Gonorrhea California STDHIV Prevention Training Center STD Clinical




- Slides: 58
Gonorrhea California STD/HIV Prevention Training Center STD Clinical Series
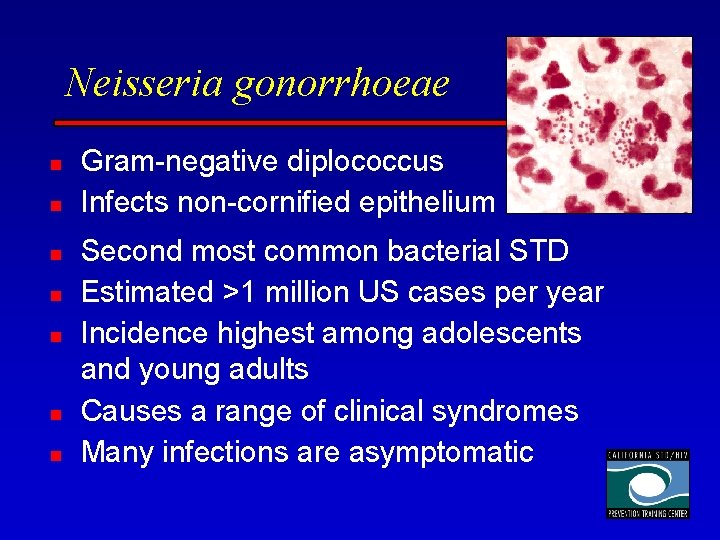
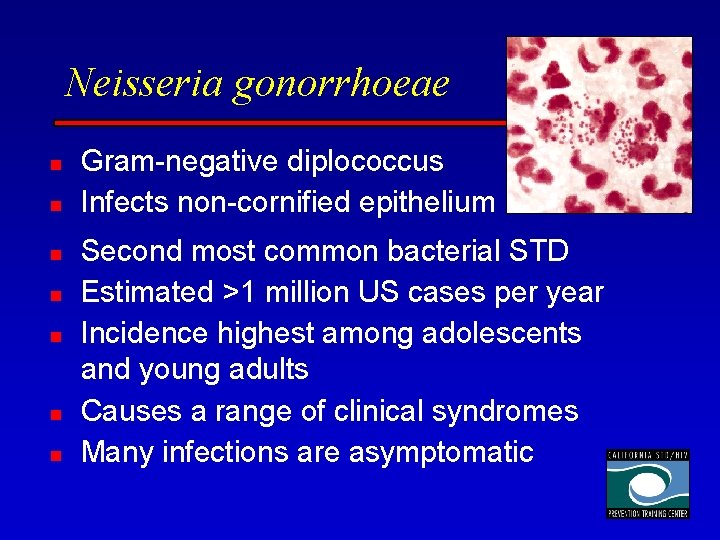
Neisseria gonorrhoeae n n n n Gram-negative diplococcus Infects non-cornified epithelium Second most common bacterial STD Estimated >1 million US cases per year Incidence highest among adolescents and young adults Causes a range of clinical syndromes Many infections are asymptomatic
History of GC n n Neisseria gonorrhoeae described by Albert Neisser in 1879 Observed in smears of purulent exudates of urethritis, cervicitis, opthalmia neonatorum Thayer Martin medium enhanced isolation of gonococcus in 1960 AKA “The Clap”
Risk Factors for GC Infection n n Urban and low SES populations Adolescents > age 20 -25 years > older n Black/Hispanic > White/API n Multiple sex partners n Inconsistent use of barrier methods n High prevalence in sexual network
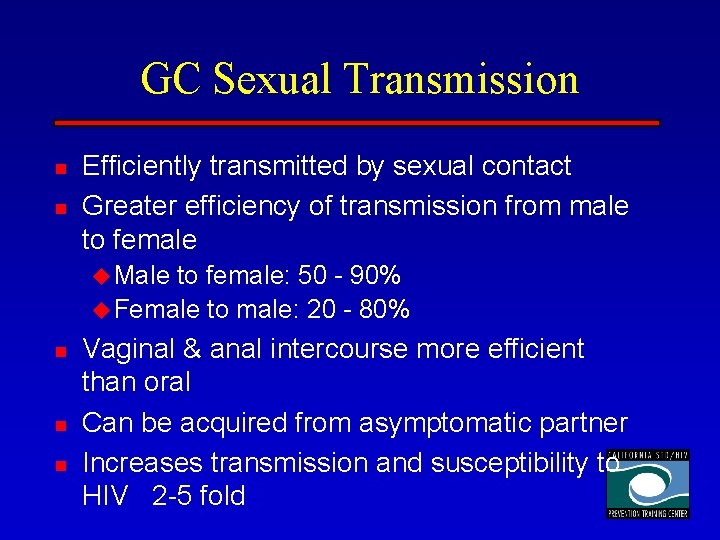
GC Sexual Transmission n n Efficiently transmitted by sexual contact Greater efficiency of transmission from male to female u Male to female: 50 - 90% u Female to male: 20 - 80% n n n Vaginal & anal intercourse more efficient than oral Can be acquired from asymptomatic partner Increases transmission and susceptibility to HIV 2 -5 fold
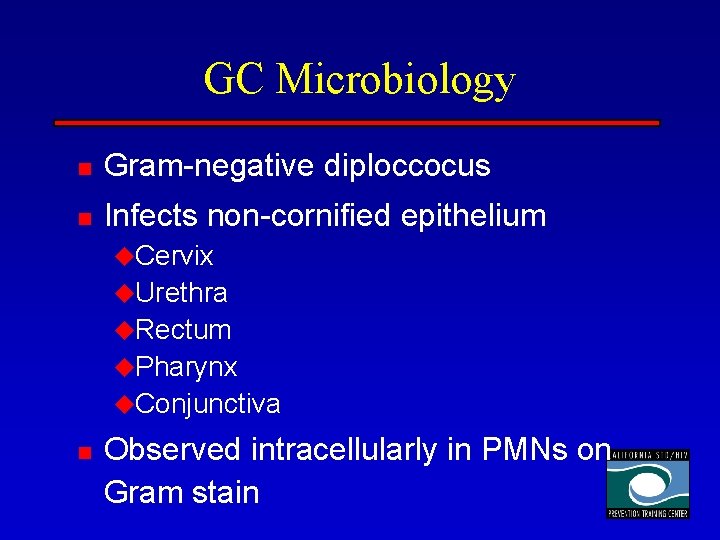
GC Microbiology n Gram-negative diploccocus n Infects non-cornified epithelium u. Cervix u. Urethra u. Rectum u. Pharynx u. Conjunctiva n Observed intracellularly in PMNs on Gram stain
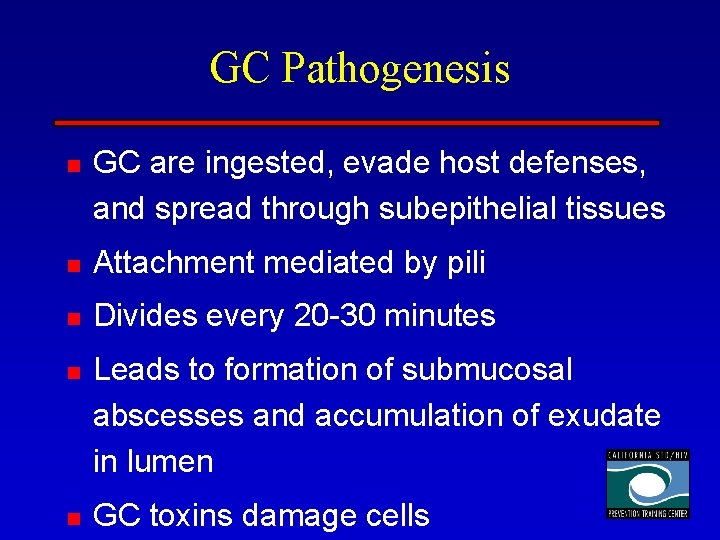
GC Pathogenesis n GC are ingested, evade host defenses, and spread through subepithelial tissues n Attachment mediated by pili n Divides every 20 -30 minutes n n Leads to formation of submucosal abscesses and accumulation of exudate in lumen GC toxins damage cells
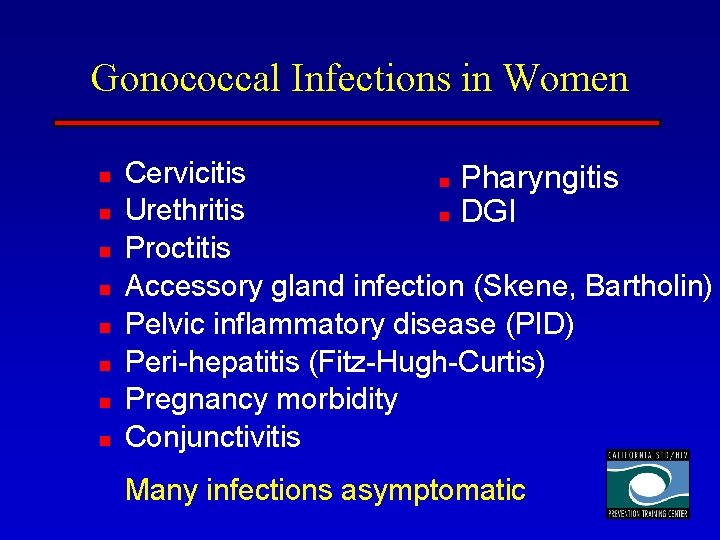
