type & location Headache (↑ICP) S: Bilateral O: Gradual C: throbbing/bursting T: worse in the morning E: coughing, sneezing Associated symptoms: • FLAWS • Focal neurological signs • Weakness • Difficulty walking • Seizures • Personality changes RFs: • History of cancer • FHx of cancer
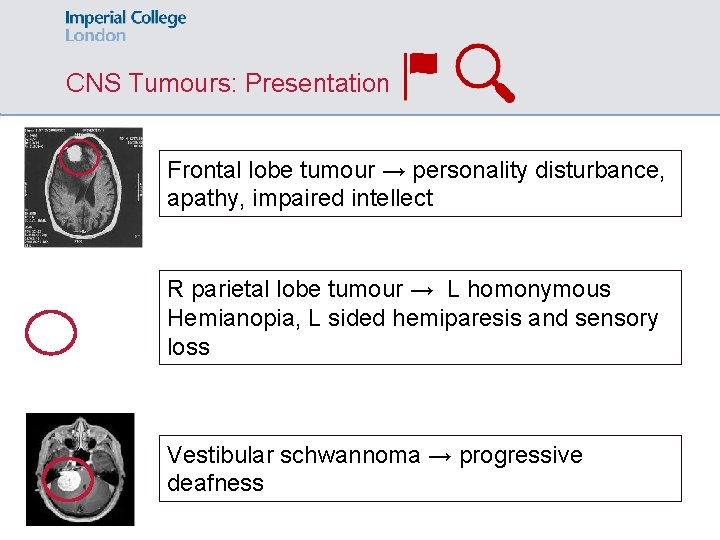
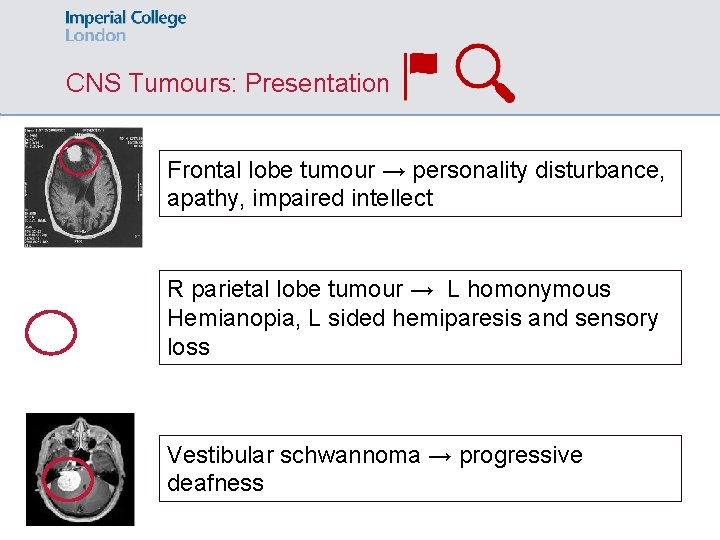
CNS Tumours: Presentation Frontal lobe tumour → personality disturbance, apathy, impaired intellect R parietal lobe tumour → L homonymous Hemianopia, L sided hemiparesis and sensory loss Vestibular schwannoma → progressive deafness
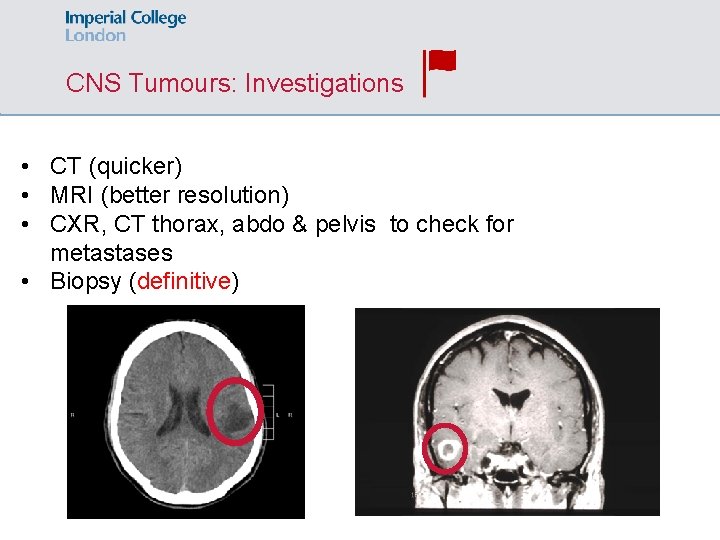
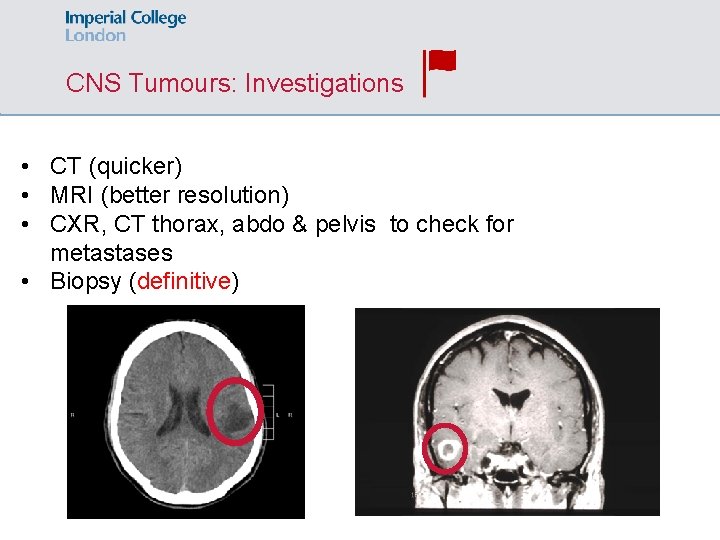
CNS Tumours: Investigations • CT (quicker) • MRI (better resolution) • CXR, CT thorax, abdo & pelvis to check for metastases • Biopsy (definitive)
