Hand hygiene audits should be routinely performed in
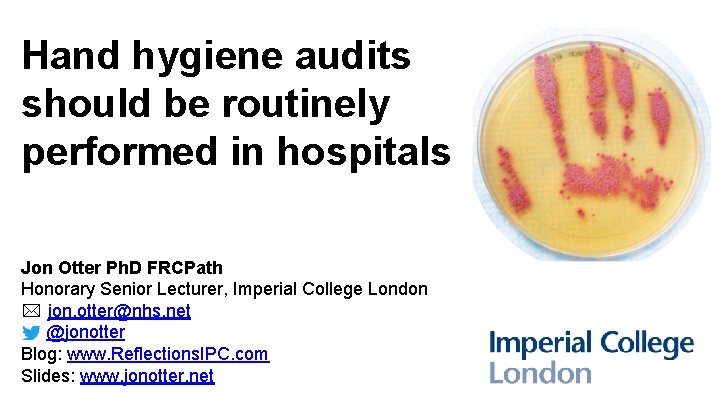
Hand hygiene audits should be routinely performed in hospitals Jon Otter Ph. D FRCPath Honorary Senior Lecturer, Imperial College London * jon. otter@nhs. net @jonotter Blog: www. Reflections. IPC. com Slides: www. jonotter. net

Hand hygiene audits should be routinely performed in hospitals
The cleaning and / or disinfection of hands using soap and water or alcohol/nonalcohol gel Hand hygiene audits should be routinely performed in hospitals
The cleaning and / or disinfection of hands using soap and water or alcohol/nonalcohol gel Clinical audit is a way to find out if healthcare is being provided in line with standards and lets care providers and patients know where their service is doing well, and where there could be improvements. The aim is to allow quality improvement to take place where it will be most helpful and will improve outcomes for patients. 1 Hand hygiene audits should be routinely performed in hospitals 1. https: //www. england. nhs. uk/clinaudit/
The cleaning and / or disinfection of hands using soap and water or alcohol/nonalcohol gel Clinical audit is a way to find out if healthcare is being provided in line with standards and lets care providers and patients know where their service is doing well, and where there could be improvements. The aim is to allow quality improvement to take place where it will be most helpful and will improve outcomes for patients. 1 Hand hygiene audits should be routinely performed in hospitals Not a one off (e. g. related to an outbreak investigation); has a set frequency (e. g. weekly, monthly, annually) 1. https: //www. england. nhs. uk/clinaudit/
