Group C Problems priorities 1 2 Establishment of

Group C
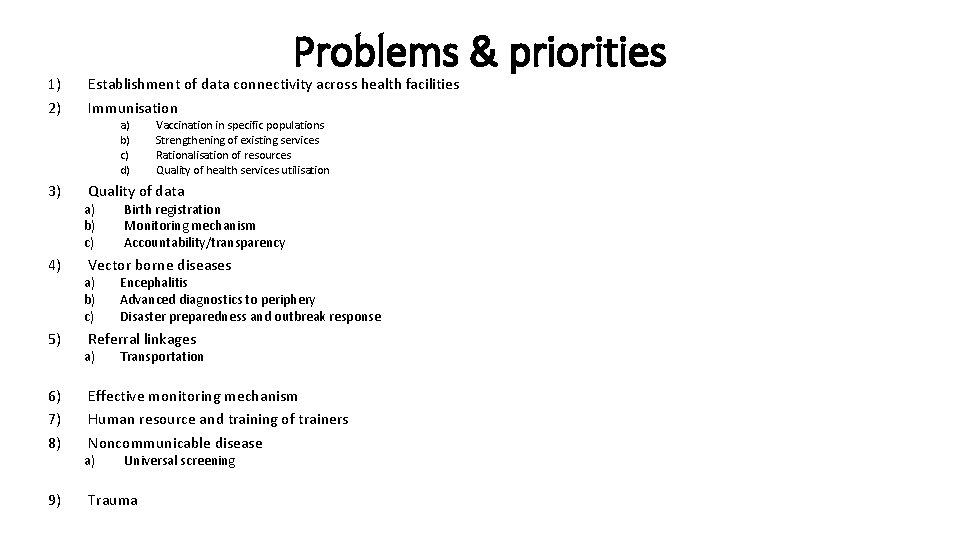
Problems & priorities 1) 2) Establishment of data connectivity across health facilities Immunisation 3) Quality of data 4) 5) 6) 7) 8) 9) a) b) c) d) a) b) c) Vaccination in specific populations Strengthening of existing services Rationalisation of resources Quality of health services utilisation Birth registration Monitoring mechanism Accountability/transparency Vector borne diseases a) b) c) Encephalitis Advanced diagnostics to periphery Disaster preparedness and outbreak response Referral linkages a) Transportation Effective monitoring mechanism Human resource and training of trainers Noncommunicable disease a) Universal screening Trauma
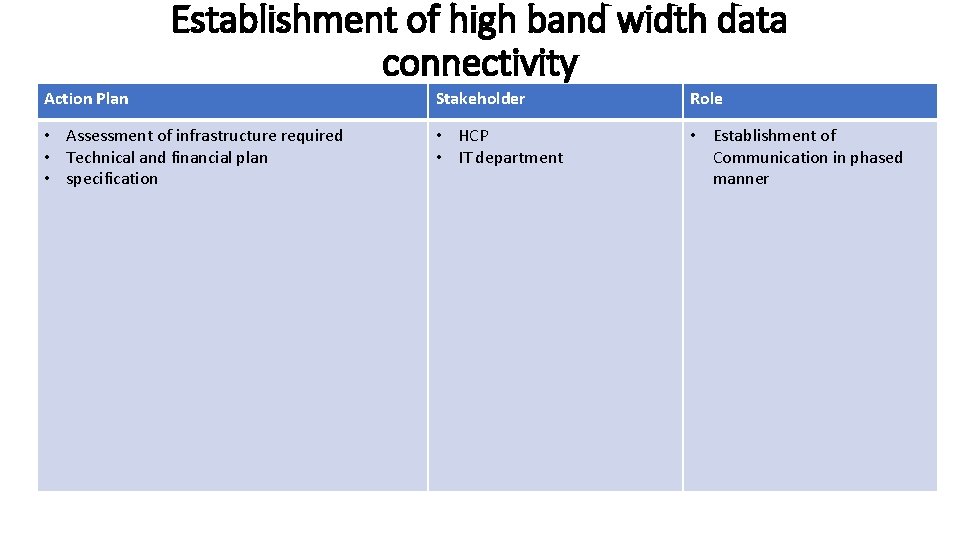
Establishment of high band width data connectivity Action Plan Stakeholder Role • Assessment of infrastructure required • Technical and financial plan • specification • HCP • IT department • Establishment of Communication in phased manner
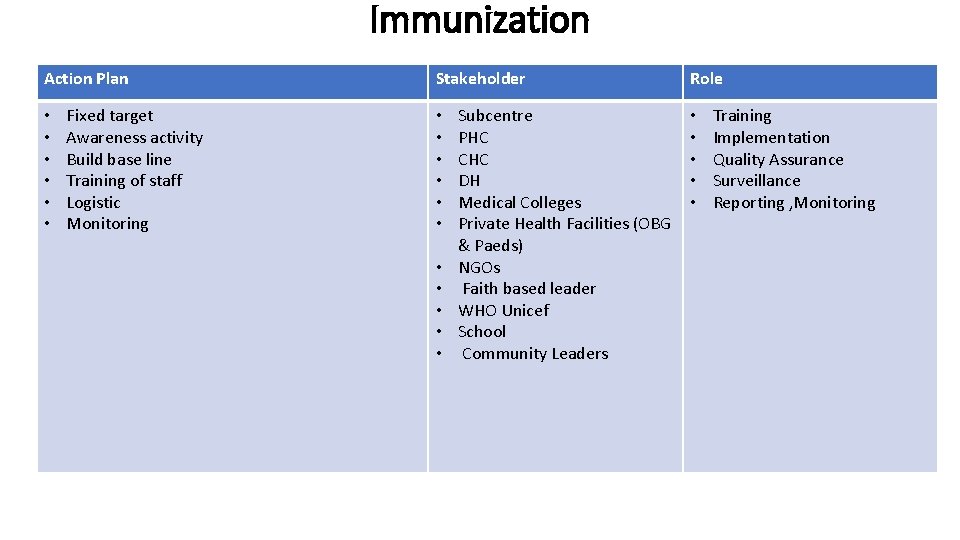
