Gram Negative Rods Enterobacteriaceae Family General Characteristics of
Gram Negative Rods
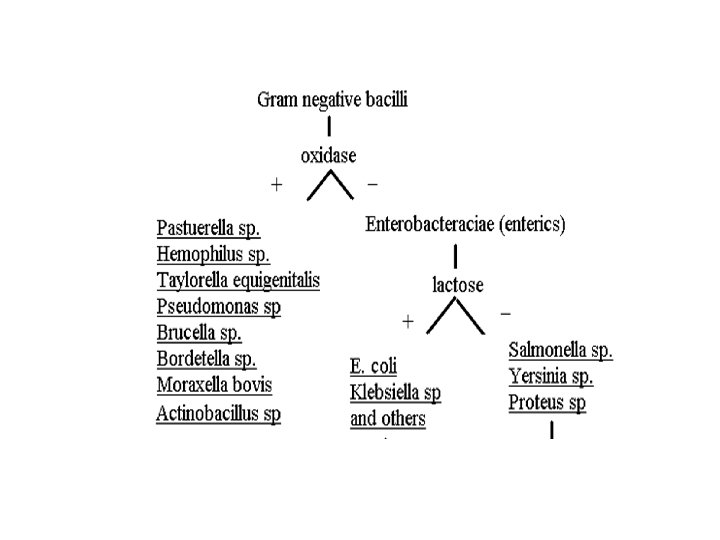
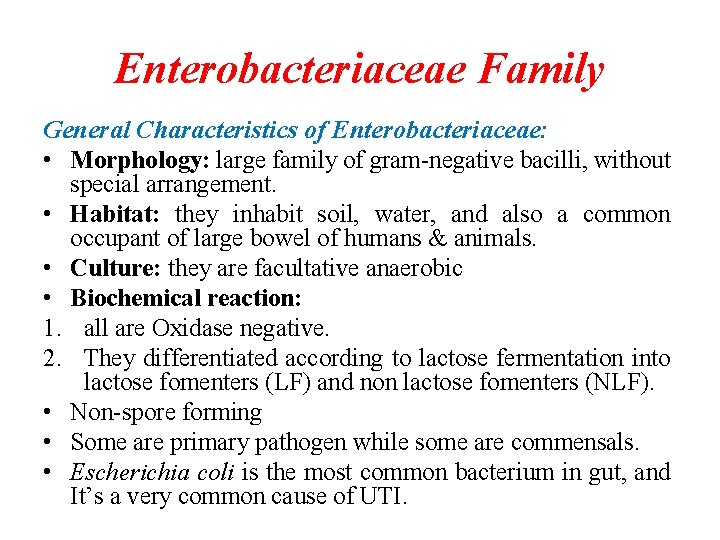
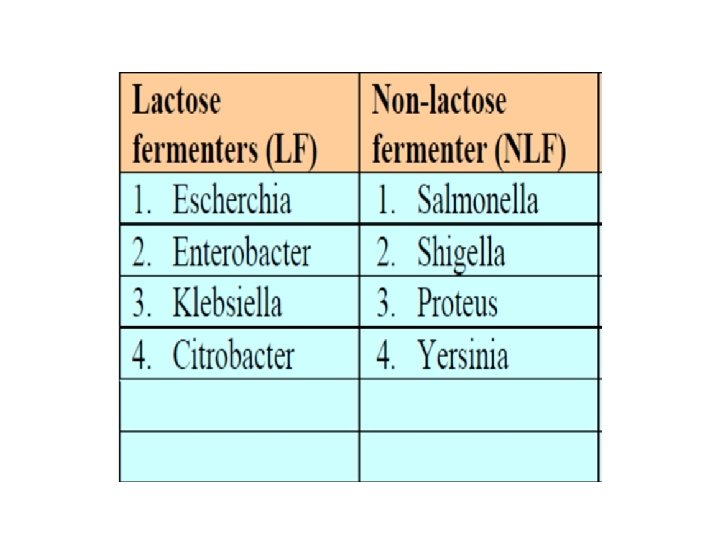
Enterobacteriaceae Family General Characteristics of Enterobacteriaceae: • Morphology: large family of gram-negative bacilli, without special arrangement. • Habitat: they inhabit soil, water, and also a common occupant of large bowel of humans & animals. • Culture: they are facultative anaerobic • Biochemical reaction: 1. all are Oxidase negative. 2. They differentiated according to lactose fermentation into lactose fomenters (LF) and non lactose fomenters (NLF). • Non-spore forming • Some are primary pathogen while some are commensals. • Escherichia coli is the most common bacterium in gut, and It’s a very common cause of UTI.
