HAMSTRING INJURY The accuracy of MRI in predicting

































- Slides: 75
HAMSTRING INJURY

The accuracy of MRI in predicting recovery and recurrence of hamstring muscle strains l l Dr N Gibbs Dr T Cross Mr M Cameron Dr M Houang J Sci Med Sport. 2004 Jun
1. Introduction 2. Literature review 3. Methods 4. Results and Discussion 5. Conclusions 6. Questions? ?

Clinical Scenario e. g. . Posterior thigh pain 7 days before World Cup Final Can he play? ?
1. Introduction
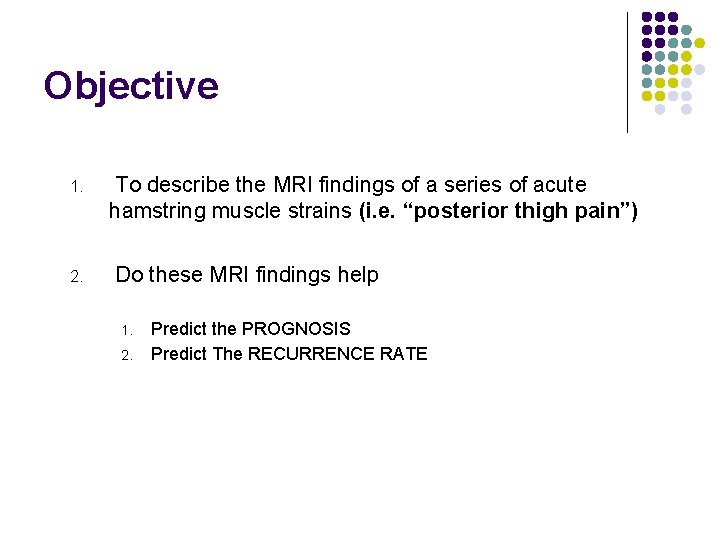
Objective 1. 2. To describe the MRI findings of a series of acute hamstring muscle strains (i. e. “posterior thigh pain”) Do these MRI findings help 1. 2. Predict the PROGNOSIS Predict The RECURRENCE RATE

Setting l l Sydney Swans Football Club 1 of 16 clubs in the National competition

Design Prospective study over 5 years (1999 -2003): Both in-season and pre-season periods
Patients 40 professional footballers Consent from Club and individual players

Australian Rules Football “Athletes at risk” l l Repetitive sprinting efforts Repetitive kicking Repetitive jumping & landing Game time approximately 100 minutes
Australian Rules Football Ideal sport ( “outdoor laboratory”) to study muscle strain injury

Australian Rules Football Hamstring strain is the most significant injury in ARF (Quadriceps strain in top 10)

Motivation for research l To better understand/diagnose Hamstring muscle strains l To better manage/rehabilitate Hamstring muscle strains
Motivation for research l To make an EARLY ACCURATE PROGNOSIS (i. e. we were unable to clinically differentiate benign from serious Hamstring strains)
Motivation for research l To better understand which “hamstring” injuries recur
2. Literature Review
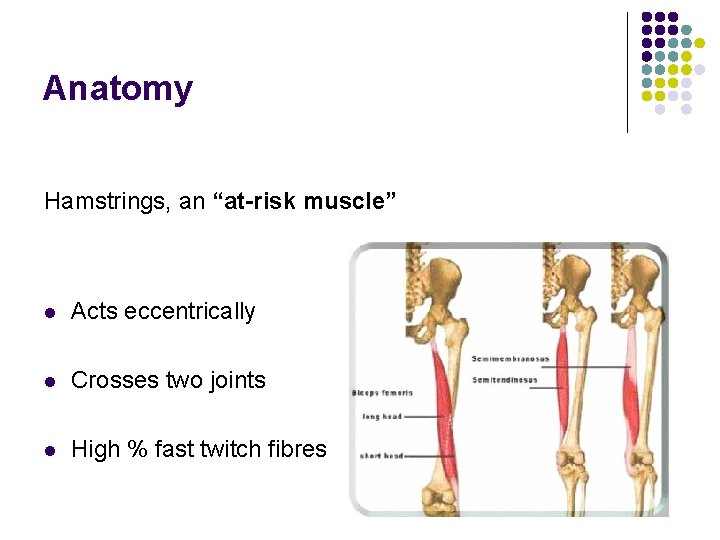
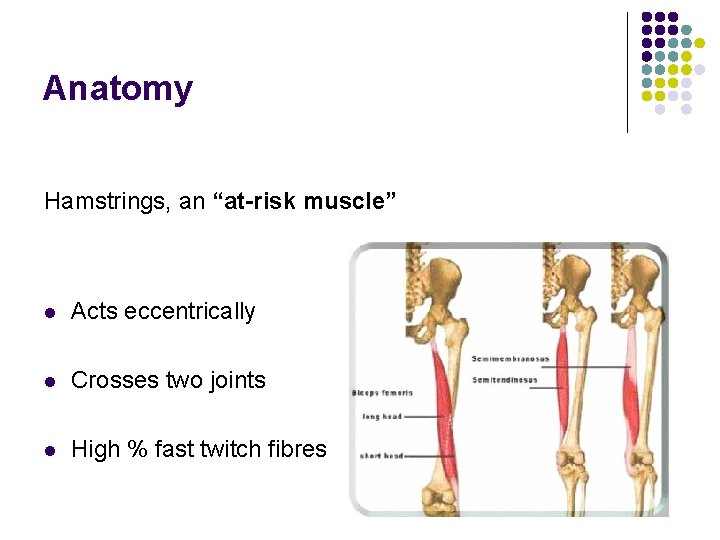
Anatomy Hamstrings, an “at-risk muscle” l Acts eccentrically l Crosses two joints l High % fast twitch fibres