Immunization Action Plan • • • Fixed target Awareness activity Build base line Training of staff Logistic Monitoring Stakeholder • • • Subcentre PHC CHC DH Medical Colleges Private Health Facilities (OBG & Paeds) NGOs Faith based leader WHO Unicef School Community Leaders Role • • • Training Implementation Quality Assurance Surveillance Reporting , Monitoring
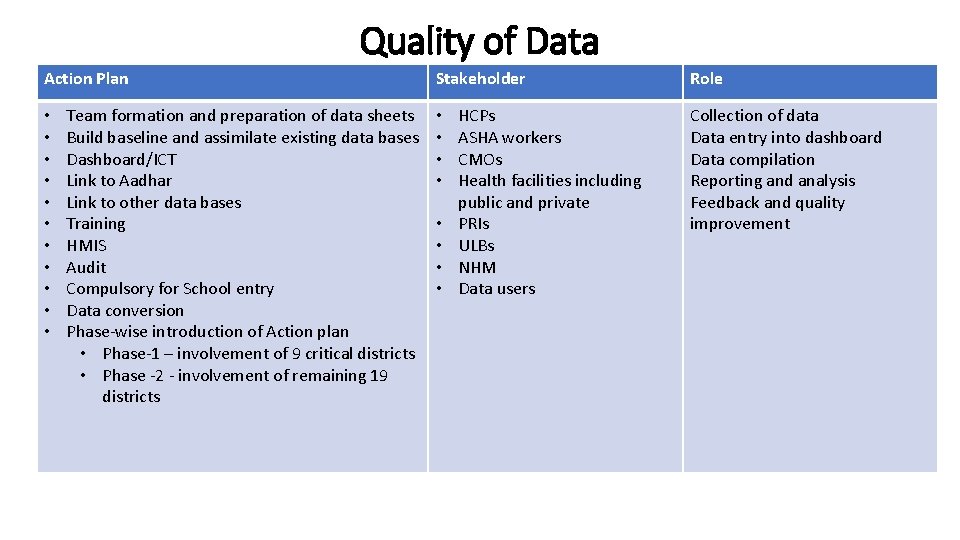
Quality of Data Action Plan • • • Team formation and preparation of data sheets Build baseline and assimilate existing data bases Dashboard/ICT Link to Aadhar Link to other data bases Training HMIS Audit Compulsory for School entry Data conversion Phase-wise introduction of Action plan • Phase-1 – involvement of 9 critical districts • Phase -2 - involvement of remaining 19 districts Stakeholder • • HCPs ASHA workers CMOs Health facilities including public and private PRIs ULBs NHM Data users Role Collection of data Data entry into dashboard Data compilation Reporting and analysis Feedback and quality improvement
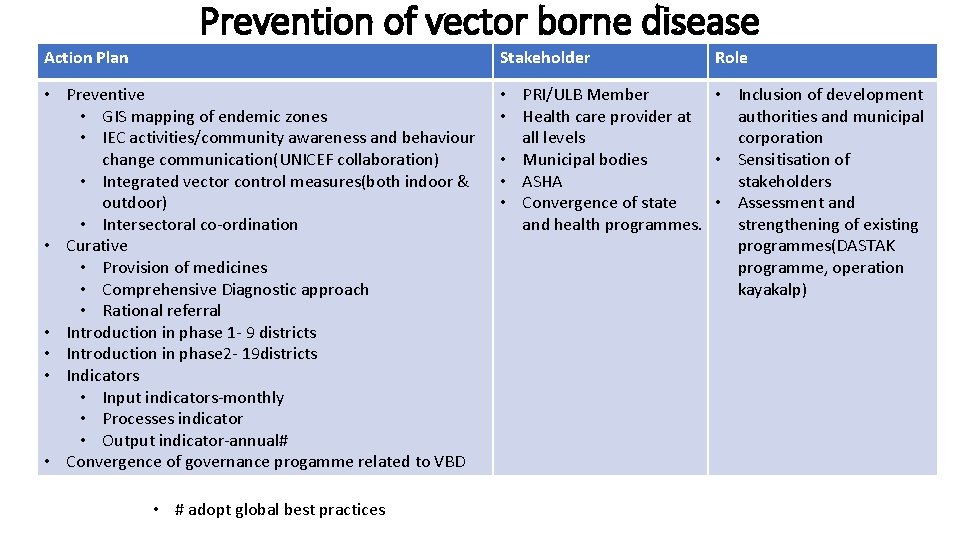
