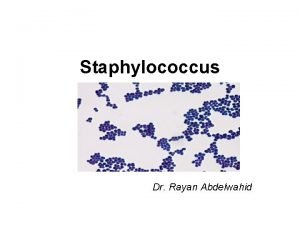
Gram Positive Cocci The Staphylococci INTRODUCTION Staphyloccocci derived














- Slides: 34
Gram Positive Cocci: The Staphylococci
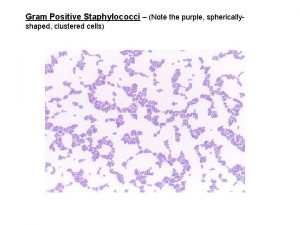
INTRODUCTION Staphyloccocci - derived from Greek “staphyle” (bunch of grapes) n Gram positive cocci arranged in clusters n Hardy organisms surviving many non physiologic conditions n Include a major human pathogen and skin commensals n

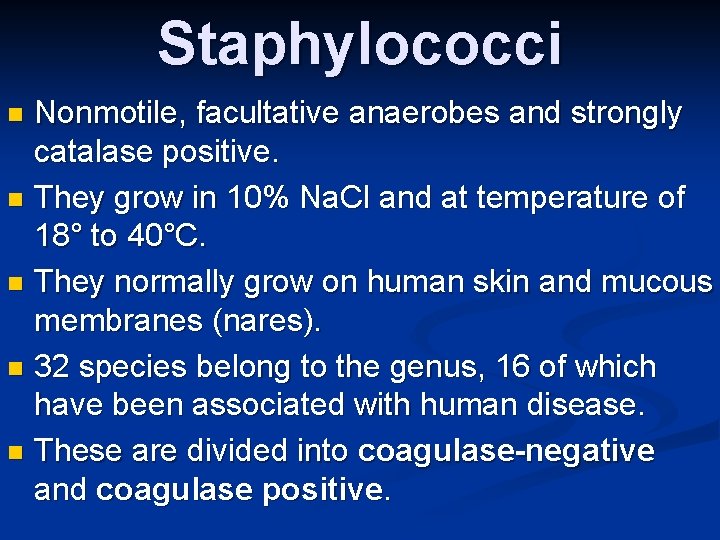
Staphylococci Nonmotile, facultative anaerobes and strongly catalase positive. n They grow in 10% Na. Cl and at temperature of 18° to 40°C. n They normally grow on human skin and mucous membranes (nares). n 32 species belong to the genus, 16 of which have been associated with human disease. n These are divided into coagulase-negative and coagulase positive. n

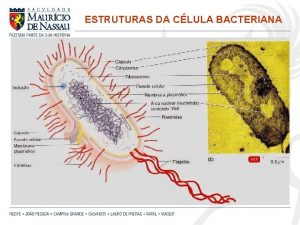
n Structure of Staphylococci Capsule (Slime) Teichoic acid Used for binding of staphylococci to fibronectin. n Protein A On Staphylococcus aureus only and it is covalently linked to peptidoglycan. It has a unique affinity for binding to FC of Ig. G. n Clumping Factor (bound coagulase) Present on most strains of Staphylococcus aureus. It binds fibrinogen converting it to fibrin causing staphylococci to clump or aggregate. n
Grouping for Clinical Purposes n 1. Coagulase positive Staphylococci n Staphylococcus aureus n 2. Coagulase negative Staphylococci n Staphylococcus epidermidis n Staphylococcus saprophyticus
Staphylococcus aureus n Bacteria commonly carried on the skin or in the nose n 25 -30% population is colonized with “staph” n Cause of infections n. Minor (skin and soft tissue) n. Major infections (blood, pneumonia, surgical site) n Staph is the most common cause of skin 7
Epidemiology n n n Present in most environments frequented by humans Readily isolated from fomites Carriage rate for healthy adults is 20 -60% Carriage is mostly in anterior nares, skin, nasopharynx, intestine Predisposition to infection include: poor hygiene and nutrition, tissue injury, preexisting primary infection, diabetes, immunodeficiency Increase in community acquired methicillin resistance - MRSA 8
Pathogenesis n n Staphylococcus aureus produces a large number of virulence factors including toxins and enzymes. Toxins: 1) Cytotoxins: Membrane-damaging. - Alpha, beta, gamma, delta and leukocidin. - Alpha toxin affects RBCs, WBCs, platelets and hepatocytes - beta toxin (sphingomyelinase C) affects RBCs, WBCs, macrophages and firbroblasts. - lysis of neutrophils releases lysosomal enzymes that
2) Exfoliative Toxin (exfoliatin, epidermolytic toxin) - It is a serine protease that has two distinct forms A and B. - Splits intercellular bridges (desmosomes) in the stratum granulosum layer of the epidermis with no cytolysis or inflammation. - Scaled skin syndrome which affects young children only. - Antibodies are protective.

