Guidelines for Basic Adult Neurological Observation CCSO 2014
Guidelines for Basic Adult Neurological Observation, CCSO 2014
WHY PERFORM A NEURLOGICAL ASSESSMENT? • The baseline neurological assessment and ongoing assessments are the most sensitive indicators of neurological change • Early detection is important for successful treatment, management and prognosis Guidelines for Basic Adult Neurological Observation, CCSO 2014
WHAT’S INCLUDED? Assessment of the following: • Level of consciousness (LOC) using the Glasgow Coma Scale (GCS) • Pupillary response • Limb movement/ strength • Vital signs Note! The administration of continuous sedation of a patient, may obscure the neurological assessment, and the accuracy of the assesment. Guidelines for Basic Adult Neurological Observation, CCSO 2014
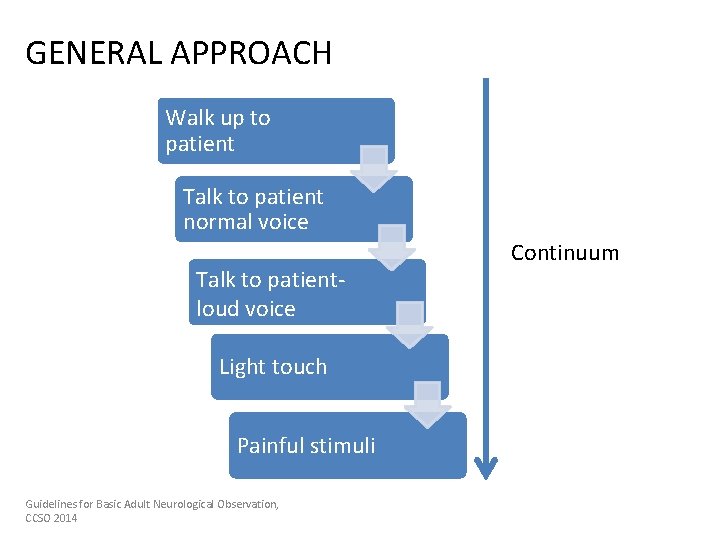
GENERAL APPROACH Walk up to patient Talk to patient normal voice Talk to patientloud voice Light touch Painful stimuli Guidelines for Basic Adult Neurological Observation, CCSO 2014 Continuum
PAINFUL STIMULI WHEN TO USE • If patient is not obeying commands AND • In the absence of any spontaneous movements TYPES OF STIMULI • Peripheral painful stimuli • Central painful stimuli Depending on the response being assessed Guidelines for Basic Adult Neurological Observation, CCSO 2014
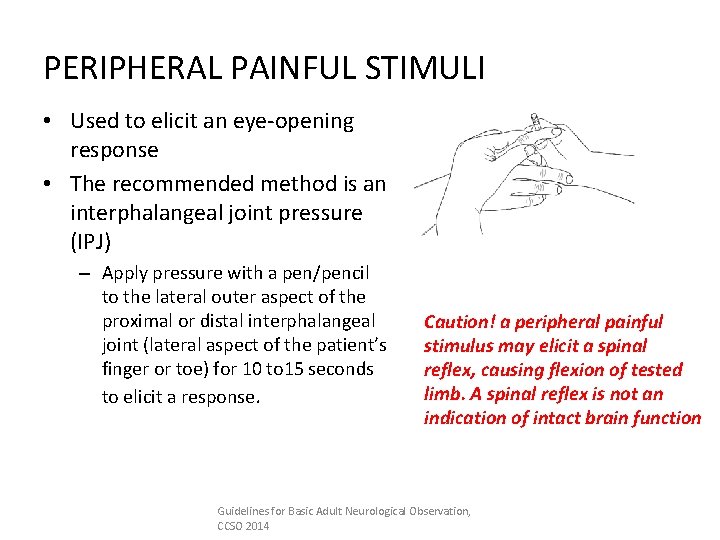
PERIPHERAL PAINFUL STIMULI • Used to elicit an eye-opening response • The recommended method is an interphalangeal joint pressure (IPJ) – Apply pressure with a pen/pencil to the lateral outer aspect of the proximal or distal interphalangeal joint (lateral aspect of the patient’s finger or toe) for 10 to 15 seconds to elicit a response. Caution! a peripheral painful stimulus may elicit a spinal reflex, causing flexion of tested limb. A spinal reflex is not an indication of intact brain function Guidelines for Basic Adult Neurological Observation, CCSO 2014
CENTRAL PAINFUL STIMULI • Used to elicit a motor response • Done by stimulating a cranial nerve, thus avoiding the possibility of eliciting a spinal reflex • Recommended methods are – Trapezius twist (CN XI) – Supra-orbital pressure (CN V) – Jaw margin pressure (CN V) Guidelines for Basic Adult Neurological Observation, CCSO 2014
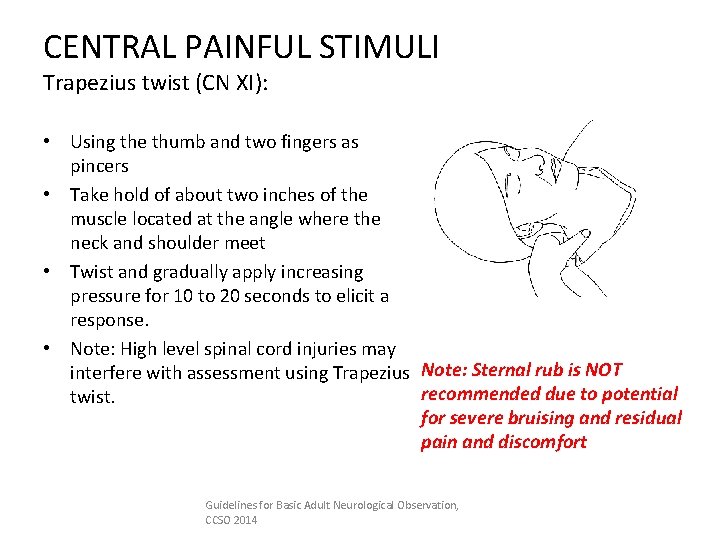
