Glenohumeral Dislocation Class Complications and Management August 21






- Slides: 40
Glenohumeral Dislocation: Class, Complications and Management August 21, 2003 Emergency XR Rounds Simon Pulfrey (with much gleaned from Dave Dyck)
Objectives • • Types of dislocations Review radiographic anatomy Types of radiographic views Key issues of physical exam Reduction strategies “Common” complications Pre and Post radiograph discussion Follow-up/discharge issues
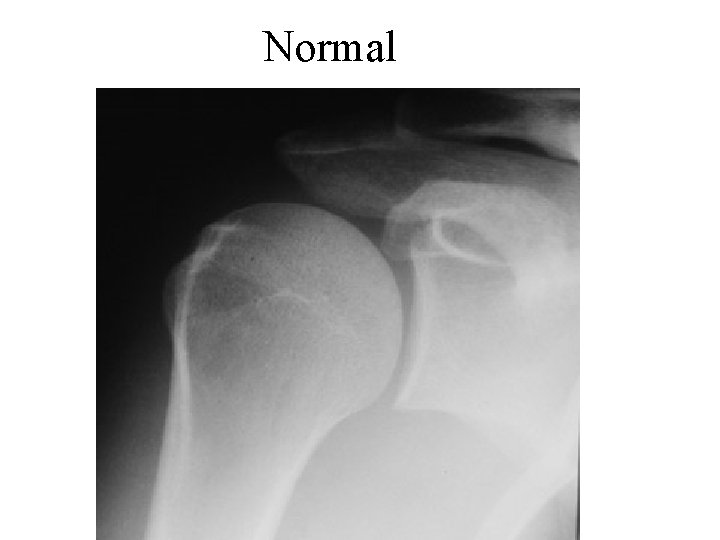
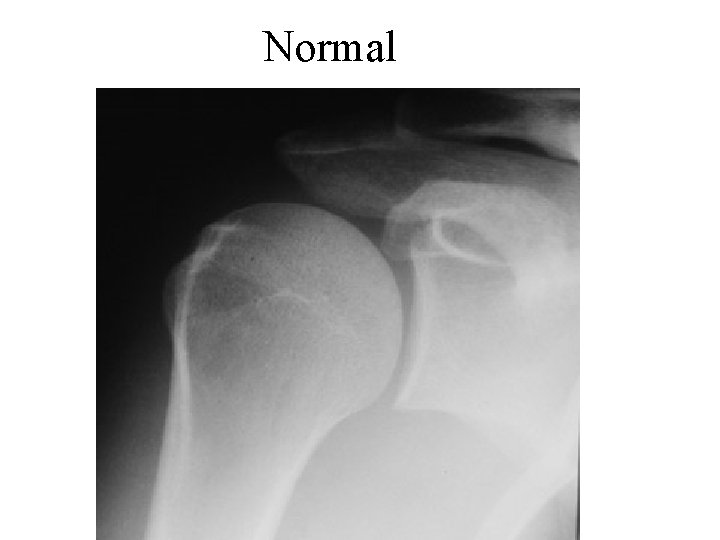
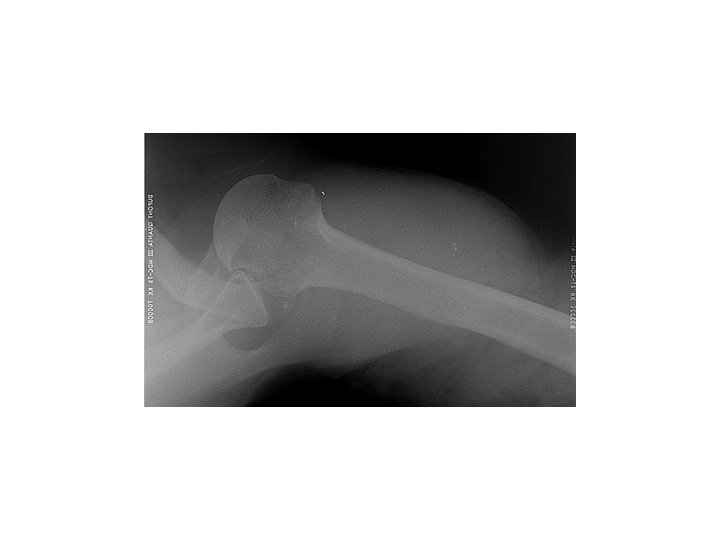
Normal
Glenohumeral Joint Dislocation • • Anterior Posterior Inferior (Luxatio Erecta) Superior
Anterior • Most common – 94 -97% of GH dislocation • 4 Types – Subcoracoid – Subglenoid – Subclavicular – Intrathoracic 99%
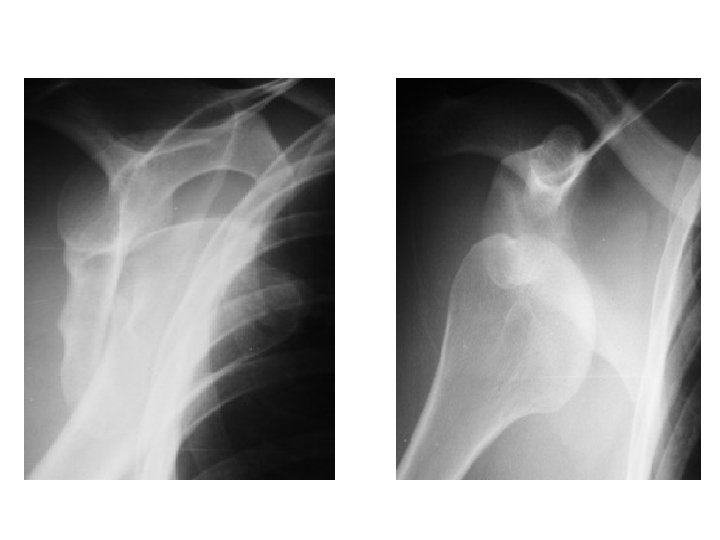
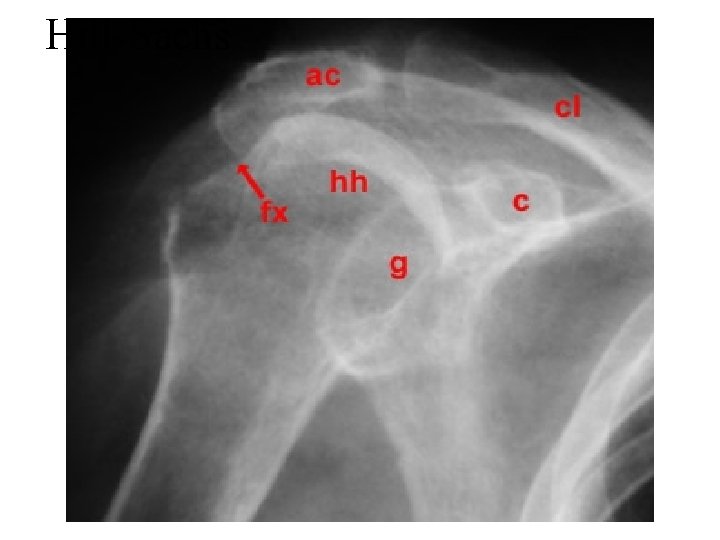
Case 1 • 29 y male, fell mountain biking - forced abduction injury to left arm, about 4 hours ago In severe pain. No prior injuries. • Holding arm in slight abduction and external rotation with right hand. • Refuses to adduct or internally rotate L arm. • L shoulder appears “squared-off”
What neurovascular exam will you do? • Neuro • Median, Ulnar, & Radial • Axillary N – Shoulder pin prick & deltoid motor activity – Injured in 5 -54% of cases – Usually >50 yrs • • Vascular Axillary Brachial Radial
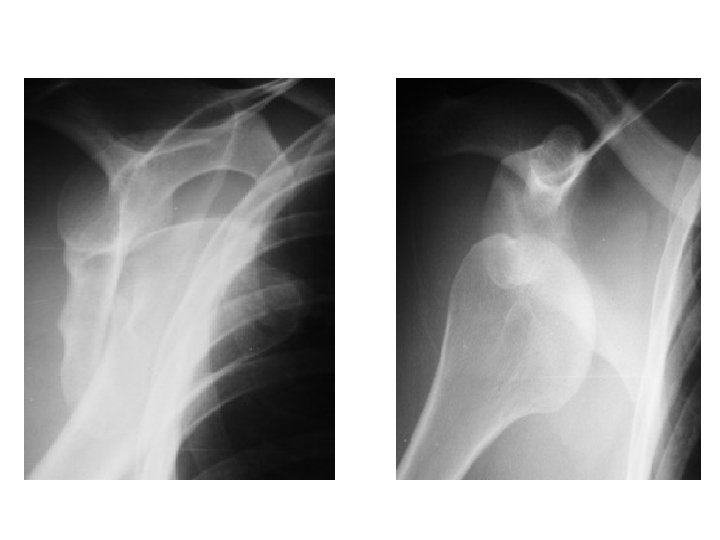
? Need for pre-reduction x-rays • Shuster, Abu-Laban, and Boyd – Banff say NO • BUT – most others say YES! • Maybe NO in patient with recurrent shoulder dislocation and non-traumatic mechanism. • Is there a fracture prior to reduction?
