Give rationales for Tracheostomy Care A Assess skin



- Slides: 18
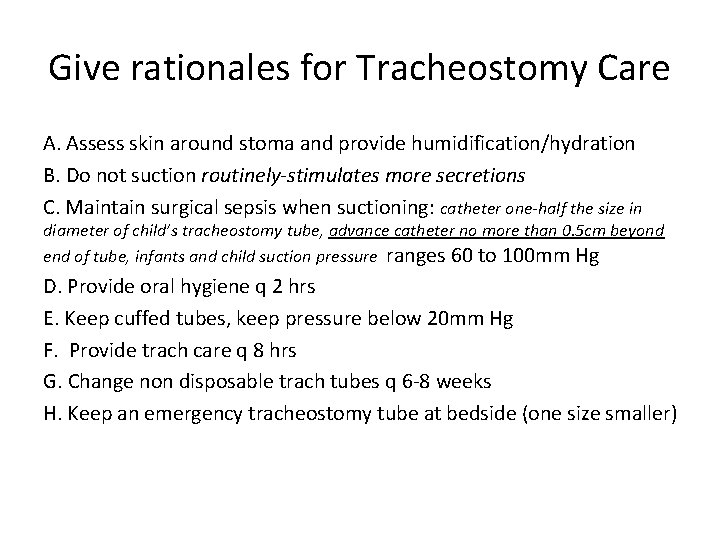
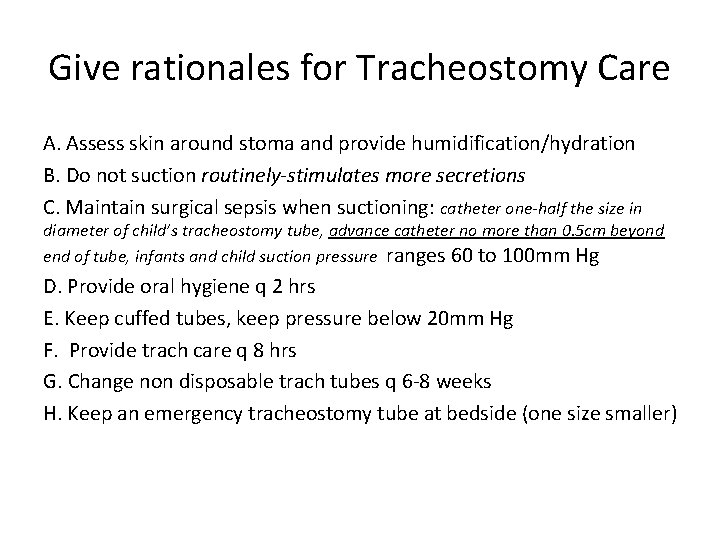
Give rationales for Tracheostomy Care A. Assess skin around stoma and provide humidification/hydration B. Do not suction routinely-stimulates more secretions C. Maintain surgical sepsis when suctioning: catheter one-half the size in diameter of child’s tracheostomy tube, advance catheter no more than 0. 5 cm beyond end of tube, infants and child suction pressure ranges 60 to 100 mm Hg D. Provide oral hygiene q 2 hrs E. Keep cuffed tubes, keep pressure below 20 mm Hg F. Provide trach care q 8 hrs G. Change non disposable trach tubes q 6 -8 weeks H. Keep an emergency tracheostomy tube at bedside (one size smaller)
Complications of Tracheostomies What is the nursing action? A. Accidental Dec annulation. B. Very Dangerous in first 72 hours-why? C. Occlusion
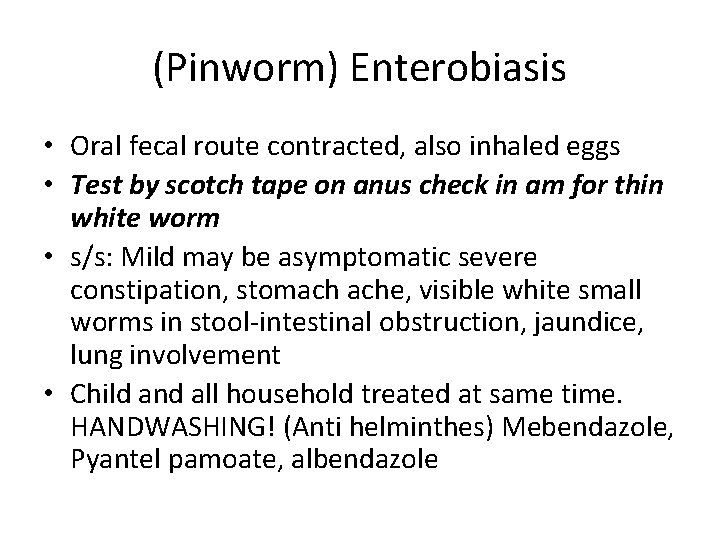