Gonococcal Infections in Women n n n n Cervicitis n Pharyngitis Urethritis n DGI Proctitis Accessory gland infection (Skene, Bartholin) Pelvic inflammatory disease (PID) Peri-hepatitis (Fitz-Hugh-Curtis) Pregnancy morbidity Conjunctivitis Many infections asymptomatic
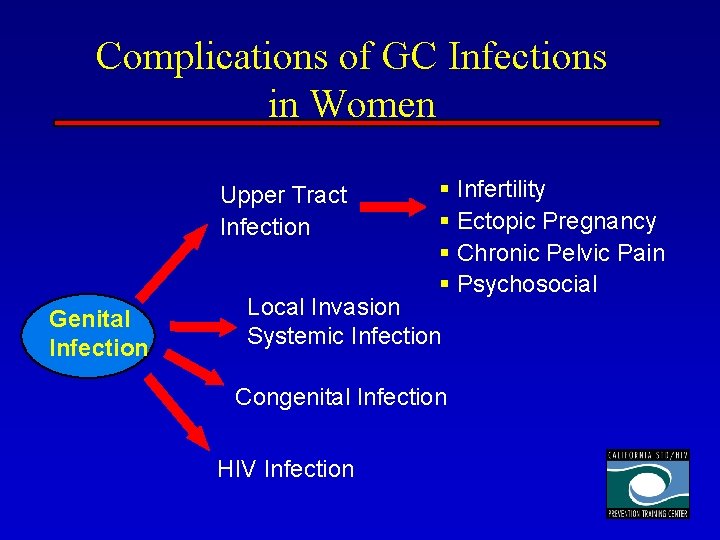
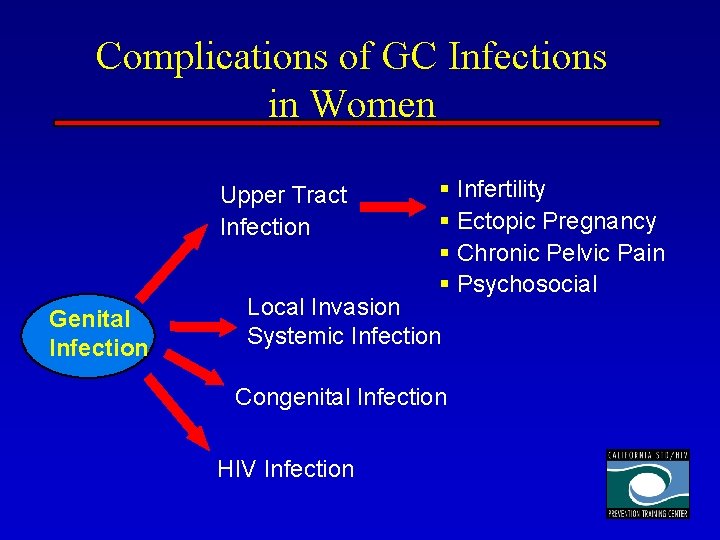
Complications of GC Infections in Women Upper Tract Infection Genital Infection § Infertility § Ectopic Pregnancy § Chronic Pelvic Pain § Psychosocial Local Invasion Systemic Infection Congenital Infection HIV Infection
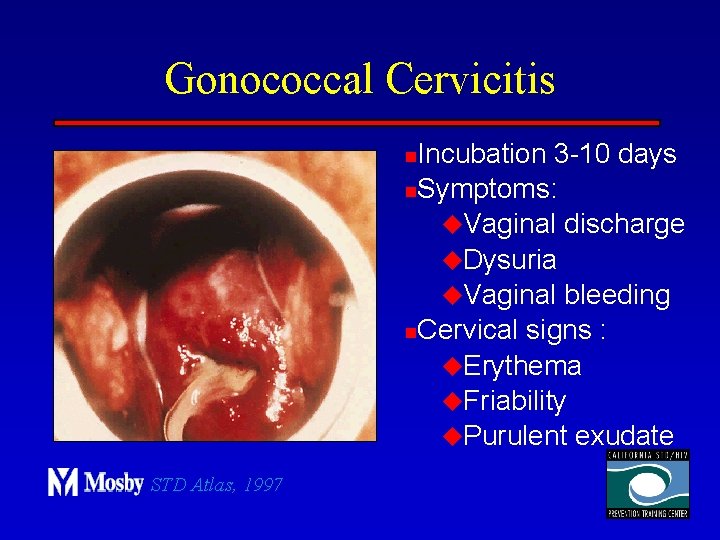
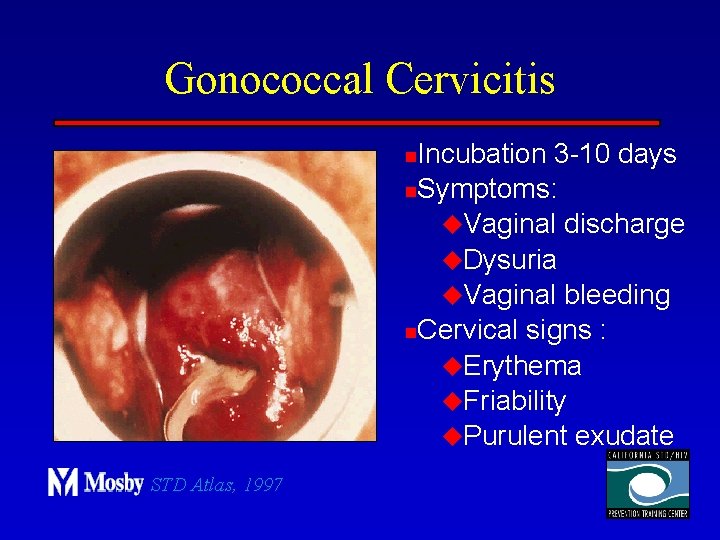
Gonococcal Cervicitis Incubation 3 -10 days n. Symptoms: u. Vaginal discharge u. Dysuria u. Vaginal bleeding n. Cervical signs : u. Erythema u. Friability u. Purulent exudate n STD Atlas, 1997
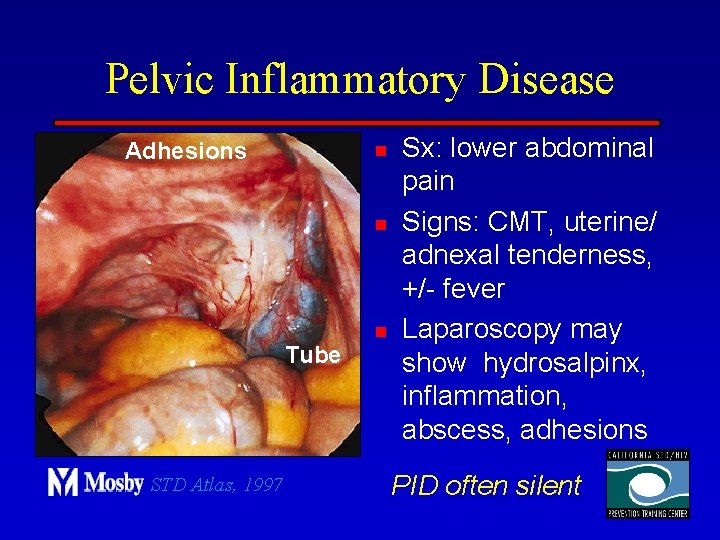
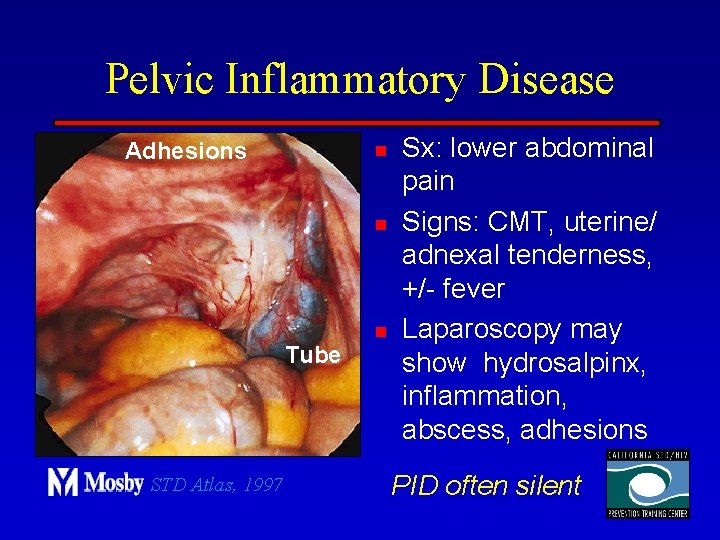
Pelvic Inflammatory Disease Adhesions n n Tube STD Atlas, 1997 n Sx: lower abdominal pain Signs: CMT, uterine/ adnexal tenderness, +/- fever Laparoscopy may show hydrosalpinx, inflammation, abscess, adhesions PID often silent
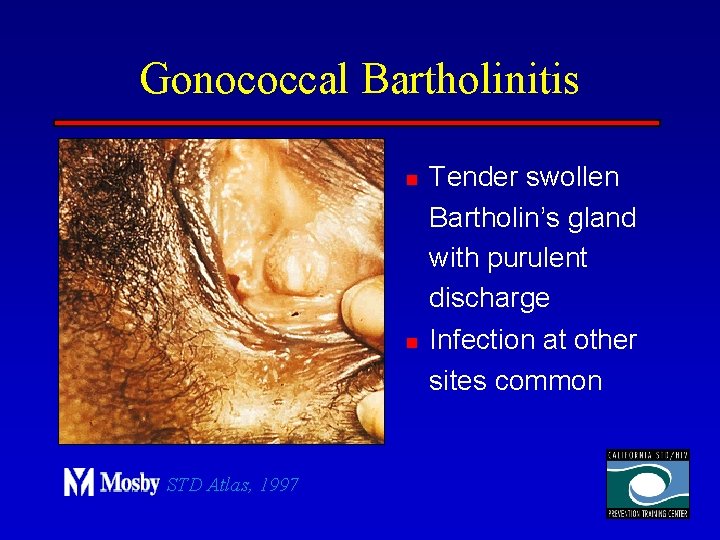
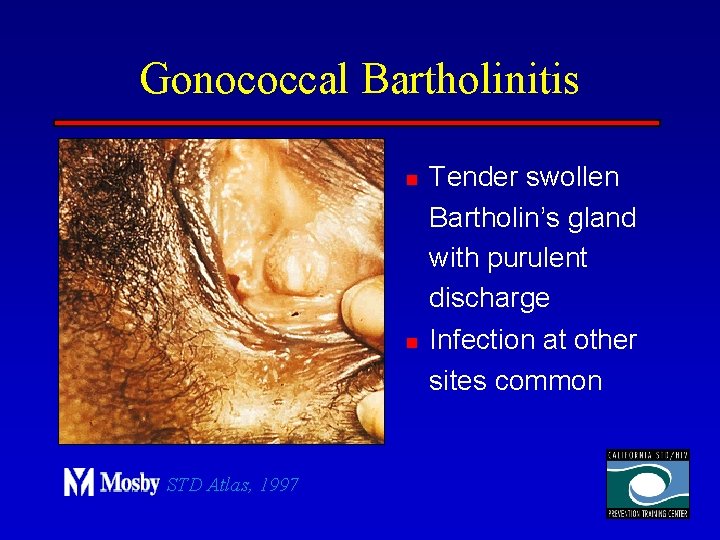
Gonococcal Bartholinitis n n STD Atlas, 1997 Tender swollen Bartholin’s gland with purulent discharge Infection at other sites common
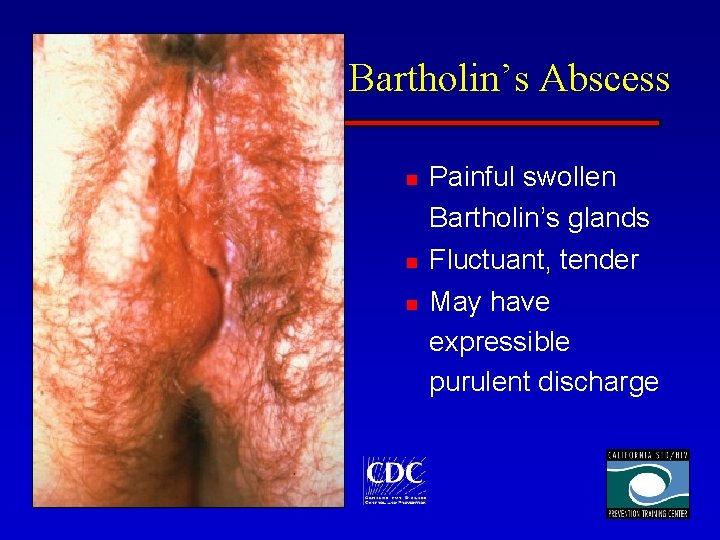
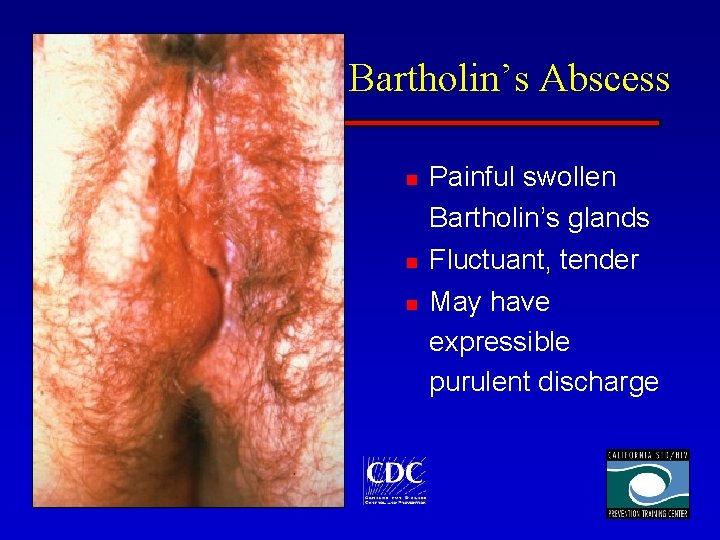
Bartholin’s Abscess n n n Painful swollen Bartholin’s glands Fluctuant, tender May have expressible purulent discharge
Gonococcal Infections in Men n n n Urethritis n Pharyngitis Epididymitis n DGI Proctitis n Urethral stricture Conjunctivitis n Penile edema Abscess of Cowper’s/Tyson’s glands Seminal vesiculitis Prostatitis Many infections asymptomatic
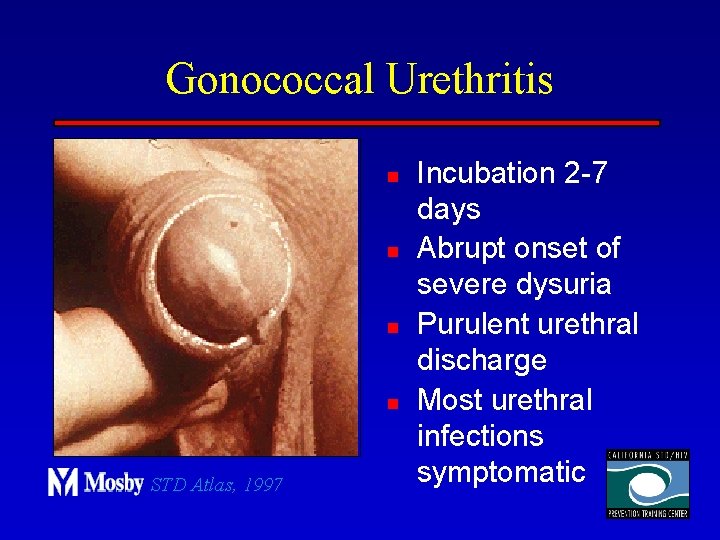
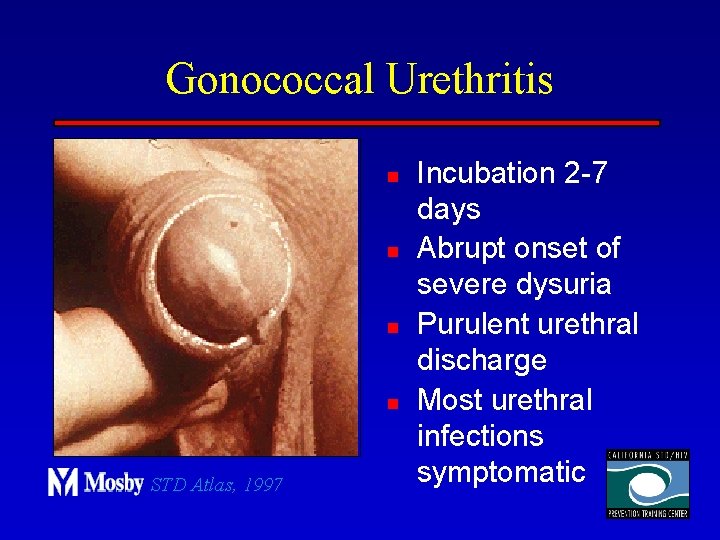
Gonococcal Urethritis n n STD Atlas, 1997 Incubation 2 -7 days Abrupt onset of severe dysuria Purulent urethral discharge Most urethral infections symptomatic
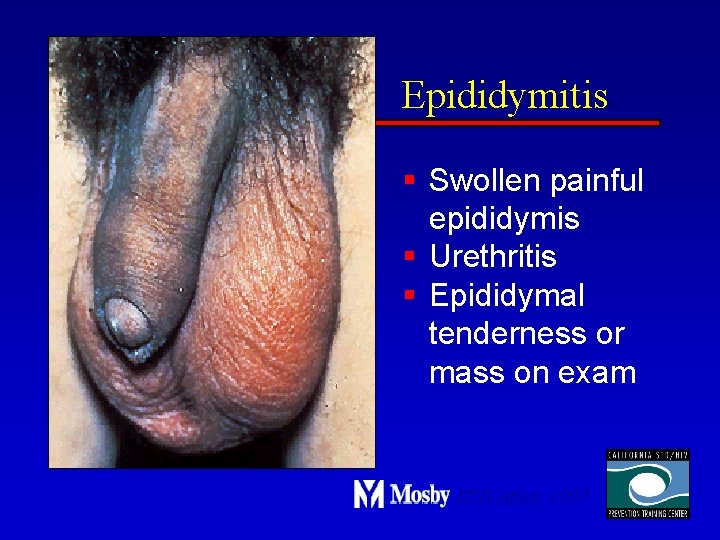
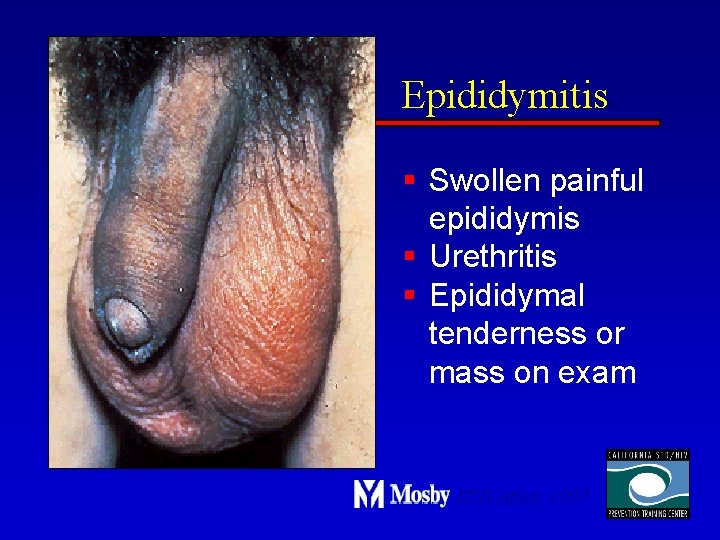