CENTRAL PAINFUL STIMULI Trapezius twist (CN XI): • Using the thumb and two fingers as pincers • Take hold of about two inches of the muscle located at the angle where the neck and shoulder meet • Twist and gradually apply increasing pressure for 10 to 20 seconds to elicit a response. • Note: High level spinal cord injuries may interfere with assessment using Trapezius Note: Sternal rub is NOT recommended due to potential twist. for severe bruising and residual pain and discomfort Guidelines for Basic Adult Neurological Observation, CCSO 2014
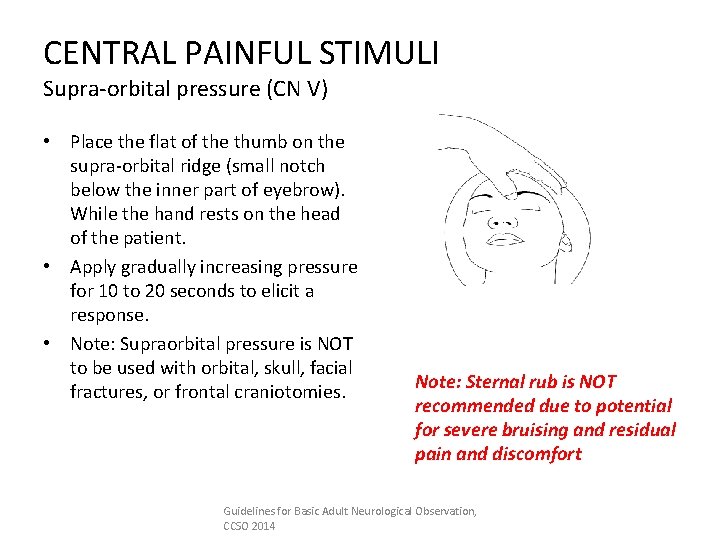
CENTRAL PAINFUL STIMULI Supra-orbital pressure (CN V) • Place the flat of the thumb on the supra-orbital ridge (small notch below the inner part of eyebrow). While the hand rests on the head of the patient. • Apply gradually increasing pressure for 10 to 20 seconds to elicit a response. • Note: Supraorbital pressure is NOT to be used with orbital, skull, facial fractures, or frontal craniotomies. Note: Sternal rub is NOT recommended due to potential for severe bruising and residual pain and discomfort Guidelines for Basic Adult Neurological Observation, CCSO 2014
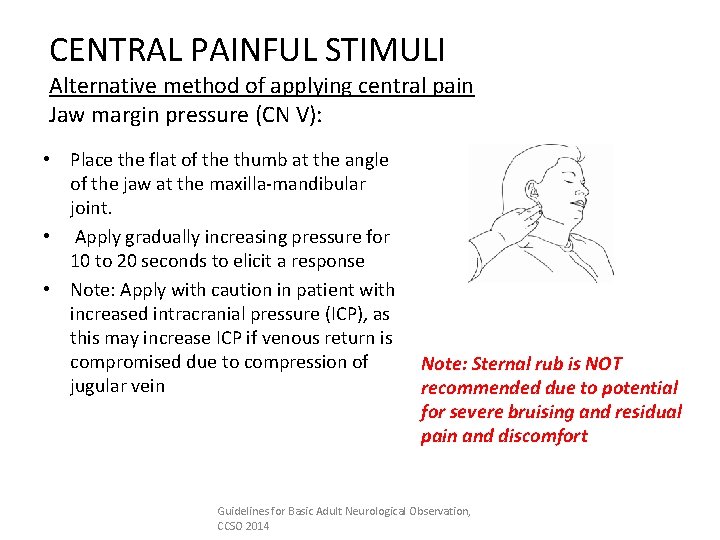
CENTRAL PAINFUL STIMULI Alternative method of applying central pain Jaw margin pressure (CN V): • Place the flat of the thumb at the angle of the jaw at the maxilla-mandibular joint. • Apply gradually increasing pressure for 10 to 20 seconds to elicit a response • Note: Apply with caution in patient with increased intracranial pressure (ICP), as this may increase ICP if venous return is compromised due to compression of jugular vein Note: Sternal rub is NOT recommended due to potential for severe bruising and residual pain and discomfort Guidelines for Basic Adult Neurological Observation, CCSO 2014
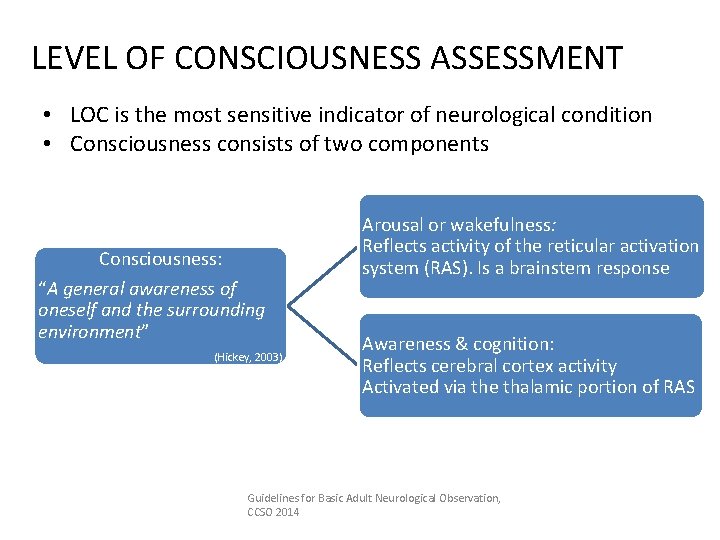
LEVEL OF CONSCIOUSNESS ASSESSMENT • LOC is the most sensitive indicator of neurological condition • Consciousness consists of two components Consciousness: “A general awareness of oneself and the surrounding environment” (Hickey, 2003) Arousal or wakefulness: Reflects activity of the reticular activation system (RAS). Is a brainstem response Awareness & cognition: Reflects cerebral cortex activity Activated via the thalamic portion of RAS Guidelines for Basic Adult Neurological Observation, CCSO 2014
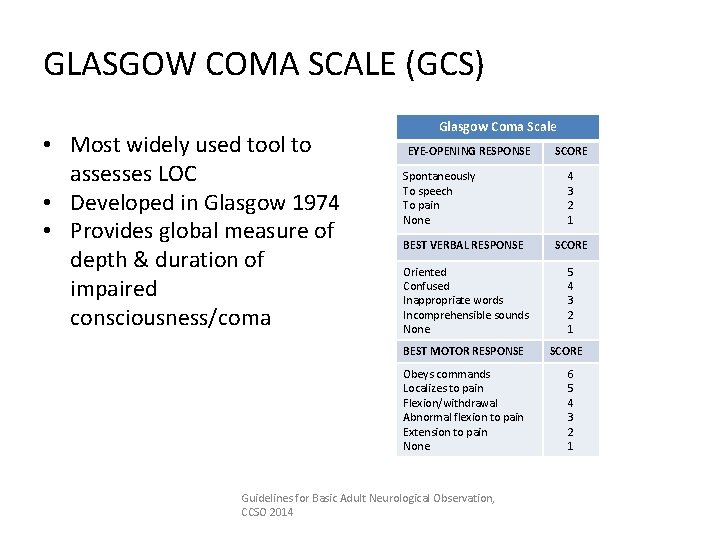