The cleaning and / or disinfection of hands using soap and water or alcohol/nonalcohol gel Clinical audit is a way to find out if healthcare is being provided in line with standards and lets care providers and patients know where their service is doing well, and where there could be improvements. The aim is to allow quality improvement to take place where it will be most helpful and will improve outcomes for patients. 1 Hand hygiene audits should be routinely performed in hospitals Not a one off (e. g. related to an outbreak investigation); has a set frequency (e. g. weekly, monthly, annually) Could be a big one or a small one, but an acute care provider of secondary or tertiary healthcare services including inpatient care 1. https: //www. england. nhs. uk/clinaudit/
Hand hygiene is really important What to audit / which standard to use? A regulatory requirement An improvement journey
Hand hygiene is really important What to audit / which standard to use? A regulatory requirement An improvement journey

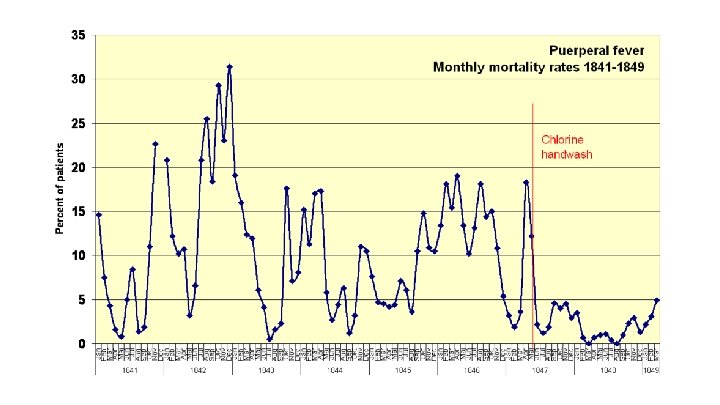
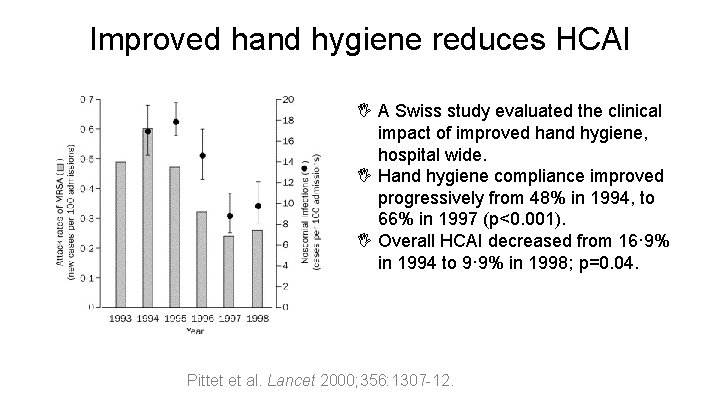
Improved hand hygiene reduces HCAI I A Swiss study evaluated the clinical impact of improved hand hygiene, hospital wide. I Hand hygiene compliance improved progressively from 48% in 1994, to 66% in 1997 (p<0. 001). I Overall HCAI decreased from 16· 9% in 1994 to 9· 9% in 1998; p=0. 04. Pittet et al. Lancet 2000; 356: 1307 -12.
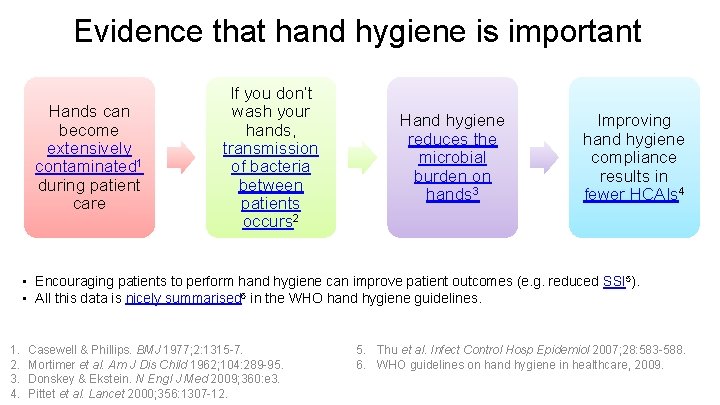
Evidence that hand hygiene is important Hands can become extensively contaminated 1 during patient care If you don’t wash your hands, transmission of bacteria between patients occurs 2 Hand hygiene reduces the microbial burden on hands 3 Improving hand hygiene compliance results in fewer HCAIs 4 • Encouraging patients to perform hand hygiene can improve patient outcomes (e. g. reduced SSI 5). • All this data is nicely summarised 6 in the WHO hand hygiene guidelines. 1. 2. 3. 4. Casewell & Phillips. BMJ 1977; 2: 1315 -7. Mortimer et al. Am J Dis Child 1962; 104: 289 -95. Donskey & Ekstein. N Engl J Med 2009; 360: e 3. Pittet et al. Lancet 2000; 356: 1307 -12. 5. Thu et al. Infect Control Hosp Epidemiol 2007; 28: 583 -588. 6. WHO guidelines on hand hygiene in healthcare, 2009.

