Guidelines for the Prevention Containment of Antimicrobial Resistance
Guidelines for the Prevention & Containment of Antimicrobial Resistance in South African Hospitals Dr Kim Faure on behalf of the Ministerial Advisory Committee for AMR of the NDOH FIDSSA conference 2019 9 th November 2019

Purpose • How to guide • Links prevention of HAIs with AMS practices at hospital level • Evidence from various international guidance documents and standards • Customised 2
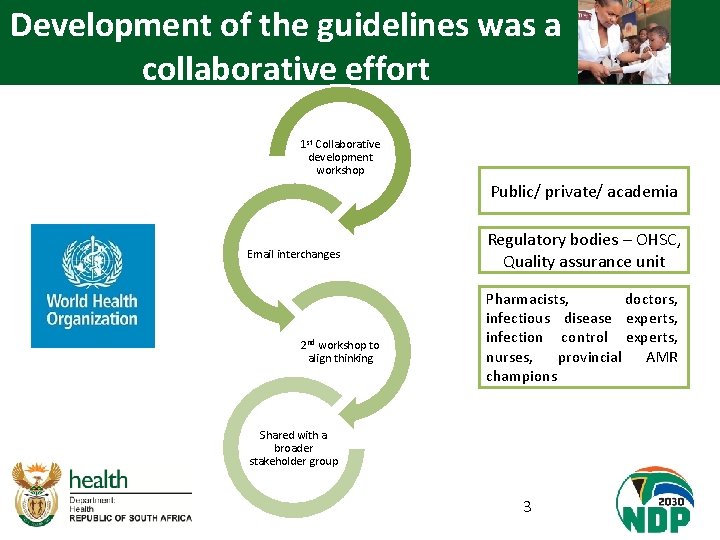
Development of the guidelines was a collaborative effort 1 st Collaborative development workshop Public/ private/ academia Email interchanges 2 nd workshop to align thinking Regulatory bodies – OHSC, Quality assurance unit Pharmacists, doctors, infectious disease experts, infection control experts, nurses, provincial AMR champions Shared with a broader stakeholder group 3
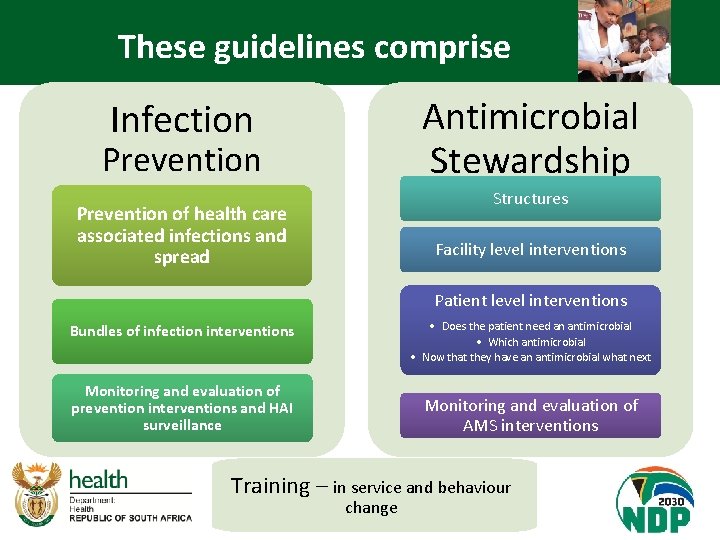
These guidelines comprise Antimicrobial Stewardship Infection Prevention Structures Prevention of health care associated infections and spread Facility level interventions Patient level interventions • Does the patient need an antimicrobial Bundles of infection interventions • Which antimicrobial • Now that they have an antimicrobial what next Monitoring and evaluation of prevention interventions and HAI surveillance Monitoring and evaluation of AMS interventions Training – in service and behaviour change 4