GLASGOW COMA SCALE (GCS) • Most widely used tool to assesses LOC • Developed in Glasgow 1974 • Provides global measure of depth & duration of impaired consciousness/coma Glasgow Coma Scale EYE-OPENING RESPONSE Spontaneously To speech To pain None SCORE 4 3 2 1 BEST VERBAL RESPONSE SCORE Oriented Confused Inappropriate words Incomprehensible sounds None 5 4 3 2 1 BEST MOTOR RESPONSE Obeys commands Localizes to pain Flexion/withdrawal Abnormal flexion to pain Extension to pain None Guidelines for Basic Adult Neurological Observation, CCSO 2014 SCORE 6 5 4 3 2 1
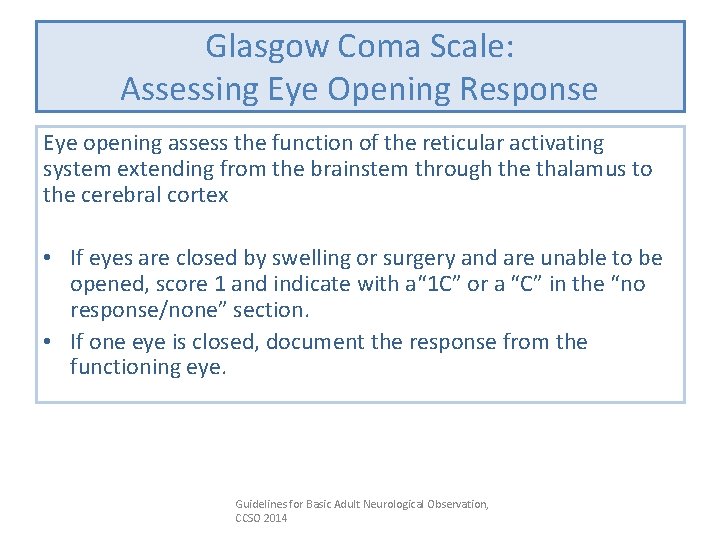
Glasgow Coma Scale: Assessing Eye Opening Response Eye opening assess the function of the reticular activating system extending from the brainstem through the thalamus to the cerebral cortex • If eyes are closed by swelling or surgery and are unable to be opened, score 1 and indicate with a“ 1 C” or a “C” in the “no response/none” section. • If one eye is closed, document the response from the functioning eye. Guidelines for Basic Adult Neurological Observation, CCSO 2014
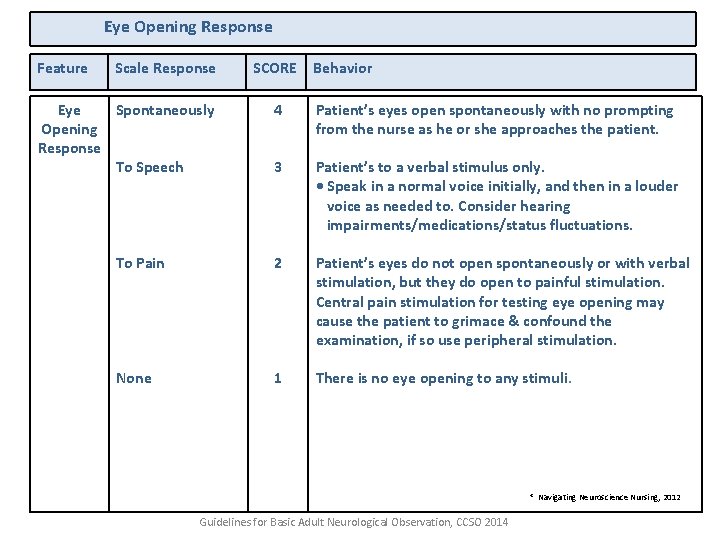
Eye Opening Response Feature Scale Response Eye Spontaneously Opening Response To Speech SCORE Behavior 4 Patient’s eyes open spontaneously with no prompting from the nurse as he or she approaches the patient. 3 Patient’s to a verbal stimulus only. • Speak in a normal voice initially, and then in a louder voice as needed to. Consider hearing impairments/medications/status fluctuations. To Pain 2 Patient’s eyes do not open spontaneously or with verbal stimulation, but they do open to painful stimulation. Central pain stimulation for testing eye opening may cause the patient to grimace & confound the examination, if so use peripheral stimulation. None 1 There is no eye opening to any stimuli. * Navigating Neuroscience Nursing, 2012 Guidelines for Basic Adult Neurological Observation, CCSO 2014
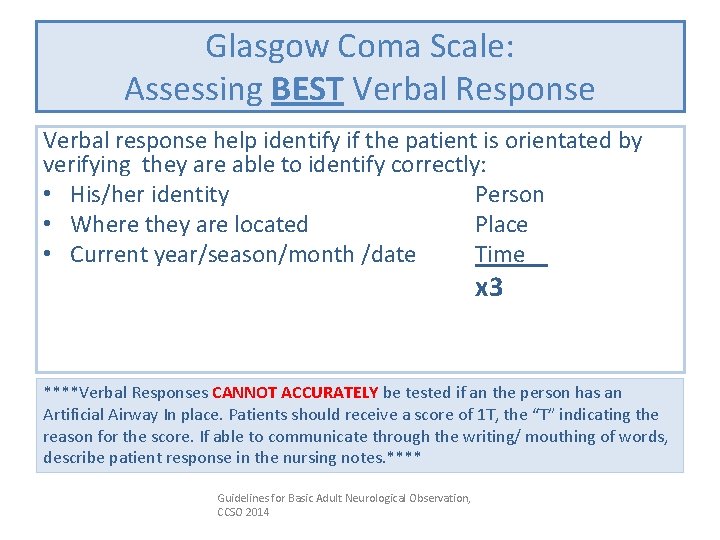
Glasgow Coma Scale: Assessing BEST Verbal Response Verbal response help identify if the patient is orientated by verifying they are able to identify correctly: • His/her identity Person • Where they are located Place • Current year/season/month /date Time x 3 ****Verbal Responses CANNOT ACCURATELY be tested if an the person has an Artificial Airway In place. Patients should receive a score of 1 T, the “T” indicating the reason for the score. If able to communicate through the writing/ mouthing of words, describe patient response in the nursing notes. **** Guidelines for Basic Adult Neurological Observation, CCSO 2014
