GRAND ROUNDS Denise A John VEI 1192007 Case




- Slides: 33
GRAND ROUNDS Denise A. John VEI 1/19/2007
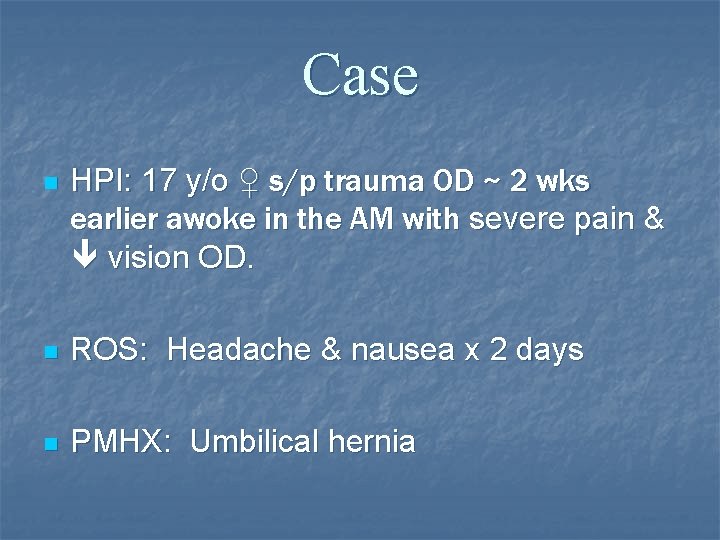
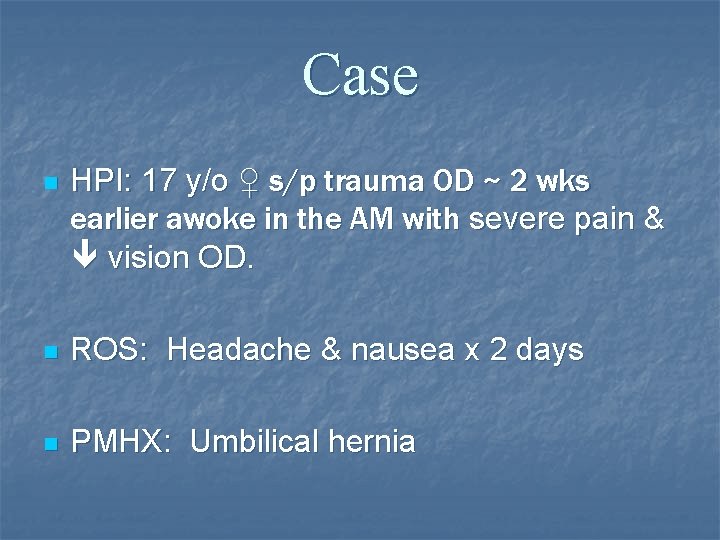
Case n HPI: 17 y/o ♀ s/p trauma OD ~ 2 wks earlier awoke in the AM with severe pain & vision OD. n ROS: Headache & nausea x 2 days n PMHX: Umbilical hernia
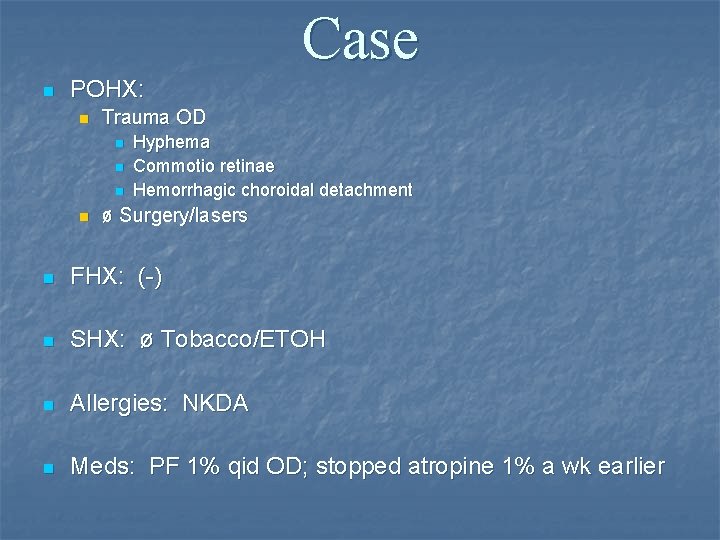
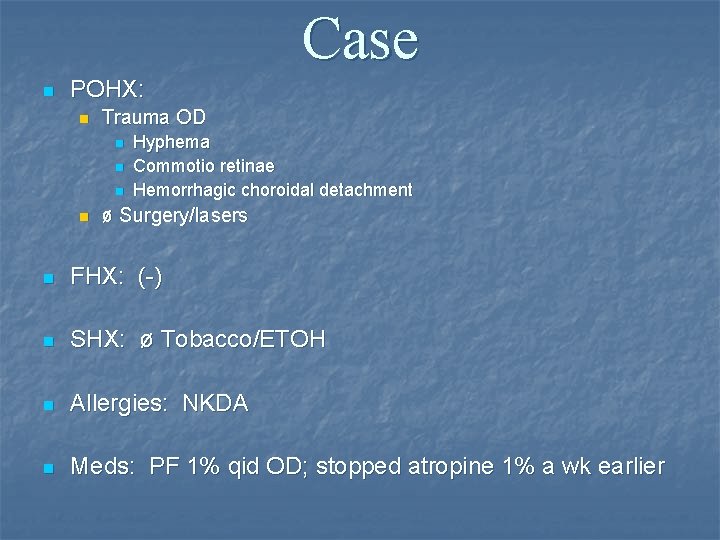
Case n POHX: n Trauma OD n n Hyphema Commotio retinae Hemorrhagic choroidal detachment ø Surgery/lasers n FHX: (-) n SHX: ø Tobacco/ETOH n Allergies: NKDA n Meds: PF 1% qid OD; stopped atropine 1% a wk earlier
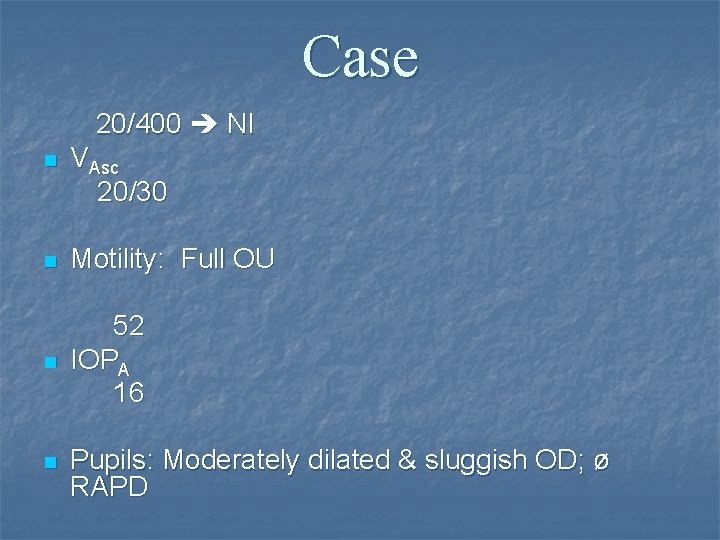
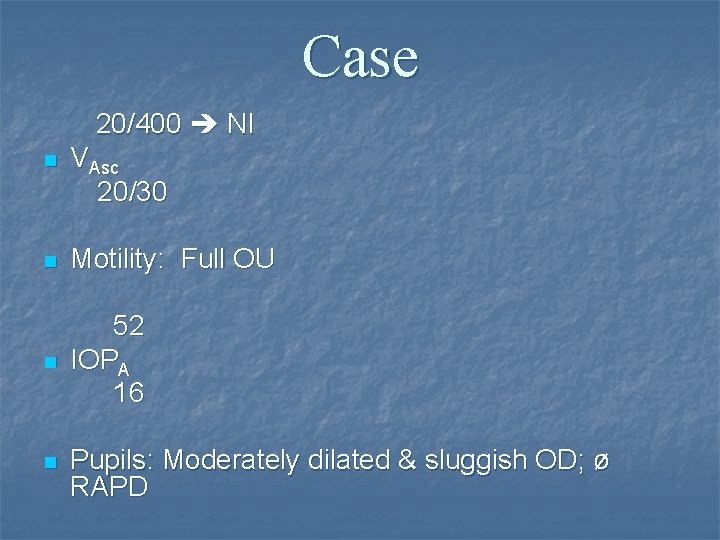
Case 20/400 NI n VAsc 20/30 n Motility: Full OU n 52 IOPA 16 n Pupils: Moderately dilated & sluggish OD; ø RAPD
