Golive Set Ready Get ready for Commonly Used







- Slides: 32

Go-live Set Ready Get ready for
Commonly Used Terminology A-19 - A billing document used or submitted to DSHS by some providers or used to authorize special payment for DSHS services. A-19 s are manually processed by Staff to initiate payment by the Agency Financial Reporting System (AFRS). Adjudication- A process in which a claim is determined valid, payable, and is account coded. Adjustments- An increase or decrease in rate or units from previously billed month. Provider. One Authorization-An agreement between DSHS, a client and/or a provider authorizing payment to the provider or client for a service that has, or will be performed. An authorization may include service begin and end dates, lengths of service, units of service and maximum number of units, rates to be paid for each service, and other service line details. 7/21/2016 2
Commonly Used Terminology (Cont’d) County Service Authorization (CSA)- An agreement between DDA, County, and Provider for Client Services Profile-A profile is a type of access to Provider. One person may have more than one profile. The profile needed for seeing county claims is EXT Provider Social Service. Remittance Advice (RA)-A PDF document that describes the payment. This includes a summary and client specific payment information Warrant- A guarantee of payment by the Washington State Treasurer. A warrant differs from a check in that a check is not a guarantee of payment and is dependent upon availability of funds. A warrant is guaranteed. 7/21/2016 3