(Pinworm) Enterobiasis • Oral fecal route contracted, also inhaled eggs • Test by scotch tape on anus check in am for thin white worm • s/s: Mild may be asymptomatic severe constipation, stomach ache, visible white small worms in stool-intestinal obstruction, jaundice, lung involvement • Child and all household treated at same time. HANDWASHING! (Anti helminthes) Mebendazole, Pyantel pamoate, albendazole
Pain medication side effects Opioids : Morphine, Fentanyl, Codeine, Respiratory depression Constipation Sedation Pruritus Nausea, Vomiting
Complications of Pertussis • • • * Pneumonia dehydration. temporary pauses in breathing as a result of severe difficulty with breathing. weight loss due to excessive vomiting. seizures low blood pressure, requiring medication.
Cranial Nerve Functions • Trigeminal Nerve: • 5 th cranial nerve (muscles of mastication) affects sensoryface, scalp, nasal and buccal mucosa • Assess: 1. Have child bite down hard and open jaw-test symmetry and strength 2. With child’s eyes closed, see if child can detect light touch in mandibular and maxillary regions 3. test corneal and blink reflex by touching cornea lightly (approach from side so that child does not blink before cornea is touched).

Reyes Syndrome • Cause: Not understood but affects liver and brain usually follows virus-affected by ASA • Assessment: Lethargy, irritability, combativeness, confusion, delirium, profuse vomiting, convulsions, loss of consciousness Prevention: no ASA
Herpes Simplex 1 oral • May occur as a primary infection or recur in a less severe form known as recurrent herpes (commonly cold sores or fever blisters) • Wear gloves! • Primary infection fever, pharynx edematous, vesicles, red, cervical lymphadenitisdehydration may result • Genital herpes 2 -only transmitted by sex

Intussusception
Intussusception • Telescoping of bowel • Occurred with rotavirus vaccine and took vaccine off market • Treated with barium enema-if not reversed surgery
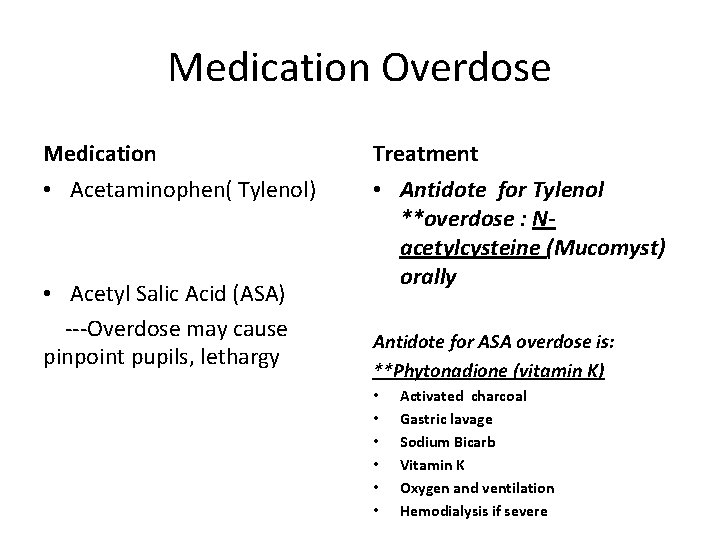
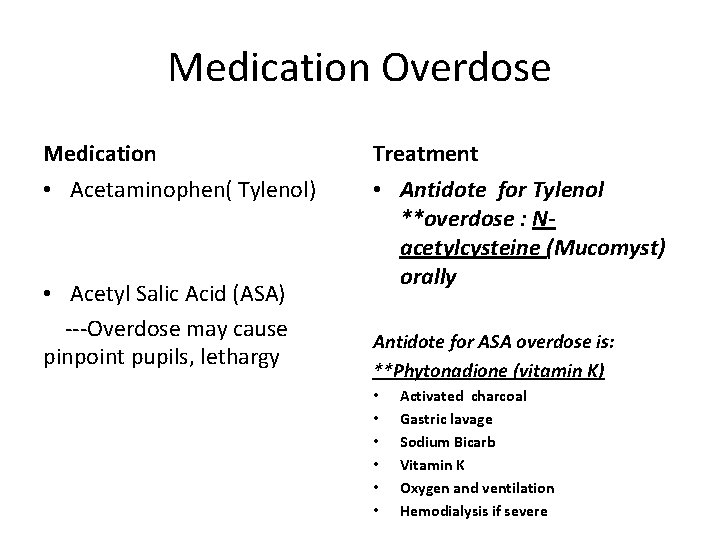
Medication Overdose Medication Treatment • Acetaminophen( Tylenol) • Antidote for Tylenol **overdose : Nacetylcysteine (Mucomyst) orally • Acetyl Salic Acid (ASA) ---Overdose may cause pinpoint pupils, lethargy Antidote for ASA overdose is: **Phytonadione (vitamin K) • • • Activated charcoal Gastric lavage Sodium Bicarb Vitamin K Oxygen and ventilation Hemodialysis if severe