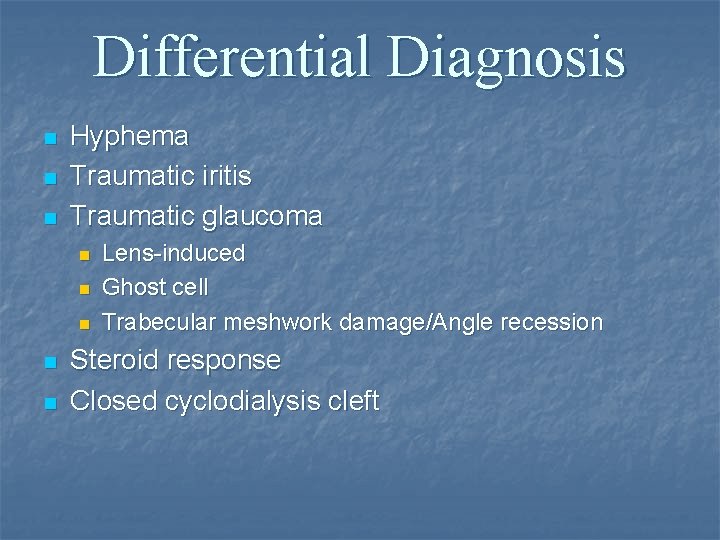
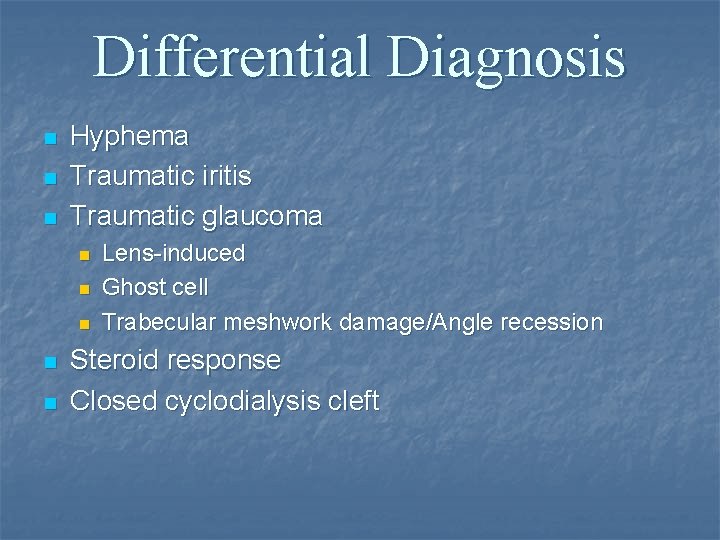
Differential Diagnosis n n n Hyphema Traumatic iritis Traumatic glaucoma n n n Lens-induced Ghost cell Trabecular meshwork damage/Angle recession Steroid response Closed cyclodialysis cleft
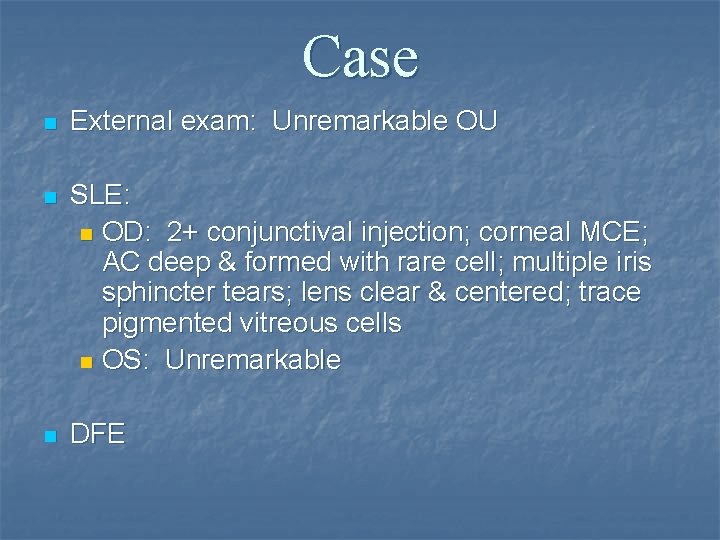
Case n External exam: Unremarkable OU n SLE: n OD: 2+ conjunctival injection; corneal MCE; AC deep & formed with rare cell; multiple iris sphincter tears; lens clear & centered; trace pigmented vitreous cells n OS: Unremarkable n DFE



Summary n Recent history of blunt trauma OD with period of IOP with the development of a hemorrhagic choroidal detachment, optic disc edema, retinal venous engorgement & macular striae now with IOP. n What is your diagnosis?
