Graduate Medical Education GME Policy Mark D Schwartz
![IME = c * [(1 + IRB ratio) 0. 405 -1] • Percentage add-on IME = c * [(1 + IRB ratio) 0. 405 -1] • Percentage add-on](https://slidetodoc.com/presentation_image_h2/e0d0f4a17cbaa3b0c0cadc555e615a44/image-8.jpg)
- Slides: 25
Graduate Medical Education (GME) Policy Mark D Schwartz MD
US Graduate Medical Education • GME in the US is the envy of the world, graduating >100, 000 new physicians for practice annually • However, there is broad consensus* that current GME policy and practice are not well aligned with the needs of the US healthcare system in the 21 st century *Inglehart JK. Financing Graduate Medical Education — Mounting Pressure for Reform. N Engl J Med 2012; 366: 1562 -1563.
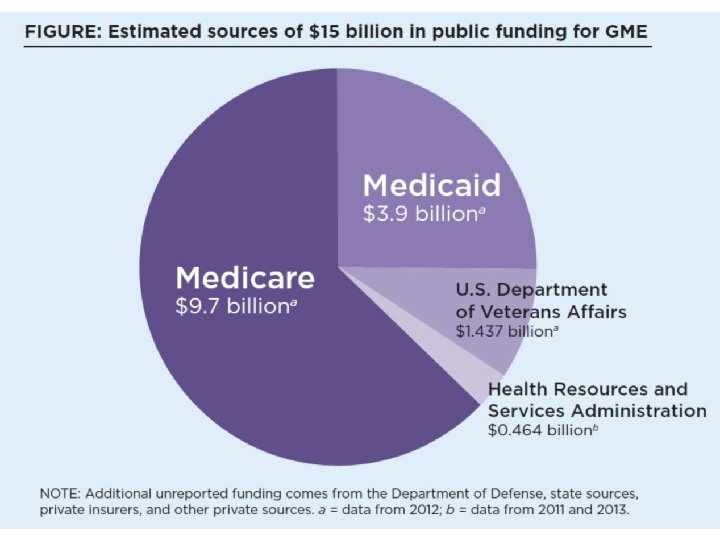
GME Policy Problems • Poor alignment of GME funding policy and US workforce needs • Inadequate accountability by hospitals and GME programs for outcomes • No transparency regarding use of funds by hospitals • Inadequate curricular focus on competencies needed for healthcare reform
