Guidelines Overview Augmentation Therapies in Major Depressive Disorder
![Guidelines: Monitoring MDD Treatment Response Guidelines APA[1] Recommendations on When and How to Use Guidelines: Monitoring MDD Treatment Response Guidelines APA[1] Recommendations on When and How to Use](https://slidetodoc.com/presentation_image_h/32170127986459186ef6f6de7437a6fc/image-11.jpg)
![Guidelines: When MDD Treatment Fails Guideline Recommendations APA[1] § Consider change in treatment if Guidelines: When MDD Treatment Fails Guideline Recommendations APA[1] § Consider change in treatment if](https://slidetodoc.com/presentation_image_h/32170127986459186ef6f6de7437a6fc/image-14.jpg)
![Adjunctive Therapies for MDD: Second. Generation Antipsychotic Agents Agent Indication 1 Aripiprazole[1] Adjunctive treatment Adjunctive Therapies for MDD: Second. Generation Antipsychotic Agents Agent Indication 1 Aripiprazole[1] Adjunctive treatment](https://slidetodoc.com/presentation_image_h/32170127986459186ef6f6de7437a6fc/image-18.jpg)
- Slides: 23
Guidelines Overview: Augmentation Therapies in Major Depressive Disorder Roger Mc. Intyre, MD, FRCPC Head, Mood Disorders Psychopharmacology Unit Professor Department of Psychiatry/Pharmacology University of Toronto, Ontario Canada Supported by an educational grant from Otsuka and Lundbeck Alliance
About These Slides § Please feel free to use, update, and share some or all of these slides in your noncommercial presentations to colleagues or patients § When using our slides, please retain the source attribution: Slide credit: clinicaloptions. com § These slides may not be published, posted online, or used in commercial presentations without permission. Please contact permissions@clinicaloptions. com for details
Disclosures The faculty reported the following financial relationships or relationships to products or devices they or their spouse/life partner have with commercial interests related to the content of this CME/CE activity: Roger S. Mc. Intyre, MD, FRCPC, has disclosed that he has received consulting fees from Allergan, Janssen, Lundbeck, Minerva, Neurocrine, Otsuka, Pfizer, Purdue, Shire, Sunovion, and Takeda and funds for research support from Stanley Medical Research Institute.