What would you like to do next?

Case n Assessment: n Spontaneous closure of a cyclodialysis cleft with IOP n Plan: n n n IOP to 32 (alphagan/cosopt/diamox) in clinic Sent home on glaucoma gtts/diamox/PF & atropine F/u 3 days
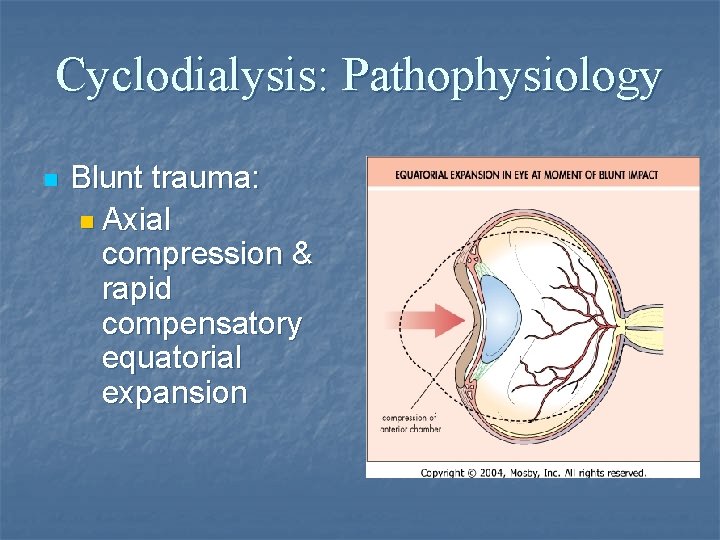
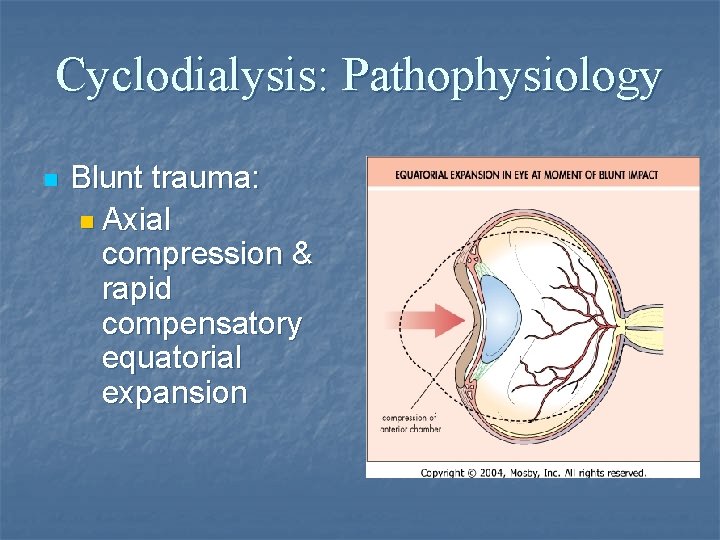
Cyclodialysis: Pathophysiology n Blunt trauma: n Axial compression & rapid compensatory equatorial expansion
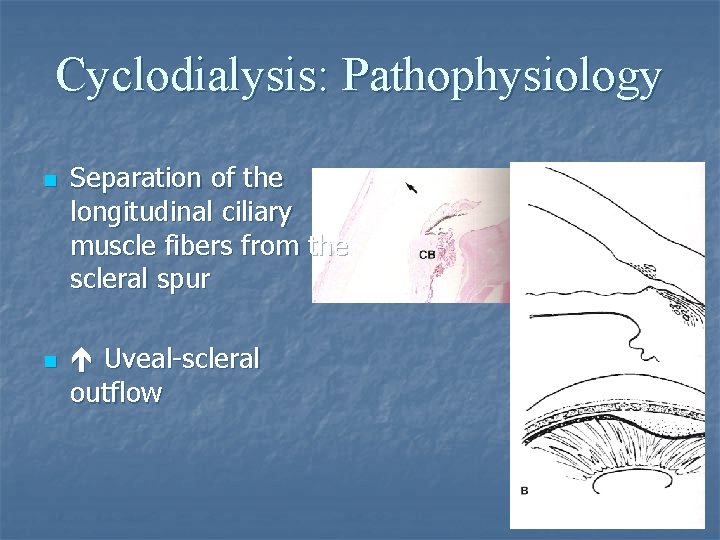
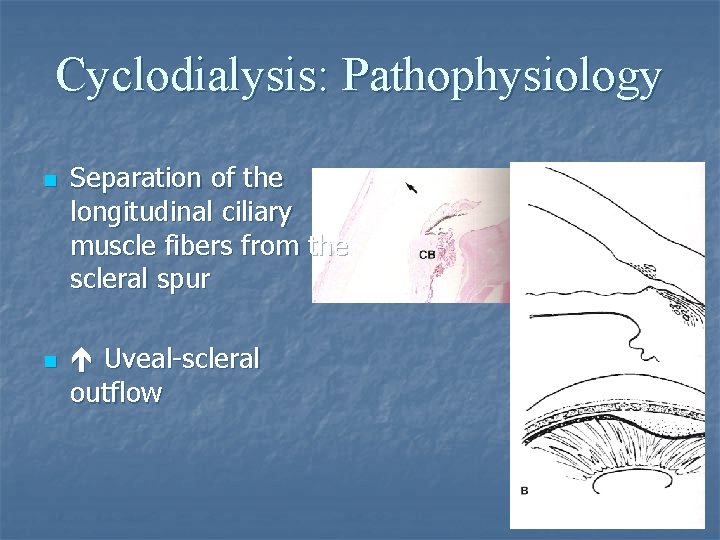
Cyclodialysis: Pathophysiology n n Separation of the longitudinal ciliary muscle fibers from the scleral spur Uveal-scleral outflow
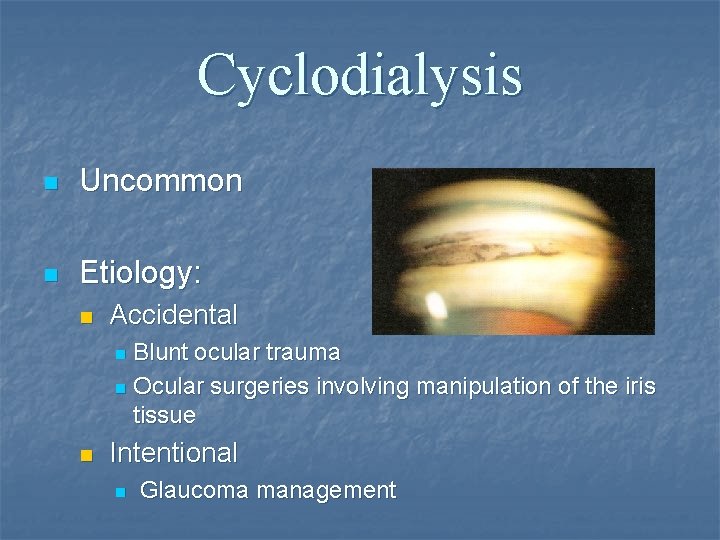
Cyclodialysis n Uncommon n Etiology: n Accidental Blunt ocular trauma n Ocular surgeries involving manipulation of the iris tissue n n Intentional n Glaucoma management
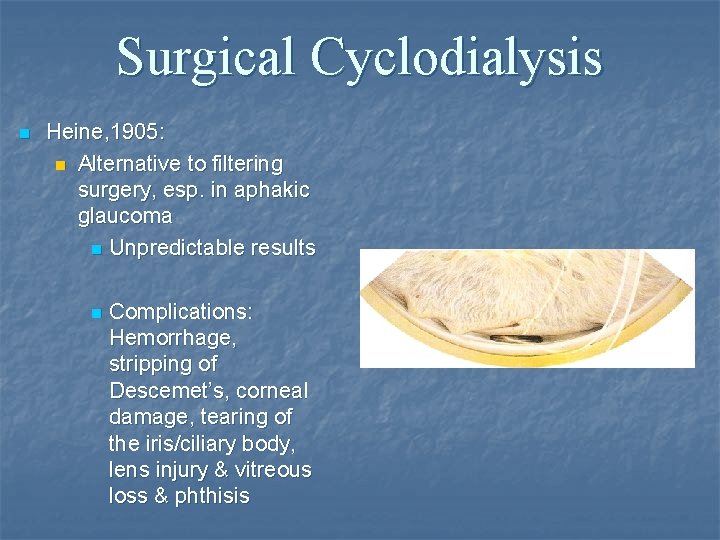
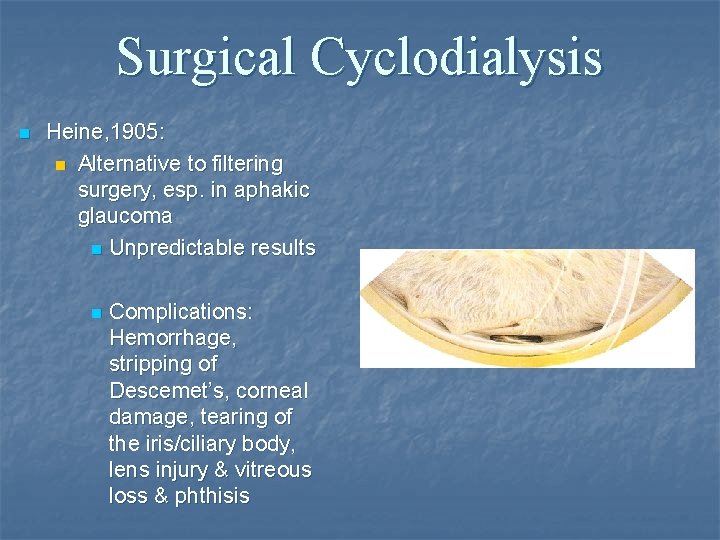
Surgical Cyclodialysis n Heine, 1905: n Alternative to filtering surgery, esp. in aphakic glaucoma n Unpredictable results n Complications: Hemorrhage, stripping of Descemet’s, corneal damage, tearing of the iris/ciliary body, lens injury & vitreous loss & phthisis
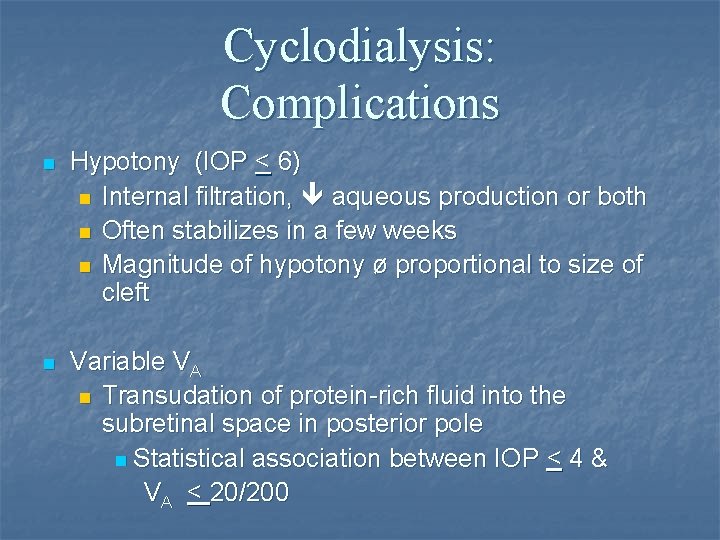
Cyclodialysis: Complications n Hypotony (IOP < 6) n Internal filtration, aqueous production or both n Often stabilizes in a few weeks n Magnitude of hypotony ø proportional to size of cleft n Variable VA n Transudation of protein-rich fluid into the subretinal space in posterior pole n Statistical association between IOP < 4 & VA < 20/200
