Gonorrhea Neisseria Gonorrhoeae https www youtube comwatch vEww
Gonorrhea Neisseria Gonorrhoeae
https: //www. youtube. com/watch? v=Eww 8 t. Gkq. GRw
Cause and Transmission Caused by the bacterium Neisseria gonorrhoeae Sometimes called gonococcus Affects the male and female mucosa primarily but can affect other body areas such as skin, gums, tongue and the throat Mucosa is the lining of the genital organs 40% transfer from pregnant woman to her baby
Background Galen A physician in early Rome first wrote about this disease He noticed a discharge from his patients and thought it was semen or Gonos Gonorrhea means the flow of seed Other names for this disease The clap Came from clappoir or the Parisian houses of prostitution in the middle ages
Background For almost 300 years syphilis and gonorrhea were thought to be the same disease The characteristic discharge of gonorrhea was considered to be the first symptoms of syphilis John Hunter, a physician in 1767 obtained pus from a patient with gonorrhea and injected himself Hunter fell victim to the effects of Syphilis and Gonorrhea since the pus was infected with both diseases He died from Syphilitic heart disease in 1793
6 Lesson I: Epidemiology: Disease in the U. S.
Background Many physicians considered Syphilis and Gonorrhea the same disease for the next 50 years
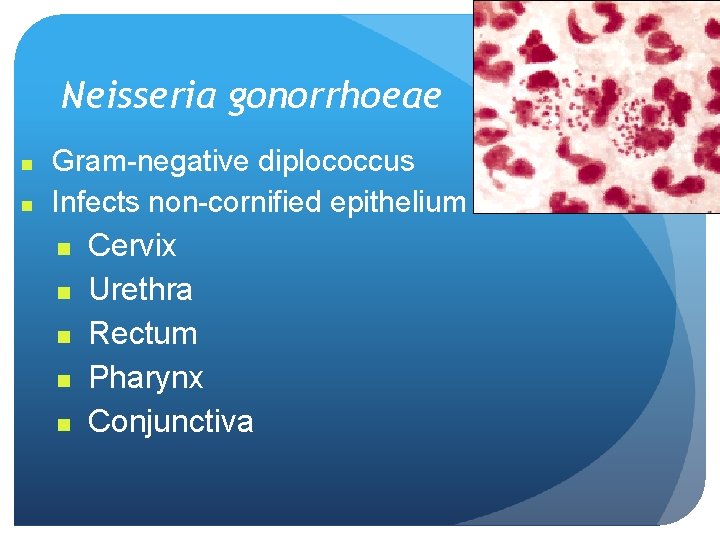
Neisseria gonorrhoeae n n Gram-negative diplococcus Infects non-cornified epithelium n n n Cervix Urethra Rectum Pharynx Conjunctiva
Neisseria gonorrhoeae Second most common bacterial STD Estimated >1 million US cases per year Incidence highest among adolescents and young adults Causes a range of clinical syndromes Many infections are asymptomatic
Neisseria gonorrhoeae described by Albert Neisser in 1879 Observed in smears of purulent exudates of urethritis, cervicitis, opthalmia neonatorum Thayer Martin medium enhanced isolation of gonococcus in 1960
Incidence and Prevalence Significant public health problem in U. S. Urban and low SES populations Adolescents > age 20 -25 years > older Black/Hispanic > White/API Multiple sex partners Increasing proportion of gonococcal infections caused by resistant organisms