Epididymitis § Swollen painful epididymis § Urethritis § Epididymal tenderness or mass on exam STD Atlas, 1997
Gonococcal Infections in Women & Men n Urethritis n Proctitis n Pharyngeal infections n Conjunctivitis n Disseminated Gonococcal Infection
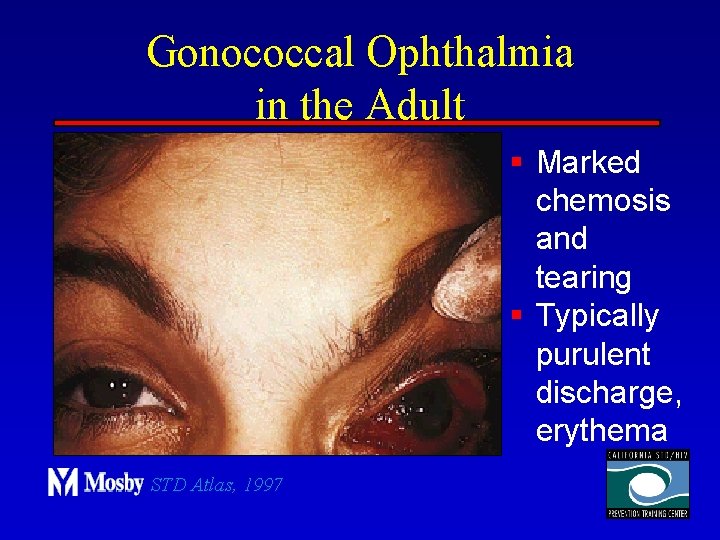
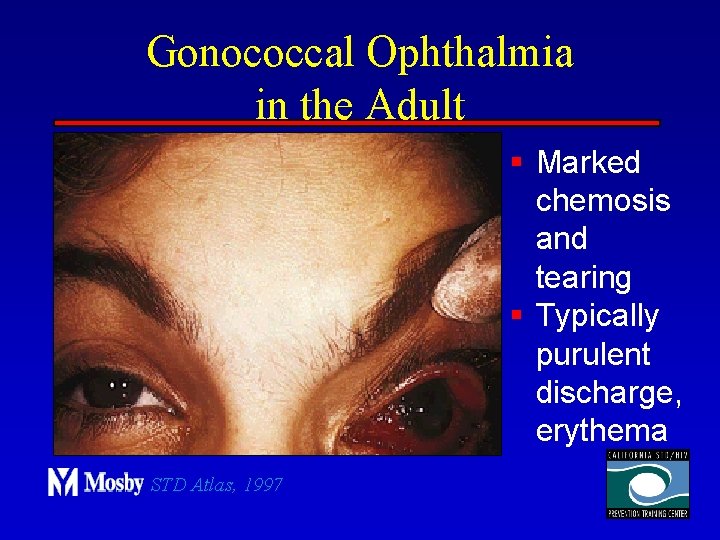
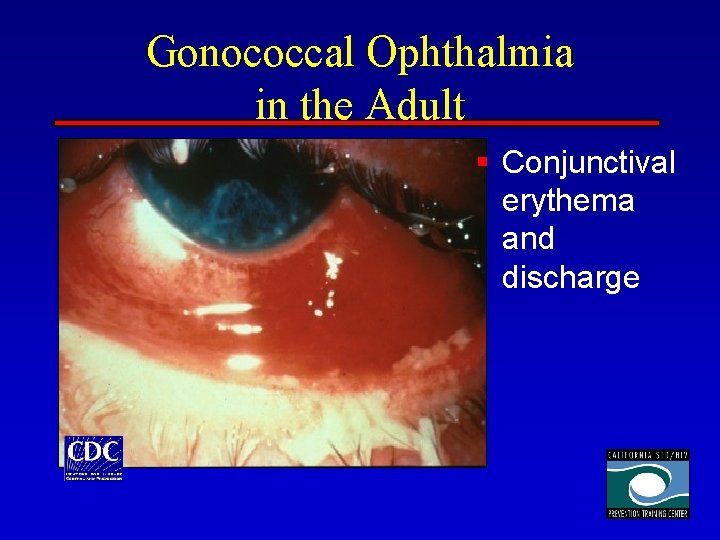
Gonococcal Ophthalmia in the Adult § Marked chemosis and tearing § Typically purulent discharge, erythema STD Atlas, 1997
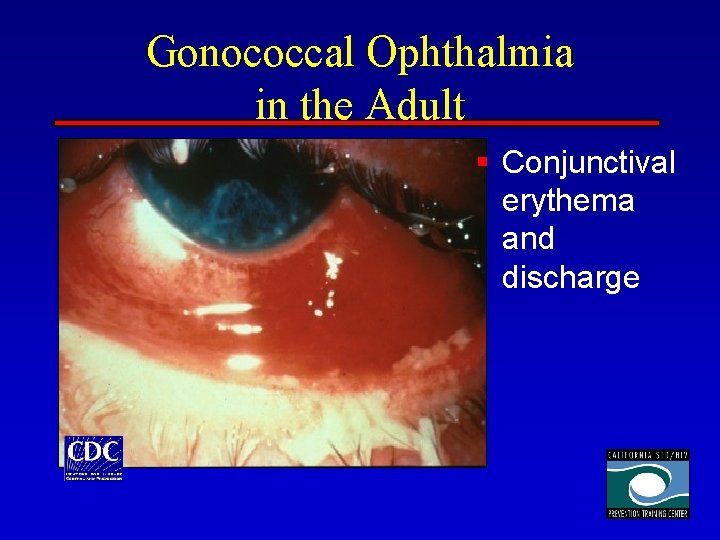
Gonococcal Ophthalmia in the Adult § Conjunctival erythema and discharge
Disseminated Gonococcal Infection n n Gonococcal bacteremia Sources of infection include symptomatic and asymptomatic infections of pharynx, urethra, cervix Occurs in < 5% of GC-infected patients More common in females Patients with congenital deficiency of C 7, C 8, C 9 are at high risk
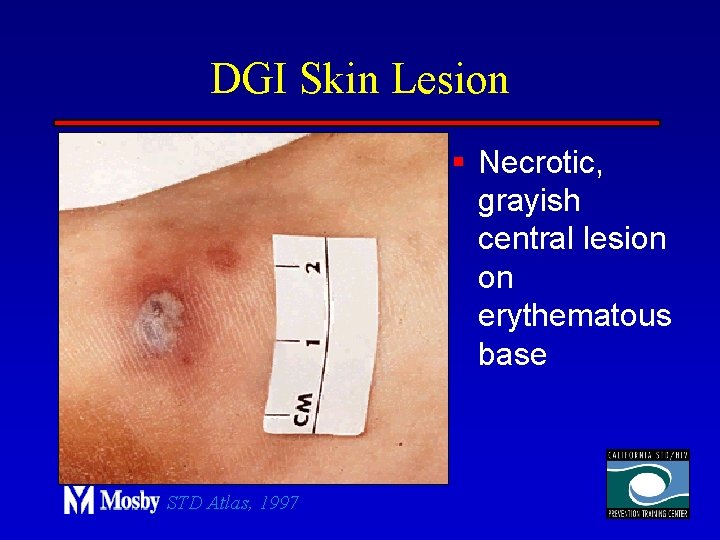
DGI Clinical Manifestations n n “Dermatitis-arthritis syndrome” u. Arthritis: 90% u. Characterized by fever, chills, skin lesions, arthralgias, tenosynovitis u. Less commonly, hepatitis, myocarditis, endocarditis, meningitis Rash characterized as macular or papular, pustular, hemorrhagic or necrotic, mostly on distal extremities
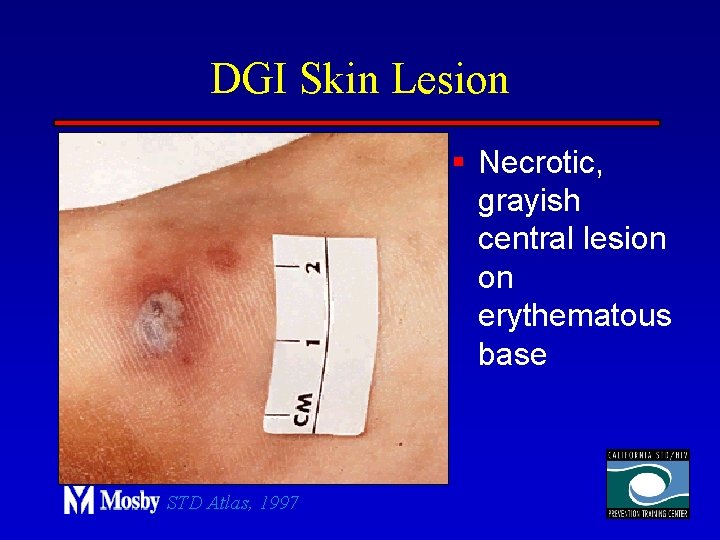
DGI Skin Lesion § Necrotic, grayish central lesion on erythematous base STD Atlas, 1997
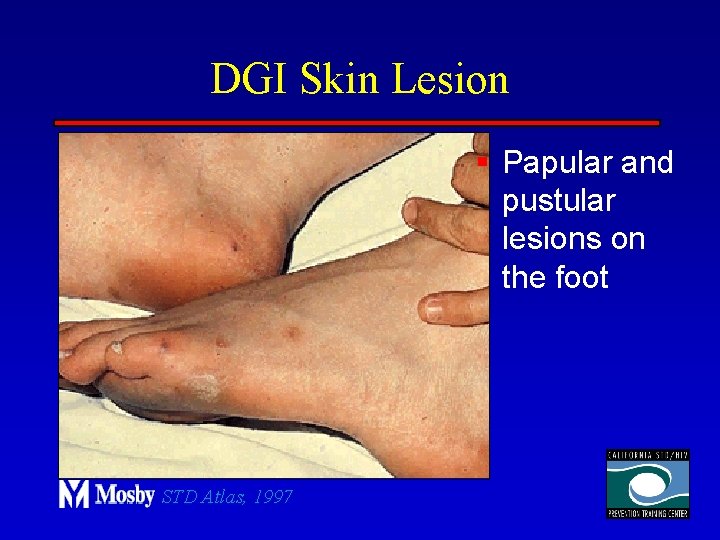
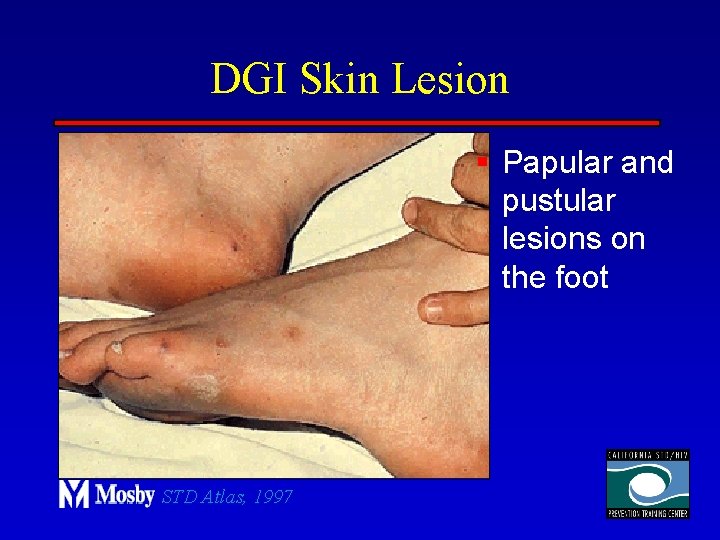
DGI Skin Lesion § Papular and pustular lesions on the foot STD Atlas, 1997

DGI Skin Lesion § Small painful midpalmar lesion on an erythematous base STD Atlas, 1997

DGI Skin Lesion § Pustular erythematous lesions
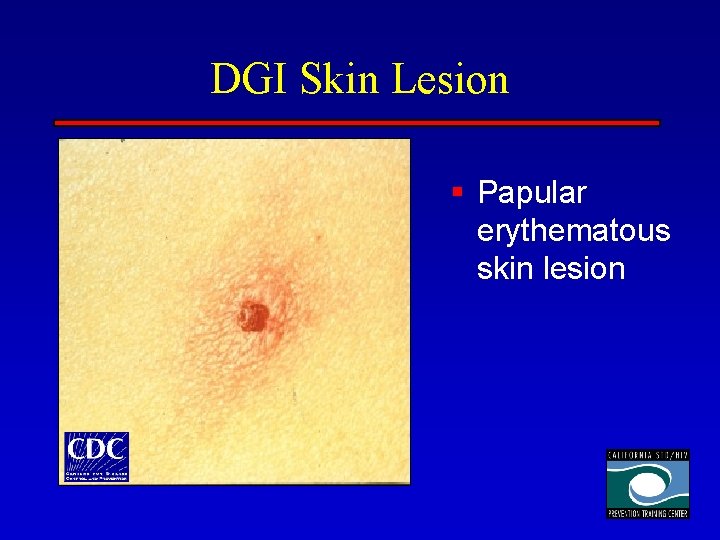
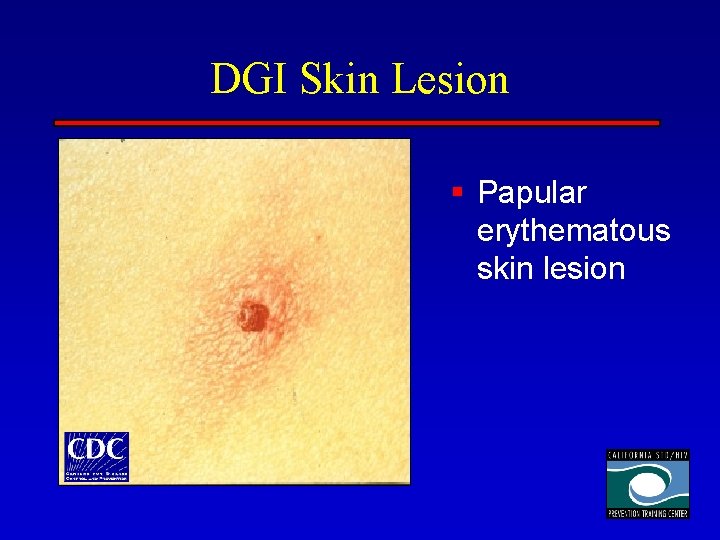
DGI Skin Lesion § Papular erythematous skin lesion
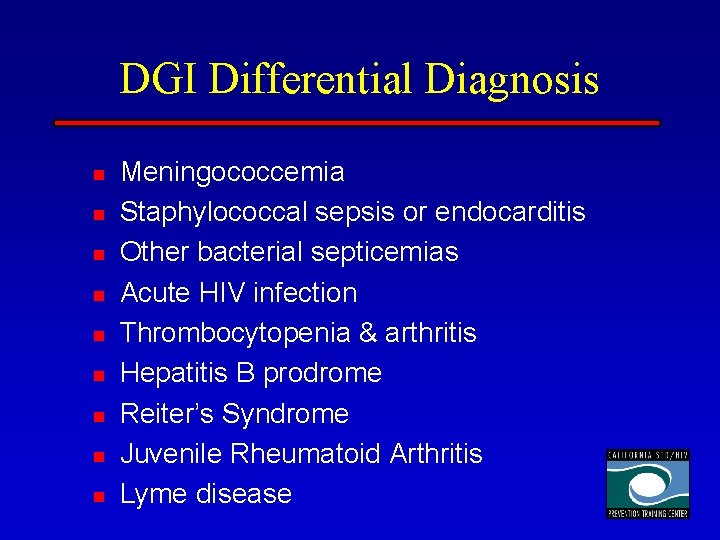
DGI Differential Diagnosis n n n n n Meningococcemia Staphylococcal sepsis or endocarditis Other bacterial septicemias Acute HIV infection Thrombocytopenia & arthritis Hepatitis B prodrome Reiter’s Syndrome Juvenile Rheumatoid Arthritis Lyme disease
