GYNECOLOGICAL ONCOLOGY Prof Roman Makarewicz Department of Oncology

- Slides: 76
GYNECOLOGICAL ONCOLOGY Prof. Roman Makarewicz Department of Oncology and Brachytherapy Collegium Medicum in Bydgoszcz
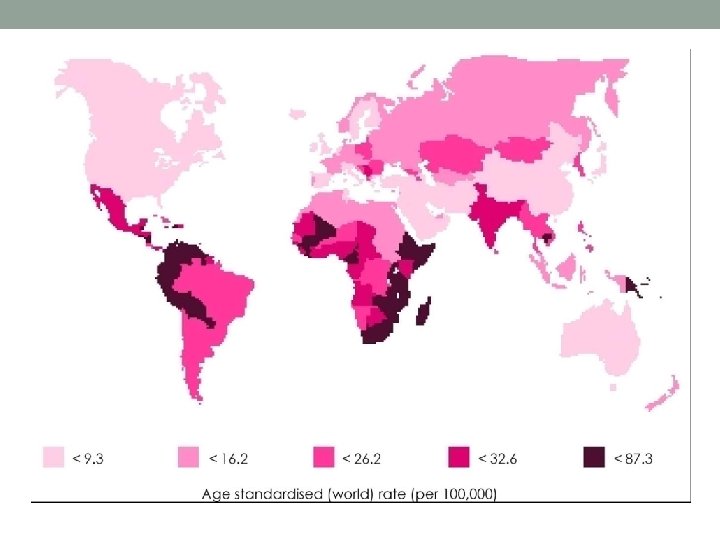
Cervical cancer • Cancer of the cervix is the most common female genital cancer in developing countries every year about 500, 000 women, acquire the disease and 75% are from frame developing countries. • About 300, 000 women also die from the disease annually and of these 75% are from developing countries.
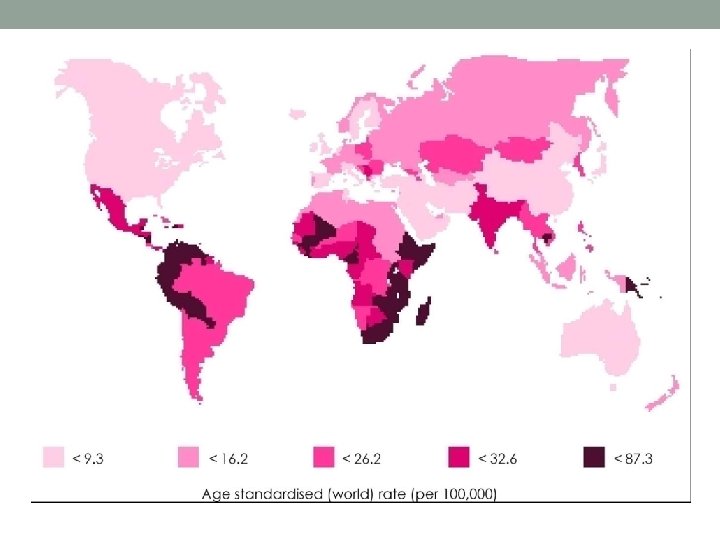
• Finland which has an advanced population based screening program has one of the lowest rates in the world.
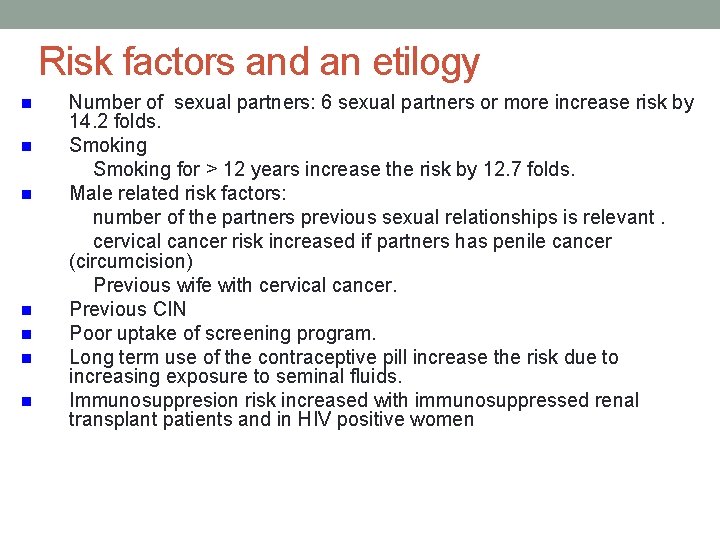
