Gingival and periodontal diseases in children The gingiva







- Slides: 73
Gingival and periodontal diseases in children.
The gingiva forms the important part of the periodontium, the supporting structure of the tooth.
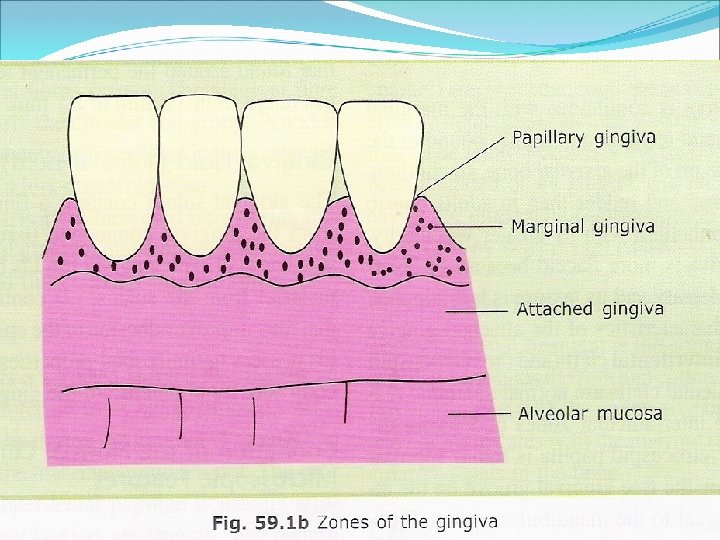
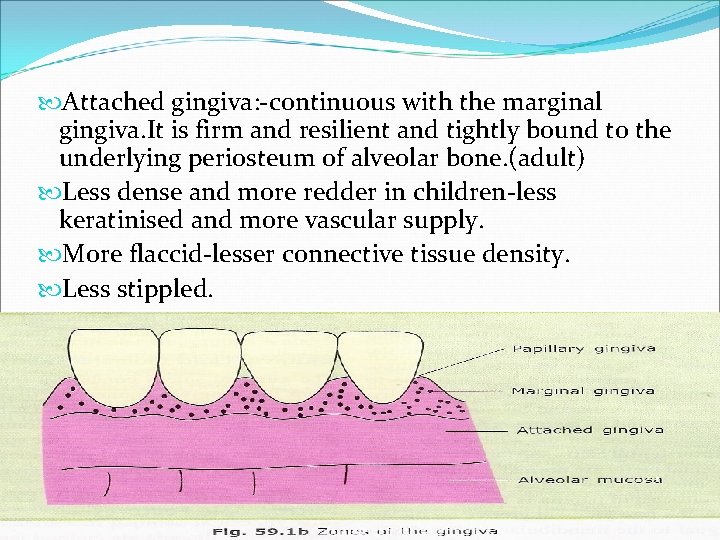
Gingiva is a masticatory type of oral mucous membrane, forms the covering of the teeth. 3 parts: Marginal gingiva. Attached gingiva. Interdental gingiva
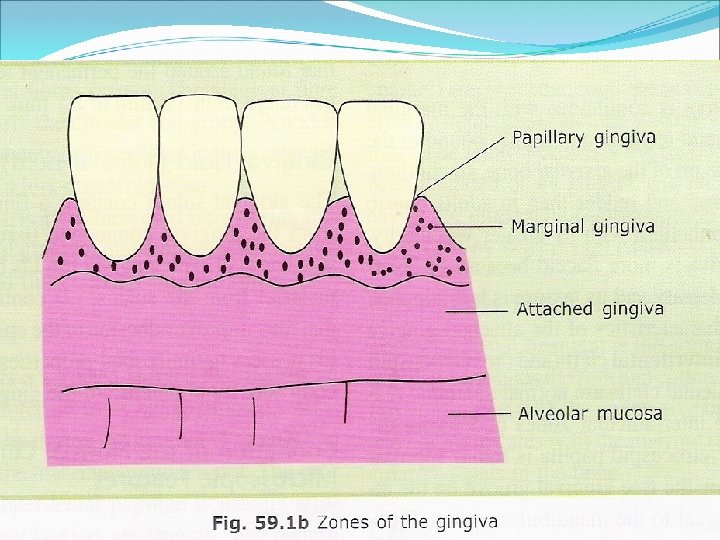

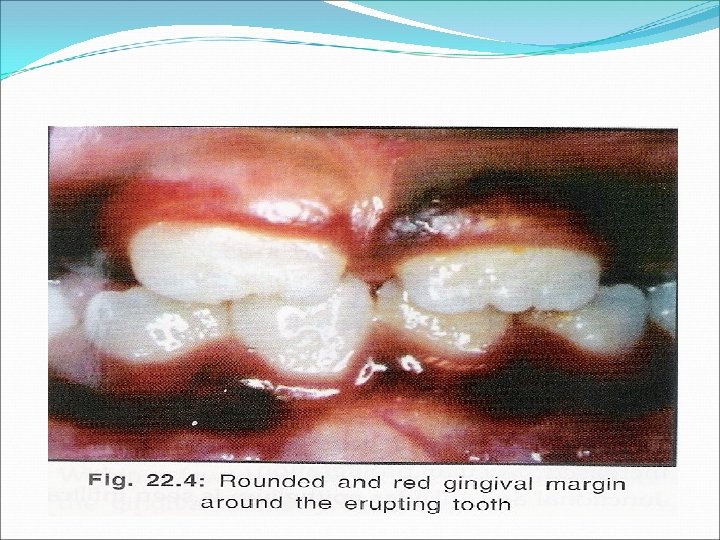
Marginal Gingiva: Gingival crevice or the sulcus and a free gingival margin. Free gingival margin-thicker and rounded-primary teeth due to morphological characterstics-cervical bulge and underlying constriction at CEJ. Knife edge in permanent dentition.