Gram-negative rods
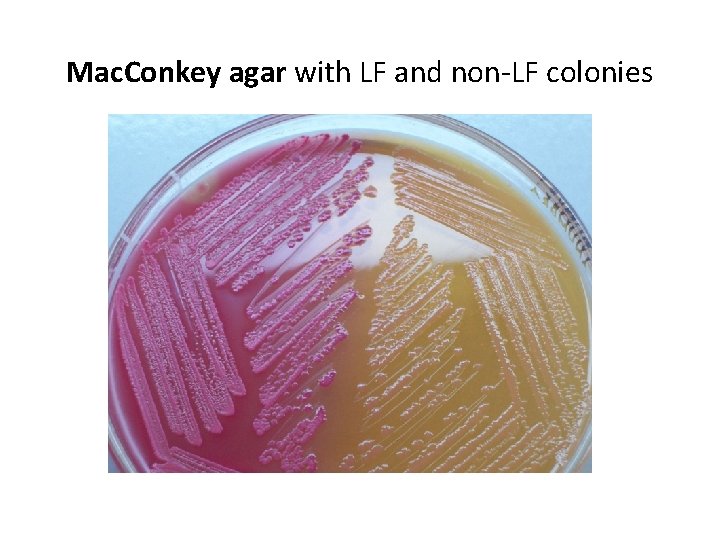
Mac. Conkey agar with LF and non-LF colonies
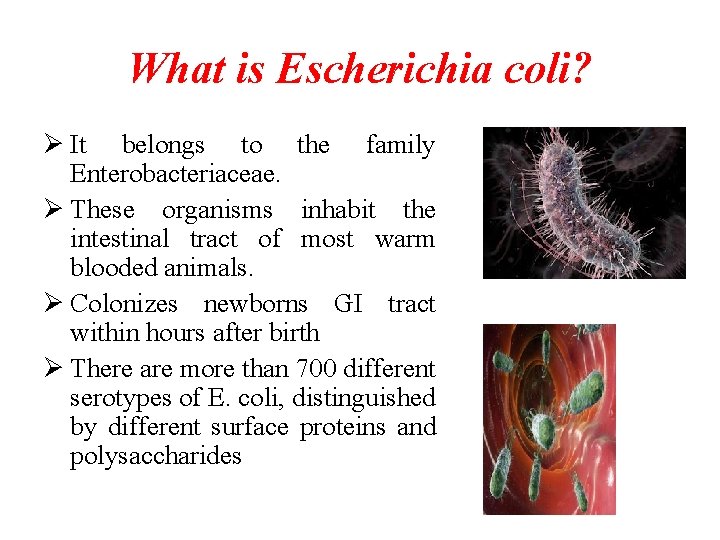
What is Escherichia coli? Ø It belongs to the family Enterobacteriaceae. Ø These organisms inhabit the intestinal tract of most warm blooded animals. Ø Colonizes newborns GI tract within hours after birth Ø There are more than 700 different serotypes of E. coli, distinguished by different surface proteins and polysaccharides
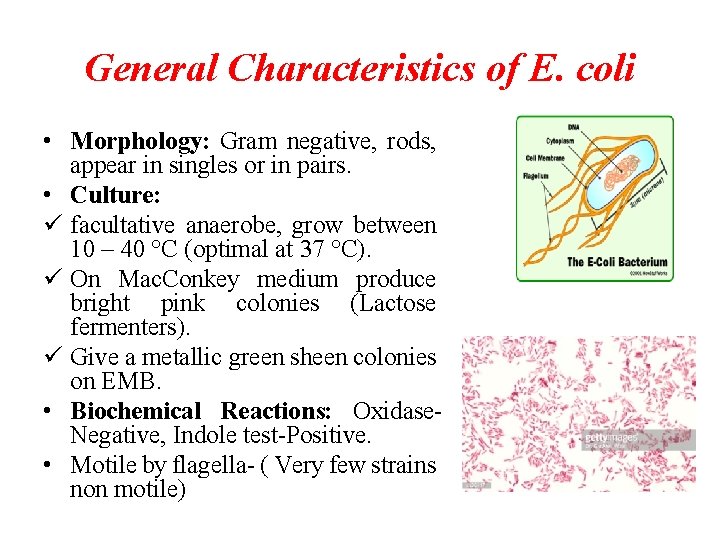
General Characteristics of E. coli • Morphology: Gram negative, rods, appear in singles or in pairs. • Culture: ü facultative anaerobe, grow between 10 – 40 °C (optimal at 37 °C). ü On Mac. Conkey medium produce bright pink colonies (Lactose fermenters). ü Give a metallic green sheen colonies on EMB. • Biochemical Reactions: Oxidase. Negative, Indole test-Positive. • Motile by flagella- ( Very few strains non motile)
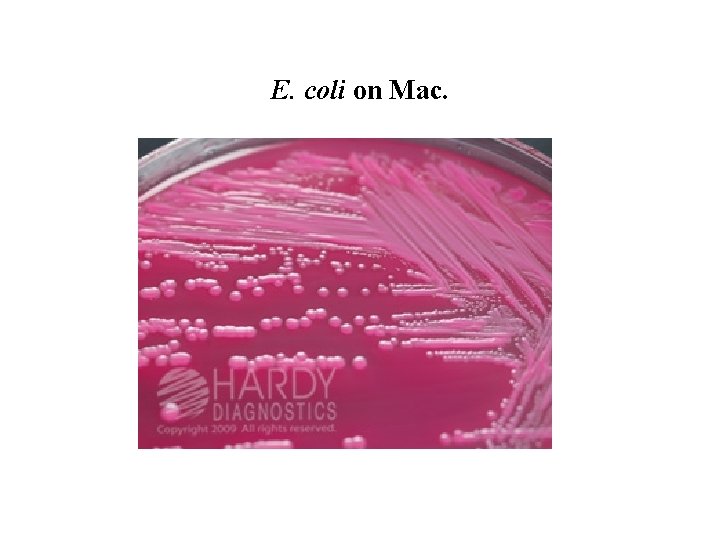
E. coli on Mac.
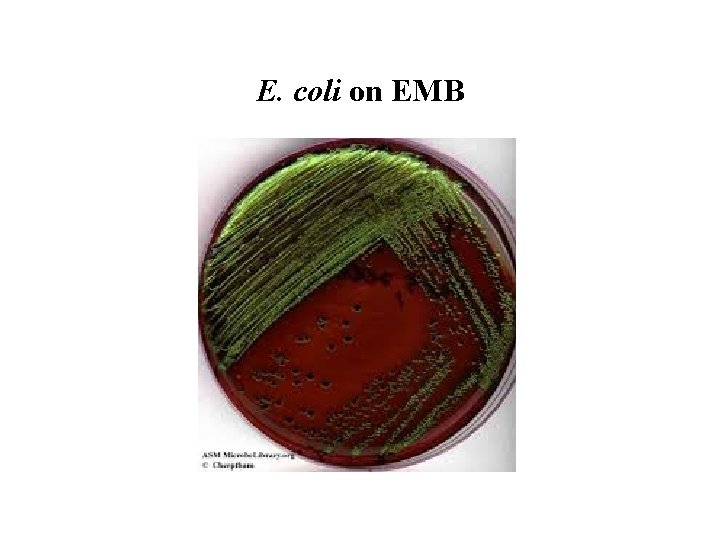
E. coli on EMB
The Beneficial E. coli 1. Protects the intestinal tract from bacterial infections 2. Aids in digestion 3. Produces our main source of vitamins B 12 and K 4. Lives symbiotically with us (we help them to live, and they help us to live)
Bad E. coli • While most E. coli are good for you, there a few strains of E. coli that are harmful to humans. • It is possible to get an individual strain of E. coli that is harmful to you. • E. coli O 157: H 7 Most notorious strain of bad E. coli: ü Produces a powerful toxin and can cause severe illness ü Most dangerous for little kids, the elderly, and the sick ü Damages the intestines, causes bloody diarrhea, and other complications ü Cause disease by making a toxin called Shiga toxin “Shiga toxin-producing” E. coli - STEC
Pseudomonas spp. • Ubiquitous bacteria, grow everywhere (in soil , water, plants, animal tissues, and other places that contain moisture). • Some strain can even grow in distilled water. • Can produce pigment. • Some strains are antibiotic-resistant bacteria. • It is an “Opportunistic Pathogen”.