Gonococcal Complications in Pregnancy n Postpartum endometritis n Septic abortions n Post-abortal PID Possible role in: § Gestational bleeding § Preterm labor and delivery § Premature rupture of membranes
Vertical Transmission and Neonatal Complications on Gonorrhea Overall vertical transmission rate ~30% Neonatal complications include: v. Ophthalmia neonatorum v. Disseminated gonococcal infection (sepsis, arthritis, meningitis) v. Scalp abscess (if fetal scalp monitor used) v. Vaginal and rectal infections v. Pharyngeal infections
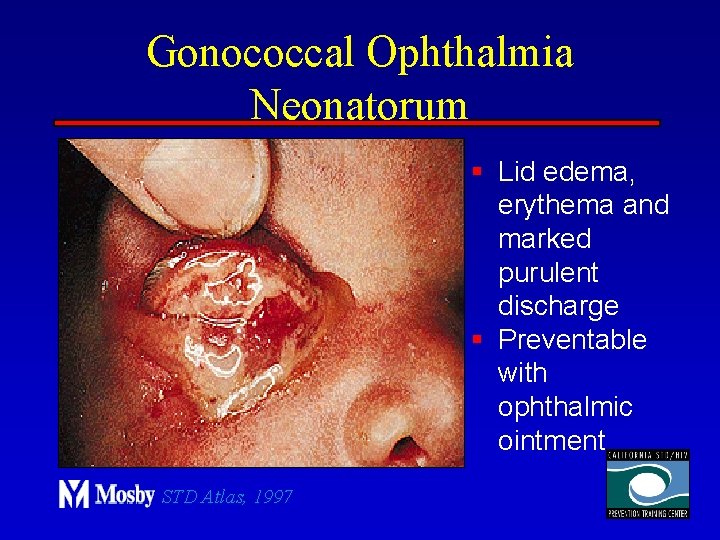
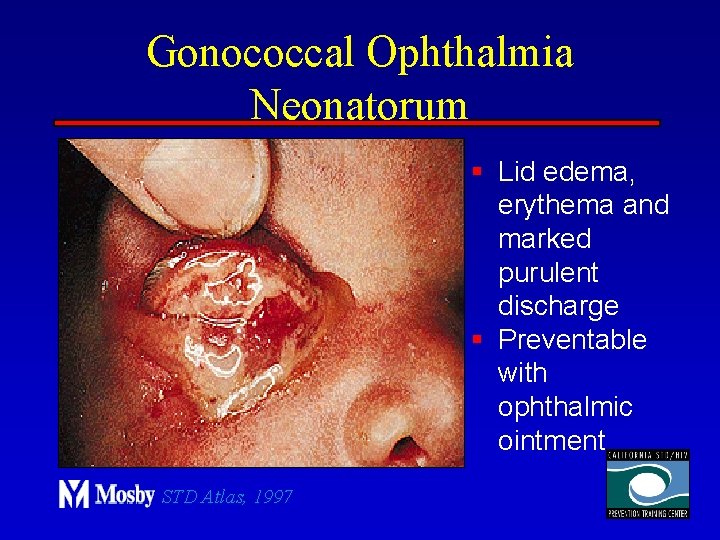
Gonococcal Ophthalmia Neonatorum § Lid edema, erythema and marked purulent discharge § Preventable with ophthalmic ointment STD Atlas, 1997
GC Infections in Children n Vulvovaginits n Urethritis n Proctitis n n All cases should be considered possible evidence of sexual abuse Culture should be obtained
GC Diagnostic Methods n Gram stain smear n Culture n Antigen Detection Tests: EIA & DFA n Nucleic Acid Detection Tests u. Probe Hybridization u. Nucleic Acid Amplification Tests (NAATs) u. Hybrid Capture

Gonorrhea Diagnostic Tests Sensitivity Gram stain 90 -95% Specificity 95% (male urethra exudate) DNA probe 85 -90% 95% Culture 80 -95% 99% NAATs * 90 -95% 98% * Able to use URINE specimens
GC Gram Stain n n In symptomatic male urethritis: u>95% sensitivity and specificity: reliable to diagnose and exclude GC In cervicitis: u 50 -70%sensitivity, 95% specificity Not useful in pharyngeal infections Accessory gland infection: similar to male urethritis Proctitis: similar to cervicitis

Gram Stain for GC: Urethral Smear n n STD Atlas, 1997 Numerous PMNs Gram negative intracellular diplococci
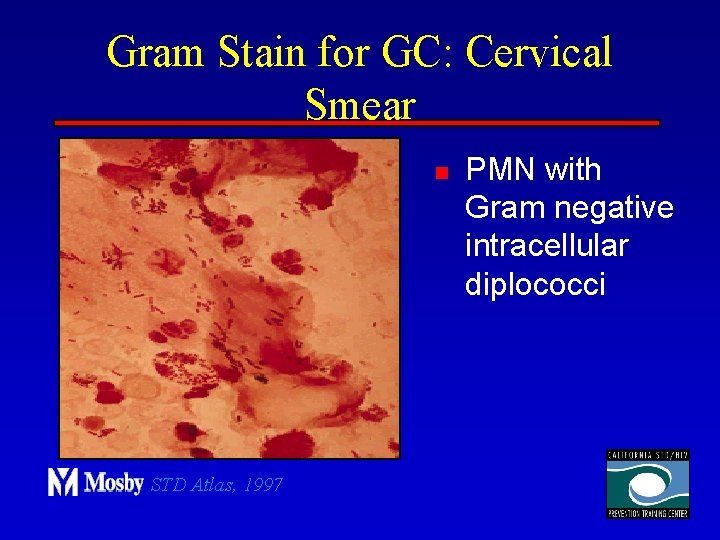
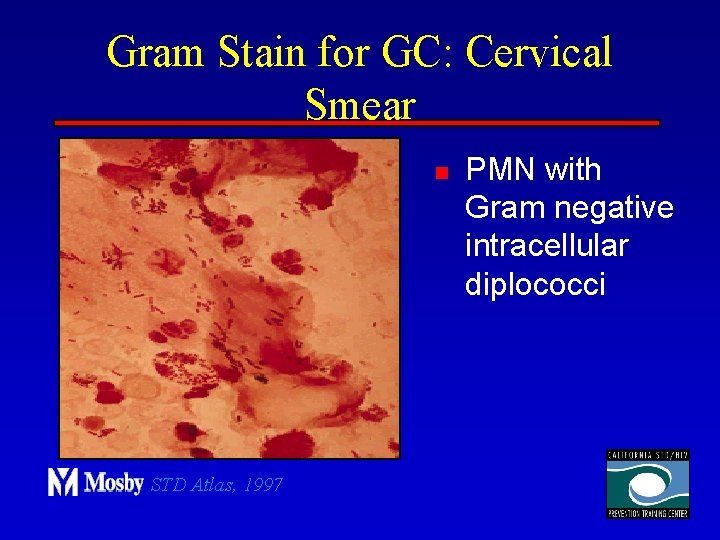
Gram Stain for GC: Cervical Smear n STD Atlas, 1997 PMN with Gram negative intracellular diplococci
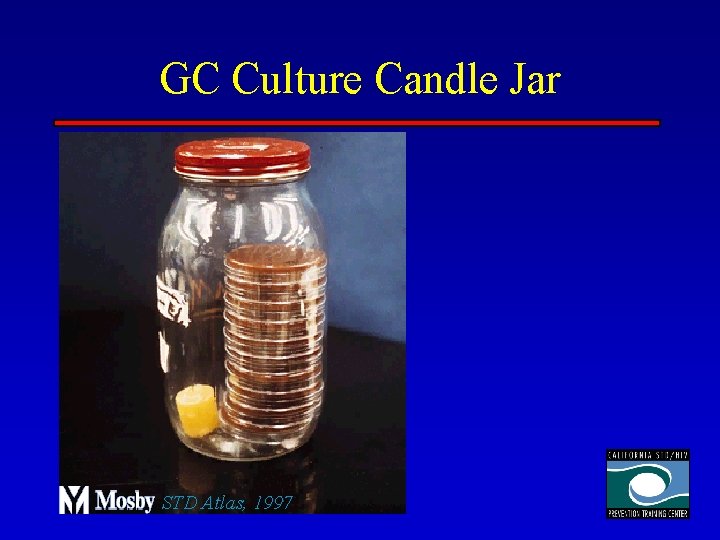
