GRAM NEGATIVE DIPLOCOCCI LAYOUT Neisseria Taxonomic classification General


- Slides: 80
GRAM NEGATIVE DIPLOCOCCI
LAYOUT: Neisseria: Taxonomic classification General features Species Pathogenic Neisseriae Other. Neisseriae. Moraxella species Oligella species

Neisseriae
TAXONOMIC CLASSIFICATION: KINGDOM: Bacteria PHYLUM: Protobacteria CLASS: Betaproteobacteria ORDER: Neisseriales CLASS: Neisseriaceae GENUS: Neisseriae
GENERAL FEATURES: ØGram Negative diplococci ØAerobes and facultative anaerobes. ØNon sporing ØNon motile ØOptimum temperature- 35 -36ºc ØOptimum ph= 7. 0 -7. 4 Ø 5 -10% CO 2 enhances growth. ØFatidious in growth requirements.
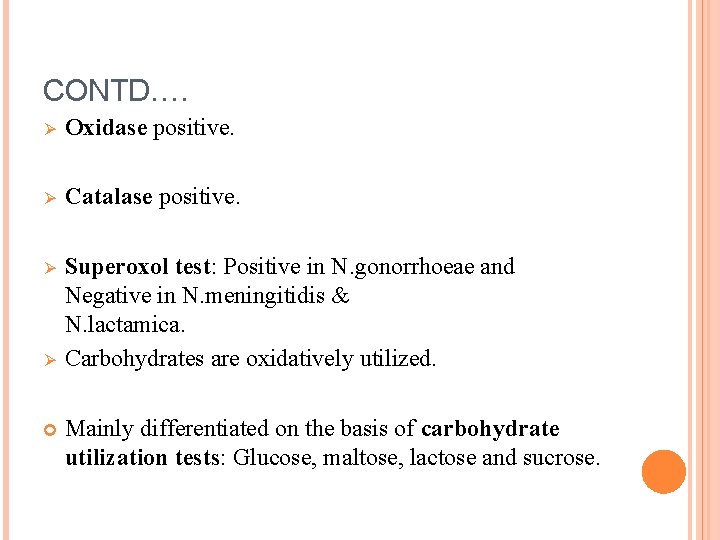
CONTD…. Ø Oxidase positive. Ø Catalase positive. Ø Superoxol test: Positive in N. gonorrhoeae and Negative in N. meningitidis & N. lactamica. Carbohydrates are oxidatively utilized. Ø Mainly differentiated on the basis of carbohydrate utilization tests: Glucose, maltose, lactose and sucrose.
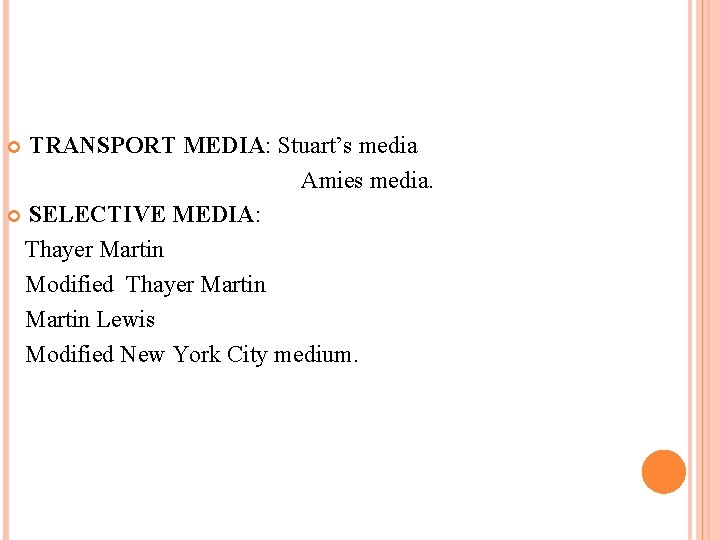
TRANSPORT MEDIA: Stuart’s media Amies media. SELECTIVE MEDIA: Thayer Martin Modified Thayer Martin Lewis Modified New York City medium.
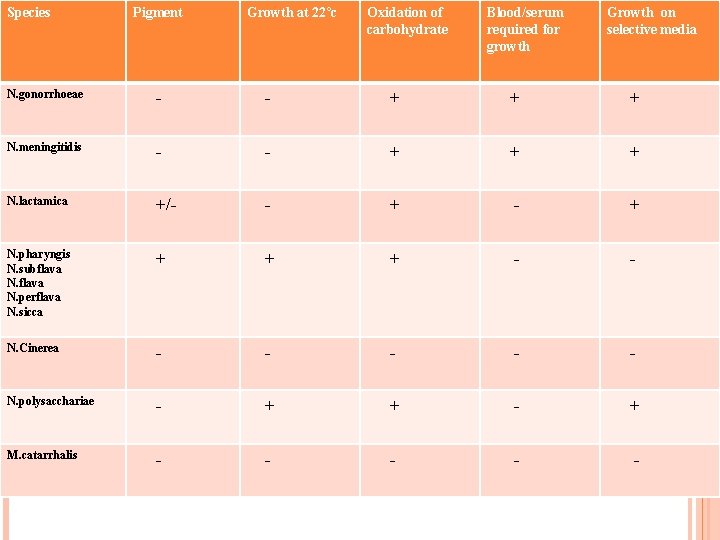
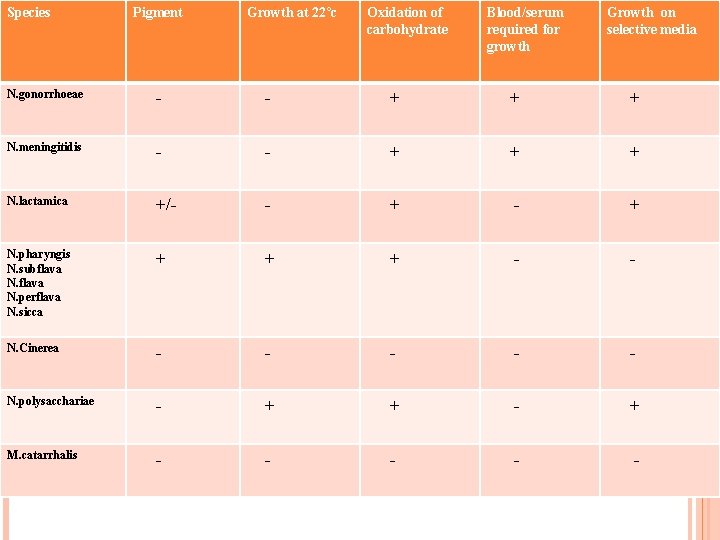
Species Pigment Growth at 22ºc Oxidation of carbohydrate Blood/serum required for growth Growth on selective media N. gonorrhoeae - - + + + N. meningitidis - - + + + N. lactamica +/- - + N. pharyngis N. subflava N. perflava N. sicca + + + - - N. Cinerea - - - N. polysacchariae - + + - + M. catarrhalis - - -
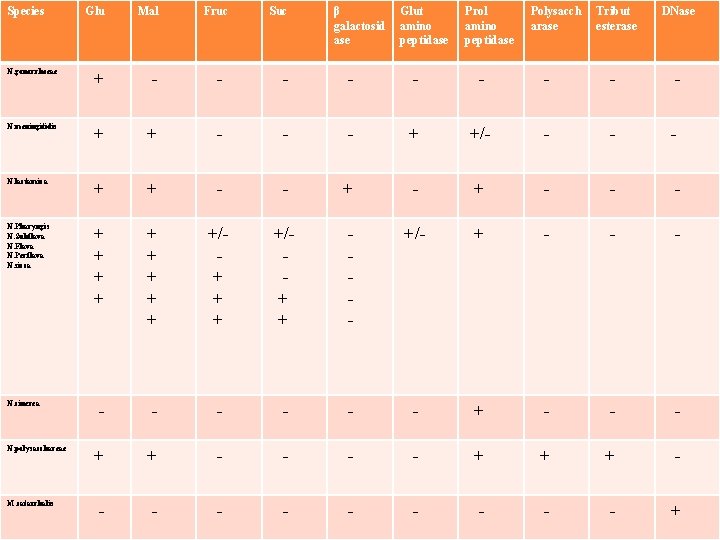
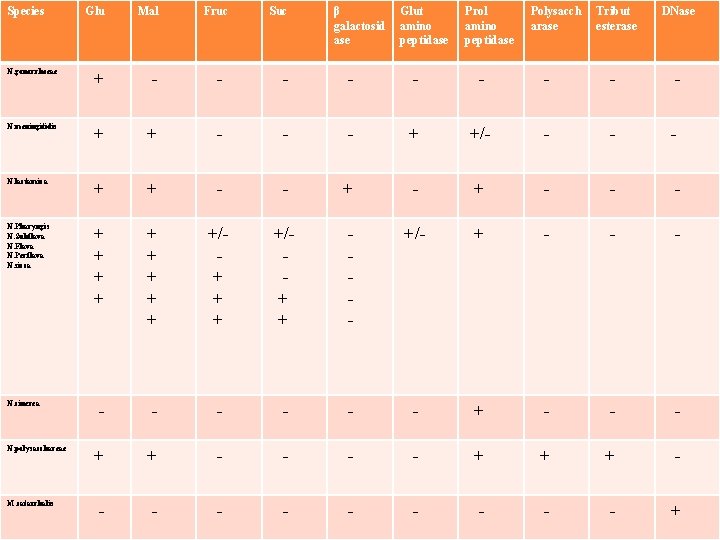
Species Glu Mal N. gonorrhoeae + - - - - - N. meningitidis + + - - - + +/- - N. lactamica + + - - - N. Pharyngis N. Subflava N. Flava N. Perflava N. sicca + + + + +/+ + - +/- + - - - - - + + - - + + + - - - - - + N. cinerea N. polysacchareae M. catarrhalis Fruc Suc β galactosid ase Glut amino peptidase Prol amino peptidase Polysacch arase Tribut esterase DNase
Important Human Pathogens Neisseria gonorrhoeae Neisseria meningitidis Other species normally colonize mucosal surfaces of oropharynx, nasopharynx and anogenital mucosal membranes
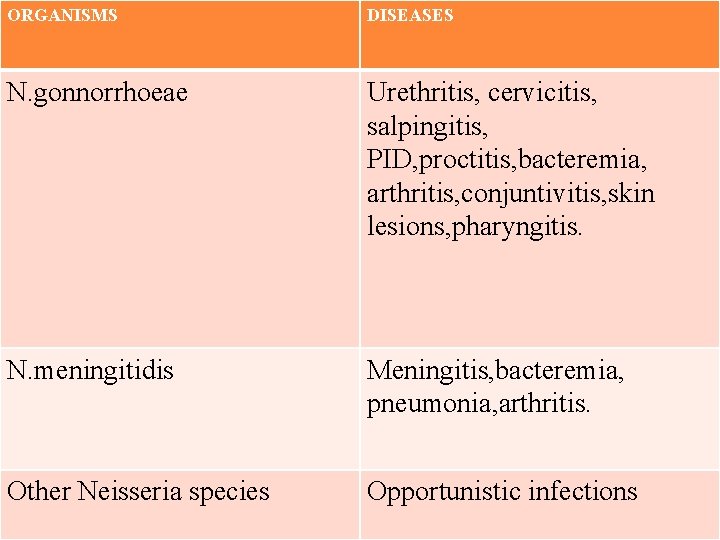
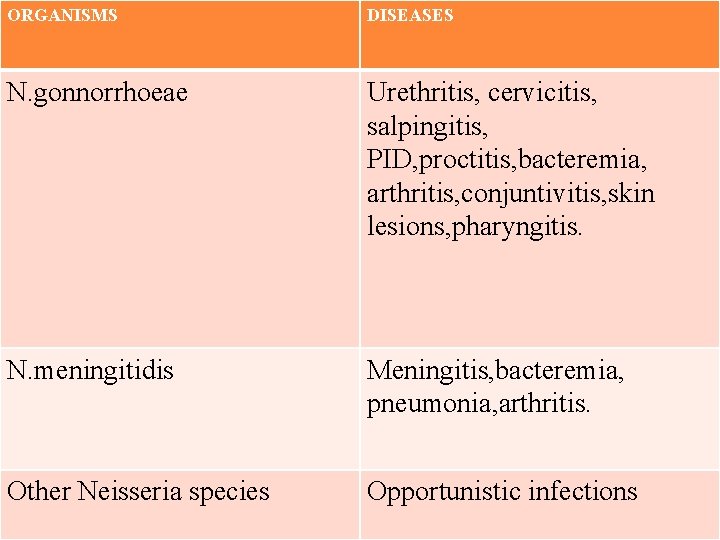
ORGANISMS DISEASES N. gonnorrhoeae Urethritis, cervicitis, salpingitis, PID, proctitis, bacteremia, arthritis, conjuntivitis, skin lesions, pharyngitis. N. meningitidis Meningitis, bacteremia, pneumonia, arthritis. Other Neisseria species Opportunistic infections
Synonyms -Diplococcus intracellularis Meningitidis -Meningococcus -Weichselbaum first discovered and isolated in 1887 from the spinal fluid of a patient. WEICHSELBAUM.