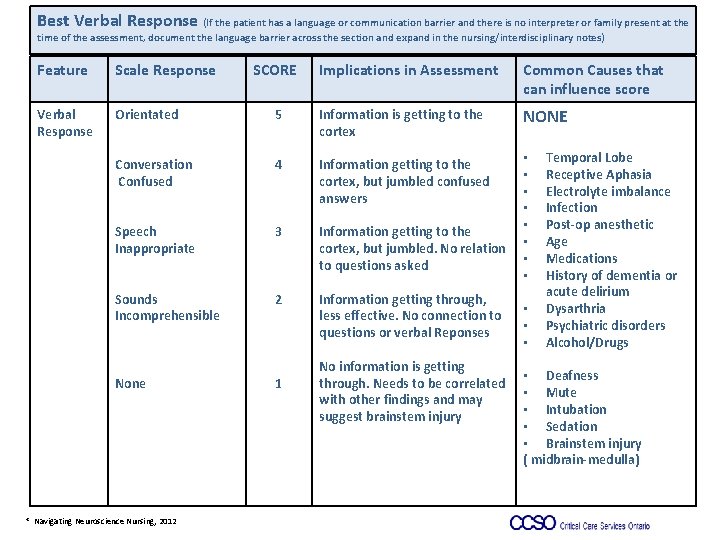
Best Verbal Response (If the patient has a language or communication barrier and there is no interpreter or family present at the time of the assessment, document the language barrier across the section and expand in the nursing/interdisciplinary notes) Feature Scale Response Verbal Response Orientated Implications in Assessment Common Causes that can influence score 5 Information is getting to the cortex NONE Conversation Confused 4 Information getting to the cortex, but jumbled confused answers Speech Inappropriate 3 Information getting to the cortex, but jumbled. No relation to questions asked • • Sounds Incomprehensible 2 Information getting through, less effective. No connection to questions or verbal Reponses None * Navigating Neuroscience Nursing, 2012 SCORE 1 No information is getting through. Needs to be correlated with other findings and may suggest brainstem injury • • • Temporal Lobe Receptive Aphasia Electrolyte imbalance Infection Post-op anesthetic Age Medications History of dementia or acute delirium Dysarthria Psychiatric disorders Alcohol/Drugs • Deafness • Mute • Intubation • Sedation • Brainstem injury ( midbrain-medulla)
Glasgow Coma Scale: Assessing BEST Motor Response Assesses area of brain, which identifies and translates sensory input into a motor response. Best response is documented • If patient is localizing spontaneously i. e. attempting to remove invasive tubes or when suctioned, do NOT use painful stimuli • If necessary, use central pain to avoid eliciting spinal reflex Guidelines for Basic Adult Neurological Observation, CCSO 2014
GCS – BEST MOTOR RESPONSE Obeying Commands: score of 6 • • The patient is able to understand obey verbal/ written/gestured commands. Acceptable commands include: “show me a thumb/two fingers”; “stick out your tongue”. Note: It is not acceptable to ask a patient to squeeze one’s hand unless he/she is also asked to release it. Hand grasping, without a release, may be merely a reflex. • If the patient is unable to obey commands, place the patient in a supine position with hands positioned at the groin area, if possible, and proceed through the assessment by applying a central painful stimulus. If applicable, loosen any limb restraints while performing assessment. Guidelines for Basic Adult Neurological Observation, CCSO 2014
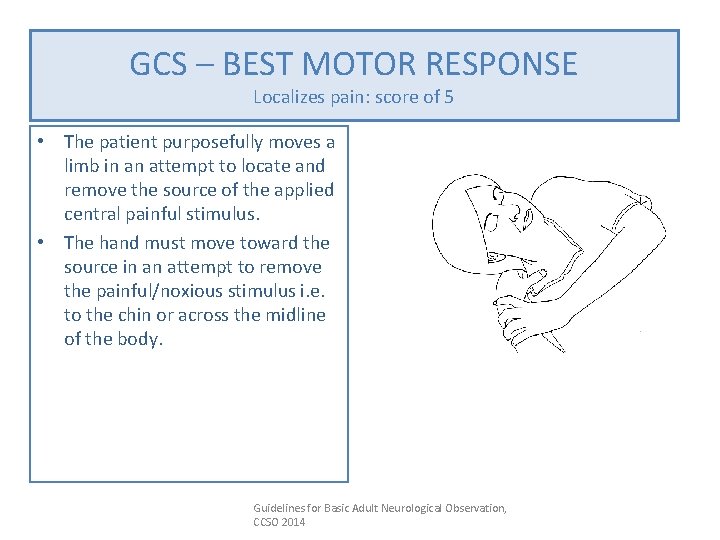