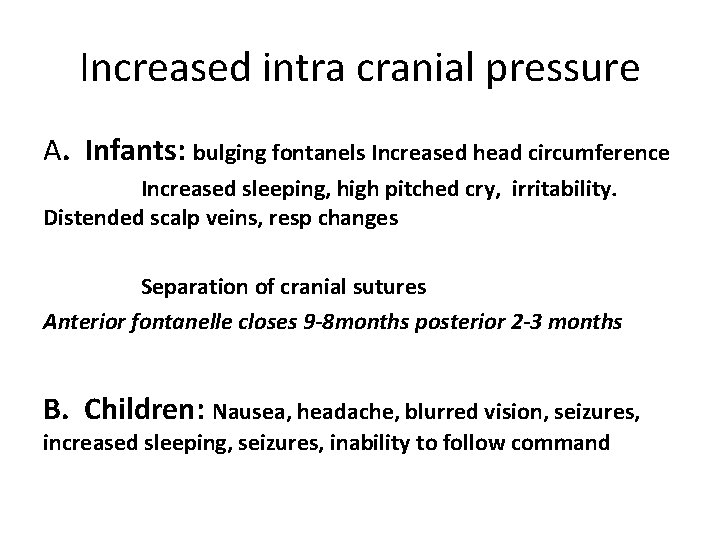
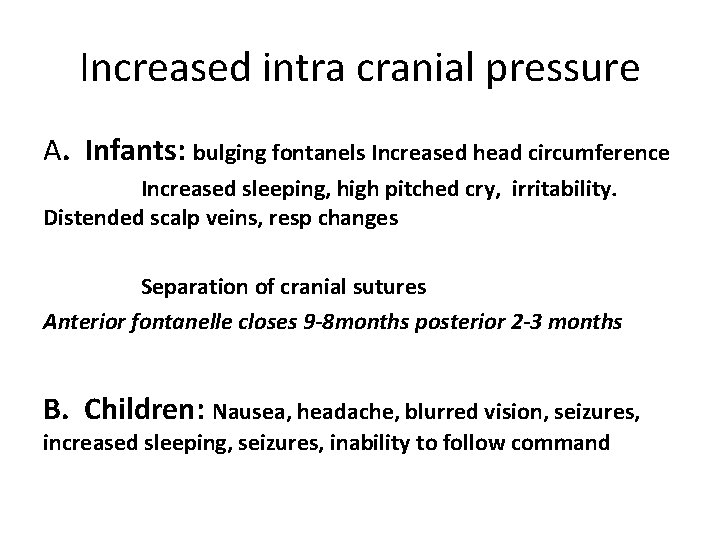
Increased intra cranial pressure A. Infants: bulging fontanels Increased head circumference Increased sleeping, high pitched cry, irritability. Distended scalp veins, resp changes Separation of cranial sutures Anterior fontanelle closes 9 -8 months posterior 2 -3 months B. Children: Nausea, headache, blurred vision, seizures, increased sleeping, seizures, inability to follow command
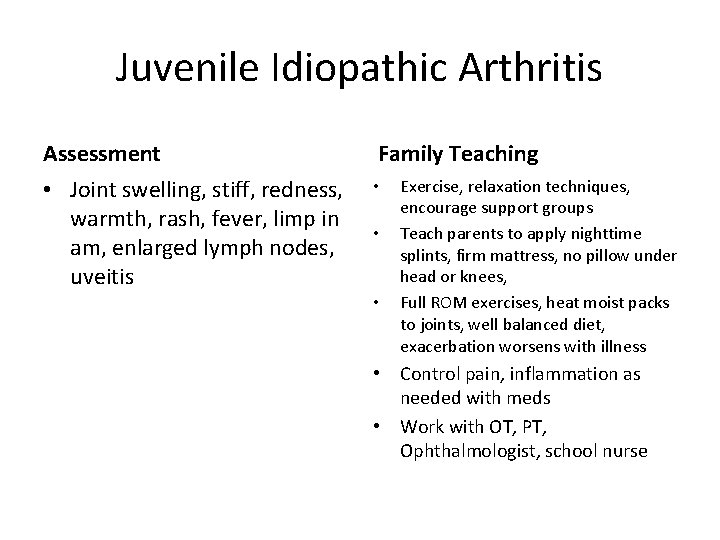
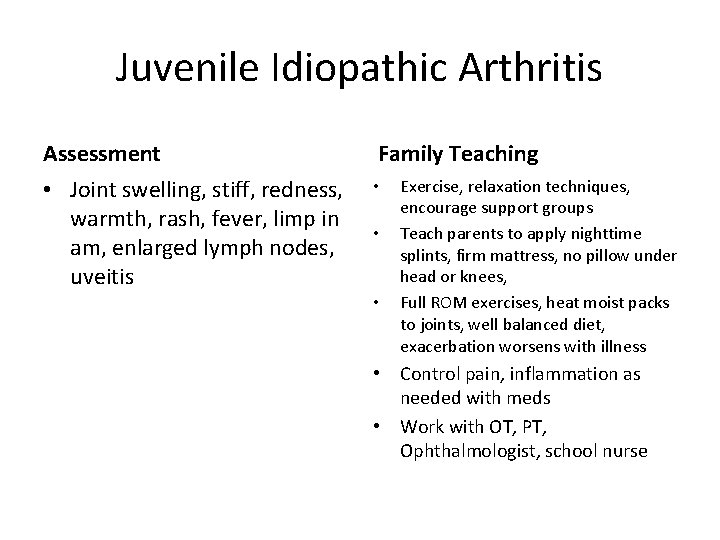
Juvenile Idiopathic Arthritis Assessment Family Teaching • Joint swelling, stiff, redness, warmth, rash, fever, limp in am, enlarged lymph nodes, uveitis • • • Exercise, relaxation techniques, encourage support groups Teach parents to apply nighttime splints, firm mattress, no pillow under head or knees, Full ROM exercises, heat moist packs to joints, well balanced diet, exacerbation worsens with illness • Control pain, inflammation as needed with meds • Work with OT, PT, Ophthalmologist, school nurse

