Gloucestershire Patient Participation Group PPG Network 22 January






- Slides: 35
Gloucestershire Patient Participation Group (PPG) Network 22 January 2016


About today / Agenda An opportunity to hear more about : q. GCCG’s approach to engagement and patient experience q. PPG Case Study q. Future Plans q. Primary care strategy q. Primary care premises …and to network with other PPGs, GCCG Lay Workers, Healthwatch and PALS.
The CCG’s approach to engagement and experience Becky Parish Associate Director Engagement and Experience GCCG
A few quick introductions… Caroline Smith, GCCG Senior Manager, Engagement and Inclusion Rachel Price, GCCG PALS Advisor Sophie Ayre, Healthwatch Gloucestershire Sheila Dwyer-Richmond, GCCG Team Secretary
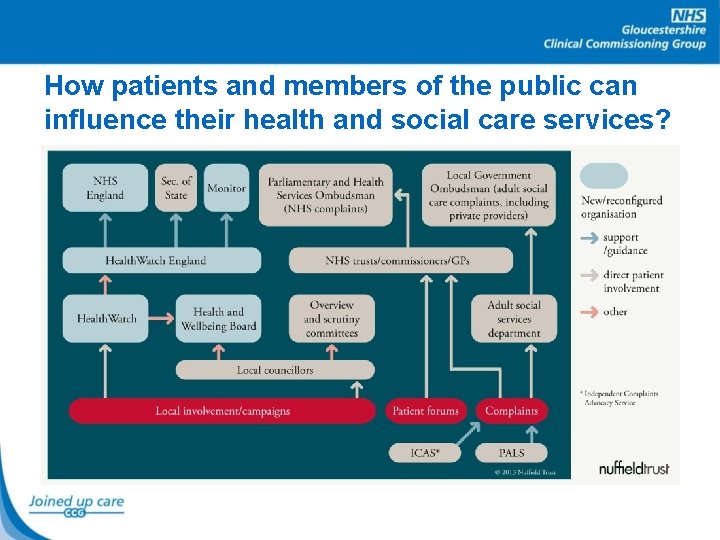
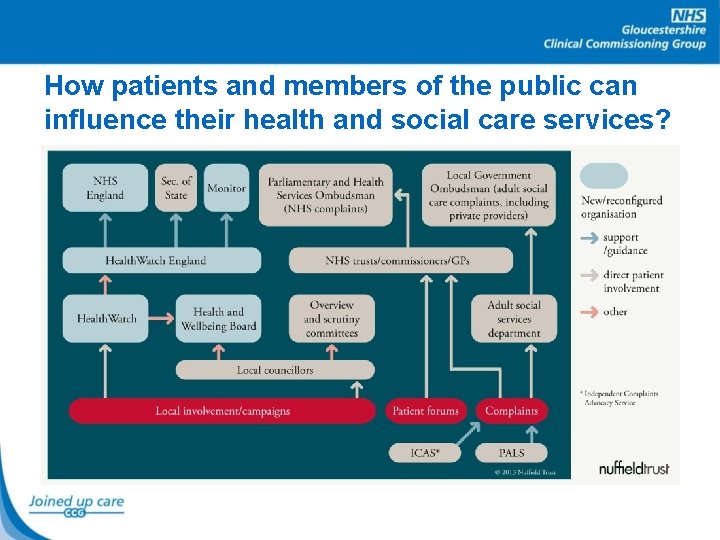
How patients and members of the public can influence their health and social care services?
Our Open Culture “We want to hear the ‘quiet voices’ and be ‘commissioners on the ground”.
What is ‘Our Open Culture’? The CCG’s aim is to makes effective engagement a reality and to ensure that the individual’s experience of care is a driver for quality and service improvement.

Why do we do it? • We have to do it: – S 14 Z 2 – Health and Social Care Act – NHS Constitution: Patient and Staff Rights and Responsibilities • We want to do it: – it ensures a better outcome for patients, their families and carers and staff satisfaction is improved!

Who do we do it with? • • People, Patients, Carers, our Staff Local Community/Voluntary Groups Healthwatch Gloucestershire Local stakeholders e. g. Health and Care Overview & Scrutiny Committee, MPs, District Councils • Border areas, county and country!