Pseudomonas spp. • Pseudomonas aeruginosa is the primary human pathogen in the genus Pseudomonas. • It’s found any wear in the environment. • Common cause of nosocomial infections. • In normal host it cause opportunistic infection. • Immunodeficiency, breaching of first line of defense, and the use of medical devices predispose the patients to P. aeruginosa infections
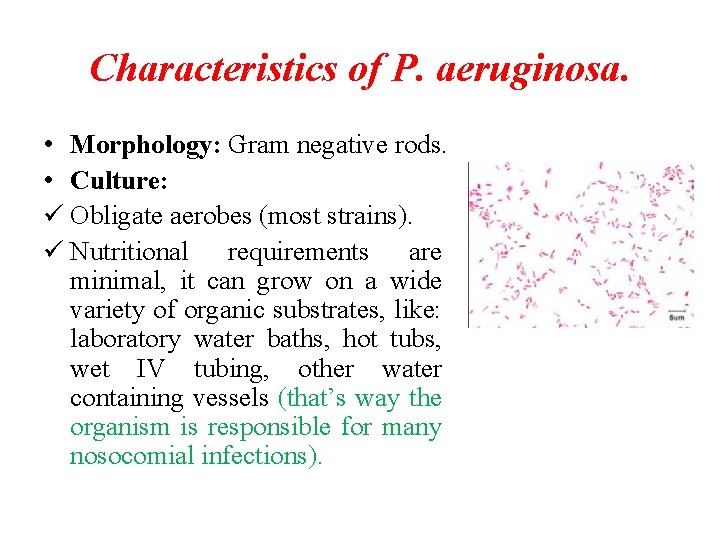
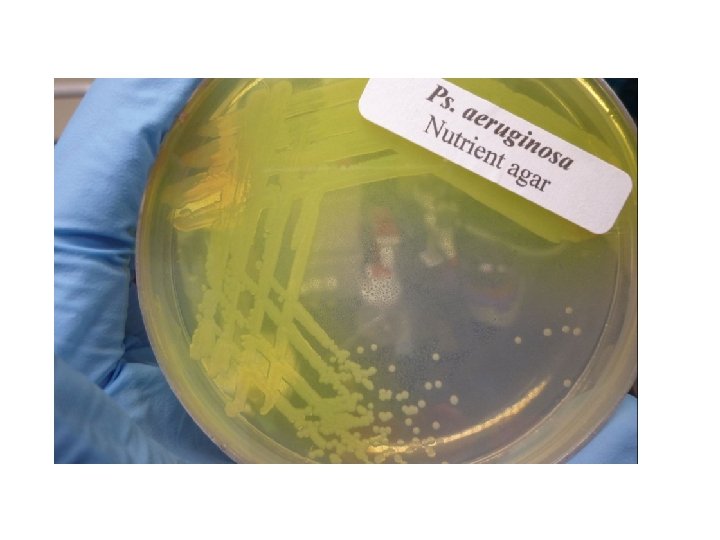
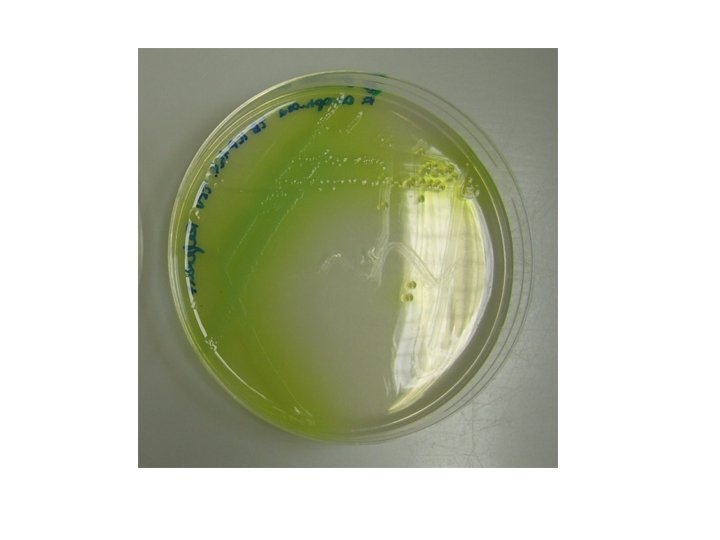
Characteristics of P. aeruginosa. • Morphology: Gram negative rods. • Culture: ü Obligate aerobes (most strains). ü Nutritional requirements are minimal, it can grow on a wide variety of organic substrates, like: laboratory water baths, hot tubs, wet IV tubing, other water containing vessels (that’s way the organism is responsible for many nosocomial infections).