GC Culture n n Requires selective media with antibiotics to inhibit competing bacteria (Modified Thayer Martin Media, NYC Medium) Sensitive to oxygen and cold temperature Requires prompt placement in high-CO 2 environment (candle jar, bag and pill, CO 2 incubator) In cases of suspected sexual abuse, culture is the only test accepted for legal purposes
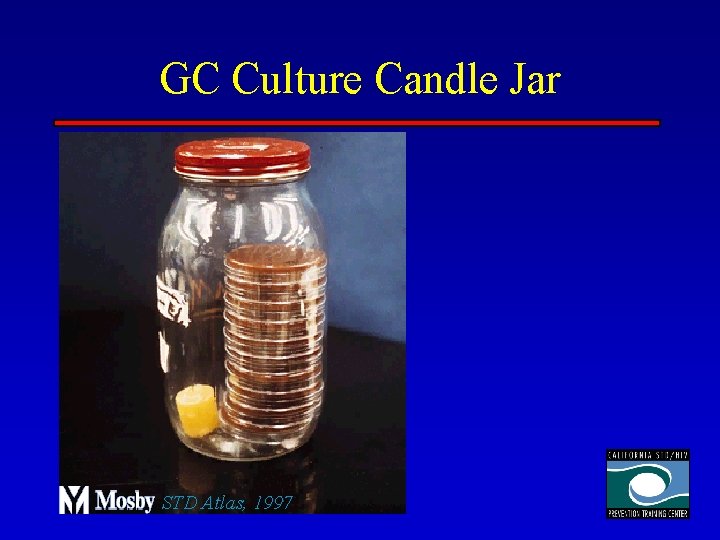
GC Culture Candle Jar STD Atlas, 1997
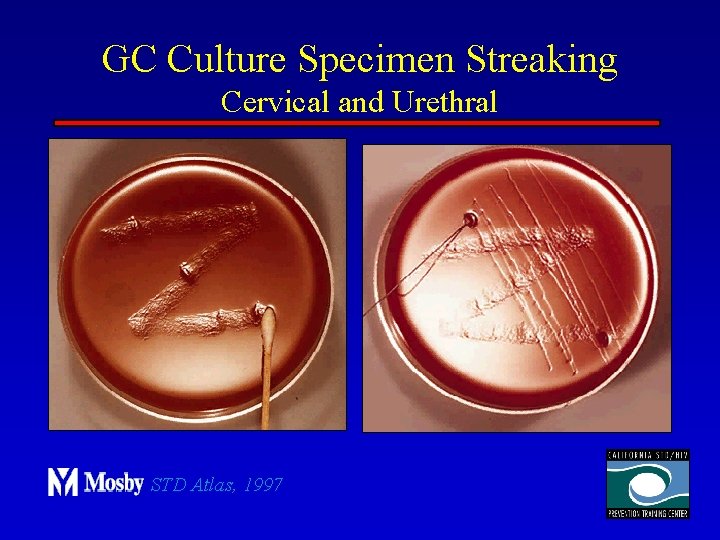
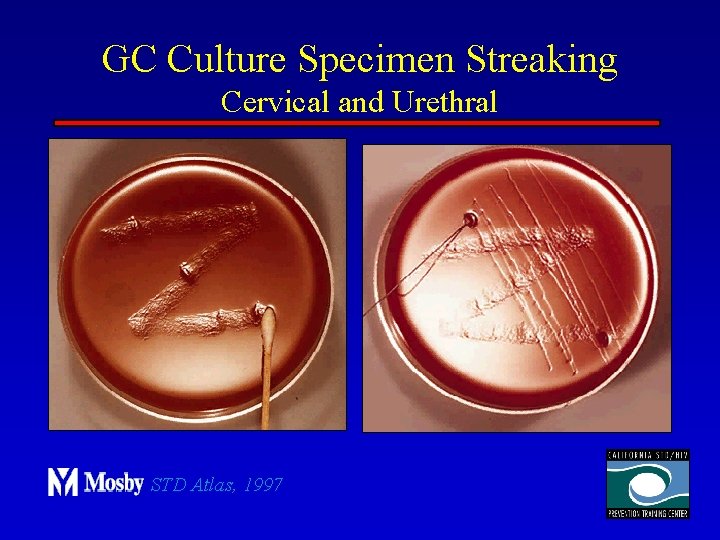
GC Culture Specimen Streaking Cervical and Urethral STD Atlas, 1997
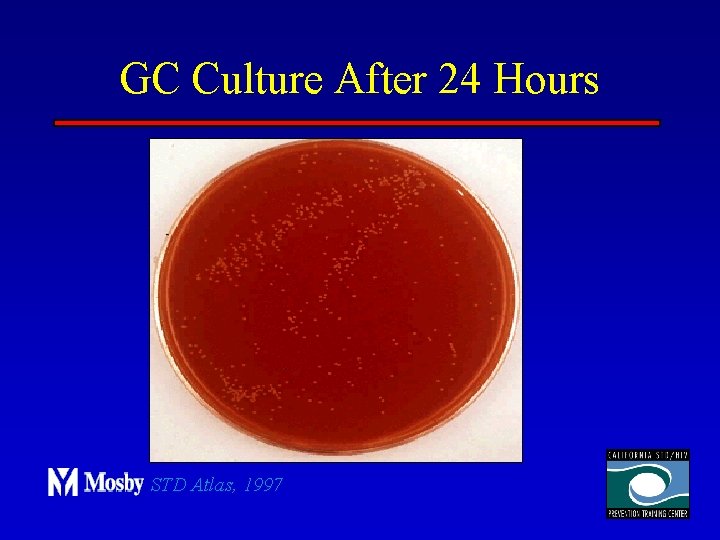
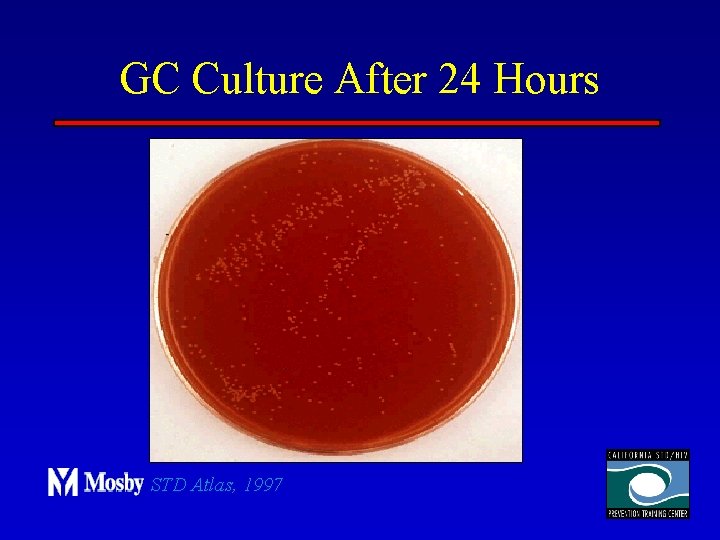
GC Culture After 24 Hours STD Atlas, 1997
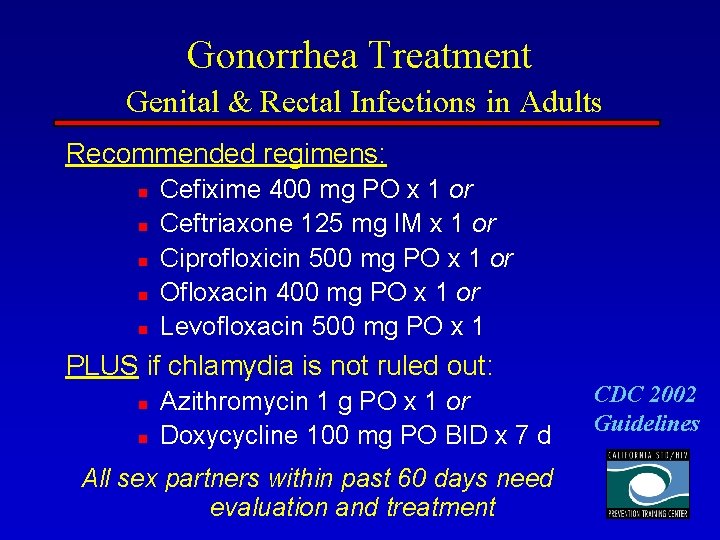
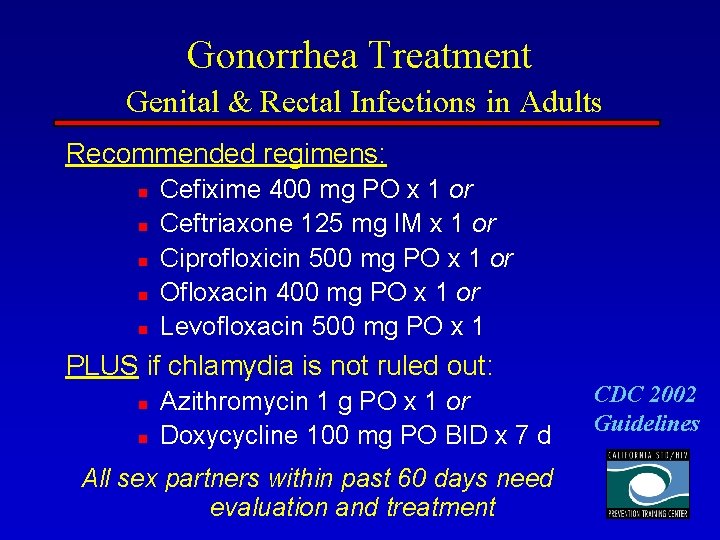
Gonorrhea Treatment Genital & Rectal Infections in Adults Recommended regimens: n n n Cefixime 400 mg PO x 1 or Ceftriaxone 125 mg IM x 1 or Ciprofloxicin 500 mg PO x 1 or Ofloxacin 400 mg PO x 1 or Levofloxacin 500 mg PO x 1 PLUS if chlamydia is not ruled out: n n Azithromycin 1 g PO x 1 or Doxycycline 100 mg PO BID x 7 d All sex partners within past 60 days need evaluation and treatment CDC 2002 Guidelines
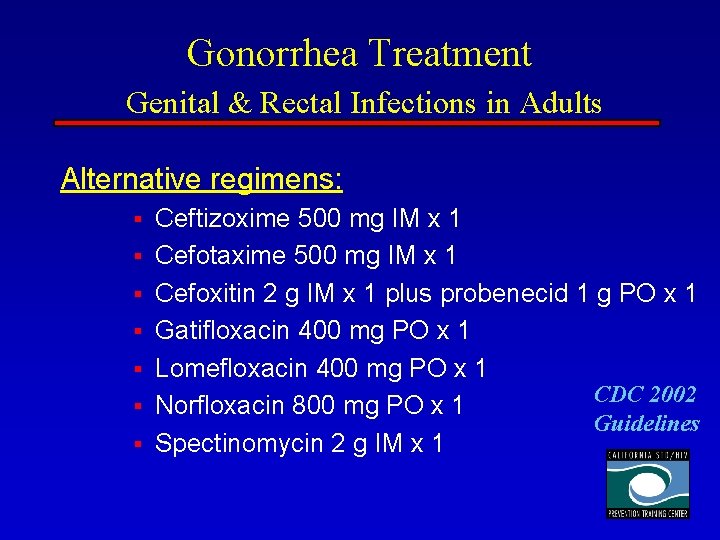
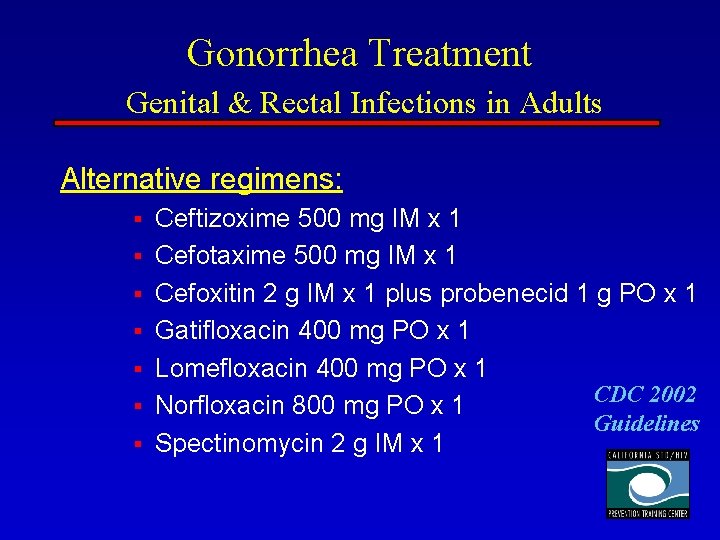
Gonorrhea Treatment Genital & Rectal Infections in Adults Alternative regimens: § § § § Ceftizoxime 500 mg IM x 1 Cefotaxime 500 mg IM x 1 Cefoxitin 2 g IM x 1 plus probenecid 1 g PO x 1 Gatifloxacin 400 mg PO x 1 Lomefloxacin 400 mg PO x 1 CDC 2002 Norfloxacin 800 mg PO x 1 Guidelines Spectinomycin 2 g IM x 1
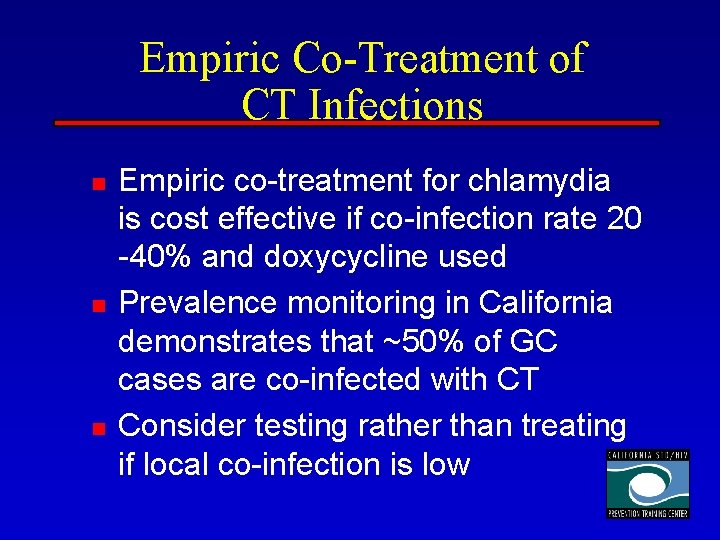
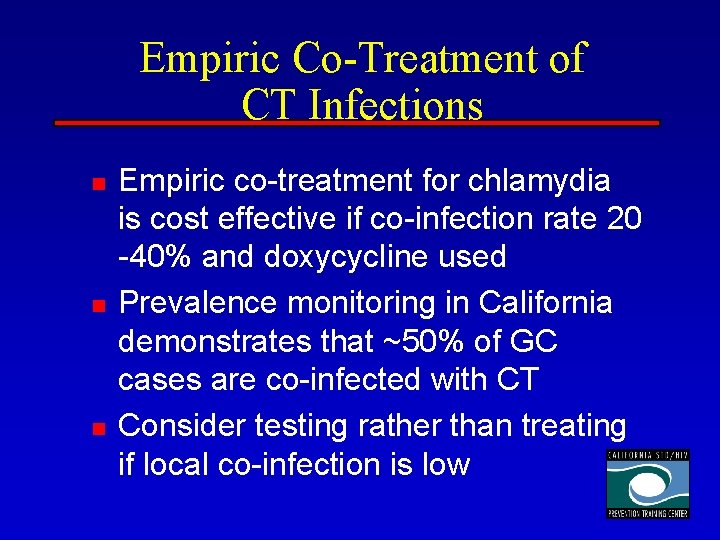
Empiric Co-Treatment of CT Infections n n n Empiric co-treatment for chlamydia is cost effective if co-infection rate 20 -40% and doxycycline used Prevalence monitoring in California demonstrates that ~50% of GC cases are co-infected with CT Consider testing rather than treating if local co-infection is low
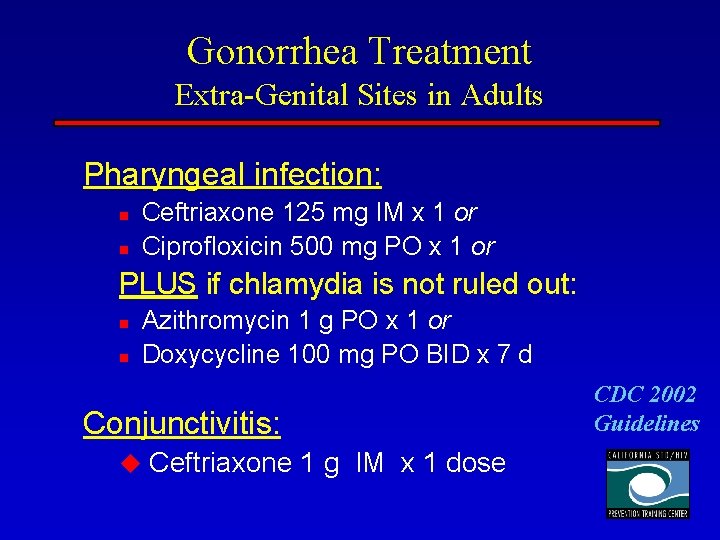
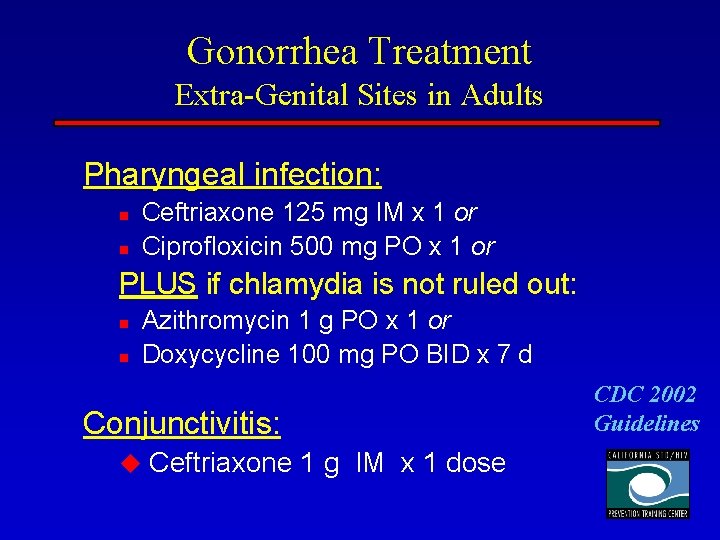
