Head and Facial Conditions Anatomy of Head and

- Slides: 42

Head and Facial Conditions
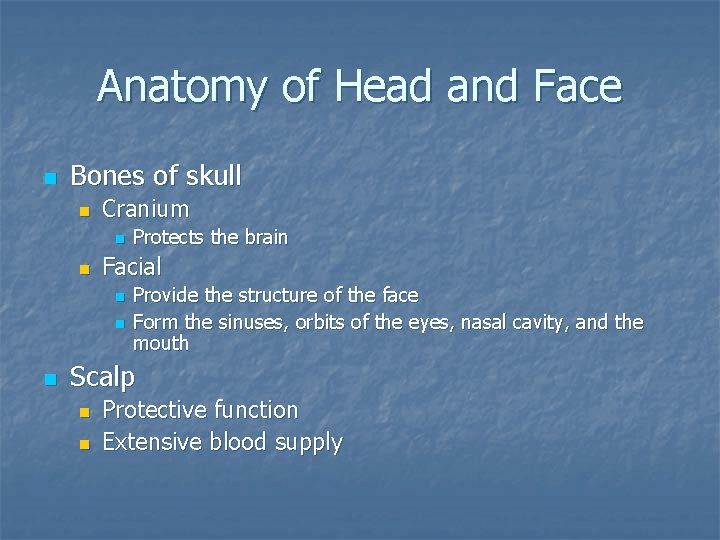
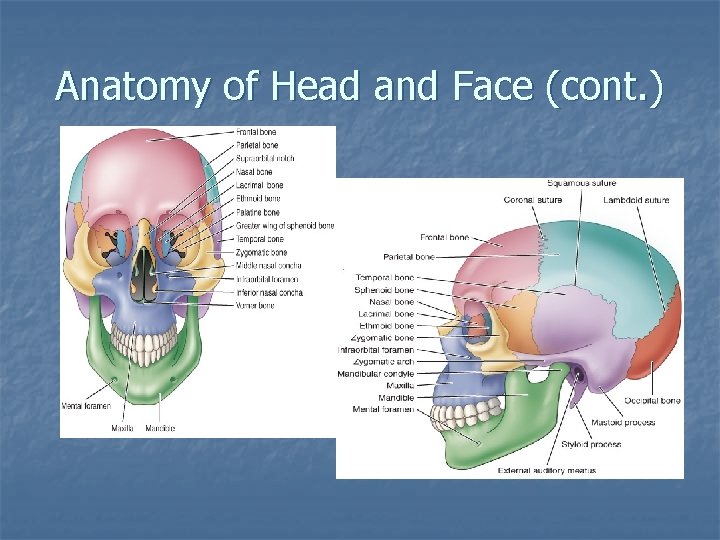
Anatomy of Head and Face n Bones of skull n Cranium n n Facial n n n Protects the brain Provide the structure of the face Form the sinuses, orbits of the eyes, nasal cavity, and the mouth Scalp n n Protective function Extensive blood supply
Anatomy of Head and Face (cont. )
Anatomy of Head and Face (cont. ) n Brain n Major regions n Cerebral hemispheres n Diencephalon n Brainstem n Cerebellum
Anatomy of Head and Face (cont. ) n Meninges n Protective tissue that encloses brain and spinal cord n Dura mater; arachnoid mater; pia mater
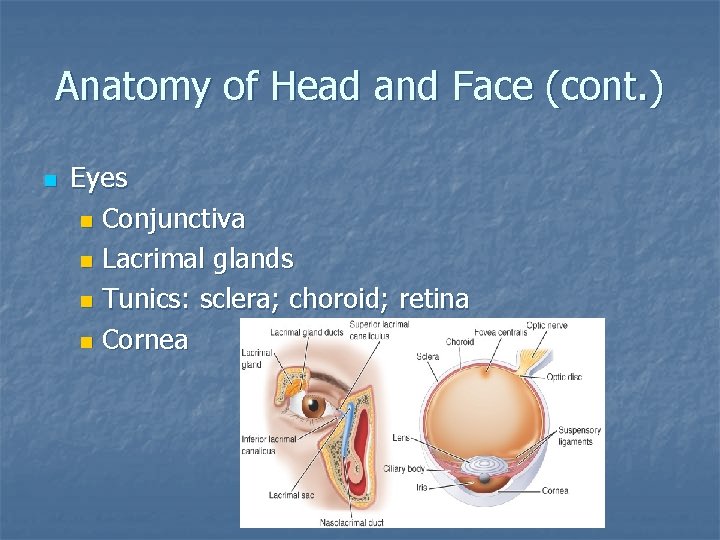
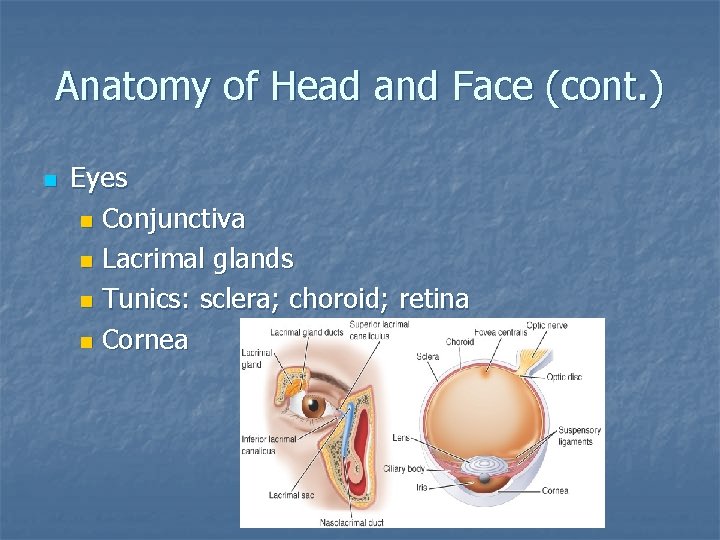
Anatomy of Head and Face (cont. ) n Eyes n Conjunctiva n Lacrimal glands n Tunics: sclera; choroid; retina n Cornea
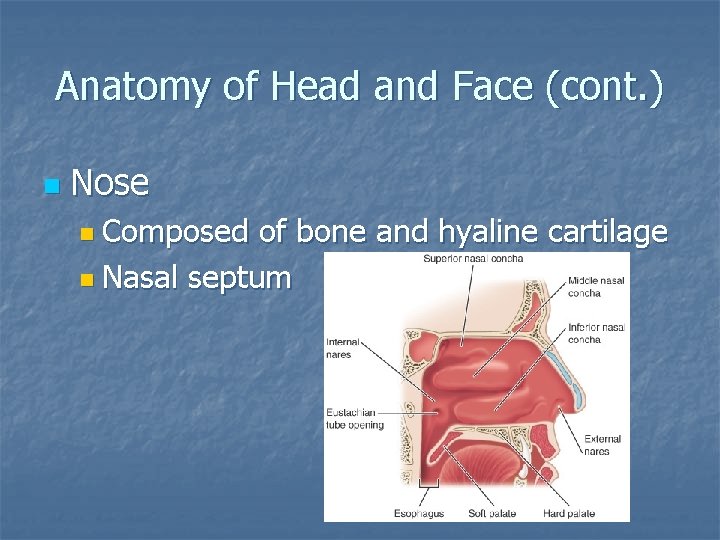
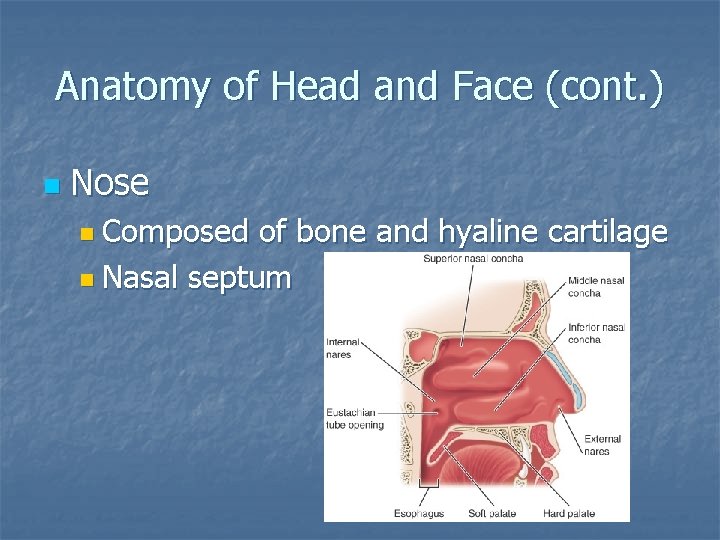
Anatomy of Head and Face (cont. ) n Nose n Composed of bone and hyaline cartilage n Nasal septum
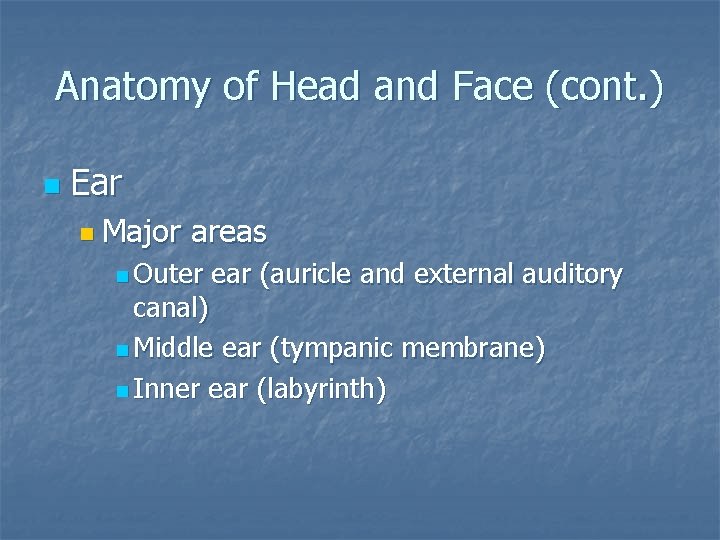
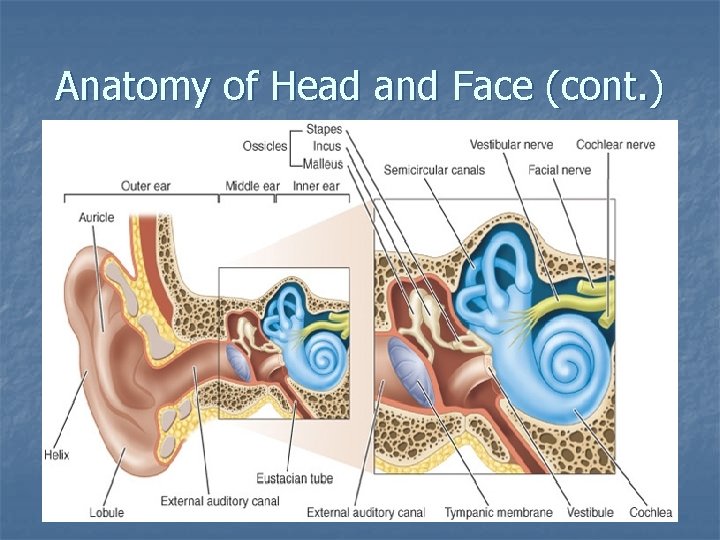
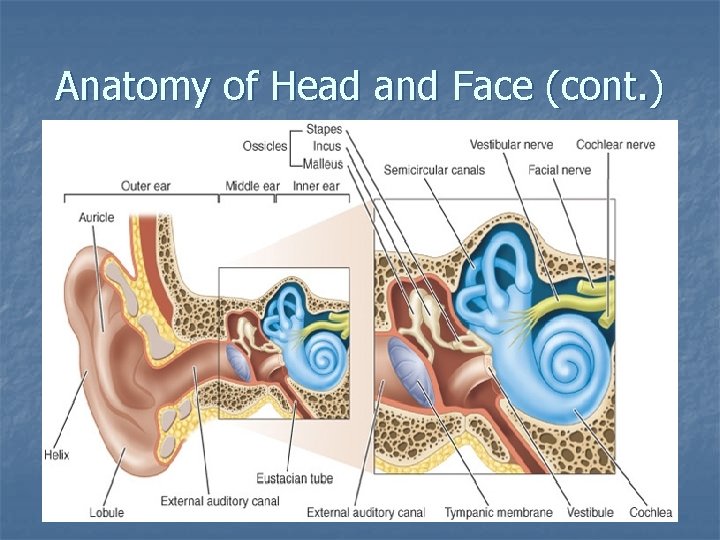
