GITLec 1 Dr Basim Sh Ahmed Oral pathology
GIT/Lec. 1 Dr. Basim. Sh. Ahmed
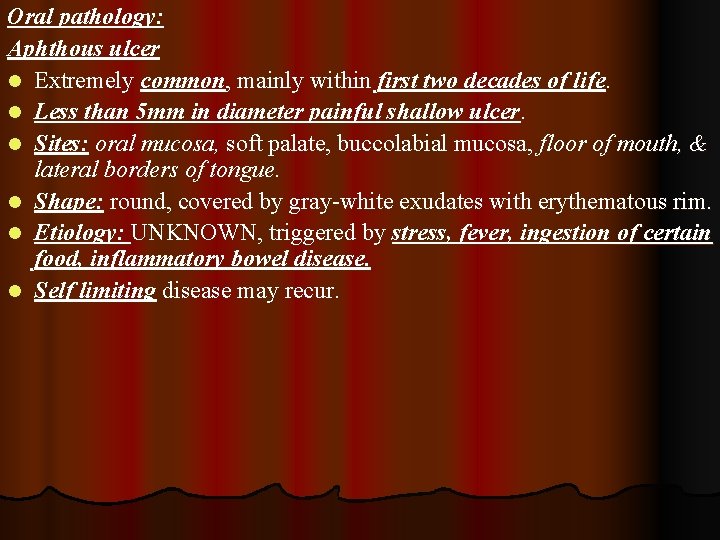
Oral pathology: Aphthous ulcer l Extremely common, mainly within first two decades of life. l Less than 5 mm in diameter painful shallow ulcer. l Sites: oral mucosa, soft palate, buccolabial mucosa, floor of mouth, & lateral borders of tongue. l Shape: round, covered by gray-white exudates with erythematous rim. l Etiology: UNKNOWN, triggered by stress, fever, ingestion of certain food, inflammatory bowel disease. l Self limiting disease may recur.
Aphthous ulcer
Herpes infection (Herpetic Stomatitis): l Extremely common, by type I Herpes Simplex Virus (HSV). l Also called cold sore (mainly at the lips & around the nasal orifices). l Transmit by Kissing (at the middle of life 3/4 of population are affected. Phases of infection: l Primary phase: is asymptomatic (virus persists in a dormant state within ganglia about the mouth e. g. trigeminal ganglia). l Reactivation phase: l Virus reactivated by (fever, excess sun or cold exposure, upper respiratory tract infection, immunosuppression & trauma)………. . Formation of solitary or multiple small vesicles containing clear fluid……. Rupture & leaving shallow painful ulcers (heal within weeks but recurrence is common). l Mic: intercellular & intracellular edema. Intranuclear viral inclusion. Giant cell formation or polykaryons.

Herpetic stomatitis
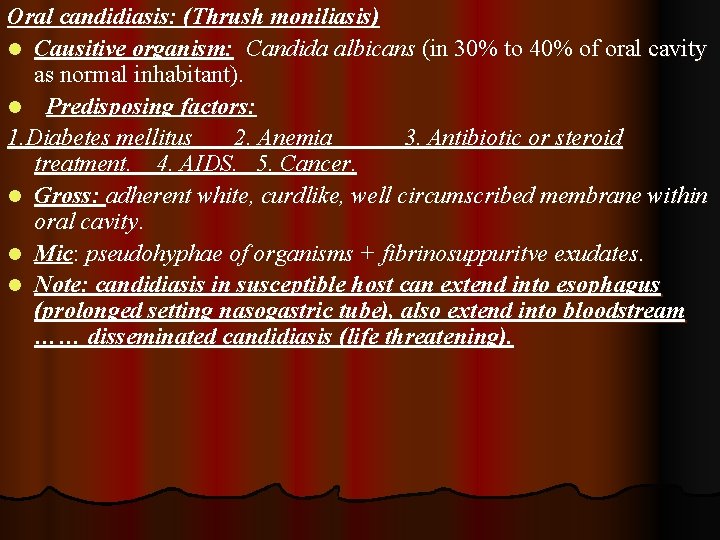
Oral candidiasis: (Thrush moniliasis) l Causitive organism: Candida albicans (in 30% to 40% of oral cavity as normal inhabitant). l Predisposing factors: 1. Diabetes mellitus 2. Anemia 3. Antibiotic or steroid treatment. 4. AIDS. 5. Cancer. l Gross: adherent white, curdlike, well circumscribed membrane within oral cavity. l Mic: pseudohyphae of organisms + fibrinosuppuritve exudates. l Note: candidiasis in susceptible host can extend into esophagus (prolonged setting nasogastric tube), also extend into bloodstream …… disseminated candidiasis (life threatening).