To classify glenohumeral dislocations • Mechanism – Traumatic vs Non-traumatic • Frequency – Primary vs Recurrent • Anatomic position of humeral head
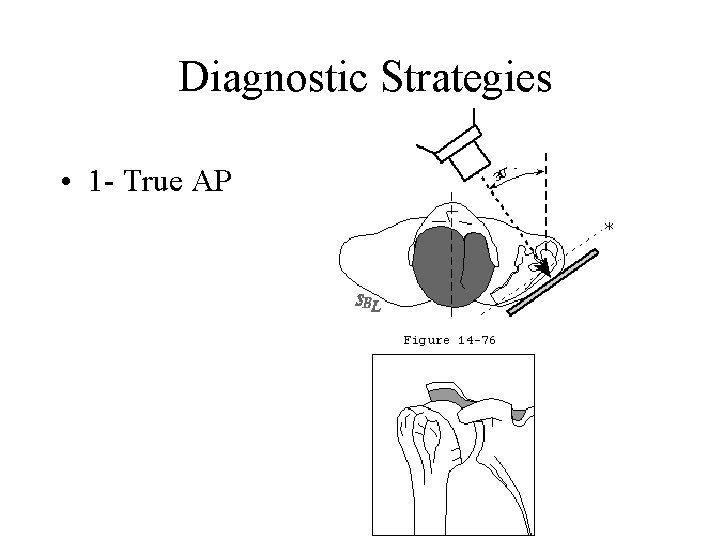
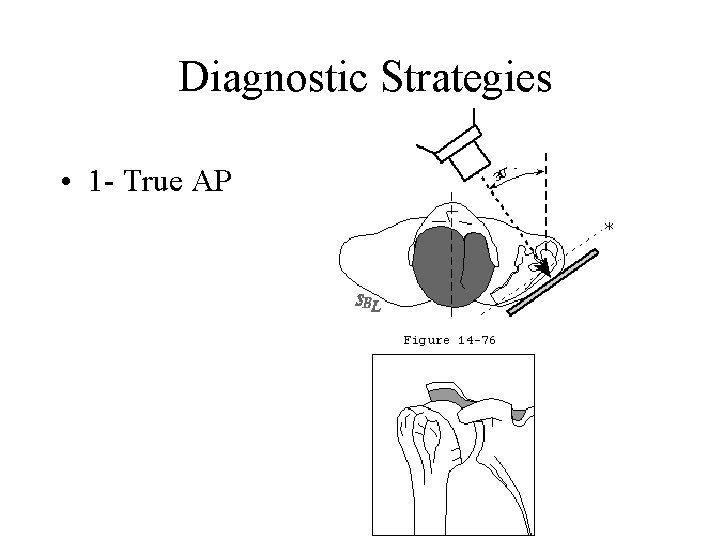
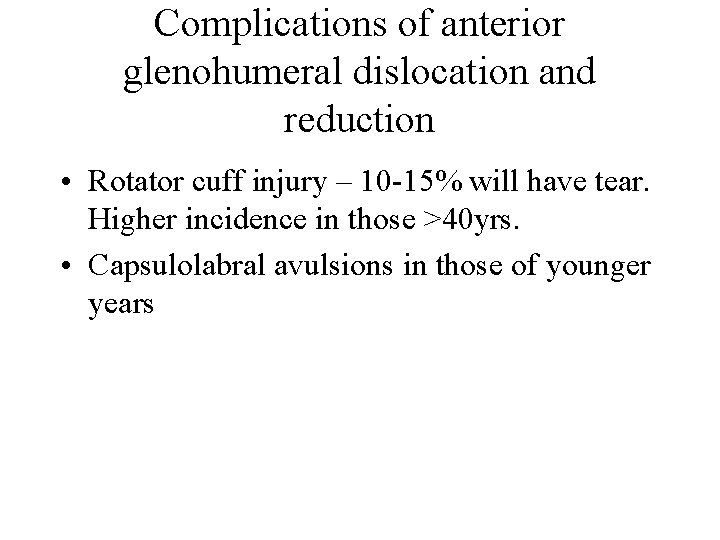
Diagnostic Strategies • 1 - True AP

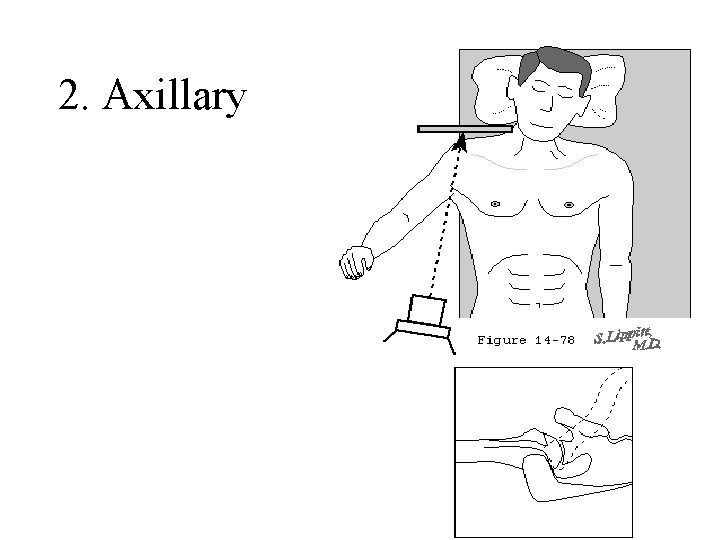
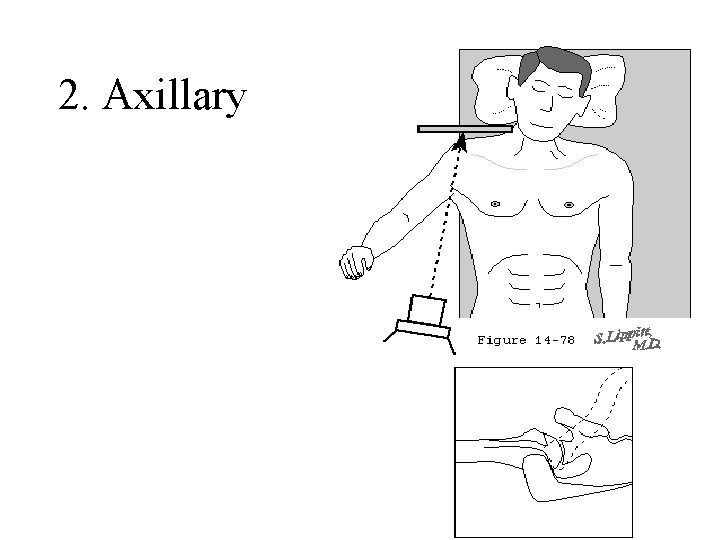
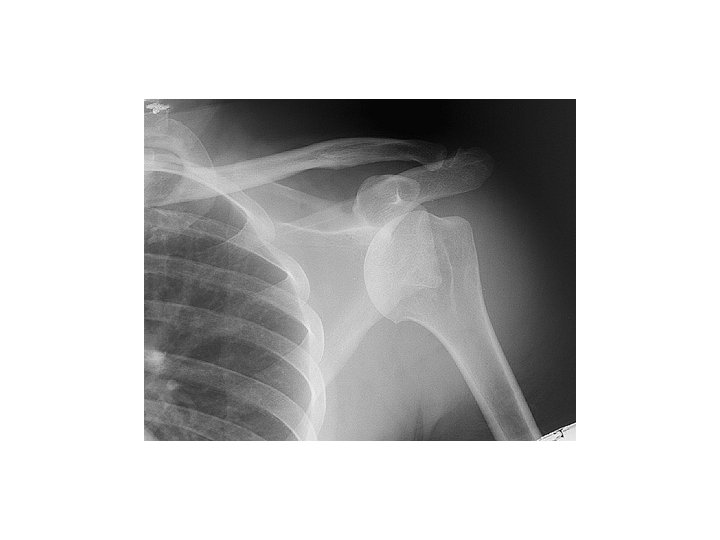
2. Axillary

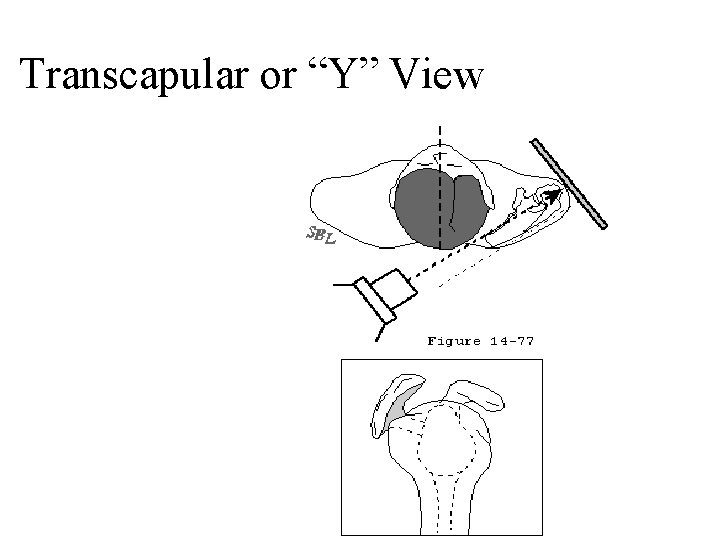
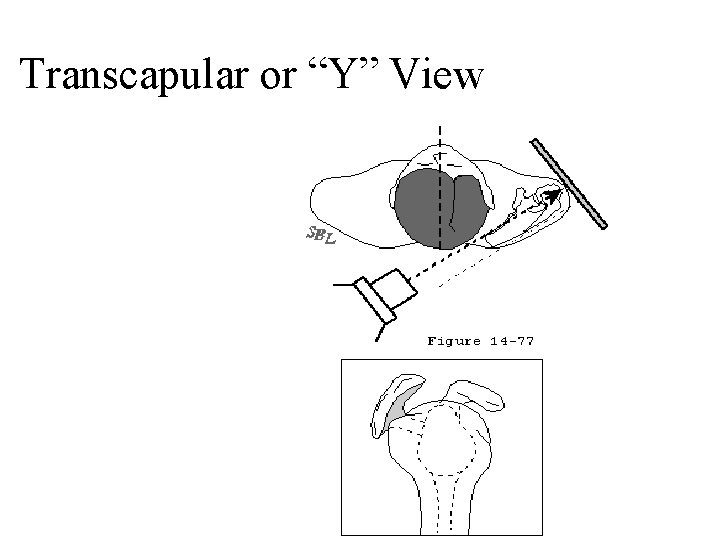