Anatomy of Head and Face (cont. ) n Ear n Major areas n Outer ear (auricle and external auditory canal) n Middle ear (tympanic membrane) n Inner ear (labyrinth)
Anatomy of Head and Face (cont. )
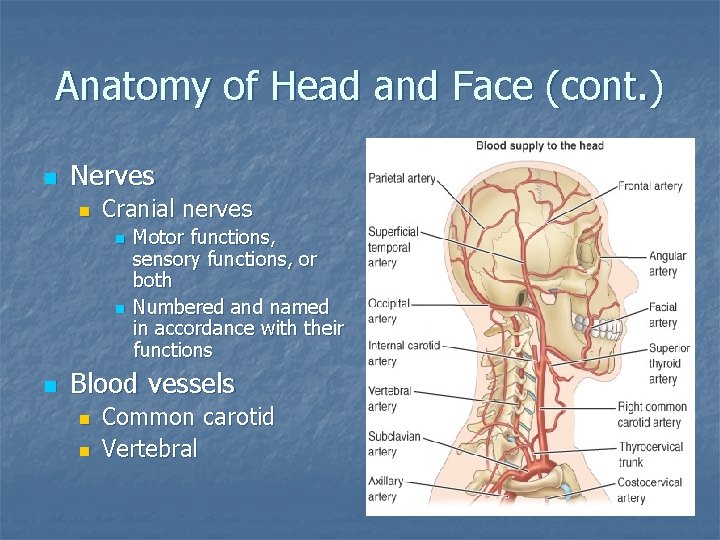
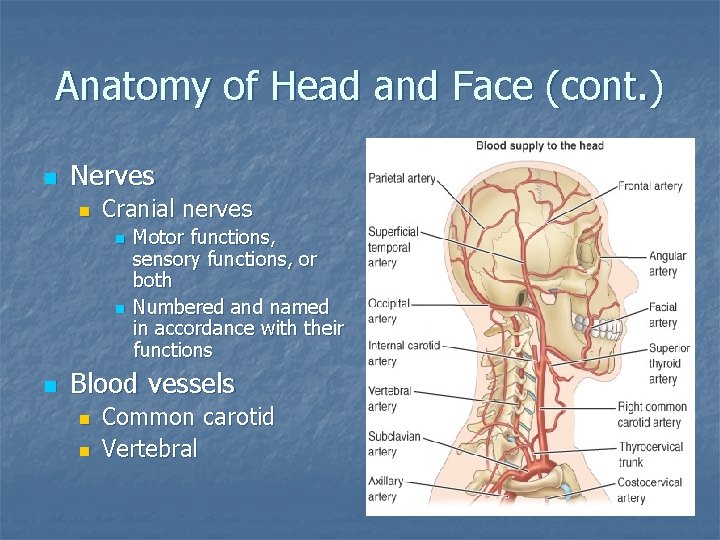
Anatomy of Head and Face (cont. ) n Nerves n Cranial nerves n n n Motor functions, sensory functions, or both Numbered and named in accordance with their functions Blood vessels n n Common carotid Vertebral
Prevention of Head and Facial Injuries n Protective equipment Helmets n Face guards n Mouth guards n Eye wear n Ear wear n Throat protectors n
Scalp Injuries n n Highly vascularized; bleeds freely Laceration n n Control bleeding Prevent contamination Assess for skull fracture (fx) Management: n n If no fx, cleanse, cover, and refer Abrasions and contusions n n Cleanse; ice and pressure 24 hours: no improvement – refer
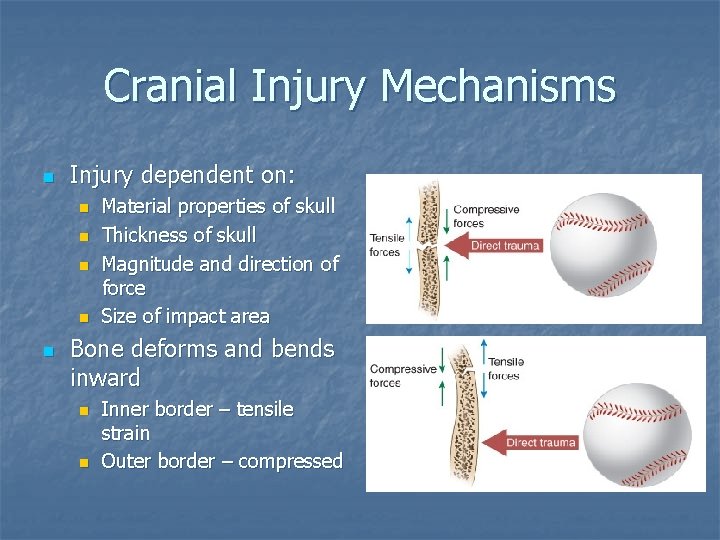
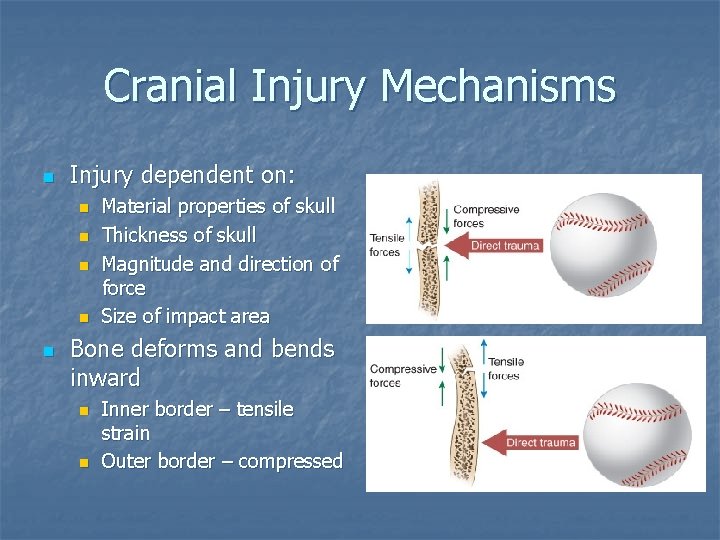
Cranial Injury Mechanisms n Injury dependent on: n n n Material properties of skull Thickness of skull Magnitude and direction of force Size of impact area Bone deforms and bends inward n n Inner border – tensile strain Outer border – compressed