Oral candidiasis
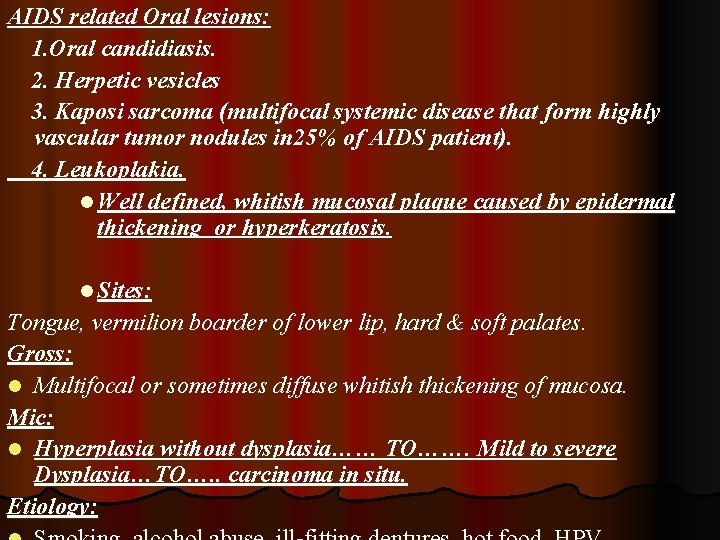
AIDS related Oral lesions: 1. Oral candidiasis. 2. Herpetic vesicles 3. Kaposi sarcoma (multifocal systemic disease that form highly vascular tumor nodules in 25% of AIDS patient). 4. Leukoplakia. l Well defined, whitish mucosal plaque caused by epidermal thickening or hyperkeratosis. l Sites: Tongue, vermilion boarder of lower lip, hard & soft palates. Gross: l Multifocal or sometimes diffuse whitish thickening of mucosa. Mic: l Hyperplasia without dysplasia…… TO……. Mild to severe Dysplasia…TO…. . carcinoma in situ. Etiology:
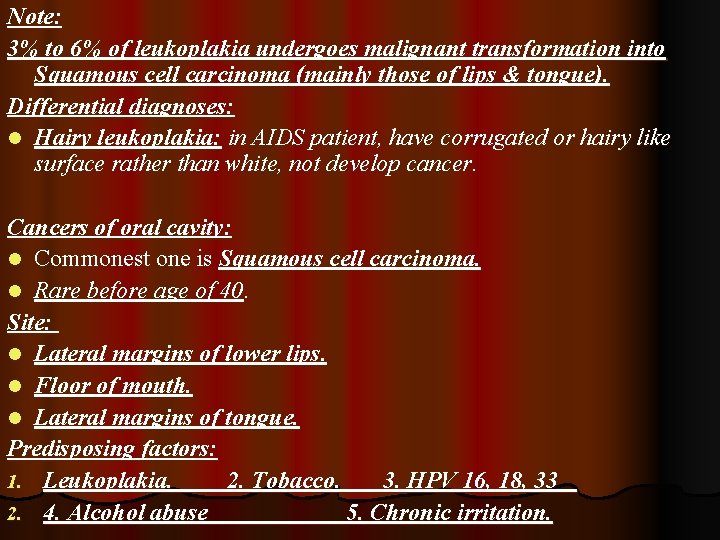
Note: 3% to 6% of leukoplakia undergoes malignant transformation into Squamous cell carcinoma (mainly those of lips & tongue). Differential diagnoses: l Hairy leukoplakia: in AIDS patient, have corrugated or hairy like surface rather than white, not develop cancer. Cancers of oral cavity: l Commonest one is Squamous cell carcinoma. l Rare before age of 40. Site: l Lateral margins of lower lips. l Floor of mouth. l Lateral margins of tongue. Predisposing factors: 1. Leukoplakia. 2. Tobacco. 3. HPV 16, 18, 33 2. 4. Alcohol abuse 5. Chronic irritation.