Cyclodialysis: Complications n n n n Shallow AC Induced hyperopia Cataract Choroidal effusion Retinal & choroidal folds Engorgement & stasis of retinal veins CME Optic disc edema
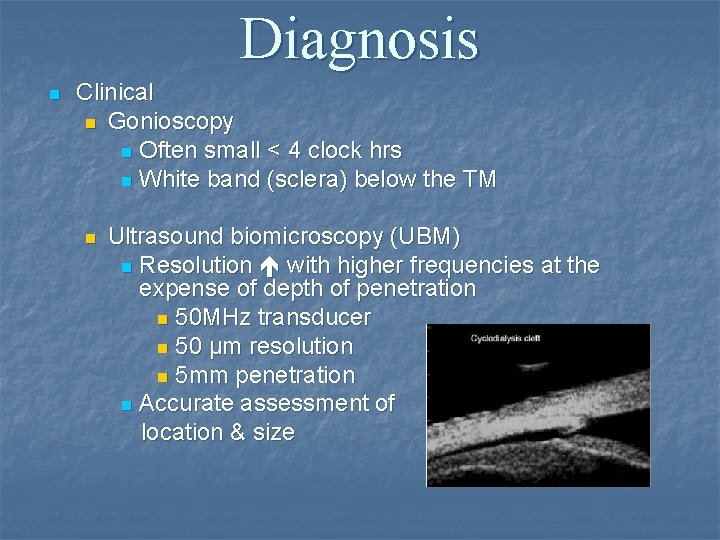
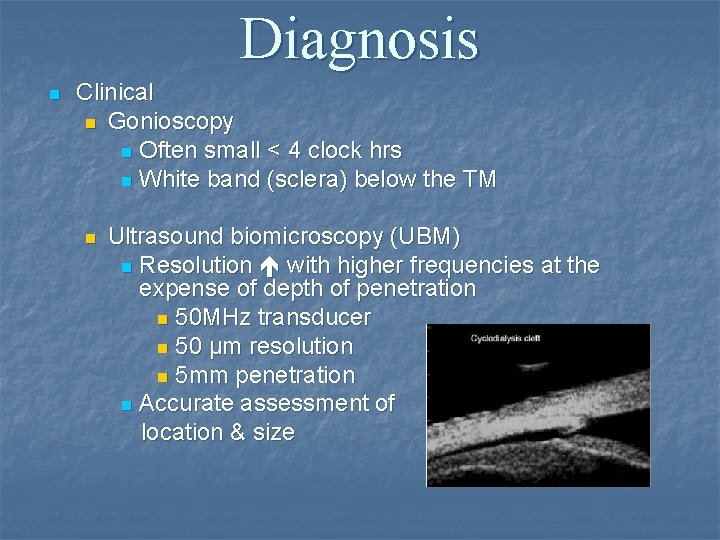
Diagnosis n Clinical n Gonioscopy n Often small < 4 clock hrs n White band (sclera) below the TM n Ultrasound biomicroscopy (UBM) n Resolution with higher frequencies at the expense of depth of penetration n 50 MHz transducer n 50 μm resolution n 5 mm penetration n Accurate assessment of location & size
Cyclodialysis: Management n Goal: Reverse hypotony n Indications for treatment: Hypotonous maculopathy + disc edema n Macular folds n Choroidal detachment n Corneal edema + worsening vision n
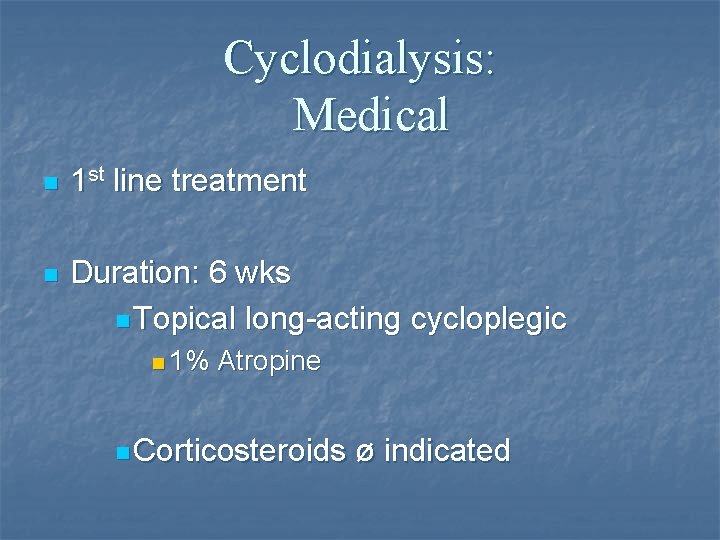
Cyclodialysis: Medical n 1 st line treatment n Duration: 6 wks n Topical long-acting cycloplegic n 1% Atropine n Corticosteroids ø indicated
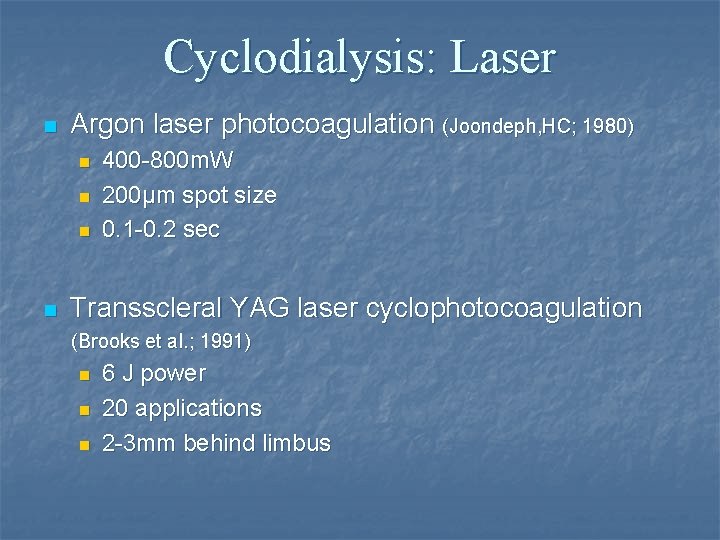
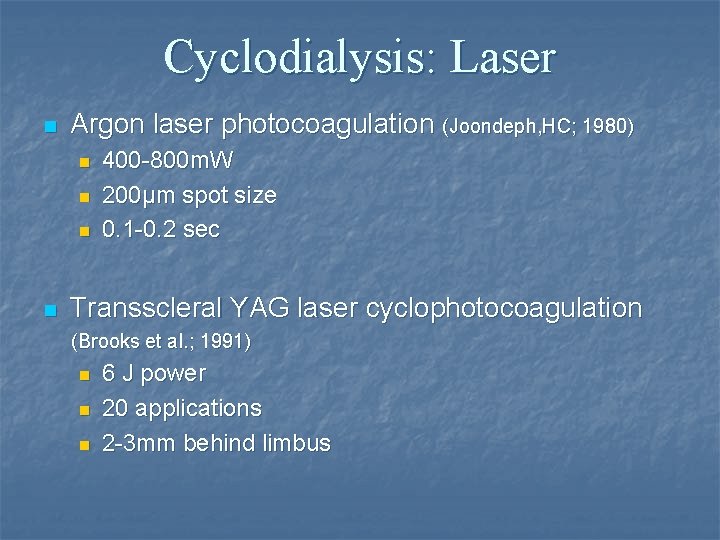
Cyclodialysis: Laser n Argon laser photocoagulation (Joondeph, HC; 1980) n n 400 -800 m. W 200μm spot size 0. 1 -0. 2 sec Transscleral YAG laser cyclophotocoagulation (Brooks et al. ; 1991) n n n 6 J power 20 applications 2 -3 mm behind limbus