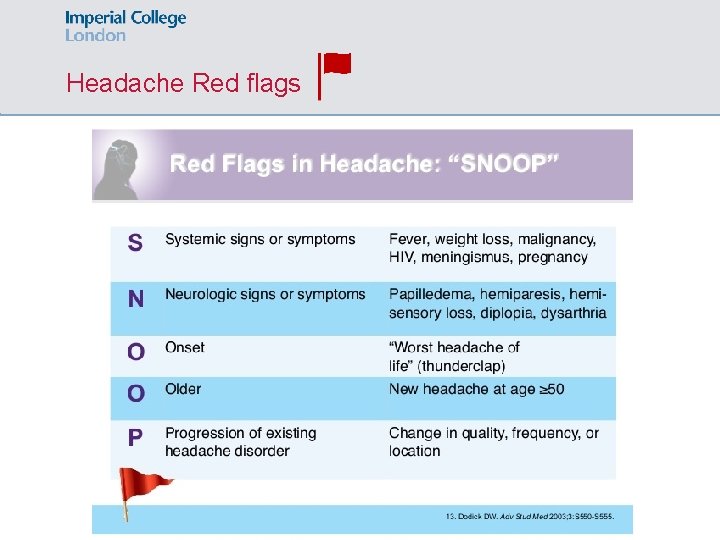
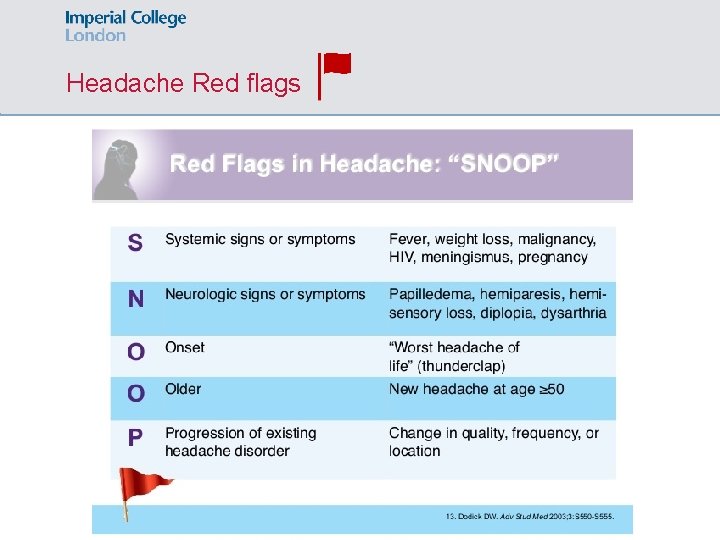
Headache Red flags
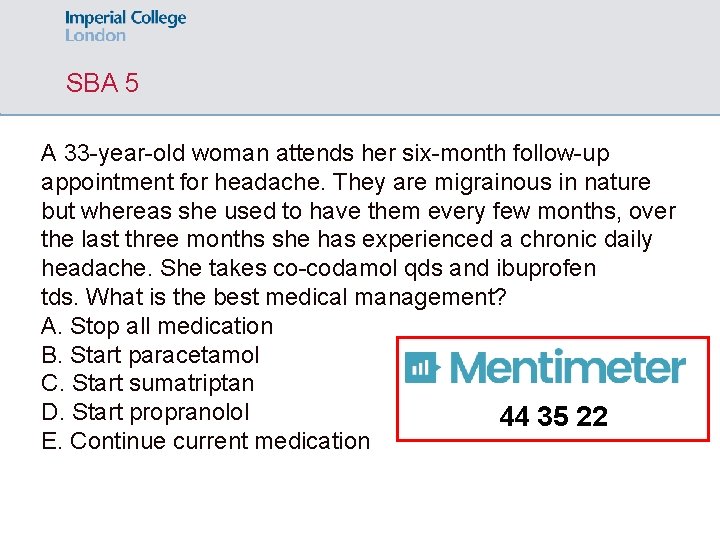
SBA 5 A 33 -year-old woman attends her six-month follow-up appointment for headache. They are migrainous in nature but whereas she used to have them every few months, over the last three months she has experienced a chronic daily headache. She takes co-codamol qds and ibuprofen tds. What is the best medical management? A. Stop all medication B. Start paracetamol C. Start sumatriptan D. Start propranolol 44 35 22 E. Continue current medication
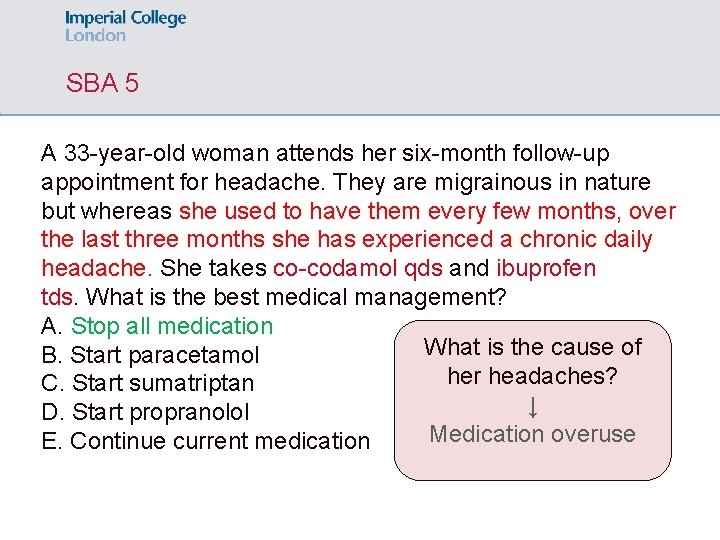
SBA 5 A 33 -year-old woman attends her six-month follow-up appointment for headache. They are migrainous in nature but whereas she used to have them every few months, over the last three months she has experienced a chronic