Kaposi’s sarcoma
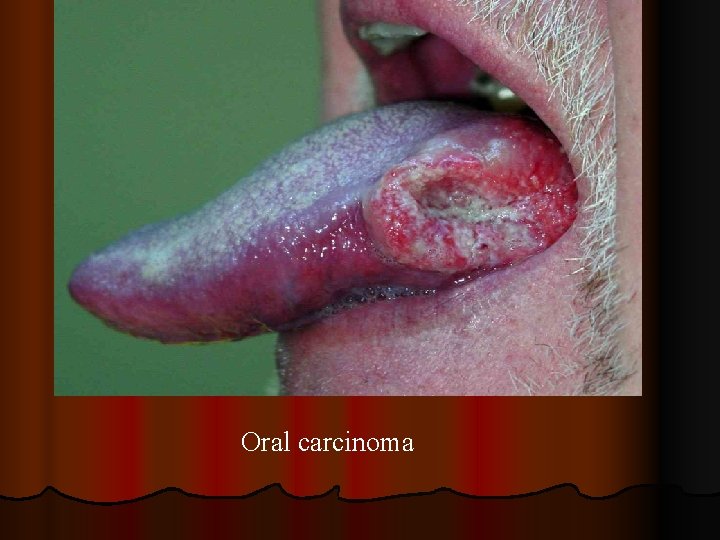
Oral carcinoma
Prognosis: l Good……. . For cancer of lips l Poor………. . for cancers of mouth & tongue. Salivary glands Pathology Sialoadenitis: Could be Viral, Bacterial & autoimmune. 1. Viral sialoadenitis: commonest one is mumps (Paramyxovirus), Mainly affect parotid gland. In adult is associated with pancreatitis, orchitis (sometimes cause sterility); while in children is self limiting. 2. Bacterial sialoadenitis: l Mostly secondary to obstruction of duct of salivary gland by stone (Sialolithiais). l Or secondary to sever dehydration state (postoperative patient) by entrance from oral cavity. l Acute bacterial sialoadenitis can complicated as abscess formation.
3. Autoimmune sialoadenitis: l Major cause of chronic sialoadenitis. l Almost bilateral (sjogren syndrome)……. (Affect all salivary & lacrimal glands)……. . result in dry mouth (Xerostomia) & dry eyes (keratoconjunctivitis sicca). l The combination of salivary & lacrimal glands inflammatory enlargement (painless) + Xerostomia ……. This is called Mikulicz syndrome. - The causes of this syndrome are (sarcoidosis, leukemia, and lymphoma). Tumors of salivary glands: l About 80% 0 f tumors are in the parotid glands. l Male = Female, 6 th- 7 th decade of life. l 70% - 80% of parotid tumors are benign, while about 50% 0 f submandibular tumors are benign.
Commonest tumor in parotid gland is BENIGN PLEOMORPHIC ADENOMA (mixed tumor). l Second commonest tumor is papillary cystadenoma lymphamatosum (Warthin tumor). l Whatever the type of tumors are presented as a mass at the angle of jaw. l Benign pleomorphic adenoma: l Form about 90% of all benign tumors of salivary glands. l Slow growing, well defined & encapsulated, rare larger than 6 cm in diameter. l Most of these arise in the superficial part of parotid. l Although it is encapsulated; microscopic examination revealed multiple sites of Capsular penetration (so need safety margin on removal by surgery).
l Mic: two parts (epithelial part arranged in forms of ducts, acini , tubules , sheets & myxoid connective tissue stroma); sometime contain foci of chondroid & bony tissue. Notes: l Primary or Recurrent benign tumors for more than 10 to 20 years may show malignant transformation. l Frequency of Malignant salivary glands tumors as followings: 1. 50% in sublingual gland. 2. 40% in submandibular gland. 3. 10% in parotid gland. l Examples on malignant glands (mucoepidemoid carcinoma, adenoid cystic carcinoma).