Transcapular or “Y” View

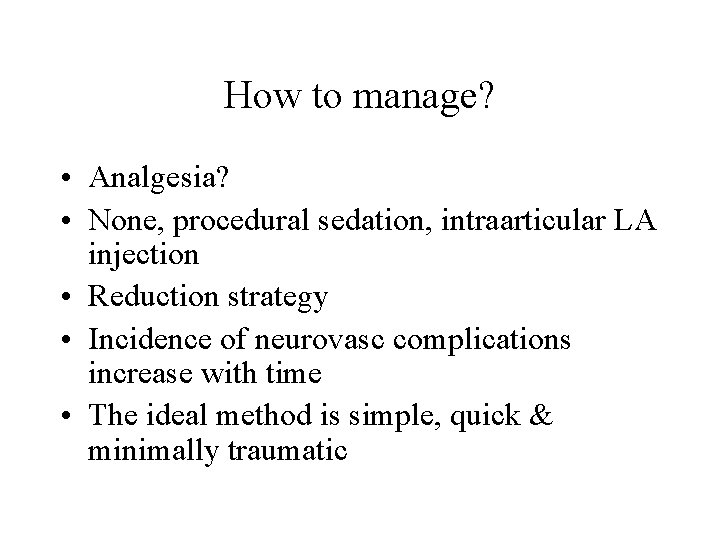
How to manage? • Analgesia? • None, procedural sedation, intraarticular LA injection • Reduction strategy • Incidence of neurovasc complications increase with time • The ideal method is simple, quick & minimally traumatic
Reduction methods • Stimson – Hanging weights. Not sedated. • Cooper&Miltch – forward elevation, flexion and abduction. • Traction-counter traction • Liedelmeyer – External rotation and abduction. • All have similar success rates • Hippocratic and Krocher are quite traumatic