GCS – BEST MOTOR RESPONSE Localizes pain: score of 5 • The patient purposefully moves a limb in an attempt to locate and remove the source of the applied central painful stimulus. • The hand must move toward the source in an attempt to remove the painful/noxious stimulus i. e. to the chin or across the midline of the body. Guidelines for Basic Adult Neurological Observation, CCSO 2014
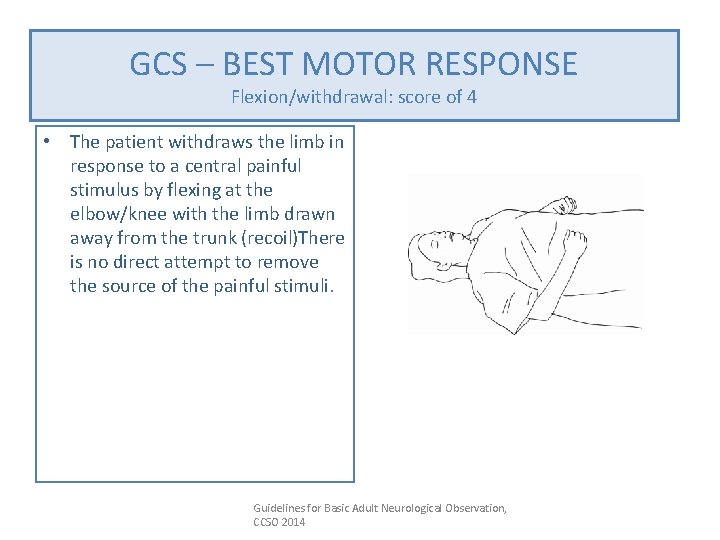
GCS –GCS BEST MOTOR RESPONSE – BEST MOTOR RESPONSE Flexion/withdrawal: score of 4 • The patient withdraws the limb in response to a central painful stimulus by flexing at the elbow/knee with the limb drawn away from the trunk (recoil)There is no direct attempt to remove the source of the painful stimuli. Guidelines for Basic Adult Neurological Observation, CCSO 2014

GCS – BEST MOTOR RESPONSE Abnormal Flexion to Pain: score of 3 • The patient flexes the limb at the elbow in response to central painful stimuli. • Accompanying this movement is shoulder adduction, wrist flexion and the making of a fist. • Flexion to pain is usually a slow movement, with no attempt to remove the painful stimuli. Guidelines for Basic Adult Neurological Observation, CCSO 2014

GCS – BEST MOTOR RESPONSE Extension to pain: score of 2 • The patient extends the limb at the elbow in response to central painful stimuli. • Accompanying this movement is adduction of the shoulder; flexion of the wrist while • the fingers either make a fist or extend. Guidelines for Basic Adult Neurological Observation, CCSO 2014
GCS – BEST MOTOR RESPONSE None: score of 1 No movement of the limbs occurs in response to painful central stimuli. Guidelines for Basic Adult Neurological Observation, CCSO 2014
Pupil Assessment Shape Size Reaction Guidelines for Basic Adult Neurological Observation, CCSO 2014
Shape Why Assess Pupil Shape? • Many neurosurgical patients are at risk of increased ICP. • Early detection of the signs and symptoms may make interventions more effective. • The baseline neurological assessment and ongoing assessments are the best indicators of changing ICP • Subtle neurological changes, such as changes in pupil shape, may indicate rising ICP Guidelines for Basic Adult Neurological Observation, CCSO 2014
Shape Assessing Pupil Shape Normal Ø Pupils should be circular and even in size Normal Variations Ø Older people may have irregular pupil margins Guidelines for Basic Adult Neurological Observation, CCSO 2014