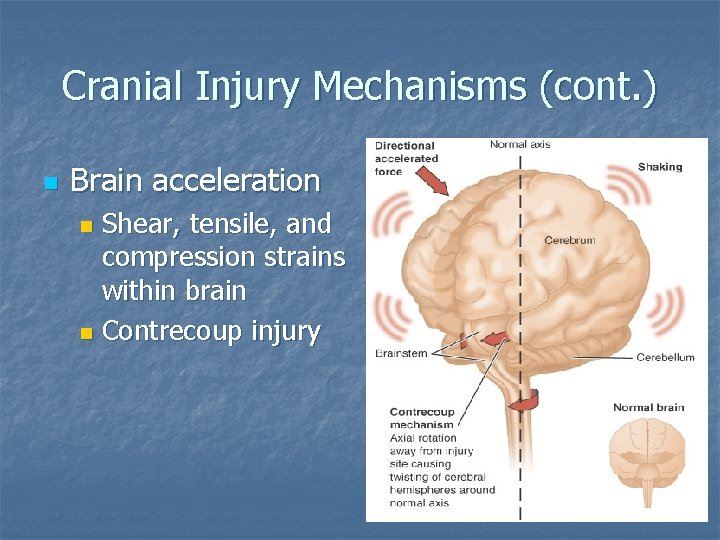
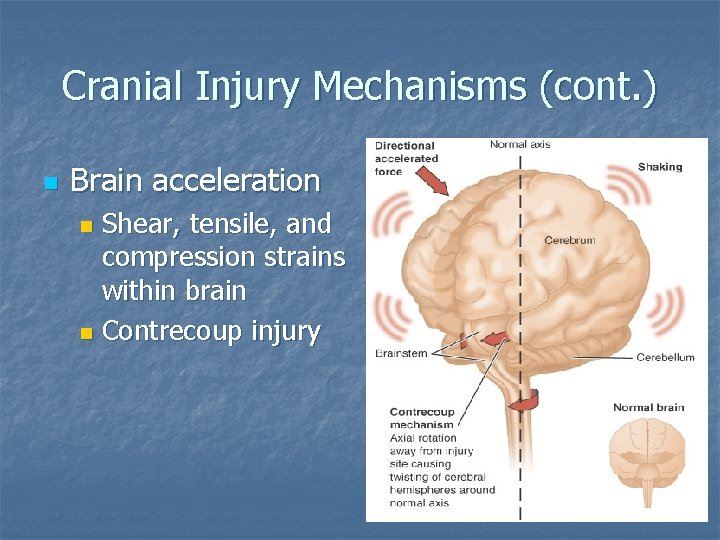
Cranial Injury Mechanisms (cont. ) n Brain acceleration Shear, tensile, and compression strains within brain n Contrecoup injury n
Cranial Injury Mechanisms (cont. ) n Focal injury n n n Diffuse injury n n Localized damage Epidural, subdural, or intracerebral hematomas Widespread disruption Concussion Accurate assessment of head injury is essential Conscious, ambulatory individual should not be considered to have only a minor injury
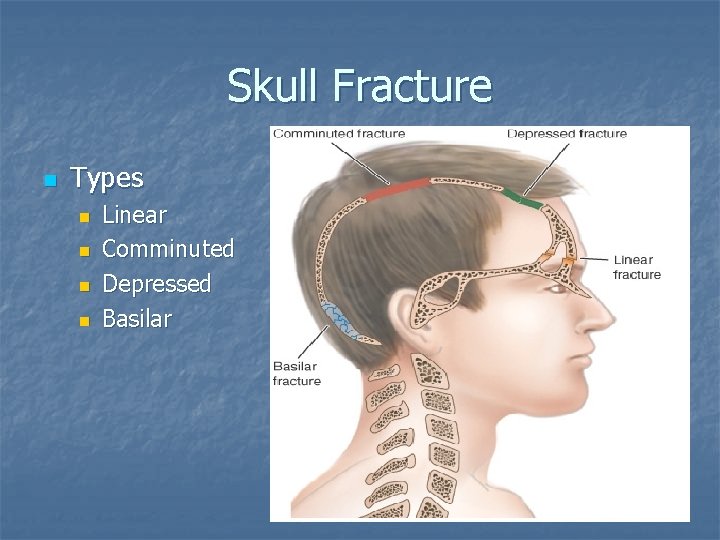
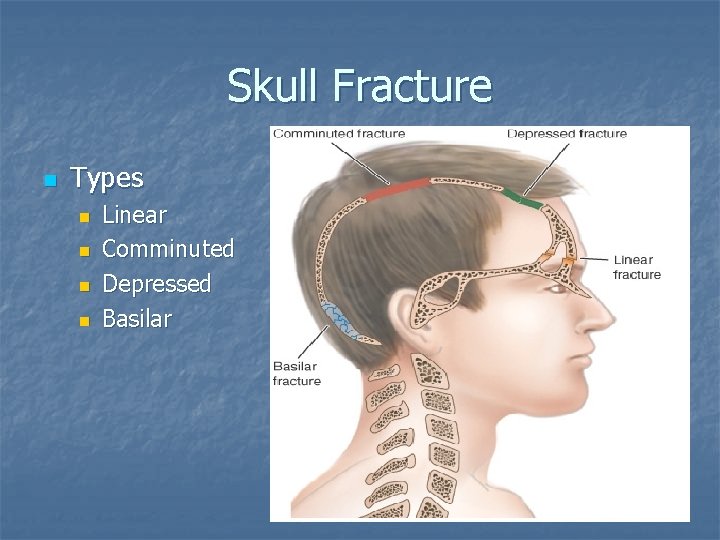
Skull Fracture n Types n n Linear Comminuted Depressed Basilar
Skull Fracture (cont. ) n Potential for varying signs and symptoms (S&S) Visible deformity–do not be misled by a “goose egg”; a fracture may be under the site n Deep laceration or severe bruise to scalp n Palpable depression or crepitus n Unequal pupils n Raccoon eyes or Battle’s sign n
Skull Fracture (cont. ) Bleeding or CSF from nose and/or ear n Loss of smell n Loss of sight or major vision disturbances n Unconsciousness 2 minutes after direct trauma to the head n n Management: activation of EMS