Risk factors and an etilogy n n n n Number of sexual partners: 6 sexual partners or more increase risk by 14. 2 folds. Smoking for > 12 years increase the risk by 12. 7 folds. Male related risk factors: number of the partners previous sexual relationships is relevant. cervical cancer risk increased if partners has penile cancer (circumcision) Previous wife with cervical cancer. Previous CIN Poor uptake of screening program. Long term use of the contraceptive pill increase the risk due to increasing exposure to seminal fluids. Immunosuppresion risk increased with immunosuppressed renal transplant patients and in HIV positive women
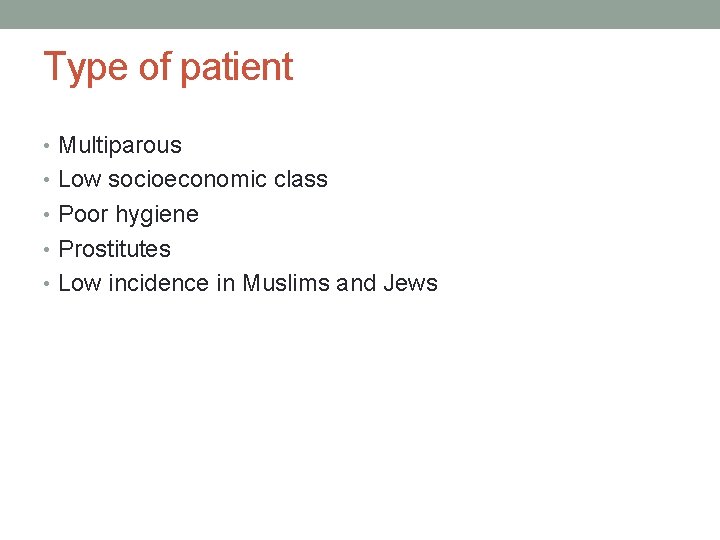
Type of patient • Multiparous • Low socioeconomic class • Poor hygiene • Prostitutes • Low incidence in Muslims and Jews

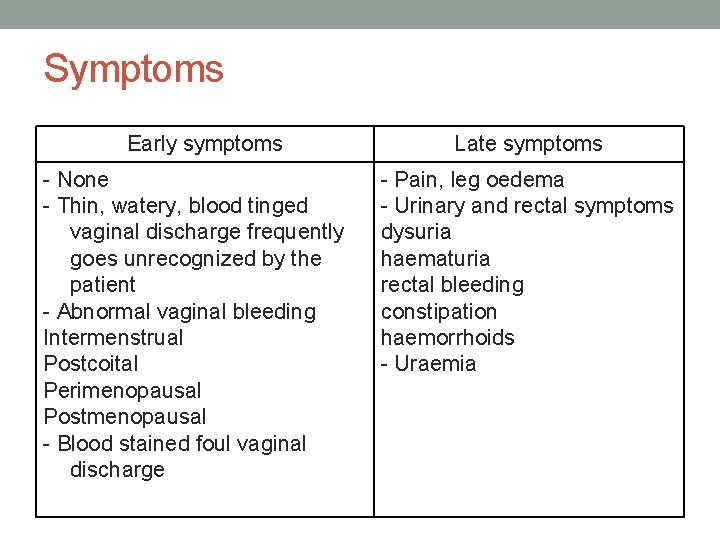
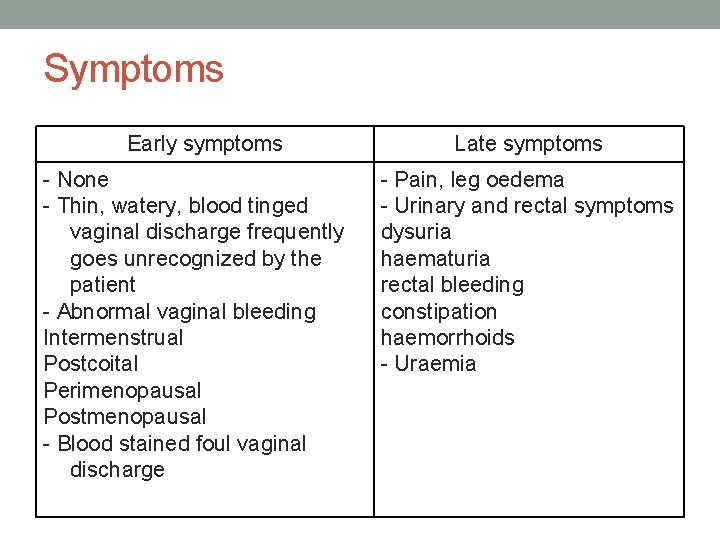