Hand hygiene is really important What to audit / which standard to use? A regulatory requirement An improvement journey
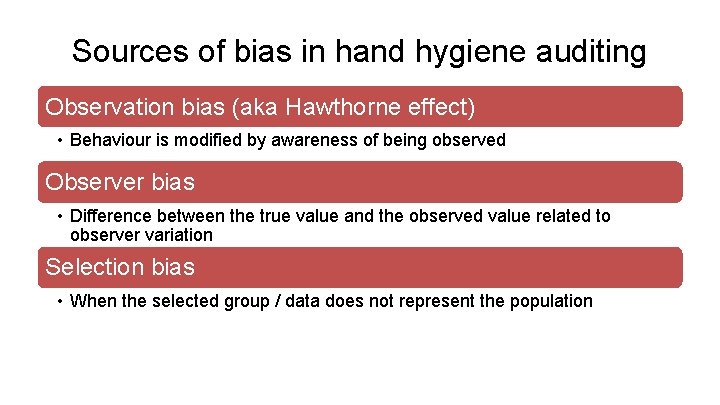
Sources of bias in hand hygiene auditing Observation bias (aka Hawthorne effect) • Behaviour is modified by awareness of being observed Observer bias • Difference between the true value and the observed value related to observer variation Selection bias • When the selected group / data does not represent the population
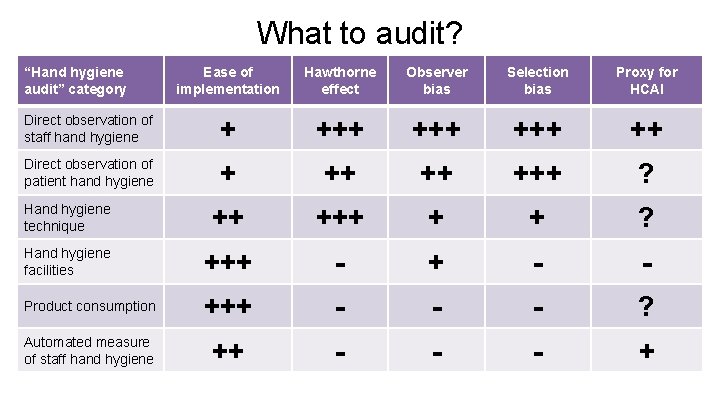
What to audit? “Hand hygiene audit” category Ease of implementation Hawthorne effect Observer bias Selection bias Proxy for HCAI Direct observation of staff hand hygiene + +++ ++ Direct observation of patient hand hygiene + ++ ++ +++ ? Hand hygiene technique ++ + + ? Hand hygiene facilities +++ - - Product consumption +++ - - - ? Automated measure of staff hand hygiene ++ - - - +
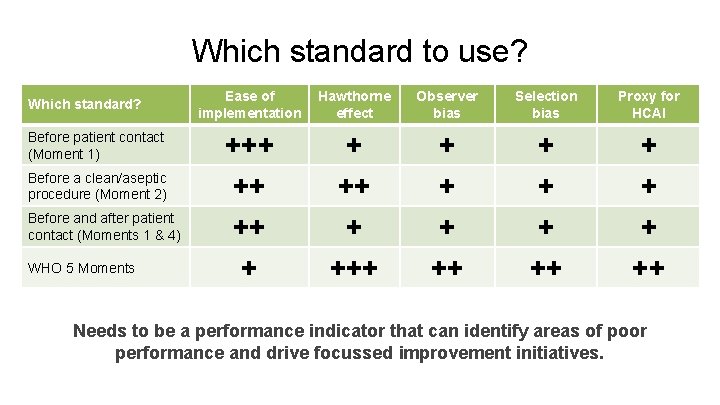
Which standard to use? Which standard? Before patient contact (Moment 1) Before a clean/aseptic procedure (Moment 2) Before and after patient contact (Moments 1 & 4) WHO 5 Moments Ease of implementation Hawthorne effect Observer bias Selection bias Proxy for HCAI +++ ++ +++ + + + ++ Needs to be a performance indicator that can identify areas of poor performance and drive focussed improvement initiatives.
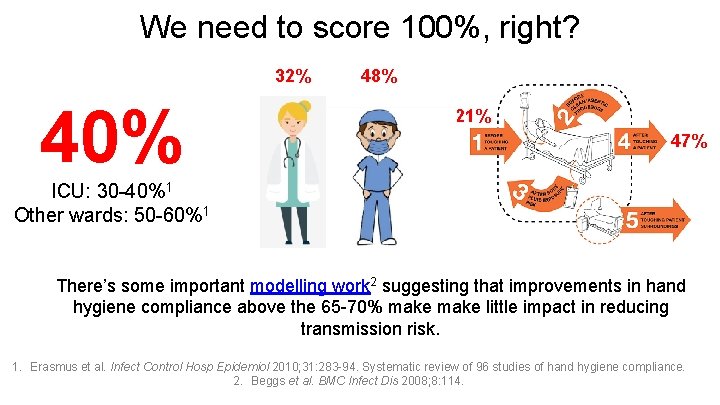
We need to score 100%, right? 32% 40% 48% 21% 47% ICU: 30 -40%1 Other wards: 50 -60%1 There’s some important modelling work 2 suggesting that improvements in hand hygiene compliance above the 65 -70% make little impact in reducing transmission risk. 1. Erasmus et al. Infect Control Hosp Epidemiol 2010; 31: 283 -94. Systematic review of 96 studies of hand hygiene compliance. 2. Beggs et al. BMC Infect Dis 2008; 8: 114.