GC Sexual Transmission Efficiently transmitted by sexual contact Greater efficiency of transmission from male to female u Male to female: 50 - 90% u Female to male: 20 - 80% Vaginal & anal intercourse more efficient than oral Can be acquired from asymptomatic partner Increases transmission and susceptibility to HIV 2 -5 fold
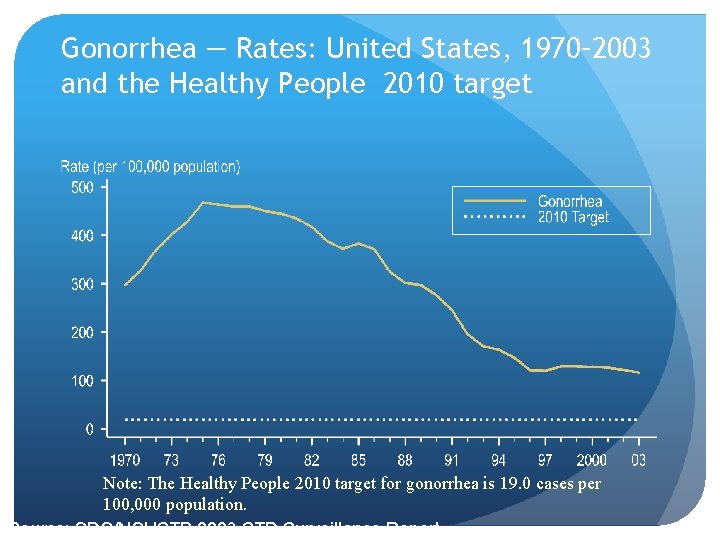
Gonorrhea — Rates: United States, 1970– 2003 and the Healthy People 2010 target Note: The Healthy People 2010 target for gonorrhea is 19. 0 cases per 100, 000 population. Source: CDC/NCHSTP 2003 STD Surveillance Report
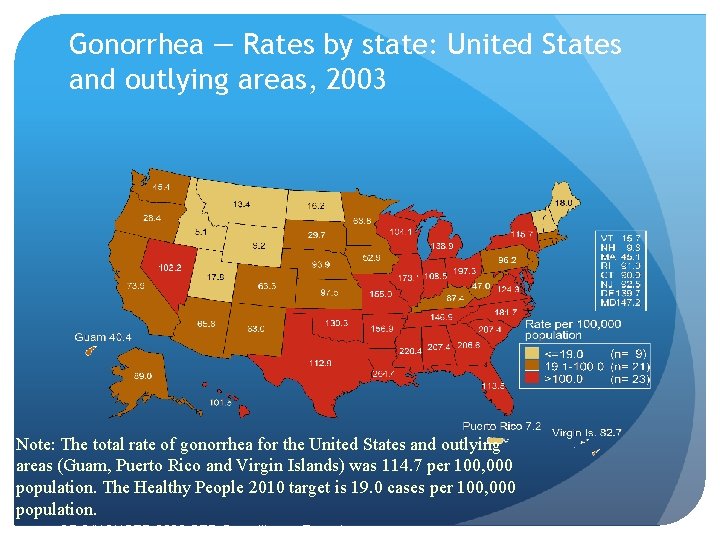
Gonorrhea — Rates by state: United States and outlying areas, 2003 Note: The total rate of gonorrhea for the United States and outlying areas (Guam, Puerto Rico and Virgin Islands) was 114. 7 per 100, 000 population. The Healthy People 2010 target is 19. 0 cases per 100, 000 population. Source: CDC/NCHSTP 2003 STD Surveillance Report
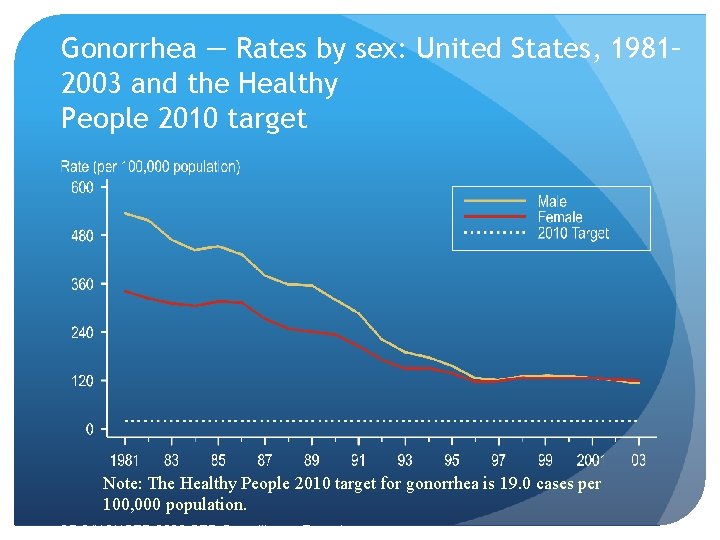
Gonorrhea — Rates by sex: United States, 1981– 2003 and the Healthy People 2010 target Note: The Healthy People 2010 target for gonorrhea is 19. 0 cases per 100, 000 population. Source: CDC/NCHSTP 2003 STD Surveillance Report
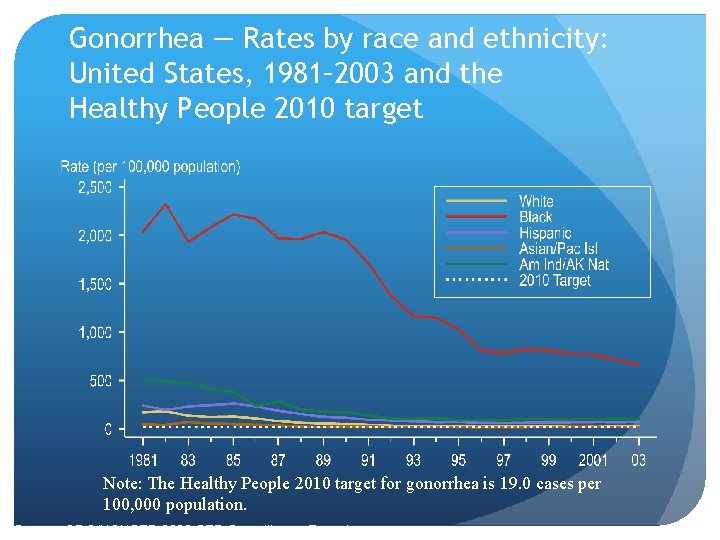
Gonorrhea — Rates by race and ethnicity: United States, 1981– 2003 and the Healthy People 2010 target Note: The Healthy People 2010 target for gonorrhea is 19. 0 cases per 100, 000 population. Source: CDC/NCHSTP 2003 STD Surveillance Report
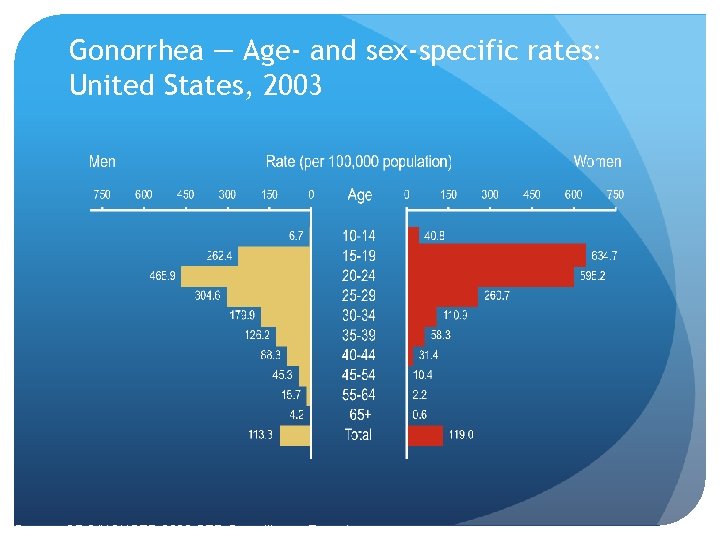
Gonorrhea — Age- and sex-specific rates: United States, 2003 Source: CDC/NCHSTP 2003 STD Surveillance Report

Risk Factors Multiple or new sex partners or inconsistent condom use Urban residence in areas with disease prevalence Adolescents, females particularly Lower socio-economic status Use of drugs Exchange of sex for drugs or money
Transmission Efficiently transmitted by: Male to female via semen Female to male urethra Rectal intercourse Fellatio (pharyngeal infection) Perinatal transmission (mother to infant)