What are the Benefits of Provider. One? ◦ Improves system editing and reduces payment errors ◦ Makes future payment system changes more efficient ◦ Reduces costs - improves cost recovery ◦ Reduces fraud ◦ Provides flexible and responsive reporting to facilitate better decisionmaking about the Medicaid program ◦ Maximizes federal matching dollars ◦ Provides timely and accurate payment 7/21/2016 4
What is Available to View in P 1? (According to your profile. Different profiles have different levels of access. ) o View the Remittance Advice (RA) o View claims history o View adjustment history o View P 1 authorizations o View location information such as addresses and phone numbers 7/21/2016 5
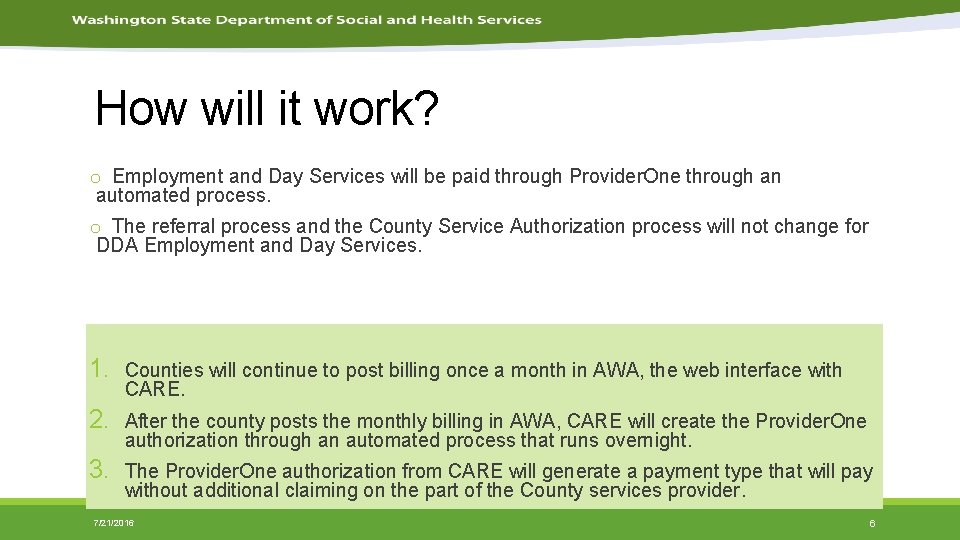
How will it work? o Employment and Day Services will be paid through Provider. One through an automated process. o The referral process and the County Service Authorization process will not change for DDA Employment and Day Services. 1. Counties will continue to post billing once a month in AWA, the web interface with CARE. 2. After the county posts the monthly billing in AWA, CARE will create the Provider. One authorization through an automated process that runs overnight. 3. The Provider. One authorization from CARE will generate a payment type that will pay without additional claiming on the part of the County services provider. 7/21/2016 6
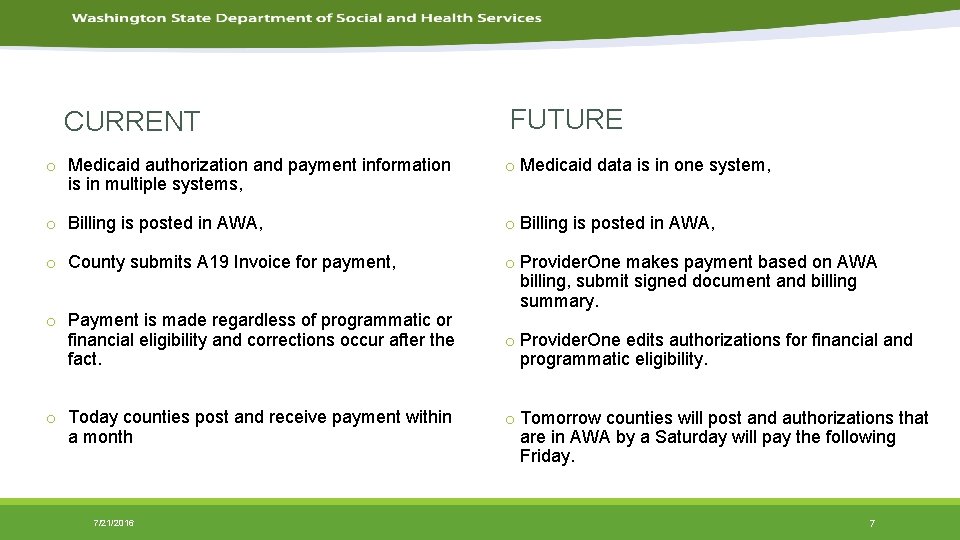
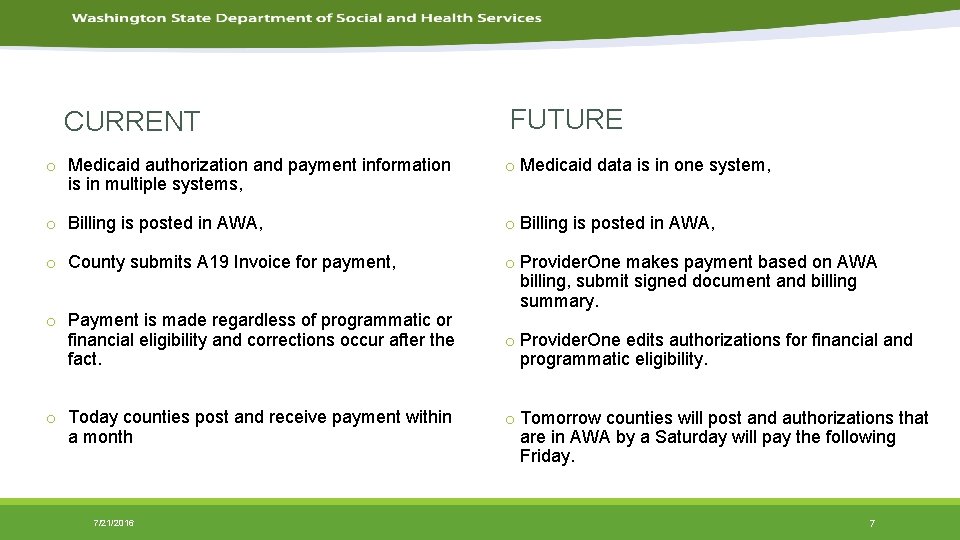