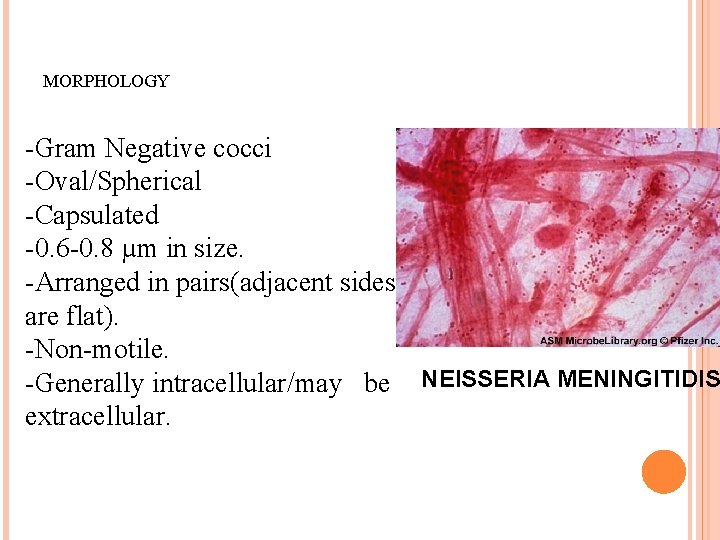
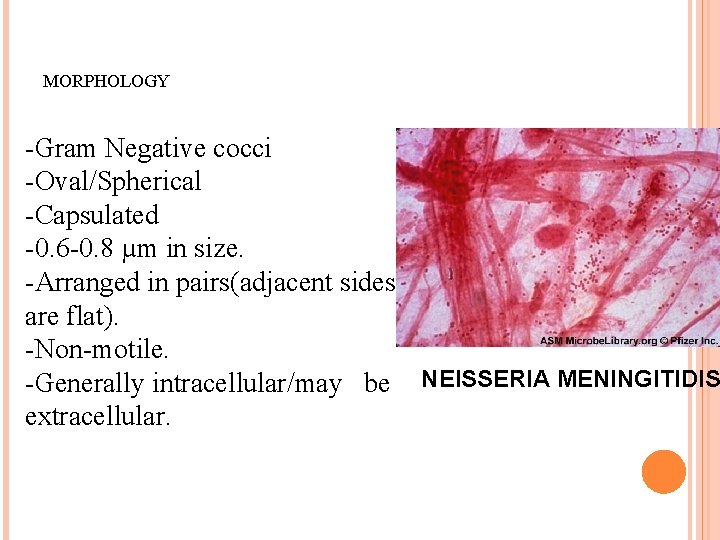
MORPHOLOGY -Gram Negative cocci -Oval/Spherical -Capsulated -0. 6 -0. 8 µm in size. -Arranged in pairs(adjacent sides are flat). -Non-motile. -Generally intracellular/may be NEISSERIA MENINGITIDIS extracellular.
CULTURAL CHARACTERISTICS: Exacting growth requirements. Blood, serum, ascitic fluid media. Strict aerobes. Opt. temperature 35°c-36°c(25 -42^c). Opt. p. H 7. 0 -7. 4. Growth facilitated by 5%-10% CO 2.
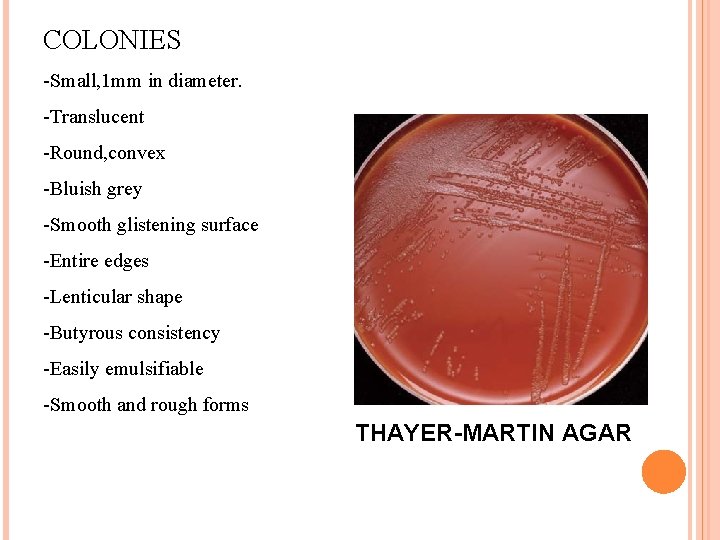
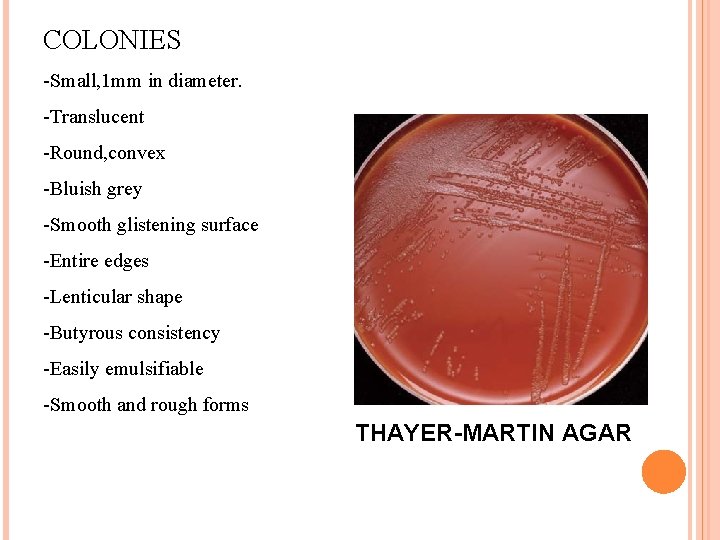
COLONIES -Small, 1 mm in diameter. -Translucent -Round, convex -Bluish grey -Smooth glistening surface -Entire edges -Lenticular shape -Butyrous consistency -Easily emulsifiable -Smooth and rough forms THAYER-MARTIN AGAR
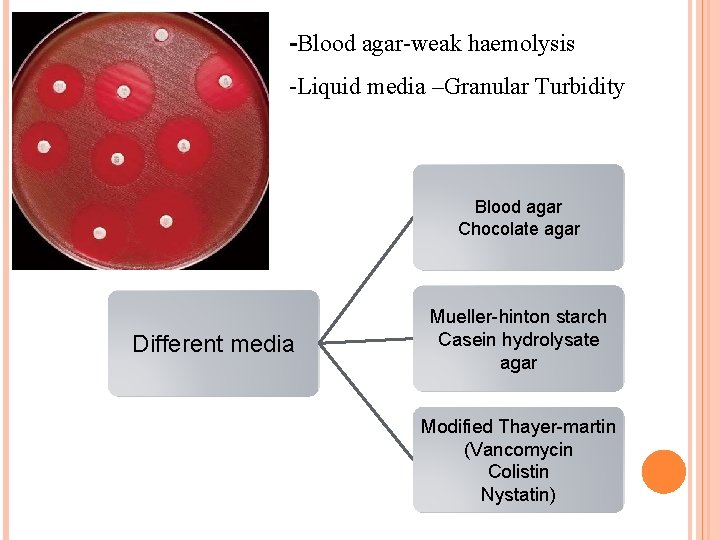
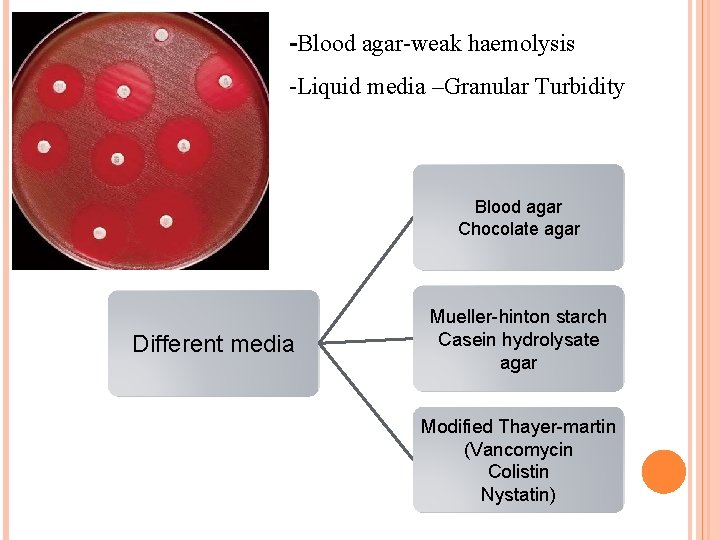
-Blood agar-weak haemolysis -Liquid media –Granular Turbidity Blood agar Chocolate agar Different media Mueller-hinton starch Casein hydrolysate agar Modified Thayer-martin (Vancomycin Colistin Nystatin)
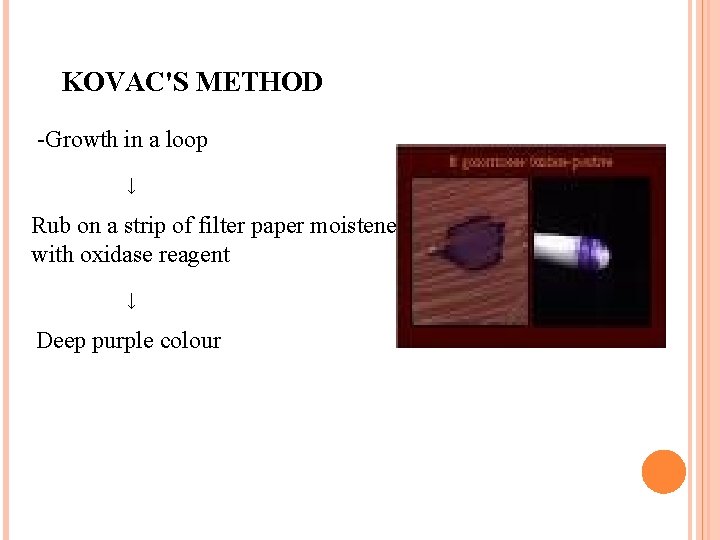
BIOCHEMICAL REACTIONS -Oxidase test positive -Freshly prepared 1% oxidase reagent ﴾tetramethyl paraphenylene diamine dihydrochloride) ↓ Culture media ↓ Deep purple colonies
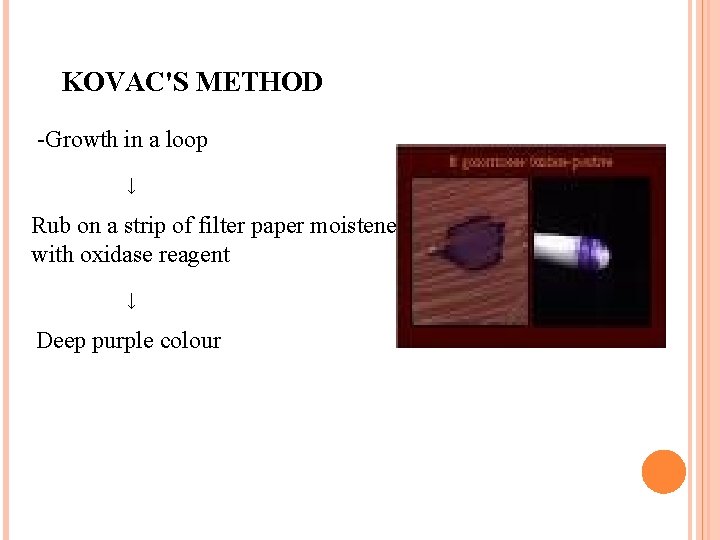
KOVAC'S METHOD -Growth in a loop ↓ Rub on a strip of filter paper moistened with oxidase reagent ↓ Deep purple colour
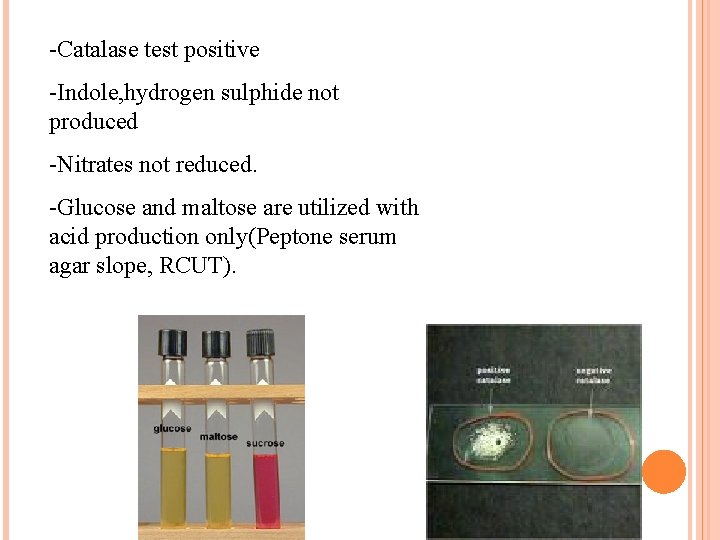
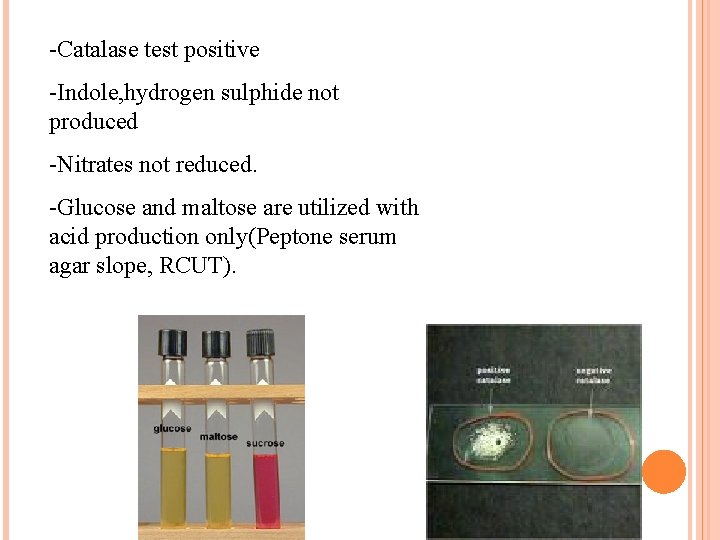
-Catalase test positive -Indole, hydrogen sulphide not produced -Nitrates not reduced. -Glucose and maltose are utilized with acid production only(Peptone serum agar slope, RCUT).