20 Lesson II: Pathogenesis
Microbiology Etiologic agent: Neisseria gonorrhoeae Gram-negative intracellular diplococcus Infects mucus-secreting epithelial cells
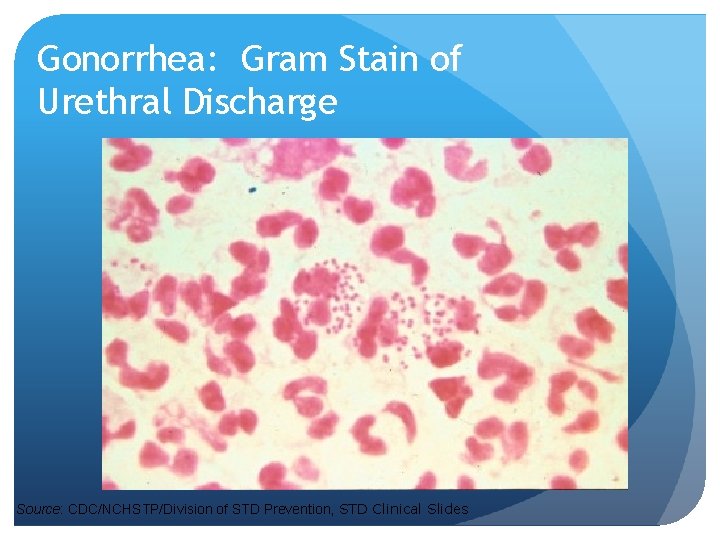
Gonorrhea: Gram Stain of Urethral Discharge Source: CDC/NCHSTP/Division of STD Prevention, STD Clinical Slides
Lesson III: Clinical Manifestations
Asymptomatic Gonorrhea Most infections are asymptomatic More women(75%) as asymptomatic than men (1%) Asymptomatic prevents elimination of this disease
Symptomatic Gonorrhea In women, Signs and Symptoms usually make their appearance after incubation of two weeks or longer Symptoms are frequently mild or nonspecific and can be overlooked Symptoms in women may include: Burning sensation upon urination Presence of unusual vaginal discharge Backache Vaginal bleeding Pain in lower abdomen
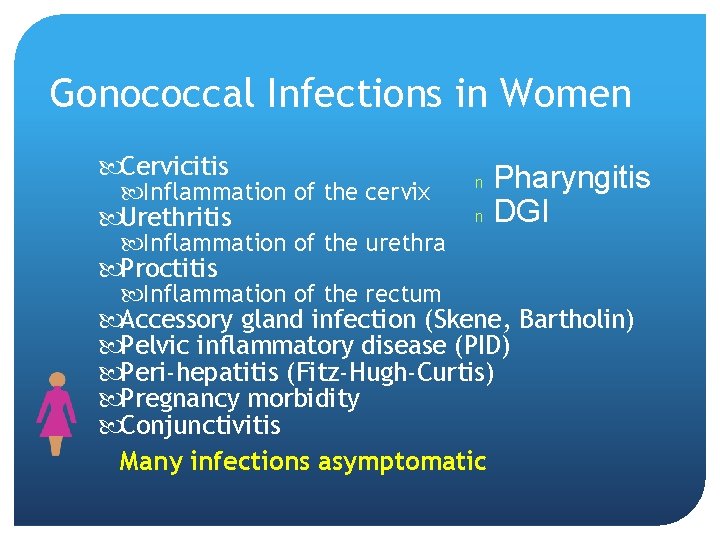
Gonococcal Infections in Women Cervicitis Inflammation of the cervix Urethritis Inflammation of the urethra Pharyngitis n DGI n Proctitis Inflammation of the rectum Accessory gland infection (Skene, Bartholin) Pelvic inflammatory disease (PID) Peri-hepatitis (Fitz-Hugh-Curtis) Pregnancy morbidity Conjunctivitis Many infections asymptomatic
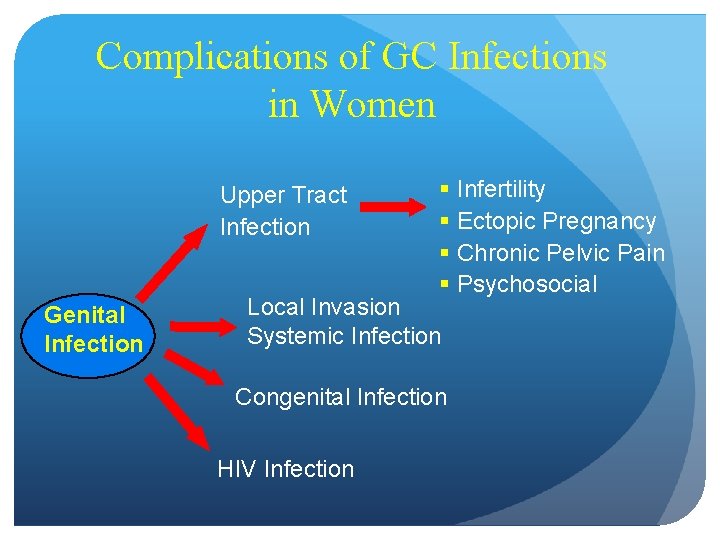
Complications of GC Infections in Women Upper Tract Infection Genital Infection § Infertility § Ectopic Pregnancy § Chronic Pelvic Pain § Psychosocial Local Invasion Systemic Infection Congenital Infection HIV Infection

Gonococcal Cervicitis Incubation 3 -10 days n. Symptoms: u. Vaginal discharge u. Dysuria u. Vaginal bleeding n. Cervical signs : u. Erythema u. Friability u. Purulent exudate n STD Atlas, 1997
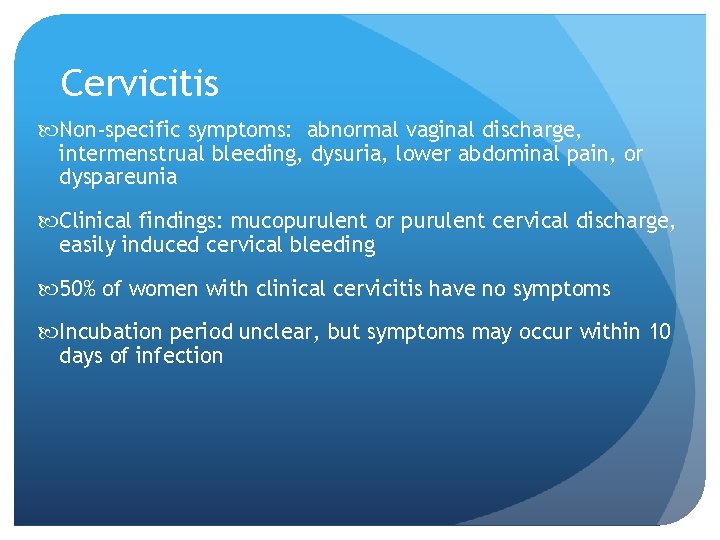
Cervicitis Non-specific symptoms: abnormal vaginal discharge, intermenstrual bleeding, dysuria, lower abdominal pain, or dyspareunia Clinical findings: mucopurulent or purulent cervical discharge, easily induced cervical bleeding 50% of women with clinical cervicitis have no symptoms Incubation period unclear, but symptoms may occur within 10 days of infection
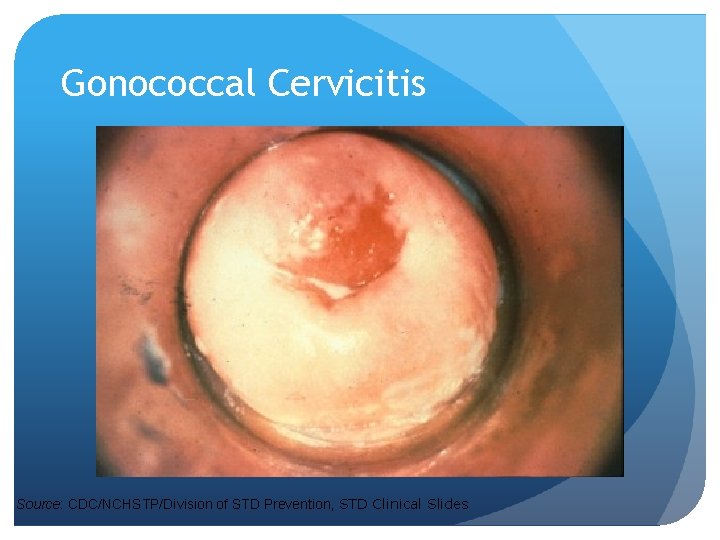