Marginal gingiva-flaccid and retractable Immature connective tissue. Immature gingival fiber system. Increased vascularisation.
Attached gingiva: -continuous with the marginal gingiva. It is firm and resilient and tightly bound to the underlying periosteum of alveolar bone. (adult) Less dense and more redder in children-less keratinised and more vascular supply. More flaccid-lesser connective tissue density. Less stippled.
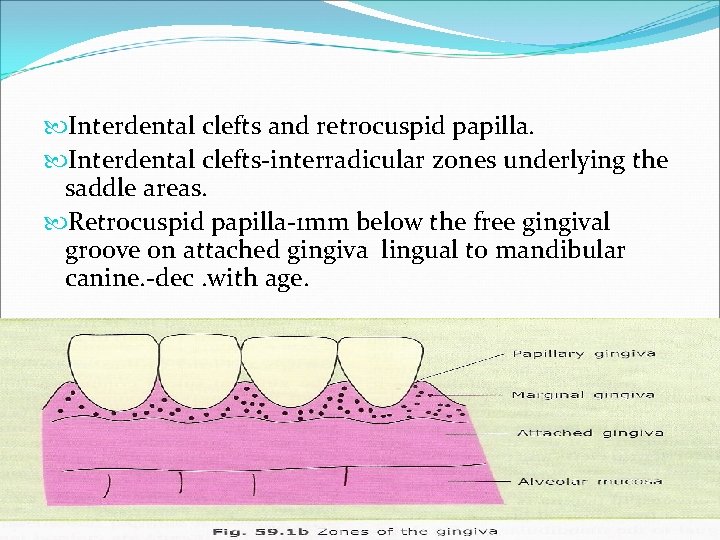
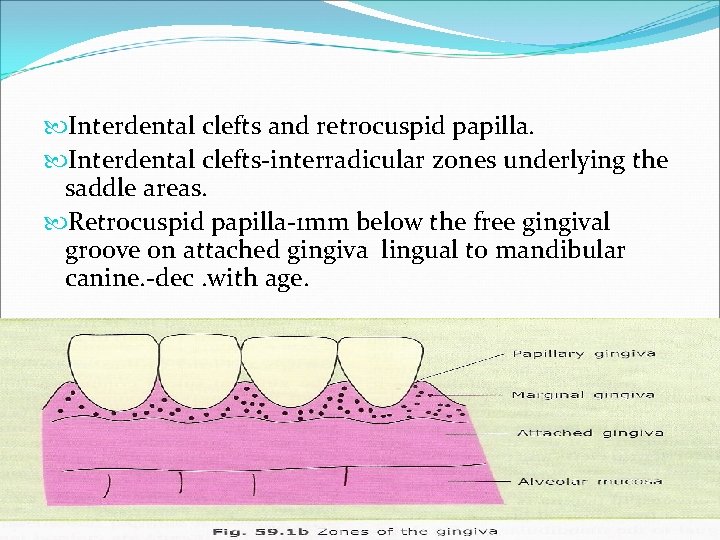
Interdental clefts and retrocuspid papilla. Interdental clefts-interradicular zones underlying the saddle areas. Retrocuspid papilla-1 mm below the free gingival groove on attached gingiva lingual to mandibular canine. -dec. with age.