RESISTANCE -Delicate Freeze drying , Microbanking, Liquid nitrogen. -Highly susceptible -Heat -Dessication -Disinfectants -Pencillin. -Alterations in p. H
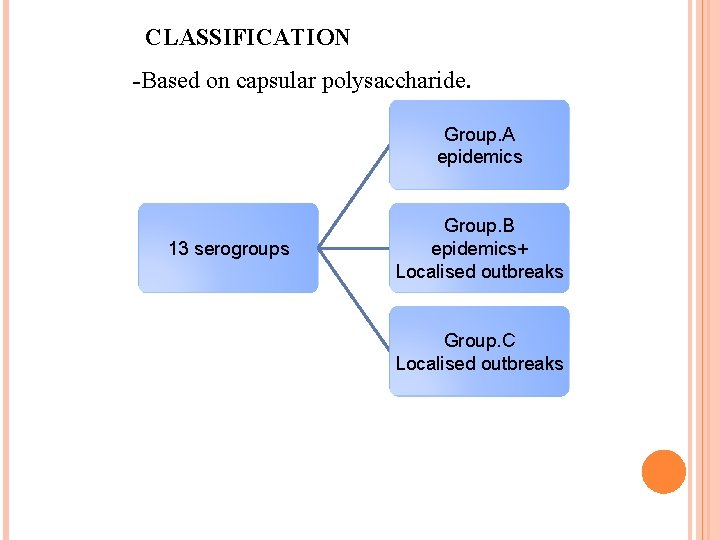
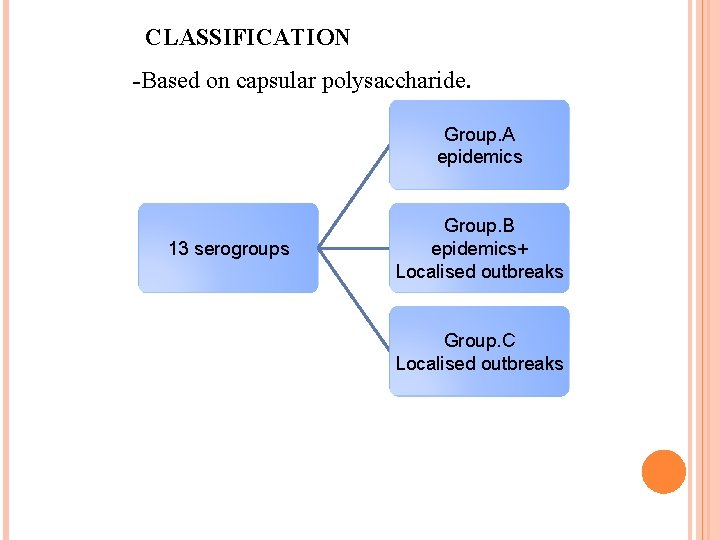
CLASSIFICATION -Based on capsular polysaccharide. Group. A epidemics 13 serogroups Group. B epidemics+ Localised outbreaks Group. C Localised outbreaks
CONTD…. Serotyping based on class 1 OMP and subtyping based on class 2 and 3 Group, type and subtype are phenotypic characteristics. Types 2, 15 and recently type 4 have been associated with group B meningococcal disease. The majority of group C meningococci belong to type 2(2 a or 2 b).
ANTIGENICITY AND VIRULENCE CAPSULE Antiphagocytic Opsonizing anti-capsular antibodies are protective. Meningococcal vaccine OUTER MEMBRANE PROTEINS 5 classes; class 5 protein(opa and opc) is involved in attachment and invasion of epithelial cells. Class 2 and 3 are major OMPs.
LIPOOLIGOSACCHARIDES Lack repeating O-Ag(Rough LPS). Lipid A moiety-portion that mediates induction of inflammatory cytokines. OTHER FACTORS: Ig. Aase Pili Iron is obtained from transferrin.
INFLAMMATORY MEDIATORS AND MOLECULES INVOLVED IN MENINGOCOCCAL DISEASE: IL-1 IL-6 IL-8 PAF PROSTAGLANDINS TNF H 2 O 2 SINGLET EXCITED OXYGEN HYDROXYL RADICAL CD 62 , ELAM-1 ICAM-1, CD 18.
PATHOGENICITY -Human pathogens –nasopharynx -Cerebrospinal meningitis -Meningococcal septicemia -Rhinitis -Pharyngitis -Conjuctivitis
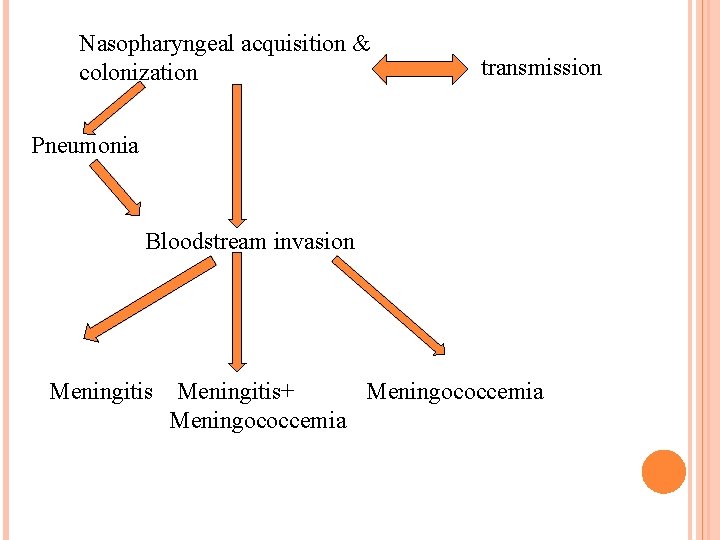
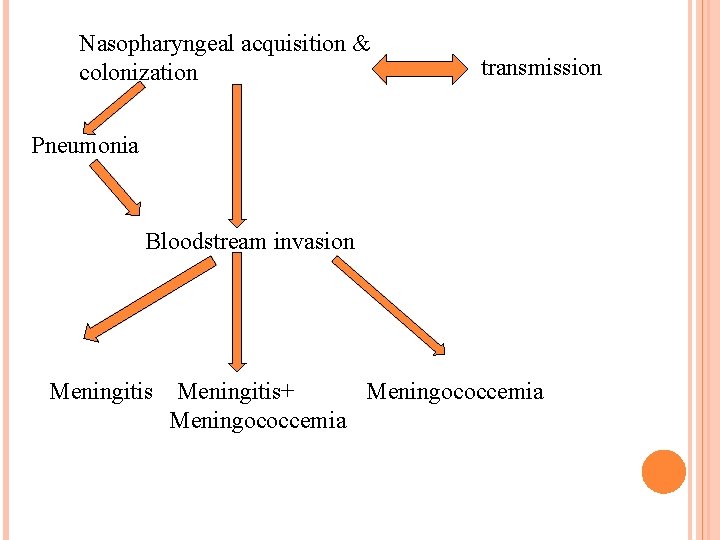
Nasopharyngeal acquisition & colonization transmission Pneumonia Bloodstream invasion Meningitis+ Meningococcemia Meningococcemia
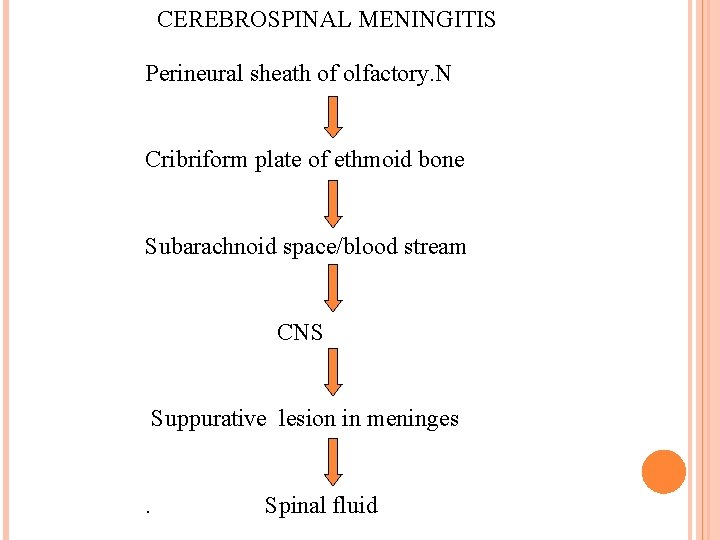
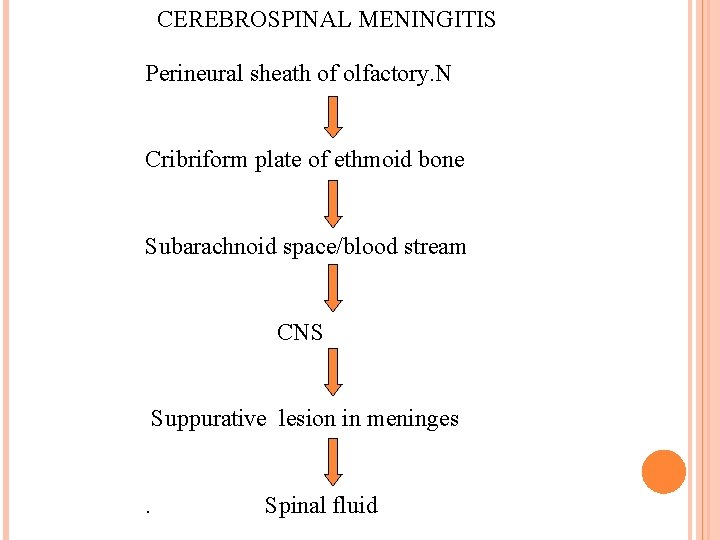
CEREBROSPINAL MENINGITIS Perineural sheath of olfactory. N Cribriform plate of ethmoid bone Subarachnoid space/blood stream CNS Suppurative lesion in meninges Spinal fluid
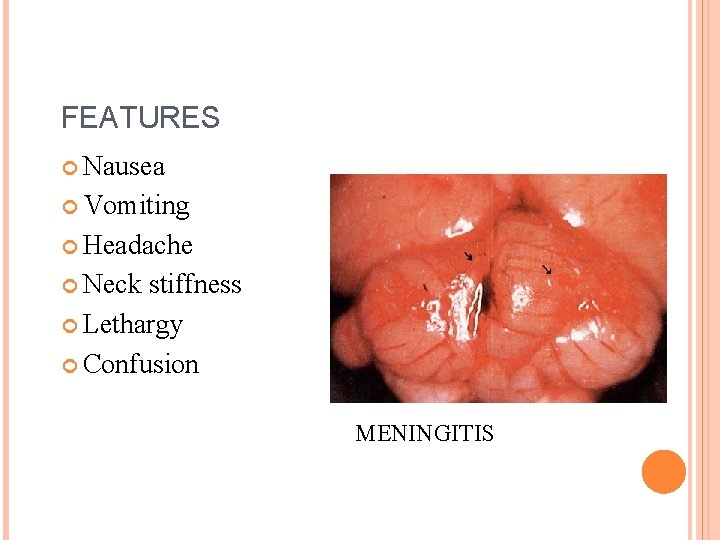
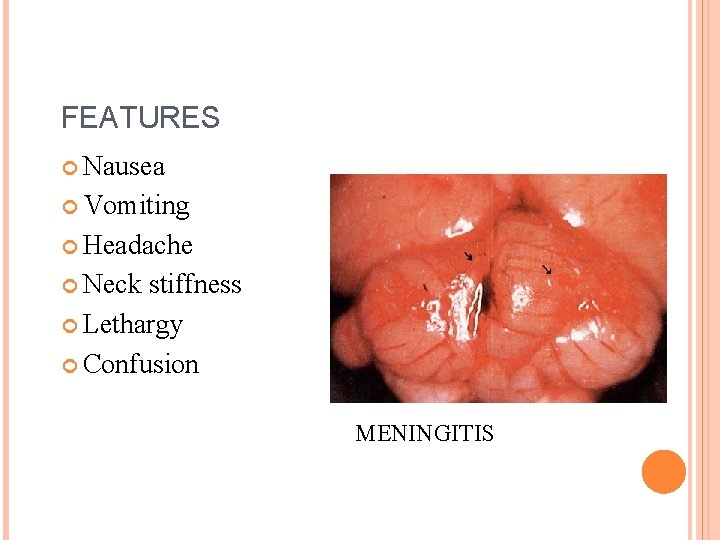
FEATURES Nausea Vomiting Headache Neck stiffness Lethargy Confusion MENINGITIS
OTHER MANIFESTATIONS Arthritis Primary meningococcal pneumonia Meningococcal pericarditis Endocarditis Conjunctivitis
COMPLICATIONS Cranial. N palsy Cortical venous thrombophlebitis Cerebral edema Children develop subdural effusion Permanent sequelae include mental retardation, deafness, hemi paresis.