Gonorrhea Treatment Extra-Genital Sites in Adults Pharyngeal infection: n n Ceftriaxone 125 mg IM x 1 or Ciprofloxicin 500 mg PO x 1 or PLUS if chlamydia is not ruled out: n n Azithromycin 1 g PO x 1 or Doxycycline 100 mg PO BID x 7 d Conjunctivitis: u Ceftriaxone 1 g IM x 1 dose CDC 2002 Guidelines
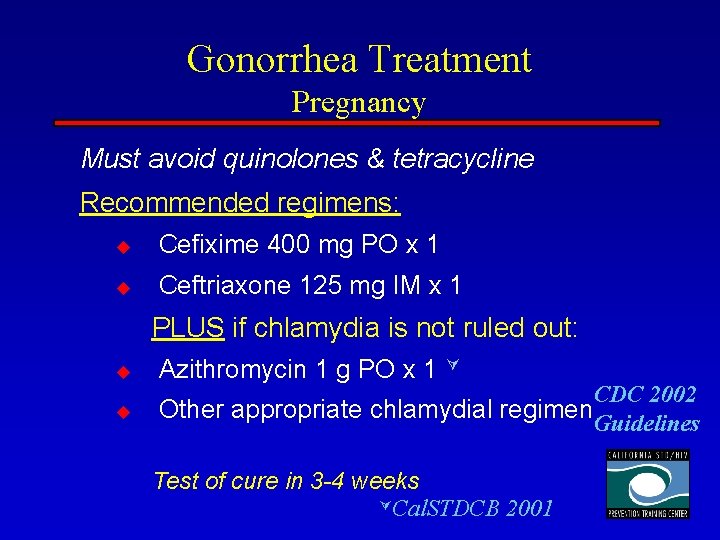
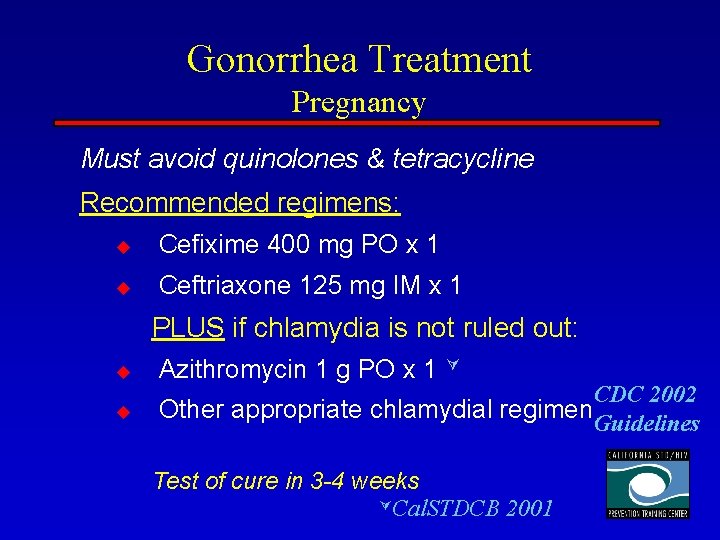
Gonorrhea Treatment Pregnancy Must avoid quinolones & tetracycline Recommended regimens: u Cefixime 400 mg PO x 1 u Ceftriaxone 125 mg IM x 1 PLUS if chlamydia is not ruled out: u u Azithromycin 1 g PO x 1 CDC 2002 Other appropriate chlamydial regimen. Guidelines Test of cure in 3 -4 weeks Cal. STDCB 2001
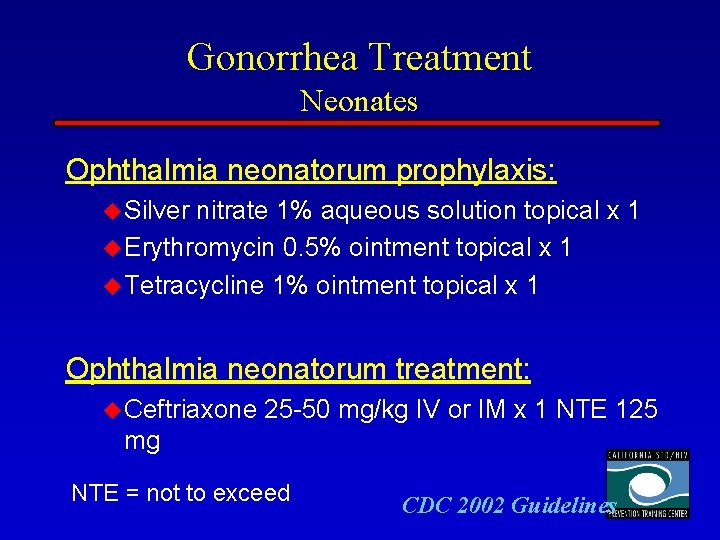
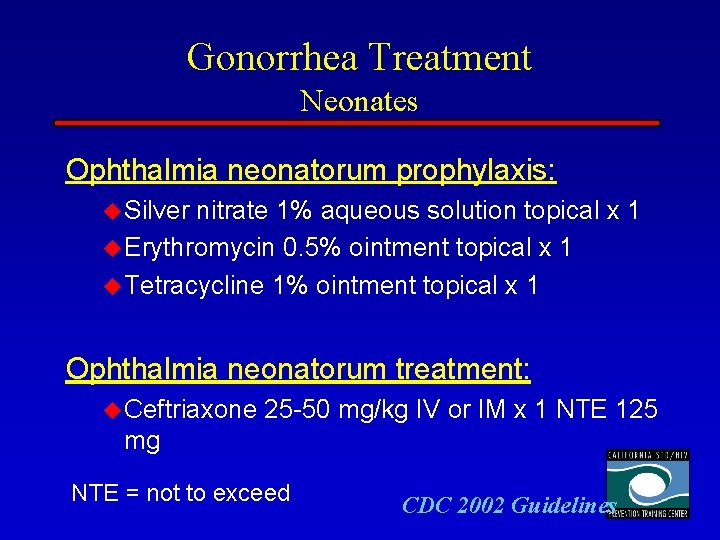
Gonorrhea Treatment Neonates Ophthalmia neonatorum prophylaxis: u Silver nitrate 1% aqueous solution topical x 1 u Erythromycin 0. 5% ointment topical x 1 u Tetracycline 1% ointment topical x 1 Ophthalmia neonatorum treatment: u Ceftriaxone 25 -50 mg/kg IV or IM x 1 NTE 125 mg NTE = not to exceed CDC 2002 Guidelines
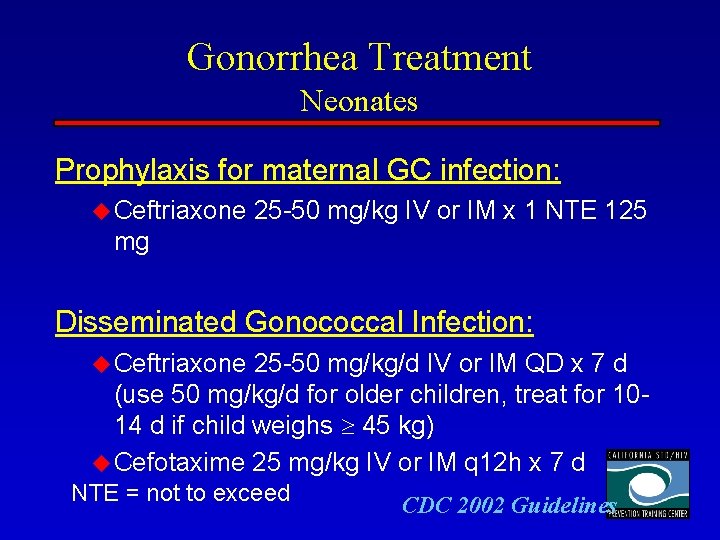
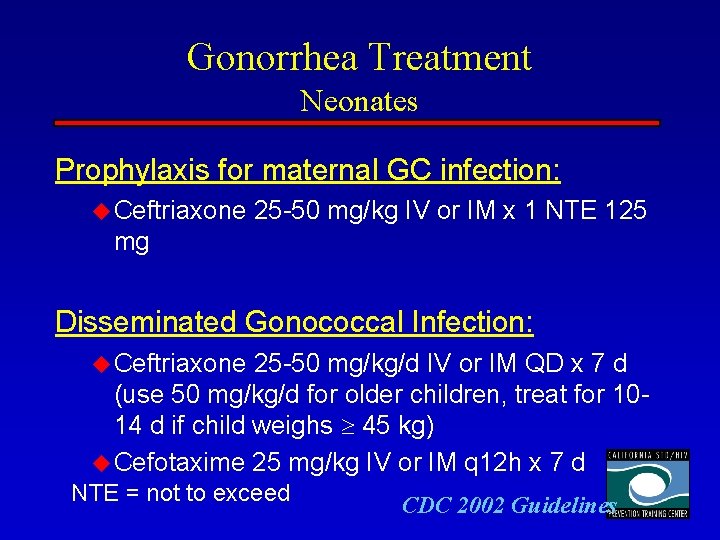
Gonorrhea Treatment Neonates Prophylaxis for maternal GC infection: u Ceftriaxone 25 -50 mg/kg IV or IM x 1 NTE 125 mg Disseminated Gonococcal Infection: u Ceftriaxone 25 -50 mg/kg/d IV or IM QD x 7 d (use 50 mg/kg/d for older children, treat for 1014 d if child weighs 45 kg) u Cefotaxime 25 mg/kg IV or IM q 12 h x 7 d NTE = not to exceed CDC 2002 Guidelines
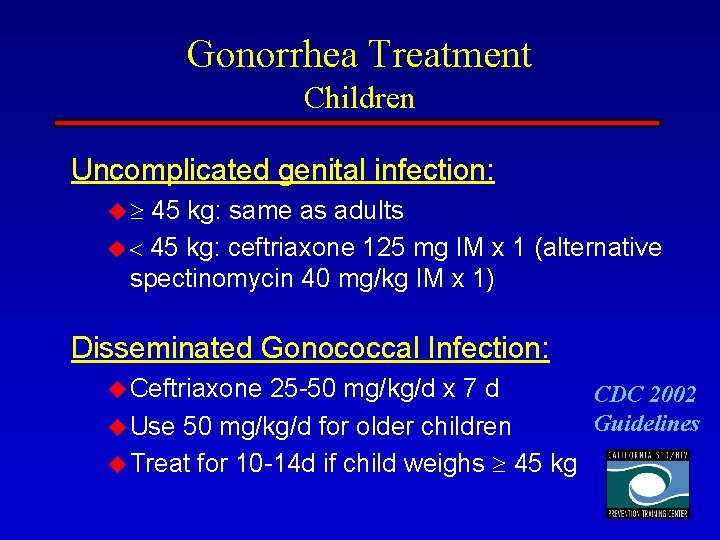
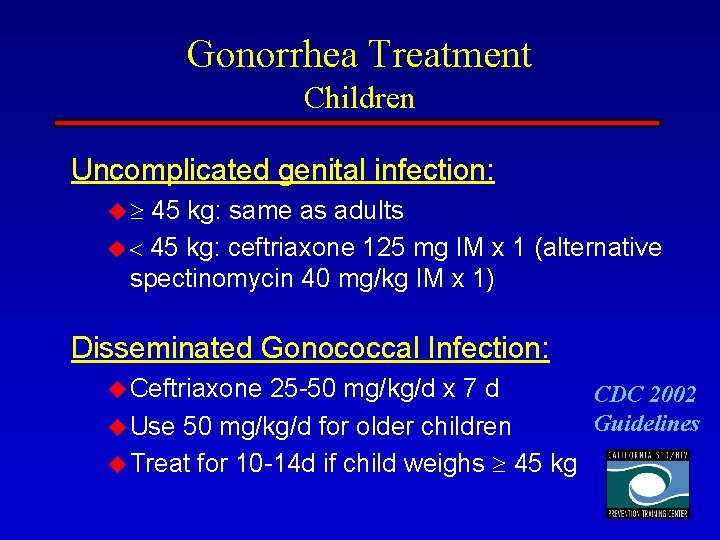
Gonorrhea Treatment Children Uncomplicated genital infection: u 45 kg: same as adults u 45 kg: ceftriaxone 125 mg IM x 1 (alternative spectinomycin 40 mg/kg IM x 1) Disseminated Gonococcal Infection: u Ceftriaxone 25 -50 mg/kg/d x 7 d CDC 2002 Guidelines u Use 50 mg/kg/d for older children u Treat for 10 -14 d if child weighs 45 kg
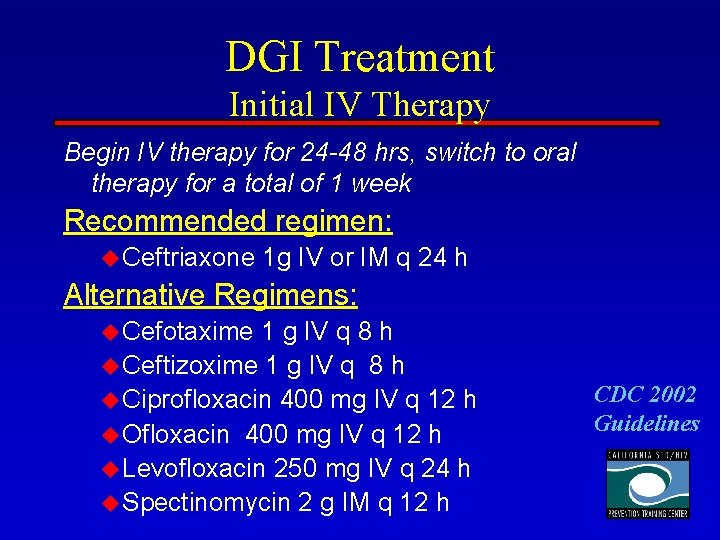
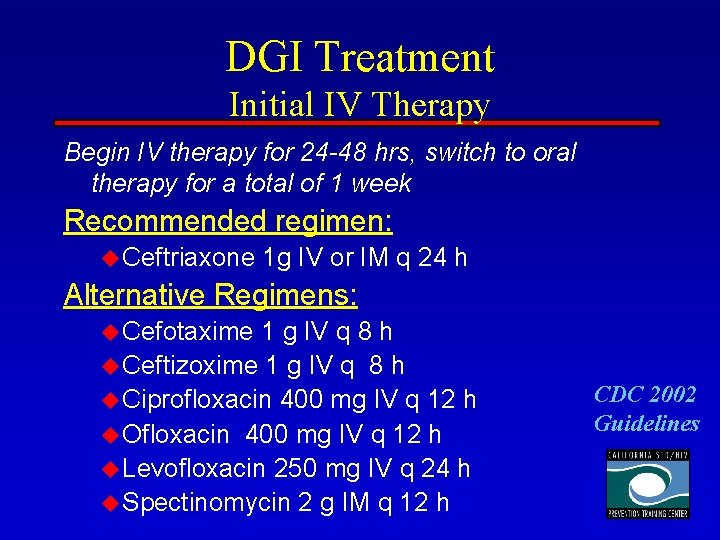