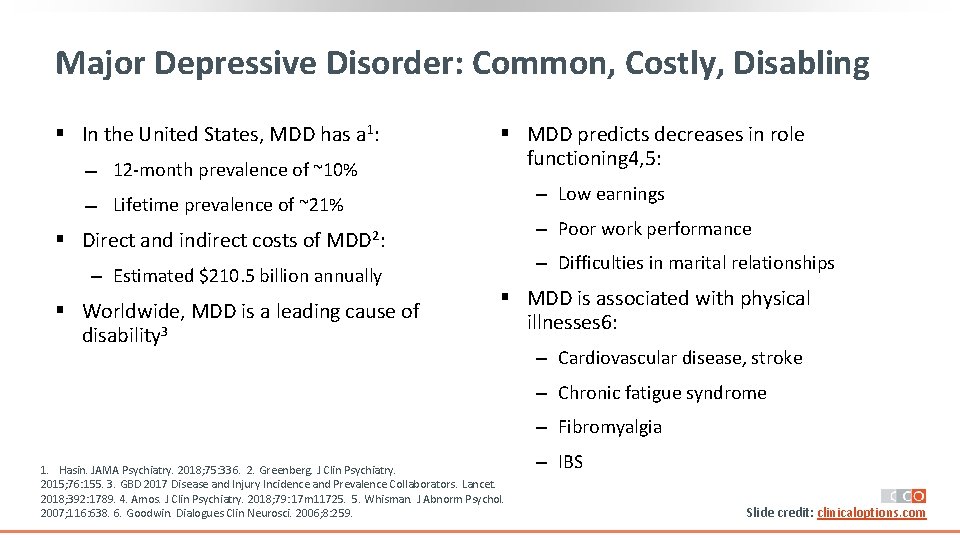
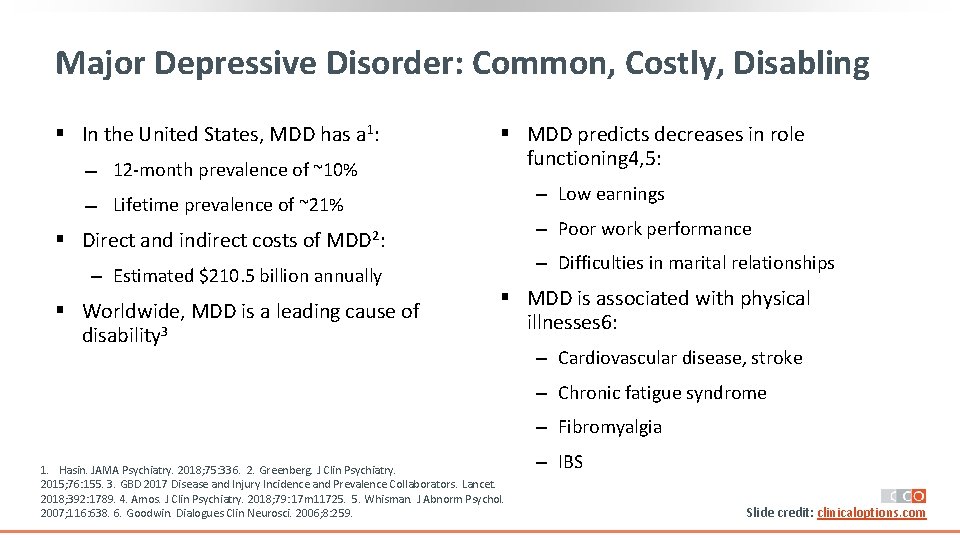
Major Depressive Disorder: Common, Costly, Disabling § In the United States, MDD has a 1: 12‐month prevalence of ~10% Lifetime prevalence of ~21% § MDD predicts decreases in role functioning 4, 5: ‒ Low earnings ‒ Poor work performance § Direct and indirect costs of MDD 2: ‒ Estimated $210. 5 billion annually § Worldwide, MDD is a leading cause of disability 3 ‒ Difficulties in marital relationships § MDD is associated with physical illnesses 6: ‒ Cardiovascular disease, stroke ‒ Chronic fatigue syndrome ‒ Fibromyalgia 1. Hasin. JAMA Psychiatry. 2018; 75: 336. 2. Greenberg. J Clin Psychiatry. 2015; 76: 155. 3. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Lancet. 2018; 392: 1789. 4. Amos. J Clin Psychiatry. 2018; 79: 17 m 11725. 5. Whisman. J Abnorm Psychol. 2007; 116: 638. 6. Goodwin. Dialogues Clin Neurosci. 2006; 8: 259. ‒ IBS Slide credit: clinicaloptions. com
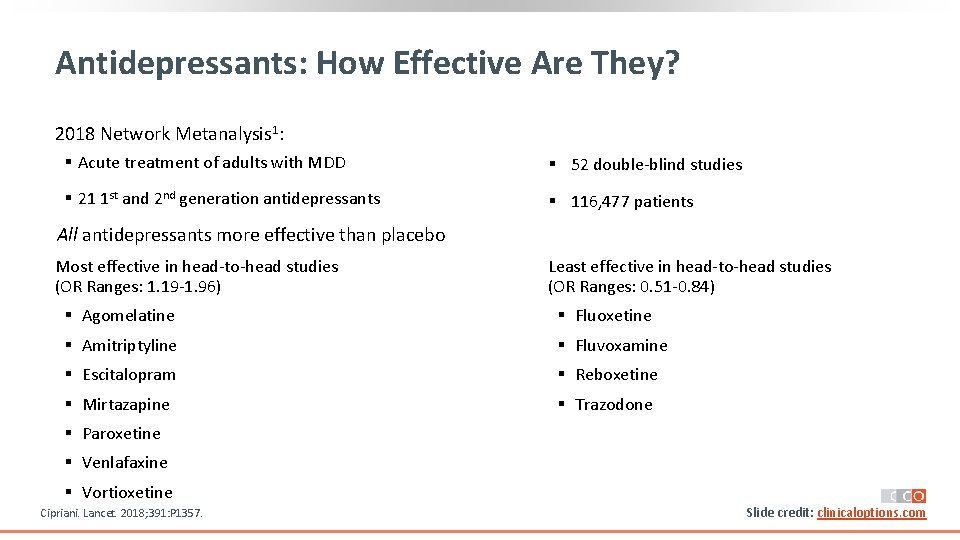
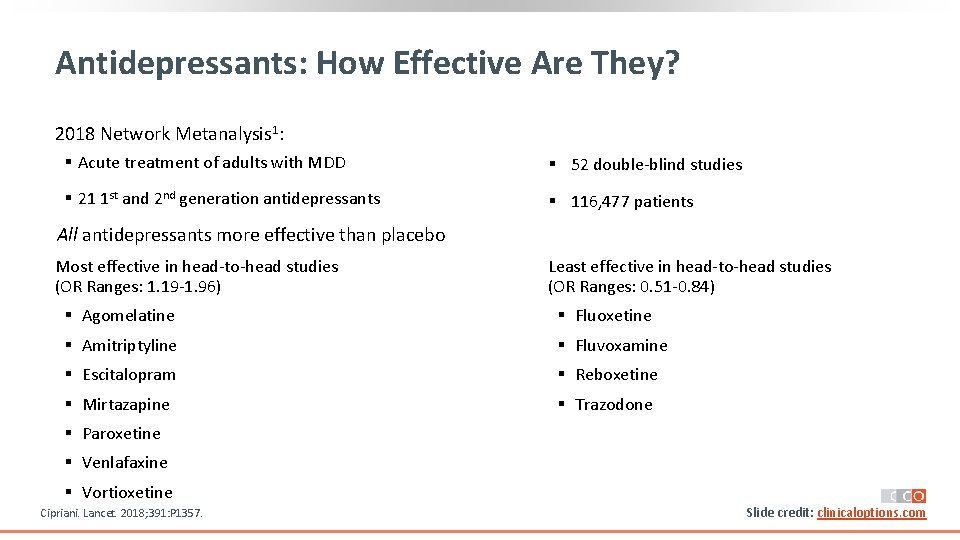
Antidepressants: How Effective Are They? 2018 Network Metanalysis 1: § Acute treatment of adults with MDD § 52 double‐blind studies § 21 1 st and 2 nd generation antidepressants § 116, 477 patients All antidepressants more effective than placebo Most effective in head‐to‐head studies (OR Ranges: 1. 19‐ 1. 96) Least effective in head‐to‐head studies (OR Ranges: 0. 51‐ 0. 84) § Agomelatine § Fluoxetine § Amitriptyline § Fluvoxamine § Escitalopram § Reboxetine § Mirtazapine § Trazodone § Paroxetine § Venlafaxine § Vortioxetine Cipriani. Lancet. 2018; 391: P 1357. Slide credit: clinicaloptions. com
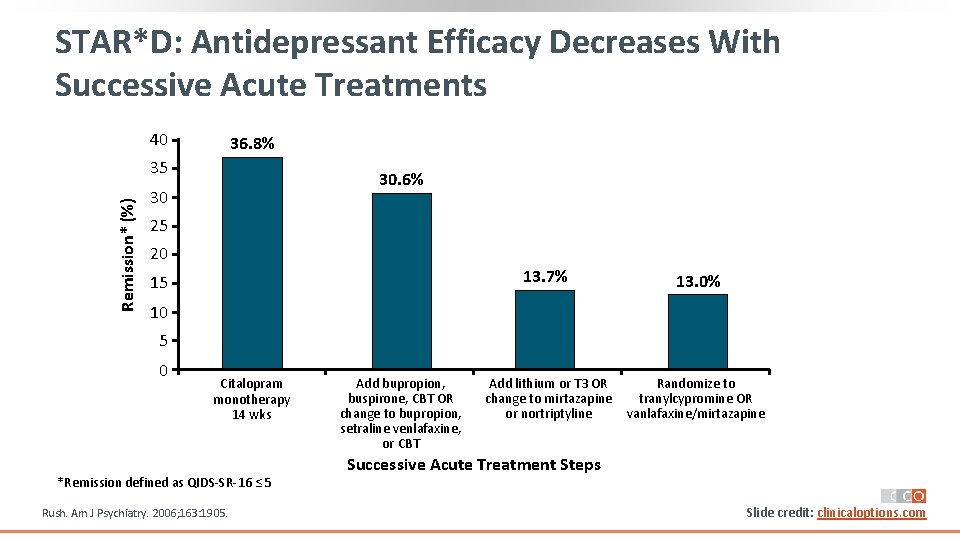
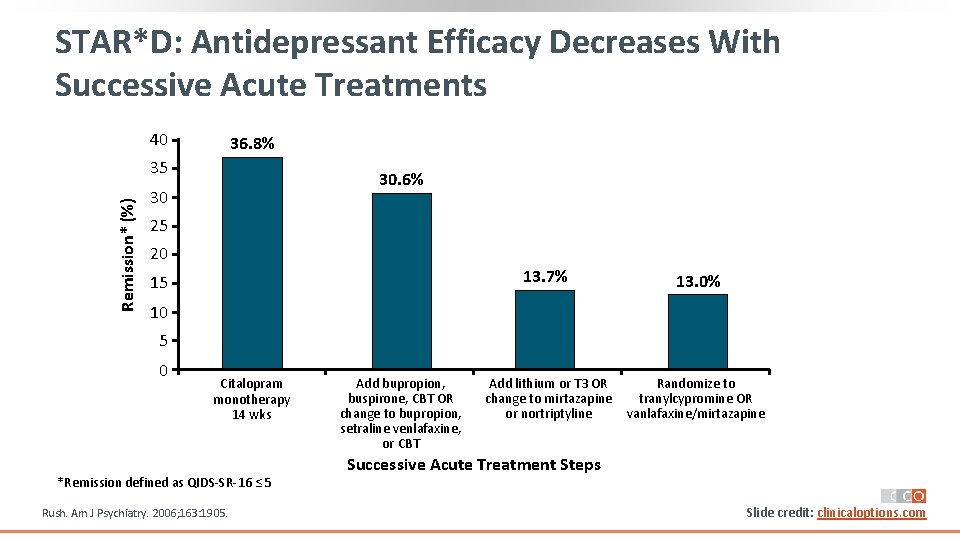
STAR*D: Antidepressant Efficacy Decreases With Successive Acute Treatments 40 36. 8% Remission* (%) 35 30. 6% 30 25 20 13. 7% 15 13. 0% 10 5 0 Citalopram monotherapy 14 wks *Remission defined as QIDS‐SR‐ 16 ≤ 5 Rush. Am J Psychiatry. 2006; 163: 1905. Add bupropion, buspirone, CBT OR change to bupropion, setraline venlafaxine, or CBT Add lithium or T 3 OR Randomize to change to mirtazapine tranylcypromine OR or nortriptyline vanlafaxine/mirtazapine Successive Acute Treatment Steps Slide credit: clinicaloptions. com