Shape Assessing Pupil Shape Abnormal Ø Oval Ovoid pupils possibly indicate: Ø Sign of increased intracranial pressure Ø Sign of brain herniation Ø Usually seen on the same side as the mass (ipsilateral) Ø The intermediate phase between normal and fully dilated and fixed Guidelines for Basic Adult Neurological Observation, CCSO 2014
Shape Abnormal Pupil Variations Some Abnormal Variations in pupil shapes occur related to: Ø Cataracts and cataract surgery may distort pupil shape Ø Disease processes: glaucoma Ø Trauma or iris inflammation Ø Syndromes, congenital defects Guidelines for Basic Adult Neurological Observation, CCSO 2014
Assessing Pupil Size Ø Size documented in mm Ø Normal range from 2 -6 mm Ø Assess after the eyes have opened and the pupils have accommodated to room light Ø A difference of 1. 5 mm between pupils should be reported to MD Guidelines for Basic Adult Neurological Observation, CCSO 2014
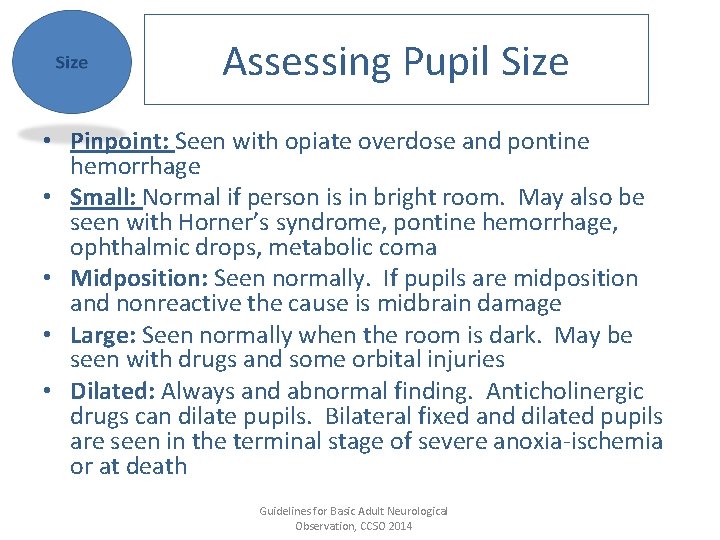
Assessing Pupil Size • Pinpoint: Seen with opiate overdose and pontine hemorrhage • Small: Normal if person is in bright room. May also be seen with Horner’s syndrome, pontine hemorrhage, ophthalmic drops, metabolic coma • Midposition: Seen normally. If pupils are midposition and nonreactive the cause is midbrain damage • Large: Seen normally when the room is dark. May be seen with drugs and some orbital injuries • Dilated: Always and abnormal finding. Anticholinergic drugs can dilate pupils. Bilateral fixed and dilated pupils are seen in the terminal stage of severe anoxia-ischemia or at death Guidelines for Basic Adult Neurological Observation, CCSO 2014
Reaction Assessing Pupil Reaction • Tests the function of cranial nerve lll • Changes in the pupil reaction may be an indicator of a change in intercranial conditions • Direct constriction: Pupil constricts in response to direct light • Consensual constriction: Pupil constricts in response to light directed in opposite eye Guidelines for Basic Adult Neurological Observation, CCSO 2014
Reaction Assessing Pupil Reaction Brisk • Normal finding • Rapid constriction when light source is introduced • Pupils should return to original size when light source removed • There should be a consensual reaction to the light source in the opposite eye Guidelines for Basic Adult Neurological Observation, CCSO 2014