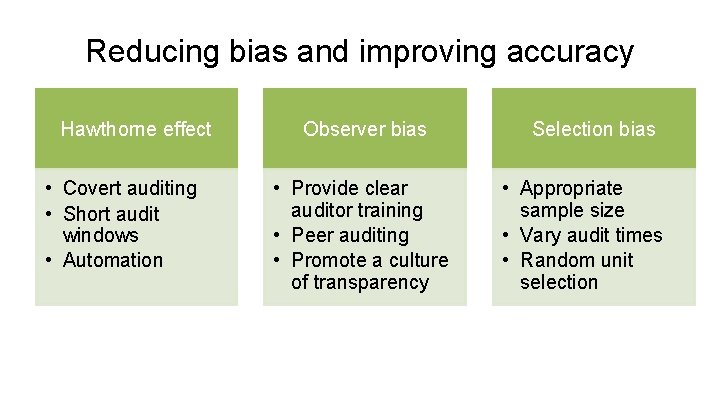
Reducing bias and improving accuracy Hawthorne effect • Covert auditing • Short audit windows • Automation Observer bias • Provide clear auditor training • Peer auditing • Promote a culture of transparency Selection bias • Appropriate sample size • Vary audit times • Random unit selection
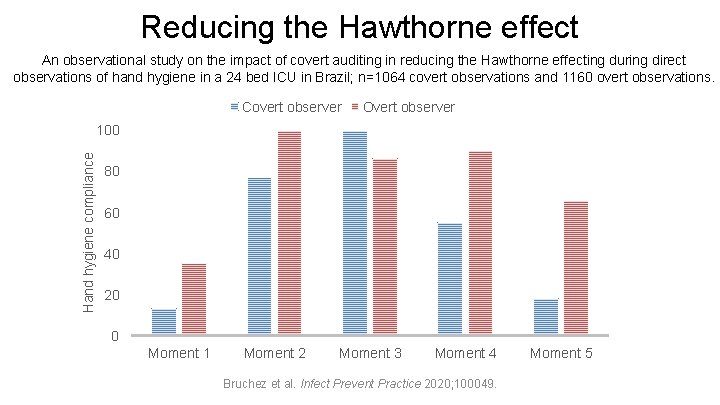
Reducing the Hawthorne effect An observational study on the impact of covert auditing in reducing the Hawthorne effecting during direct observations of hand hygiene in a 24 bed ICU in Brazil; n=1064 covert observations and 1160 overt observations. Covert observer Overt observer Hand hygiene compliance 100 80 60 40 20 0 Moment 1 Moment 2 Moment 3 Moment 4 Bruchez et al. Infect Prevent Practice 2020; 100049. Moment 5
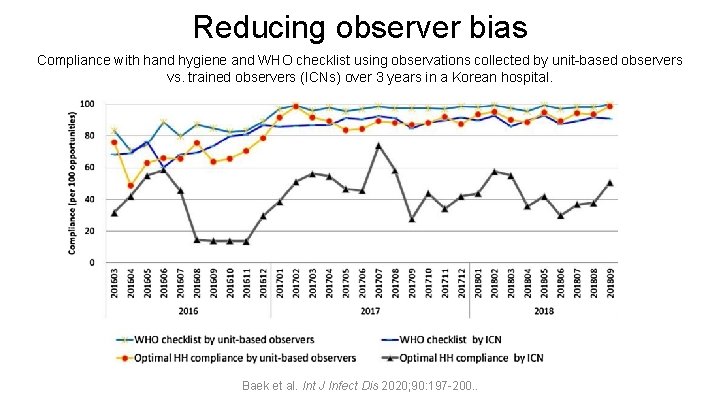
Reducing observer bias Compliance with hand hygiene and WHO checklist using observations collected by unit-based observers vs. trained observers (ICNs) over 3 years in a Korean hospital. Baek et al. Int J Infect Dis 2020; 90: 197 -200. .