GME Policy History • Pre 1965, hospitals had professional and financial responsibility for GME • Medicare founded – inappropriate to pay for GME with health care funds – Founders reluctantly decided Medicare would temporarily pay its share as educational activities enhance value of patient care • Medicare GME funding securely ensconced, with payments from the Medicare trust fund (Part A) – 1984 GME incorporated into IPPS (DRG)
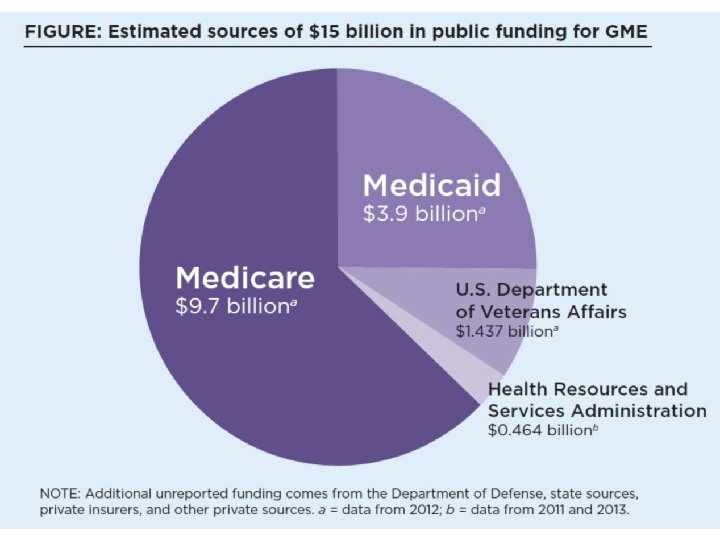
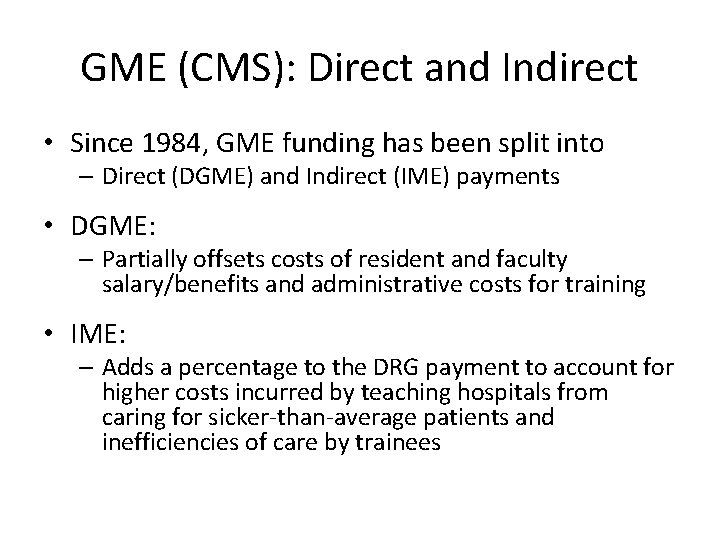
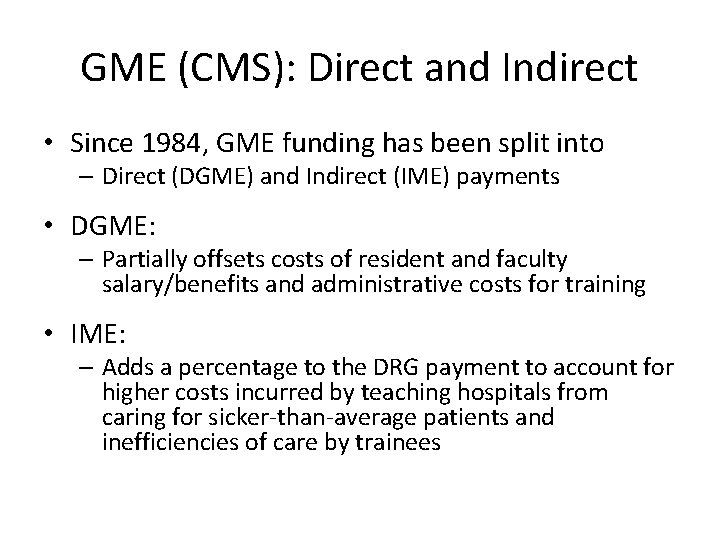
GME (CMS): Direct and Indirect • Since 1984, GME funding has been split into – Direct (DGME) and Indirect (IME) payments • DGME: – Partially offsets costs of resident and faculty salary/benefits and administrative costs for training • IME: – Adds a percentage to the DRG payment to account for higher costs incurred by teaching hospitals from caring for sicker-than-average patients and inefficiencies of care by trainees
DGME = # Residents * PRA * Medicare Share • # of Residents: 3 -year rolling average/hospital – Aggregate residency FTEs capped at 1996 levels • PRA: Per-Resident Amount from 1984 base year, updated annually by Consumer Price Index – 1. 0 FTE for initial residency period (IRP), minimum required for board eligibility, usually first 3 years – 0. 5 FTE beyond IRP (subspecialty fellowship) • Medicare Share: proportion of Medicare beneficiary inpatient/total inpatient days