Reaction Assessing Pupil Reaction Sluggish • Constriction occurs but slower than expected • Found in conditions that cause oculomotor nerve compression (CN lll) • Can be caused by increased intracranial pressure, brainstem damage, anoxia or ischemia Guidelines for Basic Adult Neurological Observation, CCSO 2014
Reaction Assessing Pupil Reaction Nonreactive or Fixed • Pupils do not react to bright light • Found in conditions that cause oculomotor nerve compression (CN lll) • Can be caused by increased intracranial pressure, brainstem damage or anoxia • May be a sign of brain death if bilateral Guidelines for Basic Adult Neurological Observation, CCSO 2014
Reaction Assessing Pupil Reaction Documentation: • Record “+” symbol if the pupil reacts • Record “-” symbol if the pupil does not react • Record “C” for closed if the eyelid is swollen shut If the pupils change from baseline or no reaction is observed this may indicate a deterioration in a patient’s condition. Guidelines for Basic Adult Neurological Observation, CCSO 2014
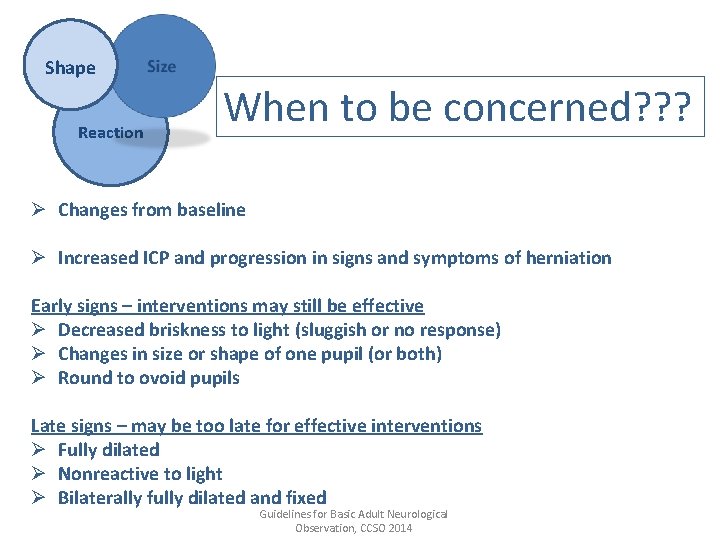
Shape Reaction When to be concerned? ? ? Ø Changes from baseline Ø Increased ICP and progression in signs and symptoms of herniation Early signs – interventions may still be effective Ø Decreased briskness to light (sluggish or no response) Ø Changes in size or shape of one pupil (or both) Ø Round to ovoid pupils Late signs – may be too late for effective interventions Ø Fully dilated Ø Nonreactive to light Ø Bilaterally fully dilated and fixed Guidelines for Basic Adult Neurological Observation, CCSO 2014
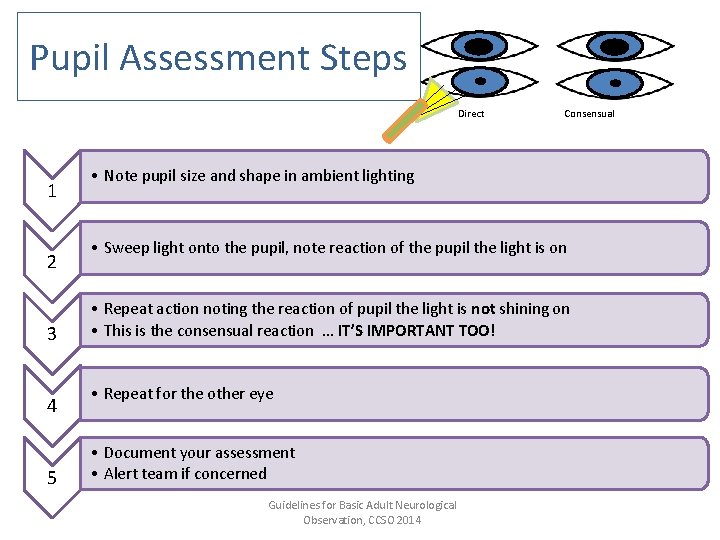
Pupil Assessment Steps Direct 1 2 3 4 5 Consensual • Note pupil size and shape in ambient lighting • Sweep light onto the pupil, note reaction of the pupil the light is on • Repeat action noting the reaction of pupil the light is not shining on • This is the consensual reaction … IT’S IMPORTANT TOO! • Repeat for the other eye • Document your assessment • Alert team if concerned Guidelines for Basic Adult Neurological Observation, CCSO 2014
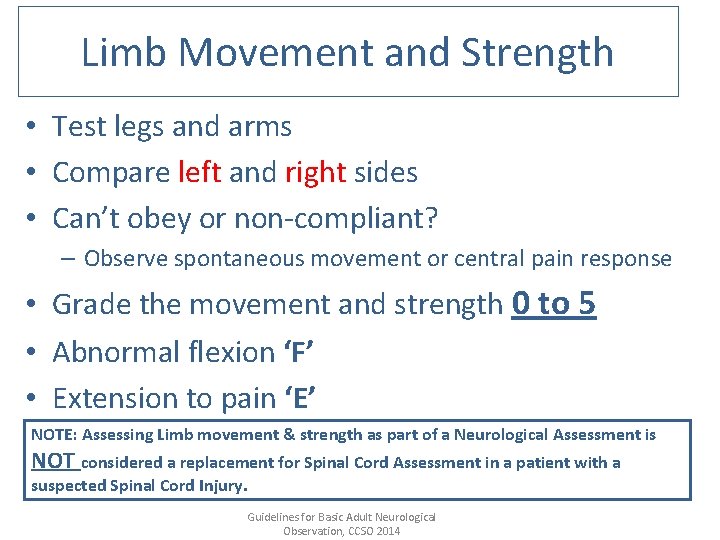
Limb Movement and Strength • Test legs and arms • Compare left and right sides • Can’t obey or non-compliant? – Observe spontaneous movement or central pain response • Grade the movement and strength 0 to 5 • Abnormal flexion ‘F’ • Extension to pain ‘E’ NOTE: Assessing Limb movement & strength as part of a Neurological Assessment is NOT considered a replacement for Spinal Cord Assessment in a patient with a suspected Spinal Cord Injury. Guidelines for Basic Adult Neurological Observation, CCSO 2014