Prevention of vector borne disease Action Plan Stakeholder • Preventive • GIS mapping of endemic zones • IEC activities/community awareness and behaviour change communication(UNICEF collaboration) • Integrated vector control measures(both indoor & outdoor) • Intersectoral co-ordination • Curative • Provision of medicines • Comprehensive Diagnostic approach • Rational referral • Introduction in phase 1 - 9 districts • Introduction in phase 2 - 19 districts • Indicators • Input indicators-monthly • Processes indicator • Output indicator-annual# • Convergence of governance progamme related to VBD • PRI/ULB Member • Inclusion of development • Health care provider at authorities and municipal all levels corporation • Municipal bodies • Sensitisation of • ASHA stakeholders • Convergence of state • Assessment and health programmes. strengthening of existing programmes(DASTAK programme, operation kayakalp) • # adopt global best practices Role
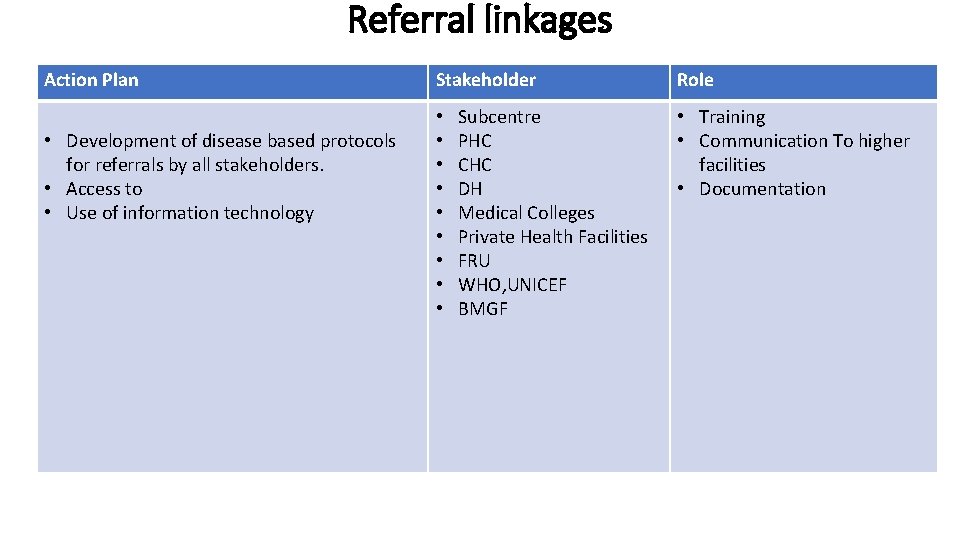