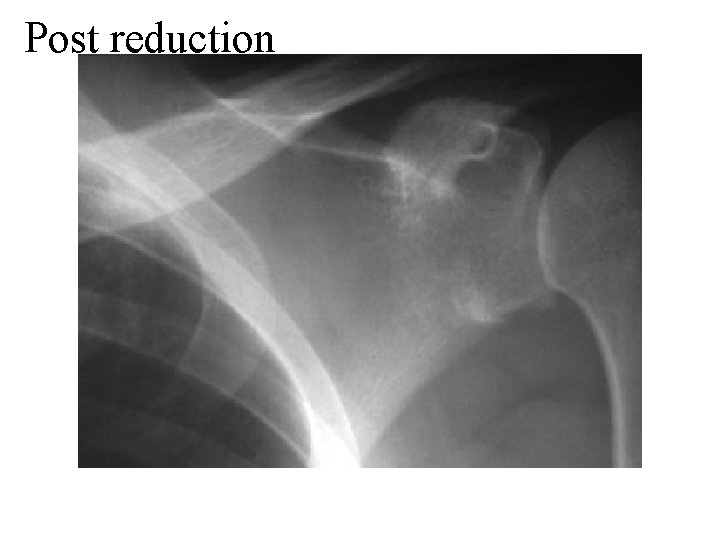
Post-Reduction Issues • Neurovascular status • Re-radiograph? – 2 small studies –Harvey et al Am J Emerg Med 1992, Hendey et al Am J Emerg Med, suggest maybe not. Rosen says do. • Need to consider every case – recurrent, trauma, age, difficulty with reduction, comorbidities… 1996

Post reduction:
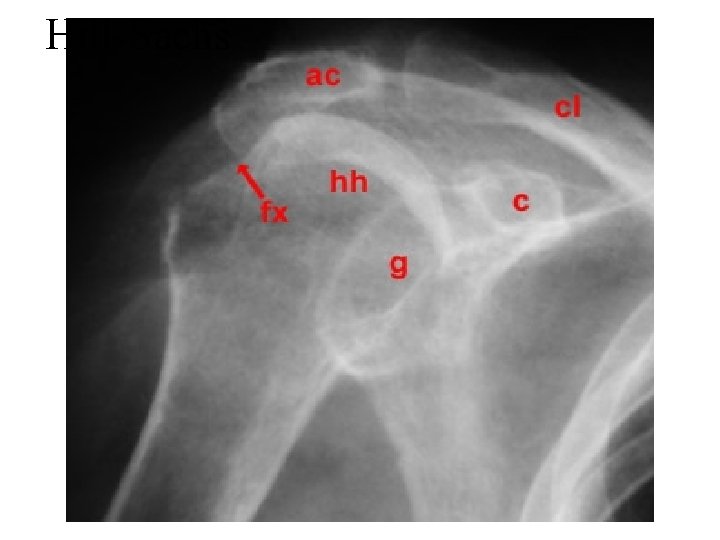
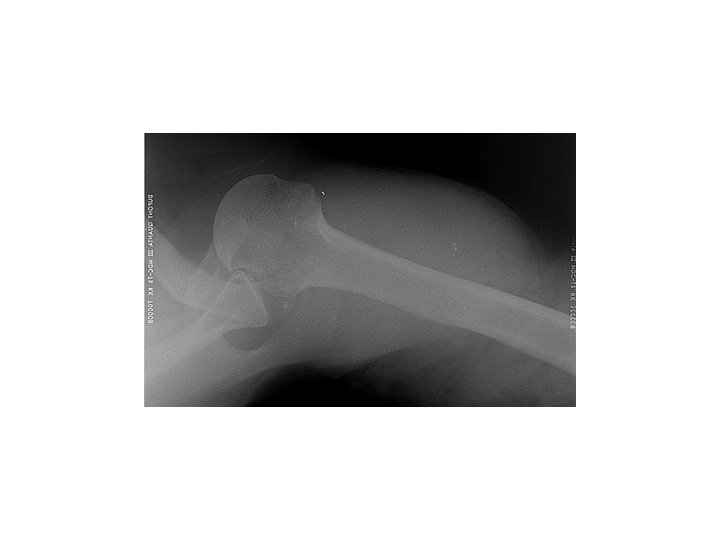
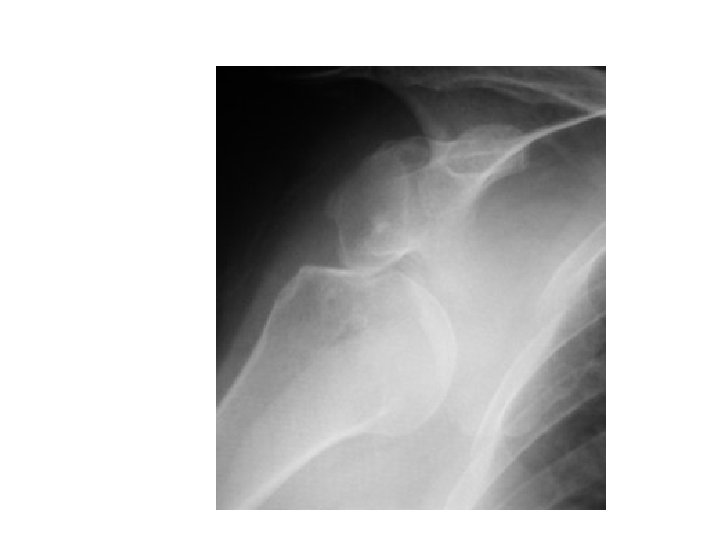
Hill-Sachs
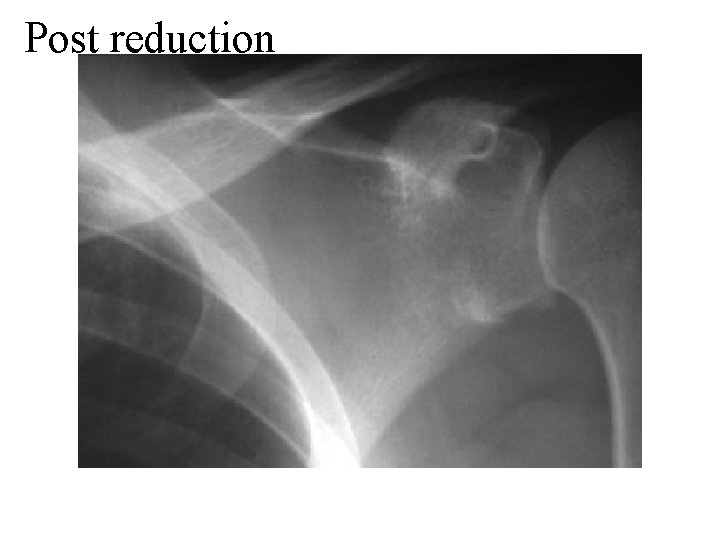