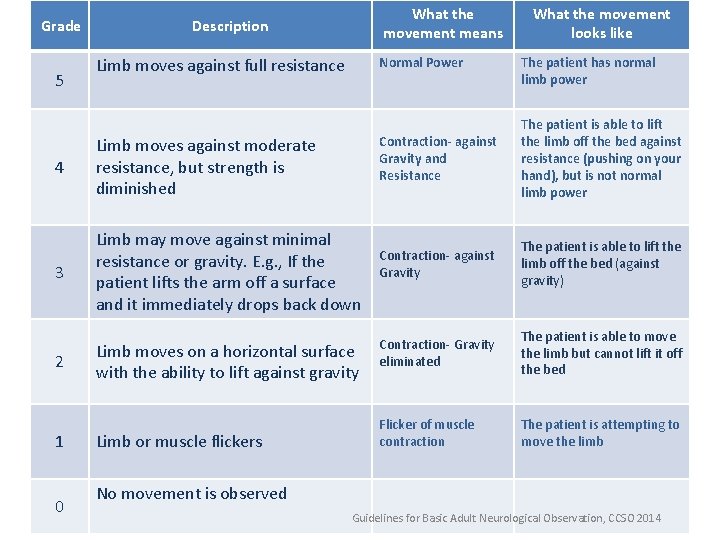
Grade 5 What the movement means Description Limb moves against full resistance Normal Power 4 Limb moves against moderate resistance, but strength is diminished 3 Limb may move against minimal resistance or gravity. E. g. , If the patient lifts the arm off a surface and it immediately drops back down 2 1 0 Limb moves on a horizontal surface with the ability to lift against gravity Limb or muscle flickers What the movement looks like The patient has normal limb power Contraction- against Gravity and Resistance The patient is able to lift the limb off the bed against resistance (pushing on your hand), but is not normal limb power Contraction- against Gravity The patient is able to lift the limb off the bed (against gravity) Contraction- Gravity eliminated The patient is able to move the limb but cannot lift it off the bed Flicker of muscle contraction The patient is attempting to move the limb No movement is observed Guidelines for Basic Adult Neurological Observation, CCSO 2014
Not Applicable for: Ø Spinal Cord Pathology – Use ASIA scoring Ø If unable to assess limb movement/strength due to limb Fractures/Limb Traction. Document not applicable on patient care record, and document reason in interdisciplinary notes Guidelines for Basic Adult Neurological Observation, CCSO 2014
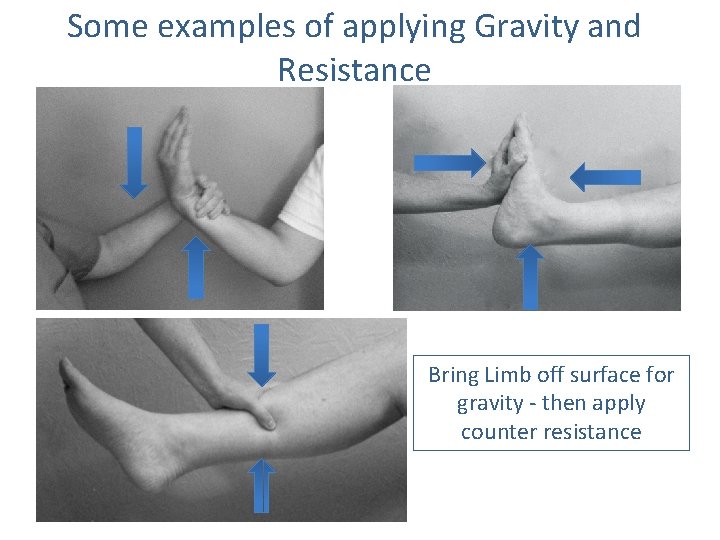
Some examples of applying Gravity and Resistance Bring Limb off surface for gravity - then apply counter resistance
Vital Signs • Increasing fluctuations in vital signs including blood pressure, heart rate and respiratory rate coupled with a deteriorating GCS and Neurological status can indicate rising intercranaial pressure. • This can be a emergency and may need to be addressed IMMEDIATELY!
Vital Signs • Documentation of the vital signs with GCS, pupil response, and limb movement completes the patient picture and should be documented as frequently as the performing of the neurological assessment. Guidelines for Basic Adult Neurological Observation, CCSO 2014

In Summary…. . A complete Neurological Assessment includes the assessment and documentation of the following: • Level of consciousness (LOC) using the Glasgow Coma Scale (GCS) • Pupillary Response • Limb Movement/ Strength • Vital signs Guidelines for Basic Adult Neurological Observation, CCSO 2014
- Slides: 44