Interdental gingiva: -interdental spacing. Saddle areas-well keratinised. less risk of development of inflammatory lesions. Low prevalance of periodontal lesions in children.
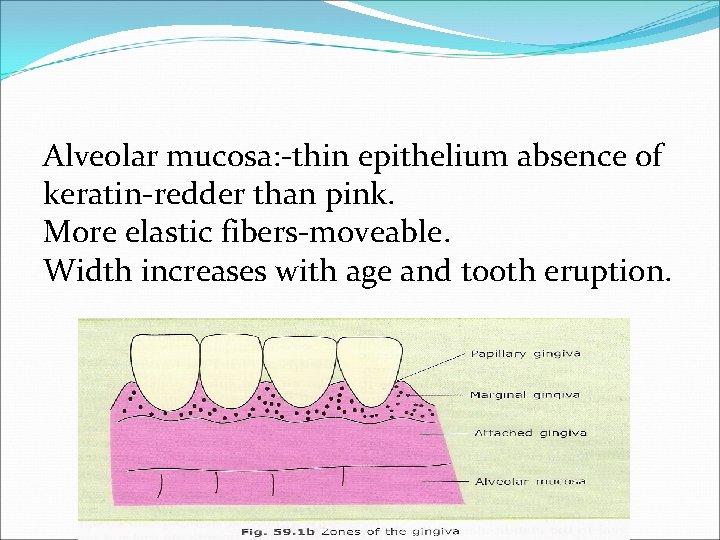
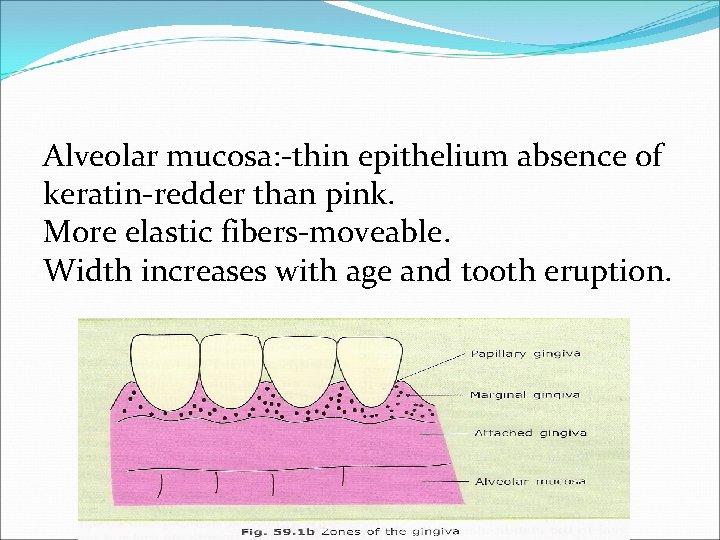
Alveolar mucosa: -thin epithelium absence of keratin-redder than pink. More elastic fibers-moveable. Width increases with age and tooth eruption.
Gingival sulcus: -shallow crevice or space around the tooth bounded by the surface of tooth on one side and the epithelium lining the free margin of the gingiva on the other. normal depth is 2 -3 mm. Primary dentition it more mean value range from 1. 4 mm-2. 1 mm
Alveolar bone: -less calcified, more vascular, larger marrow space, thin lamina dura, flat interdental crests.