DGI Treatment Initial IV Therapy Begin IV therapy for 24 -48 hrs, switch to oral therapy for a total of 1 week Recommended regimen: u Ceftriaxone 1 g IV or IM q 24 h Alternative Regimens: u Cefotaxime 1 g IV q 8 h u Ceftizoxime 1 g IV q 8 h u Ciprofloxacin 400 mg IV q 12 h u Ofloxacin 400 mg IV q 12 h u Levofloxacin 250 mg IV q 24 h u Spectinomycin 2 g IM q 12 h CDC 2002 Guidelines
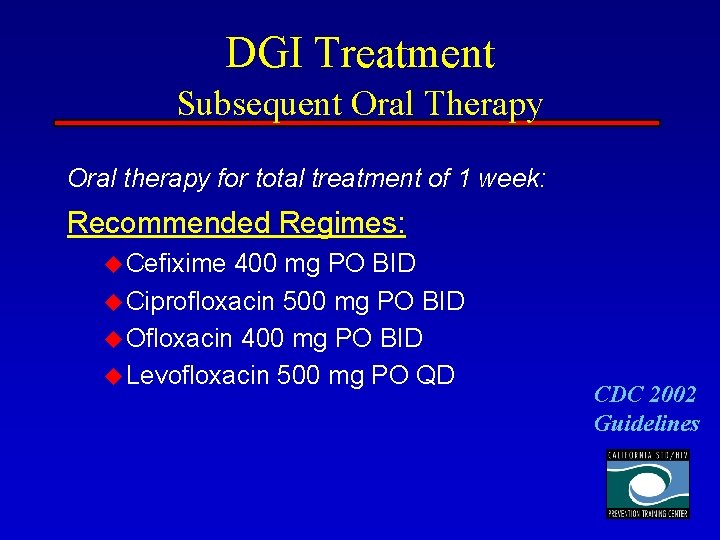
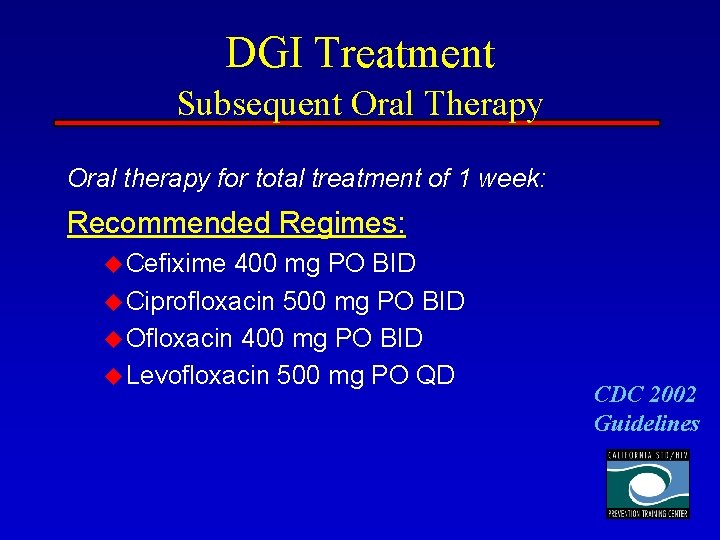
DGI Treatment Subsequent Oral Therapy Oral therapy for total treatment of 1 week: Recommended Regimes: u Cefixime 400 mg PO BID u Ciprofloxacin 500 mg PO BID u Ofloxacin 400 mg PO BID u Levofloxacin 500 mg PO QD CDC 2002 Guidelines
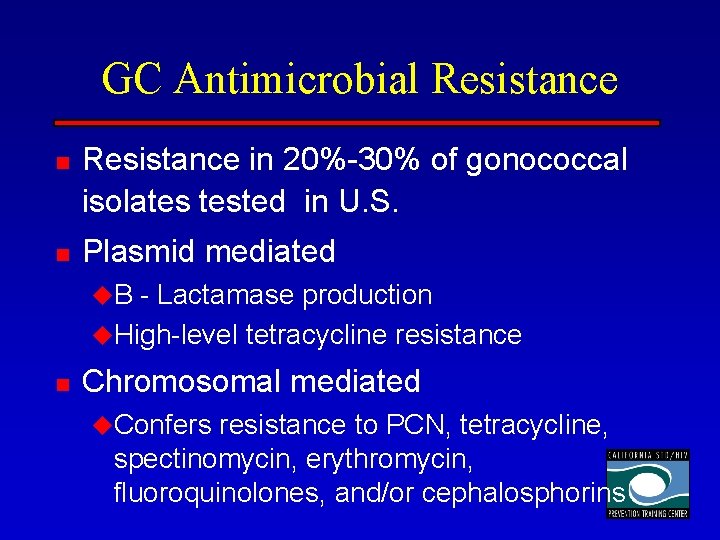
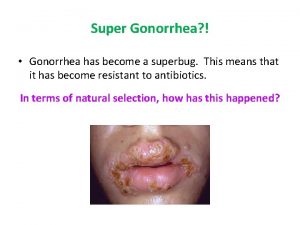
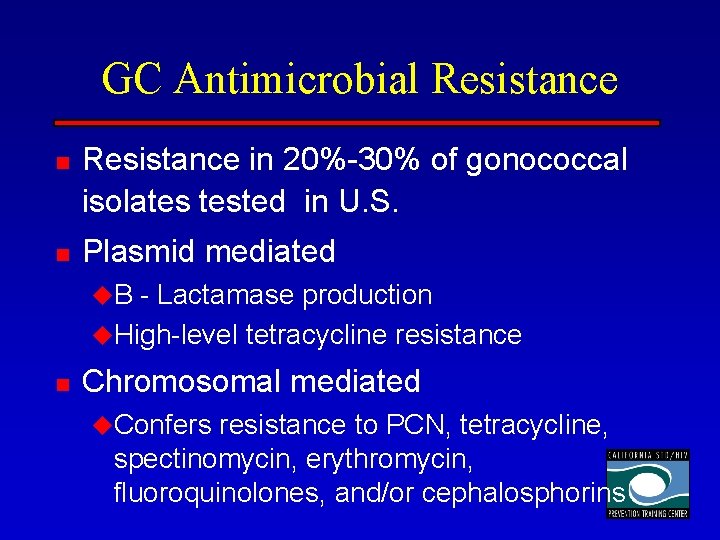
GC Antimicrobial Resistance n n Resistance in 20%-30% of gonococcal isolates tested in U. S. Plasmid mediated u. B - Lactamase production u. High-level tetracycline resistance n Chromosomal mediated u. Confers resistance to PCN, tetracycline, spectinomycin, erythromycin, fluoroquinolones, and/or cephalosphorins
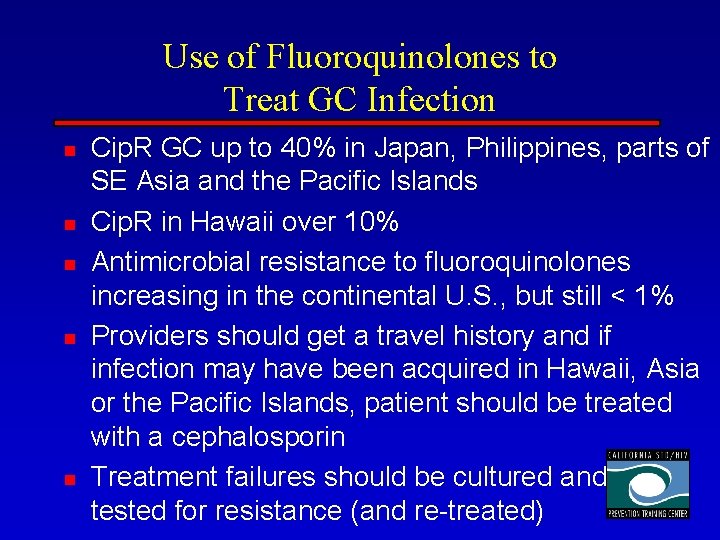
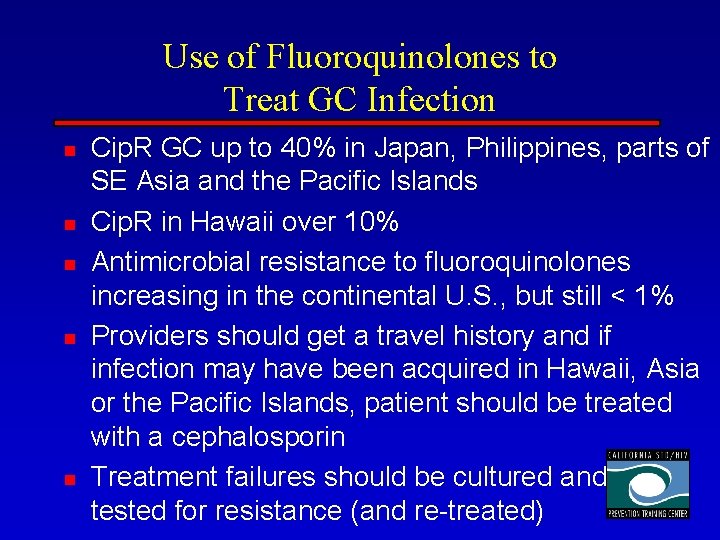
Use of Fluoroquinolones to Treat GC Infection n n Cip. R GC up to 40% in Japan, Philippines, parts of SE Asia and the Pacific Islands Cip. R in Hawaii over 10% Antimicrobial resistance to fluoroquinolones increasing in the continental U. S. , but still < 1% Providers should get a travel history and if infection may have been acquired in Hawaii, Asia or the Pacific Islands, patient should be treated with a cephalosporin Treatment failures should be cultured and tested for resistance (and re-treated)
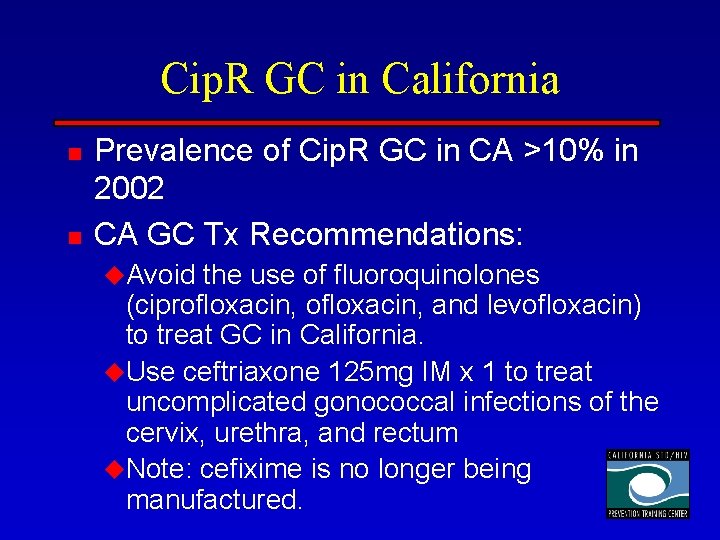
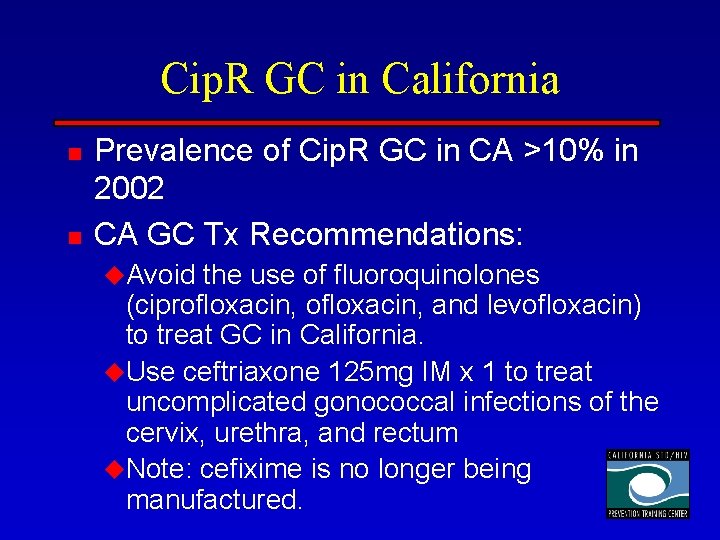
Cip. R GC in California n n Prevalence of Cip. R GC in CA >10% in 2002 CA GC Tx Recommendations: u. Avoid the use of fluoroquinolones (ciprofloxacin, and levofloxacin) to treat GC in California. u. Use ceftriaxone 125 mg IM x 1 to treat uncomplicated gonococcal infections of the cervix, urethra, and rectum u. Note: cefixime is no longer being manufactured.