Symptoms Early symptoms - None - Thin, watery, blood tinged vaginal discharge frequently goes unrecognized by the patient - Abnormal vaginal bleeding Intermenstrual Postcoital Perimenopausal Postmenopausal - Blood stained foul vaginal discharge Late symptoms - Pain, leg oedema - Urinary and rectal symptoms dysuria haematuria rectal bleeding constipation haemorrhoids - Uraemia
Pathology type • • Squamous cell carcinoma-90% Adenocarcinoma-10%
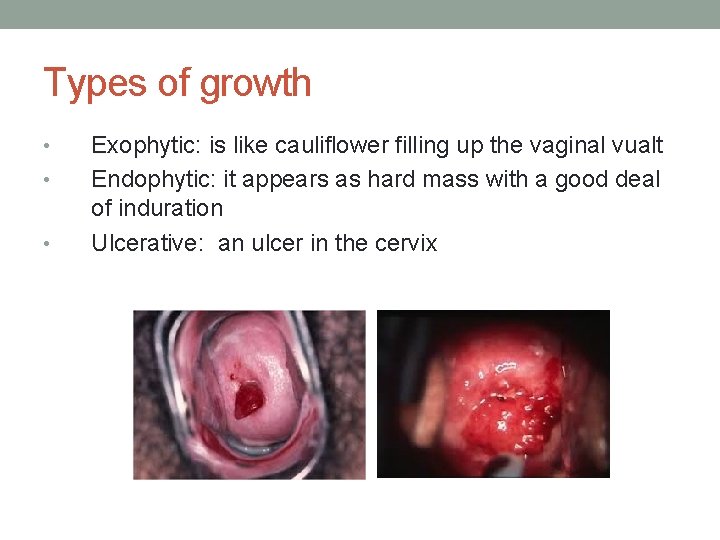
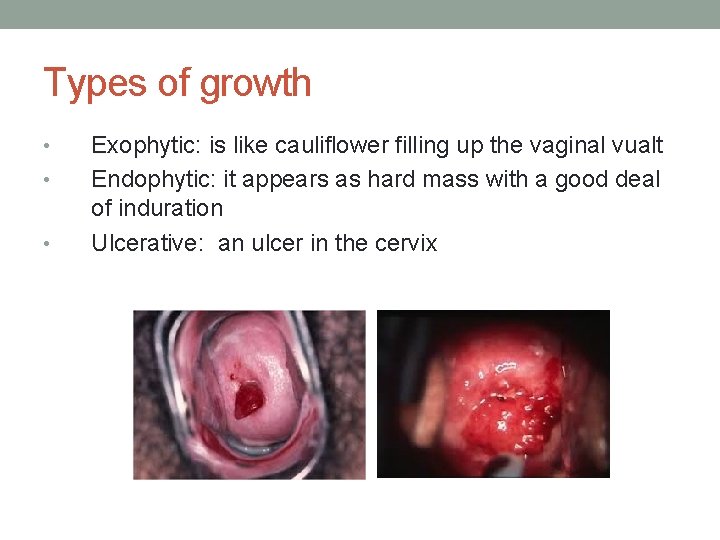
Types of growth • • • Exophytic: is like cauliflower filling up the vaginal vualt Endophytic: it appears as hard mass with a good deal of induration Ulcerative: an ulcer in the cervix
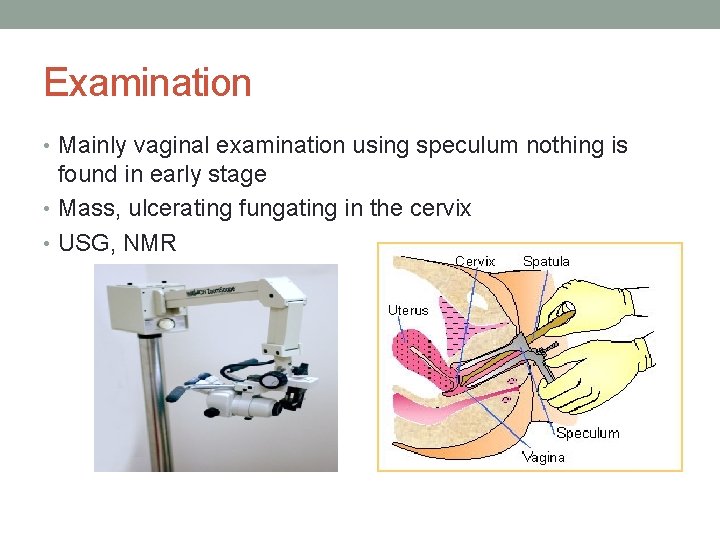
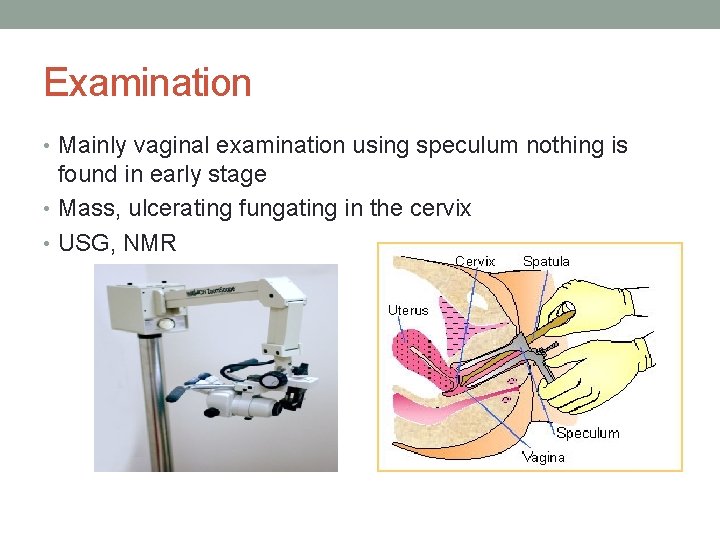