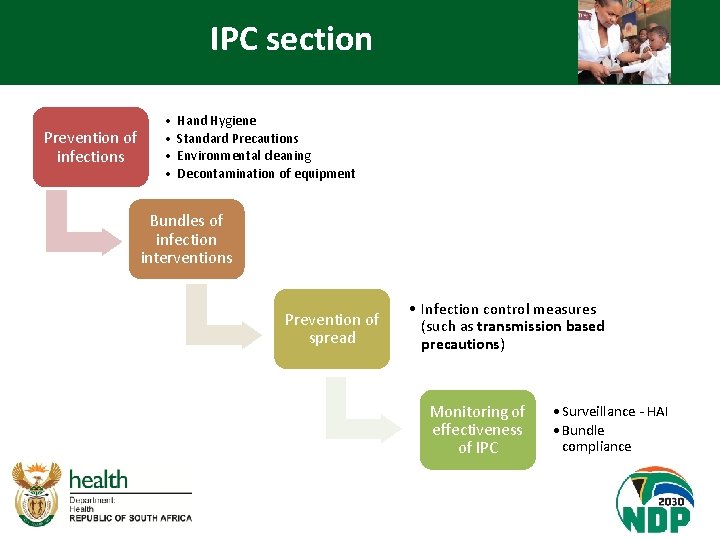
IPC section Prevention of infections • • Hand Hygiene Standard Precautions Environmental cleaning Decontamination of equipment Bundles of infection interventions Prevention of spread • Infection control measures (such as transmission based precautions) Monitoring of effectiveness of IPC • Surveillance - HAI • Bundle compliance
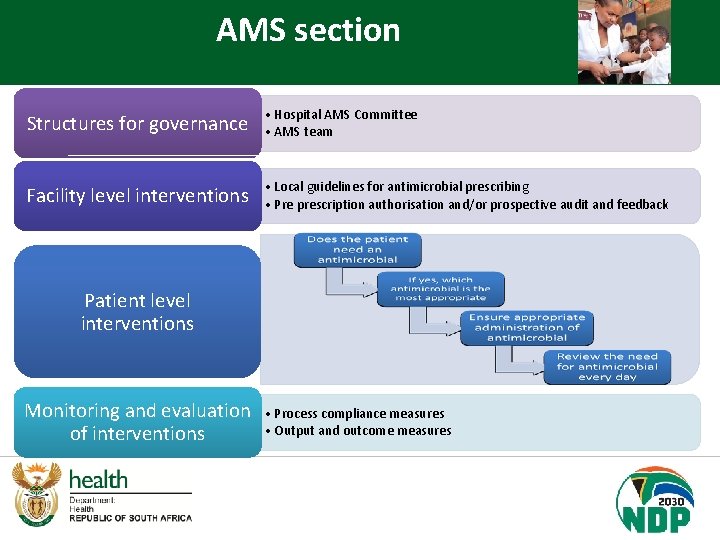
AMS section Structures for governance • Hospital AMS Committee • AMS team Facility level interventions • Local guidelines for antimicrobial prescribing • Pre prescription authorisation and/or prospective audit and feedback Patient level interventions Monitoring and evaluation of interventions • Process compliance measures • Output and outcome measures
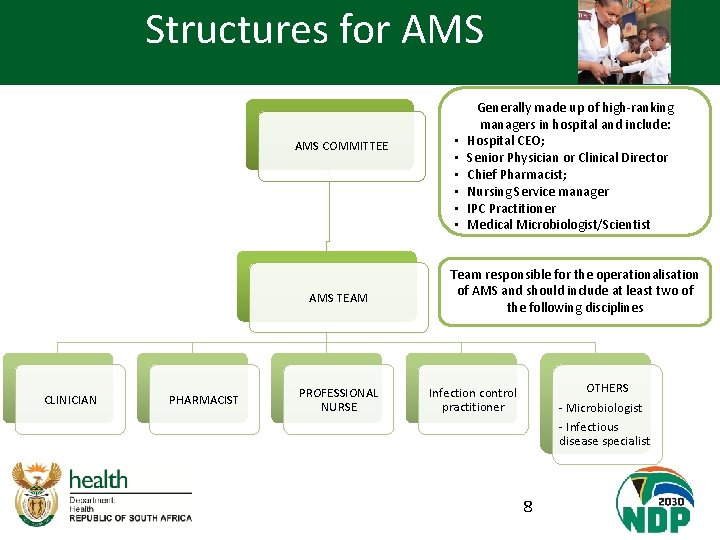
Structures for AMS COMMITTEE AMS TEAM CLINICIAN PHARMACIST PROFESSIONAL NURSE • • • Generally made up of high-ranking managers in hospital and include: Hospital CEO; Senior Physician or Clinical Director Chief Pharmacist; Nursing Service manager IPC Practitioner Medical Microbiologist/Scientist Team responsible for the operationalisation of AMS and should include at least two of the following disciplines OTHERS - Microbiologist - Infectious disease specialist Infection control practitioner 8