Function Main Function during sprinting And kicking is to deceleration of knee extension and hip flexion

AFL injury database l Cause 20% of all missed AFL games l Recurrence rate 34%
Literature review Pomeranz (1993) • Retrospective study of Hamstring strains • n=14 • Prognosis associated with size (cross-sectional area%) of muscle strain injury on MRI scan
3. Methods
Methods Inclusion criteria 1. History acute onset of posterior thigh pain/ache or tightness while training or playing 2. Examination : tenderness over the posterior thigh : other signs elicited but not the subject of this study

Methods Exclusion criteria 1. History of trauma to posterior thigh (Contusion) 2. Delayed onset of posterior thigh pain (DOMS) 3. Recurrence of posterior thigh pain in ipsilateral thigh in same season
Methods MRI within 24 -72 hours • T 1, T 2 with fat suppression, STIR • Axial, coronal planes (both thighs imaged) (Axial T 2 with fat suppression most useful images)
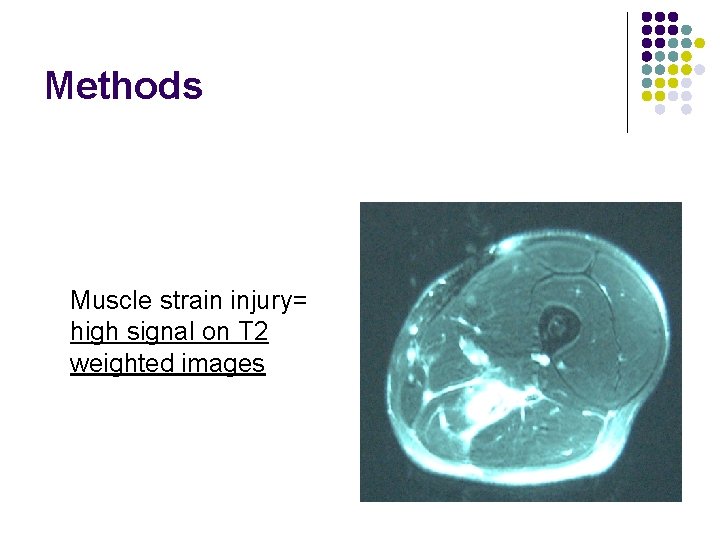
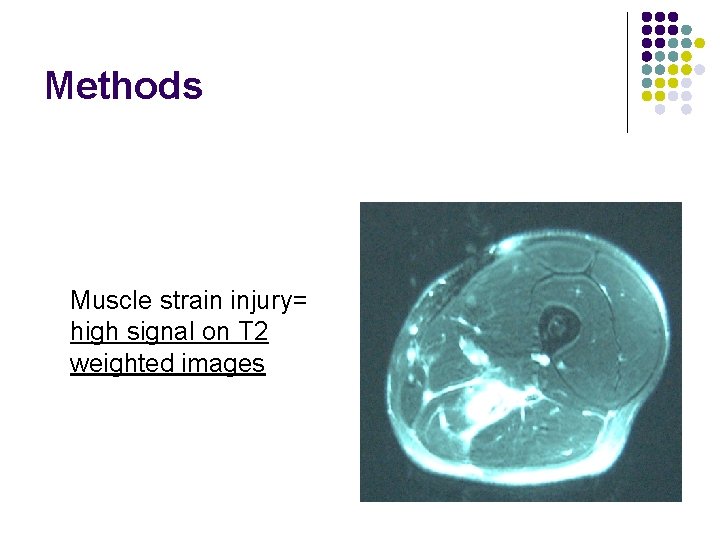
Methods Muscle strain injury= high signal on T 2 weighted images
Methods MRI diagnosis Location (MRI category) 1. 2. Which Hamstring muscle (s) injured Location of injury with respect to known musculotendinous junctions
Methods MRI diagnosis Size 1. Cross sectional area % (CSA) 2. Length (cm)
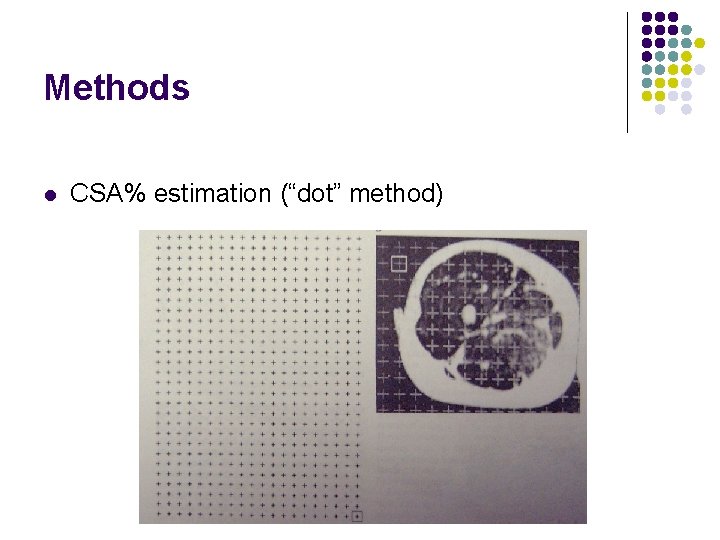
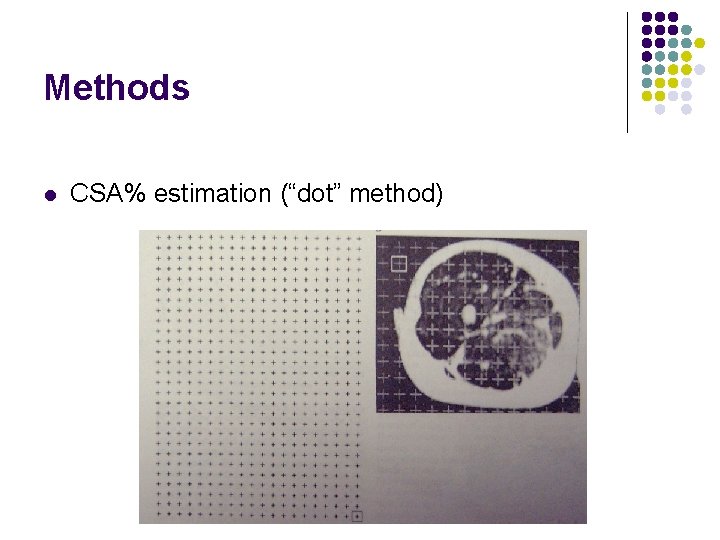
Methods l CSA% estimation (“dot” method)
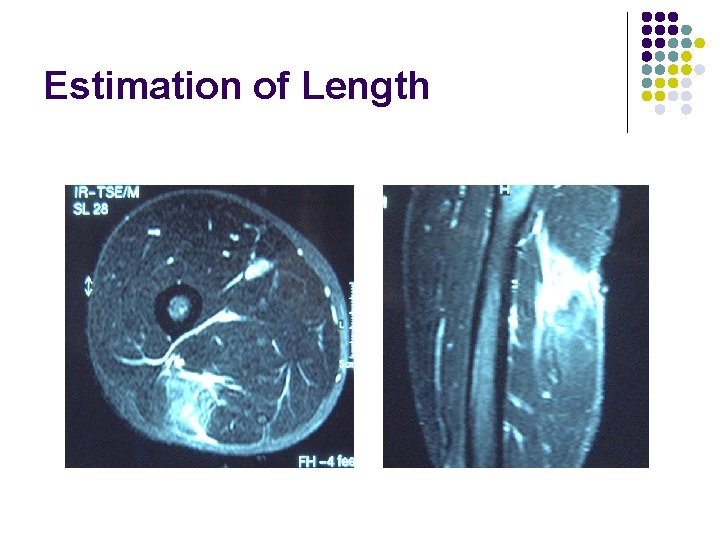
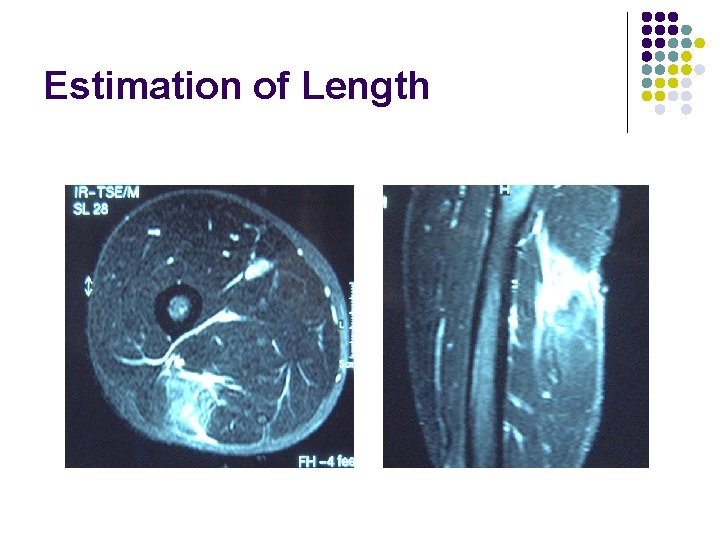
Estimation of Length