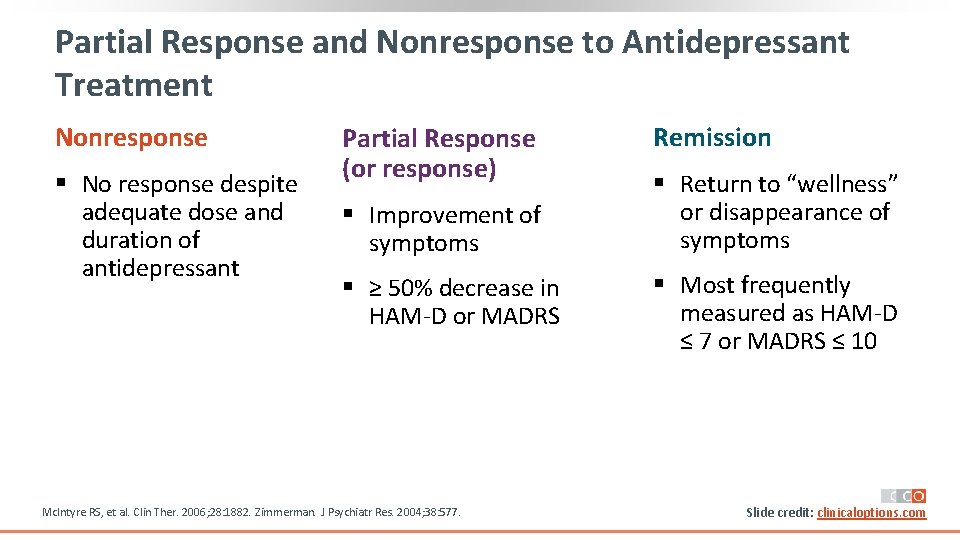
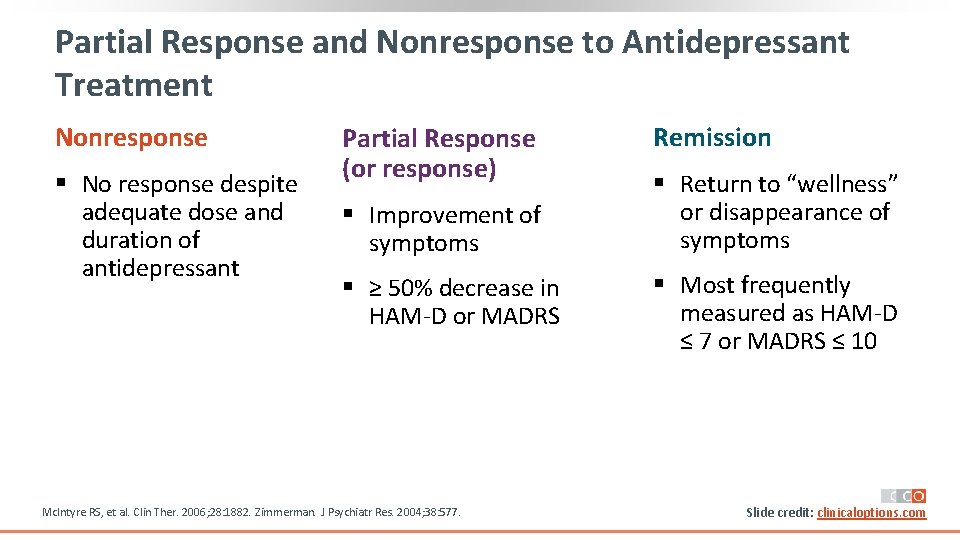
Partial Response and Nonresponse to Antidepressant Treatment Nonresponse § No response despite adequate dose and duration of Nonresponse antidepressant Partial Response (or response) § Improvement of symptoms Partial Response No response despite § ≥ 50% decrease in or Response adequate dose and duration of antidepressant HAM‐D or MADRS Mc. Intyre RS, et al. Clin Ther. 2006; 28: 1882. Zimmerman. J Psychiatr Res. 2004; 38: 577. Remission § Return to “wellness” or disappearance of symptoms Remission § Most frequently HAM‐D < 7 measured as HAM‐D or ≤ 7 or MADRS ≤ 10 MADRS < 10 or 8 Slide credit: clinicaloptions. com
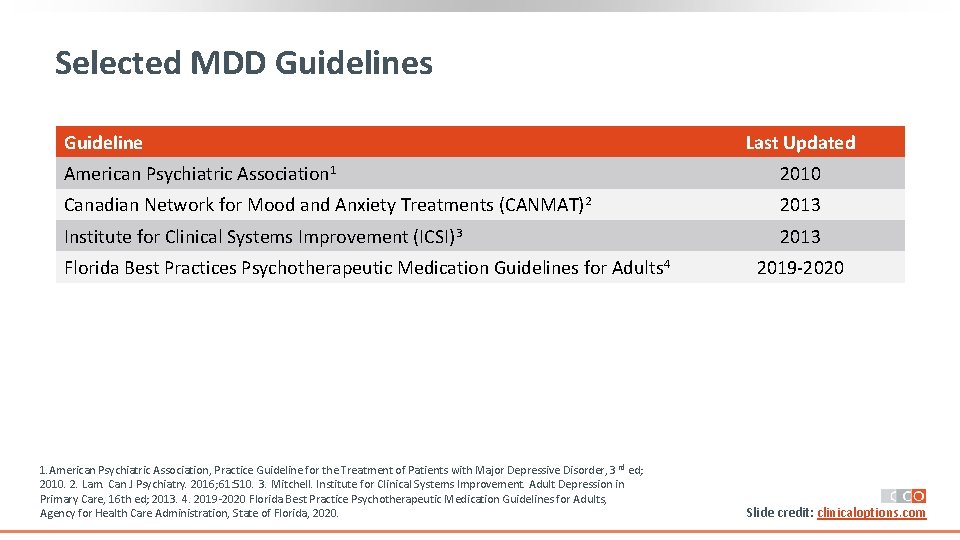
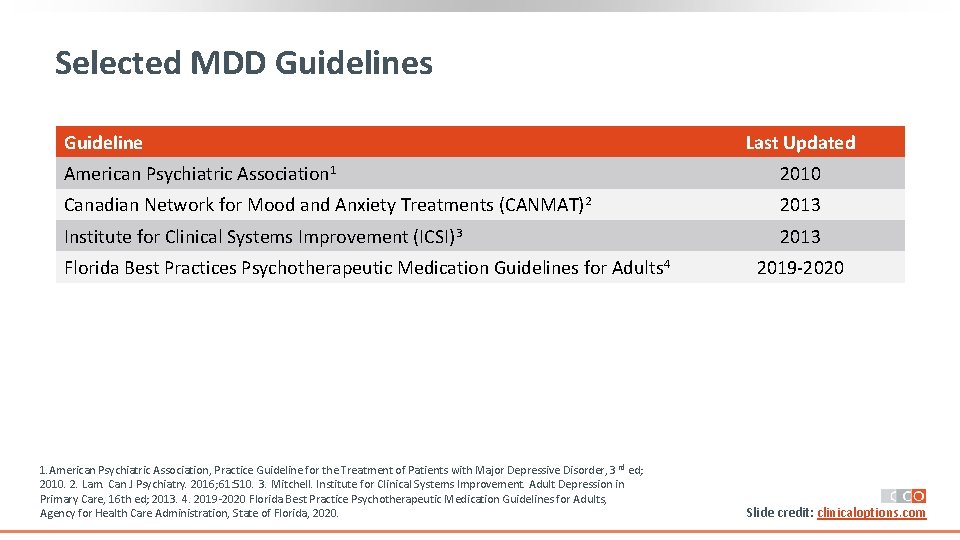
Selected MDD Guidelines Guideline Last Updated American Psychiatric Association 1 2010 Canadian Network for Mood and Anxiety Treatments (CANMAT)2 2013 Institute for Clinical Systems Improvement (ICSI)3 2013 Florida Best Practices Psychotherapeutic Medication Guidelines for Adults 4 1. American Psychiatric Association, Practice Guideline for the Treatment of Patients with Major Depressive Disorder, 3 rd ed; 2010. 2. Lam. Can J Psychiatry. 2016; 61: 510. 3. Mitchell. Institute for Clinical Systems Improvement. Adult Depression in Primary Care, 16 th ed; 2013. 4. 2019‐ 2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults, Agency for Health Care Administration, State of Florida, 2020. 2019‐ 2020 Slide credit: clinicaloptions. com
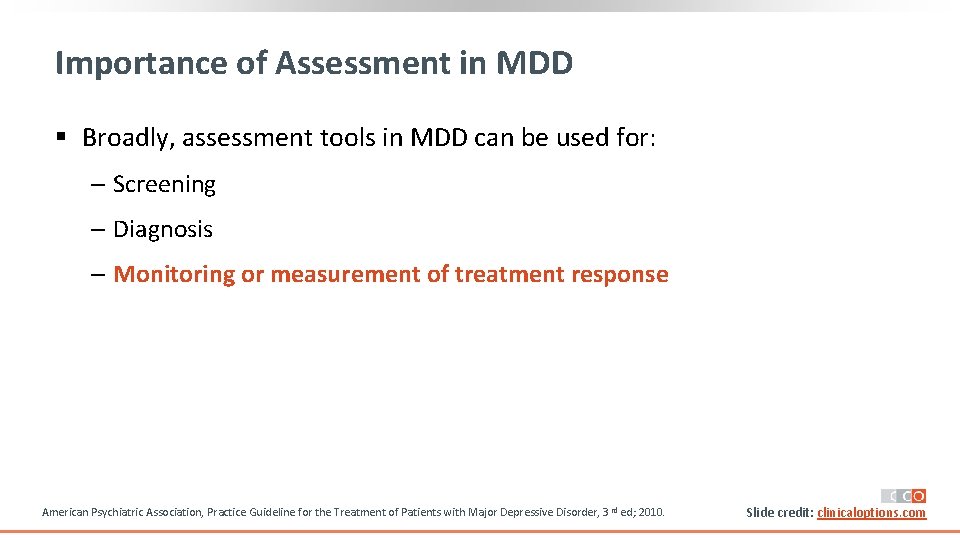
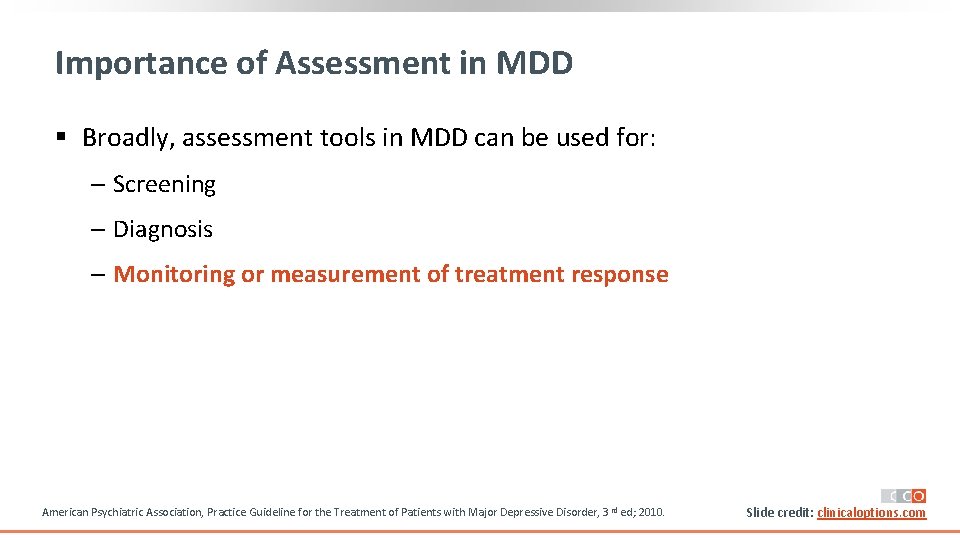
Importance of Assessment in MDD § Broadly, assessment tools in MDD can be used for: ‒ Screening ‒ Diagnosis ‒ Monitoring or measurement of treatment response American Psychiatric Association, Practice Guideline for the Treatment of Patients with Major Depressive Disorder, 3 rd ed; 2010. Slide credit: clinicaloptions. com
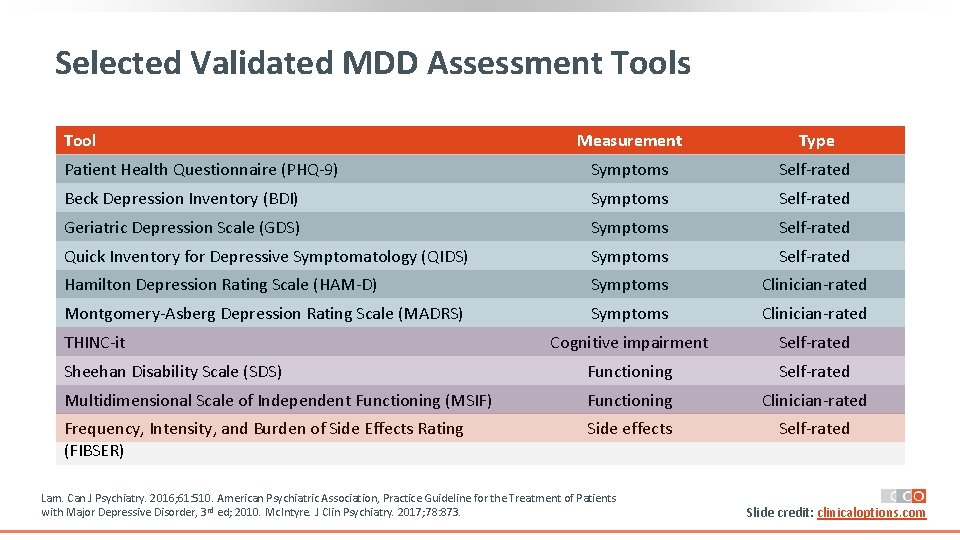
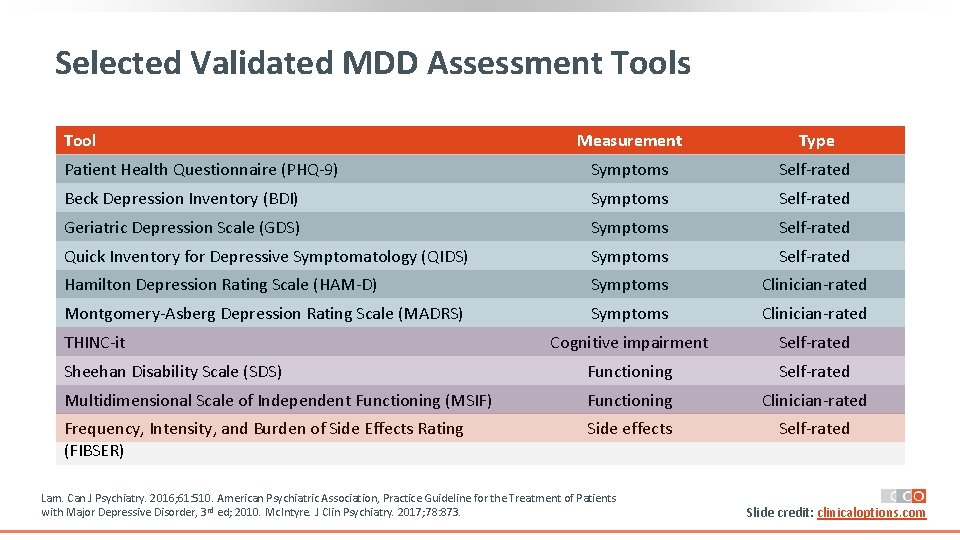