4) Enterotoxins - Six serologically distinct types (A-F) - Heat stable (resist 100°C for 30 minutes) - Resistant to hydrolysis by gastric and jejunal enzymes. - Act centrally. - Enterotoxin A is most commonly associated with disease. - Enterotoxin B is associated with pseudomembranous colitis. - Enterotoxins C and D commonly contaminate milk products.

n Enzymes 1) Catalase 2) Coagulase (bound and free). It reacts with plasma factor globulin (coagulase reacting factor) to form staphylothrombin (thrombin-like) which converts fibrinogen to fibrin. 3) Hyaluronidase 4) Fibrinolysin (staphylokinase) 5) Lipase 6) Nuclease
DISEASES n Toxin mediated n Food poisoning n toxic shock syndrome n Scalded skin syndrome n Due to direct effect of organism n Local lesions of skin n Deep abscesses n Systemic infections
Clinical Syndromes A) Diseases of Staphylococcus aureus n Scalded skin syndrome - Abrupt onset with localized perioral erythema that spreads to cover the entire body within 2 days. - Nikolsky sign - Large bullae or cutaneous blisters form, followed by desquamation of the epithelium. - Lesions are devoid from organisms or white blood cells. - Recovery without scarring in 7 -10 days is associated with antibody production against the toxin.

Impetigo of the n newborn Toxemia n Scalded skin • syndrome Toxic shock • syndrome Figure 21. 4

Toxic Shock Syndrome - Primarily a disease of menstruating women and other adults. - Originally associated with the use of highly absorbent tampons, which apparently foster the growth of staphylococci. - Nowadays, TSS more commonly follows staphylococcal infection of traumatic or surgical wounds, and it occurs in men as well as women. - Abrupt onset of fever, hypotension and diffuse erythematous rash with multiple organ dysfunction. - Desquamation follows involving the entire skin including palms and soles. - Risk of recurrence is as high as 65%. n
Food Poisoning - Follows ingestion of enterotoxin in improperly prepared or refrigerated food. - Commonly associated with processed meat (ham, salted pork) custard, filled pastries, potato salad and ice cream. - Source of contamination is food handlers. - The incubation period is in the range of four hours and symptoms last for less than 24 hours, n
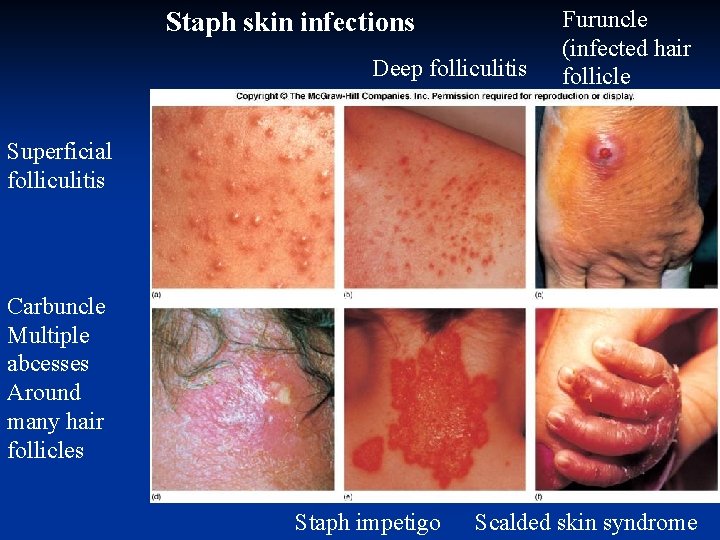
Cutaneous Infections - Abscess: a well-defined area in tissue that contains pus. n - Abscesses in the skin are called boils, or, in medical parlance, furuncles. Multiple interconnected abscesses are called carbuncles (coalescence of furuncles). - Staphylococci may spread in the subcutaneous or submucosal tissue and cause a diffuse inflammation called cellulitis. - Impetigo and stye are other staphylococcal infection.
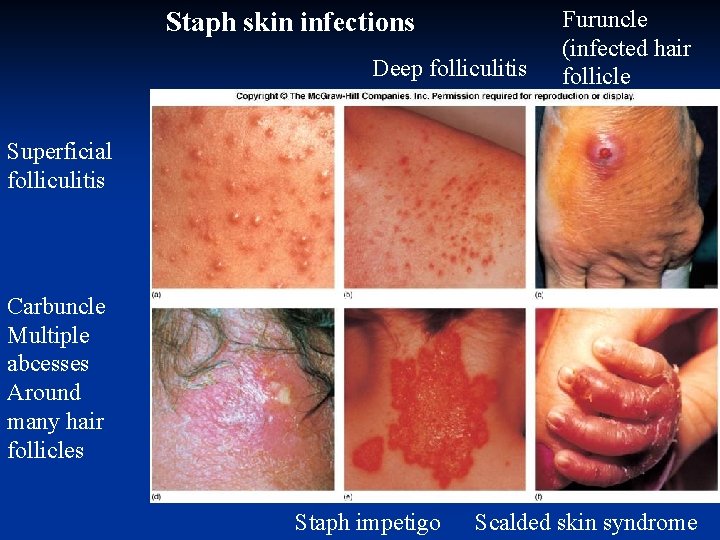
Staph skin infections Deep folliculitis Furuncle (infected hair follicle Superficial folliculitis Carbuncle Multiple abcesses Around many hair follicles Staph impetigo Scalded skin syndrome