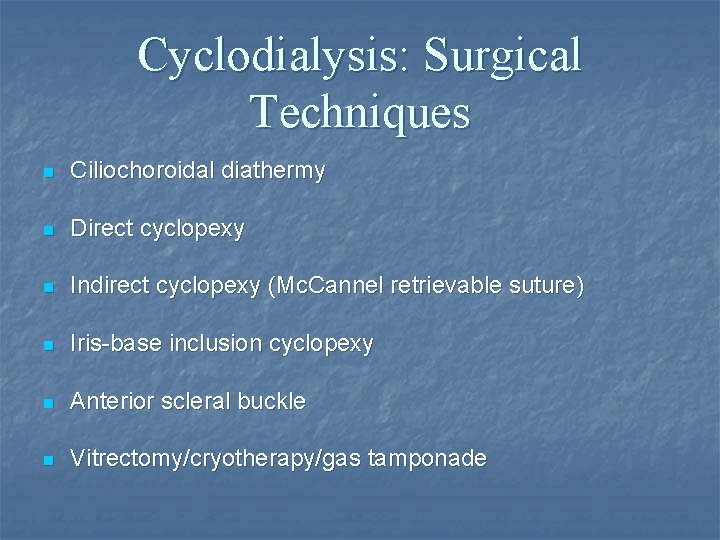
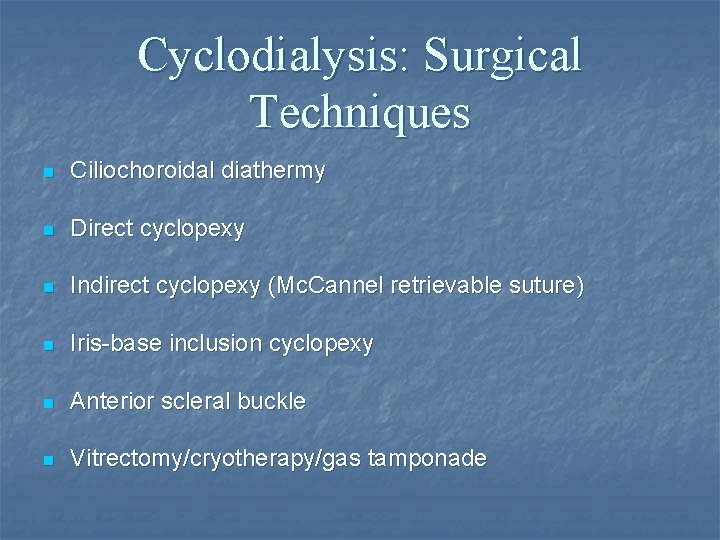
Cyclodialysis: Surgical Techniques n Ciliochoroidal diathermy n Direct cyclopexy n Indirect cyclopexy (Mc. Cannel retrievable suture) n Iris-base inclusion cyclopexy n Anterior scleral buckle n Vitrectomy/cryotherapy/gas tamponade
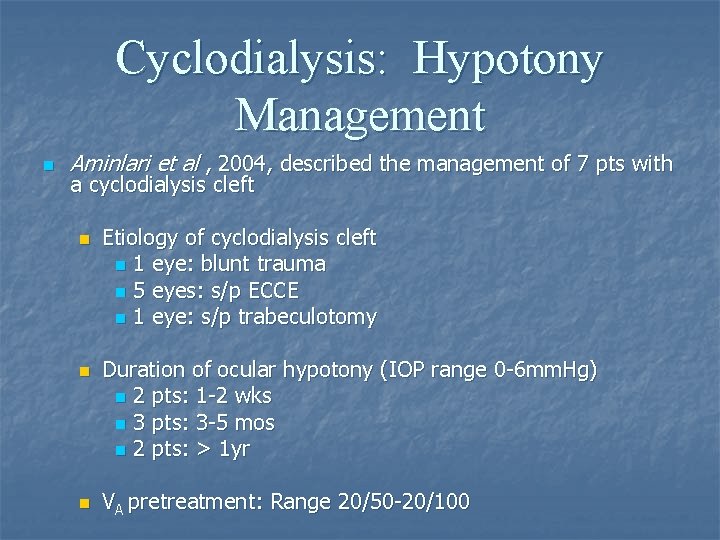
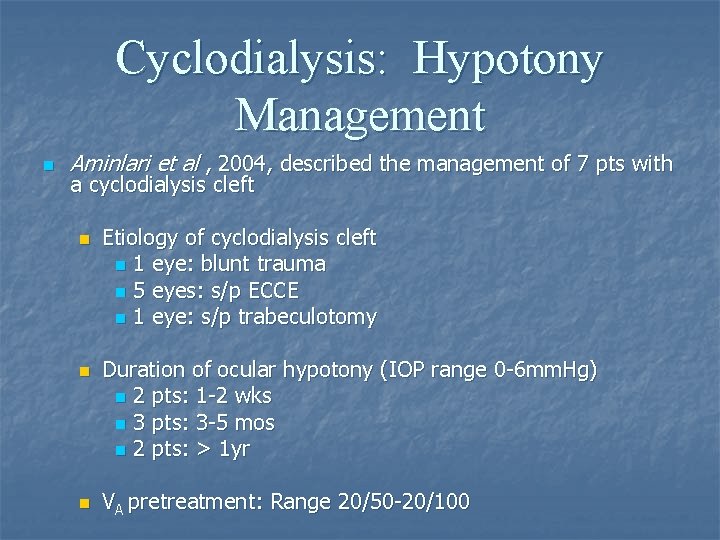
Cyclodialysis: Hypotony Management n Aminlari et al , 2004, described the management of 7 pts with a cyclodialysis cleft n n n Etiology of cyclodialysis cleft n 1 eye: blunt trauma n 5 eyes: s/p ECCE n 1 eye: s/p trabeculotomy Duration of ocular hypotony (IOP range 0 -6 mm. Hg) n 2 pts: 1 -2 wks n 3 pts: 3 -5 mos n 2 pts: > 1 yr VA pretreatment: Range 20/50 -20/100
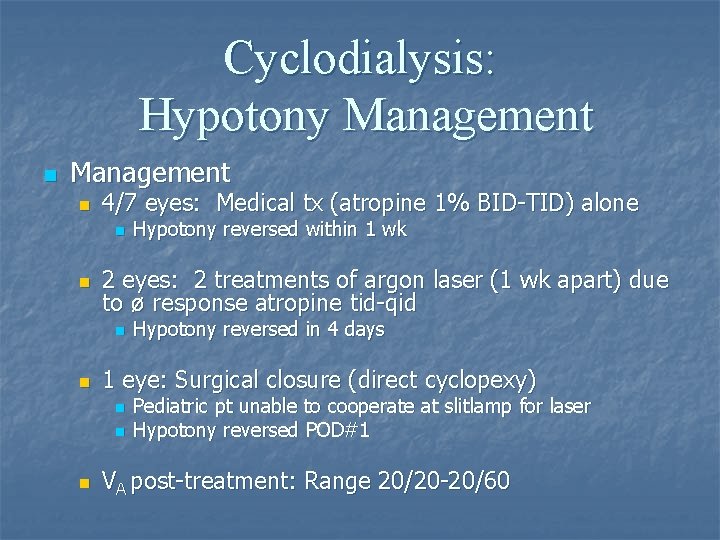
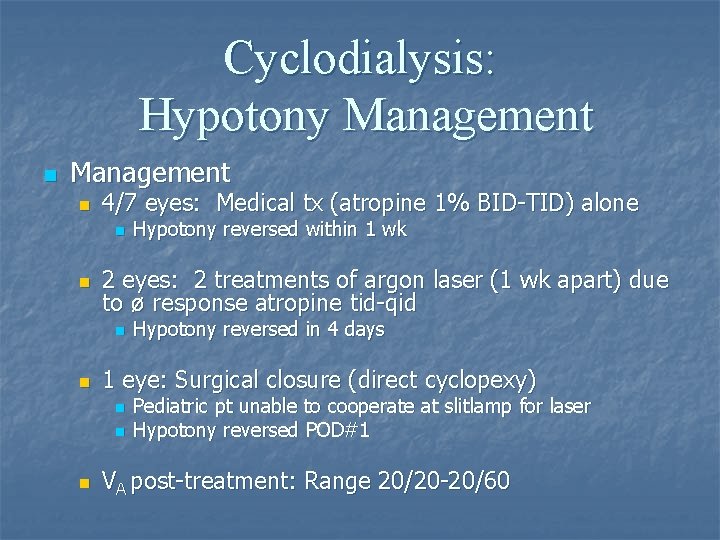
Cyclodialysis: Hypotony Management n 4/7 eyes: Medical tx (atropine 1% BID-TID) alone n n 2 eyes: 2 treatments of argon laser (1 wk apart) due to ø response atropine tid-qid n n Hypotony reversed in 4 days 1 eye: Surgical closure (direct cyclopexy) n n n Hypotony reversed within 1 wk Pediatric pt unable to cooperate at slitlamp for laser Hypotony reversed POD#1 VA post-treatment: Range 20/20 -20/60
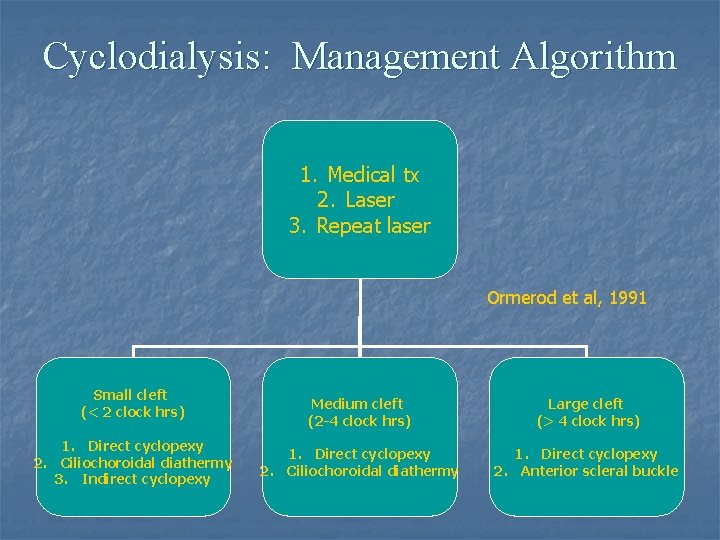
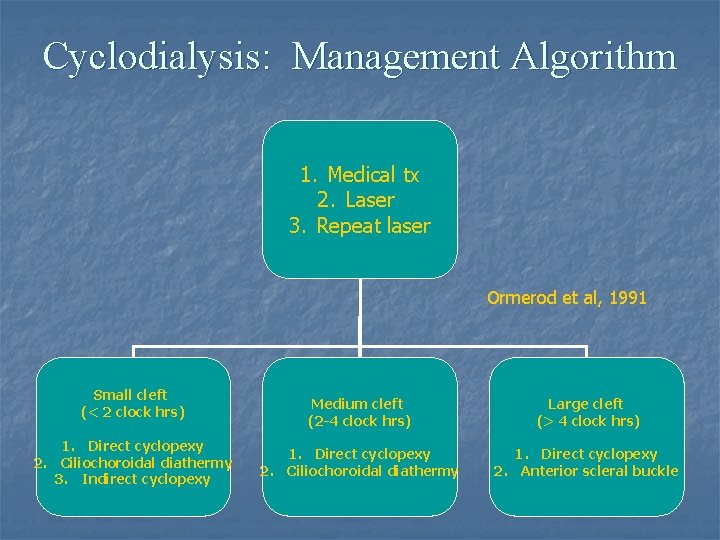