Selected Validated MDD Assessment Tools Tool Measurement Type Patient Health Questionnaire (PHQ‐ 9) Symptoms Self‐rated Beck Depression Inventory (BDI) Symptoms Self‐rated Geriatric Depression Scale (GDS) Symptoms Self‐rated Quick Inventory for Depressive Symptomatology (QIDS) Symptoms Self‐rated Hamilton Depression Rating Scale (HAM‐D) Symptoms Clinician‐rated Montgomery‐Asberg Depression Rating Scale (MADRS) Symptoms Clinician‐rated Cognitive impairment Self‐rated Sheehan Disability Scale (SDS) Functioning Self‐rated Multidimensional Scale of Independent Functioning (MSIF) Functioning Clinician‐rated Frequency, Intensity, and Burden of Side Effects Rating (FIBSER) Side effects Self‐rated THINC‐it Lam. Can J Psychiatry. 2016; 61: 510. American Psychiatric Association, Practice Guideline for the Treatment of Patients APA Diagnostic and Statistical Manual of Mental Disorders, 5 th ed. Washington, DC: 2013. with Major Depressive Disorder, 3 rd ed; 2010. Mc. Intyre. J Clin Psychiatry. 2017; 78: 873. Slide credit: clinicaloptions. com
![Guidelines Monitoring MDD Treatment Response Guidelines APA1 Recommendations on When and How to Use Guidelines: Monitoring MDD Treatment Response Guidelines APA[1] Recommendations on When and How to Use](https://slidetodoc.com/presentation_image_h/32170127986459186ef6f6de7437a6fc/image-11.jpg)
Guidelines: Monitoring MDD Treatment Response Guidelines APA[1] Recommendations on When and How to Use Rating Scales § Assess adequacy of treatment (appropriate dose, duration) § Assess symptoms using standardized measurement instruments CANMAT[2] § Monitor outcomes and support clinical decision‐making § Conduct ongoing evaluation of functional impairment and quality of life § Patient‐rated questionnaires are simpler to use and more efficient § Assess symptom severity during initial evaluation/treatment, after medication changes, and when patient reports change in symptoms Florida Best Practice Guideline[3] 1. American Psychiatric Association, Practice Guideline for the Treatment of Patients with Major Depressive Disorder, 3 rd ed; 2010. 2. Kennedy. Can J Psychiatry. 2016; 61: 540. 3. 2019‐ 2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults, Agency for Health Care Administration, State of Florida, 2020. Slide credit: clinicaloptions. com