Impetigo n
Systemic Infections n 1. With obvious focus n Osteomyelitis, septic arthritis n 2. No obvious focus n heart (infective endocarditis) n Brain(brain abscesses) n 3. Associated With predisposing factors n multiple abscesses, septicemia(IV drug users)
n Osteomyelitis and septic arthritis - Hematogenous or direct spread - It involves metaphyseal area of long bones with sudden onset of localized pain and fever. - Positive blood culture in 50% of cases. - Vertebral involvement is common in adults. - Septic arthritis results from intraarticular injection or infection of abnormal joints.
n Bacteremia and Endocarditis - The focus is unknown in 30% of cases. - Acute endocarditis is fatal in about 50% of cases. - Hospital acquired in more than 50% of cases. n Pneumonia and Empyema - Due to aspiration of oral secretions or hematogenous spread from a distant site.

MRSA Case Categorization Healthcare-associated: n Hospital-onset: Cases with positive culture obtained >48 hrs after hospital admission (may also have risk factors) n Community-onset: Cases with at least 1 of the following risk factors: n Invasive device at time of admission; h/o MRSA infection or colonization; h/o surgery, hospitalization, dialysis, or residence in a LTC facility in 12 months preceding culture n Community-associated: Cases with n
MRSA Risk Factors n Previous MRSA Infection/Colonization n Close skin-to-skin contact n Breaks in skin (cuts, abrasions, skin disease, surgical sites) n Contaminated items and surfaces n Crowded living conditions n Inadequate personal hygiene 28
CA-MRSA Risk Groups n Children n Daycare (attendees/care givers/family members) Elementary School (attendees/teachers/family members) n Residential School for Developmentally Delayed (attendees/teachers/care givers) Athletes (high school and college) Prison Inmates Military Recruits Homeless Individuals Injecting Drug Users Men who have Sex with Men n n n 29