Examination • Mainly vaginal examination using speculum nothing is found in early stage • Mass, ulcerating fungating in the cervix • USG, NMR
Pretreatment evaluation • Review history • o o o General examination: Anaemia Lymphadenopathy-Supraclavicular LN Renal area Liver or any palpable mass Oedema • o o o Laboratory tests: Chest X- ray MRI Ultrasound
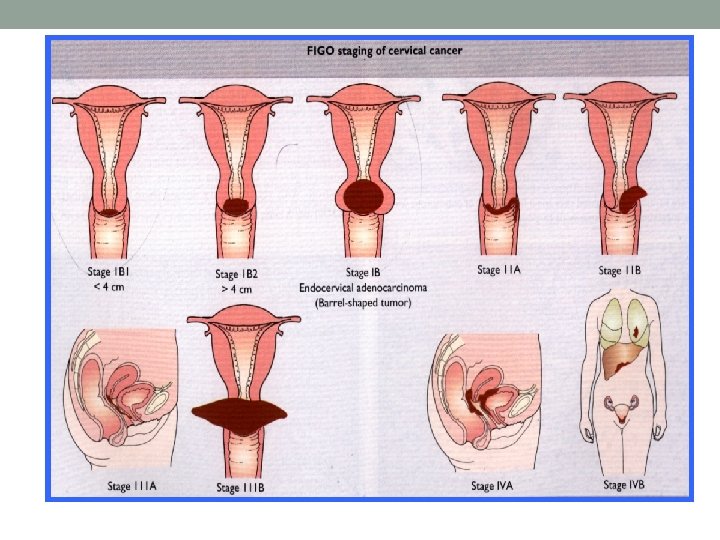
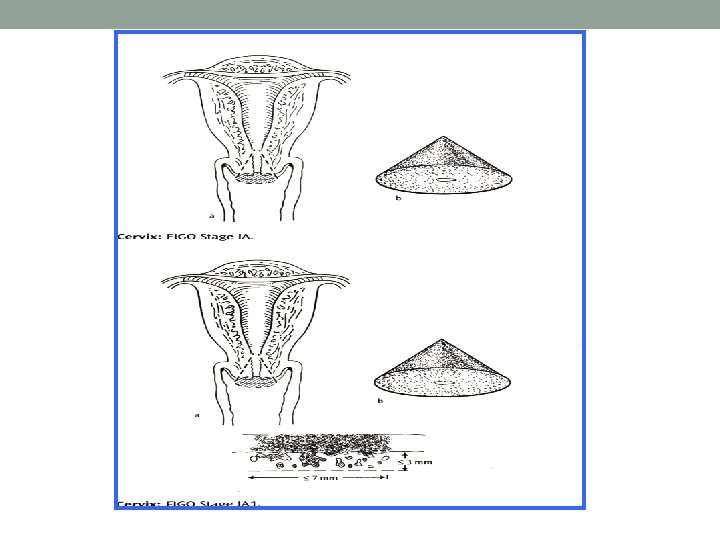
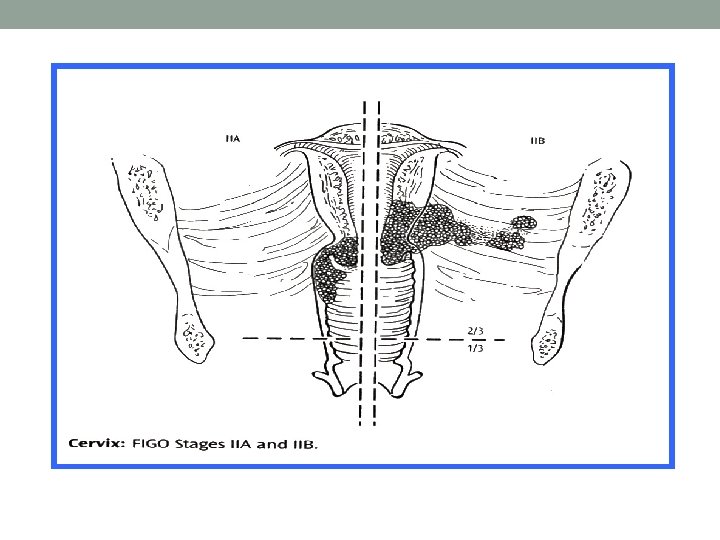
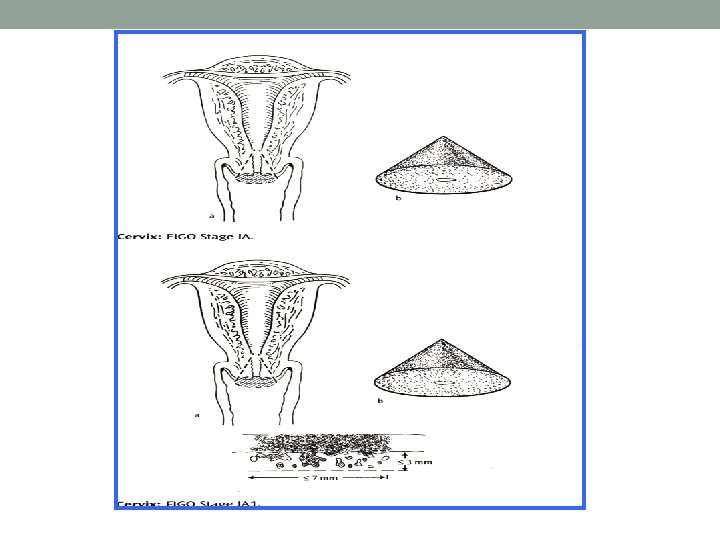
Staging Best to follow FIGO system • Examination under anaesthesia • Bimanual palpation • Cervical biopsy, uterine biopsy • MRI
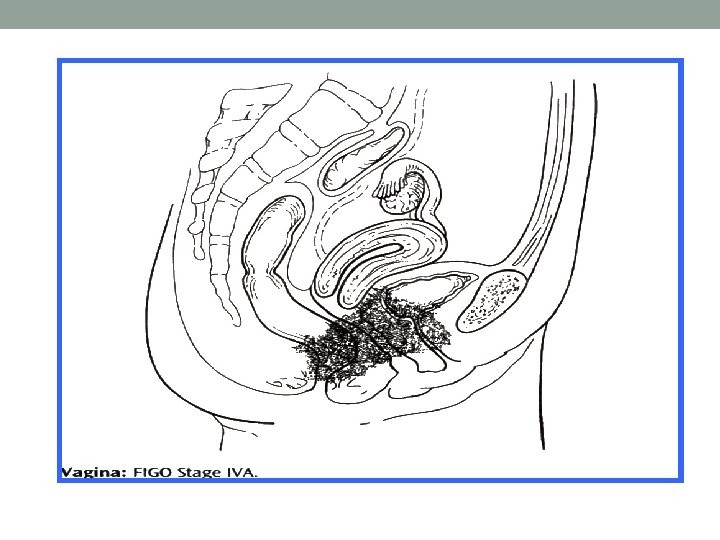
Stages of cancer cervix • Once cancer cervix is found (diagnosed), more tests will be done to find out if the cancer cells have spread to other parts of the body. This testing is called staging • TO PLAN TREATMENT, A DOCTOR NEEDS TO KNOW THE STAGE OF THE DISEASE