How can people get involved? People get involved in many ways: • Contact Patient Advice and Liaison Service (PALS) • Contribute to Clinical Programme Groups • Inform new service procurements e. g. Out of Hours Service • Join Locality Groups • Join Project Groups • Feedback on service change reviews such as Emergency Department changes – Surveys, visit the GCCG Information Bus, attend community events, follow us on twitter
PPGs From 1 April 2015 contractual requirement for all English practices to: • form a PPG • make reasonable efforts for this to be representative of the practice population • engage with the PPG including obtaining patient feedback and, where the practice and PPG agree, act on suggestions for improvement. Most practices in Gloucestershire have a PPG. It is expected for CQC inspection.
Examples of PPGs getting involved? • • • Procuring (buying) new services Closing a practice Promoting healthy lifestyles Reducing waste Influencing commissioning decisions PPG Blog
PPG Case Study Gill Cocks and Jan Knightly Winchcombe Medical Centre PPG

Events & Outreach Equipment & Facilities Teen health Privacy screen Diabetes TV monitor Women’s health Spirometer Carers ECG machine Men’s health Keeping out of A&E Advice Message in a bottle Surveys Outpatients Resusc. trolley Wheelchair
Looking Ahead Plans for the Future Ian Goodall, Associate Director of Operational Planning and PMO
Context for the 5 Year Forward View Much has improved over the last 20 years e. g. • More care in people’s own homes • More people spending less time in hospital e. g. after a hip replacement • Significant advances in treatment of illness and injury • People are living longer (success story!) and needing more health and care input than ever before Which means: • More people living with complex illnesses, long term conditions and disabilities • Increasing demand for services and public expectations
Why Change? • More funding is being put into the NHS (£ 3. 8 billion next year), but there is still an estimated £ 22 billion a year in savings that the NHS needs to find by 2020/2021 • As a system, the Gloucestershire Health Community will need to find efficiency savings of around £ 200 million over the same period • Need to continue to improve the quality of our health services
Comments from Engagement So Far • There should be a greater focus on prevention • Workforce issues are, or will be, a problem particularly in Primary Care • Better joint working between health and social care • More support should be given to patients, particularly those with long term conditions • More support for mental health services • Bigger role for pharmacies to give advice to patients • Better use of technology (e. g. telemedicine)