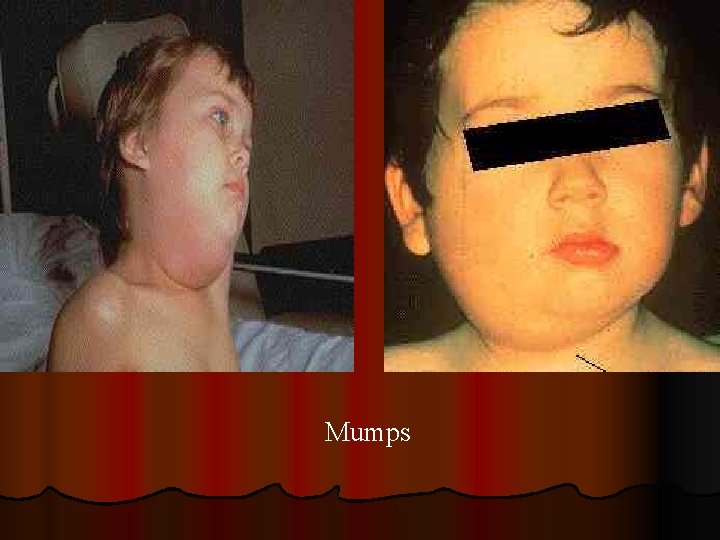
Mumps

Sjogren’s syndrome
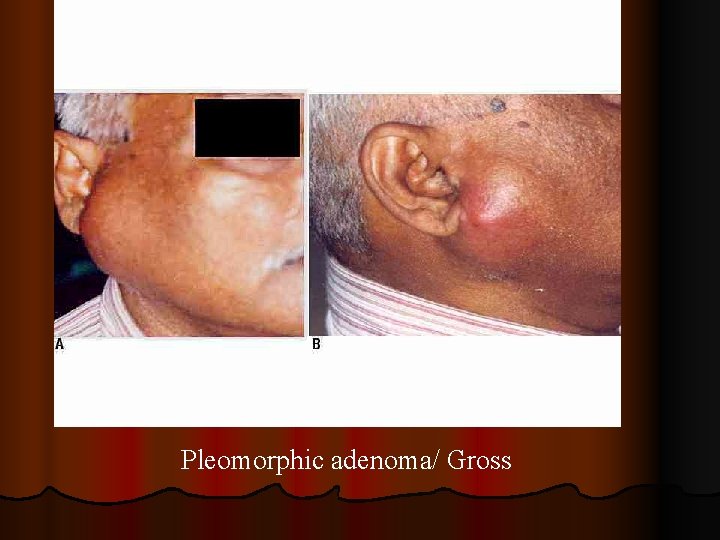
Pleomorphic adenoma/ Gross
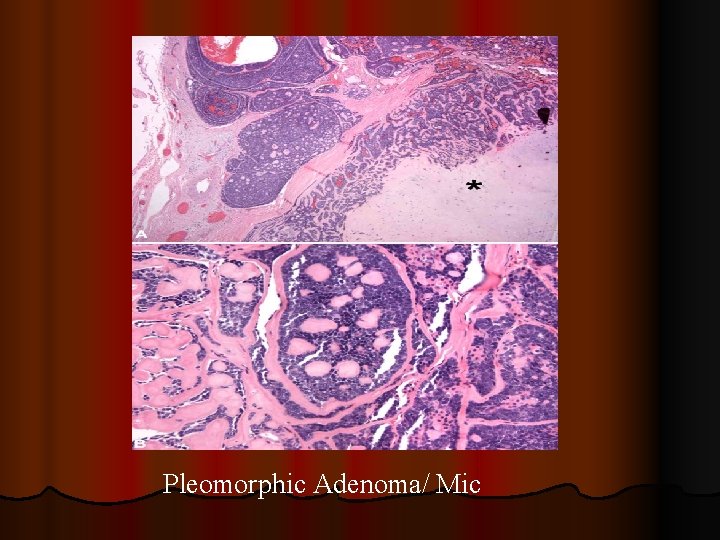
Pleomorphic Adenoma/ Mic

Thank you
- Slides: 20