A nurse is caring for a school age child who has JIA. Which of the following are appropriate home care instructions? *A. Sleep on a firm mattress B. Use cold compresses for joint pain C. Take ibuprophen on an empty stomach *D. Take frequent rest periods throughout the day *E. Perform range of motion exercises
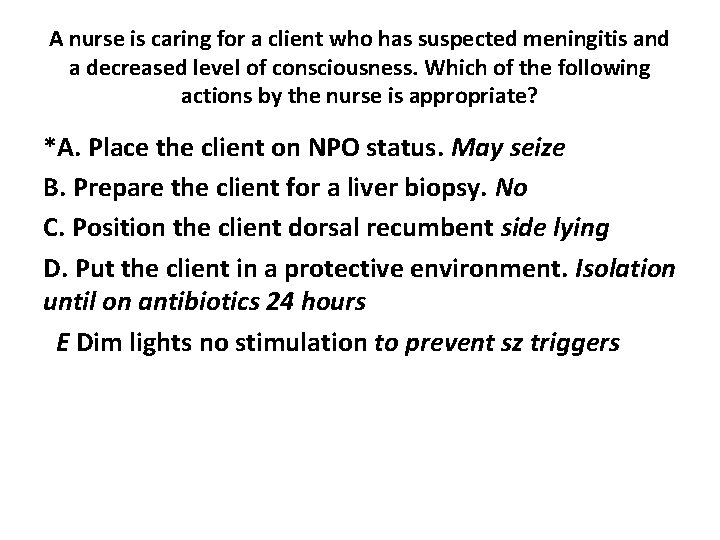
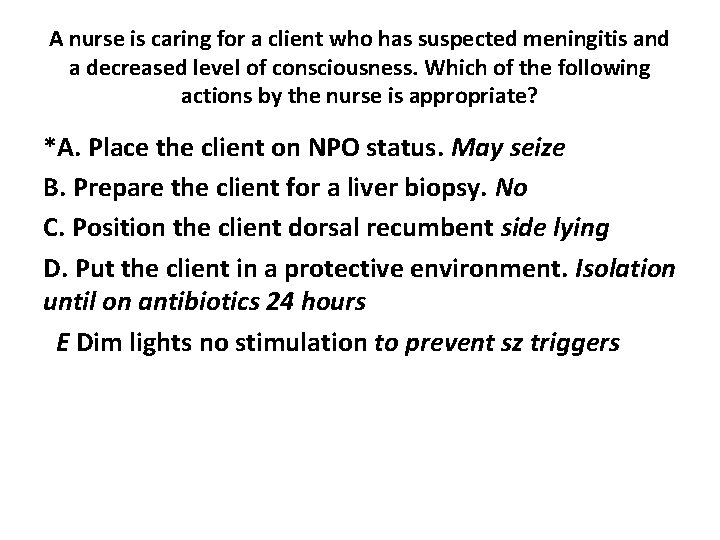
A nurse is caring for a client who has suspected meningitis and a decreased level of consciousness. Which of the following actions by the nurse is appropriate? *A. Place the client on NPO status. May seize B. Prepare the client for a liver biopsy. No C. Position the client dorsal recumbent side lying D. Put the client in a protective environment. Isolation until on antibiotics 24 hours E Dim lights no stimulation to prevent sz triggers
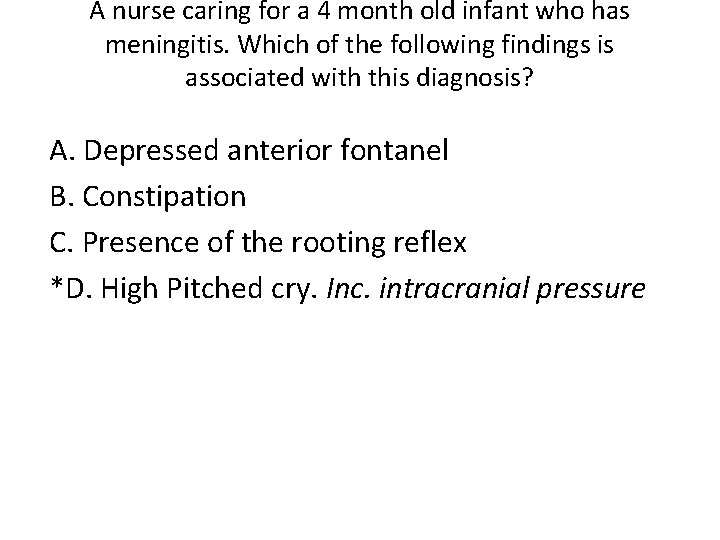
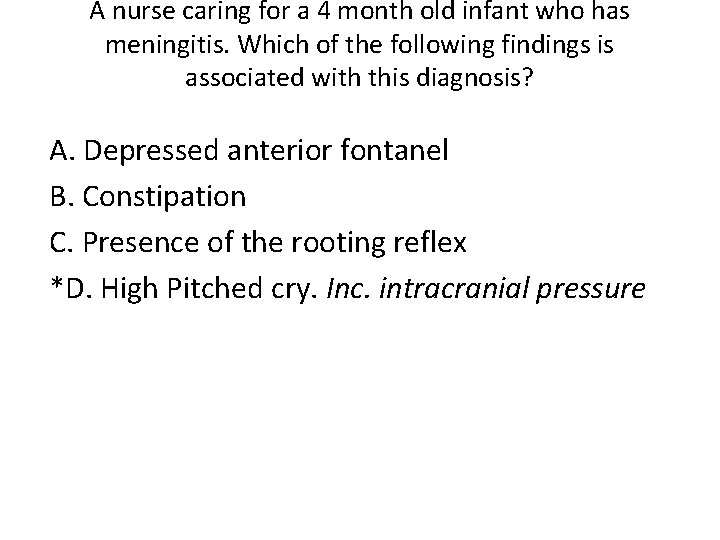