Methods MRI diagnosis: miscellaneous features… • T 2 hyper intensity • muscle fibre disruption • Perifascial fluid • Scarring/fibrosis
Methods What if more than one muscle injured? (i. e. double injury etc. ) 1. Primary muscle injured= greatest CSA% 2. Secondary muscle injury= smaller CSA%

Methods (rehabilitation phase) l No universally accepted rehabilitation regimen exists for muscle strain injuries

Methods (rehabilitation phase) Rehabilitation was standardised Phase 1 : Acute management l RICE/crutches first 48 hours l Intensive Physiotherapy • • • soft tissue therapy flexibility strengthening
Methods (rehabilitation phase) Phase 2: Remodeling phase l l Eligible to start running program when, l Full pain free ROM l Complete 3 x 10 repetitions of single leg hops pain free 4 Stage running/kicking program (sport specific to ARF) was designed at beginning of study
Methods (rehabilitation phase) 4 stage running/kicking program l Run alternate days Physiotherapist/Sports Scientist supervision Combined with intensive physiotherapy l 5 minute jog warm up/cool down l Stage 1 : jog 10 mins x 2 l Stage 2 : 80 m intervals ( 40 -60 %) 3 x 5 repetitions l Stage 3: 80 m intervals (90 -100%) 3 x 5 repetitions (staged kicking program commenced) l Stage 4: 80 m intervals (sport specific drills at 90 -100%) 3 x 5 repetitions l Integrate into team training l l
Methods (rehabilitation phase) 4 stage running/kicking programs • Some advanced rapidly • Others delayed by symptoms of high grade posterior thigh pain, weakness and dysfunction Decision to return to Full Training : Collaborative

Rehabilitation interval (RI) RI= time from the injury to the return to full training (measured in days)
2. Results and Discussion
Results of acute MRI images l l 31 acute clinical HAMSTRING strains were imaged Authors were not blinded to these MRI’s
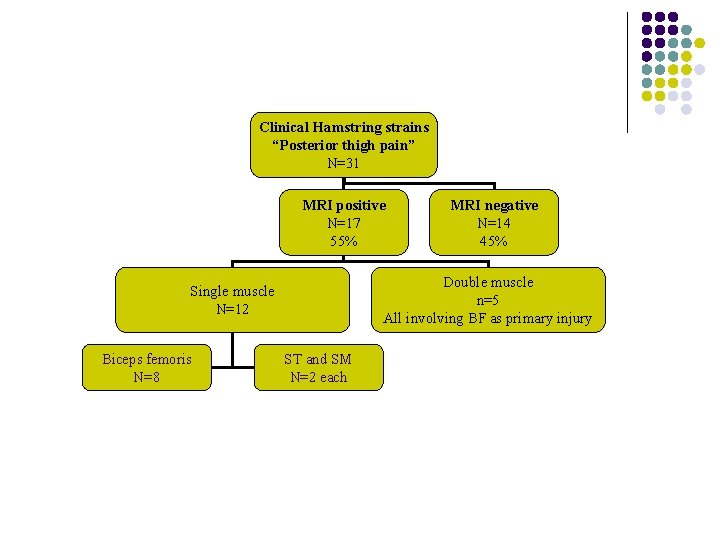
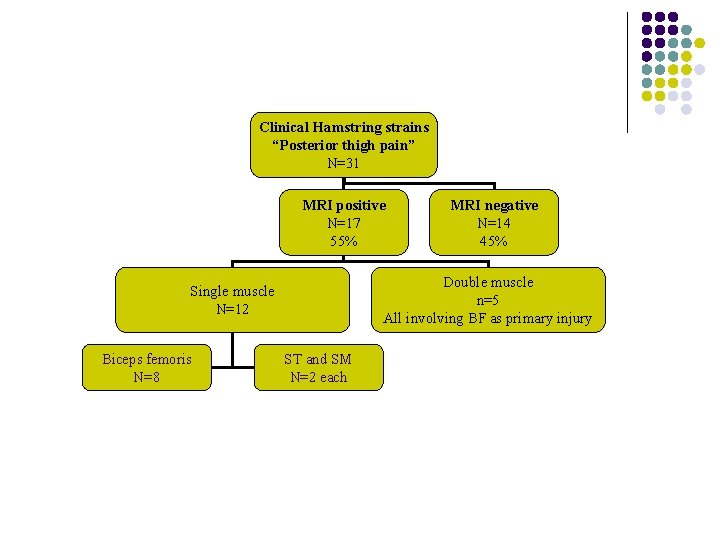
Clinical Hamstring strains “Posterior thigh pain” N=31 MRI positive N=17 55% Double muscle n=5 All involving BF as primary injury Single muscle N=12 Biceps femoris N=8 MRI negative N=14 45% ST and SM N=2 each
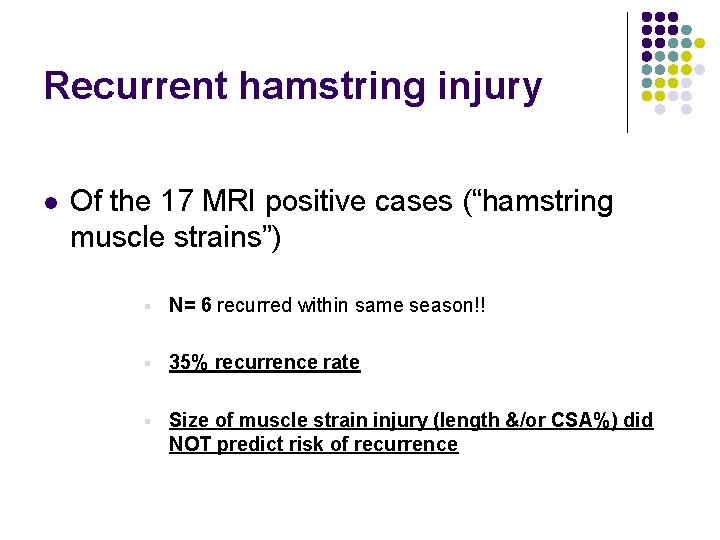
Recurrent hamstring injury l Of the 17 MRI positive cases (“hamstring muscle strains”) § N= 6 recurred within same season!! § 35% recurrence rate § Size of muscle strain injury (length &/or CSA%) did NOT predict risk of recurrence