Post reduction
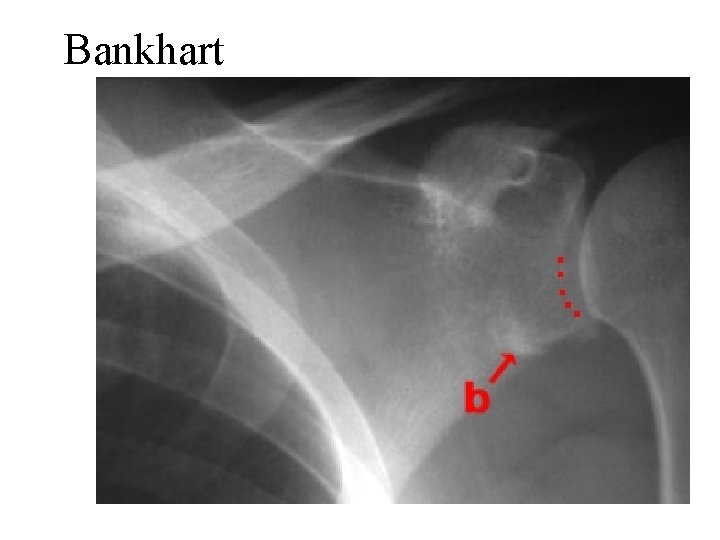
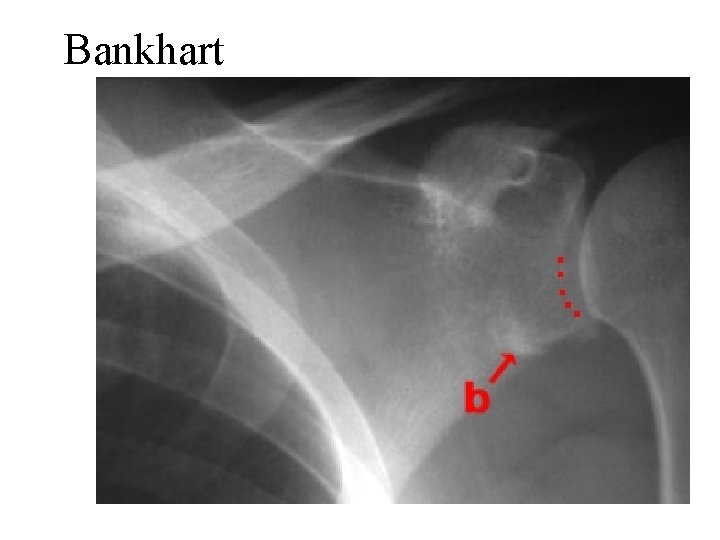
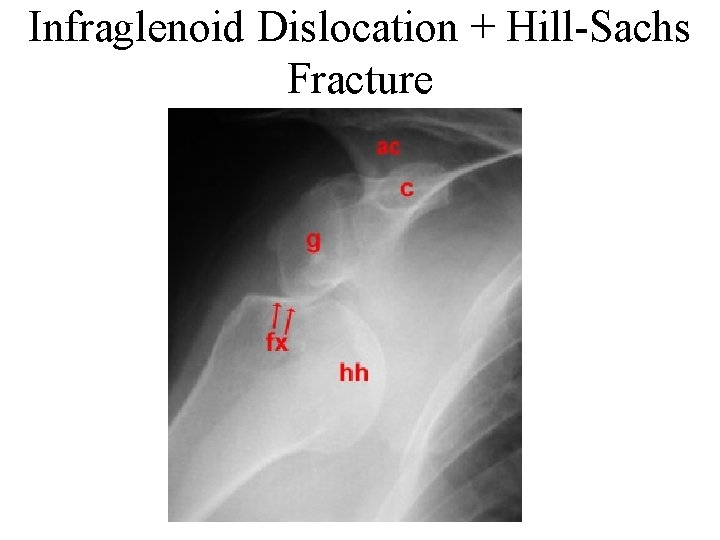
Bankhart
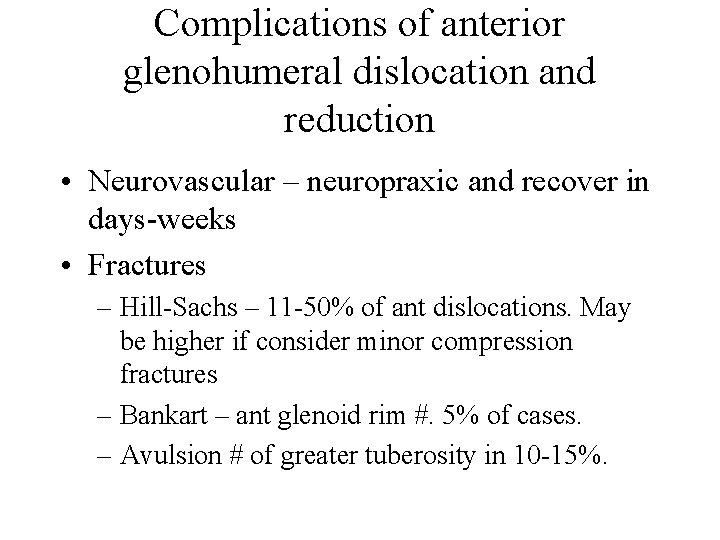
Complications of anterior glenohumeral dislocation and reduction • Neurovascular – neuropraxic and recover in days-weeks • Fractures – Hill-Sachs – 11 -50% of ant dislocations. May be higher if consider minor compression fractures – Bankart – ant glenoid rim #. 5% of cases. – Avulsion # of greater tuberosity in 10 -15%.