CURRENT FUTURE o Medicaid authorization and payment information is in multiple systems, o Medicaid data is in one system, o Billing is posted in AWA, o County submits A 19 Invoice for payment, o Provider. One makes payment based on AWA billing, submit signed document and billing summary. o Payment is made regardless of programmatic or financial eligibility and corrections occur after the fact. o Today counties post and receive payment within a month 7/21/2016 o Provider. One edits authorizations for financial and programmatic eligibility. o Tomorrow counties will post and authorizations that are in AWA by a Saturday will pay the following Friday. 7
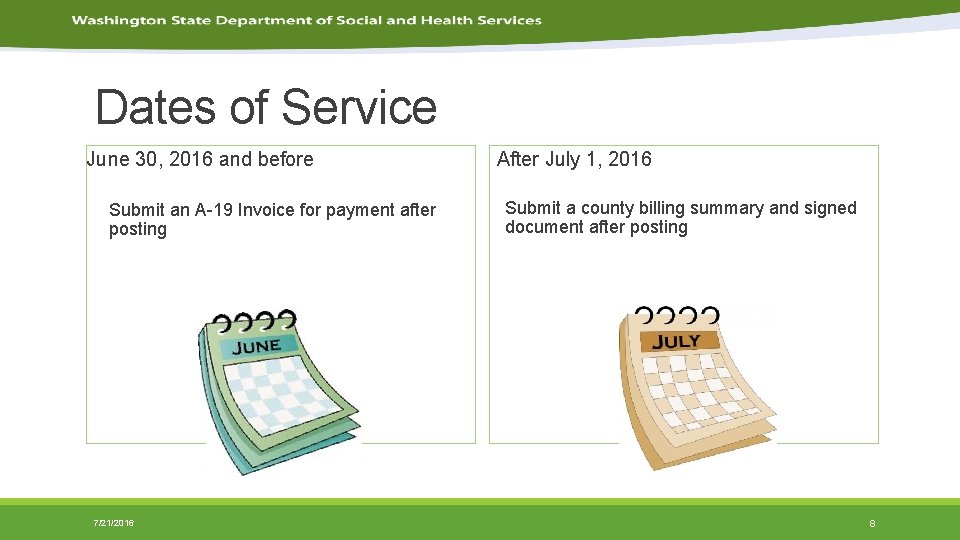
Dates of Service June 30, 2016 and before Submit an A-19 Invoice for payment after posting 7/21/2016 After July 1, 2016 Submit a county billing summary and signed document after posting 8
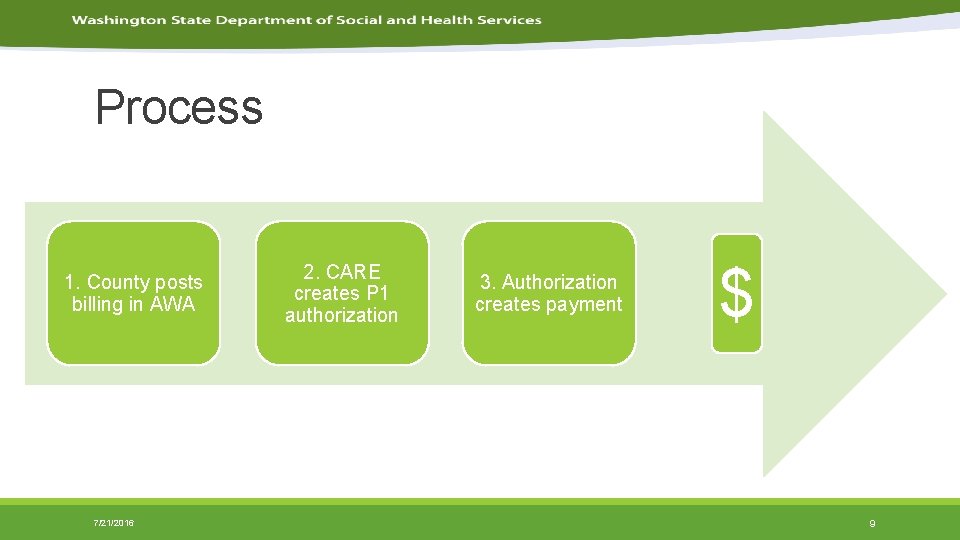
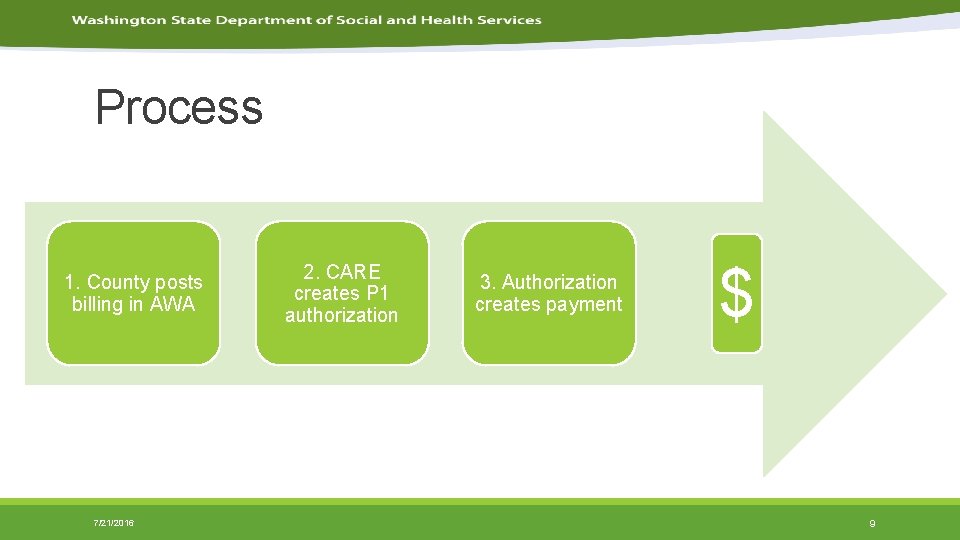
Process 1. County posts billing in AWA 7/21/2016 2. CARE creates P 1 authorization 3. Authorization creates payment $ 9
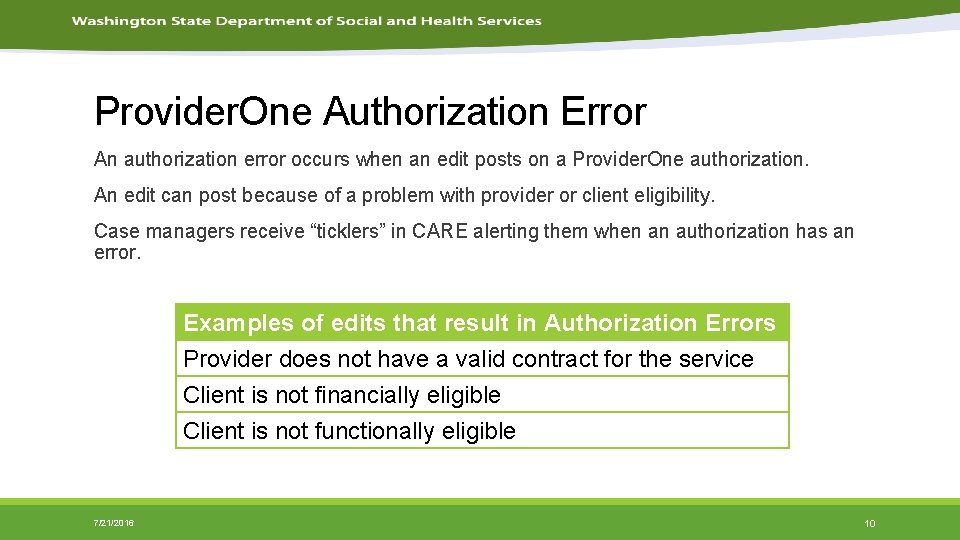
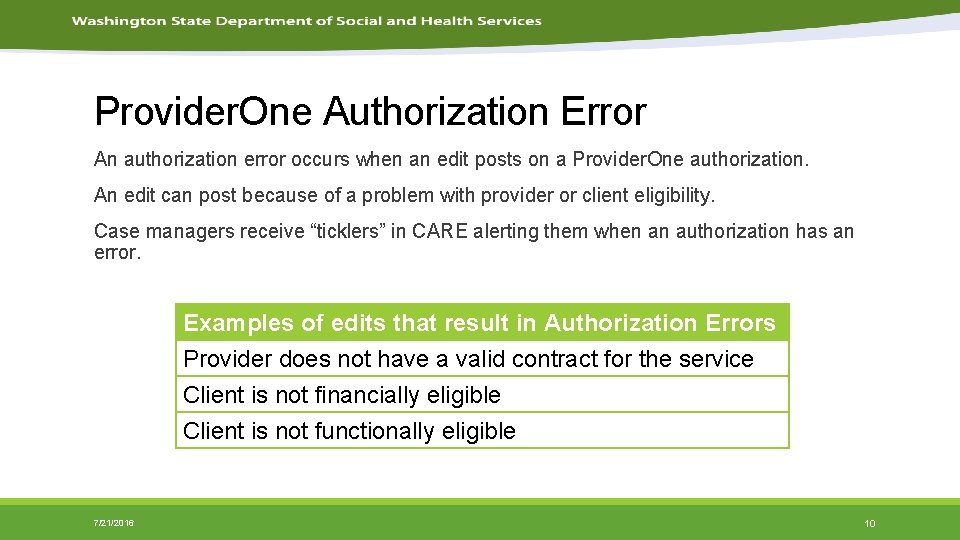
Provider. One Authorization Error An authorization error occurs when an edit posts on a Provider. One authorization. An edit can post because of a problem with provider or client eligibility. Case managers receive “ticklers” in CARE alerting them when an authorization has an error. Examples of edits that result in Authorization Errors Provider does not have a valid contract for the service Client is not financially eligible Client is not functionally eligible 7/21/2016 10
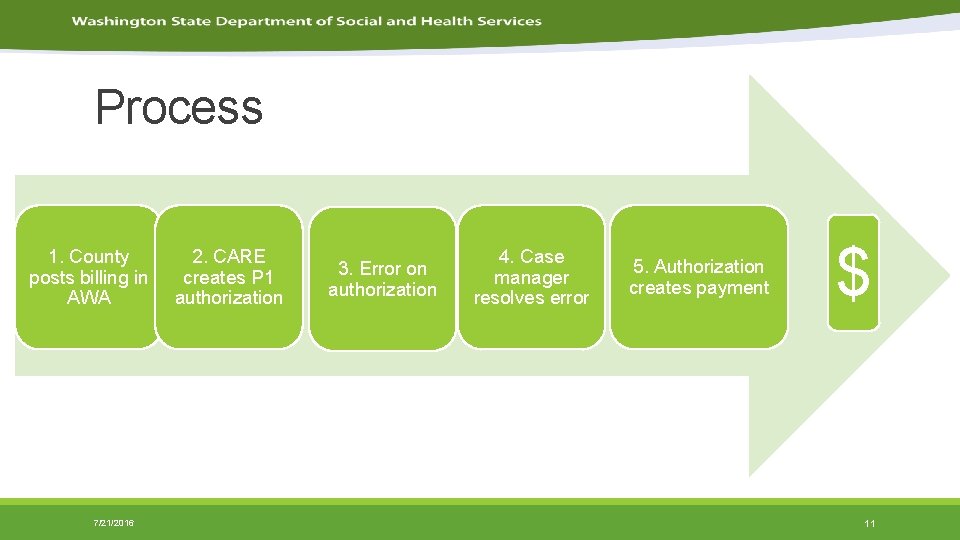
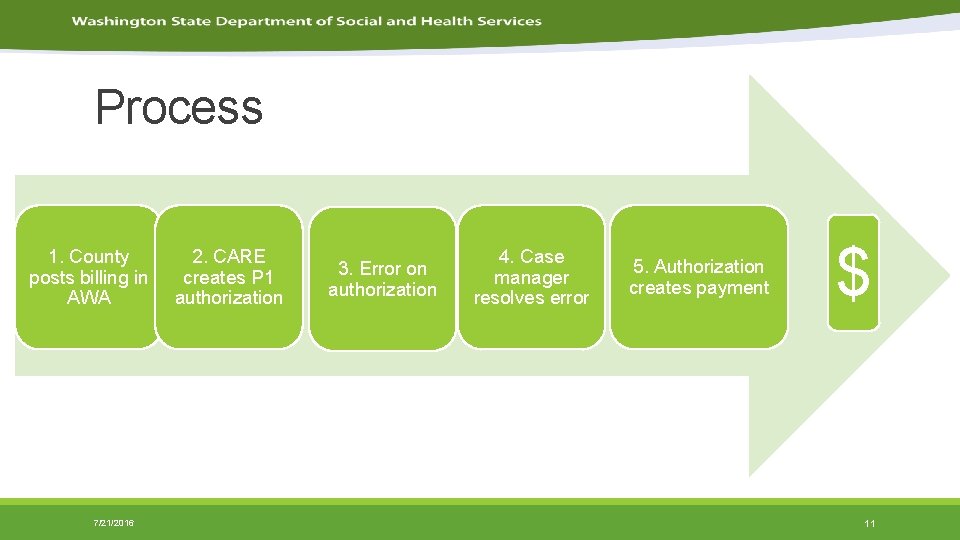
Process 1. County posts billing in AWA 7/21/2016 2. CARE creates P 1 authorization 3. Error on authorization 4. Case manager resolves error 5. Authorization creates payment $ 11