Gonococcal Cervicitis Source: CDC/NCHSTP/Division of STD Prevention, STD Clinical Slides

Urethritis Symptoms: dysuria, however, most women are asymptomatic 40%-60% of women with cervical gonococcal infection may have urethral infection
Complications in Women Accessory gland infection Bartholin’s glands Skene’s glands Pelvic Inflammatory Disease (PID) Fitz-Hugh-Curtis Syndrome Perihepatitis
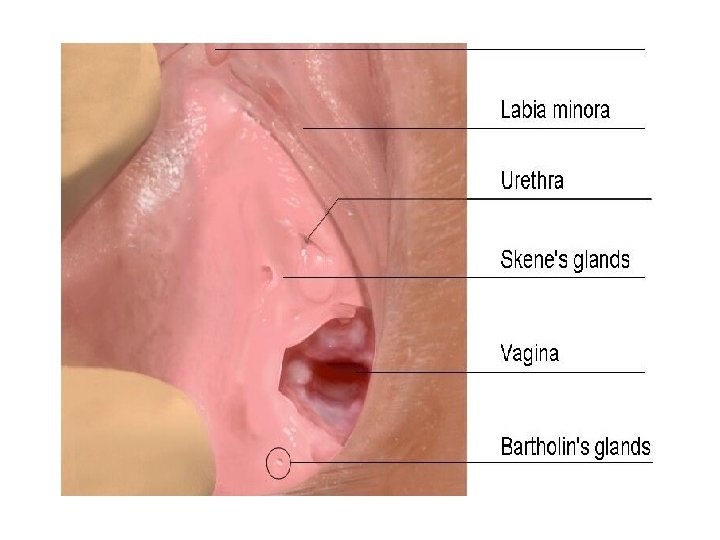
Bartholin’s and Skene’s Glands The Bartholin's glands (also called Bartholin glands or greater vestibular glands) are two pea sized glands located slightly posterior to the opening of the vagina. The glands secrete mucous to lubricate the vagina During sexual arousal, the Skene's gland becomes swollen with blood, stimulating nerve fibers associated with it. Ongoing stimulation of the area can produce an orgasm
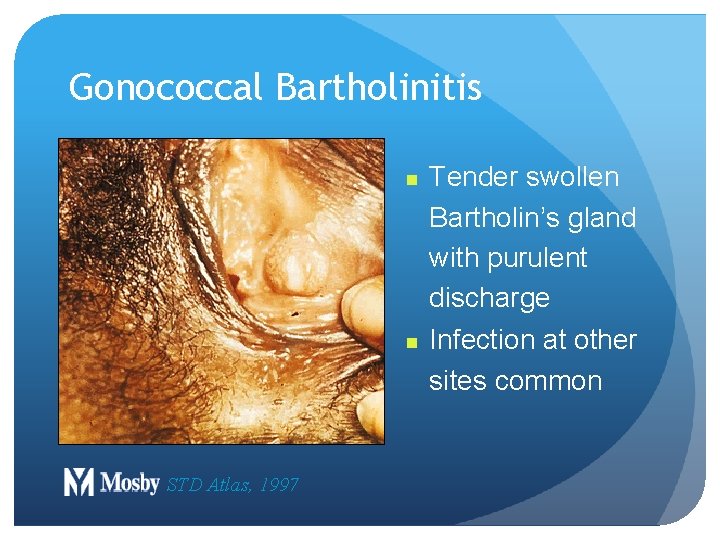
Gonococcal Bartholinitis n n STD Atlas, 1997 Tender swollen Bartholin’s gland with purulent discharge Infection at other sites common
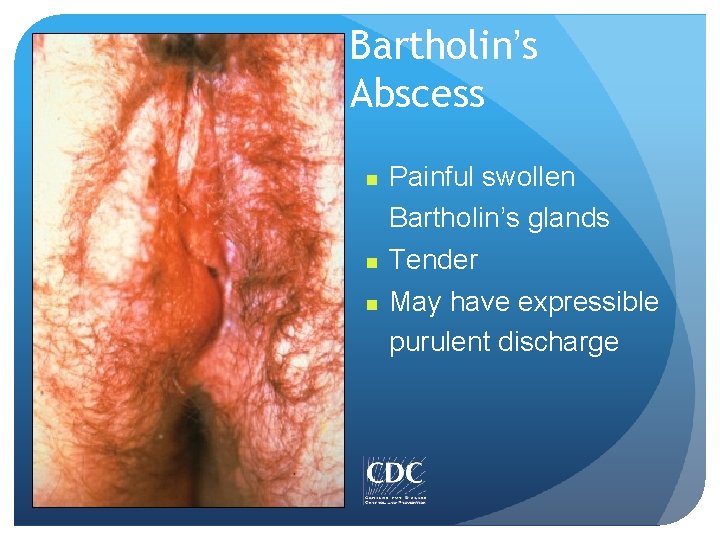
Bartholin’s Abscess n n n Painful swollen Bartholin’s glands Tender May have expressible purulent discharge


Pelvic Inflammatory Disease (PID) 10 – 15% of gonorrhea cases have PID At times women may experience pain during sexual intercourse, sterility and ectopic pregnancy
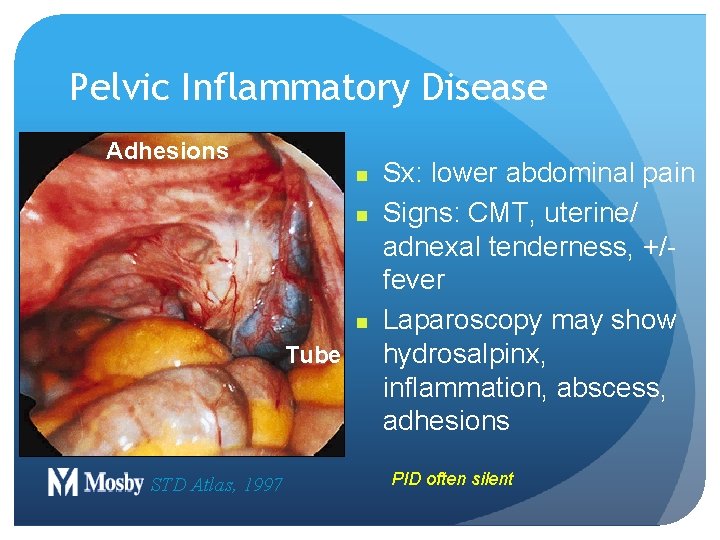
Pelvic Inflammatory Disease Adhesions n n n Tube STD Atlas, 1997 Sx: lower abdominal pain Signs: CMT, uterine/ adnexal tenderness, +/fever Laparoscopy may show hydrosalpinx, inflammation, abscess, adhesions PID often silent
Fitz-Hugh-Curtis Syndrom Failure to diagnose PID can result in acute morbidity, including tuboovarian abscess, endometritis, Fitz. Hugh-Curtis syndrome (perihepatitis), and other chronic sequelae. Perihepatitis secondary to gonorrhea presents as right upper quadrant pain and nausea.
Syndromes in Men and Women Anorectal infection Pharyngeal infection Conjunctivitis Disseminated gonococcal infection (DGI)
Symptomatic Gonorrhea Signs and Symptoms in men appear 3 to 5 days after sexual intercourse with an infected partner Symptoms include: Burning sensation on urination Pus-like creamy white or yellow discharge from the penis