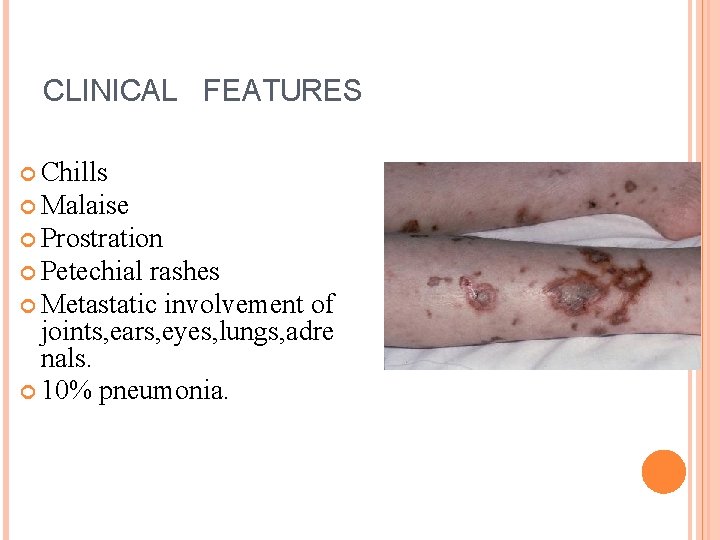
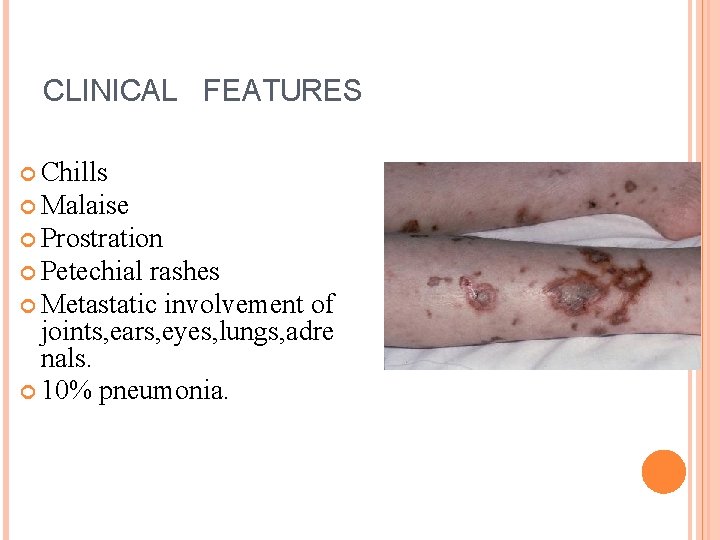
CLINICAL FEATURES Chills Malaise Prostration Petechial rashes Metastatic involvement of joints, ears, eyes, lungs, adre nals. 10% pneumonia.
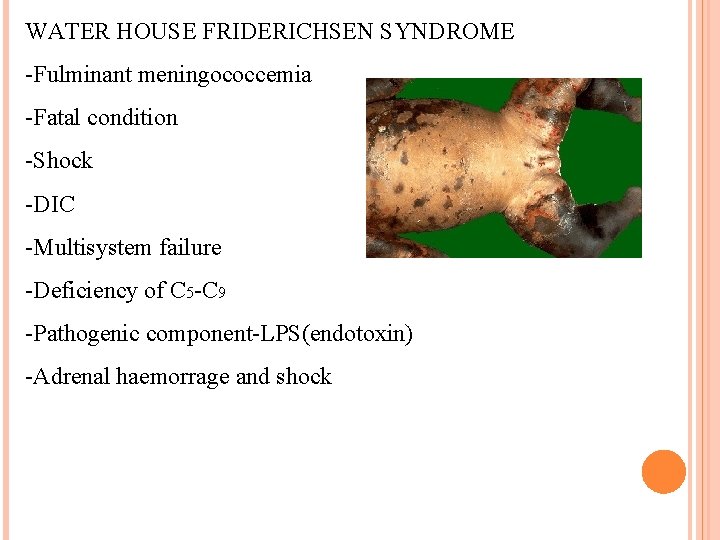
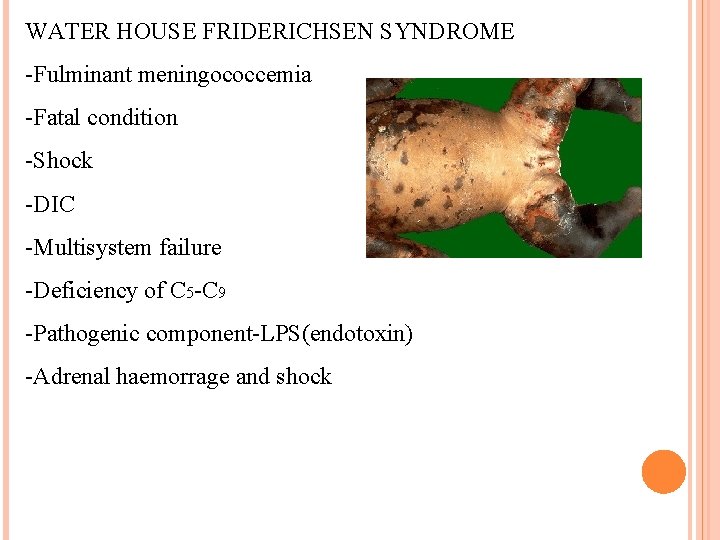
WATER HOUSE FRIDERICHSEN SYNDROME -Fulminant meningococcemia -Fatal condition -Shock -DIC -Multisystem failure -Deficiency of C 5 -C 9 -Pathogenic component-LPS(endotoxin) -Adrenal haemorrage and shock
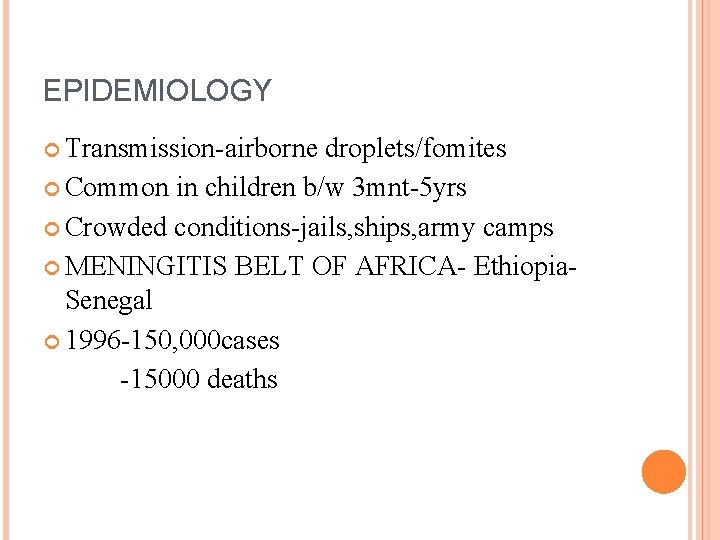
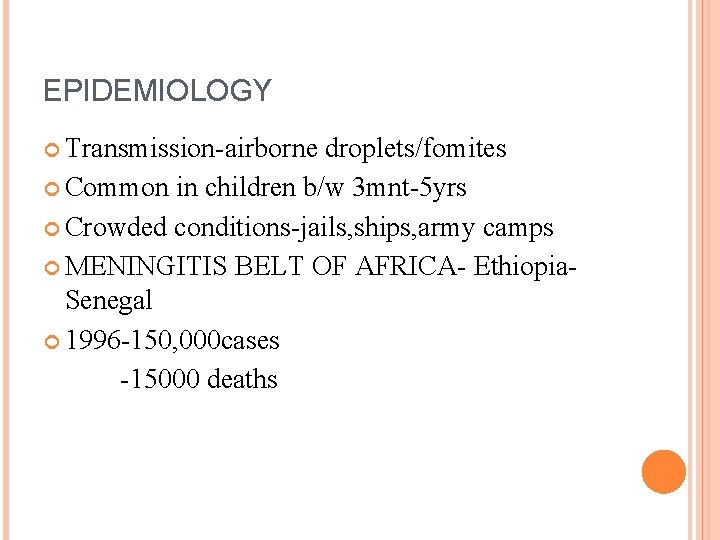
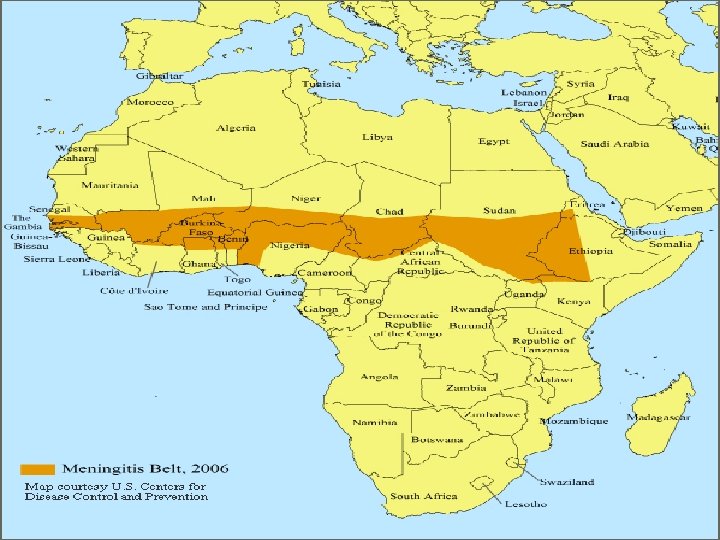
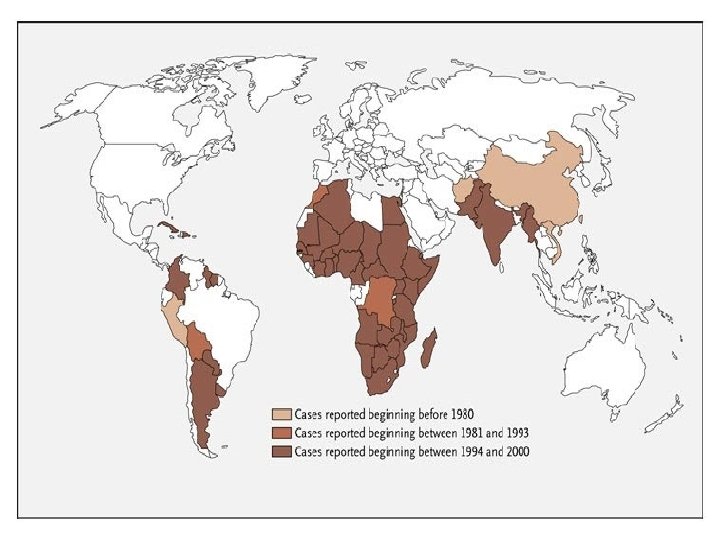
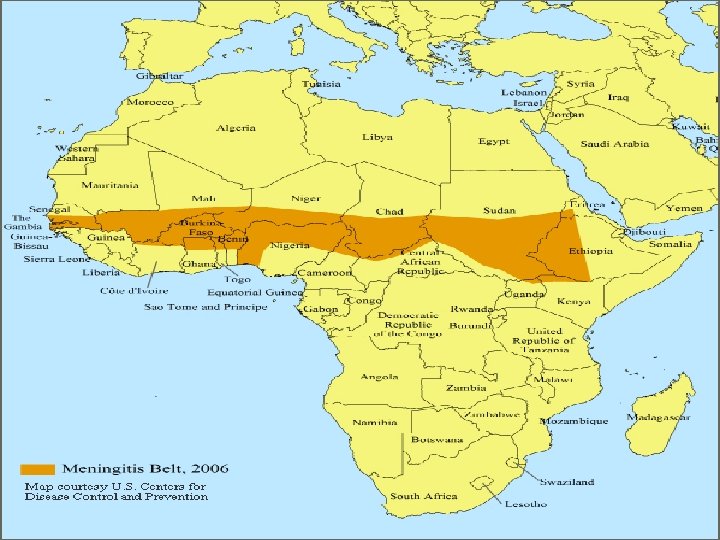
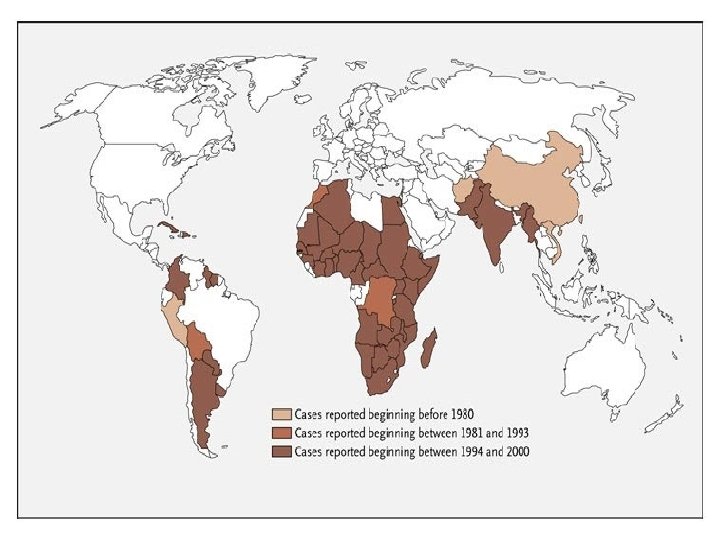
EPIDEMIOLOGY Transmission-airborne droplets/fomites Common in children b/w 3 mnt-5 yrs Crowded conditions-jails, ships, army camps MENINGITIS BELT OF AFRICA- Ethiopia- Senegal 1996 -150, 000 cases -15000 deaths
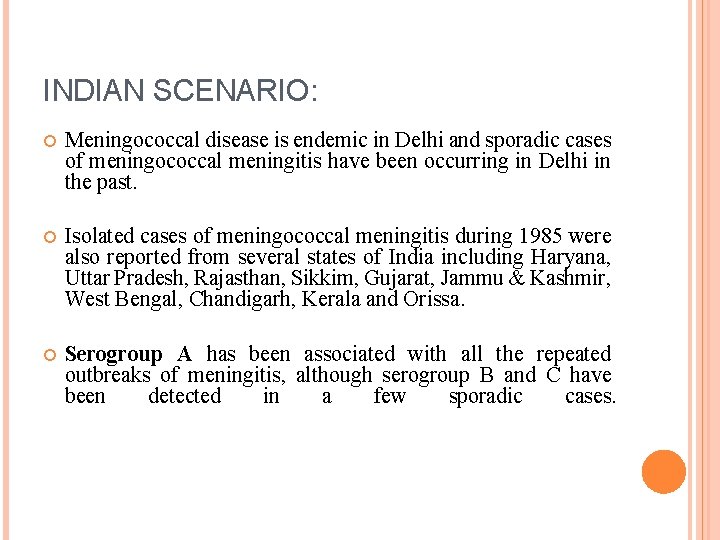
INDIAN SCENARIO: Meningococcal disease is endemic in Delhi and sporadic cases of meningococcal meningitis have been occurring in Delhi in the past. Isolated cases of meningococcal meningitis during 1985 were also reported from several states of India including Haryana, Uttar Pradesh, Rajasthan, Sikkim, Gujarat, Jammu & Kashmir, West Bengal, Chandigarh, Kerala and Orissa. Serogroup A has been associated with all the repeated outbreaks of meningitis, although serogroup B and C have been detected in a few sporadic cases.
LAB DIAGNOSIS: CSF COLLECTION
CSF EXAMINATION: General appearance: Purulent Biochemical parameters: Glucose <35 mg/100 ml , proteins 80 -500 mg/100 ml. v Cytology: 400 -20, 000 PMNs/µl. v Centrifuge the CSF sample v Plate out the deposit on BA and CA and incubate at 37ºc in 5 -10% CO 2 for 24 hours. v Add glucose broth to remaining deposit, incubate overnight and subculture in the same way. Examine the colonies by Gram stain and Oxidase test.
CONTD…. Make 2 smears of the centrifuged deposit and stain with Gram stain and methylene blue respectively. FITC coupled antiserum may be examined for the direct identification of the meningococcal serogroup responsible for infection. Divide the supernatant into 2 aliquots- one for biochemical reactions and the other for menigococcal polysaccharide antigen detection by latex agglutination, CIEP or coagglutination. Biochemical reactions v Antibiotic sensitivity testing. v Serogrouping. v v