Cyclodialysis: Management Algorithm 1. Medical tx 2. Laser 3. Repeat laser Ormerod et al, 1991 Small cleft (< 2 clock hrs) 1. Direct cyclopexy 2. Ciliochoroidal diathermy 3. Indirect cyclopexy Medium cleft (2 -4 clock hrs) Large cleft (> 4 clock hrs) 1. Direct cyclopexy 2. Ciliochoroidal diathermy 1. Direct cyclopexy 2. Anterior scleral buckle
Cyclodialysis: Management n Cyclodialysis cleft may close spontaneously due to… n n n Inflammatory response hyphema Cycloplegia n May occur within first 6 wks n More common in children
Cyclodialysis: Management n Following resolution, a self-limited ocular hypertension is common within the first 2 wks n IOP rarely > 45 mm. Hg n Miotics are contraindicated
Cyclodialysis: Prognosis n Vision often improves after hypotony is corrected (IOP: 6 -12 mm. Hg) Best results with early correction n Vision may improve rapidly or take months n n Delay of treatment > 8 wks the risk of losing 1 -3 snellen lines of vision
Back to our patient… n VA 20/60; IOP nrl on f/u appt. n Tapered pred forte; atropine continued; glaucoma gtts/diamox stopped n ~ 2 wks after IOP normalized, recurrence of IOP (38); VA 20/50+2; glaucoma gtts resumed; PF/atropine stopped n ~ 2 wk f/u IOP normalized; VA 20/25 -2; glaucoma gtts continued n Follow-up 3 mos