Recurrent hamstring injury l Of the 14 MRI negative cases § None recurred within same season!! § 0 % recurrence rate
Statistical analysis Statistician analyzed data § t-tests independent samples (dependent vs. independent variables) § Two-way analysis of variance
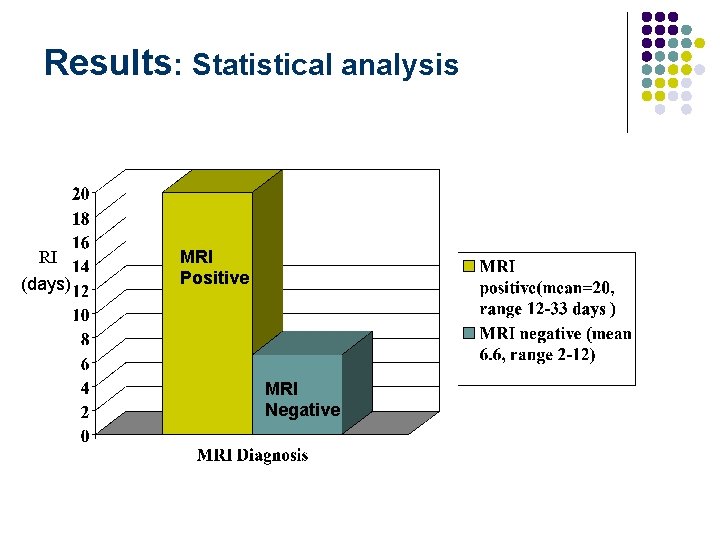
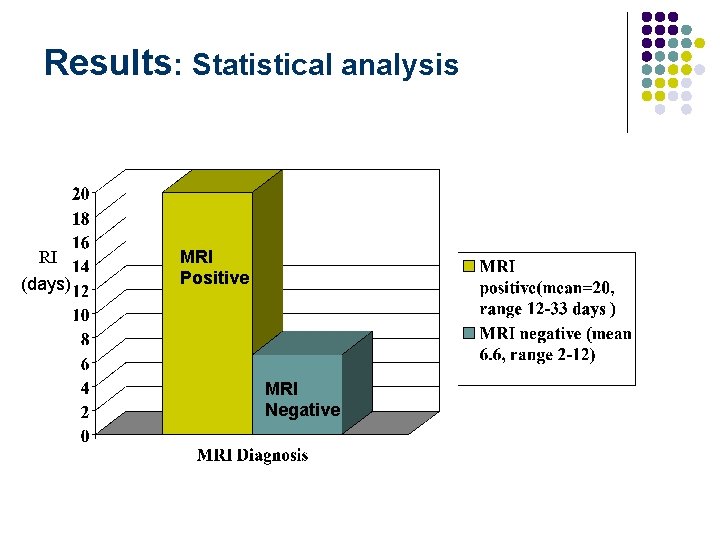
Results: Statistical analysis RI (days) MRI Positive MRI Negative