Referral linkages Action Plan • Development of disease based protocols for referrals by all stakeholders. • Access to • Use of information technology Stakeholder • • • Subcentre PHC CHC DH Medical Colleges Private Health Facilities FRU WHO, UNICEF BMGF Role • Training • Communication To higher facilities • Documentation
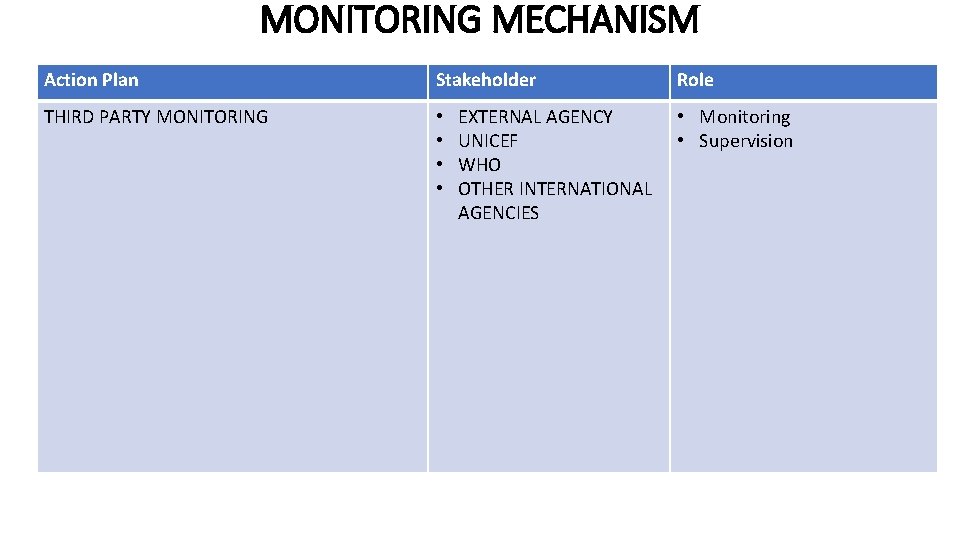
MONITORING MECHANISM Action Plan Stakeholder THIRD PARTY MONITORING • • EXTERNAL AGENCY UNICEF WHO OTHER INTERNATIONAL AGENCIES Role • Monitoring • Supervision
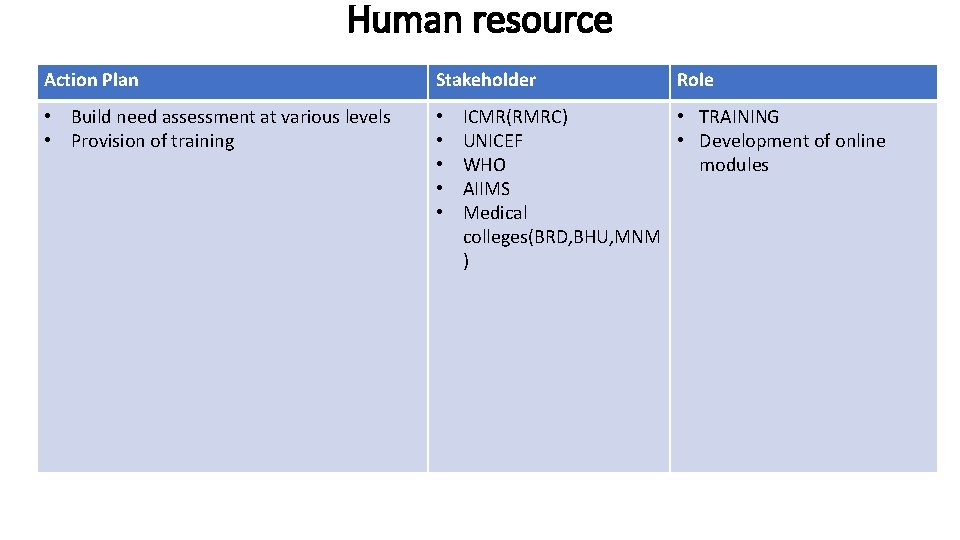
Human resource Action Plan Stakeholder • Build need assessment at various levels • Provision of training • • • Role ICMR(RMRC) • TRAINING UNICEF • Development of online WHO modules AIIMS Medical colleges(BRD, BHU, MNM )
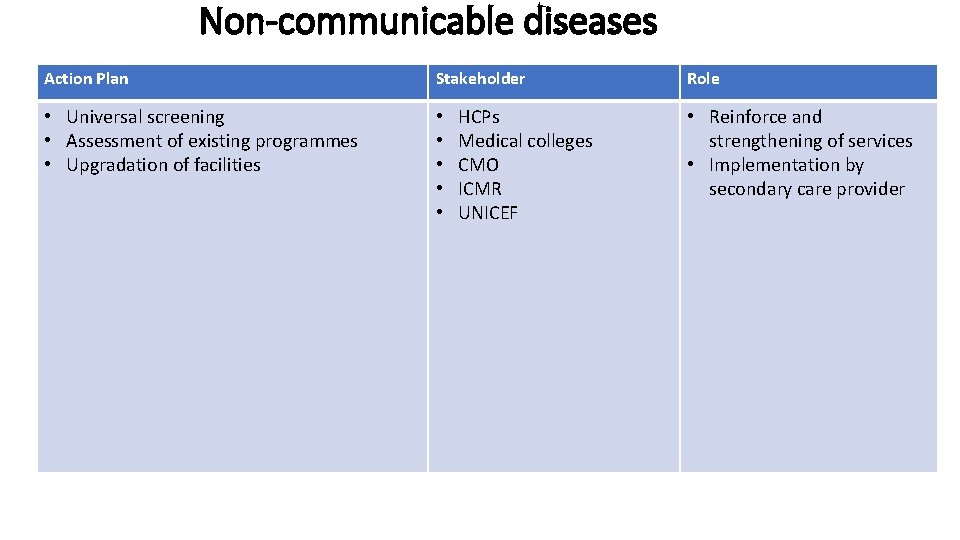
Non-communicable diseases Action Plan Stakeholder • Universal screening • Assessment of existing programmes • Upgradation of facilities • • • HCPs Medical colleges CMO ICMR UNICEF Role • Reinforce and strengthening of services • Implementation by secondary care provider
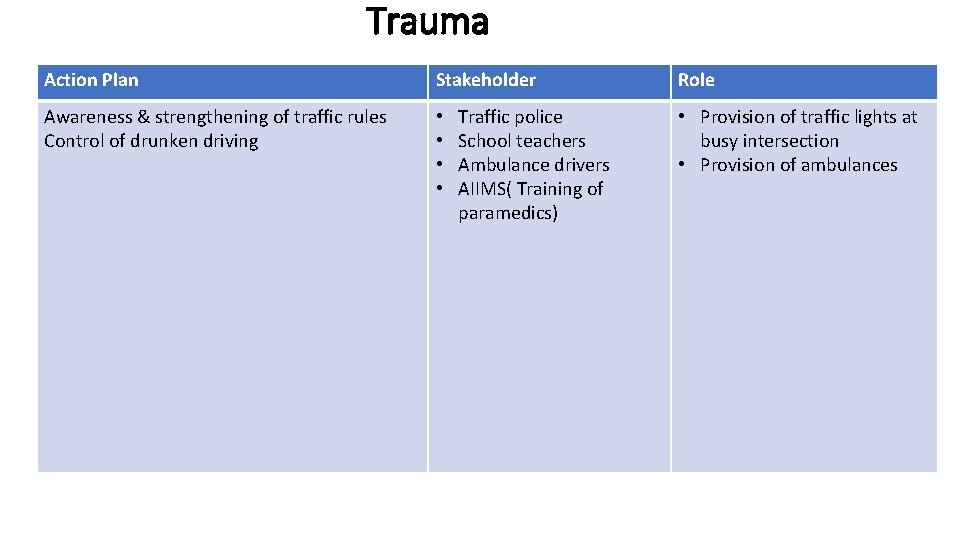