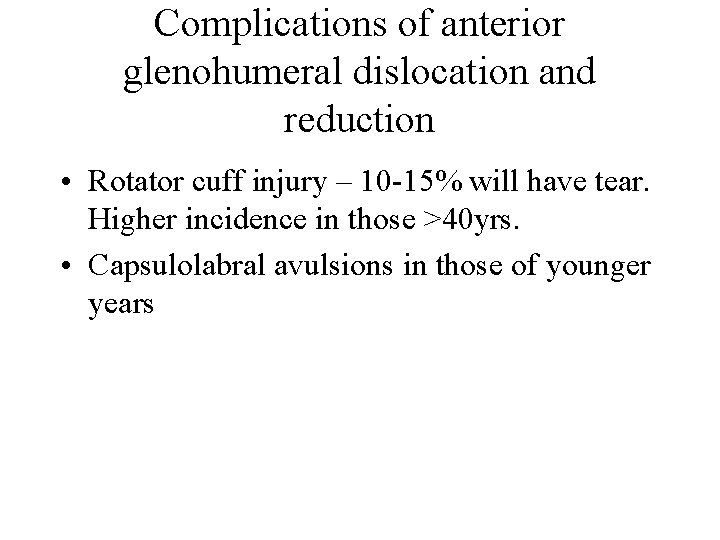
Complications of anterior glenohumeral dislocation and reduction • Rotator cuff injury – 10 -15% will have tear. Higher incidence in those >40 yrs. • Capsulolabral avulsions in those of younger years
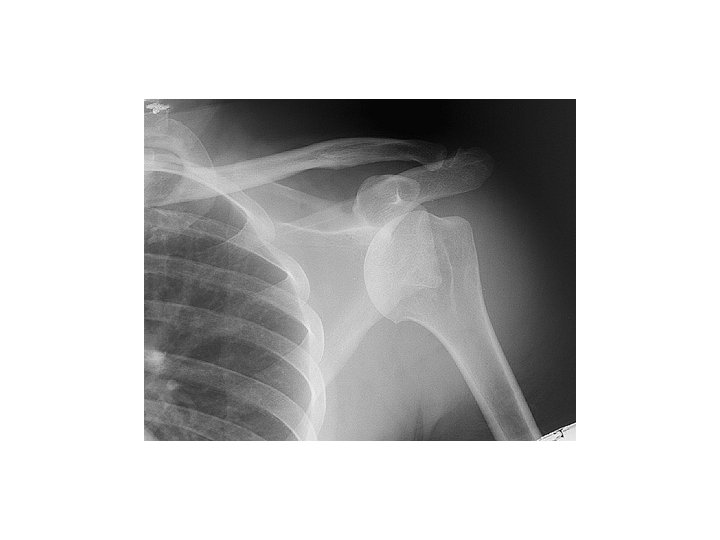
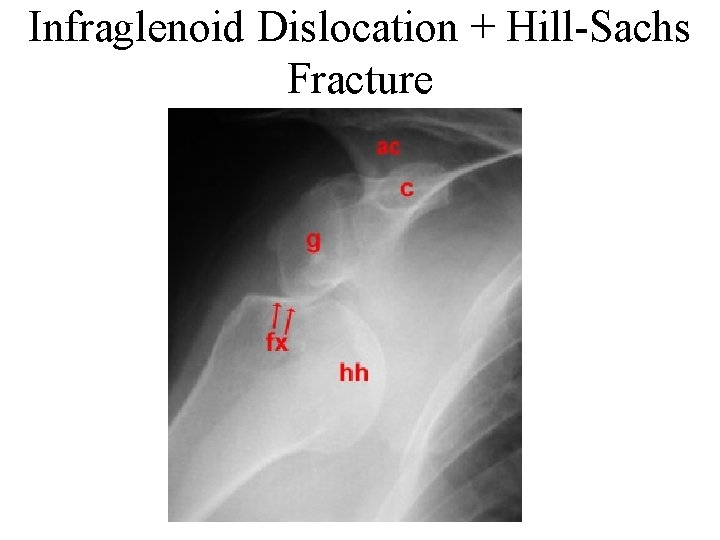
Infraglenoid Dislocation + Hill-Sachs Fracture
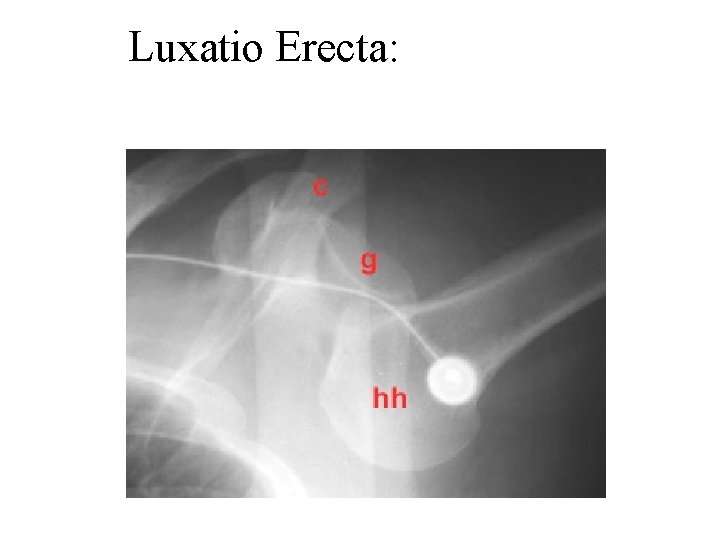
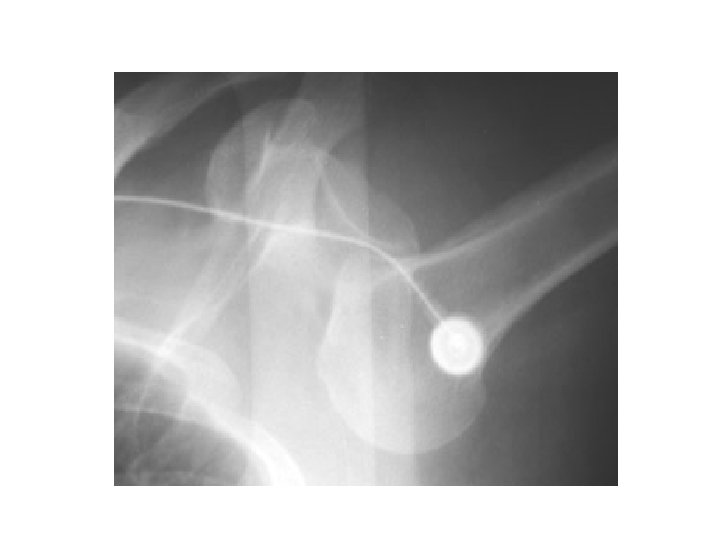
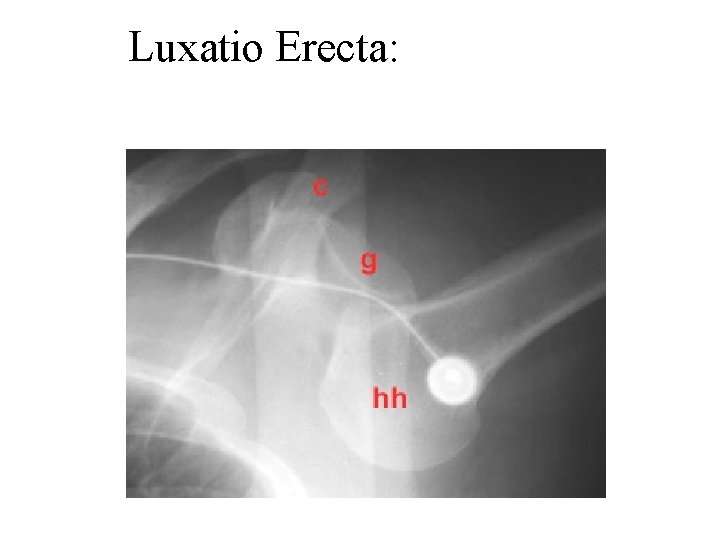
Luxatio Erecta:
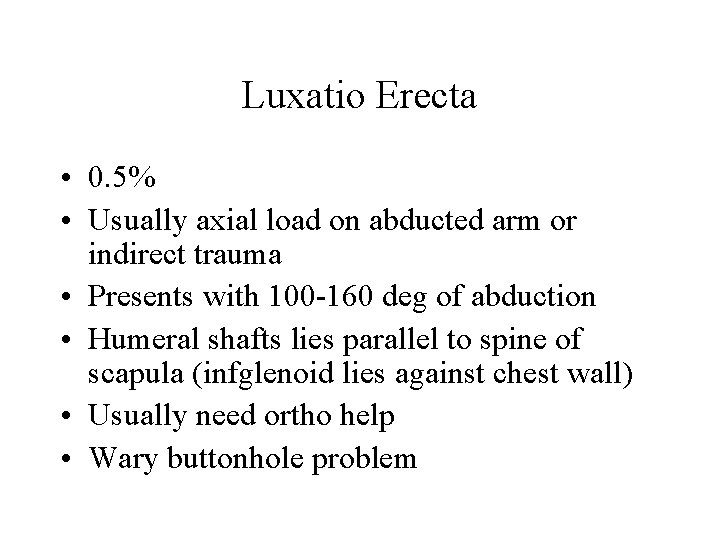
Luxatio Erecta • 0. 5% • Usually axial load on abducted arm or indirect trauma • Presents with 100 -160 deg of abduction • Humeral