Take home points… n Cyclodialysis cleft should be considered with IOP in setting of blunt trauma. n Closed cyclodialysis cleft should be considered with IOP and a history of blunt trauma (within 6 wks) and IOP with signs of hypotony maculopathy &/or choroidal detachment. n Hypotony is the major complication & is responsible for vision loss. n A hypotonous cyclodiaysis cleft without retinopathy does not require treatment. n Goal of treatment is to reverse the hypotony n Medical treatment is the primary form of management for the first 6 wks.
References n n n n n Ormerod et al. Management of a hypotonous cyclodialysis cleft. Ophth 1991; 98 (9): 1384 -93 Tran et al. UBM in the diagnosis & management of cyclodialysis cleft. Asian J Ophth, Vol. 4 (3) 2002; 11 -15 Hansen et al. Visualized cyclodialysis: an additional option in glaucoma surgery. Acta Ophth. 1986; 64: 142 -45 Joondeph HC. Management of postoperative & post-traumatic cyclodialysis clefts with argon laser photocoagulation. Ophth Surg. 1980; 11: 186 -88 Brooks et al. Noninvasive closure of a persistent cyclodialysis cleft. Ophth. 1996; 103: 1943 -45 Aminlari et al. Medical/surgical/laser management of cyclodialysis cleft. Arch Ophth. 2004; 122; 399 -404 Alward. Color Atlas of Gonioscopy. AAO. 2001 BCSC. Glaucoma. AAO. 2004 -5 Yanoff. Traumatic Glaucomas. 2 nd Ed. 2004 Allingham et al. Shield’s testbook of glaucoma. Traumatic Glaucomas. 5 th Ed. 2005
 Color 1192007
Color 1192007 Utmb grand rounds
Utmb grand rounds Duke medicine grand rounds
Duke medicine grand rounds Nursing grand rounds presentation example
Nursing grand rounds presentation example Denise johnson case