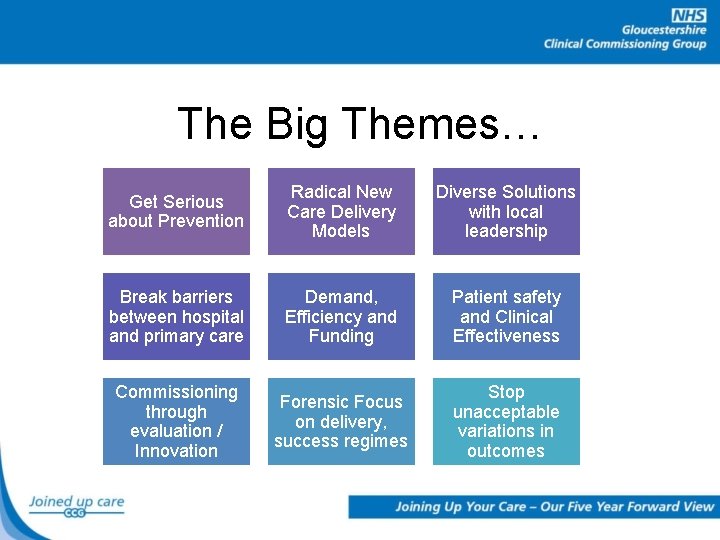
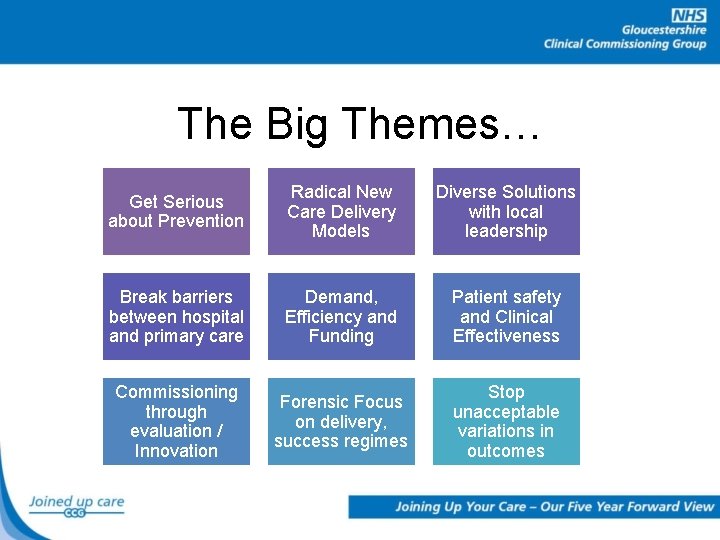
The Big Themes… Get Serious about Prevention Radical New Care Delivery Models Diverse Solutions with local leadership Break barriers between hospital and primary care Demand, Efficiency and Funding Patient safety and Clinical Effectiveness Commissioning through evaluation / Innovation Forensic Focus on delivery, success regimes Stop unacceptable variations in outcomes
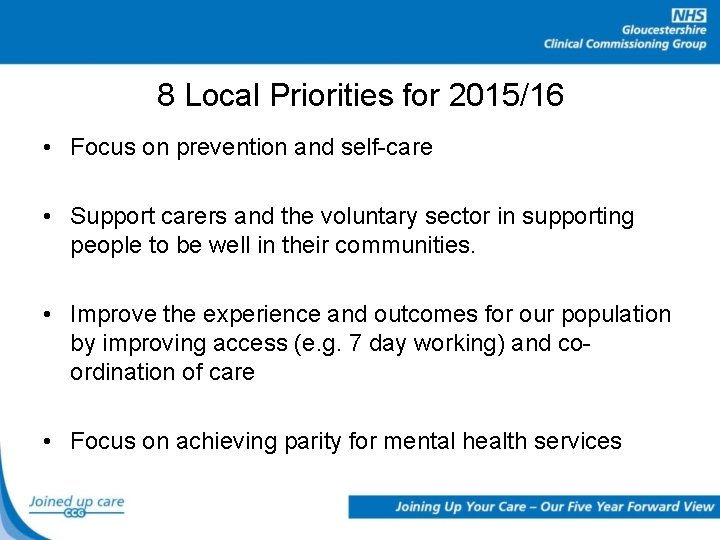
8 Local Priorities for 2015/16 • Focus on prevention and self-care • Support carers and the voluntary sector in supporting people to be well in their communities. • Improve the experience and outcomes for our population by improving access (e. g. 7 day working) and coordination of care • Focus on achieving parity for mental health services
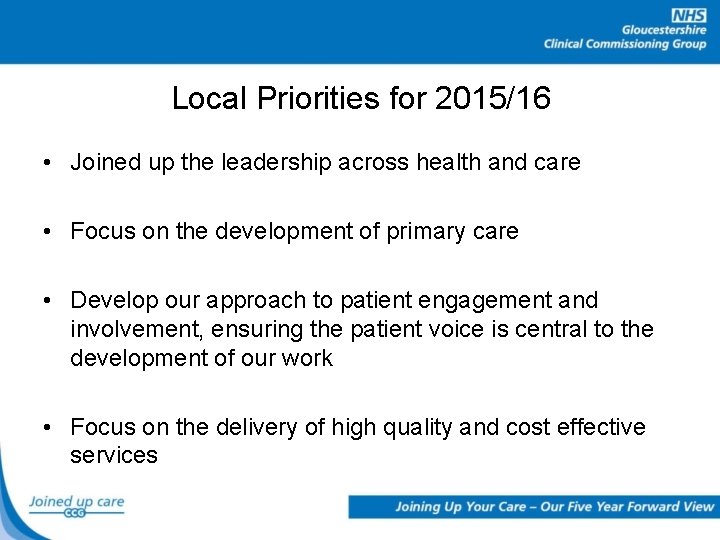
Local Priorities for 2015/16 • Joined up the leadership across health and care • Focus on the development of primary care • Develop our approach to patient engagement and involvement, ensuring the patient voice is central to the development of our work • Focus on the delivery of high quality and cost effective services