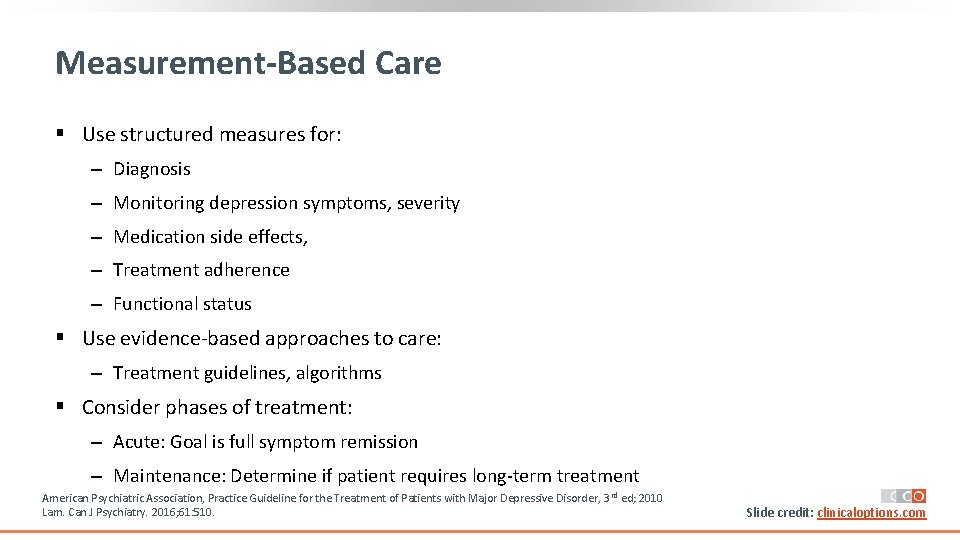
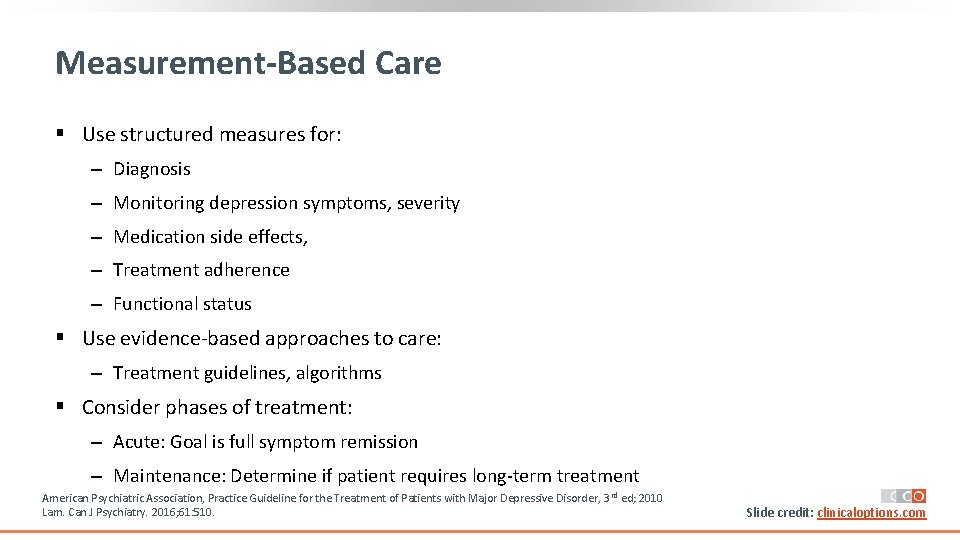
Measurement-Based Care § Use structured measures for: ‒ Diagnosis ‒ Monitoring depression symptoms, severity ‒ Medication side effects, ‒ Treatment adherence ‒ Functional status § Use evidence‐based approaches to care: ‒ Treatment guidelines, algorithms § Consider phases of treatment: ‒ Acute: Goal is full symptom remission ‒ Maintenance: Determine if patient requires long‐term treatment American Psychiatric Association, Practice Guideline for the Treatment of Patients with Major Depressive Disorder, 3 rd ed; 2010 Lam. Can J Psychiatry. 2016; 61: 510. Slide credit: clinicaloptions. com
MDD: Integrated Care Model § Patient access to providers § Timely crisis intervention Problem‐focused care Interdisciplinary care team § Structured treatment protocols § Systematic follow‐up VA/Do. D Clinical Practice Guideline for the Management of Major Depressive Disorders, 2016. § Patient/family education § Facilitated self‐ management Slide credit: clinicaloptions. com
![Guidelines When MDD Treatment Fails Guideline Recommendations APA1 Consider change in treatment if Guidelines: When MDD Treatment Fails Guideline Recommendations APA[1] § Consider change in treatment if](https://slidetodoc.com/presentation_image_h/32170127986459186ef6f6de7437a6fc/image-14.jpg)
Guidelines: When MDD Treatment Fails Guideline Recommendations APA[1] § Consider change in treatment if patient has not fully responded to acute phase treatment over 4‐ 8 weeks CANMAT[2] § If no early improvement after 2‐ 4 weeks, consider switching or adding adjunctive treatments § If early improvement, continue treatment for 6‐ 8 weeks; if remission is not attained consider switching or treatment augmentation Florida Best Practice Guideline[3] § If initial treatment is ineffective or not tolerated, evaluate adherence, optimize dose § If response is still insufficient, switch to different therapy or augment with psychotherapy, atypical antipsychotic FDA approved for MDD, another antidepressant (do not combine SSRI with SNRI), intranasal esketamine or intravenous racemic ketamine 1. American Psychiatric Association, Practice Guideline for the Treatment of Patients with Major Depressive Disorder, 3 rd ed; 2010. 