30

31

32
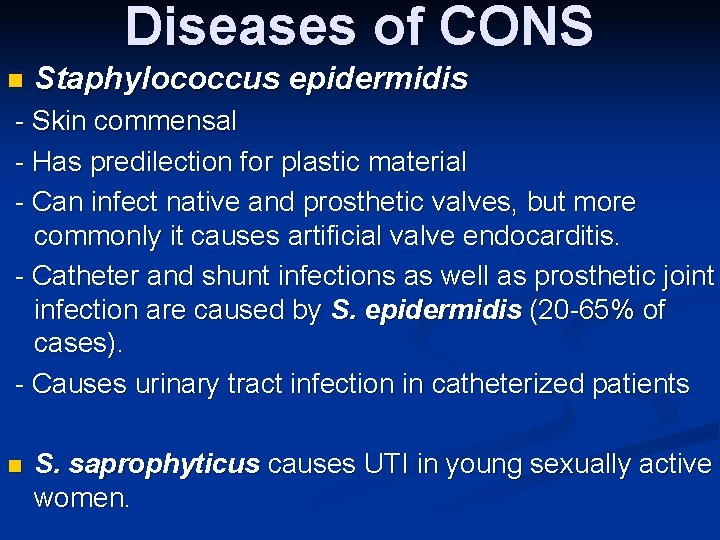
Diseases of CONS n Staphylococcus epidermidis - Skin commensal - Has predilection for plastic material - Can infect native and prosthetic valves, but more commonly it causes artificial valve endocarditis. - Catheter and shunt infections as well as prosthetic joint infection are caused by S. epidermidis (20 -65% of cases). - Causes urinary tract infection in catheterized patients n S. saprophyticus causes UTI in young sexually active women.

DIAGNOSIS n 1. In all pus forming lesions n Gram stain and culture of pus n 2. In all systemic infections n Blood culture n 3. In infections of other tissues n Culture of relevant tissue or exudate
 Staphylococcus epidermidis en agar sangre
Staphylococcus epidermidis en agar sangre Gram positive cocci
Gram positive cocci Biochemical test
Biochemical test Gram positive cocci
Gram positive cocci Gram positive cocci
Gram positive cocci Gram positive cocci
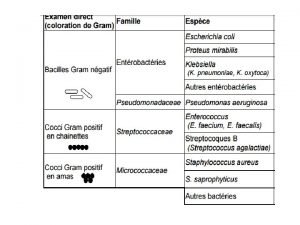
Gram positive cocci Cocci gram + en amas
Cocci gram + en amas Streptococcus gram negative
Streptococcus gram negative Qcm cocci gram positif
Qcm cocci gram positif Coagulase negative staphylococcus
Coagulase negative staphylococcus Bactrias
Bactrias 20 gram fenol dicampur dengan 30 gram air
20 gram fenol dicampur dengan 30 gram air Eubatteri
Eubatteri Mesofase pada padatan dapat berupa
Mesofase pada padatan dapat berupa Grams to gram
Grams to gram Bactérias gram positivas e gram negativas
Bactérias gram positivas e gram negativas 30 gram asam asetat (bm=60) dilarutkan dalam 45 gram air
30 gram asam asetat (bm=60) dilarutkan dalam 45 gram air Perbedaan gram positif dan gram negatif
Perbedaan gram positif dan gram negatif Satuan kwintal
Satuan kwintal L
L Staph aureus morphology
Staph aureus morphology Sarcinae
Sarcinae Staphylococcus aureus cocci or bacilli
Staphylococcus aureus cocci or bacilli Rods or cocci
Rods or cocci Difference selective and differential media
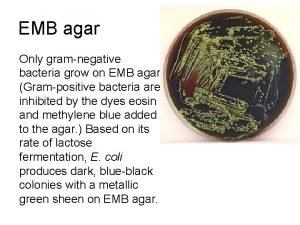
Difference selective and differential media Helen mc
Helen mc Differential vs selective media
Differential vs selective media Staphylococcus epidermidis on emb agar
Staphylococcus epidermidis on emb agar Gram negative bacilli chinese letter
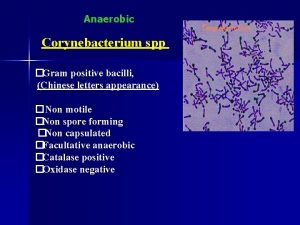
Gram negative bacilli chinese letter Spirochete infection
Spirochete infection Gram positive bacteria
Gram positive bacteria Gram
Gram Gram positive bacili
Gram positive bacili Gram positive cell wall
Gram positive cell wall Gram negative and positive bacteria
Gram negative and positive bacteria