Facial Conditions n Facial soft tissue conditions Contusions, abrasions, and lacerations are managed the same as elsewhere on the body n Complicated injuries—immediate physician referral n
Facial Conditions (cont. ) n Temporomandibular joint conditions n S&S Inability to open and/or close mouth (dislocation and meniscus displacement) n Malocclusion n Joint crepitus with opening and closing n Pain with opening and biting n Deviation of the mandible on opening (toward side of injury) n
Facial Conditions (cont. ) n Fractures n Zygomatic n n n S&S: cheek appears flat or depressed, double vision, numbness in affected cheek Management: ice, immediate referral Mandibular n n n Common: mandibular angle and condyles S&S: malocclusion, changes in speech, oral bleeding, + tongue blade Management: ice, immediate referral
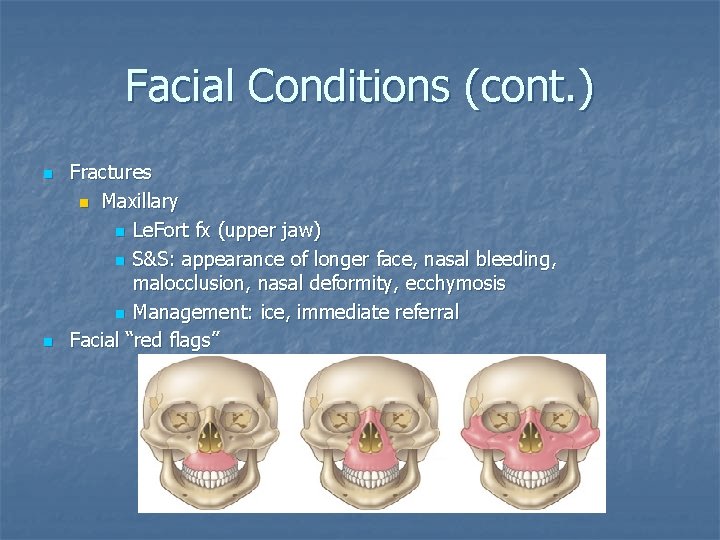
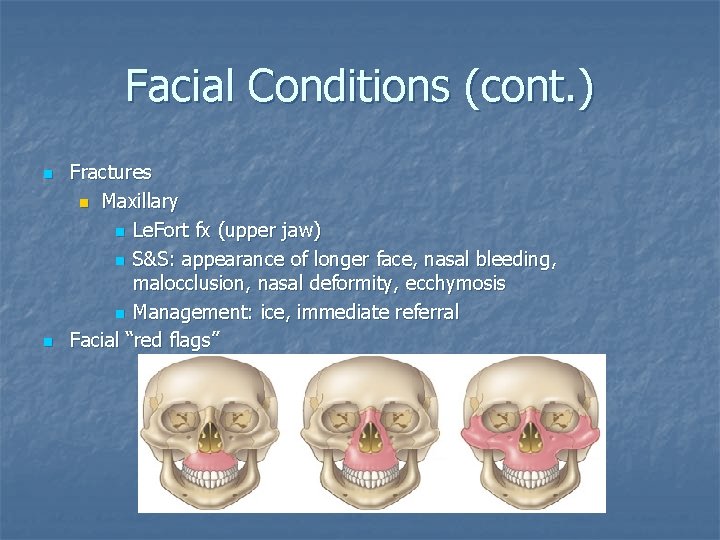
Facial Conditions (cont. ) n n Fractures n Maxillary n Le. Fort fx (upper jaw) n S&S: appearance of longer face, nasal bleeding, malocclusion, nasal deformity, ecchymosis n Management: ice, immediate referral Facial “red flags”