2. Kennedy. Can J Psychiatry. 2016; 61: 540. 3. 2019‐ 2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults, Agency for Health Care Administration, State of Florida, 2020. Slide credit: clinicaloptions. com
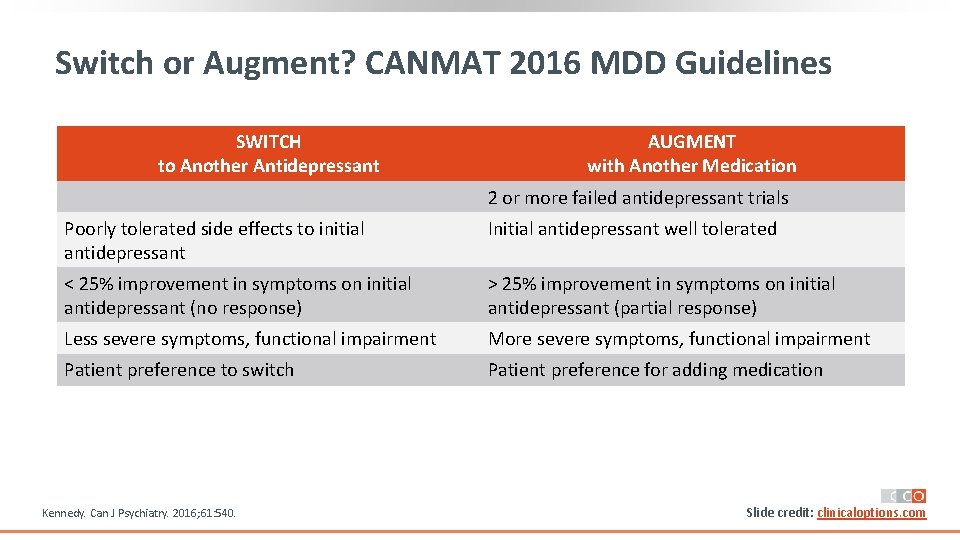
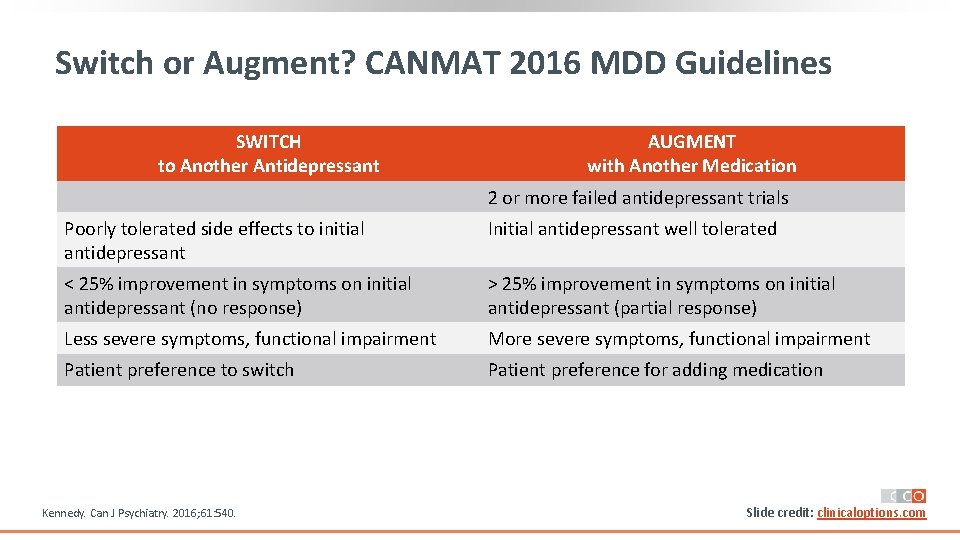
Switch or Augment? CANMAT 2016 MDD Guidelines SWITCH to Another Antidepressant AUGMENT with Another Medication 2 or more failed antidepressant trials Poorly tolerated side effects to initial antidepressant Initial antidepressant well tolerated < 25% improvement in symptoms on initial antidepressant (no response) > 25% improvement in symptoms on initial antidepressant (partial response) Less severe symptoms, functional impairment More severe symptoms, functional impairment Patient preference to switch Patient preference for adding medication Kennedy. Can J Psychiatry. 2016; 61: 540. Slide credit: clinicaloptions. com
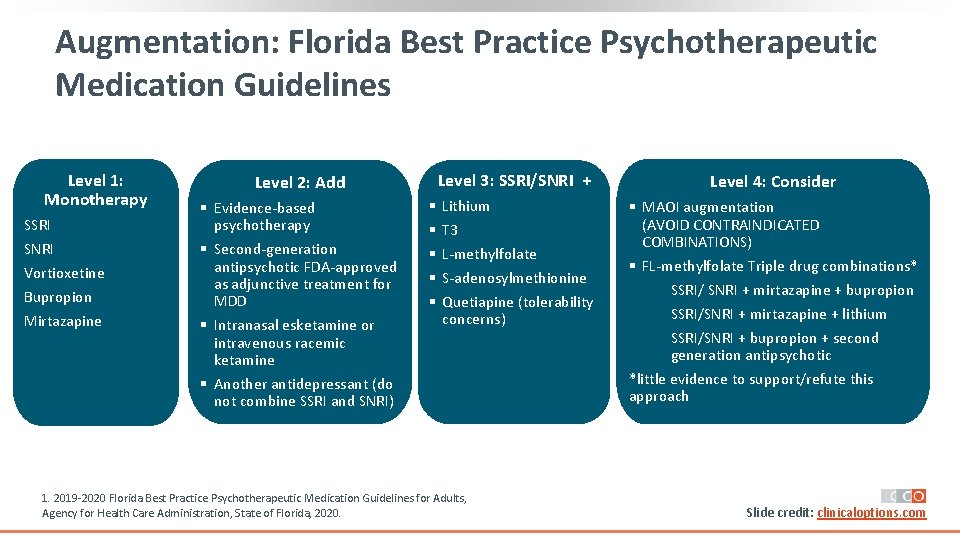
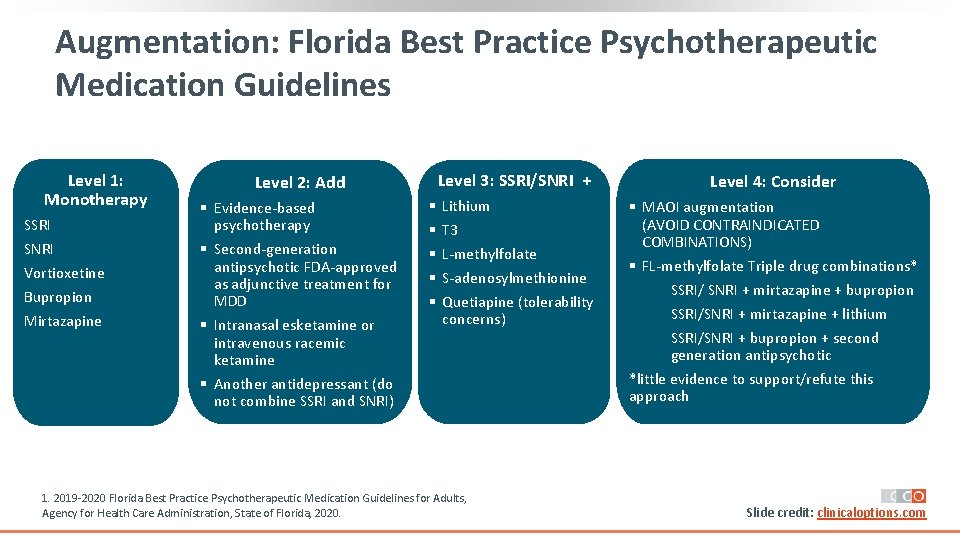
Augmentation: Florida Best Practice Psychotherapeutic Medication Guidelines Level 1: Monotherapy SSRI SNRI Vortioxetine Bupropion Mirtazapine Level 2: Add § Evidence‐based psychotherapy § Second‐generation antipsychotic FDA‐approved as adjunctive treatment for MDD § Intranasal esketamine or intravenous racemic ketamine § Another antidepressant (do not combine SSRI and SNRI) § § § Level 3: SSRI/SNRI + Level 4: Consider Lithium T 3 L‐methylfolate S‐adenosylmethionine Quetiapine (tolerability concerns) § MAOI augmentation (AVOID CONTRAINDICATED COMBINATIONS) § FL‐methylfolate Triple drug combinations* SSRI/ SNRI + mirtazapine + bupropion SSRI/SNRI + mirtazapine + lithium SSRI/SNRI + bupropion + second generation antipsychotic *little evidence to support/refute this approach 1. 2019‐ 2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults, Agency for Health Care Administration, State of Florida, 2020. Slide credit: clinicaloptions. com
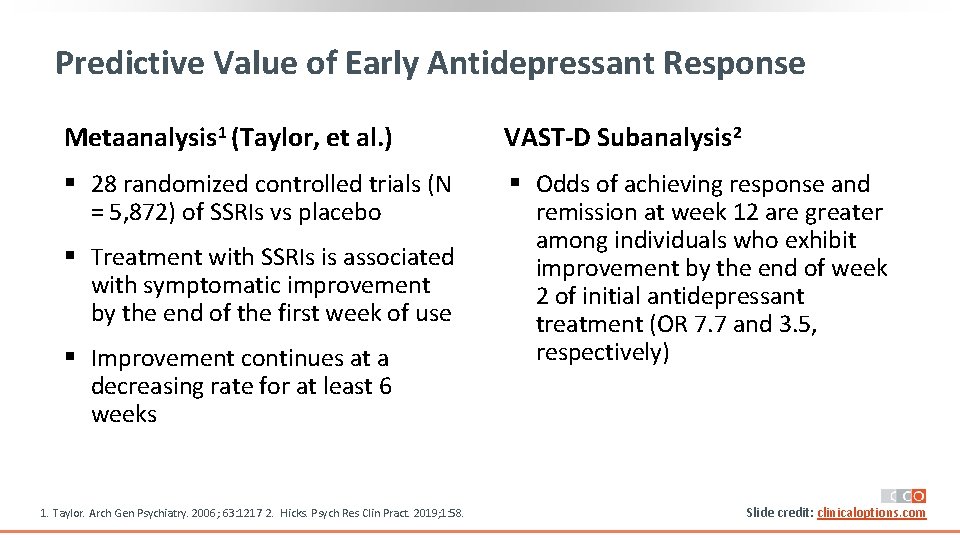
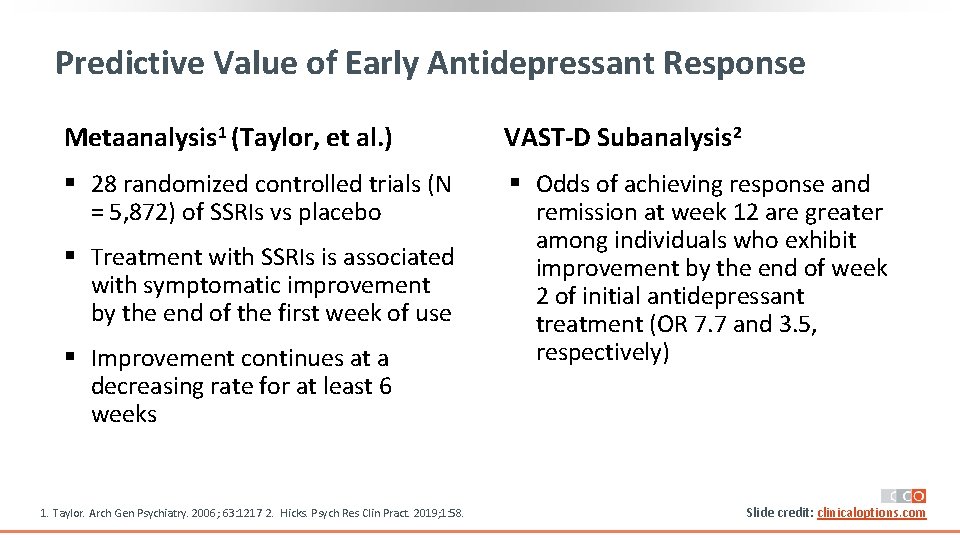