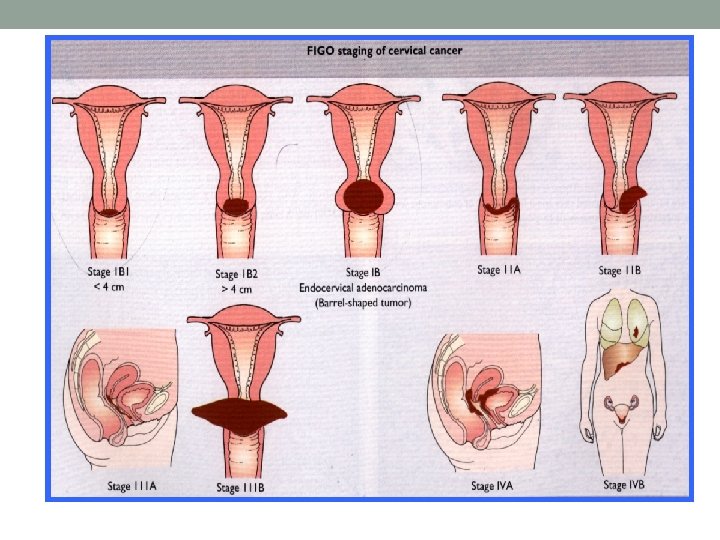
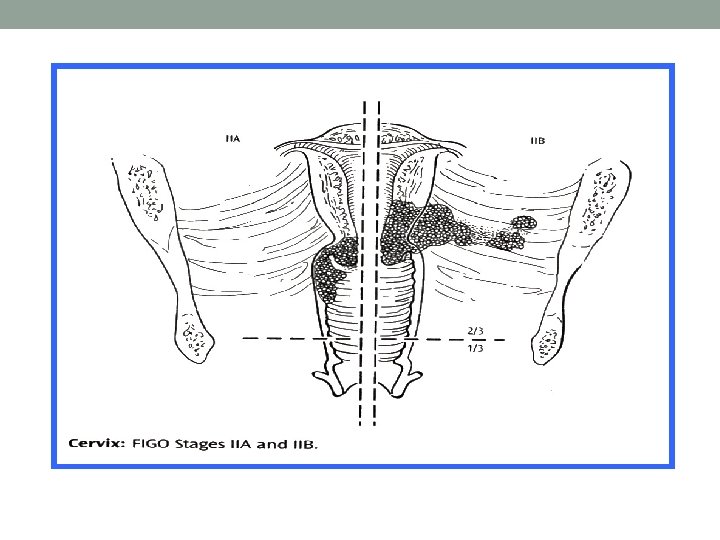
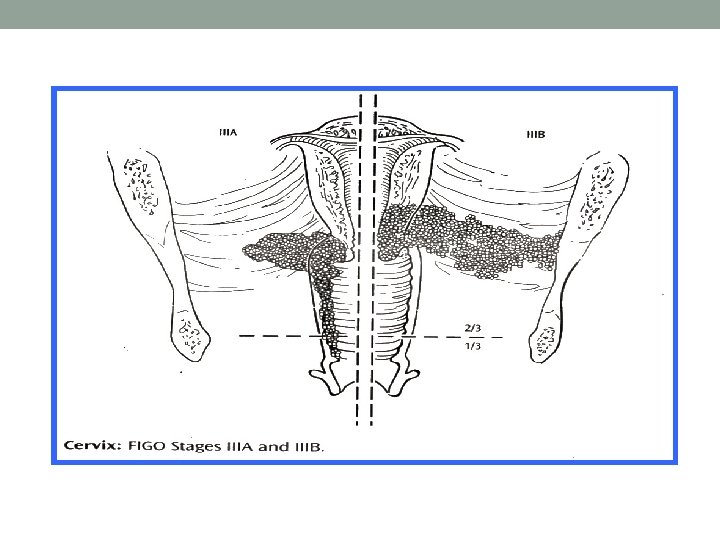
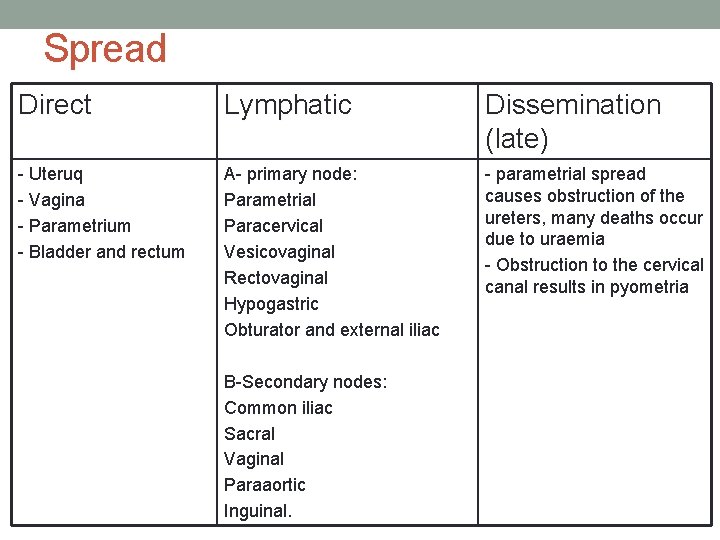
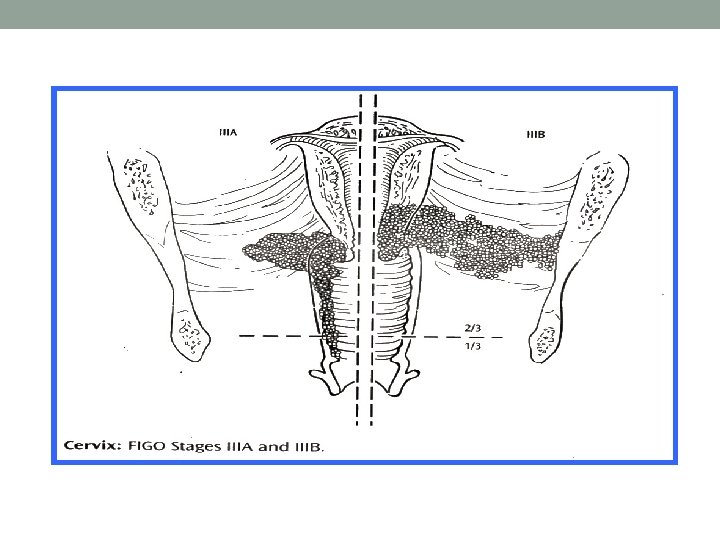
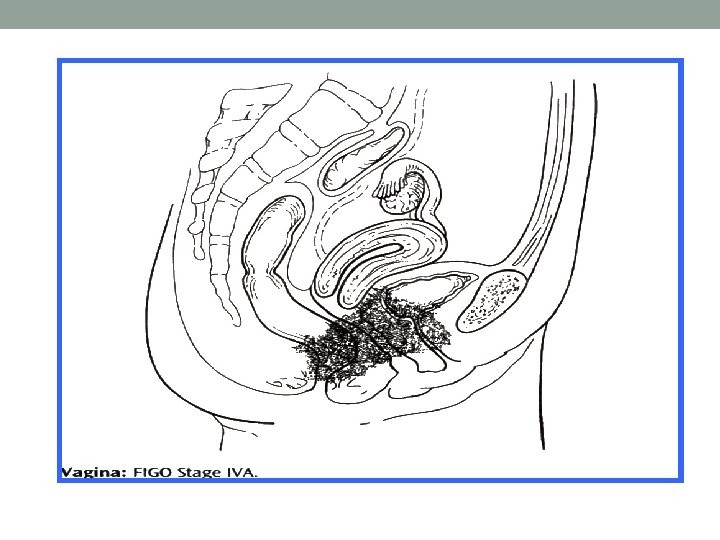
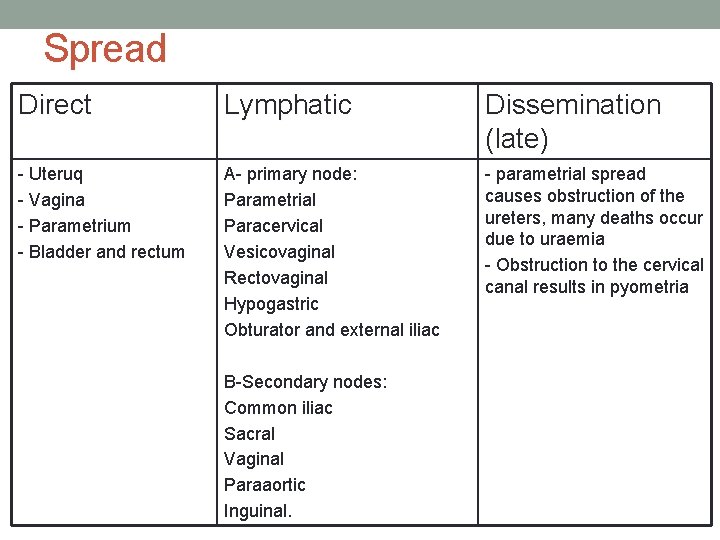
Spread Direct Lymphatic Dissemination (late) - Uteruq - Vagina - Parametrium - Bladder and rectum A- primary node: Parametrial Paracervical Vesicovaginal Rectovaginal Hypogastric Obturator and external iliac - parametrial spread causes obstruction of the ureters, many deaths occur due to uraemia - Obstruction to the cervical canal results in pyometria B-Secondary nodes: Common iliac Sacral Vaginal Paraaortic Inguinal.