Why only gingivitis Less periodontitis in children A)More anabolic activity due to increase metabolism. B)Absence of bacteria responsible for periodontal disease-Spirochetes and B. melaninogenicus. C)Altered composition of plaque. D)Decreased leukocytic migratory rate –low levels of immmunoglobulins specific for plaque bacteria.
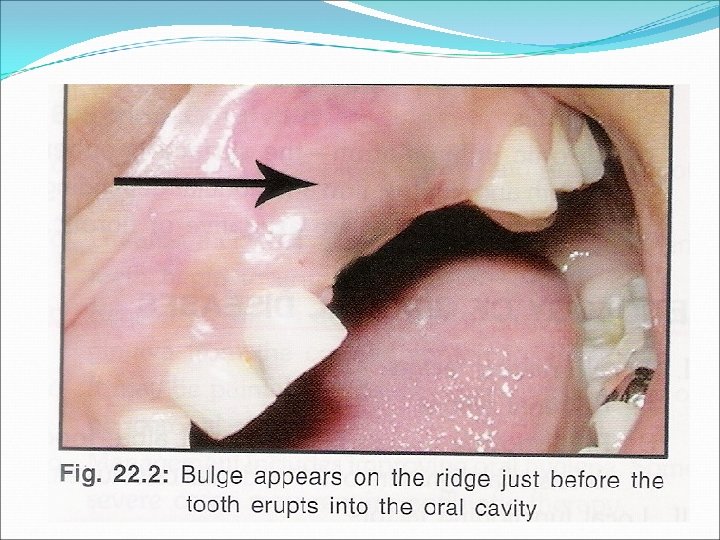
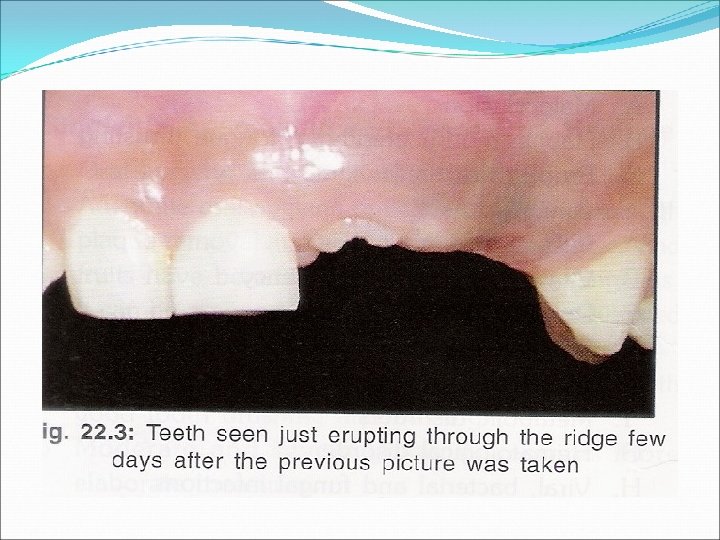
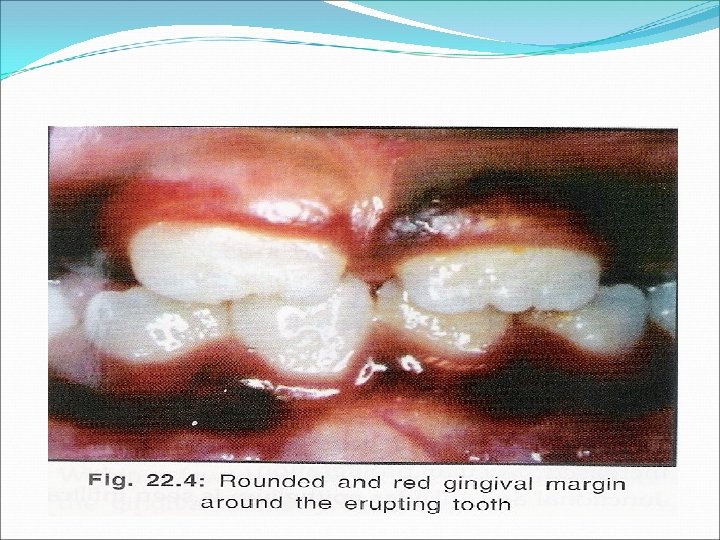
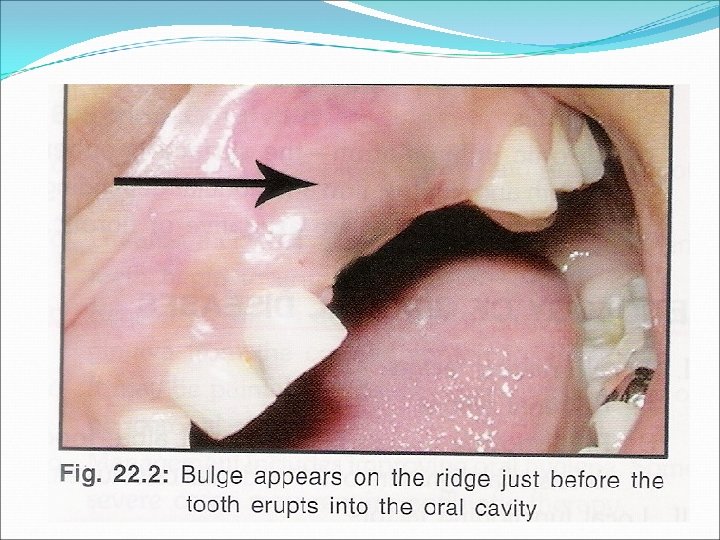
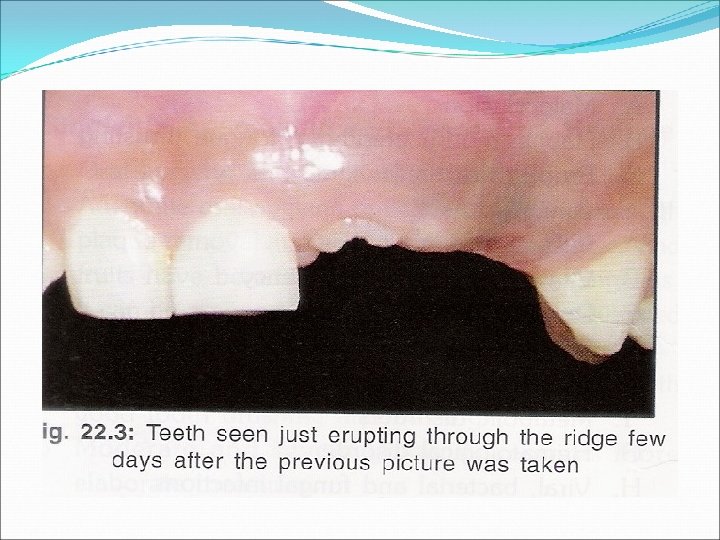
Physiologic changes associated with tooth eruption: Pre-eruptive stage. Eruptive stage. Post eruptive stage.

Gingivitis: -inflammatory involvement of gingival tissues. Inflammatory exudate Edema. Destruction of collagenous gingival fiber. Ulceration of epithelium.
Stages of gingivitis: Stage 1: -Initial lesion 2 -4 days Mild change in color. Vascular dilatation. Junctional epithilium and sulcular epitheliuminfiltrated by polymorphonuclear cells.
Stage 2: 4 -7 days. More vascular proliferation. Junctional and sulcular epithelium-infiltrated by polymorphonuclear cells, rete pegs formation. Lymphocytes are predominent. Loss of collagen. c/f-erythema, bleeding on probing
Stage 3: -Established lesion 14 -21 days. Increased vascular proliferation and blood stasis. More severe changes seen in junctional and sulcular epithelium. Severe loss of collagen. Plasma cells are predominent. Changes in color, size, texture
Stage 4: -advanced lesion. Lesion extends in to alveolar bone. Periodontal distruction. Clinical features: Gingival bleeding. Change in color. Change in the consistency of gingiva. Changes in the surface texture of the gingiva.