MRI Positive l n=17 l Mean RI=20. 2 days l significantly longer RI (p=0. 001)
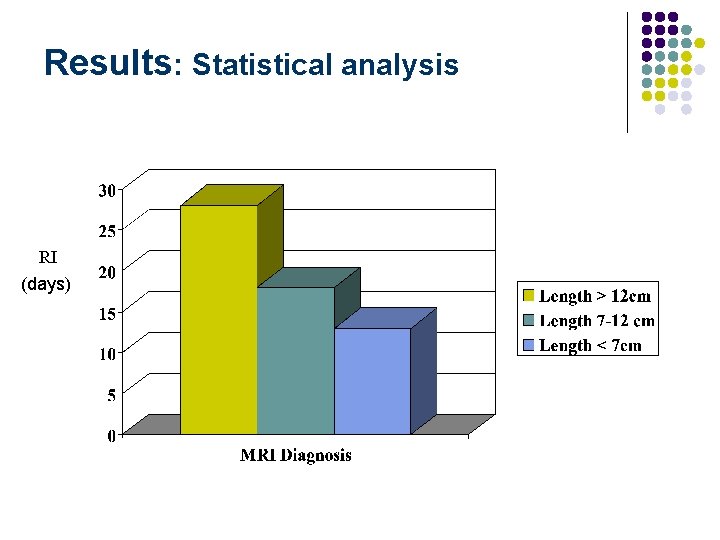
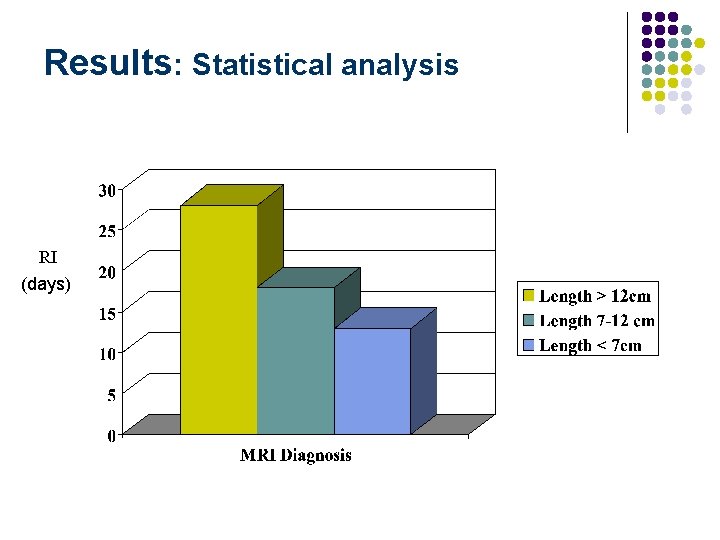
Results: Statistical analysis RI (days)

MRI & Prognosis l Length of intra-muscular signal correlates best with RI r=0. 84, p<0. 001 l CSA% & RI r=0. 78 l Size really does matter
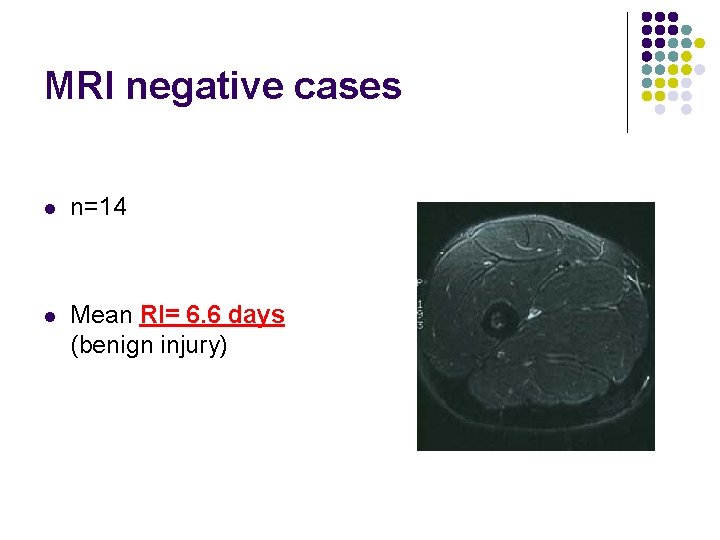
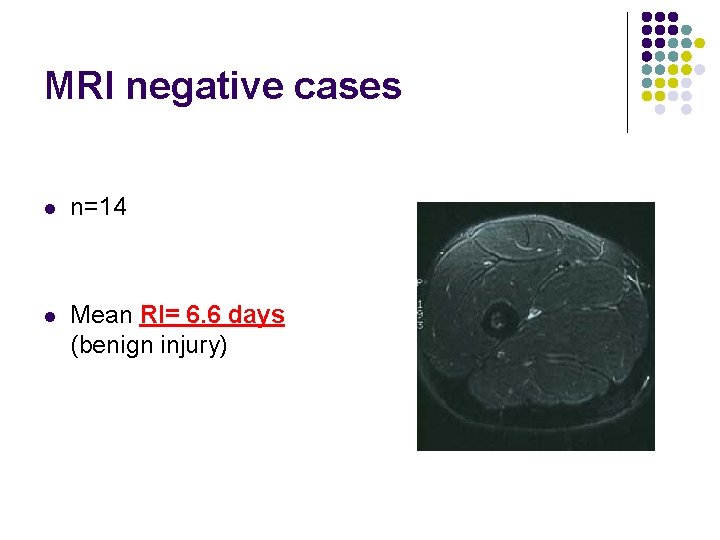
MRI negative cases l n=14 l Mean RI= 6. 6 days (benign injury)
MRI negative cases Hypotheses l MRI done too early l Strain injury too small to resolve l Other causes of “Posterior thigh pain”
Other causes of posterior thigh pain l Somatic Referred pain l l Lumbosacral spine Pelvis
Other causes of posterior thigh pain l Neuromeningeal tethering l l Nerve root ( “radiculopathy”) Piriformis syndrome Hamstring syndrome Within HS muscles