Case Manager Role • There is no change to the referral process or County Service Authorization process for the case manager. Most case managers will experience little impact from this change. • Case managers already resolve authorization errors for services billed through Provider. One. • Case managers will be informed of the payment of county services through Provider. One via a Management Bulletin. Case Managers: Attend to CSA and Referral process Attend to P 1 authorization ticklers Escalate authorization or payment issues to supervisor Escalate CSA or referral issues to supervisor 7/21/2016 12
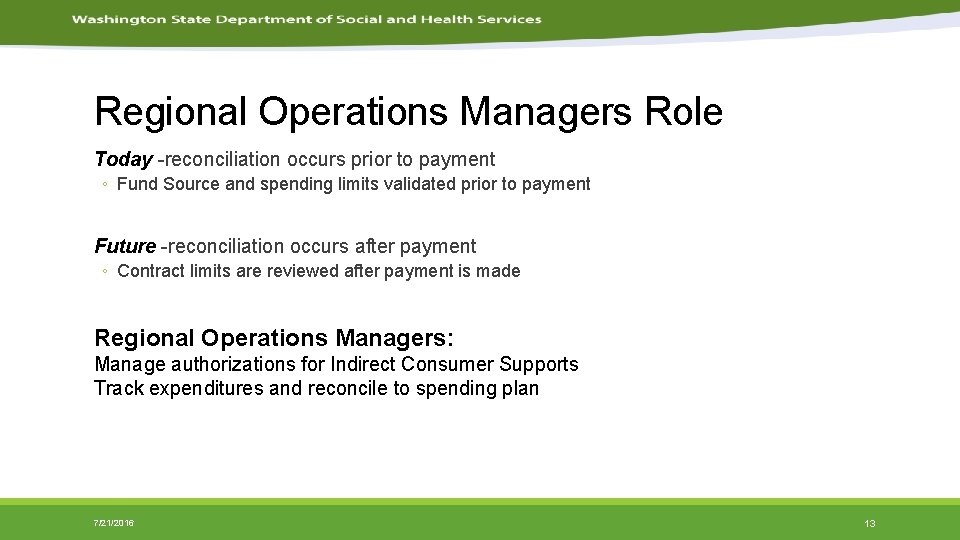
Regional Operations Managers Role Today -reconciliation occurs prior to payment ◦ Fund Source and spending limits validated prior to payment Future -reconciliation occurs after payment ◦ Contract limits are reviewed after payment is made Regional Operations Managers: Manage authorizations for Indirect Consumer Supports Track expenditures and reconcile to spending plan 7/21/2016 13
County Role • The Counties will still upload billing into AWA using the same process, but will now have access to the Provider. One system. • You can now log in to Provider. One to view billing information. County Role: Post billing in AWA Submit County Billing Summary and signed document to Regional Operations Manager Escalate Referral, CSA or P 1 authorization concerns to Case Manager Escalate Indirect Consumer P 1 authorization concerns to Regional Operations Managers 7/21/2016 14
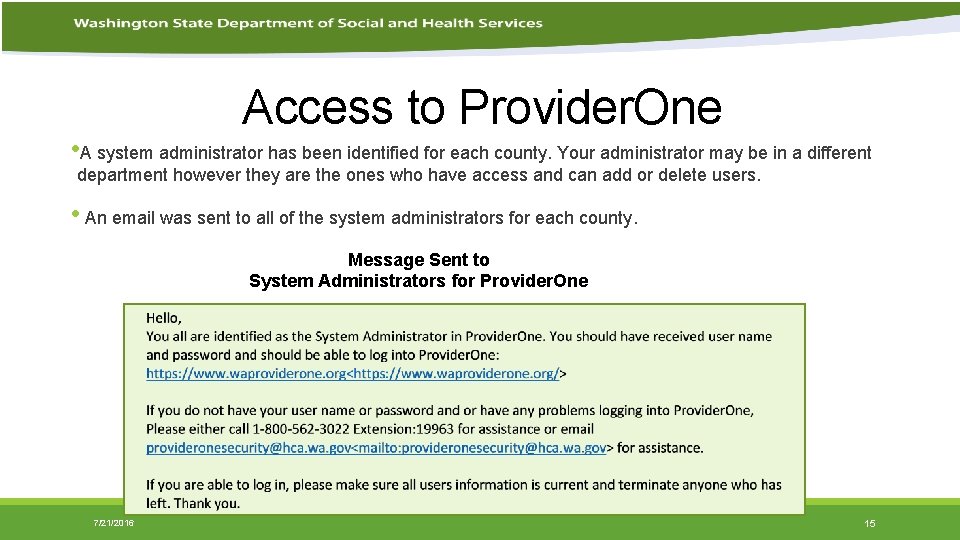
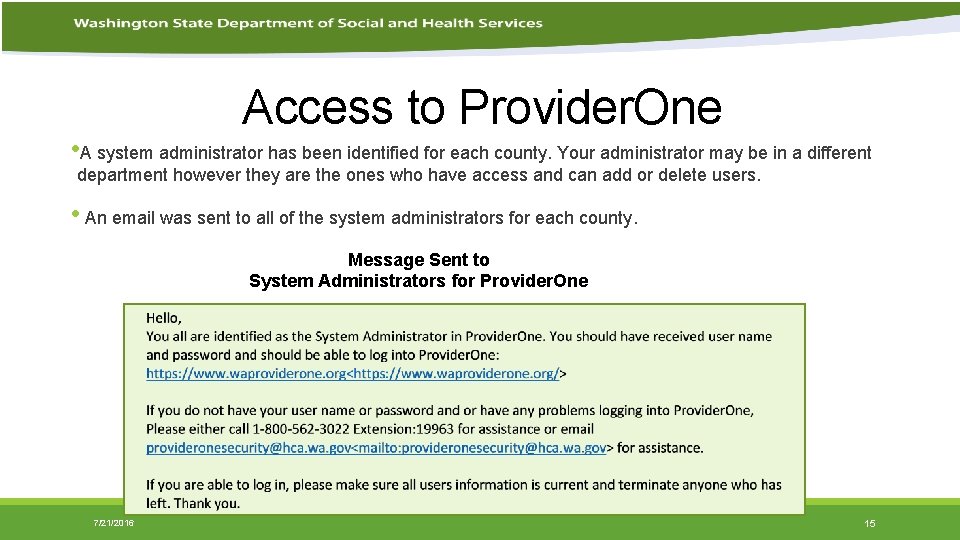