Nasal Conditions n Epistaxis n n n Anterior – bleeding from anterior septum Posterior – bleeding from lateral wall Management: ice, mild pressure, slight forward head tilt; nasal plug; 5 minutes – physician referral Deviated septum n S&S n n n Consistent difference in airflow between the 2 sides of the nose when one nostril is blocked Confirm using otoscope Management: physician referral
Nasal Conditions (cont. ) n Fractures n n n Most common: lateral displacement Range of severity varies S&S Asymmetry – especially with lateral force n Epistaxis n Crepitus n n n Management: control bleeding; refer Nasal “red flags”
Oral and Dental Conditions n Periodontal disease n S&S of gingivitis n Tender, swollen, or bleeding gums n Change in the gums' color from pink to dusky red n Plaque and bacteria that cover the teeth not readily visible
Oral and Dental Conditions (cont. ) n S&S of periodontitis n Swollen or recessed gums n Unpleasant taste in the mouth n Bad breath n Tooth pain n Drainage or pus around one or more teeth n Management: referral to dentist
Oral and Dental Conditions (cont. ) n Dental caries (tooth decay) n n Primarily caused by plaque. . . dissolves the tooth enamel…allows bacteria to infect the center of the tooth S&S n n n Pain during chewing Sensitivity to hot/cold foods and beverages If tooth abscess is present: § § n Throbbing pain Sharp or shooting pain Management: refer to dentist