Trauma Action Plan Stakeholder Awareness & strengthening of traffic rules Control of drunken driving • • Traffic police School teachers Ambulance drivers AIIMS( Training of paramedics) Role • Provision of traffic lights at busy intersection • Provision of ambulances
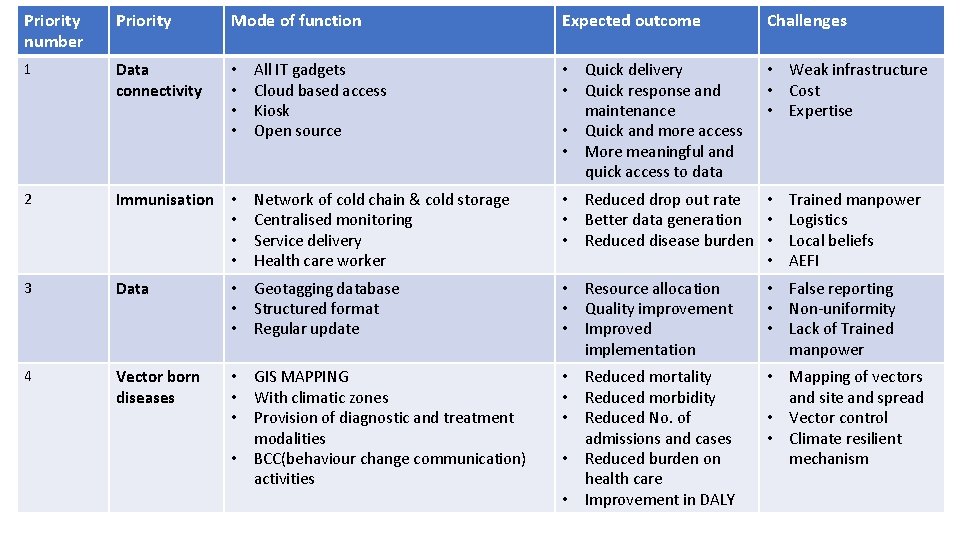
Priority number Priority Mode of function Expected outcome Challenges 1 Data connectivity • • All IT gadgets Cloud based access Kiosk Open source • Quick delivery • Quick response and maintenance • Quick and more access • More meaningful and quick access to data • Weak infrastructure • Cost • Expertise 2 Immunisation • • Network of cold chain & cold storage Centralised monitoring Service delivery Health care worker • Reduced drop out rate • Trained manpower • Better data generation • Logistics • Reduced disease burden • Local beliefs • AEFI 3 Data • Geotagging database • Structured format • Regular update • Resource allocation • Quality improvement • Improved implementation • False reporting • Non-uniformity • Lack of Trained manpower 4 Vector born diseases • GIS MAPPING • With climatic zones • Provision of