Access to Provider. One • A system administrator has been identified for each county. Your administrator may be in a different department however they are the ones who have access and can add or delete users. • An email was sent to all of the system administrators for each county. Message Sent to System Administrators for Provider. One 7/21/2016 15
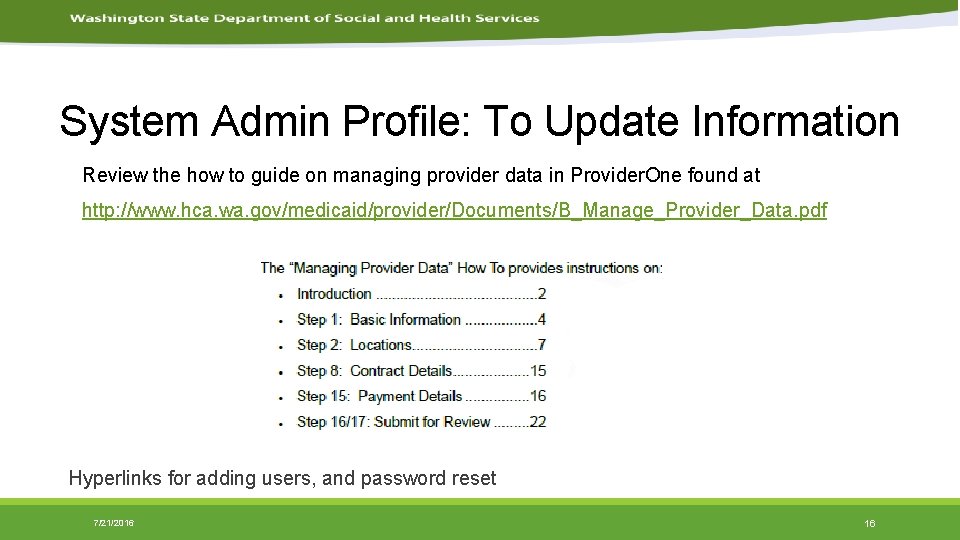
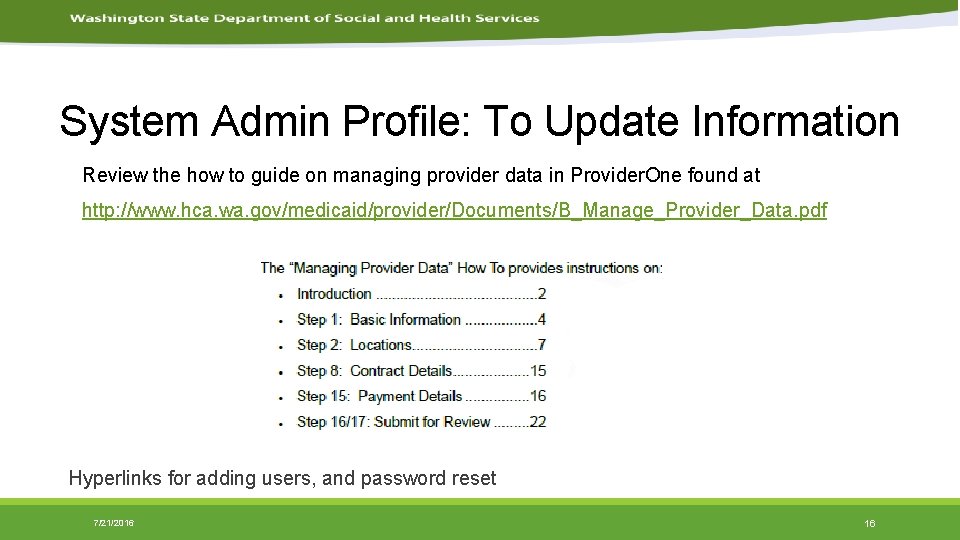
System Admin Profile: To Update Information Review the how to guide on managing provider data in Provider. One found at http: //www. hca. wa. gov/medicaid/provider/Documents/B_Manage_Provider_Data. pdf Hyperlinks for adding users, and password reset 7/21/2016 16

System Admin Profile: Another Resource to Update Info Another guide to review the how to guide on managing provider data in Provider. One found at http: //www. hca. wa. gov/medicaid/provider/documents/manual_maintaininguseraccounts. pdf 7/21/2016 17
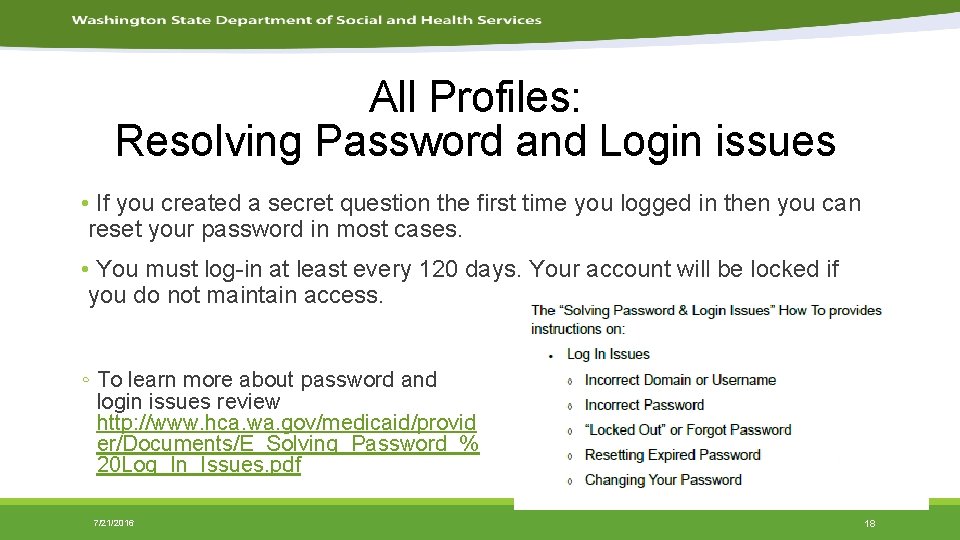
All Profiles: Resolving Password and Login issues • If you created a secret question the first time you logged in then you can reset your password in most cases. • You must log-in at least every 120 days. Your account will be locked if you do not maintain access. ◦ To learn more about password and login issues review http: //www. hca. wa. gov/medicaid/provid er/Documents/E_Solving_Password_% 20 Log_In_Issues. pdf 7/21/2016 18
EXT Provider Social Service Profile: The System Administrator can give themselves or others this profile. To see the Remittance Advice, claims or authorizations you need to be logged into Provider. One with the profile EXT Provider Social Service. * Logging in to Provider. One has benefits but it not necessary to receive payment for DDA Employment and Day services. 7/21/2016 19