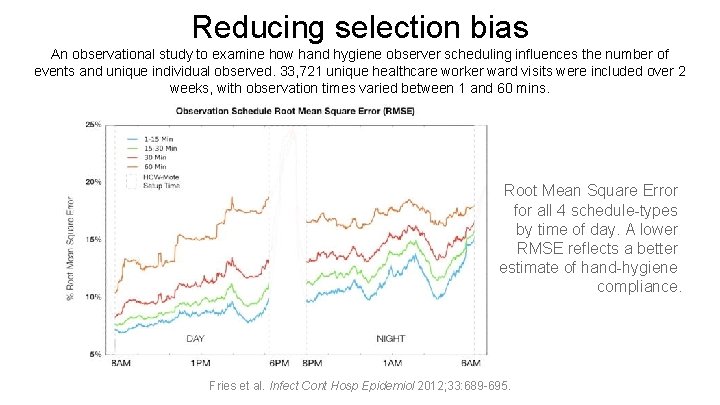
Reducing selection bias An observational study to examine how hand hygiene observer scheduling influences the number of events and unique individual observed. 33, 721 unique healthcare worker ward visits were included over 2 weeks, with observation times varied between 1 and 60 mins. Root Mean Square Error for all 4 schedule-types by time of day. A lower RMSE reflects a better estimate of hand-hygiene compliance. Fries et al. Infect Cont Hosp Epidemiol 2012; 33: 689 -695.
Hand hygiene is really important What to audit / which standard to use? A regulatory requirement An improvement journey
A regulatory requirement Health and Social Care Act NICE Quality Standard 61 (IPC) CQC National Hand Hygiene Policy
Health and Social Care Act Preventing infections reduces the overall need to use antimicrobials and helps to reduce selection pressure for the development of antimicrobial resistance. • Policy should be based on evidence-based guidelines, including those on hand hygiene at the point of care and the use of personal protective equipment; • Policy should be easily accessible and be understood by all groups of staff, service users and the public. • Compliance with the policy should be audited https: //assets. publishing. service. gov. uk/government/uploads/system/uploads/attachment_data/file/449049/Code_of_practice_280715_acc. pdf
NICE Quality Standard 61 (IPC) • Quality statement: People receive healthcare from healthcare workers who decontaminate their hands immediately before and after every episode of direct contact or care. • Quality measure: Evidence of local arrangements to ensure that regular local hand hygiene observation audits are undertaken. • What the quality statement means for different audiences – commissioners: Ensure that they commission services in which healthcare workers are trained in effective hand decontamination techniques and decontaminate their hands immediately before and after every episode of direct contact or care, and that hand hygiene observation audits are carried out regularly. https: //www. nice. org. uk/guidance/qs 61/chapter/Quality-statement-3 -Hand-decontamination. (Selected sections. )
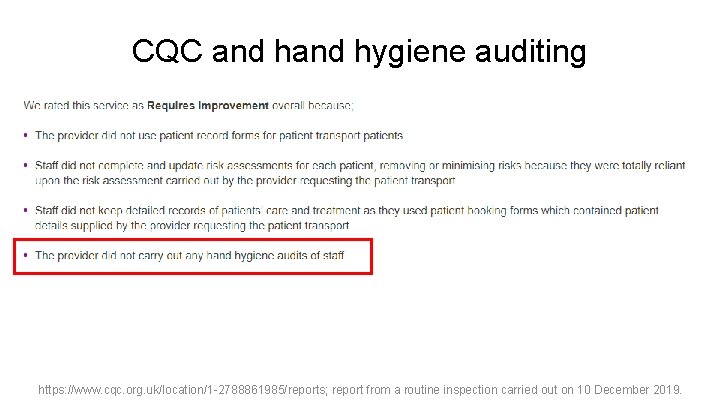
CQC and hygiene auditing https: //www. cqc. org. uk/location/1 -2788861985/reports; report from a routine inspection carried out on 10 December 2019.