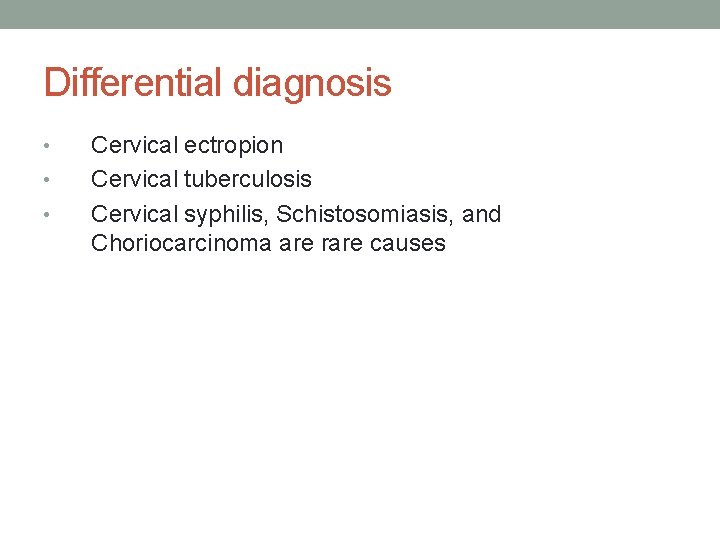
Differential diagnosis • • • Cervical ectropion Cervical tuberculosis Cervical syphilis, Schistosomiasis, and Choriocarcinoma are rare causes
Treatment • Surgical • Radiotherapy & Surgery • Radiotherapy and Chemotherapy followed by Surgery • Palliative treatment
The choice of treatment will depend on • Fitness of the patients • Age of the patients • Stage of disease • Type of lesion • Experience and the resources available
Surgical procedure • The classic surgical procedure is the Wertheim’s hystrectomy for stage Ib, IIa, and some cases of IIb in young and fat patient
Werthemeim’s hystrectomy • Total abdominal hystrectomy including the parametrium • Pelvic lymphadenectomy • 3 cm vaginal cuff • The original operation conserved the ovaries, since squamous cell carcinoma does not spread directly to the ovaries • Oophorectomy should be performed in cases of adenocarcinoma as there is 5 -10% of ovarian metastases
Surgery offers several advantage • It allows presentation of the ovaries (radiotherapy will destroythem) • There is better chance of preserving sexual function • (vaginal stonosis occur in up 85% of irradiates • Psychological feeling of removing the disease from the body • More accute staging and prognosis
Complications of surgery • • • Haemorrhage: primary or secondary Injury to the bladder, ureters Bladder dysfunction Fistula Lymphocele Shortening of the vagina
INDICATIONS OF P/O XRT FOLLOWING WERTHEIM’S HYSTERECTOMY (STAGE I, IIa): • Positive pelvic lymph nodes • Tumour close to resection margins and/or parametrial extension
Radiotherapy • Stage IIb and III • Radical Radiotherapy • External irradiation (Teletherapy) • Intracavitary radiation (Brachytherapy) • In some cases of stage IIa or b radio and chemotherapy to be given then followed by simple hysterectomy
Prognosis Depends on: • Age of the patient • Fitness of the patient • Stage of the disease • Type of the tumour • Adequacy of treatment
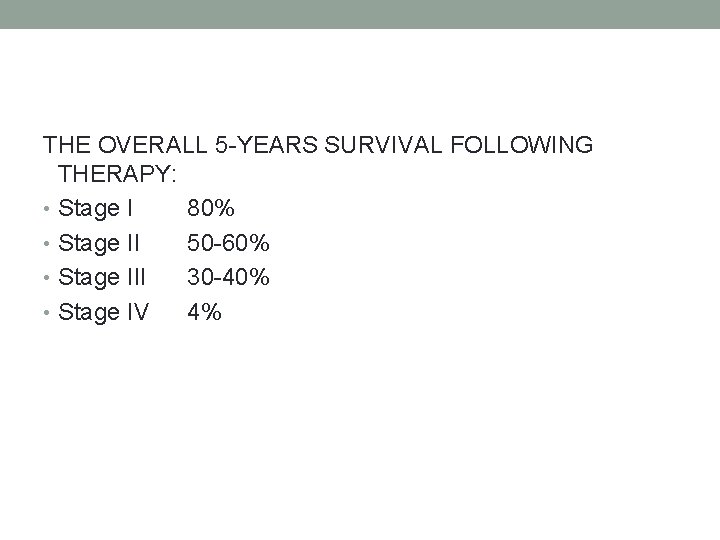
THE OVERALL 5 -YEARS SURVIVAL FOLLOWING THERAPY: • Stage I 80% • Stage II 50 -60% • Stage III 30 -40% • Stage IV 4%
Management of recurrent disease • • 1. Local recurrence: Radiation - if not used Pelvic exenturation 2. Distant disease Chemotherapy
Conclusions • Cancer of the cervix is still quite common, reduction in incidence depends on the quality of the screening program • The etiology appears to be multifactorial the prime oncogenic agent is probably [HPV-16, 18] • Clinical presentation is with intermenstrual, post coital, postmenospausal bleeding or following abnormal cytology • Tumour spreads locally to involve the uterus bladder, vagina, parametrium, ureters, rectum and bone
• Spread also to the internal and external iliac, obdurator and common iliac nodes then to para-aortic nodes • Distant metastasis spread to liver, lung and bone • Microinvasion squamous tumour carry a good prognosis allowing conservative treatment initially if required
• Early invasive squamous cell disease (stage Ib, IIa and in some cases of IIb) may be treated by either a Wertheime’s hysterectomy or radiotherapy as first line treatment • Advanced stage (IIb, III, IV) treated by radio or chemotherapy
• Glandular tumours (adenocarcinomas) are not detectable by screening are associated with skip lesions and require radical surgery
Endometrial cancer • The exact cause is unknown • Estrogen replacement therapy • Tamoxifen • Women who have been treated with tamoxifen, a drug used to prevent and treat breast cancer may have a slighty increased risk of developing endometrial cancer
Diagnosis • Hysteroscope/endoscope tube with vision is inserted into uterus through the cervix • Allows the doctor to view the inside of the uterus and collect endometrial tissue samples
Signs and symptoms • Early symptoms • Vaginal bleeding or spotting in postmenopausal women • All bleeding without conection with periods between normal periods: extremely long, heavy or frequent episods of bleeding after sexual intercourses • Vaginal discharge • Late symptoms • Weight loss • Anemia • Lower abdominal pain