![IME c 1 IRB ratio 0 405 1 Percentage addon IME = c * [(1 + IRB ratio) 0. 405 -1] • Percentage add-on](https://slidetodoc.com/presentation_image_h2/e0d0f4a17cbaa3b0c0cadc555e615a44/image-8.jpg)
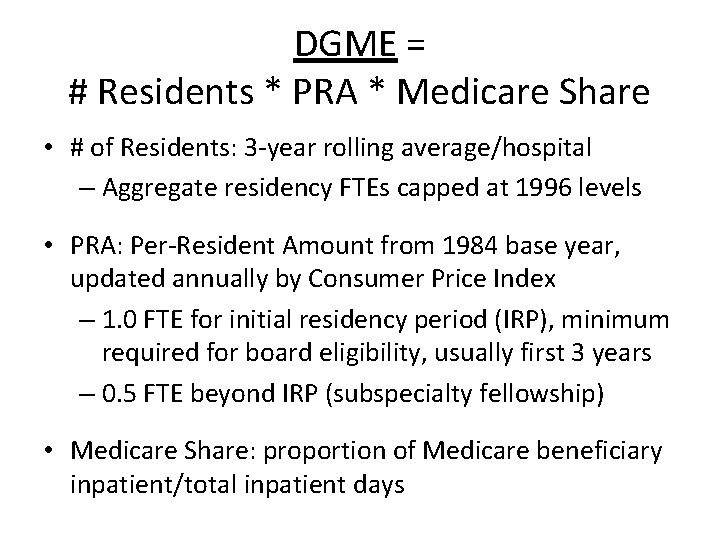
IME = c * [(1 + IRB ratio) 0. 405 -1] • Percentage add-on to Medicare DRG payment to adjust for teaching intensity – IRB: intern/resident to bed ratio – C is an IME multiplier set by policy; c=1. 34 5. 5% increase in IME adjustment for every 10% increase in IRB • ~1, 100 hospitals get IME adjustments to IPPS payments ranging from <1% to 48% – ~200 hospitals get 2/3 of the funds • Med. PAC’s calculation is that across all hospitals, a 10% increase in teaching intensity (IRB) is associated with only a 2. 7% increase in Medicare costs per discharge
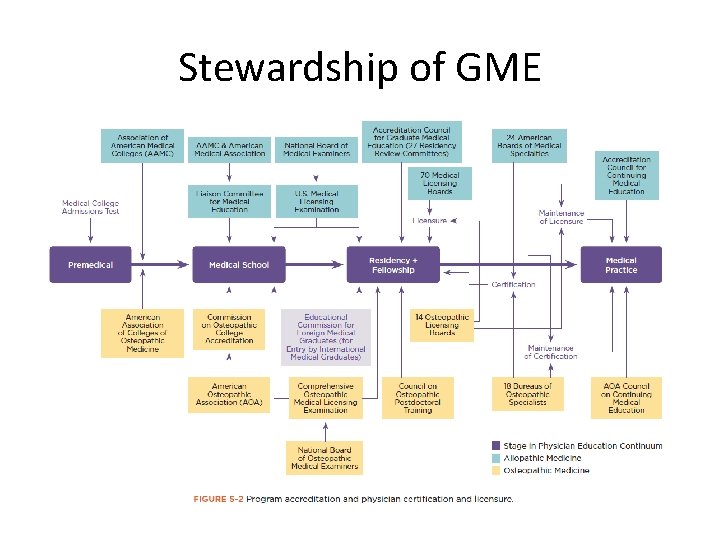
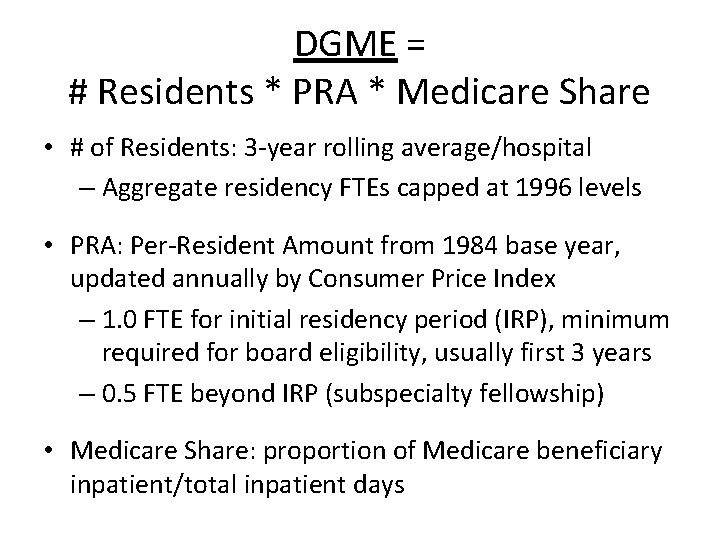
Stewardship of GME
Core Policy Questions • Is GME a public good or a hospital cost? • Is GME an educational or patient care expense? • What is the appropriate role for Medicare in supporting GME? • Should Medicare GME shape the physician workforce? • Should Medicare GME remain mandatory spending (Part A) vs. discretionary spending?