Standard infection control precautions: national hand hygiene and personal protective equipment policy Organisations must: • have systems and resources to implement and monitor compliance with infection prevention and control as specified in this policy in all care areas; compliance monitoring includes all staff (permanent, agency and, where required, external contractors). https: //improvement. nhs. uk/resources/national-hand-hygiene-and-personal-protective-equipment-policy/
Hand hygiene is really important What to audit / which standard to use? A regulatory requirement An improvement journey

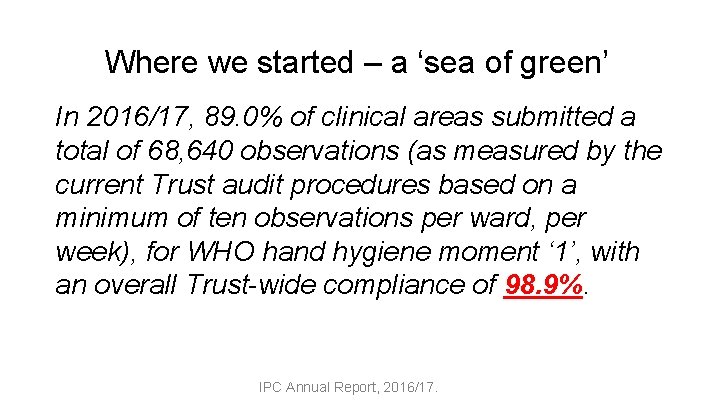
Where we started – a ‘sea of green’ In 2016/17, 89. 0% of clinical areas submitted a total of 68, 640 observations (as measured by the current Trust audit procedures based on a minimum of ten observations per ward, per week), for WHO hand hygiene moment ‘ 1’, with an overall Trust-wide compliance of 98. 9%. IPC Annual Report, 2016/17.
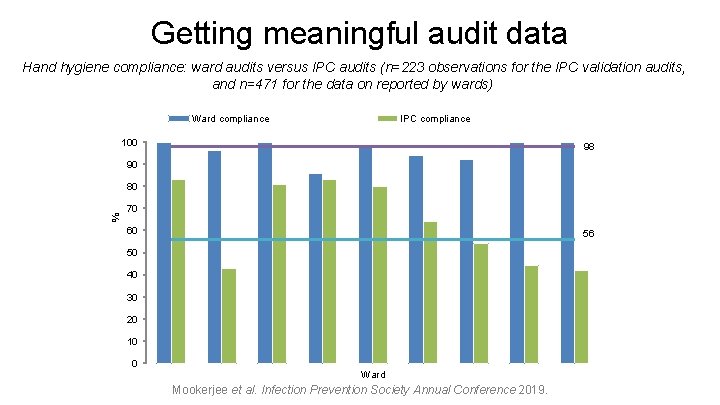
Getting meaningful audit data Hand hygiene compliance: ward audits versus IPC audits (n=223 observations for the IPC validation audits, and n=471 for the data on reported by wards) Ward compliance IPC compliance 100 98 90 % 80 70 60 56 50 40 30 20 10 0 Ward Mookerjee et al. Infection Prevention Society Annual Conference 2019.
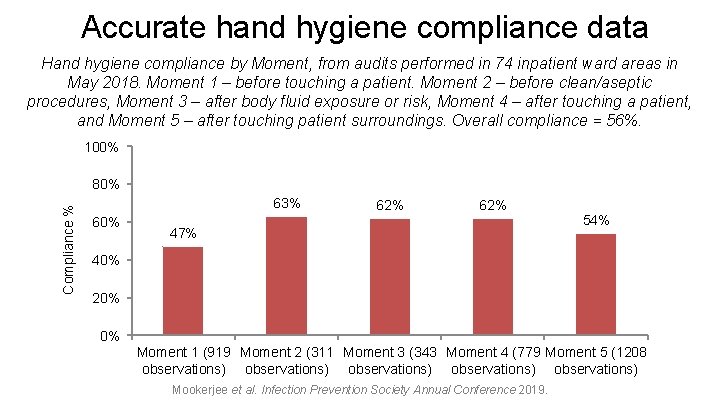
Accurate hand hygiene compliance data Hand hygiene compliance by Moment, from audits performed in 74 inpatient ward areas in May 2018. Moment 1 – before touching a patient. Moment 2 – before clean/aseptic procedures, Moment 3 – after body fluid exposure or risk, Moment 4 – after touching a patient, and Moment 5 – after touching patient surroundings. Overall compliance = 56%. 100% Compliance % 80% 63% 60% 62% 47% 54% 40% 20% 0% Moment 1 (919 Moment 2 (311 Moment 3 (343 Moment 4 (779 Moment 5 (1208 observations) observations) Mookerjee et al. Infection Prevention Society Annual Conference 2019.