diagnostic and treatment modalities • BCC(behaviour change communication) activities • Reduced mortality • Reduced morbidity • Reduced No. of admissions and cases • Reduced burden on health care • Improvement in DALY • Mapping of vectors and site and spread • Vector control • Climate resilient mechanism
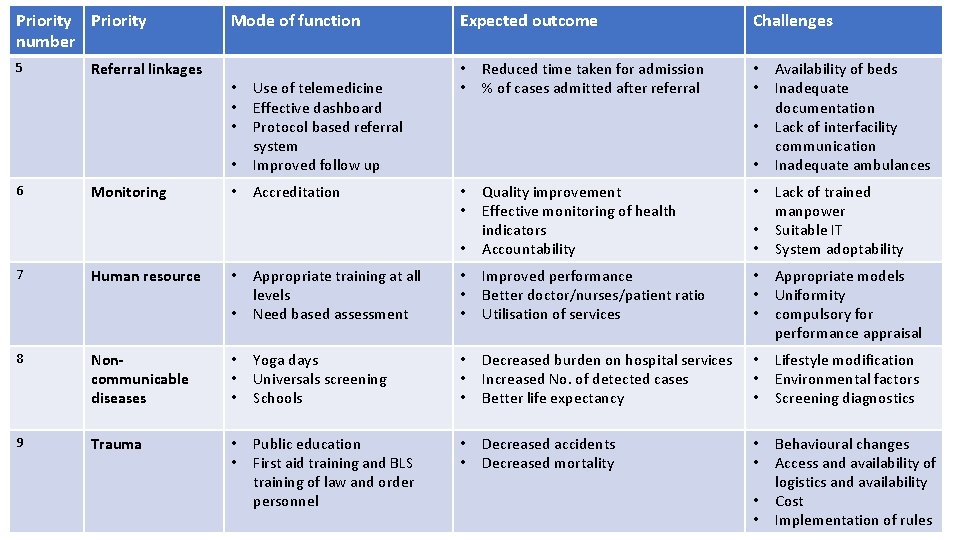
Priority number 5 6 7 Referral linkages Monitoring Human resource Mode of function • Use of telemedicine Effective dashboard Protocol based referral system Improved follow up • Accreditation • • • Expected outcome • • Reduced time taken for admission % of cases admitted after referral Challenges • • Availability of beds Inadequate documentation Lack of interfacility communication Inadequate ambulances • • Quality improvement Effective monitoring of health indicators Accountability • Appropriate training at all levels Need based assessment • • • Improved performance Better doctor/nurses/patient ratio Utilisation of services • • • Appropriate models Uniformity compulsory for performance appraisal • • • Lack of trained manpower