Type of endometrial cancer • Type 1 • Caused by excess estrogen • Type 2 • Etiology unknown, but it doesn’t seem to be caused by too much estrogen
Type 1 • Not very aggressive • Slow to spread to other tissues • Grades 1 or 2 • Occur most commonly in pre- and peri- menopausal women • History of estrogen exposure and endometrial hyperplasia • Carry a good prognosis
Type 2 • Occur in older, post-menopausal women • More common in African-Americans • More likely to grow and spread outside of the uterus • Carry a poorer prognosis
Endometrial adenocarcioma • 80% of uterine neoplasms • It arises from the glands of the endometrium • Essential is grade which says how aggressive cancer is • 40% Grade 1, 20% Grade 2, 40% Grade 3 • Example of type II cancer • The uterine papillary serous cancer (5% of cancers) • The uterine clear cell cancer (2% of cancers) • Both are aggressive and have high recurrence rate
Treatment for endometrial cancer • Depends on: • The stage of the disease • Overall health of the patient • Primary treatment is the surgery • Radiation therapy, hormonotherapy and chemotherapy may be used as an adjuvant treatment or in patients with metastatic or recurrent disease • Hysterectomy • Simple • Total including the cervix • Total with salpingo-ophorectomy with nodal sampling • With pelvic lymphadectomy • The procedures are done using a low transverse incision or a vertical incision
Chemotherapy • Treatment that uses drugs to stop the growth of cancer cells, either by killing the cells or by stopping the cells from dividing • Treatment usually involves a combination of two or three drugs giving intravenously • When chemotherapy is given • Adjuvant tretment once every 21 days (6 -8 cycles) • Metastatic disease (to progression) • When drugs are used to treat endometrial cancer • Carboplatin • Cisplatin • Doxorubcin • Paclitaxel • Cyclophosphamide
Radiation therapy • The purpose is: • To get rid of any tumor cells that may be left in the body after surgery • Candidates: • Depends on: • Grade 2 and 3 • How deeply is invasion • Pathologic diagnosis • Methods: • Vaginal brachytherapy • External beam RT
Hormonotherapy • Progestins as the main hormone treatment for endometrial cancer • Medroxyprogesterone acelate (Provere) • Megestrol acelate (Megace)
• There is no effective screening programme • Occasionally cervical smears contain endometrial cancer cells • Ultrasound thickness more than 5 mm in postmenopausal patients indicates a need for endometrial staging and one attention
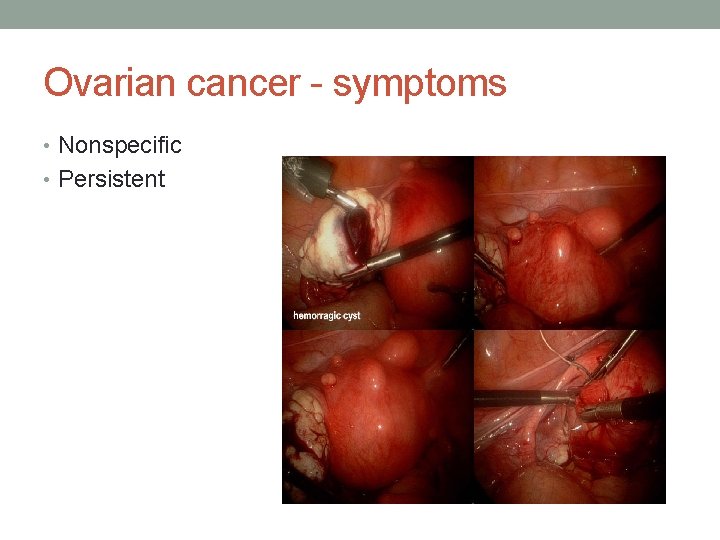
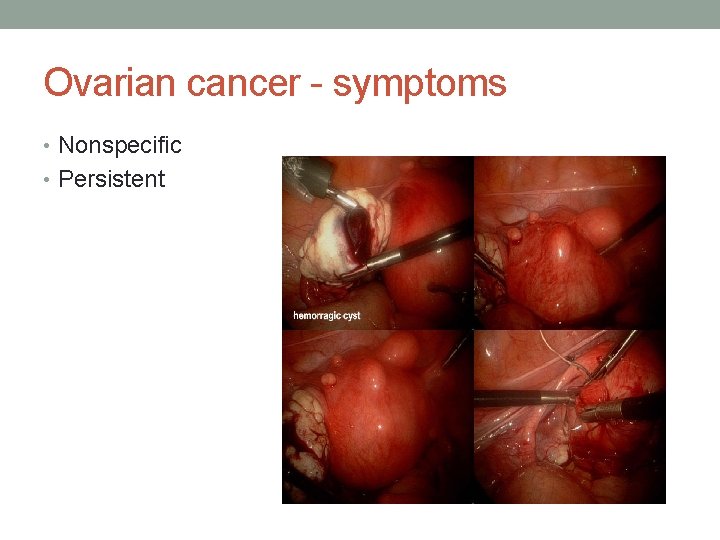
Ovarian cancer - symptoms • Nonspecific • Persistent
Symptoms • Bloating • Pelvic or abdominal pain • Difficulty eating or feeling full quickly • Urgency or urinary frequency • Most common is abdominal enlargement
Symptoms Other symptoms commonly reported • Fatigue • Indigestion • Back pain • Pain with intercourse • Constipation • Menstrual irregularities
Risk Factors • Genetic predisposition • Family history is strongest risk • Breast-ovarian cancer syndrome • Lynch II syndrome • Cancer of colon, breast, endometrium and HNPCC Age Annual incidence in women age 50 -75 is 50 per 100, 000, twice the rate in younger women
Risk Factors • Decrease risk: • Pregnancy • Breast feeding • Tubal ligation • Hysterectomy • Increase risk: • Infertility • Endometriosis • Peri or postmenopausal history of medications
Screening Tests • There is no standardized test to detect ovarian cancer at an early stage • CA-125: most widely used screening method § Specificity is limited § False elevations in: endometriosis, fibroids, cirrhosis w/- ascites, PID, cancers of breast, lung, pancreas, pleural or peritoneal fluid due to any cancer
Staging The Federation Internationale de Gynecologie et d'Obstetrique (FIGO) and the American Joint Committee on Cancer (AJCC) have designated staging.