EXT Provider Social Service Profile: View and Download the Remittance Advice (RA) In P 1, click on View Payment, and the RA payment list appears which shows the basic information for each RA. Each RA is based on a location. Once you click on the RA number the option to open the RA will be available. 7/21/2016 20

Paid Amount Client Section Payment Date 7/21/2016 21

RA Code Explanation Section This area will explain the code, if one is displayed in the Claim Detail of the RA Claim Adjustment Reason and Remark Codes Claim Adjustment Reason Code Every claim that has gone through the adjudication process and has been finalized will have a Claim Adjustment Reason Code applied to the claim or to each line on a multi line claim. The Code may be an informational code or may be an encompassing denial code. Remittance Advice Remark Codes A claim/service denied with one of the encompassing Claim Adjustment Reason Codes will also contain a Remittance Advice Remark Code which helps explain the information that is lacking on the claim/service line. The codes will be located on the Remittance Advice at each line and also on the claim totals line in the two columns on the right side of the RA. 7/21/2016 22
EXT Provider Social Service Profile: View the status of a submitted claim In P 1 click on Social Service Claims Inquiry, (under the Social Services authorizations and billing menu) The search page will appear which allows you to search by TCN, Client ID and service period, or social service authorization and service period 7/21/2016 23
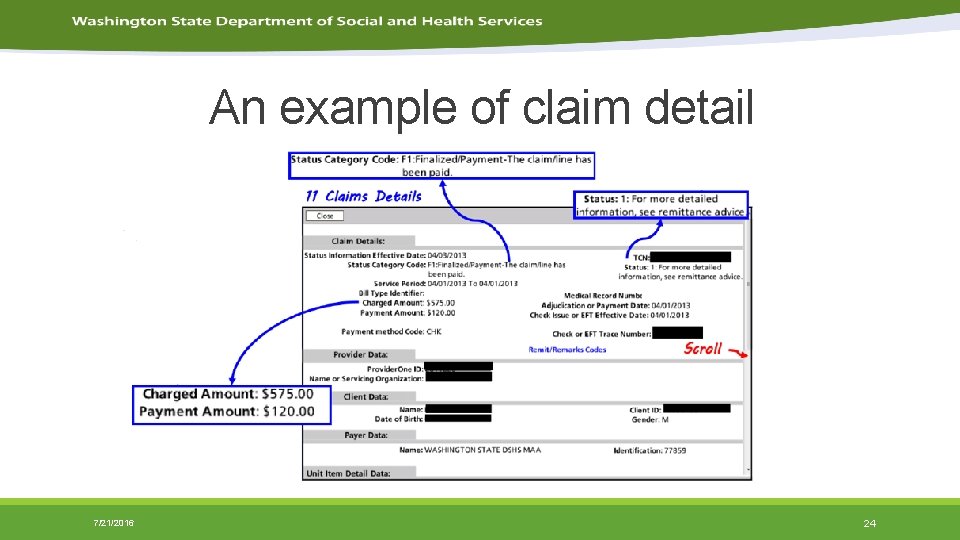
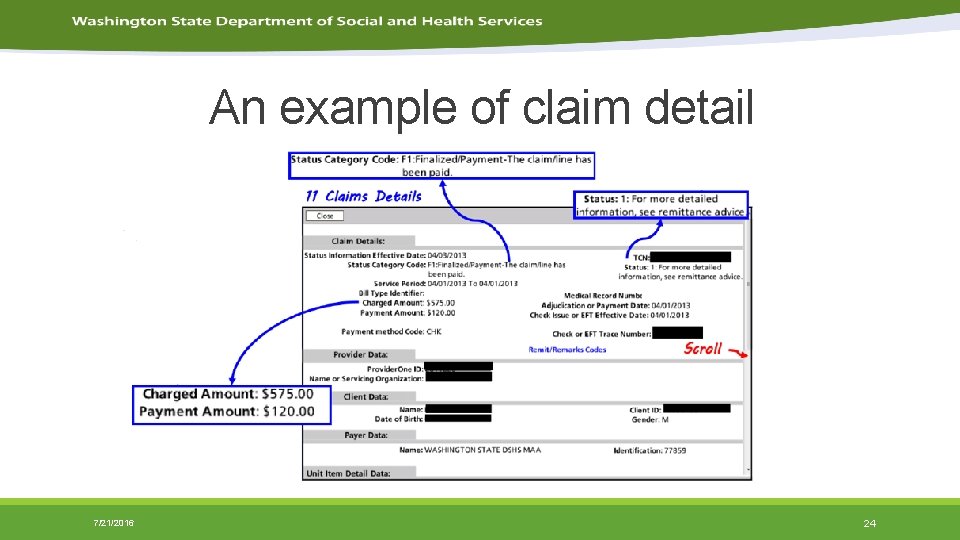
An example of claim detail 7/21/2016 24
New Reports • P 1_32092 DDA Employment and Day Services Billing Reconciliation Report • P 1_33810 DDA Employment and Day Services Billing Adjustment Report 7/21/2016 25
P 1_32092 DDA Employment and Day Services Billing Reconciliation Report Purpose of report: To identify the difference between what counties have billed and what P 1 has paid or denied, broken out by Account Title/Service, Program/RAC, and associated detail. There is a summary and a detailed report. Summary Report shows: • Amounts billed through ADSA Web Access (AWA) by RAC and Account Title/Service Code. • Amounts paid through Provider. One, and the difference between P 1 amount paid and AWA amount billed. Detail Report shows: • Amounts authorized and paid by client identifier, authorization number, and different claims statuses. 7/21/2016 26
P 1_33810 DDA Employment and Day Services Billing Adjustment Report Purpose of report: To identify AWA and Provider. One authorizations that do not match payments out of Provider. One. The report shows P 1 amounts authorized and paid, as well as configuration data attached to the client or provider such as RAC, Taxonomy, Service, and Rate. Report shows: Records with discrepancies between authorized and paid amounts. 7/21/2016 27
Additional Resources Learn more about Provider. One http: //www. hca. wa. gov/medicaid/provider/Pages/index. aspx Links to Provider. One Documents/Training http: //www. hca. wa. gov/medicaid/provider/pages/provideronemanuals. aspx http: //www. hca. wa. gov/medicaid/provider/pages/training. aspx Provider. One Login Access https: //www. waproviderone. org/ 7/21/2016 28