Gonococcal Infections in Men Urethritis Epididymitis Proctitis Conjunctivitis Pharyngitis n DGI n Urethral stricture Abscess of Cowper’s/Tyson’s glands n Penile edema Seminal vesiculitis Prostatitis Many infections asymptomatic n
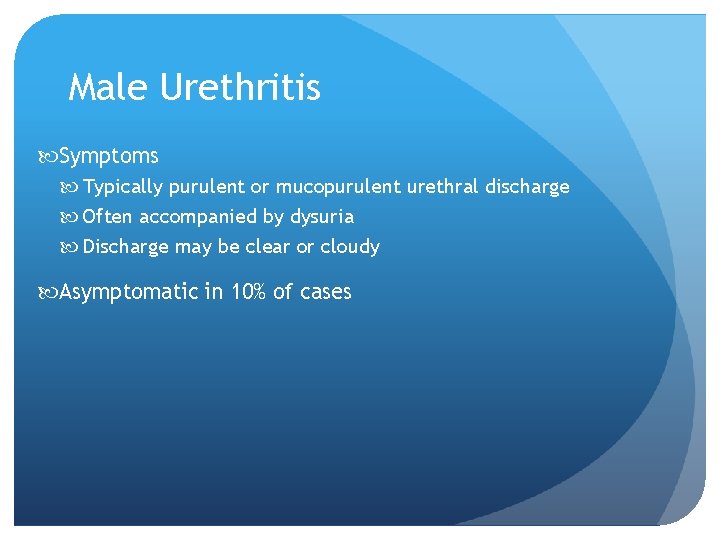
Male Urethritis Symptoms Typically purulent or mucopurulent urethral discharge Often accompanied by dysuria Discharge may be clear or cloudy Asymptomatic in 10% of cases
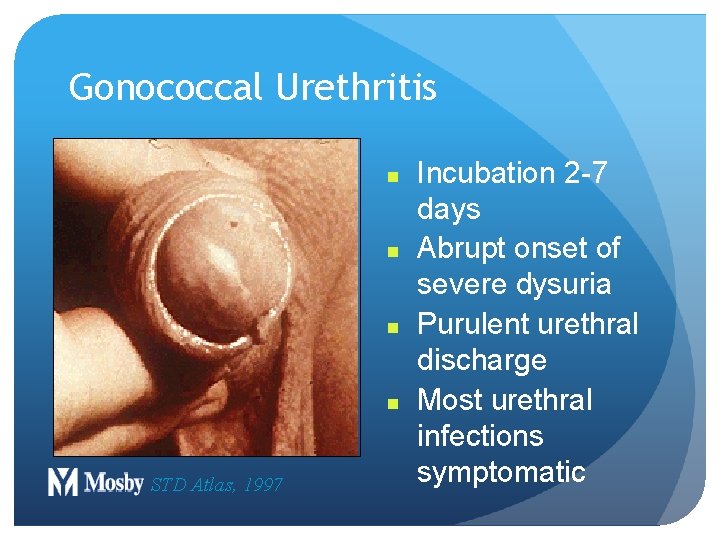
Gonococcal Urethritis n n STD Atlas, 1997 Incubation 2 -7 days Abrupt onset of severe dysuria Purulent urethral discharge Most urethral infections symptomatic
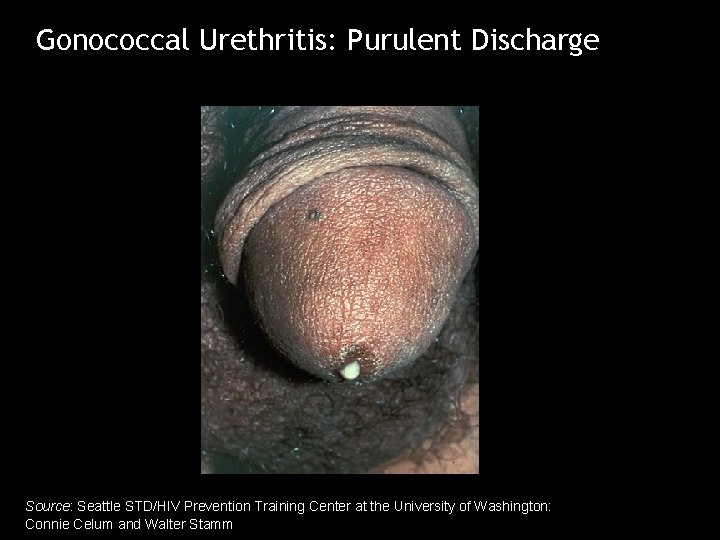
Gonococcal Urethritis: Purulent Discharge Source: Seattle STD/HIV Prevention Training Center at the University of Washington: Connie Celum and Walter Stamm

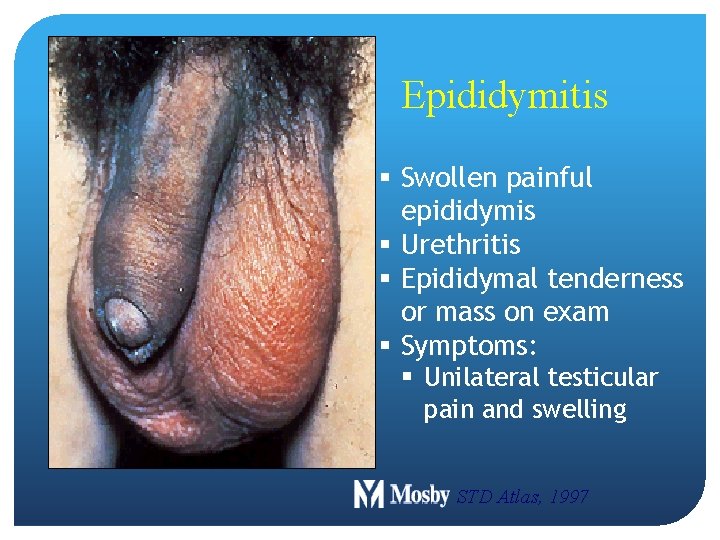
Epididymitis § Swollen painful epididymis § Urethritis § Epididymal tenderness or mass on exam § Symptoms: § Unilateral testicular pain and swelling STD Atlas, 1997
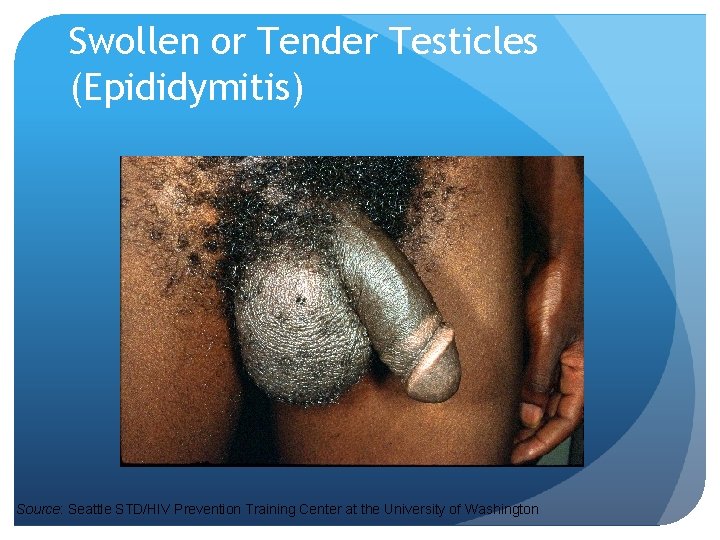
Swollen or Tender Testicles (Epididymitis) Source: Seattle STD/HIV Prevention Training Center at the University of Washington
Gonococcal Infections in Women & Men n Urethritis n Proctitis n Pharyngeal infections n Conjunctivitis n Disseminated Gonococcal Infection
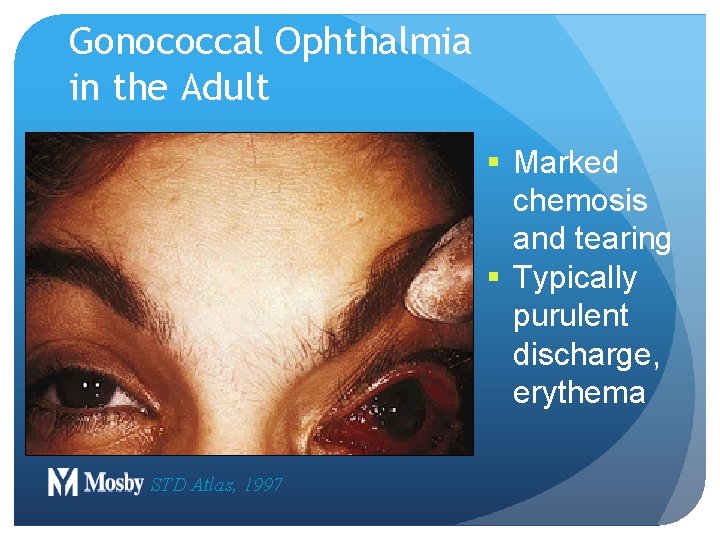
Gonococcal Ophthalmia in the Adult § Marked chemosis and tearing § Typically purulent discharge, erythema STD Atlas, 1997
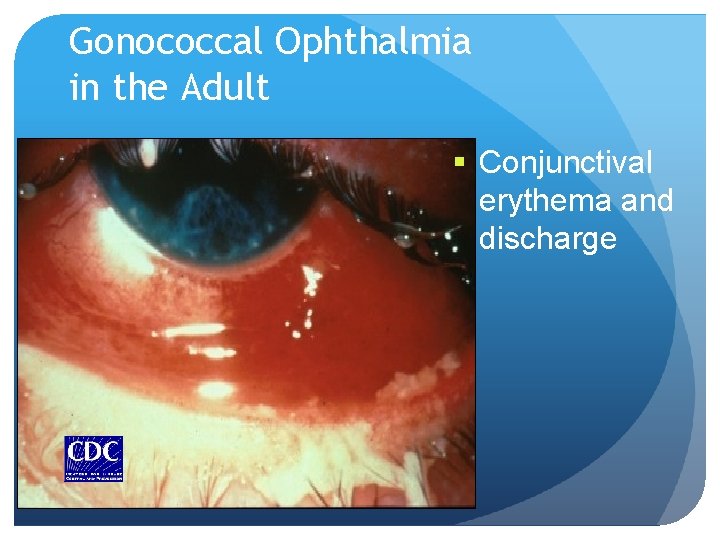
Gonococcal Ophthalmia in the Adult § Conjunctival erythema and discharge
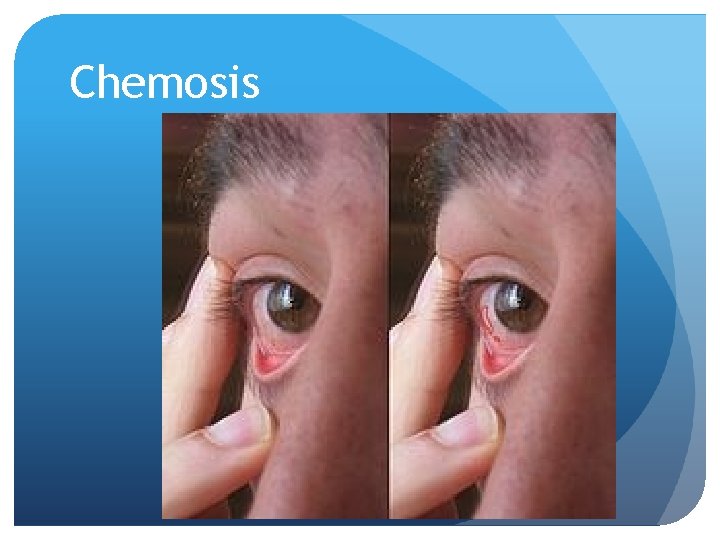
Chemosis
Disseminated Gonococcal Infection Gonococcal bacteremia Sources of infection include symptomatic and asymptomatic infections of pharynx, urethra, cervix Occurs in < 5% of GC-infected patients More common in females