Primary Care Strategy Helen Goodey Director of Primary Care and Locality Development
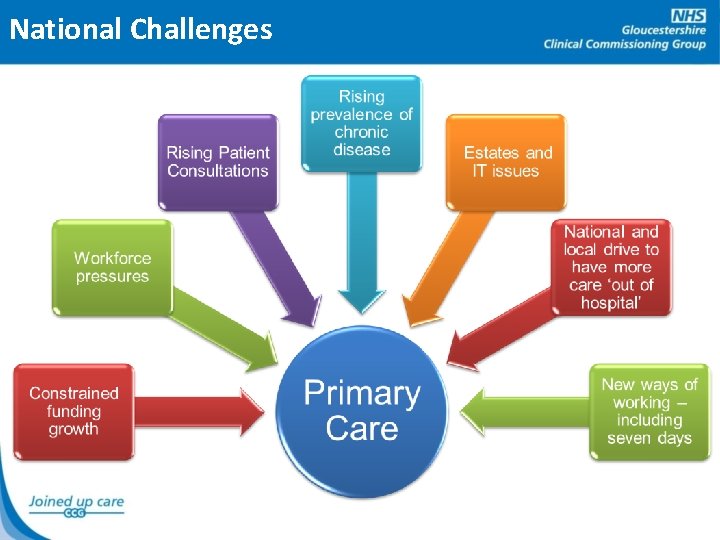
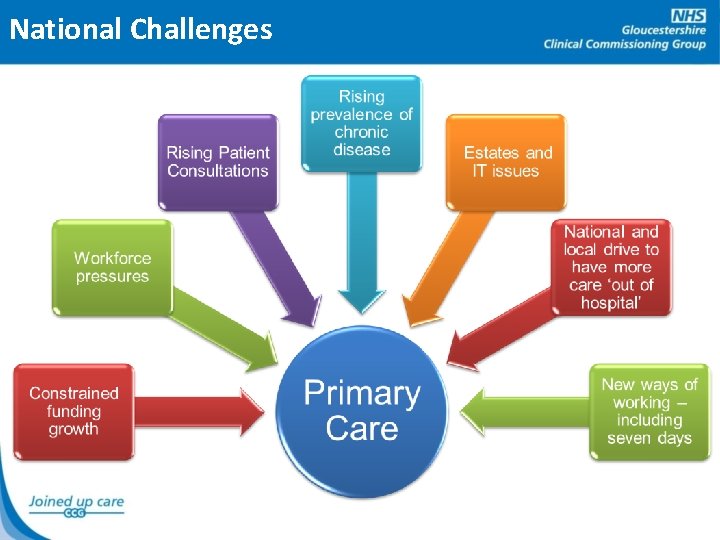
National Challenges
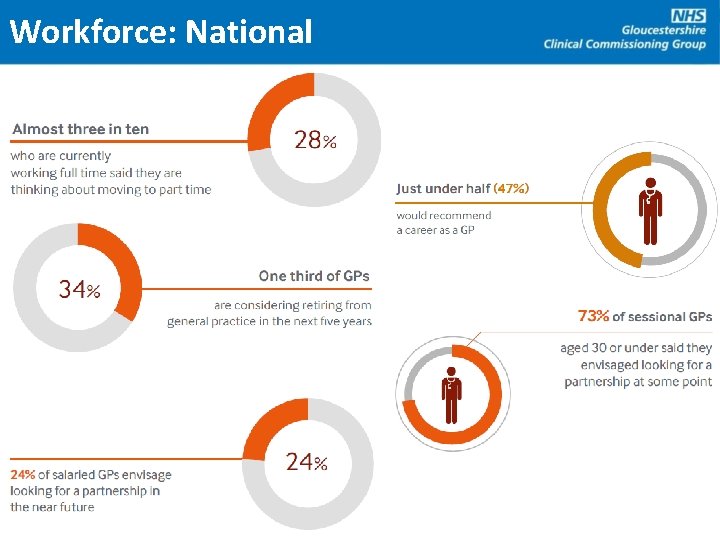
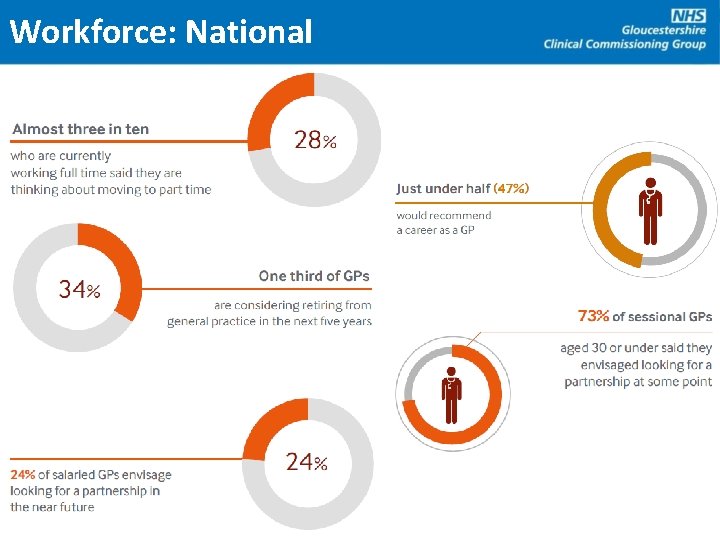
Workforce: National
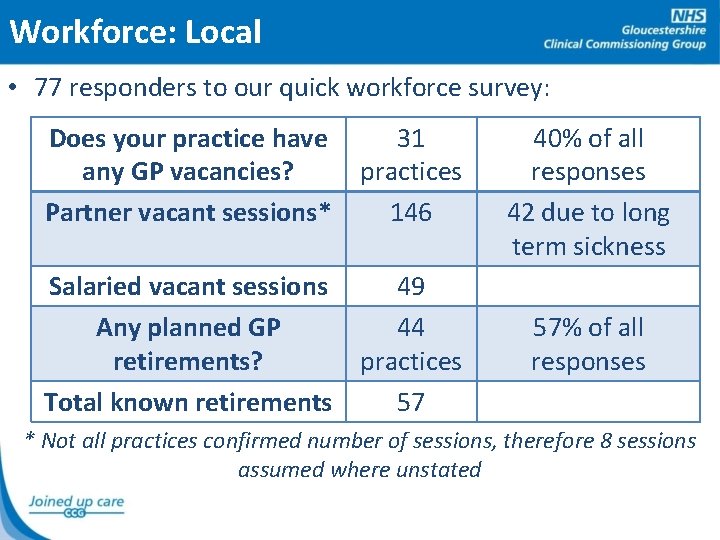
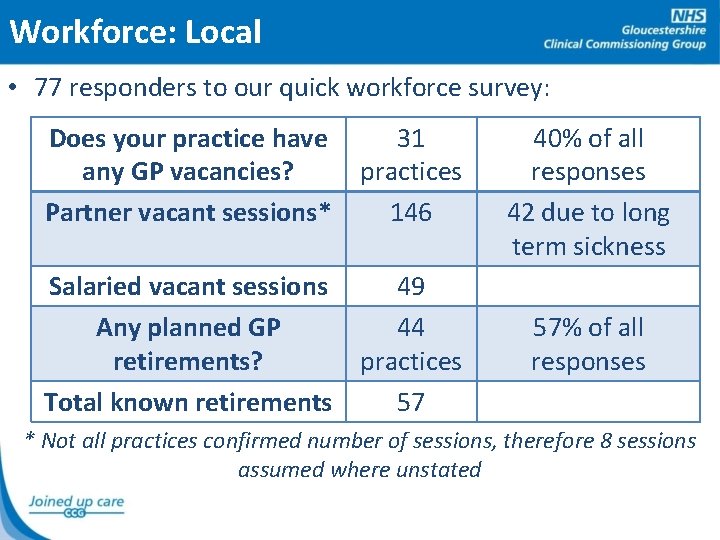
Workforce: Local • 77 responders to our quick workforce survey: Does your practice have any GP vacancies? Partner vacant sessions* 31 practices 146 Salaried vacant sessions 49 Any planned GP 44 retirements? practices Total known retirements 57 40% of all responses 42 due to long term sickness 57% of all responses * Not all practices confirmed number of sessions, therefore 8 sessions assumed where unstated
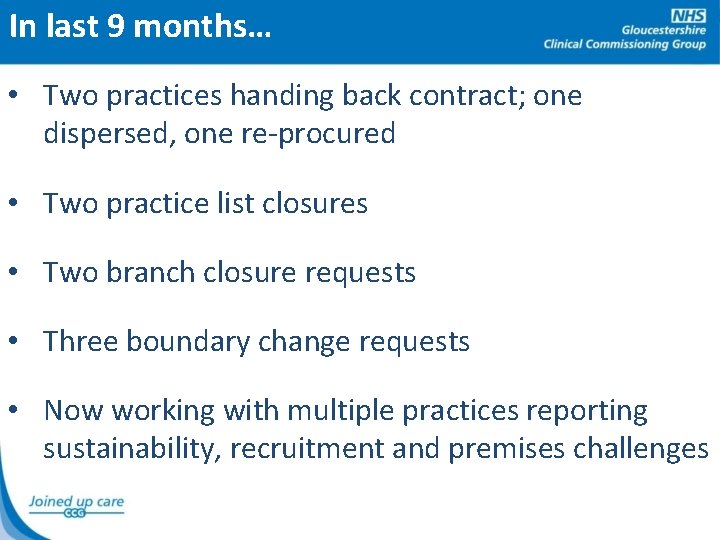
In last 9 months… • Two practices handing back contract; one dispersed, one re-procured • Two practice list closures • Two branch closure requests • Three boundary change requests • Now working with multiple practices reporting sustainability, recruitment and premises challenges
Question: Have you experienced pressures in Primary Care?