Audit Improvement Comms
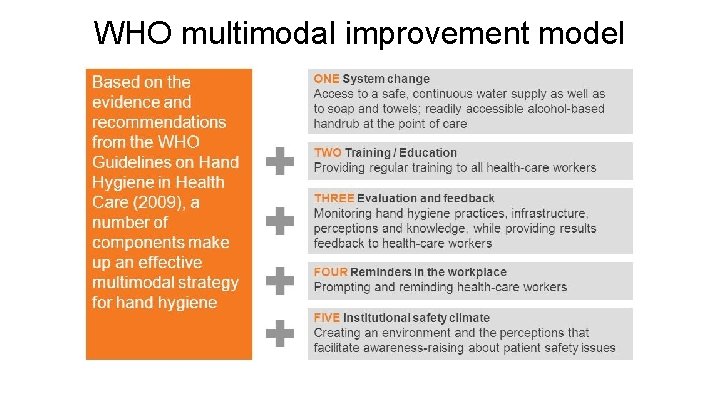
WHO multimodal improvement model
Improvement journey I All wards: locally developed improvement plans. I “Focus wards” with lowest audit results selected to create locally development improvement plans supported by the Improvement Team and IPC. I Specific staff groups: therapists targeted for further support.
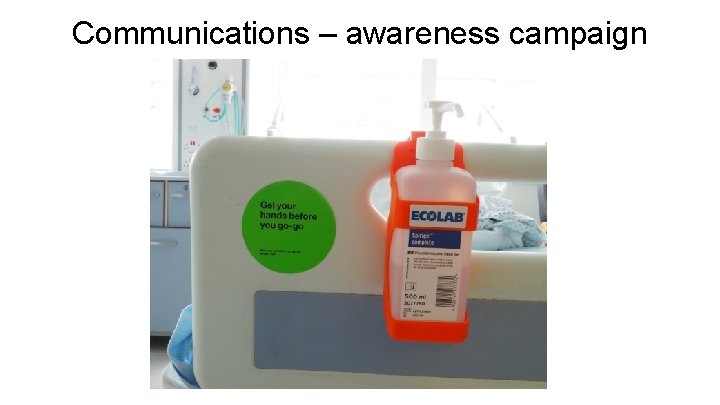
Communications – awareness campaign
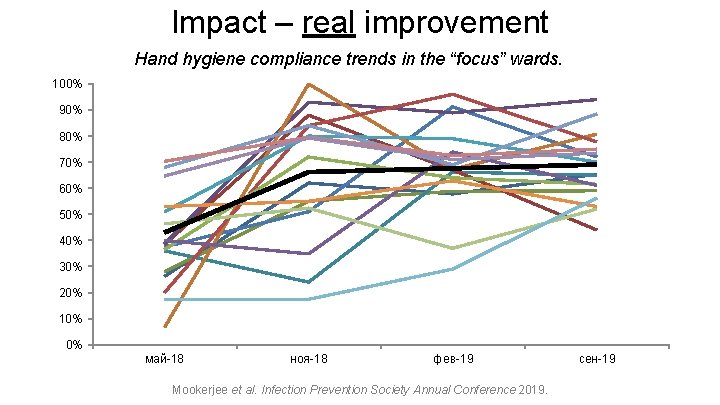
Impact – real improvement Hand hygiene compliance trends in the “focus” wards. 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% май-18 ноя-18 фев-19 Mookerjee et al. Infection Prevention Society Annual Conference 2019. сен-19
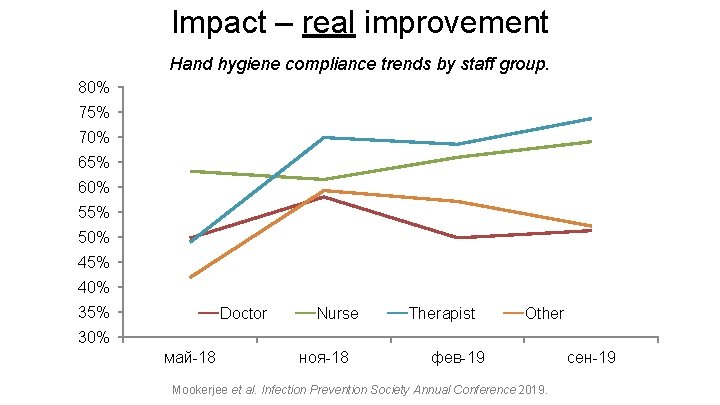
Impact – real improvement Hand hygiene compliance trends by staff group. 80% 75% 70% 65% 60% 55% 50% 45% 40% 35% Doctor Nurse Therapist Other 30% май-18 ноя-18 фев-19 Mookerjee et al. Infection Prevention Society Annual Conference 2019. сен-19
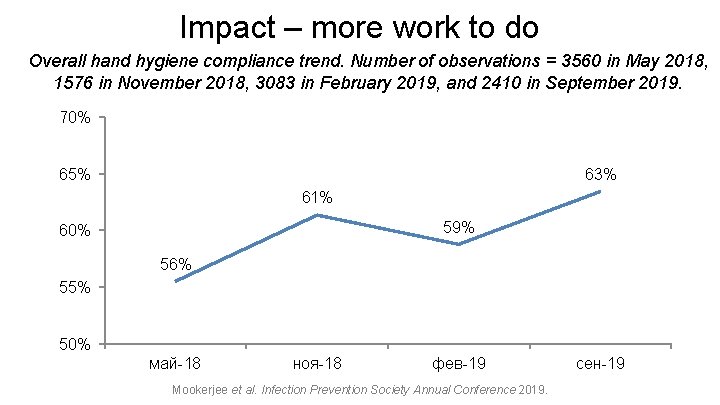
Impact – more work to do Overall hand hygiene compliance trend. Number of observations = 3560 in May 2018, 1576 in November 2018, 3083 in February 2019, and 2410 in September 2019. 70% 65% 63% 61% 59% 60% 56% 55% 50% май-18 ноя-18 фев-19 Mookerjee et al. Infection Prevention Society Annual Conference 2019. сен-19
Hand hygiene audits should be routinely performed in hospitals because… • Clinical audit is the best way to measure the performance of a clinical service • Audit programmes related to IPC practice are a legal and regulatory requirement • Low levels of hand hygiene are a warning sign that HCAIs are imminent • Good quality routine hand hygiene audit data is the only way to launch a meaningful hand hygiene improvement programme