DGI Clinical Manifestations “Dermatitis-arthritis syndrome” Arthritis: 90% Characterized by fever, chills, skin lesions, arthralgias, tenosynovitis Less commonly, hepatitis, myocarditis, endocarditis, meningitis Rash characterized as macular or papular, pustular, hemorrhagic or necrotic, mostly on distal extremities
DGI Arthritis Gonorrhea is the most common cause of arthritis in the adolescent. However, arthritis (septic or reactive) is a rare complication of this disease. Additional complications Corneal scarring after ocular gonococcal infections Destruction of cardiac valves in gonococcal endocarditis eath from congestive heart failure related to endocarditis Central nervous system (CNS) complications of gonococcal meningitis

DGI Skin Lesion § Necrotic, grayish central lesion on erythematous base STD Atlas, 1997
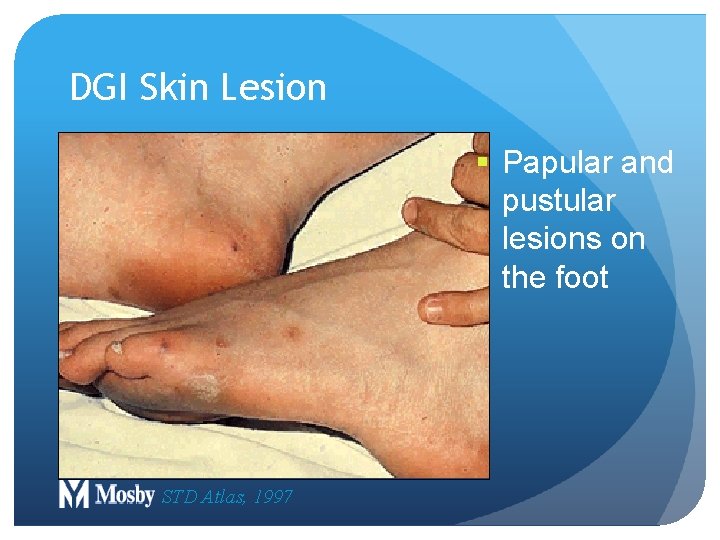
DGI Skin Lesion § Papular and pustular lesions on the foot STD Atlas, 1997
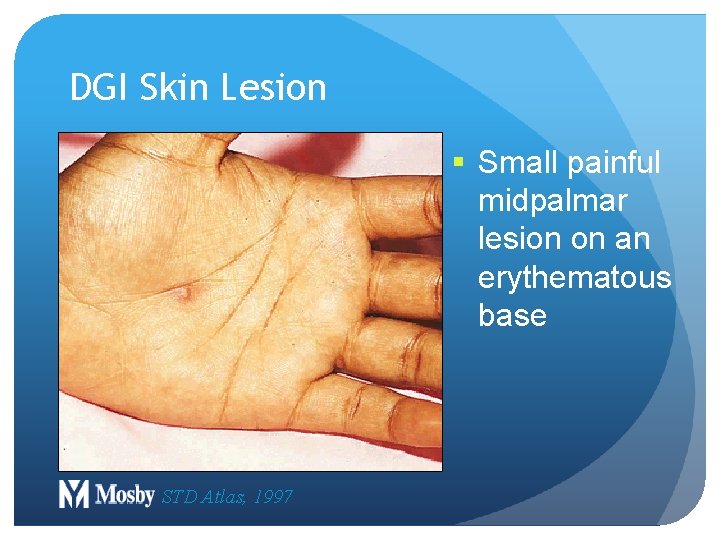
DGI Skin Lesion § Small painful midpalmar lesion on an erythematous base STD Atlas, 1997
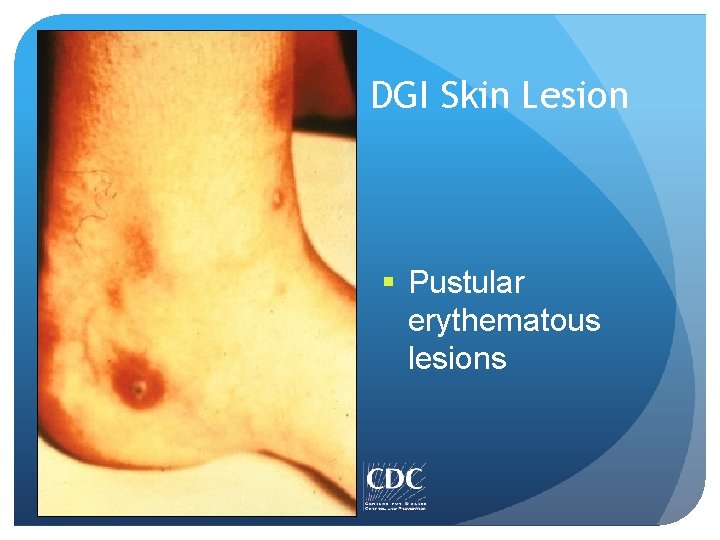
DGI Skin Lesion § Pustular erythematous lesions
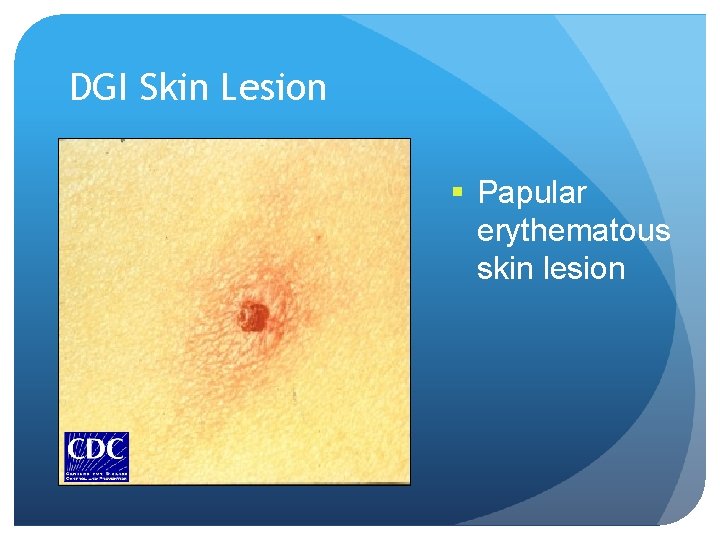
DGI Skin Lesion § Papular erythematous skin lesion
DGI Differential Diagnosis Meningococcemia Staphylococcal sepsis or endocarditis Other bacterial septicemias Acute HIV infection Thrombocytopenia & arthritis Hepatitis B prodrome Reiter’s Syndrome Juvenile Rheumatoid Arthritis Lyme disease
Gonococcal Complications in Pregnancy Postpartum endometritis Septic abortions Post-abortal PID Possible role in: § Gestational bleeding § Preterm labor and delivery § Premature rupture of membranes
Gonorrhea Infection in Children Perinatal: infections of the conjunctiva, pharynx, respiratory tract Older children (>1 year): considered possible evidence of sexual abuse
Vertical Transmission and Neonatal Complications on Gonorrhea Overall vertical transmission rate ~30% Neonatal complications include: v Ophthalmia neonatorum v Disseminated gonococcal infection (sepsis, arthritis, meningitis) v Scalp abscess (if fetal scalp monitor used) v Vaginal and rectal infections v Pharyngeal infections
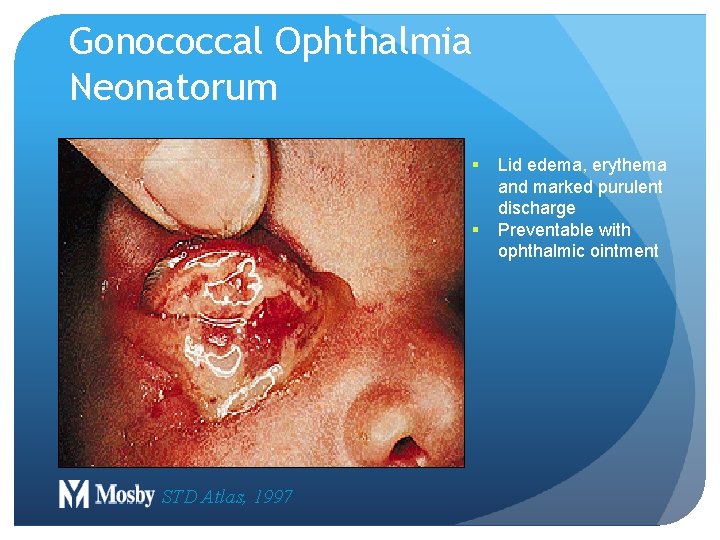