Suitable IT System adoptability 8 Noncommunicable diseases • • • Yoga days Universals screening Schools • • • Decreased burden on hospital services Increased No. of detected cases Better life expectancy • • • Lifestyle modification Environmental factors Screening diagnostics 9 Trauma • • Public education First aid training and BLS training of law and order personnel • • Decreased accidents Decreased mortality • • Behavioural changes Access and availability of logistics and availability Cost Implementation of rules • •
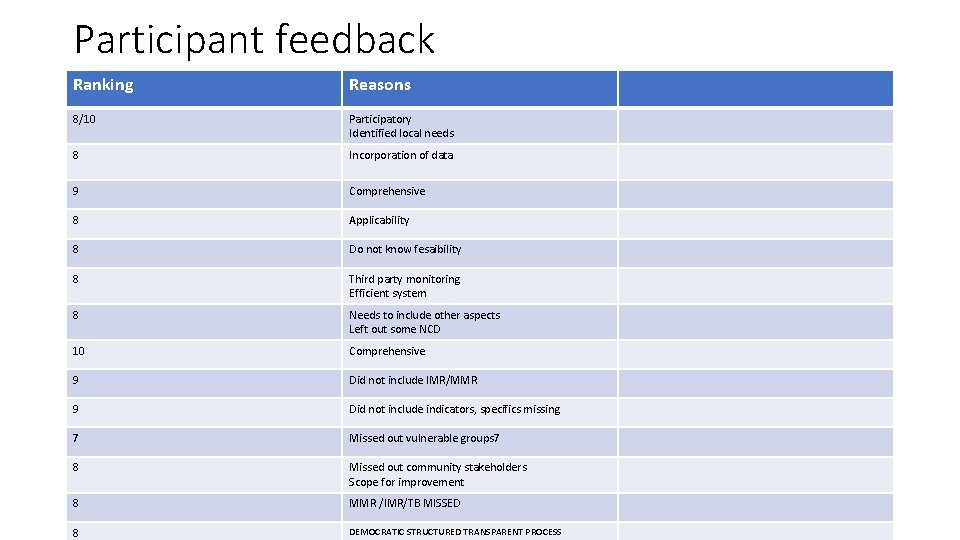
Participant feedback Ranking Reasons 8/10 Participatory Identified local needs 8 Incorporation of data 9 Comprehensive 8 Applicability 8 Do not know fesaibility 8 Third party monitoring Efficient system 8 Needs to include other aspects Left out some NCD 10 Comprehensive 9 Did not include IMR/MMR 9 Did not include indicators, specifics missing 7 Missed out vulnerable groups 7 8 Missed out community stakeholders Scope for improvement 8 MMR /IMR/TB MISSED 8 DEMOCRATIC STRUCTURED TRANSPARENT PROCESS
- Slides: 14