Predictive Value of Early Antidepressant Response Metaanalysis 1 (Taylor, et al. ) VAST-D Subanalysis 2 § 28 randomized controlled trials (N = 5, 872) of SSRIs vs placebo § Odds of achieving response and remission at week 12 are greater among individuals who exhibit improvement by the end of week 2 of initial antidepressant treatment (OR 7. 7 and 3. 5, respectively) § Treatment with SSRIs is associated with symptomatic improvement by the end of the first week of use § Improvement continues at a decreasing rate for at least 6 weeks 1. Taylor. Arch Gen Psychiatry. 2006; 63: 1217 2. Hicks. Psych Res Clin Pract. 2019; 1: 58. Slide credit: clinicaloptions. com
![Adjunctive Therapies for MDD Second Generation Antipsychotic Agents Agent Indication 1 Aripiprazole1 Adjunctive treatment Adjunctive Therapies for MDD: Second. Generation Antipsychotic Agents Agent Indication 1 Aripiprazole[1] Adjunctive treatment](https://slidetodoc.com/presentation_image_h/32170127986459186ef6f6de7437a6fc/image-18.jpg)
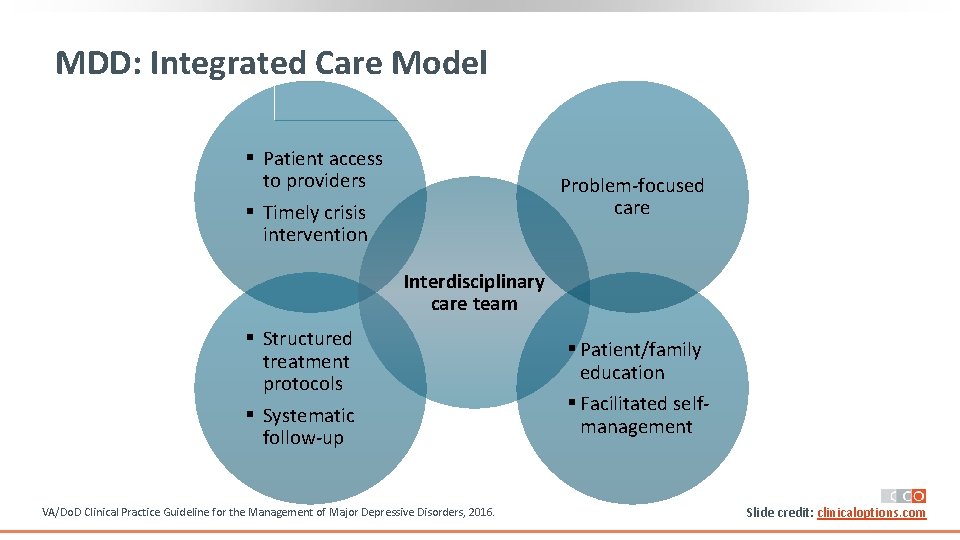
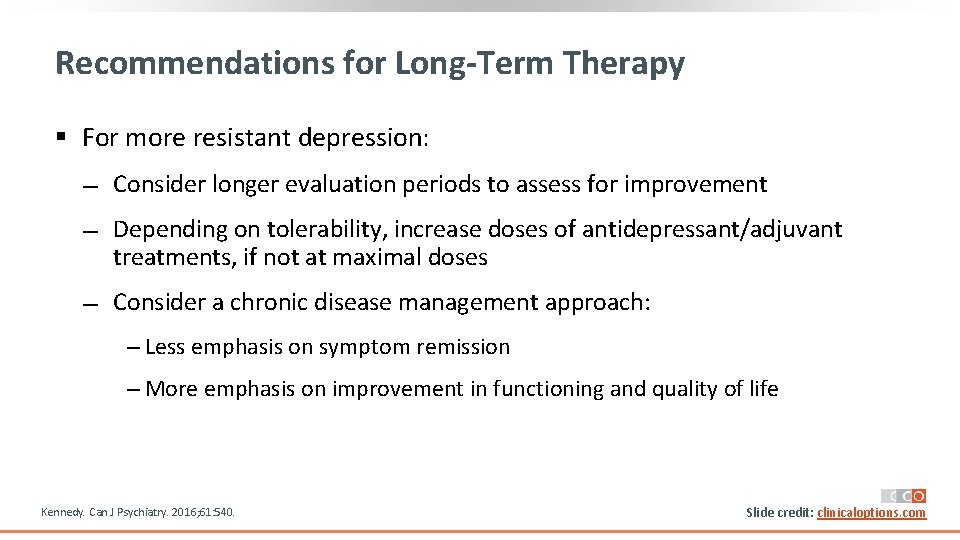
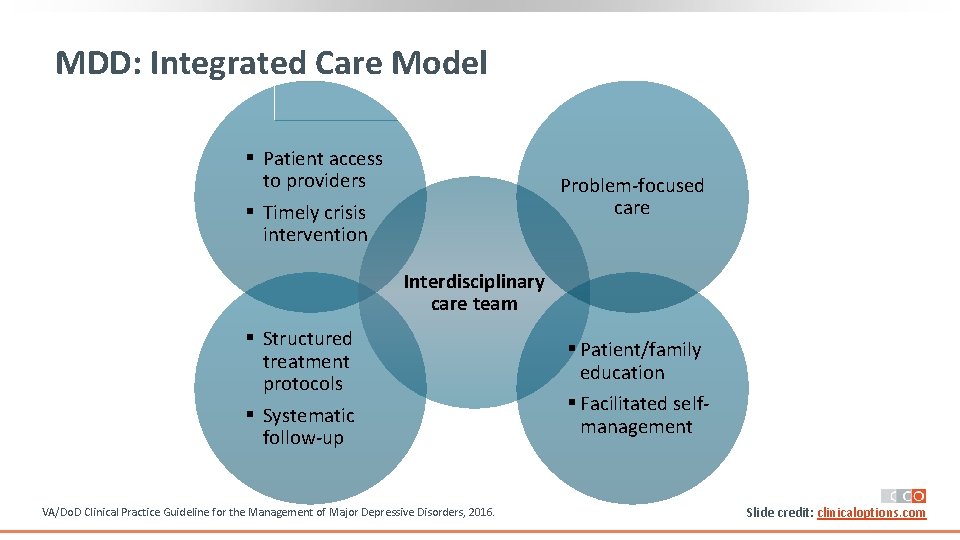
Adjunctive Therapies for MDD: Second. Generation Antipsychotic Agents Agent Indication 1 Aripiprazole[1] Adjunctive treatment for adults with MDD Brexpiprazole[2] Adjunctive therapy to antidepressants for MDD Quetiapine XR[3] Adjunctive therapy to antidepressants for adults with MDD Olanzapine + fluoxetine[4] Treatment‐resistant depression* *MDD in adults who do not respond to 2 separate trials of different antidepressants of adequate dose and duration in the current episode. 1. Aripiprazole PI. 2. Brexpiprazole PI. 3. Quetiapine XR PI. 4. Olanzapine/fluoxetine PI. Slide credit: clinicaloptions. com
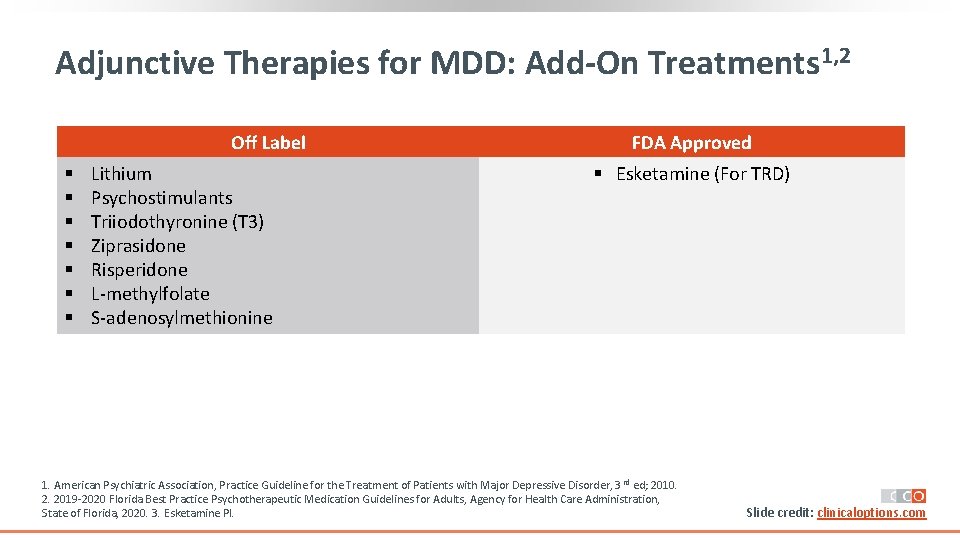
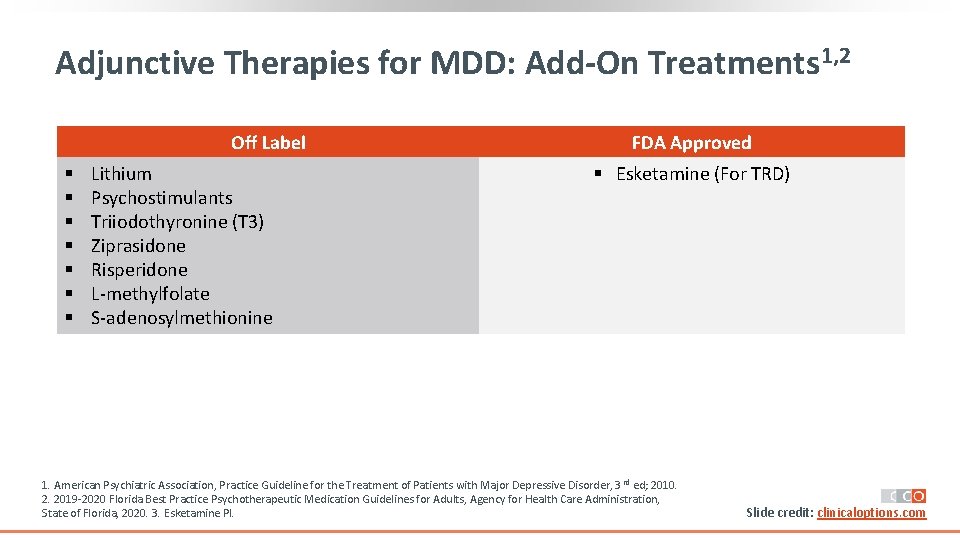
Adjunctive Therapies for MDD: Add-On Treatments 1, 2 Off Label § § § § Lithium Psychostimulants Triiodothyronine (T 3) Ziprasidone Risperidone L‐methylfolate S‐adenosylmethionine FDA Approved § Esketamine (For TRD) 1. American Psychiatric Association, Practice Guideline for the Treatment of Patients with Major Depressive Disorder, 3 rd ed; 2010. 2. 2019‐ 2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults, Agency for Health Care Administration, State of Florida, 2020. 3. Esketamine PI. Slide credit: clinicaloptions. com