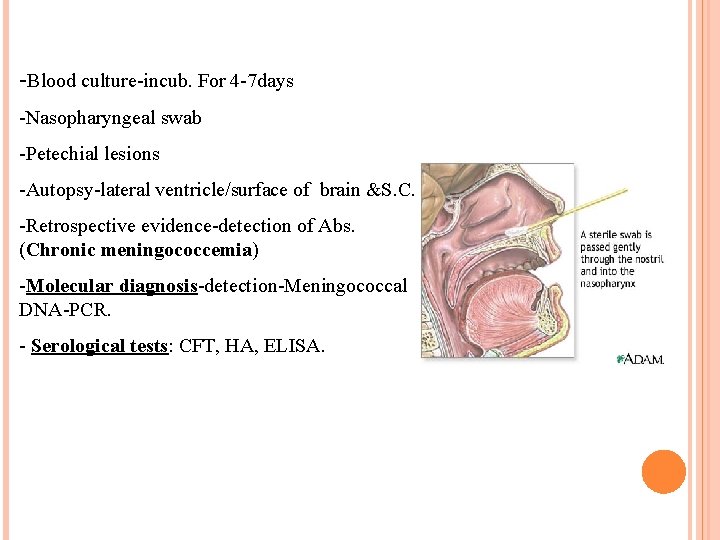
-Blood culture-incub. For 4 -7 days -Nasopharyngeal swab -Petechial lesions -Autopsy-lateral ventricle/surface of brain &S. C. -Retrospective evidence-detection of Abs. (Chronic meningococcemia) -Molecular diagnosis-detection-Meningococcal DNA-PCR. - Serological tests: CFT, HA, ELISA.
TREATMENT: Penicillin G or ceftriaxone(Confirmed cases). Emperical treatment: Upto 3 months: ampicillin+cefotaxime or ceftriaxone. 3 months to 7 years: cefotaxime or ceftriaxone. >7 years: ampicillin or penicillin G + cefotaxime or ceftriaxone. Dexamethasone may be started 15 minutes before starting antibiotics.
PREVENTION -Meningococcal polysaccharide vaccines(univalent and polyvalent vaccines). ANTIMICROBIAL PROPHYLAXIS Rifampicin , Ciprofloxacin.
VACCINES: Five serogroups, A, B, C, Y and W 135 are responsible for virtually all cases of the disease in humans. Vaccines are currently available against four of the five strains, and a vaccine against the B strain is in development. Menactra, Menomune of Sanofi-Aventis, Mencevax of Glaxo. Smith. Kline and Nm. Vac 4 -A/C/Y/W 135 (has not been licensed in the US) of JN-International Medical Corporation are the commonly used vaccines. Vaccines offer significant protection from three to five years (plain polysaccharide vaccine Menomune, Mencevax and Nm. Vac-4) to more than eight years (conjugate vaccine Menactra).
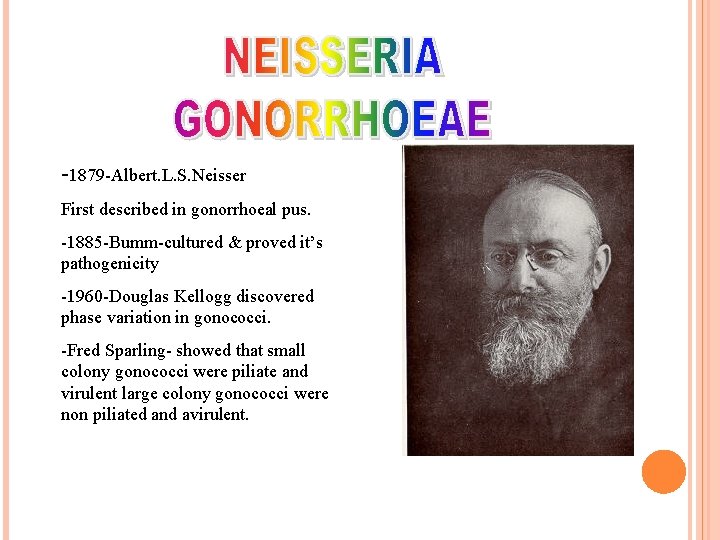
-1879 -Albert. L. S. Neisser First described in gonorrhoeal pus. -1885 -Bumm-cultured & proved it’s pathogenicity -1960 -Douglas Kellogg discovered phase variation in gonococci. -Fred Sparling- showed that small colony gonococci were piliate and virulent large colony gonococci were non piliated and avirulent.
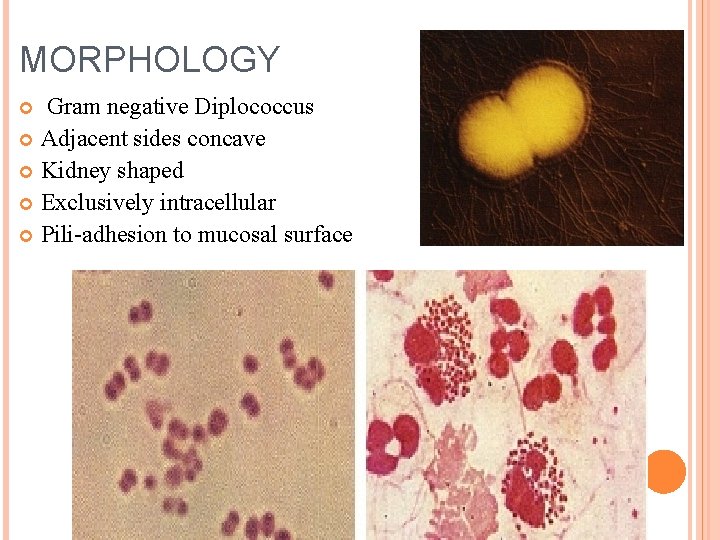
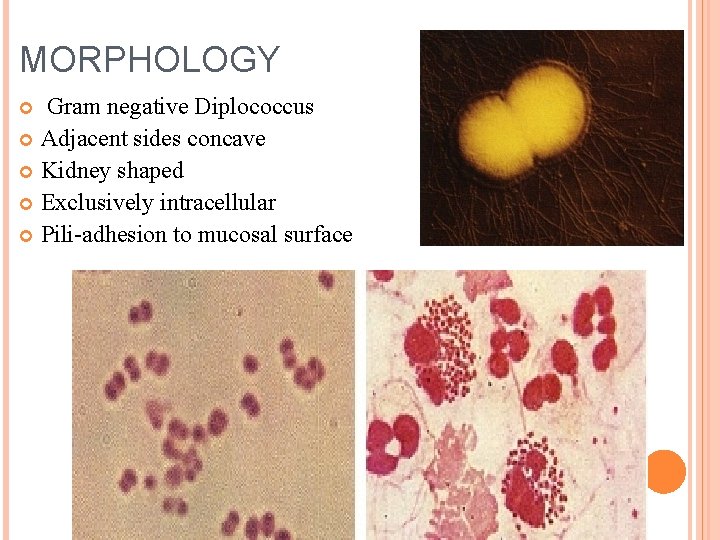
MORPHOLOGY Gram negative Diplococcus Adjacent sides concave Kidney shaped Exclusively intracellular Pili-adhesion to mucosal surface
CULTURAL CHARACTERISTICS Aerobes/ facultative anaerobes p. H -7. 2 -7. 6 Temp. 35ºc-36ºc 5 -10% CO 2 Chocolate agar, Mueller-hinton agar, Thayer martin media, Modified TM medium, Modified NYCM.
