Group B Strep in Pregnancy Why screen for
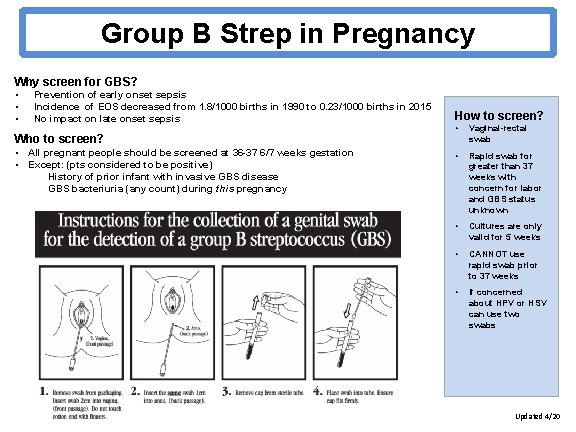
Group B Strep in Pregnancy Why screen for GBS? • • • Prevention of early onset sepsis Incidence of EOS decreased from 1. 8/1000 births in 1990 to 0. 23/1000 births in 2015 No impact on late onset sepsis Who to screen? • • All pregnant people should be screened at 36 -37 6/7 weeks gestation Except: (pts considered to be positive) History of prior infant with invasive GBS disease GBS bacteriuria (any count) during this pregnancy How to screen? • Vaginal-rectal swab • Rapid swab for greater than 37 weeks with concern for labor and GBS status unknown • Cultures are only valid for 5 weeks • CANNOT use rapid swab prior to 37 weeks • If concerned about HPV or HSV can use two swabs Updated 4/20

Group B Strep in Pregnancy Who to treat during labor? • • Intrapartum prophylaxis with antibiotics indicated if: History of prior infant with invasive GBS disease Positive GBS in urine culture this pregnancy Unknown GBS plus less than 37 weeks gestation hx of GBS previous pregnancy SROM > 18 hours or fever greater than 100 (as part of treatment for chorioamnionitis) Not indicated for scheduled C-section without SROM or labor What if there is true penicillin allergy? • • During prenatal care, assess risk for anaphylaxis with PCN- high risk if prior urticaria, wheezing, angioedema or anaphylaxis Low risk- treat with cefazolin High risk- need to order sensitivities for erythromycin and clindamycin If susceptible to both- treat with clindamycin If resistant to either or unknown- treat with vancomycin Note anaphylaxis risk, sensitivities, and antibiotic plan in problem list What is adequate treatment? • IV antibiotic administered at least 4 hours prior to delivery Medications Options are in your L&D Admit Powerplan! Penicillin 5 million units IV loading, then 2. 5 million units IV q 4 h Cefazolin 2 g IV loading, then 1 g IV q 8 h Clindamycin 900 mg IV q 8 h Vancomycin 1 g IV q 12 h
- Slides: 2