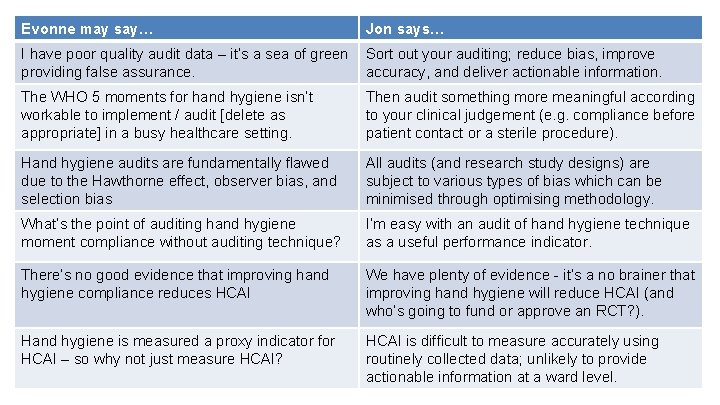
Evonne may say… Jon says… I have poor quality audit data – it’s a sea of green providing false assurance. Sort out your auditing; reduce bias, improve accuracy, and deliver actionable information. The WHO 5 moments for hand hygiene isn’t workable to implement / audit [delete as appropriate] in a busy healthcare setting. Then audit something more meaningful according to your clinical judgement (e. g. compliance before patient contact or a sterile procedure). Hand hygiene audits are fundamentally flawed due to the Hawthorne effect, observer bias, and selection bias All audits (and research study designs) are subject to various types of bias which can be minimised through optimising methodology. What’s the point of auditing hand hygiene moment compliance without auditing technique? I’m easy with an audit of hand hygiene technique as a useful performance indicator. There’s no good evidence that improving hand hygiene compliance reduces HCAI We have plenty of evidence - it’s a no brainer that improving hand hygiene will reduce HCAI (and who’s going to fund or approve an RCT? ). Hand hygiene is measured a proxy indicator for HCAI – so why not just measure HCAI? HCAI is difficult to measure accurately using routinely collected data; unlikely to provide actionable information at a ward level.


Acknowledgements • Colleges in the Imperial IPC Team, Improvement Team, and Hygiene Improvement Group
Hand hygiene audits should be routinely performed in hospitals Jon Otter Ph. D FRCPath Honorary Senior Lecturer, Imperial College London * jon. otter@nhs. net @jonotter Blog: www. Reflections. IPC. com Slides: www. jonotter. net
- Slides: 47