GME Policy Strategies • Market-based approach – Government hands off educational policy and workforce distribution • Regulatory approach – Government drives GME outcomes • Incentive-based approach – Influence GME via funding policy
GME Constituencies Advisory Organizations • Med. PAC • COGME • NAM (IOM) Stakeholders • AAMC (& AHA) • ACGME • Every specialty society…
Advisory Organizations • Med. PAC - Medicare Payment Advisory Commission – Independent agency established by the Balanced Budget Act of 1997 to advise Congress on Medicare • COGME - Council on Graduate Medical Education (HRSA) – Authorized by Congress (1986) to assess physician workforce trends, training issues and financing policies • NAM – National Academy of Medicine (NAS) – Established 1970 as IOM, non-partisan, independent advisor to the US (“Supreme Court of Science”)
Med. PAC • Hold back $3. 5 B and pay out via pay for performance program as per Secretary’s standards and metrics • HHS should collect data and publish annual report GME funding, costs, and use per institution • HHS to report on financial impact of GME on institutions with focus on variable impact by specialty • Conduct workforce analysis number and mix of physicians needed in US
COGME • Increase PC physicians in the US to 40% (from 32%) • Increase reimbursement for PC physicians from 54% to 70% of that for all other physicians (as in 1990 s) • Medical schools should develop an accountable mission statement and measures of social responsibility … to foster a physician workforce of 40% PC • Increase # of PC training slots (Title VII) and move more training into ambulatory, community practice environment • Expand focus on geographic and socioeconomic distribution – NHSC, Title VII, and CHC funds
Stakeholders • AAMC - Association of American Medical Colleges (1876) – Private, independent, non-profit representing all medical schools and teaching hospitals – Hospital Community • AHA – American Hospital Association (non-profits) • FAH - Federation American Hospitals (for-profits, 20%) • ACGME - Accreditation Council for Graduate Medical Education – Private, independent, non-profit responsible for GME accreditation