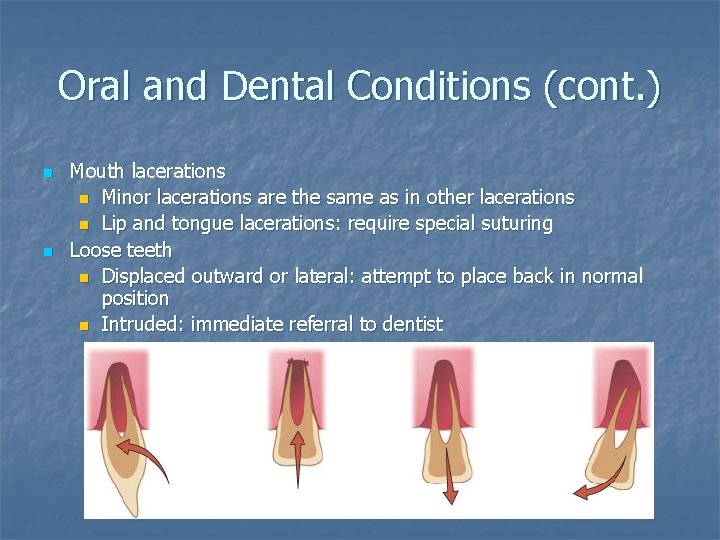
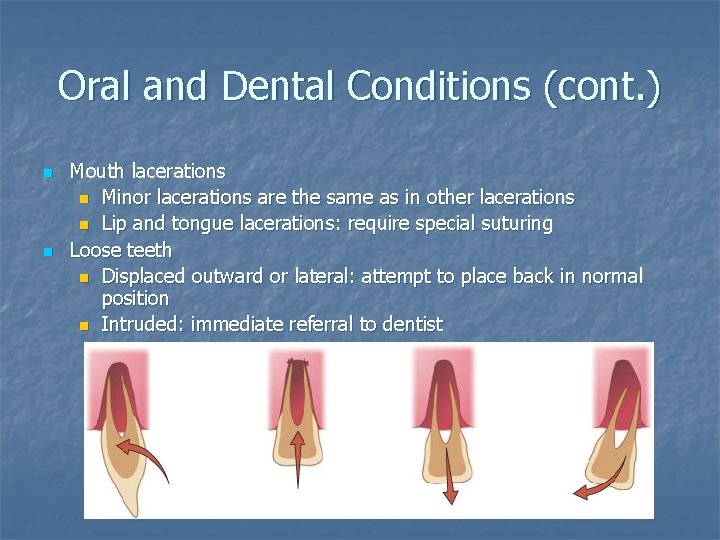
Oral and Dental Conditions (cont. ) n n Mouth lacerations n Minor lacerations are the same as in other lacerations n Lip and tongue lacerations: require special suturing Loose teeth n Displaced outward or lateral: attempt to place back in normal position n Intruded: immediate referral to dentist
Oral and Dental Conditions (cont. ) n Fractured tooth Enamel: no symptoms n Dentin: pain and increased sensitivity to heat and cold n Pulp or root: severe pain and sensitivity n Management: refer to dentist n
Oral and Dental Conditions (cont. ) n Dislocated tooth Time is of the essence; refer n Hold tooth by crown n Do not rub the tooth or remove any dirt; milk or saline n n Oral and dental “red flags”
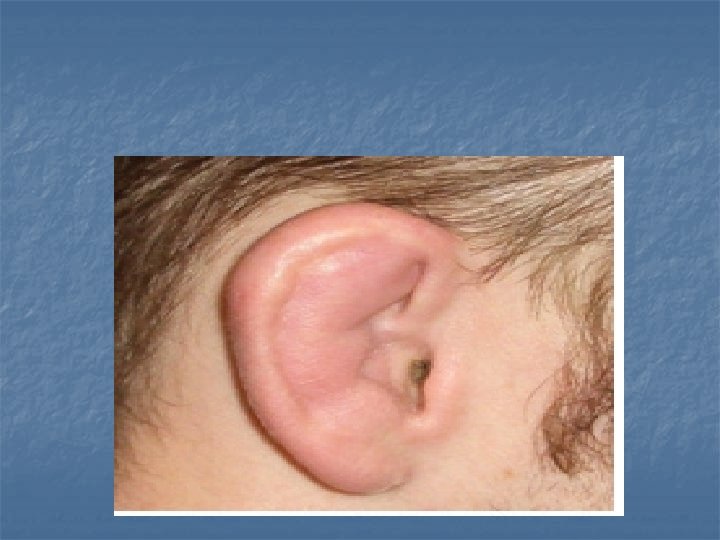
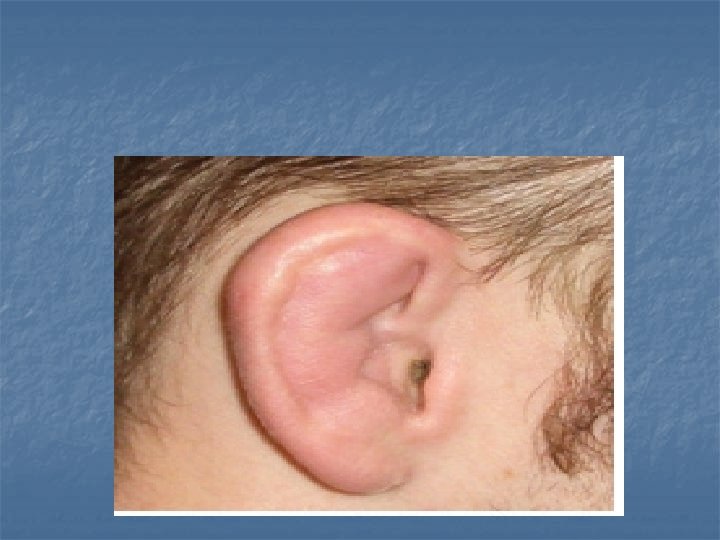
Ear Conditions n Cauliflower ear (auricular hematoma) n n n Repeated trauma pulls cartilage away from perichondrium – hematoma forms Untreated – forms a fibrosis Management: ice; possible aspiration by physician Key is prevention! Impacted cerumen (wax) n n Possible hearing loss or muffled hearing Management: irrigate canal with warm water