shafts lies parallel to spine of scapula (infglenoid lies against chest wall) • Usually need ortho help • Wary buttonhole problem

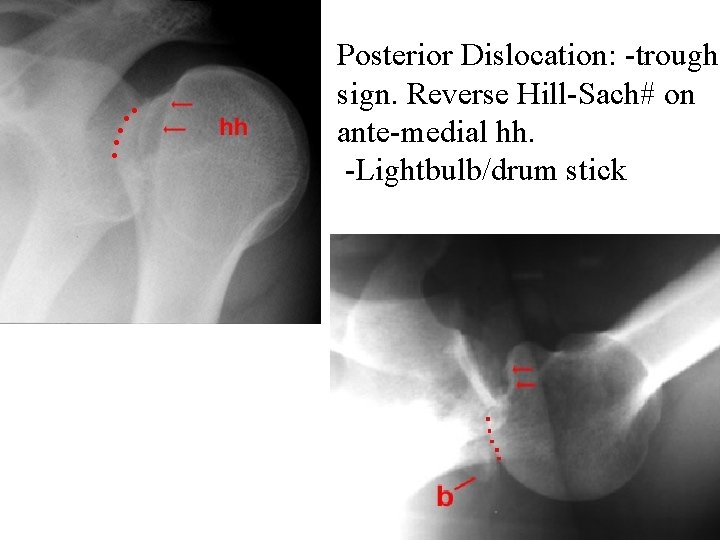
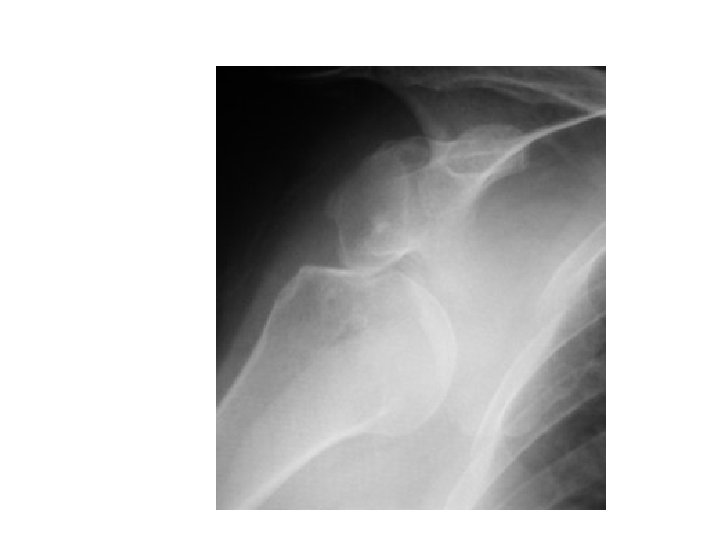
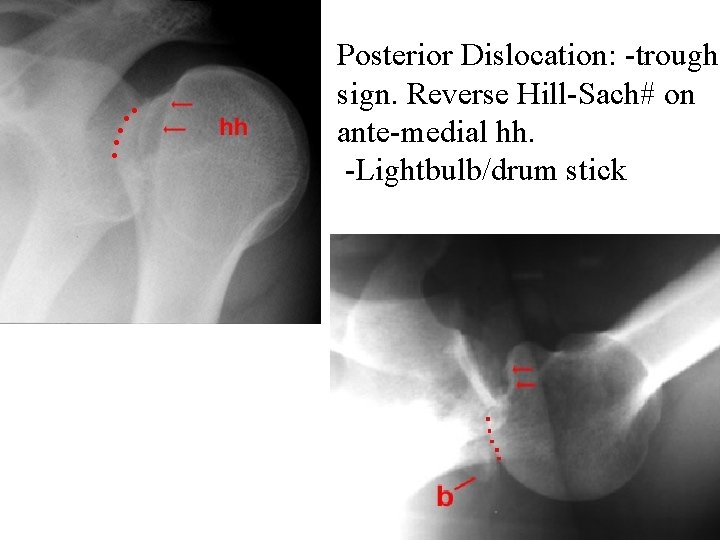
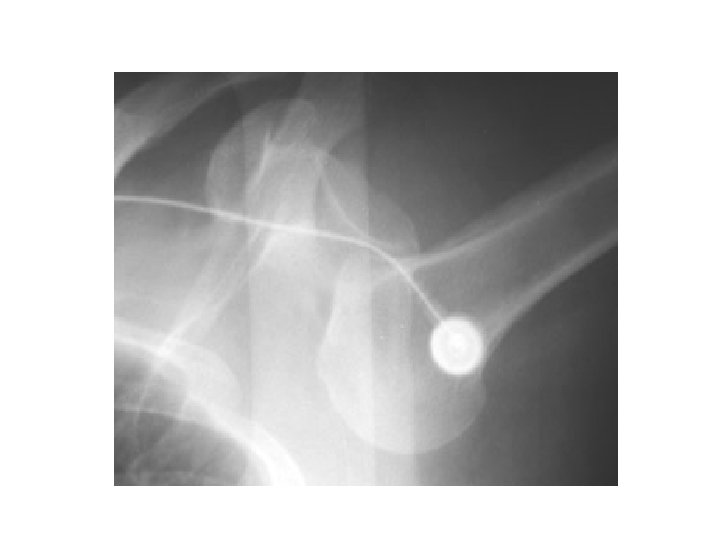
Posterior Dislocation: -trough sign. Reverse Hill-Sach# on ante-medial hh. -Lightbulb/drum stick
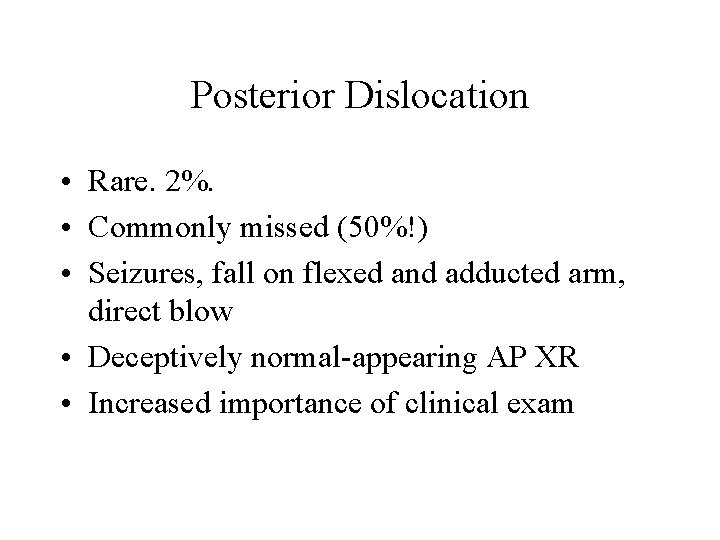
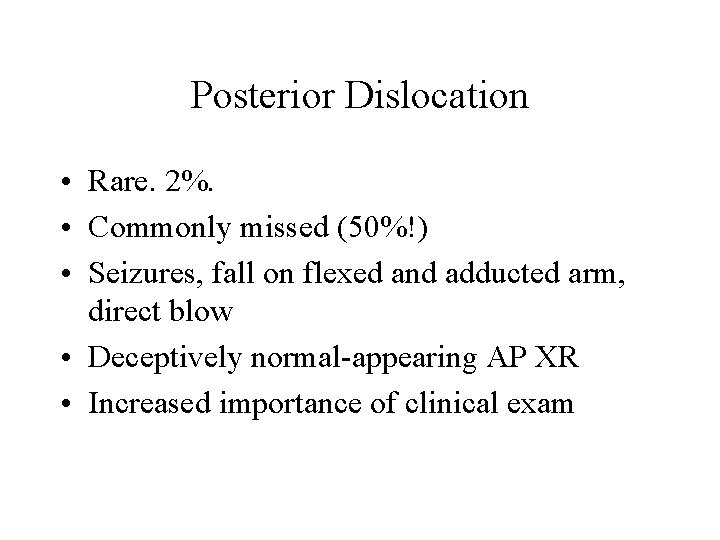
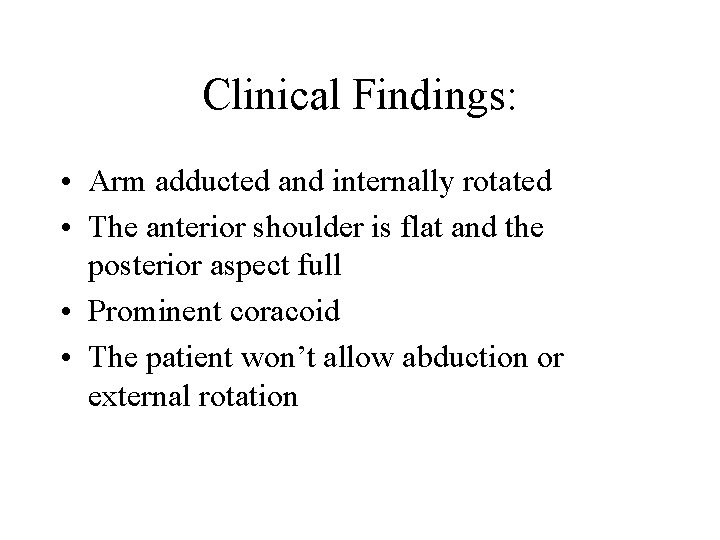
Posterior Dislocation • Rare. 2%. • Commonly missed (50%!) • Seizures, fall on flexed and adducted arm, direct blow • Deceptively normal-appearing AP XR • Increased importance of clinical exam