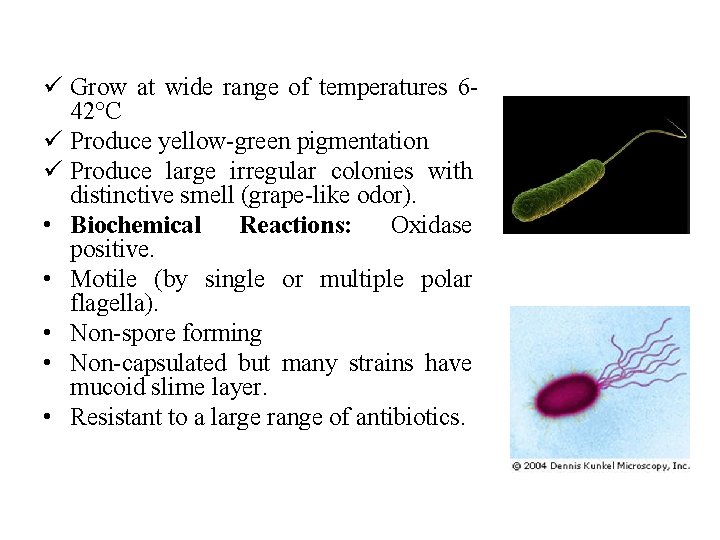
ü Grow at wide range of temperatures 642°C ü Produce yellow-green pigmentation ü Produce large irregular colonies with distinctive smell (grape-like odor). • Biochemical Reactions: Oxidase positive. • Motile (by single or multiple polar flagella). • Non-spore forming • Non-capsulated but many strains have mucoid slime layer. • Resistant to a large range of antibiotics.
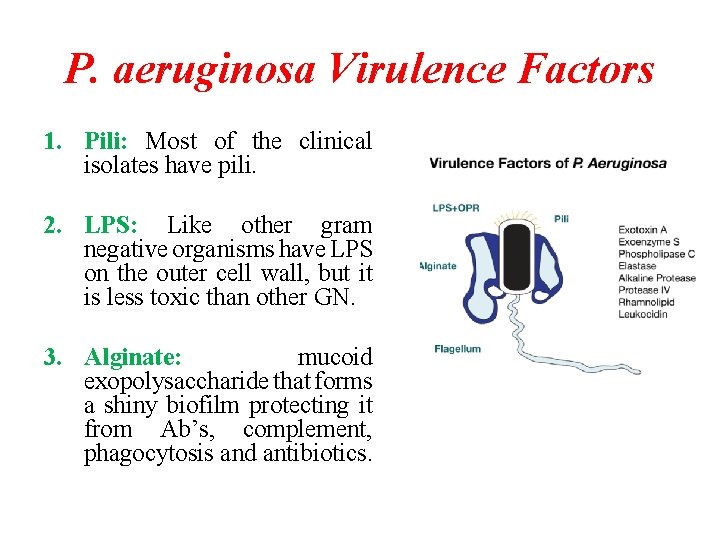
P. aeruginosa Virulence Factors 1. Pili: Most of the clinical isolates have pili. 2. LPS: Like other gram negative organisms have LPS on the outer cell wall, but it is less toxic than other GN. 3. Alginate: mucoid exopolysaccharide that forms a shiny biofilm protecting it from Ab’s, complement, phagocytosis and antibiotics.
4. Exotoxin A: similar to Diphtheria toxin it inhibit protein synthesis (cause corneal damage). 5. Hemolysin: it break down lipids & contribute to tissue invasion & destruction. it is toxic to alveolar macrophages. 6. Proteases: play a major role during acute infection, It also have a rule in tissue invasion especially in corneal infections. 7. Elastase: destruction of elastin-containing tissues (eg. blood vessels, lung tissue, skin), collagen, immunoglobulins and complement.
Clinical Significance of P. auroginosa Some clinical diseases caused by P. auroginosa: • Pulmonary infections. • Burn wound infections and other skin and soft tissue infections (life threatening). • UTI’s (especially catheterized) • External Otitis (swimmer’s ear) • Eye infections and corneal ulceration via contaminated contact lens cleaning fluids. • Pseudomonal Endocarditis
Pulmonary Infections • Can range form asymptomatic colonization to severe necrotizing bronchopenumonia. • Colonization is seen in patients with cystic fibrosis, chronic lung disease and neutropenia. • Mucoid strains are commonly isolated from chronic pulmonary patients and are more difficult to eradicate. • Predisposing conditions include previous therapy with broad spectrum abs , use of respiratory therapy equipment. • Mortality rate can be as high as 70% for invasive brnchopneumonia
Pseudomonas Corneal Ulcer • It is the most dreaded of all corneal infections. • There is rapid invasion and affection of deeper layers causing a central necrosis area within 48 hours and a ring abscess around corneal periphery. • Pus is mucus in consistency and greenish in color. • Hypopyon is unusually large. • Commonly associated with soft as well as extended contact lens wear.