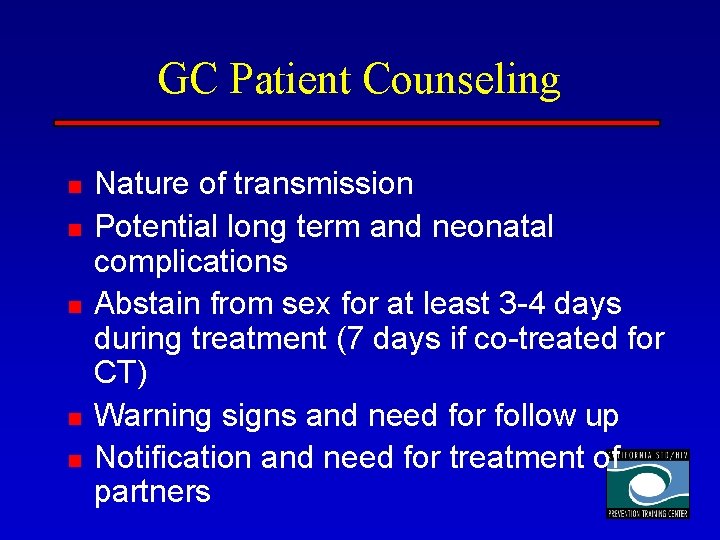
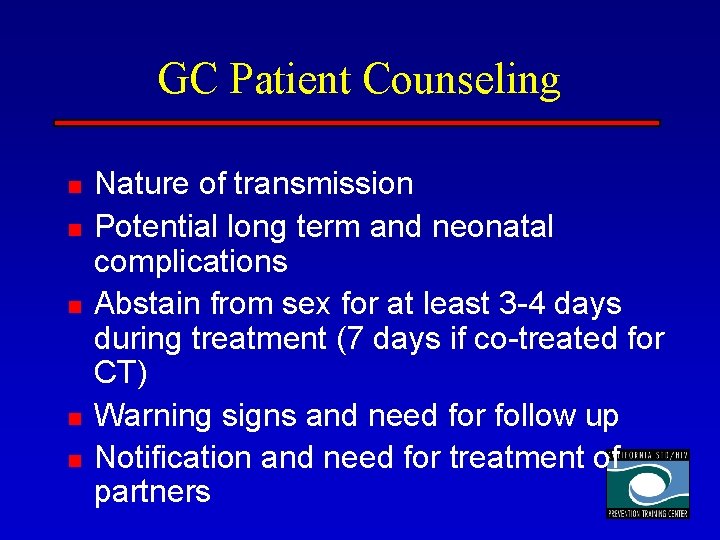
GC Patient Counseling n n n Nature of transmission Potential long term and neonatal complications Abstain from sex for at least 3 -4 days during treatment (7 days if co-treated for CT) Warning signs and need for follow up Notification and need for treatment of partners
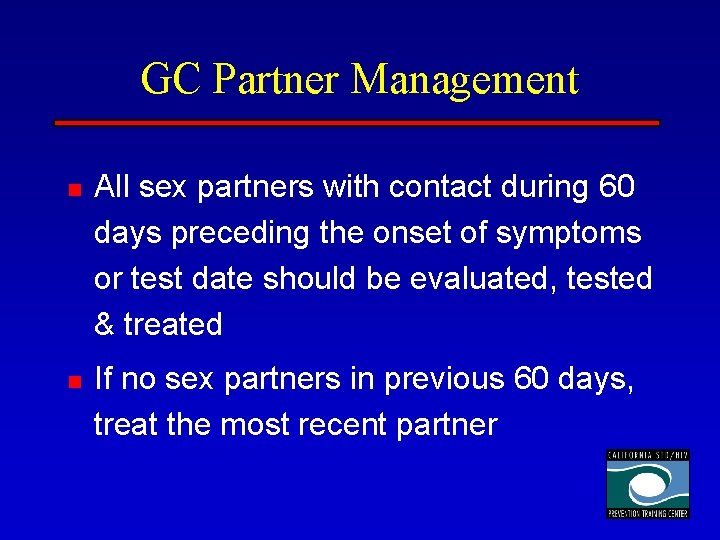
GC Partner Management n n All sex partners with contact during 60 days preceding the onset of symptoms or test date should be evaluated, tested & treated If no sex partners in previous 60 days, treat the most recent partner
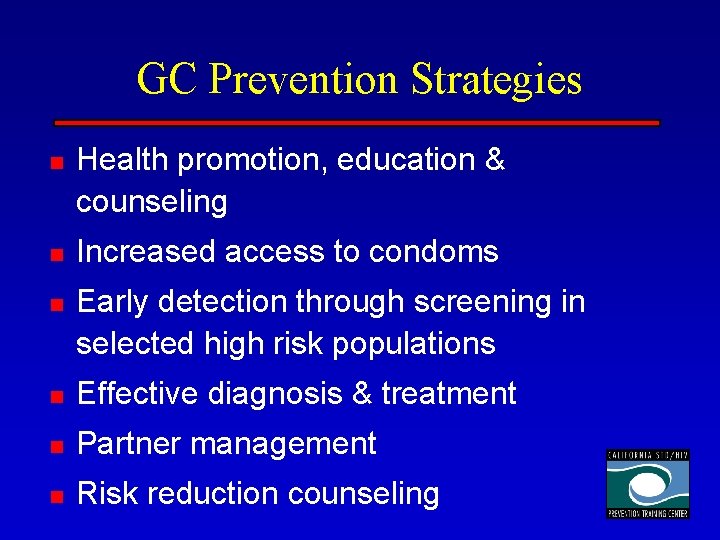
GC Prevention Strategies n n n Health promotion, education & counseling Increased access to condoms Early detection through screening in selected high risk populations n Effective diagnosis & treatment n Partner management n Risk reduction counseling
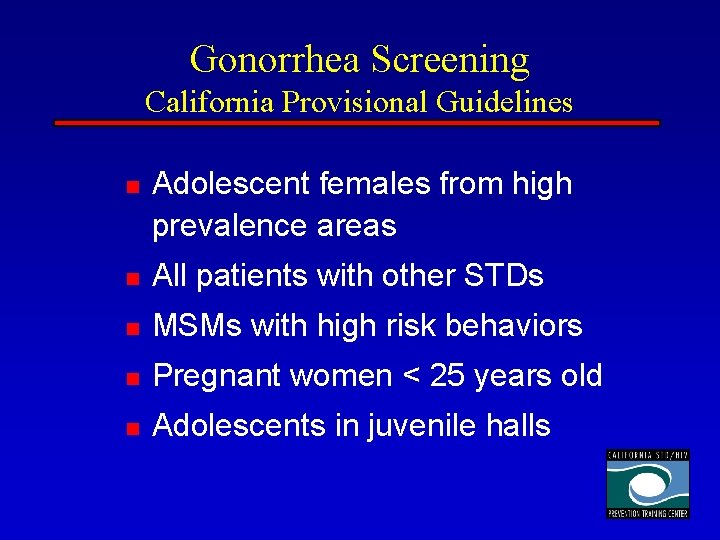
Gonorrhea Screening California Provisional Guidelines n Adolescent females from high prevalence areas n All patients with other STDs n MSMs with high risk behaviors n Pregnant women < 25 years old n Adolescents in juvenile halls
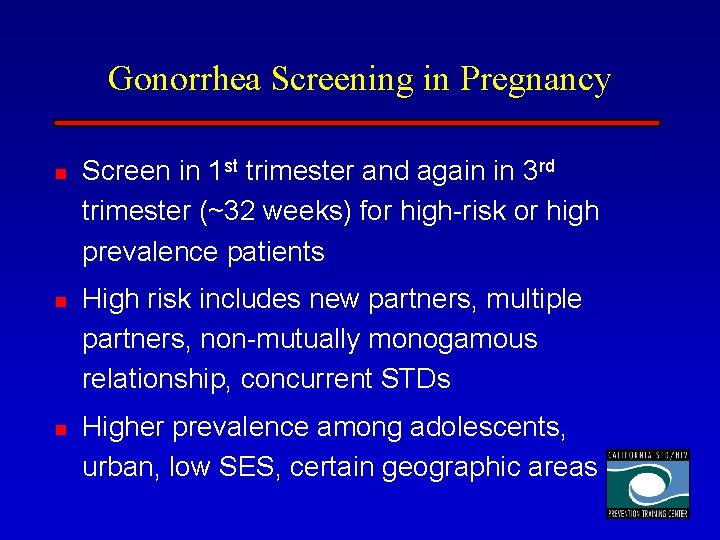
Gonorrhea Screening in Pregnancy n n n Screen in 1 st trimester and again in 3 rd trimester (~32 weeks) for high-risk or high prevalence patients High risk includes new partners, multiple partners, non-mutually monogamous relationship, concurrent STDs Higher prevalence among adolescents, urban, low SES, certain geographic areas
 Primary prevention secondary prevention tertiary prevention
Primary prevention secondary prevention tertiary prevention Dr grace alfonsi
Dr grace alfonsi Std partner notification laws california
Std partner notification laws california Papilomma
Papilomma Cmv microcephaly
Cmv microcephaly Gonorrhea symptoms female
Gonorrhea symptoms female Neisseria gonorrhoeae ph
Neisseria gonorrhoeae ph Stds that cannot be cured
Stds that cannot be cured Symptoms of gonorrhea
Symptoms of gonorrhea Gonorrhea
Gonorrhea Diplococcus gram negatif
Diplococcus gram negatif Youtube
Youtube Gonorrhea
Gonorrhea Gonorrhea
Gonorrhea Indiana prevention resource center
Indiana prevention resource center Spill prevention control and countermeasure training ppt
Spill prevention control and countermeasure training ppt Alankrita singh ips
Alankrita singh ips Bullying prevention training
Bullying prevention training Electrical safety signs and symbols ppt
Electrical safety signs and symbols ppt Was it sexual abuse quiz
Was it sexual abuse quiz Spill prevention control & countermeasures training
Spill prevention control & countermeasures training Robbery awareness
Robbery awareness Army suicide prevention training
Army suicide prevention training Jain center of northern california
Jain center of northern california Southern california earthquake data center
Southern california earthquake data center California service center laguna niguel
California service center laguna niguel California lti training
California lti training University clinical center tuzla
University clinical center tuzla Yale center for clinical investigation
Yale center for clinical investigation University clinical center tuzla
University clinical center tuzla Fda clinical investigator training course
Fda clinical investigator training course Basic clinical observations training
Basic clinical observations training Student doctor method of clinical training
Student doctor method of clinical training Oracle clinical training ppt
Oracle clinical training ppt Asbmt clinical research training course
Asbmt clinical research training course Mrc senior clinical fellowship
Mrc senior clinical fellowship Texasassessment telpas training center
Texasassessment telpas training center Pratt & whitney customer training center
Pratt & whitney customer training center Nipt test kuwait
Nipt test kuwait Boardman training center
Boardman training center International training center ilo
International training center ilo Iec training center
Iec training center Highveld training centre
Highveld training centre Telpas headset requirements
Telpas headset requirements Green world international training center
Green world international training center Telpas calibration certificate
Telpas calibration certificate Green world international training center
Green world international training center Robert bosch training
Robert bosch training Tmss training center
Tmss training center International training center of the ilo
International training center of the ilo Joint special operations medical training center
Joint special operations medical training center Rwj training center
Rwj training center Western regional training center
Western regional training center Wave training center
Wave training center Hp training center
Hp training center Green world management consultant & training institute
Green world management consultant & training institute Telpas rater manual 2020
Telpas rater manual 2020 Cheongpyeong heaven and earth training center
Cheongpyeong heaven and earth training center Training is expensive without training it is more expensive
Training is expensive without training it is more expensive