daily headache. She takes co-codamol qds and ibuprofen tds. What is the best medical management? A. Stop all medication What is the cause of B. Start paracetamol her headaches? C. Start sumatriptan ↓ D. Start propranolol Medication overuse E. Continue current medication
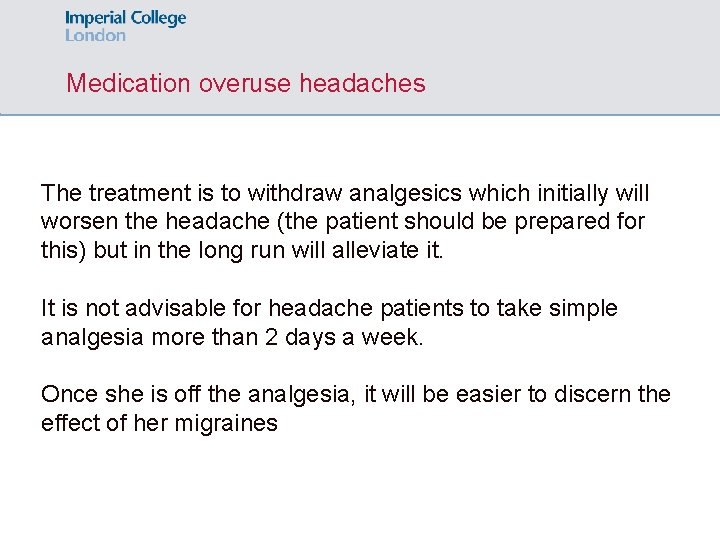
Medication overuse headaches The treatment is to withdraw analgesics which initially will worsen the headache (the patient should be prepared for this) but in the long run will alleviate it. It is not advisable for headache patients to take simple analgesia more than 2 days a week. Once she is off the analgesia, it will be easier to discern the effect of her migraines
ic_meded Feedback https: //docs. google. com/forms/d/e/1 FAIp. QLSf 8 Erll. J 2 bet. Obz. IT 6 NE_DLIt. X 4 Tok. Ehzkr. AEg. LVZwcb 1_DQ/viewform? usp=sf_link