Getting Help Direct Service CSA or Provider. One Authorizations- Case Manager Indirect Consumer Supports- Regional Operations Manager AWA billing issues- Employment Specialist AWA technical support- ADSHELPDESK@dshs. wa. gov Provider. One Login, Security or help updating information https: //fortress. wa. gov/hca/p 1 contactus/SSProvider_Web. Form 7/21/2016 29

DDA Employment Specialists-Help with AWA Billing Issues Region 1 Carrie Bayha. CS@dshs. wa. gov 509. 374. 2128 Region 2 Rod Duncan Dunca. RA@dshs. wa. gov 425. 339. 4855 Region 3 Geoff Nisbet nisbeg@dshs. wa. gov 360. 725. 4304 7/21/2016 30
Webinar 1 August 16, 2016 10: 30 -12: 00 https: //attendee. gotowebinar. com/register/682605781905191938 ◦ Review previous training topics ◦ Ask questions of specialists from HCA and DSHS Webinar 2 August 31, 2016 1: 00 -2: 30 https: //attendee. gotowebinar. com/register/6525065325256080641 ◦ Review previous training topics ◦ Billing adjustments (Change in previously billed units or rate) Webinar 3 (same material as Webinar 2) September 20, 2016 1: 00 -2: 30 https: //attendee. gotowebinar. com/register/8206691394139951620 ◦ Review previous training topics ◦ Billing adjustments (Change in previously billed units or rate) July 2016 7/21/2016 31

Beth Krehbiel ◦ Beth. Krehbiel@dshs. wa. gov ◦ 360 -725 -3440 Peggy Dotson ◦ Peggy. Dotson@dshs. wa. gov ◦ 360 -725 -2541 Jennifer Popchockhakim ◦ Jennifer. Popchockhakim@dshs. wa. gov ◦ 360 -725 -3275 July 2016 7/21/2016 32