Denise johnson case Deus semper maior
Deus semper maior Sangere på vei til lundamo
Sangere på vei til lundamo Bevegelsesenergi formel
Bevegelsesenergi formel Daca iti vei opri piciorul ziua sabatului
Daca iti vei opri piciorul ziua sabatului Vei international
Vei international Hinduismen bilder
Hinduismen bilder Best case worst case average case
Best case worst case average case 473 rounded to the nearest ten
473 rounded to the nearest ten Christmas table quiz seomra ranga
Christmas table quiz seomra ranga Tabular dimensioning
Tabular dimensioning Five layers of neurosis
Five layers of neurosis A is an odd number which rounds to 100 000
A is an odd number which rounds to 100 000 Maintenance rounds
Maintenance rounds Schwartz rounds facilitator training
Schwartz rounds facilitator training Sam rounds
Sam rounds Quality teaching rounds coding sheet
Quality teaching rounds coding sheet Red, white & blue bite size rounds tortilla chips
Red, white & blue bite size rounds tortilla chips Readiness rounds
Readiness rounds Breech marks
Breech marks Harvard instructional rounds
Harvard instructional rounds Denise yaghmourian
Denise yaghmourian Denise lord
Denise lord Jacqui saburido
Jacqui saburido Denise schout
Denise schout Denise gabuzda
Denise gabuzda Dr denise wood
Dr denise wood Denise farrelly
Denise farrelly Denise trimble
Denise trimble Weeds denise
Weeds denise