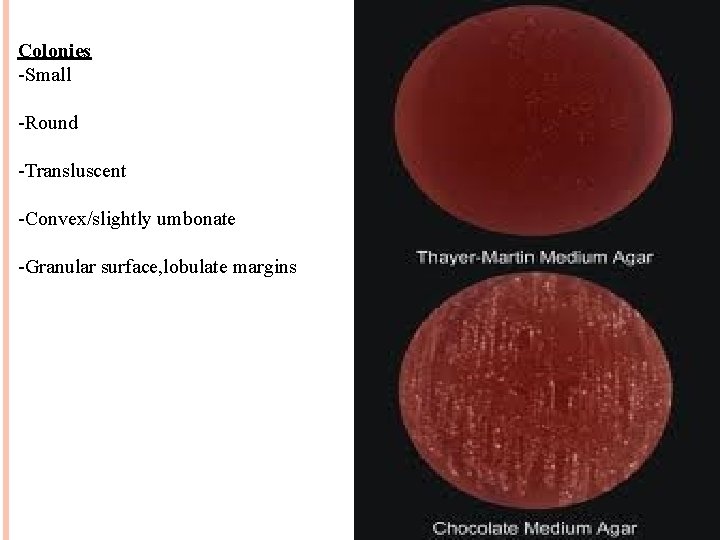
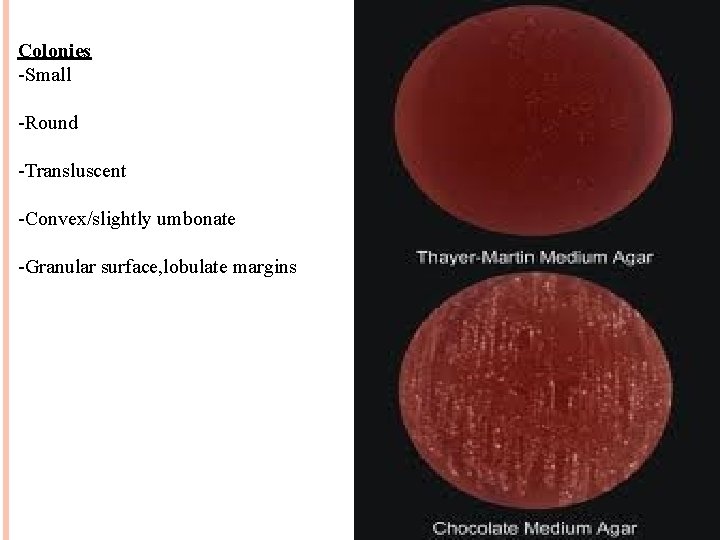
Colonies -Small -Round -Transluscent -Convex/slightly umbonate -Granular surface, lobulate margins
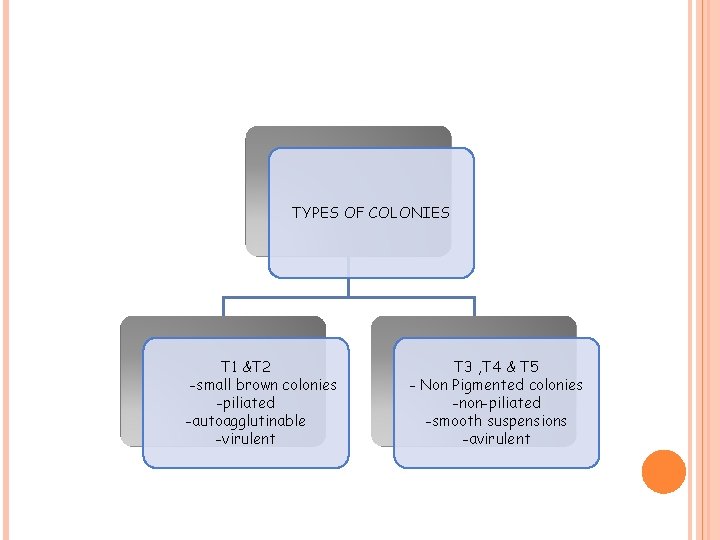
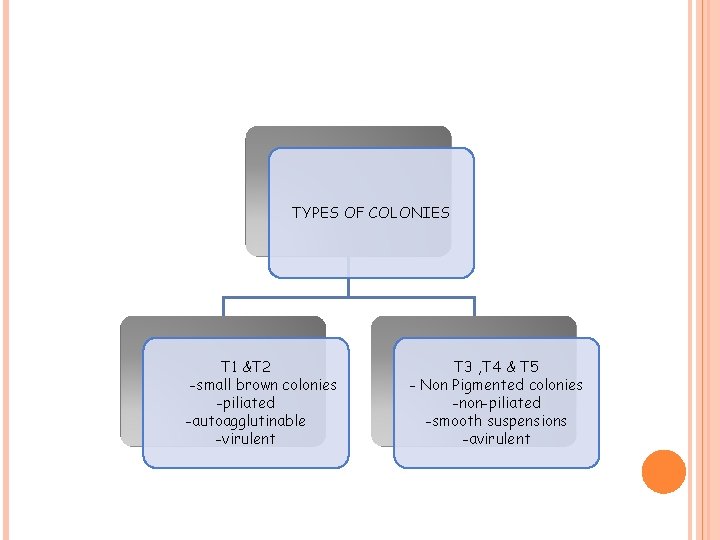
TYPES OF COLONIES T 1 &T 2 -small brown colonies -piliated -autoagglutinable -virulent T 3 , T 4 & T 5 - Non Pigmented colonies -non-piliated -smooth suspensions -avirulent
BIOHEMICAL FEATURES: Utilize only glucose. Catalase positive. Oxidase positive. Superoxol test positive
RESISTANCE Delicate Killed-heat, drying, antiseptics. Dies-1 -2 hrs outside the body in exudates. Cultures dies-3 -4 days. Survives-slant culture-35˚c-sterile paraffin wax. Stored-(-70˚c) for yrs.
ANTIBIOTIC RESISTANCE: Chromosomally resistant N. gonorrhoeae(CMRNG). PPNG(Penicillinase producing N. gonorrhoeae): Mainly 3. 2 MDa and 4. 4 MDa plasmids(TEM-1 β lactamase). Tetracycline resistant N. gonorrhoeae(TTNG): 25. 2 MDa plasmid- tet. M gene.
ANTIGENIC PROPERTIES -Pili -Hair-like structure -Composed of repeating peptides subunits(pilins). Pilins contain 159 amino acids. -Cyanogen bromide digestion has recognized 3 regions. Region 2 is receptor binding region and 3 is type specific region.
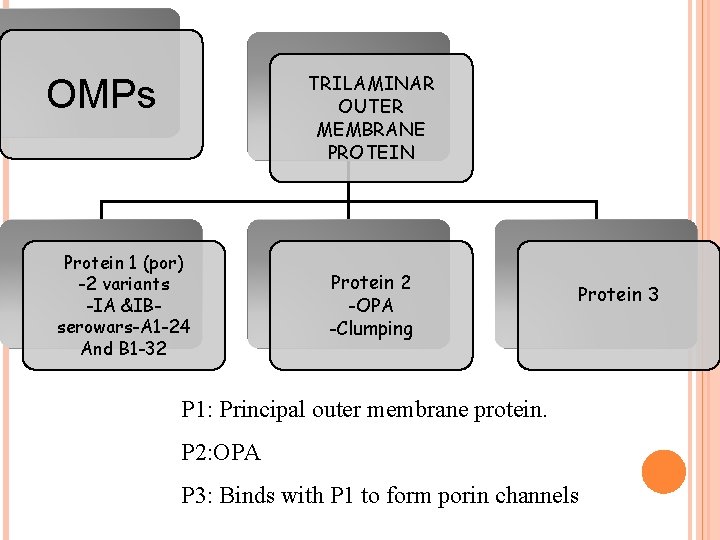
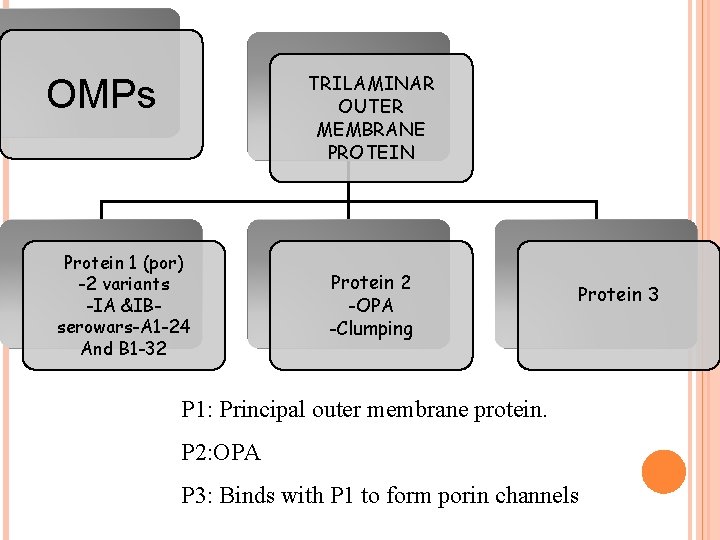
TRILAMINAR OUTER MEMBRANE PROTEIN OMPs Protein 1 (por) -2 variants -IA &IBserowars-A 1 -24 And B 1 -32 Protein 2 -OPA -Clumping Protein 3 P 1: Principal outer membrane protein. P 2: OPA P 3: Binds with P 1 to form porin channels
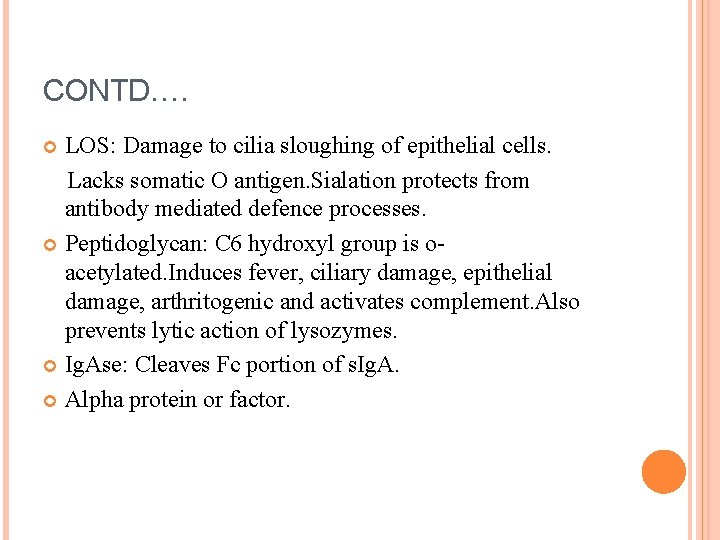
CONTD…. LOS: Damage to cilia sloughing of epithelial cells. Lacks somatic O antigen. Sialation protects from antibody mediated defence processes. Peptidoglycan: C 6 hydroxyl group is oacetylated. Induces fever, ciliary damage, epithelial damage, arthritogenic and activates complement. Also prevents lytic action of lysozymes. Ig. Ase: Cleaves Fc portion of s. Ig. A. Alpha protein or factor.