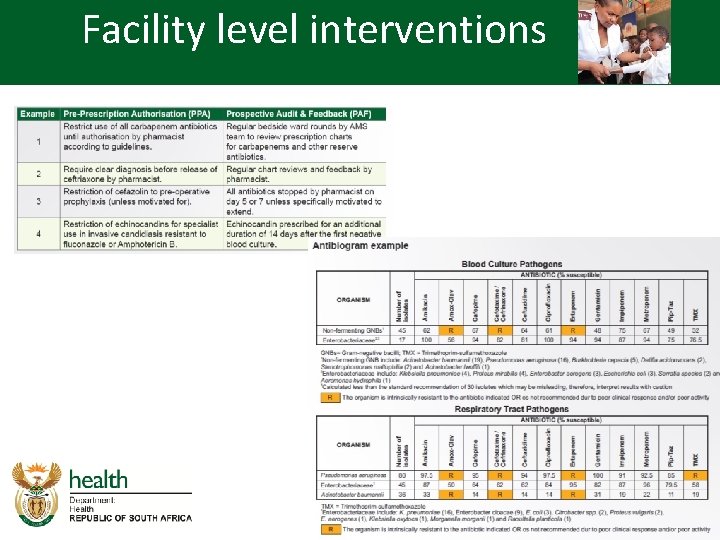
Facility level interventions 9
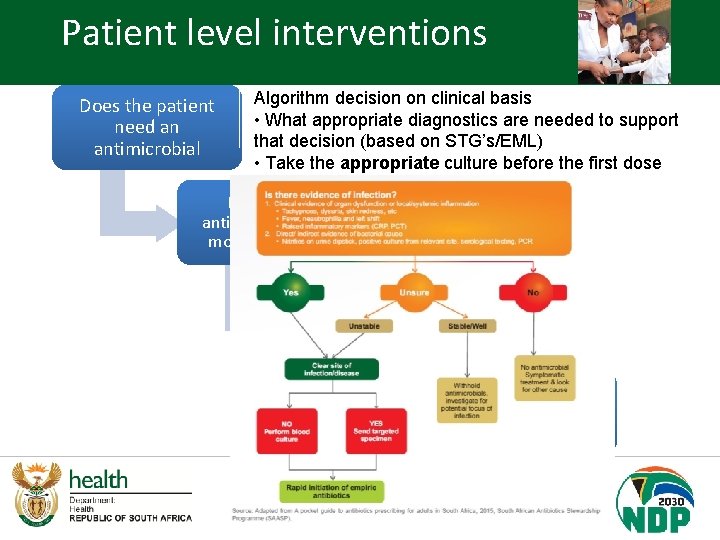
Patient level interventions Does the patient need an antimicrobial Algorithm decision on clinical basis • What appropriate diagnostics are needed to support that decision (based on STG’s/EML) • Take the appropriate culture before the first dose If yes, which antimicrobial is the most appropriate Ensure appropriate administration of antimicrobial Review the need for antimicrobial every day
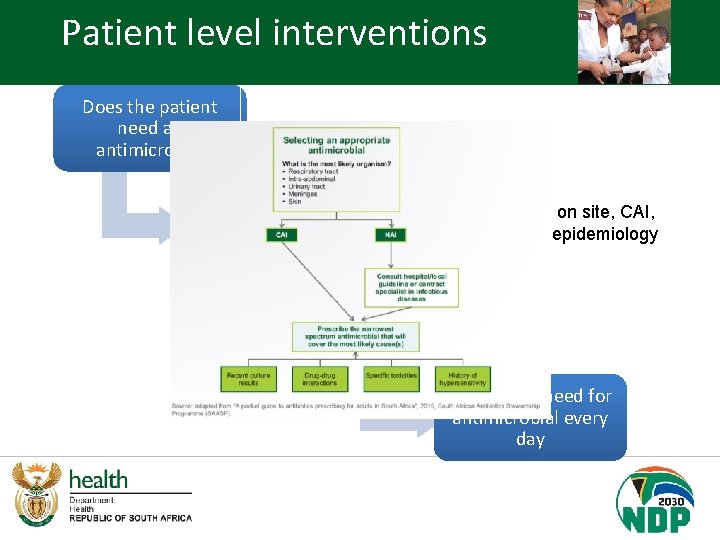
Patient level interventions Does the patient need an antimicrobial If yes, which antimicrobial is the most appropriate Empiric therapy based on site, CAI, HAI and local hospital epidemiology Ensure appropriate administration of antimicrobial Review the need for antimicrobial every day
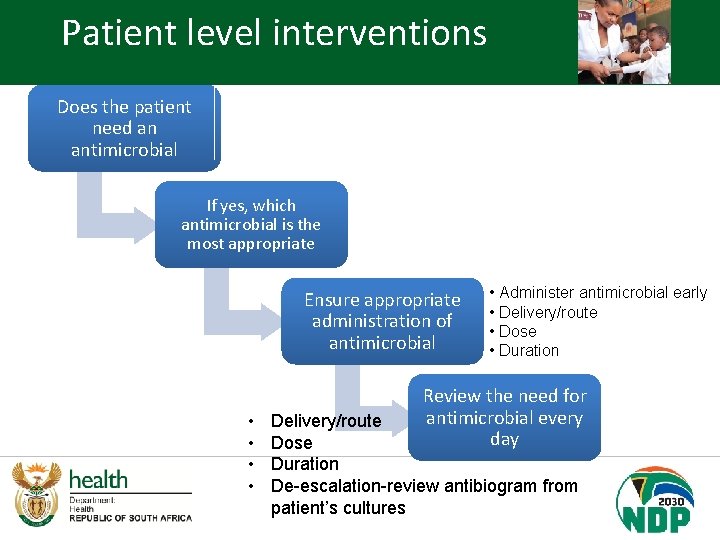
Patient level interventions Does the patient need an antimicrobial If yes, which antimicrobial is the most appropriate Ensure appropriate administration of antimicrobial • • • Administer antimicrobial early • Delivery/route • Dose • Duration Review the need for antimicrobial every day Delivery/route Dose Duration De-escalation-review antibiogram from patient’s cultures