Gonococcal Ophthalmia Neonatorum § § STD Atlas, 1997 Lid edema, erythema and marked purulent discharge Preventable with ophthalmic ointment
GC Infections in Children Vulvovaginits Urethritis Proctitis All cases should be considered possible evidence of sexual abuse Culture should be obtained
Lesson IV: Diagnosis
GC Diagnostic Methods Gram stain smear Culture Antigen Detection Tests: EIA & DFA Nucleic Acid Detection Tests Probe Hybridization Nucleic Acid Amplification Tests (NAATs) Hybrid Capture
Clinical Considerations In cases of suspected sexual abuse Legal standard is culture with multiple tests to confirm the identity of Neisseria gonorrhoeae
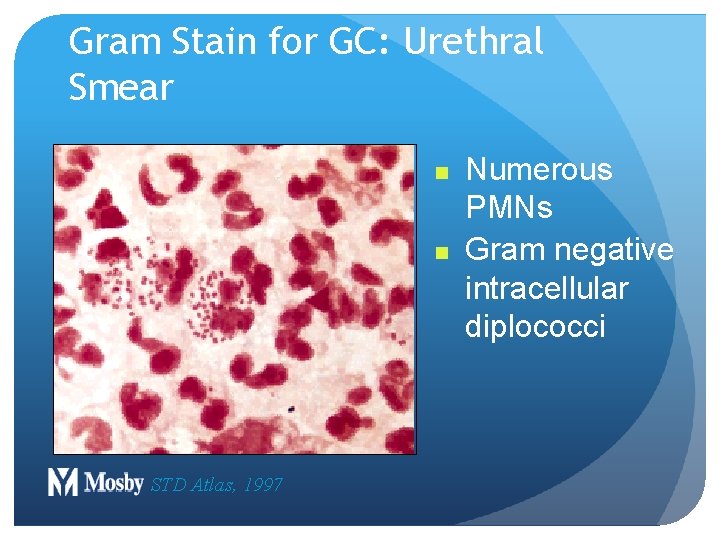
Gram Stain for GC: Urethral Smear n n STD Atlas, 1997 Numerous PMNs Gram negative intracellular diplococci
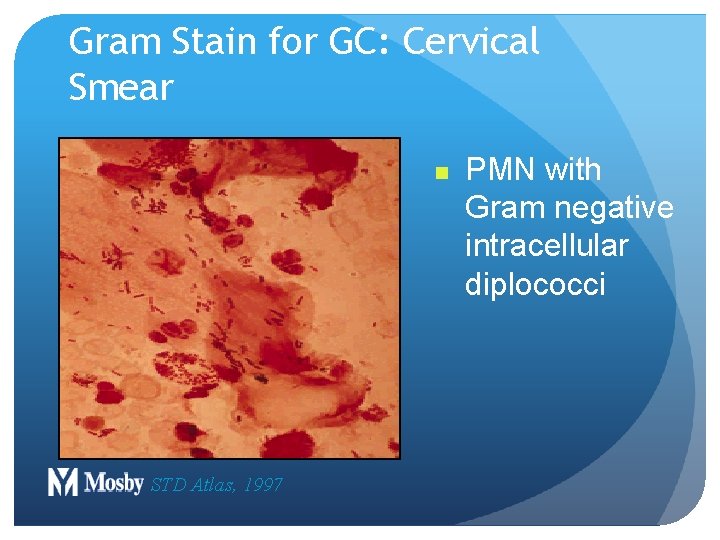
Gram Stain for GC: Cervical Smear n STD Atlas, 1997 PMN with Gram negative intracellular diplococci
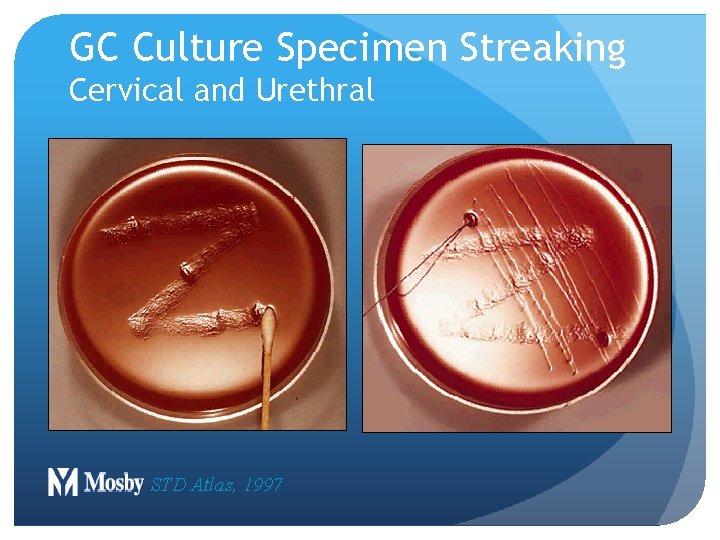
GC Culture Specimen Streaking Cervical and Urethral STD Atlas, 1997
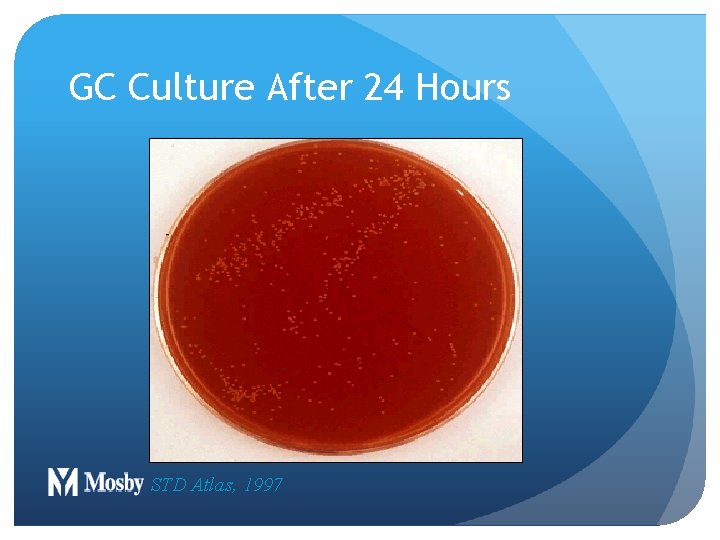
GC Culture After 24 Hours STD Atlas, 1997
77 Lesson V: Patient Management
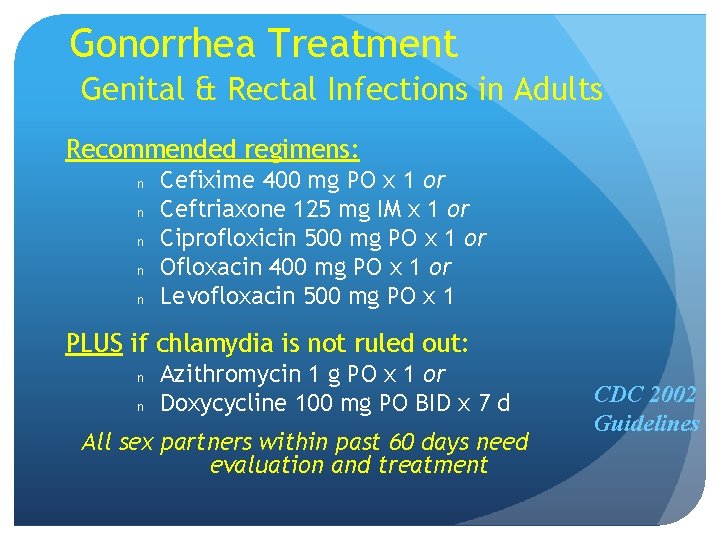
Gonorrhea Treatment Genital & Rectal Infections in Adults Recommended regimens: n n n Cefixime 400 mg PO x 1 or Ceftriaxone 125 mg IM x 1 or Ciprofloxicin 500 mg PO x 1 or Ofloxacin 400 mg PO x 1 or Levofloxacin 500 mg PO x 1 PLUS if chlamydia is not ruled out: n n Azithromycin 1 g PO x 1 or Doxycycline 100 mg PO BID x 7 d All sex partners within past 60 days need evaluation and treatment CDC 2002 Guidelines
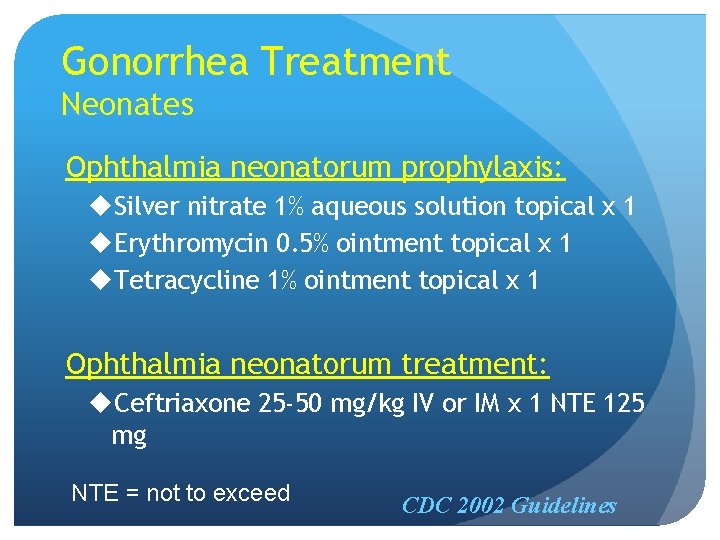
Gonorrhea Treatment Neonates Ophthalmia neonatorum prophylaxis: u. Silver nitrate 1% aqueous solution topical x 1 u. Erythromycin 0. 5% ointment topical x 1 u. Tetracycline 1% ointment topical x 1 Ophthalmia neonatorum treatment: u. Ceftriaxone 25 -50 mg/kg IV or IM x 1 NTE 125 mg NTE = not to exceed CDC 2002 Guidelines
GC Antimicrobial Resistance in 20%-30% of gonococcal isolates tested in U. S. Plasmid mediated B - Lactamase production High-level tetracycline resistance Chromosomal mediated Confers resistance to PCN, tetracycline, spectinomycin, erythromycin, fluoroquinolones, and/or cephalosphorins