Stage I ovarian cancer • limited to the ovaries. • Stage IA: tumour limited to 1 ovary, the capsule is intact, no tumour on ovarian surface and no malignant cells in ascites or peritoneal washings. • Stage IB: tumour limited to both ovaries, capsules intact, no tumour on ovarian surface and no malignant cells in ascites or peritoneal washings. • Stage IC: tumour is limited to 1 or both ovaries with any of the following: capsule ruptured, tumour on ovarian surface, malignant cells in ascites or peritoneal washings.
Stage II ovarian cancer • tumors involving 1 or both ovaries with pelvic extension and/or implants. • Stage IIA: extension and/or implants on the uterus and/or fallopian tubes. No malignant cells in ascites or peritoneal washings. • Stage IIB: extension to and/or implants on other pelvic tissues. No malignant cells in ascites or peritoneal washings. • Stage IIC: Pelvic extension and/or implants (stage IIA or stage IIB) with malignant cells in ascites or peritoneal washings.
Stage III ovarian cancer • tumours involving 1 or both ovaries with microscopically confirmed peritoneal implants outside the pelvis. Superficial liver metastasis equals stage III. • • Stage IIIA: microscopic peritoneal metastasis beyond pelvis (no macroscopic tumour). • Stage IIIB: macroscopic peritoneal metastasis beyond pelvis less than 2 cm in greatest dimension. • Stage IIIC: peritoneal metastasis beyond pelvis greater than 2 cm in greatest dimension and/or regional lymph node metastasis.
Stage IV ovarian cancer tumours involving 1 or both ovaries with distant metastasis. Parenchymal liver metastasis equals stage IV.
Treatment Options • The treatment of ovarian cancers based on the stage of the disease which is a reflection of the extent or spread of the cancer to other parts of the body. • It also depends on histologic cell type, and the patient's age and overall condition. • There are basically three forms of treatment of ovarian cancer: • surgery • Chemotherapy • radiation treatment,
GENERAL GUIDELINES: • Standard treatment is surgery (staging and optimal debulking) followed by adjuvant chemotherapy in most cases. Even if optimal surgery is not possible, removing as much tumor as possible will provide significant palliation of symptoms. • Borderline lesions may be treated with conservative surgery
GENERAL GUIDELINES: • Germ cell tumors are treated with surgery and multi-agent chemotherapy in most cases • Advanced epithelial ovarian cancer is very sensitive to chemotherapy with responses in the range of 70 -80% to first-line chemotherapy. The majority, however, relapse and ultimately die of chemotherapy-resistant disease. Second-line chemotherapy to date is disappointing in all forms of epithelial ovarian cancer with virtually no chance of successful second-line treatment following failure of initial regime.
Stage I • Generally a total abdominal hysterectomy, removal of both ovaries and fallopian tubes, omentectomy, biopsy of lymph nodes and other tissues in the pelvis and abdomen, is done. Young women whose disease is confined to one ovary are often treated by a unilateral salpingo-oophorectomy without a hysterectomy and removal of the opposite ovary being performed • Depending on the pathologist's interpretation of the tissue removed, there may be no further treatment if the cancer is low grade, or if the tumor is high grade the patient may receive combination chemotherapy.
Stage II • Treatment is almost always hysterectomy and bilateral salpingo-oophorectomy as well as debulking of as much of the tumor as possible and sampling of lymph nodes and other tissues in the pelvis and abdomen that are suspected of harboring cancer. After the surgical procedure, treatment may be one of the following: 1) combination chemotherapy with or without radiation therapy or 2) combination chemotherapy.
Stage III • Treatment is the same as for Stage II ovarian cancer. Following the surgical procedure, the patient may either receive combination chemotherapy possibly followed by additional surgery to find and remove any remaining cancer.
Stage IV • CYTOREDUCTIVE SURGERY/DEBULKING: • surgery to remove as much of the tumor as possible. • Most researchers consider residual disease of <1 cm to be optimal debulking surgery. followed by combination chemotherapy
CHEMOTHERAPY • Prolongs remission and survival • Also used for palliative treatment in advanced n recurrent disease • Administered in all cases beyond stage Ia • Earlier single agents were used, nowadays combination therapy is favoured
CHEMOTHERAPY • No chemotherapeutic agent kills all cancer cells in one treatment , Tf treatment needs to be repeated several times • All agents used should be active against that particular tumor • should have different modes of action to avoid drug resistance n should have differenr mechanisms of toxicity.
CHEMOTHERAPY • This allows each of them to be used as nearv to the full dose as possible. • Drugs are given at 3 weeks intervals • Intraperitoneal chemotherapy is also done
• The initial treatment of ovarian cancer is called first-line therapy. • If the cancer continues to grow with first-line therapy or returns after first-line therapy, additional treatment, called second-line therapy, may be administered. • If the tumor continues to grow after second-line therapy, the next therapy is called third-line therapy, and so on.
First-Line Chemotherapy • First-line chemotherapy for ovarian cancer typically consists of two drugs given together. The combination =paclitaxel + platinum drug—either carboplatin or cisplatin. • Select women may benefit from administration of chemotherapy directly into the abdomen—called intraperitoneal therapy—in addition to conventional intravenous administration.
Second-Line Chemotherapy • The choice of drugs for second-line therapy depends largely on which drugs were administered for first-line therapy and how long it has been since the first-line therapy was stopped. • chemotherapy drugs) for the treatment of ovarian cancer that has returned: GEMZAR (gemcitabine HCl for injection) plus another chemotherapy, carboplatin, is indicated , 6 months after their first-line therapy;
SIDE EFFECTS
While chemotherapy drugs kill cancer cells, they also damage some normal cells, causing side effects. These side effects will depend on the type of drugs given, the amount taken, and how long treatment lasts. Temporary side effects might include the following: • nausea and vomiting • loss of appetite • hair loss • hand foot rashes • kidney or nerve damage • mouth sores
• an increased chance of infection (from a shortage of white blood cells) • bleeding or bruising after minor cuts (from a shortage of platelets) • tiredness (from low red blood cell counts)
Ovarian Cancer Follow up • Monitor CA-125 • Physical Exam • Including pelvic exam • CT scan/PET scan as clinically indicated • Consider family history evaluation if not done previously