4 D’s of appropriate administration of Antimicrobials Delivery • Review indications for IV daily • Always aim for oral Dose De-escalation Duration • Weight • Renal function • Correct intervals • Most infections require less than 7 days • Narrow the spectrum of antimicrobial based on drug susceptibility testing Antimicrobial Prescription charts 13
Role of nurses in administration The administration of antibiotics is a critical driver of antibiotic resistance and presents a complex set of challenges that is by no means a linear process. Administration of antibiotics includes seven steps namely (i) early administration of a correct antibiotic, (ii) the correct dose, (iii) the appropriate route of delivery, (iv) the correct duration, (v) The correct frequency, (vi) the correct patient and (vii) the correct documentation. 14

Roles and responsibilities of the team spelled out clearly Clinician Pharmacists Nurse IPC practitioner Microbiologist 15
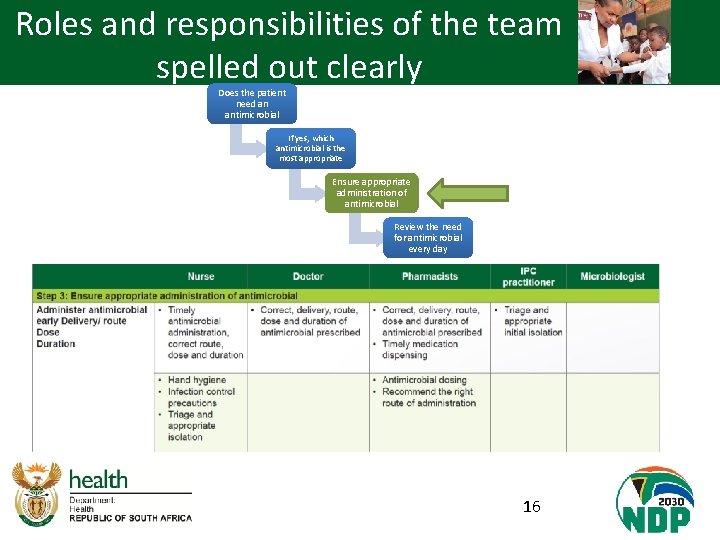
Roles and responsibilities of the team spelled out clearly Does the patient need an antimicrobial If yes, which antimicrobial is the most appropriate Ensure appropriate administration of antimicrobial Review the need for antimicrobial every day 16

The ultimate aim …. . . The right patient receives The right antibiotic for The right indication at The right dose and duration 17

Acknowledgements 18
Thank you! http: //www. health. gov. za/index. php/antimicro bial-resistance 19
- Slides: 18