81 Lesson VI: Prevention
Screening Pregnancy A test for N. gonorrhoeae should be performed at the first prenatal visit for women at risk or those living in an area in which the prevalence of N. gonorrhoeae is high. Repeat test during the 3 rd trimester for those at continued risk. Other populations can be screened based on local disease prevalence and patient’s risk behaviors.
Partner Management Evaluate and treat all sex partners for N. gonorrhoeae and C. trachomatis infections if contact was within 60 days of symptoms or diagnosis. If a patient’s last sexual intercourse was >60 days before onset of symptoms or diagnosis, the patient’s most recent sex partner should be treated. Avoid sexual intercourse until therapy is completed and both partners no longer have symptoms.
Reporting Laws and regulations in all states require that persons diagnosed with gonorrhea are reported to public health authorities by clinicians, labs, or both.
Patient Counseling/Education Nature of disease Usually symptomatic in males and asymptomatic in females Untreated infections can result in PID, infertility, and ectopic pregnancy in women and epididymitis in men Transmission issues Efficiently transmitted Risk reduction Utilize prevention strategies
GC Patient Counseling Nature of transmission Potential long term and neonatal complications Abstain from sex for at least 3 -4 days during treatment (7 days if co-treated for CT) Warning signs and need for follow up Notification and need for treatment of partners
GC Prevention Strategies Health promotion, education & counseling Increased access to condoms Early detection through screening in selected high risk populations Effective diagnosis & treatment Partner management Risk reduction counseling
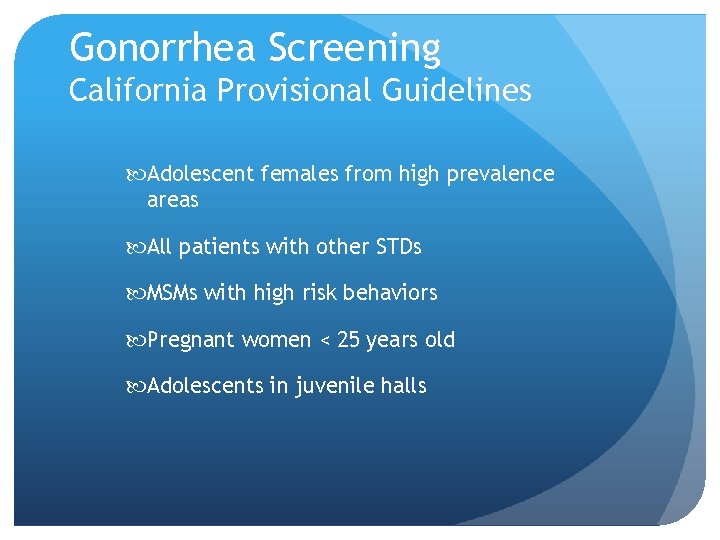
Gonorrhea Screening California Provisional Guidelines Adolescent females from high prevalence areas All patients with other STDs MSMs with high risk behaviors Pregnant women < 25 years old Adolescents in juvenile halls
- Slides: 88