Other causes of posterior thigh pain l Intrinsic Muscle causes l l Tender points Trigger points Adhesions/fibrosis/scarr ing Tendinopathy/bursitis

Other causes of posterior thigh pain l “Not to be missed” l l l l Avulsion Fractures Complete rupture proximal HS Stress Fractures Compartment syndromes Tumours (benign and malignant) Infections (bone/soft tissue) Rheumatologic

CONCLUSIONS
Conclusions MRI defines muscle strain injury objectively: “probe beneath the surface of the skin”
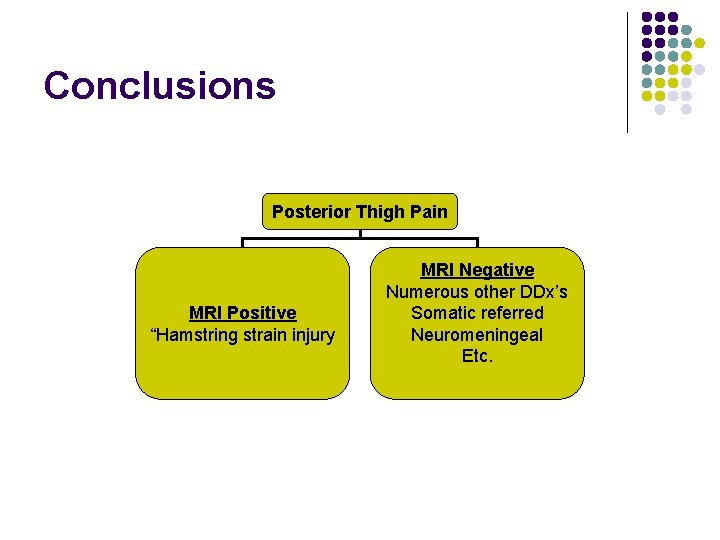
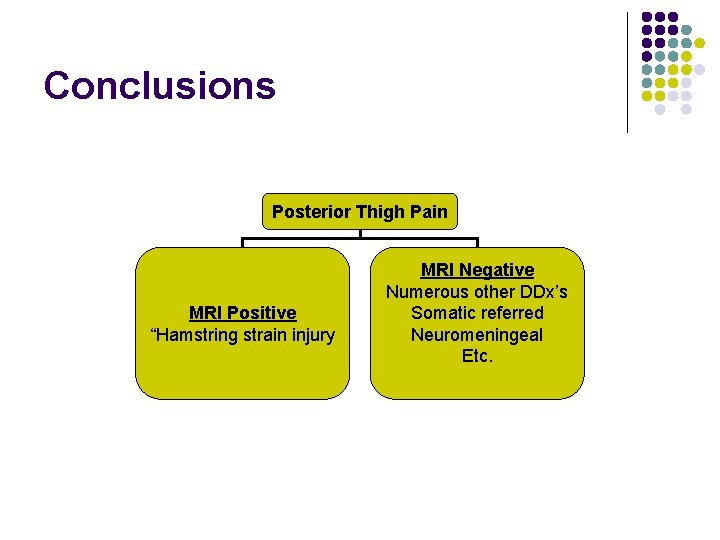
Conclusions Posterior Thigh Pain MRI Positive “Hamstring strain injury MRI Negative Numerous other DDx’s Somatic referred Neuromeningeal Etc.

Conclusions All 17 MRI positive cases of muscle strain injury occurred about known muscle-tendon junctions (This concurs with basic science studies)

Conclusions The Biceps femoris was the most commonly injured muscle (8 single, 5 “double” injuries)
Conclusions Tenderness over the posterior thigh does not always = muscle strain injury Concept of “MRI NEGATIVE” diagnosis

Conclusions RI (days) MRI Positive MRI Negative

Conclusions l Size ( LENGTH and CSA%) of muscle strain injury is also predictive of RI

Conclusions Indications for MRI Acute MRI for elite athletes Soccer World Cup 2002

e. g. Posterior thigh pain 7 days before Final Can he play? ? YES : if MRI negative NO: if MRI positive
Conclusions Indications for MRI If no MRI available? Suspect MRI positive if troubled by high grade posterior thigh pain in rehabilitation