Second-Generation Antipsychotic Agents: Potential Side Effects § Weight gain § Hyperprolactinemia § Glucose dysregulation § Akathisia § Diabetes § Tardive dyskinesia § Dyslipidemia § Neuroleptic malignant syndrome § Hypertriglyceridemia § QTc prolongation American Psychiatric Association, Practice Guideline for the Treatment of Patients with Major Depressive Disorder, 3 rd ed; 2010 2019‐ 2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults, Agency for Health Care Administration, State of Florida, 2020. Slide credit: clinicaloptions. com
Second-Generation Antipsychotic Agents: Managing Side Effects § Consider potential advantages and disadvantages for individual patients before prescribing § Lower doses are typically used in combination with antidepressants, compared to doses for bipolar disorder and psychosis § Decreasing dose may minimize risk of side effects § Monitor for side effects, including sedation, weight gain, akathisia and extrapyramidal symptoms § Monitor weight and body mass index, and metabolic indices at baseline and regular intervals American Psychiatric Association, Practice Guideline for the Treatment of Patients with Major Depressive Disorder, 3 rd ed; 2010 2019‐ 2020 Florida Best Practice Psychotherapeutic Medication Guidelines for Adults, Agency for Health Care Administration, State of Florida, 2020. Slide credit: clinicaloptions. com
Recommendations for Long-Term Therapy § For more resistant depression: Consider longer evaluation periods to assess for improvement Depending on tolerability, increase doses of antidepressant/adjuvant treatments, if not at maximal doses Consider a chronic disease management approach: ‒ Less emphasis on symptom remission ‒ More emphasis on improvement in functioning and quality of life Kennedy. Can J Psychiatry. 2016; 61: 540. Slide credit: clinicaloptions. com
Go Online for More CCO Coverage of Depression! CME-certified activities with expert faculty commentary Additional unlocked slidesets with key information clinicaloptions. com/internal-medicine