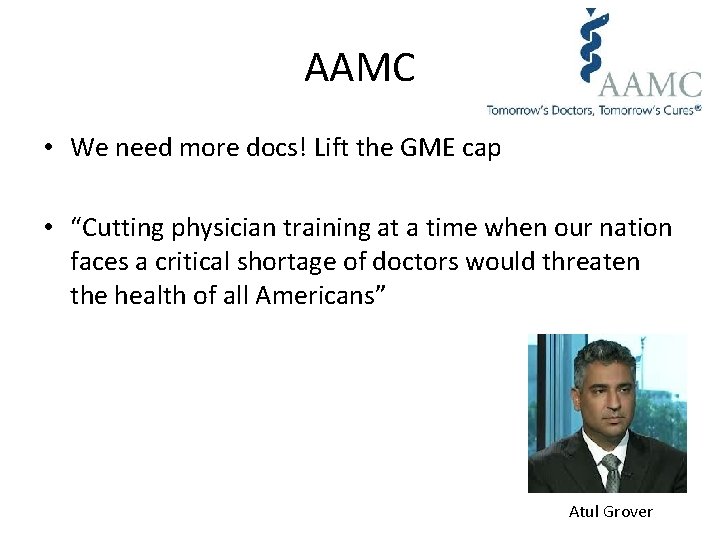
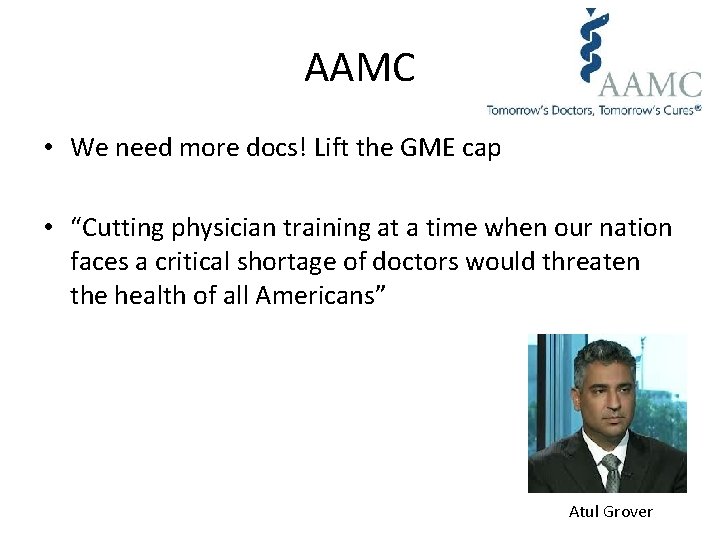
AAMC • We need more docs! Lift the GME cap • “Cutting physician training at a time when our nation faces a critical shortage of doctors would threaten the health of all Americans” Atul Grover
ACGME • Evaluates and accredits more than 9, 000 GME programs in 135 specialties and subspecialties • CEO Tom Nasca – ACGME will transform GME – Self-regulation > federal funding policy
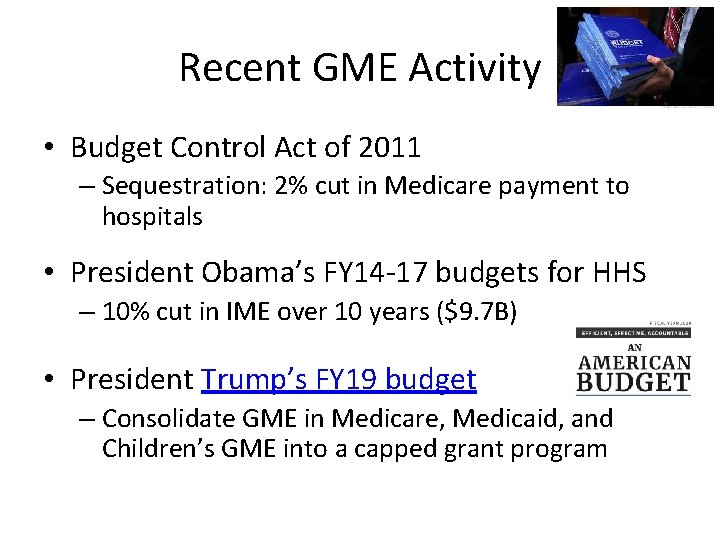
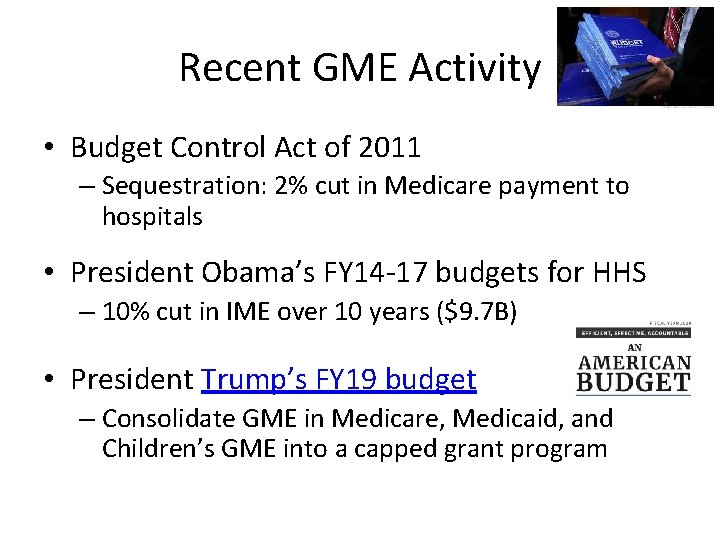
Recent GME Activity • Budget Control Act of 2011 – Sequestration: 2% cut in Medicare payment to hospitals • President Obama’s FY 14 -17 budgets for HHS – 10% cut in IME over 10 years ($9. 7 B) • President Trump’s FY 19 budget – Consolidate GME in Medicare, Medicaid, and Children’s GME into a capped grant program
Resident Physician Shortage Reduction Act of 2017 • S. 1148: Sen. Bill Nelson (D-FL) – 4 bipartisan cosponsors (Sen. Schumer) • H. R. 2267: Rep. Joseph Crowley (D-NY) – 73 bipartisan cosponsors • Increase by 15, 000 slots/5 years – ½ for shortage specialties (HRSA? ) – Prioritize teaching hospitals • In states with new med schools/branches • Over GME cap • Emphasizing ambulatory training
• $3. 5 B in empirically unjustified IME • Physician shortage – desire to raise GME cap by hospital community • Desire to increase accountability and transparency of GME by Med. PAC, CMS, and policy-makers • trade increased $/GME for P 4 P
Pay for Performance in GME • Hold back a portion of payment and distribute in pay for performance policy • Phase in… – Pay for reporting structure/process outcomes • Teaching environment – ambulatory/community sites, multi-professional teams, PCMH practice model, meaningful use of EHR • Curriculum content – ACGME competencies, team (microsystem) skills, evidence-based medicine, care coordination skills, practice-based learning • Specialty mix – favoring fields in shortage (PC)
Who to hold accountable? • Who should be on the hook? – Hospitals – Programs – Trainees