Thank-you Questions?
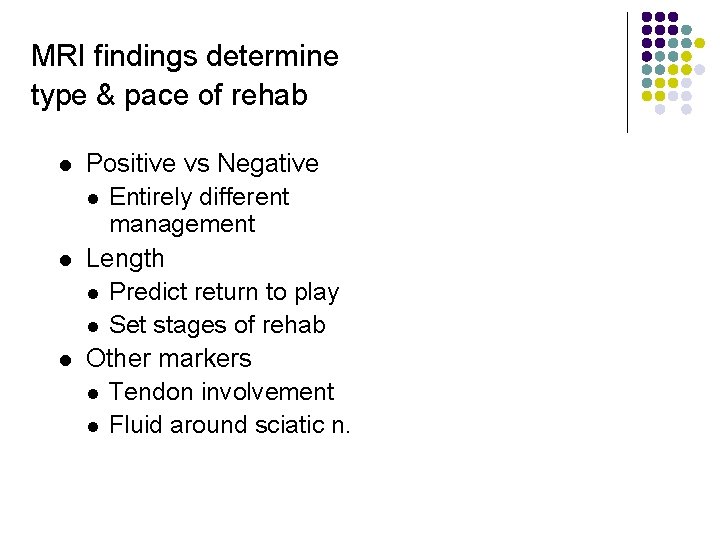
MRI findings determine type & pace of rehab l l l Positive vs Negative l Entirely different management Length l Predict return to play l Set stages of rehab Other markers l Tendon involvement l Fluid around sciatic n.

REHABILITATION l l Promote healing l Regeneration > Scarring Restore flexibility of injured region l Prevent shortening l l Common finding in retrospective studies Restore strength of hamstring group l Retraining of hip extension & knee flexion l Prevent shortening of angle of peak torque l More prone to damage with eccentric ex l Due to injury or rehab or inherent Running Re-Training Correct contributing factors if possible Brockett et al 2002
RUNNING RETRAINING l l l Formalised by G. Reid – Hockey background Allows return to competitive sport prior to complete healing of injury site Involves: l Running early – when stair walking pain-free l Running is progressed in stages of speed increments l Jog then Fartlek l Running 90 m intervals EZ l l 5 stages till sprinting Controlled sport specific drills prior to returning to training
Possible mechanism l l l Retraining of muscles responsible for the hip extensor & knee flexor torque during running BF-S & L, ST, SM, Glut, AM, Gastroc Change in relative contribution of each muscle Any change in recruitment yet to be determined Sufficient slack in the system l Inhibit the injured muscle l Facilitate remaining muscles

Observations 1. l l 2. l l l Large single hamstring strains exhibit obvious inhibition Lower resting tone on palpation Poor recruitment during isometric contraction Double hamstring muscle strains 14 BF & ST injuries – 9 recurred within rehab or within 12/12 64% recurrence rate – double the norm May reflect an inability of the system to adequately compensate for the injured muscle Role of dual channel biofeedback Early or later stages of rehab Similar effect as suggested by Sherry & Best

Sherry & Best 2004 l l l RCT of 2 programmes 24 grade 1 -2 hamstring injuries Stretch & Strength (11) l l Stat bike, static & C-R stretches, isometric to conc to ecc strength X’s with cuff wts, T/B & BW Progressive Agility & Trunk Stabilisation (13) l l l JOSPT Sidestepping, grapevines, fwd & bwd steps while sidestepping, balance exercises, jogging on spot, trunk stabilisation X’s Progressive intensity Both programmes involved sport practice when pain- free

Sherry & Best 2004 l l STST - mean RTS 37. 4 days PATS - mean RTS 22. 2 days JOSPT (10 -95, sd 27. 6) (10 -35, sd 8. 3) p=0. 2455 l Recurrence rates l l l STST PATS 54. 5% at 2 wks, 70% at 1 yr 0% at 2 wks, 7. 7% at 1 yr p=0. 003 Allows regeneration > scar Better prevention of atrophy Better trunk stability, co-ordination or motor control

Contributing Factors l Strength L/R balance, H/Q balance Burkett 1970, Yamamoto 1993, Orchard et al 1997, Cameron et al 2003 l Inadequate strength for function required § § l Eg. Running & bending or jumping Determine mechanism Specific Flexibility l l Bennell et al 2003 Ankle Dorsiflexion < 10 cm p=0. 036 Hip Flexors – MTT > 0 degs p=0. 051
Contributing Factors l Other injuries and Gluteal Function l l l Previous calf injury Orchard 2001 Previous knee injury or osteitis pubis Verrall et al 2001 Altered biomechanical factors - inherent or due to injury Ankle sprain ↓ glut function Bullock-Saxton et al 1994 Poor lower limb motor control Cameron et al 2003

Summary – Hammy Rehab l Diagnosis l Muscle strain or posterior thigh pain (PTP) l l MRI & clinical testing Extent of strain injury - MRI l Re-training Programme l Pre-disposing factors