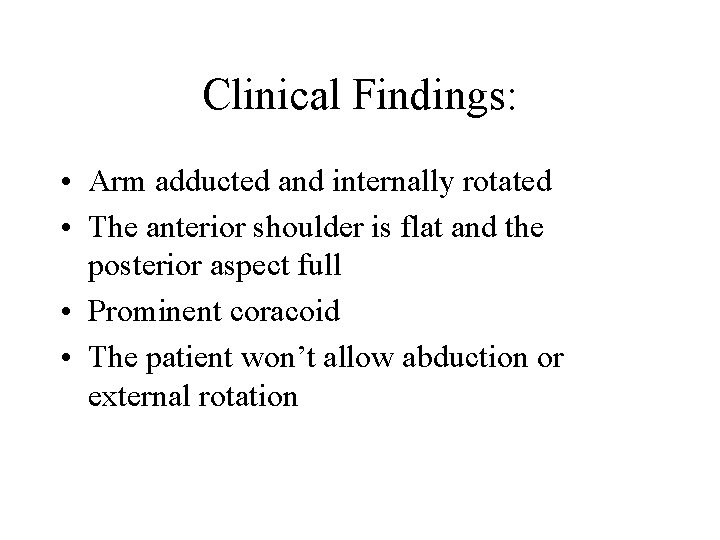
Clinical Findings: • Arm adducted and internally rotated • The anterior shoulder is flat and the posterior aspect full • Prominent coracoid • The patient won’t allow abduction or external rotation

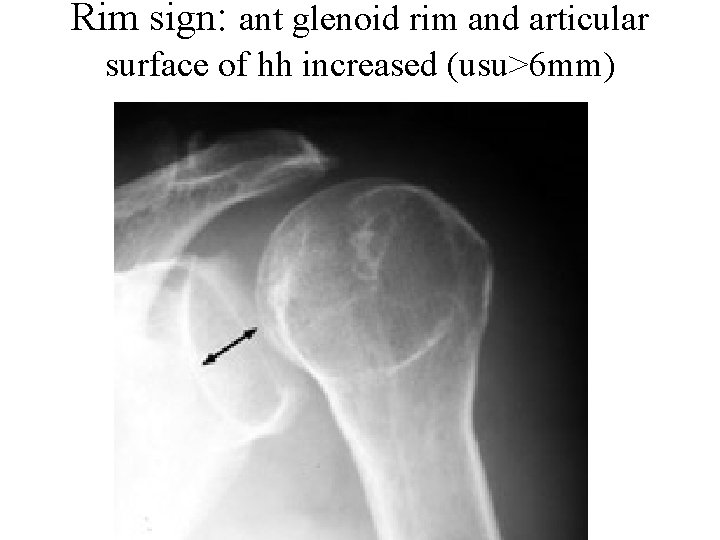
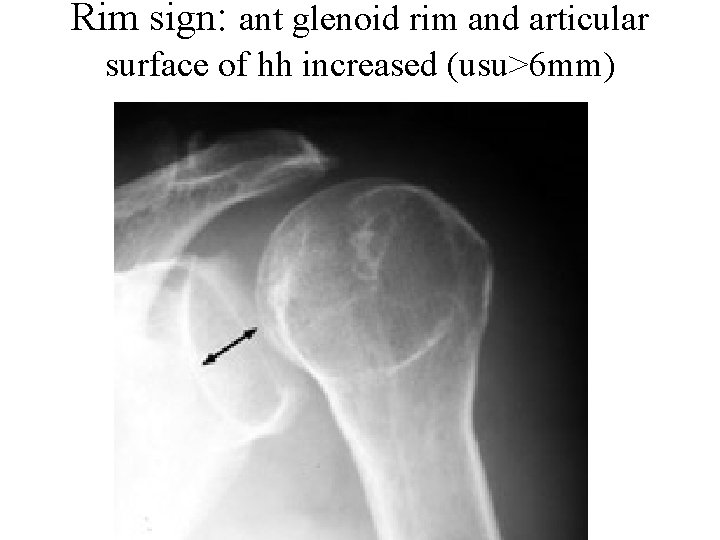
Rim sign: ant glenoid rim and articular surface of hh increased (usu>6 mm)
Summary • Reduce ASAP • Wary neurovascular status, fractures & rotator cuff injuries • Consider necessity of pre & post reduction films on an individual basis • Know well three methods of reduction • Suspect posterior dislocations in appropriate pts