Ear Conditions (cont. ) n Otitis externa (swimmer’s ear) n n Bacterial infection to lining of external auditory canal S&S: pain, itching Management: ear drops, custom ear plugs Otitis media n n n Middle ear infection due to bacteria or virus S&S: earache, hearing difficulty, possible serous otitis Management: physician referral
Ear Conditions (cont. ) n Tympanic membrane rupture n Caused by: n Infection n Direct trauma n Changes in pressure n Loud, sudden noises n Foreign objects in the ear
Ear Conditions (cont. ) n S&S n Very painful n Tinnitus n Pus-filled or bloody drainage from the ear n Sudden decrease in ear pain followed by drainage n Hearing loss n n Management: physician referral Ear “red flags”
Eye Conditions n Preorbital ecchymosis (black eye) Assessment n Management: ice, referral to ophthalmologist n n Foreign bodies S&S: intense pain, tearing n Management n Not embedded: removal, inspection n Embedded: do not touch, activate EMS n
Eye Conditions (cont. ) n Sty Infection of sebaceous gland of eyelash n Starts as a red nodule; progresses into a painful pustule n Management: moist heat compress n
Eye Conditions (cont. ) n Conjunctivitis (pink eye) n n n S&S: itching, burning, watering, red appearance Management: infectious; refer to physician Corneal abrasion n n S&S: pain, tearing, photophobia, irritated with blinking and eye movement, feeling of “something in the eye” Management: drops and eye patch
Eye Conditions (cont. ) n Corneal laceration S&S: severe pain, decreased visual acuity n Management: cover with no pressure, activate EMS, transport supine or upright n
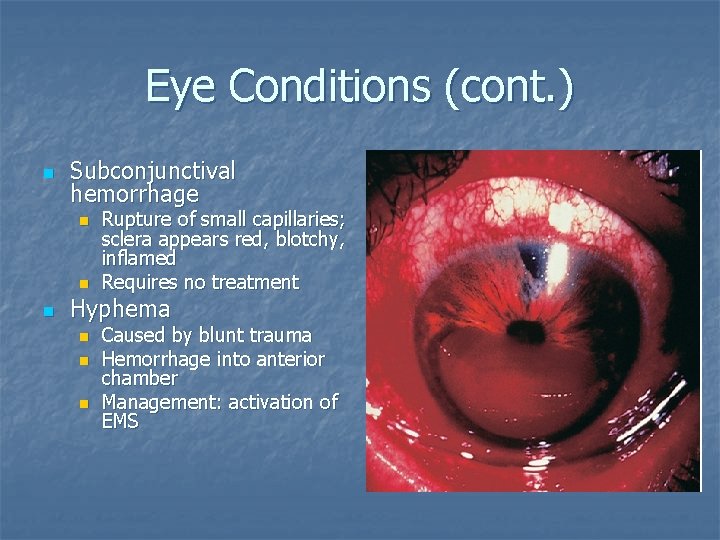
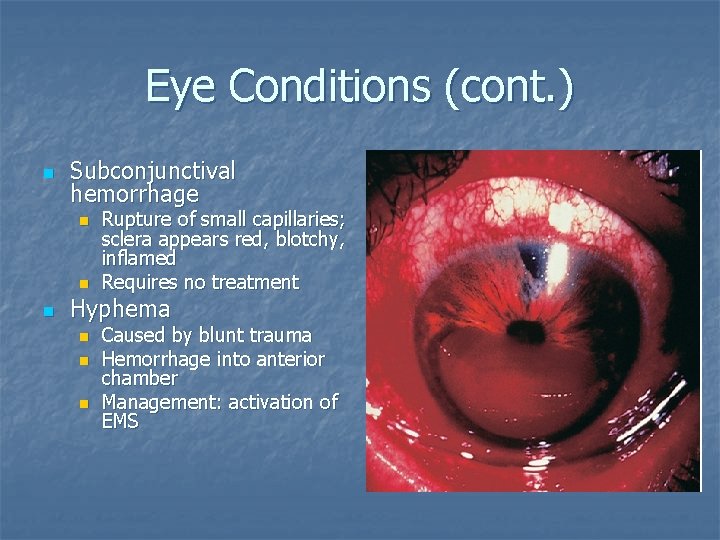
Eye Conditions (cont. ) n Subconjunctival hemorrhage n n n Rupture of small capillaries; sclera appears red, blotchy, inflamed Requires no treatment Hyphema n n n Caused by blunt trauma Hemorrhage into anterior chamber Management: activation of EMS
Eye Conditions (cont. ) n Detached retina n Can occur with or without trauma n S&S: floaters and light flashes n Management: patch both eyes; refer to ophthalmologist
Eye Conditions (cont. ) n Orbital “blowout” fracture n n Impact from a blunt object, usually larger than the eye orbit S&S: Diplopia n Numbness below eye n Lack of eye movement n Recessed downward displacement of globe n n n Management: ice; immediate referral to physician Eye “red flags”