Pseudomonas Corneal Ulcer
Treatment & Prevention • It is difficult to find antibiotics effective against P. aeruginosa because of its rapid development of resistance mutations and its own innate mechanisms of antibiotic resistance. • Generally a combination of two bactericidal antibiotics is essential for treatment
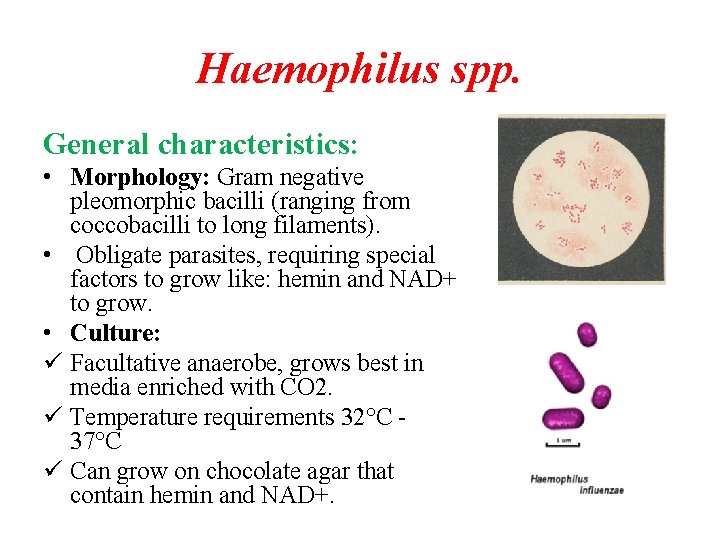
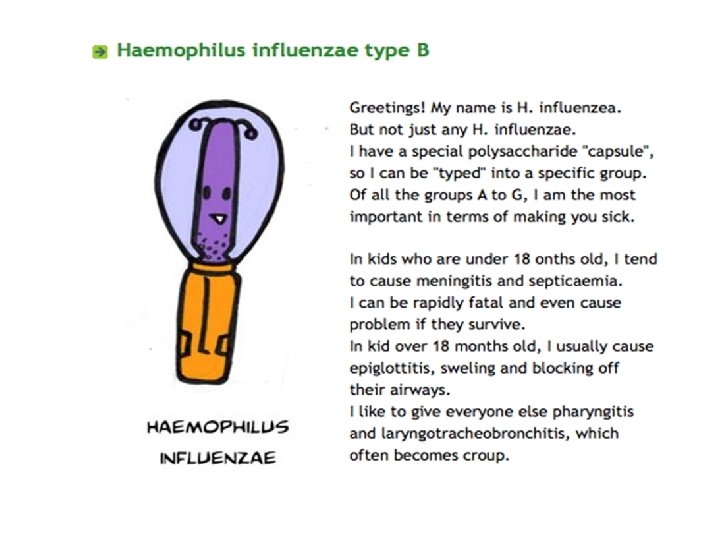
Haemophilus spp. General characteristics: • Morphology: Gram negative pleomorphic bacilli (ranging from coccobacilli to long filaments). • Obligate parasites, requiring special factors to grow like: hemin and NAD+ to grow. • Culture: ü Facultative anaerobe, grows best in media enriched with CO 2. ü Temperature requirements 32°C 37°C ü Can grow on chocolate agar that contain hemin and NAD+.
• The organism tend to cause widespread epidemics. • Non-motile. • Non-spore forming. • May produce capsule (6 capsular types have been distinguished a, b, c, d, e & f)
Haemophilus spp. • The commonest clinical isolate is Haemophilus influenzae (serotype b is most virulent type) • • The other species of the genus include: H. ducreyi H. parainfleunziae. H. aegyptius (eye infection)
Haemophilus influenzae
Pathogenecity of H. influenzae • Enters the body through respiratory tract. • Can produce Ig. A protease which helps in its attachment to respiratory mucosa. • It can cause respiratory infections such as otitis media, sinusitis and pneumonia (mostly non capsulated forms) • From this site, it can enter bloodstream and disseminate to distant sites (mostly capsulated forms (tybe b) is responsible for these diseases)
Treatment & Prevention Treatment: Third-generation cephalosporin such as ceftriaxone is drug of choice in meningitis and other serious infections. Prevention: By vaccination (Hib vaccine)
- Slides: 35