A nurse caring for a 4 month old infant who has meningitis. Which of the following findings is associated with this diagnosis? A. Depressed anterior fontanel B. Constipation C. Presence of the rooting reflex *D. High Pitched cry. Inc. intracranial pressure
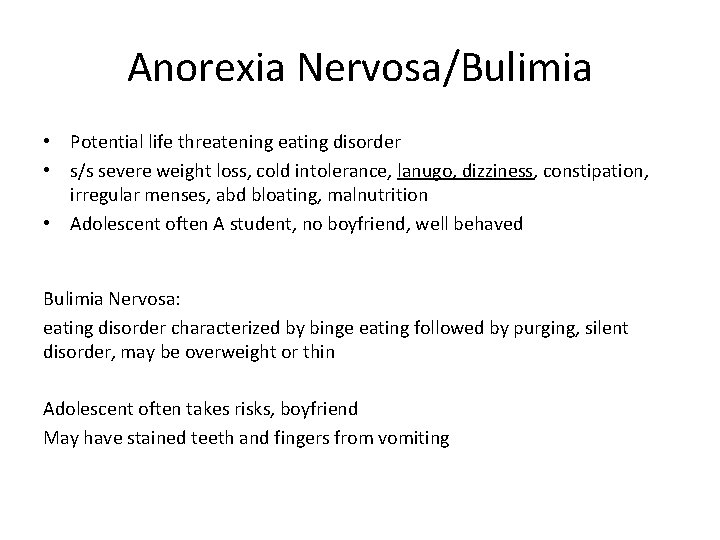
Anorexia Nervosa/Bulimia • Potential life threatening eating disorder • s/s severe weight loss, cold intolerance, lanugo, dizziness, constipation, irregular menses, abd bloating, malnutrition • Adolescent often A student, no boyfriend, well behaved Bulimia Nervosa: eating disorder characterized by binge eating followed by purging, silent disorder, may be overweight or thin Adolescent often takes risks, boyfriend May have stained teeth and fingers from vomiting
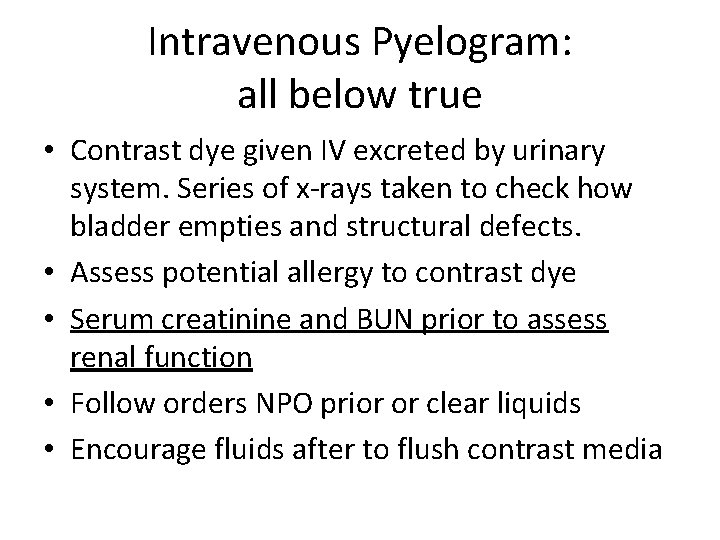
Intravenous Pyelogram: all below true • Contrast dye given IV excreted by urinary system. Series of x-rays taken to check how bladder empties and structural defects. • Assess potential allergy to contrast dye • Serum creatinine and BUN prior to assess renal function • Follow orders NPO prior or clear liquids • Encourage fluids after to flush contrast media