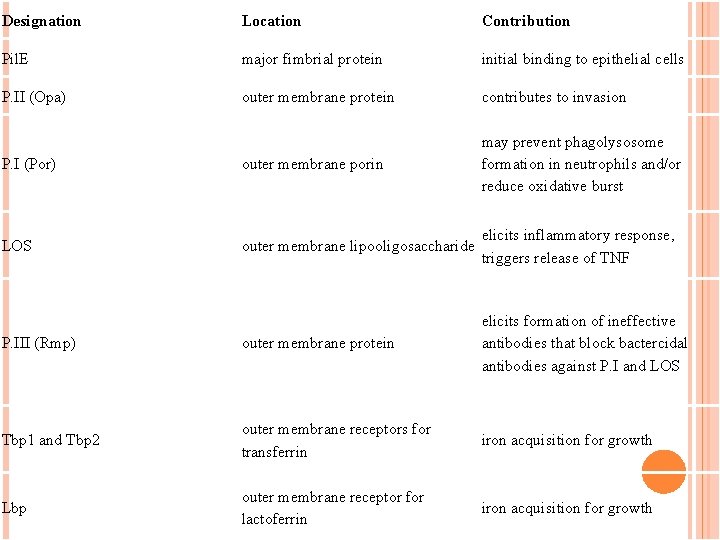
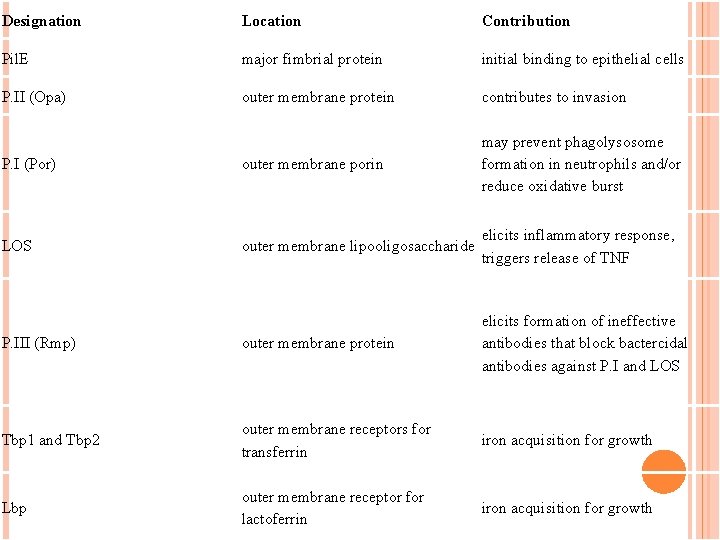
Designation Location Contribution Pil. E major fimbrial protein initial binding to epithelial cells P. II (Opa) outer membrane protein contributes to invasion P. I (Por) outer membrane porin may prevent phagolysosome formation in neutrophils and/or reduce oxidative burst LOS outer membrane lipooligosaccharide elicits inflammatory response, triggers release of TNF P. III (Rmp) outer membrane protein elicits formation of ineffective antibodies that block bactercidal antibodies against P. I and LOS Tbp 1 and Tbp 2 outer membrane receptors for transferrin iron acquisition for growth Lbp outer membrane receptor for lactoferrin iron acquisition for growth
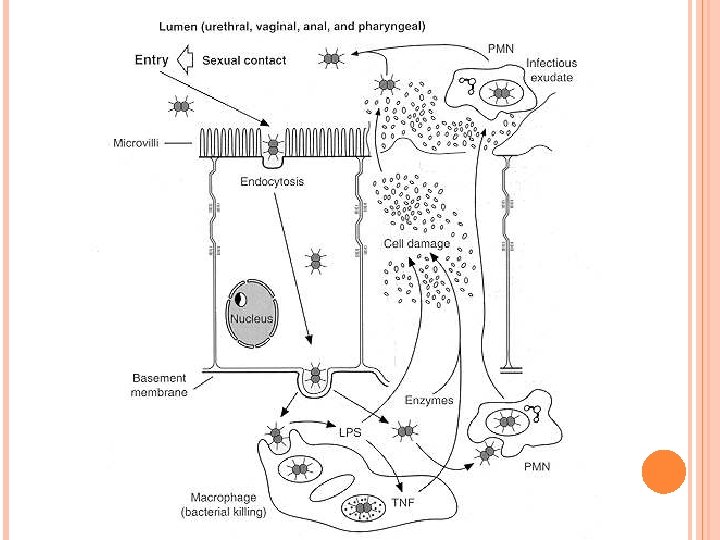
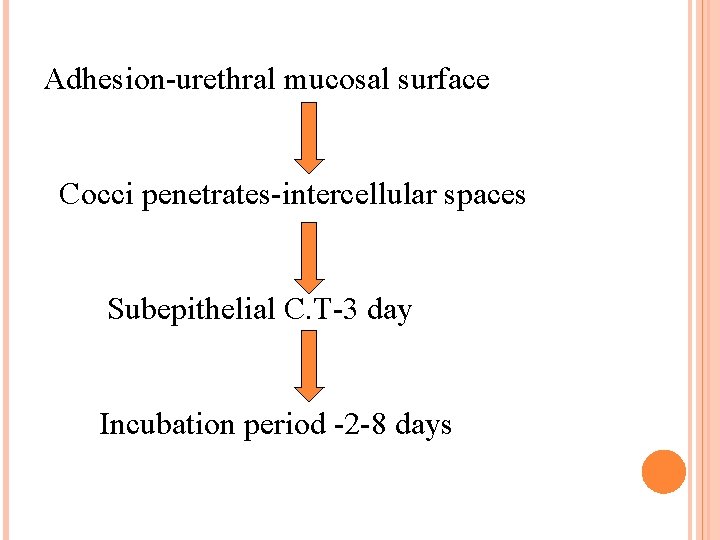
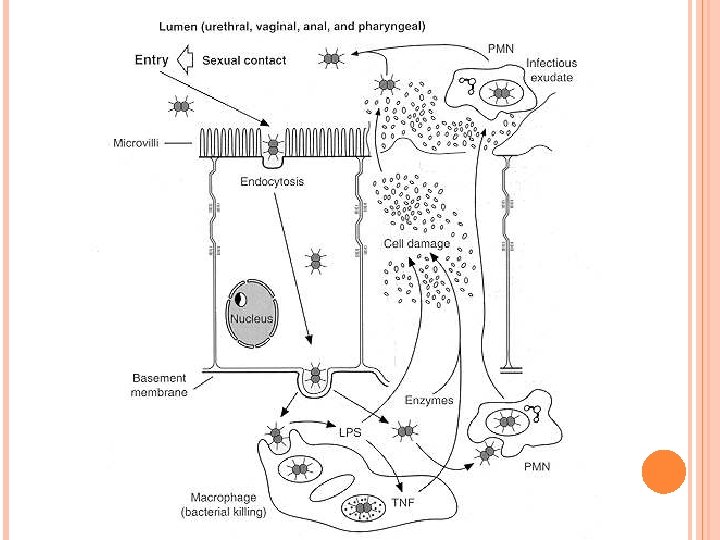
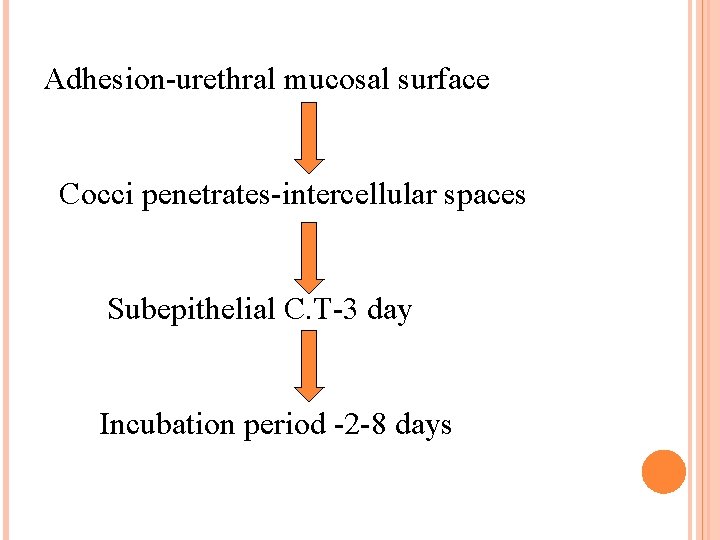
Adhesion-urethral mucosal surface Cocci penetrates-intercellular spaces Subepithelial C. T-3 day Incubation period -2 -8 days
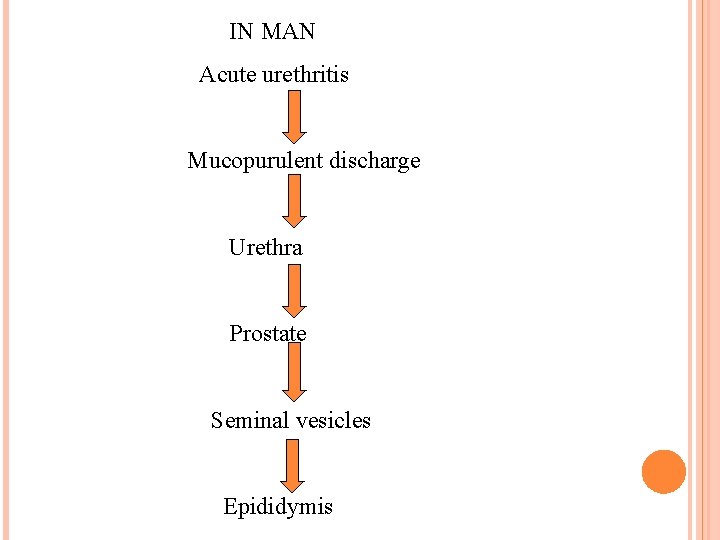
IN MAN Acute urethritis Mucopurulent discharge Urethra Prostate Seminal vesicles Epididymis
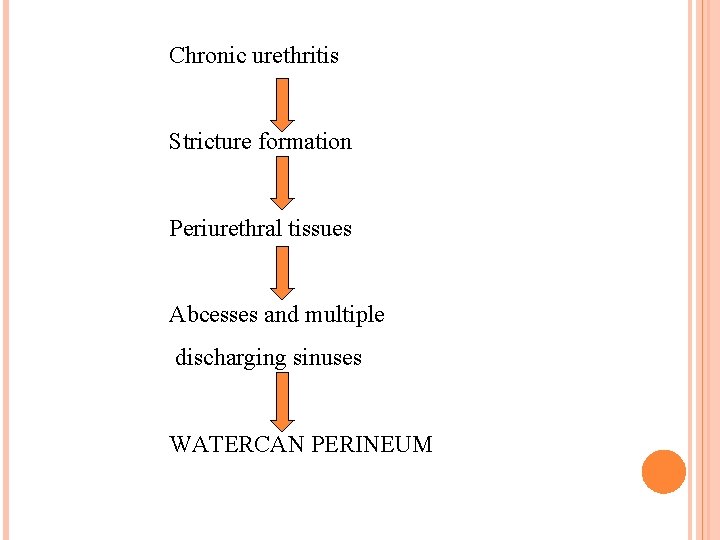
Chronic urethritis Stricture formation Periurethral tissues Abcesses and multiple discharging sinuses WATERCAN PERINEUM
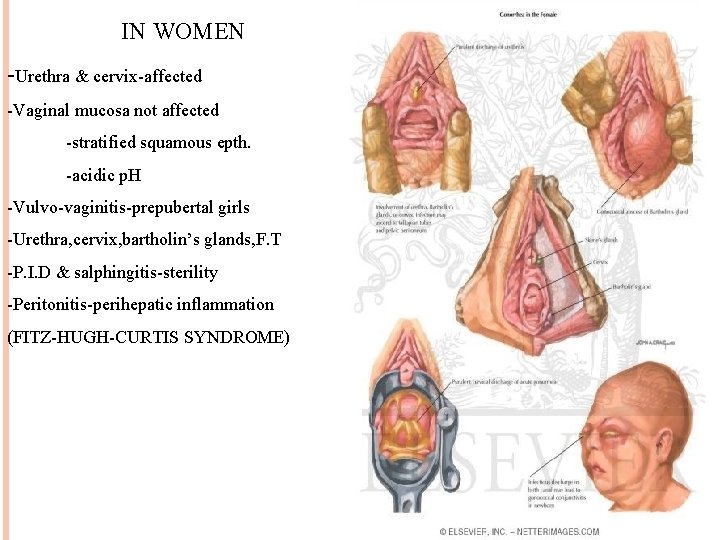
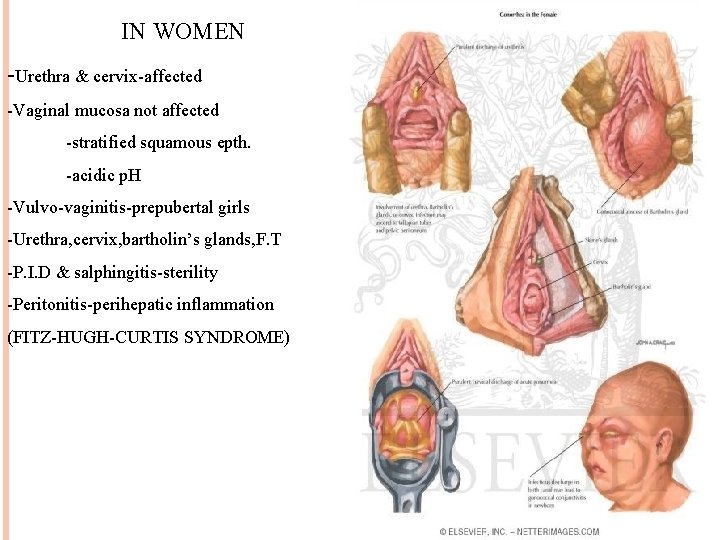
IN WOMEN -Urethra & cervix-affected -Vaginal mucosa not affected -stratified squamous epth. -acidic p. H -Vulvo-vaginitis-prepubertal girls -Urethra, cervix, bartholin’s glands, F. T -P. I. D & salphingitis-sterility -Peritonitis-perihepatic inflammation (FITZ-HUGH-CURTIS SYNDROME)
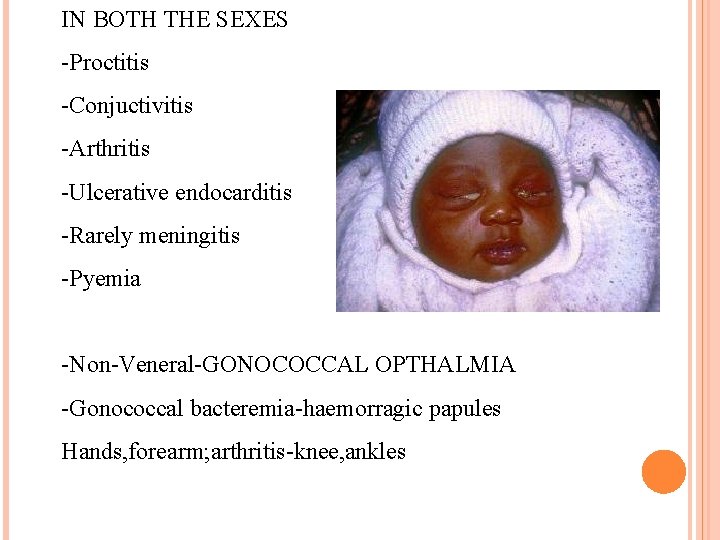
IN BOTH THE SEXES -Proctitis -Conjuctivitis -Arthritis -Ulcerative endocarditis -Rarely meningitis -Pyemia -Non-Veneral-GONOCOCCAL OPTHALMIA -Gonococcal bacteremia-haemorragic papules Hands, forearm; arthritis-knee, ankles
ANORECTAL GONORRHOEA -Anorectal pain/pruritus -Tenesmus -Purulent rectal discharge -Rectal bleeding PHARYNGEAL GONORRHOEA OCULAR GONORRHOEA -Autoinoculation-from infected site
EPIDEMIOLOGY Source-human carrier Mode of infection-venereal Non-venereal-OPHTHALMIA NEONATORUM 1% Silver nitrate-CREDE’S METHOD 1970 -Global incidence-16 million Higher in B-blood group people. Most common in the age group of 15 -29 years. Risk factors include unprotected intercourse and multiple sexual partners. Proctitis , throat infections , arthritis and disseminated infections can also be seen.