What are GCCG doing? • Project groups established (Estates, Workforce, Quality) • Additional investment: • More GP appointments January – March, weekdays and Saturdays • Focus on patients with respiratory conditions • Choice+ - additional on-the-day appointments • More practice nurse training • “GP retainers” and practice vacancy advertising • Equipment to enable practices to work remotely • Clinical Pharmacists in practice
Primary Care Strategy • Gloucestershire Primary Care Strategy: • Based on national, countywide, locality visions • Likely to mean “extended” primary care, i. e. more services available at or near your practice • Practices working together locally to perhaps deliver greater availability / accessibility • More integrated with other local services • Will incorporate Premises and Workforce strategies
A Vision for Working in Primary Care? “To be a resilient, vibrant and clinically effective Primary Care Service for Gloucestershire patients so they can stay well for longer, and receive out of hospital care wherever possible. To do this, we will offer a good work-life balance for us and our staff, reduce bureaucracy to focus on patient care, maintain and grow income sustainably, offer excellent training opportunities and attract and retain the best staff. ”
Short Break
Primary Care Infrastructure Andrew Hughes Locality Implementation Manager GCCG
Questions

 Gambar
Gambar Kevin buck change management
Kevin buck change management Umbraco training uk
Umbraco training uk Balingbing
Balingbing Inclusion gloucestershire
Inclusion gloucestershire Patient 2 patient
Patient 2 patient Modul ppg prakarya dan kewirausahaan
Modul ppg prakarya dan kewirausahaan Apa itu banpem ppg
Apa itu banpem ppg One ppg recognition & rewards
One ppg recognition & rewards Pcf to ppg conversion
Pcf to ppg conversion Slo and ppg examples
Slo and ppg examples Contoh rancangan karya
Contoh rancangan karya Suryanti unesa
Suryanti unesa Pengembangan perangkat pembelajaran daring ppg
Pengembangan perangkat pembelajaran daring ppg Resume orientasi ppg
Resume orientasi ppg Open space ppg
Open space ppg Ppg programme
Ppg programme Ppg adstock
Ppg adstock Ppgspada
Ppgspada Guru pamong ppg
Guru pamong ppg Gesundheit central european lung cancer patient ne
Gesundheit central european lung cancer patient ne Hm life insurance
Hm life insurance He was born in salzburg austria on january 27 1756
He was born in salzburg austria on january 27 1756 Zodiac for january 20
Zodiac for january 20 January 4, 1643
January 4, 1643 January february march season
January february march season January february maruary
January february maruary January 2006 chemistry regents answers
January 2006 chemistry regents answers Kent chemistry reference table
Kent chemistry reference table January 2012 chemistry regents answers
January 2012 chemistry regents answers January starts the year poem risa jordan
January starts the year poem risa jordan Ib physics hl grade boundaries
Ib physics hl grade boundaries Respect traits
Respect traits January 2006 calendar
January 2006 calendar January 27 1756
January 27 1756 When was mozart born and died
When was mozart born and died