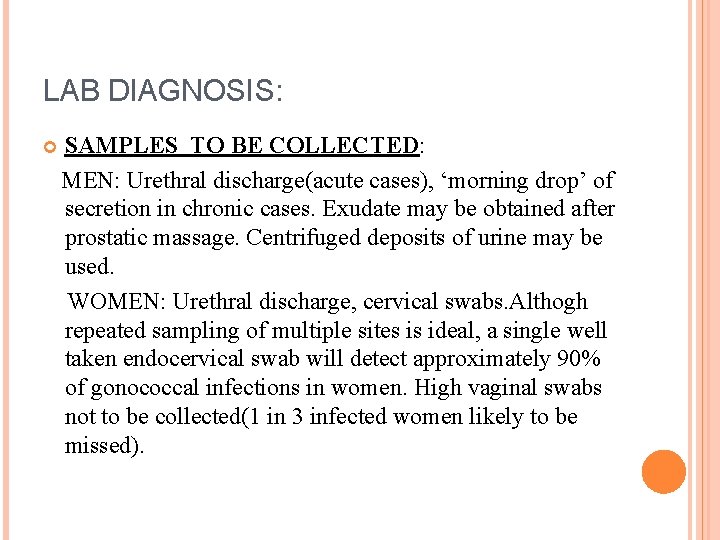
LAB DIAGNOSIS: SAMPLES TO BE COLLECTED: MEN: Urethral discharge(acute cases), ‘morning drop’ of secretion in chronic cases. Exudate may be obtained after prostatic massage. Centrifuged deposits of urine may be used. WOMEN: Urethral discharge, cervical swabs. Althogh repeated sampling of multiple sites is ideal, a single well taken endocervical swab will detect approximately 90% of gonococcal infections in women. High vaginal swabs not to be collected(1 in 3 infected women likely to be missed).
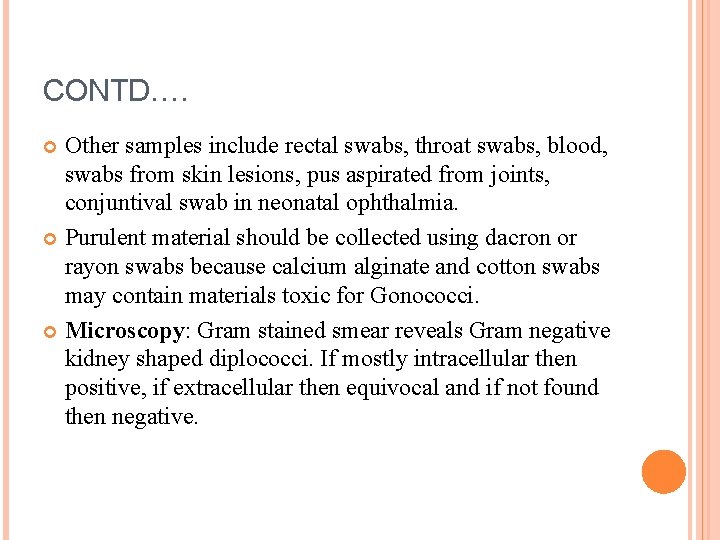
CONTD…. Other samples include rectal swabs, throat swabs, blood, swabs from skin lesions, pus aspirated from joints, conjuntival swab in neonatal ophthalmia. Purulent material should be collected using dacron or rayon swabs because calcium alginate and cotton swabs may contain materials toxic for Gonococci. Microscopy: Gram stained smear reveals Gram negative kidney shaped diplococci. If mostly intracellular then positive, if extracellular then equivocal and if not found then negative.
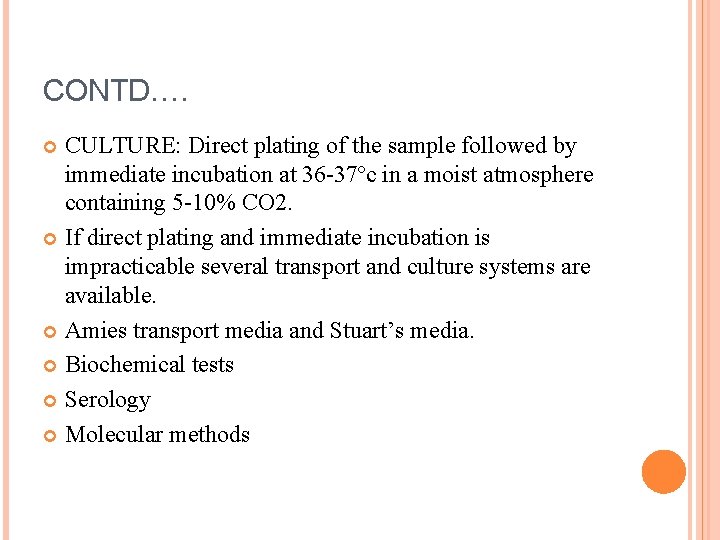
CONTD…. CULTURE: Direct plating of the sample followed by immediate incubation at 36 -37ºc in a moist atmosphere containing 5 -10% CO 2. If direct plating and immediate incubation is impracticable several transport and culture systems are available. Amies transport media and Stuart’s media. Biochemical tests Serology Molecular methods
TREATMENT AND PROPHYLAXIS: Ceftriaxone+ doxycycline/tetracycline/azithromycin. If penicillin sensitive ( NON PPNG) then amoxycillin+probenecid and doxycycline. No effective vaccine. Health education, contact tracing , monogamy and use of condoms are the only preventive measures.
OTHER NEISSERIA SPECIES: N. elongata ssp nitroreducens N. weaveri ssp nov N. gonorrhoeae ssp kochii N. flavescens N. mucosa
MORAXELLA: Moraxella sps were formerly called Neisseria and later Branhamella sps. Separated from Neisseriae based on DNA base composition, fatty acid composition and inability to produce acid from carbohydrates. Moraxellas may be involved in opportunistic infections in compromised patients. These occur as components of the normal flora of the upper respiratory tract, the conjuntiva, the skin and genital tract.
MORAXELLA CATARRHALIS: Oval Gram negative cocci about 0. 8µm in size. May occur singly, but majority of these are diplococci with adjacent sides flattened. Sometimes these may occur in groups of 4. May be found within polymorphonuclear leucocytes. Aerobes Non sporing, non capsulate and non motile. Optimum temperature is 36ºc but many strains may grow at 22οc. CO 2 is not an absolute requirement. Most srains grow on Nutrient agar.
CONTD…. Some strains grow on selective media for pathogenic Neisseriae. Colonies on Blood agar or Chocolate agar are 1 -2 mm in size, non haemolytic, friable, white or greyish, convex with an entire margin later becoming irregular. After 48 hours colonies are larger, more elevated with a raised opaque centre. Oxidase positive Catalase positive Do not utilize carbohydrates.
CONTD…. Reduce nitrates to nitrites. Produce DNase. More resistant than meningococcus and gonococcus. Cultures may remain viable for several months at 20^c if prevented from drying. May survive in sputum for 3 -4 weeks. Susceptible to a wide range of antibiotics but many strains produce β-lactamase and are resistant to penicillin and ampicillin.
CONTD…. It is found in the respiratory tracts of 1. 5 -5. 4% of healthy young and middle-aged adults, 26. 5% of healthy elderly people and 50. 8% of healthy children. It is therefore recognized as a significant potential pathogen of the respiratory tract, including the sinuses, bronchi and larynx. 20% of the cases of sinusitis are due to M. catarrhalis. Chronic bronchitis among smokers is often caused by M. catarrhalis. Although laryngitis is often caused by this organism, about 90% of cases are due to viruses.
LAB DIAGNOSIS: (1)Specimens collected are sputum and transtracheal aspirates. (2) Microscopy (3) Culture(some strains on selective media used for pathogenic Neisseriae). (4) Oxidase test, RCUT test, test for β-lactamase production.
OTHER MORAXELLA SPECIES Moraxella lacunata: Causes purulent conjuntivitis(angular blepharoconjuntivitis). Moraxella lacunata and M. atlantae require serum for growth. Loefflers medium supports the growth of M. lacunata and M. liquifaciens. Moraxella lacunata produces gelatinase.
OLIGELLA: Recently delineated from Moraxella on the basis of DNA: Rrna hybridization and serological tests. O. urethralis is a rare cause of septic arthritis. Can be misidentified as N. gonorrhoeae as it is nonmotile, Gram negative diplococcus, both oxidase and catalase positivewhich will grow on Thayer-Martin medium. However, Oligella will grow on Mac Conkeys agar.
REFERENCES: Saunder’s text and review series by: T. Stuart Walker. Mackie & Mc Cartney Practical Medical Microbiology-14 th edition Jawetz Medical Microbiology-24 th edition. Bailey & Scott’s Diagnostic Microbiology-12 th edition. Textbook of Microbiology by Ananthanarayan and Paniker-8 th edition. Color atlas & textbook of diagnostic microbiology(Elmer. W. Koneman)-5 th edition
CONTD…. Todar’s online textbook of bacteriology Internet