Etiology of gingival diseases: 1. Local irritating factors: A)bact. plaque. B)predisposing factors: - material alba, food debries, malalignment of teeth, dental calculus.
2)Local functioning factors: A)Malocclusion B)Habits 3)systemic factors: A)Puberty. B)Vitamin or protein deficiency. C)Drugs and chemicals. D)Pregnancy.
E)Metabolic disorder. D)Viral, bacterial and fungal infection.
Classification of gingival diseases: A)Simple gingivitis. 1)Eruption gingivitis. 2)Gingivitis associated with poor oral hygiene. B)Acute gingival inflammation. 1)Herpes simplex virus infection. 2)Recurrent apthous ulcer.
3)Acute necrotizing ulcerative gingivitis. 4)Acute candidiasis. 5)Acute bacterial infection. C)Chronic non specific gingivitis.
D)Conditioned gingival enlargement. 1)Puberty gingivitis. 2)Fibromatosis. 3)Phenytoin-induced gingival overgrowth. E)Scorbutic gingivitis
simple gingivitis: a)Eruption gingivitis: Treatment: -pericoronitis-phenol 5%, 15 ml of tincture of iodine and 20 ml of glycerine. Pericoronitis with swelling and lymphnode enlargement. antibiotics
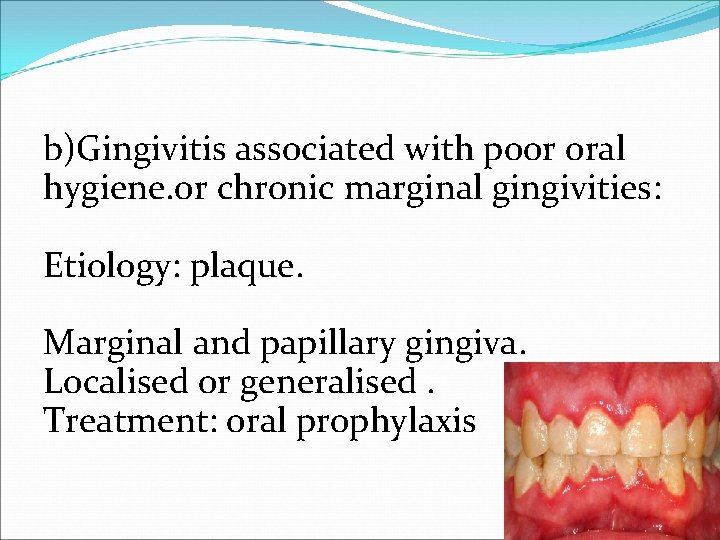
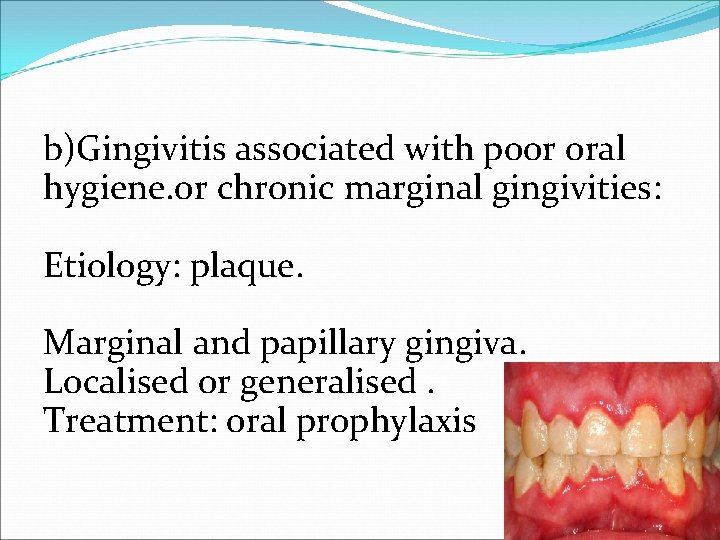
b)Gingivitis associated with poor oral hygiene. or chronic marginal gingivities: Etiology: plaque. Marginal and papillary gingiva. Localised or generalised. Treatment: oral prophylaxis

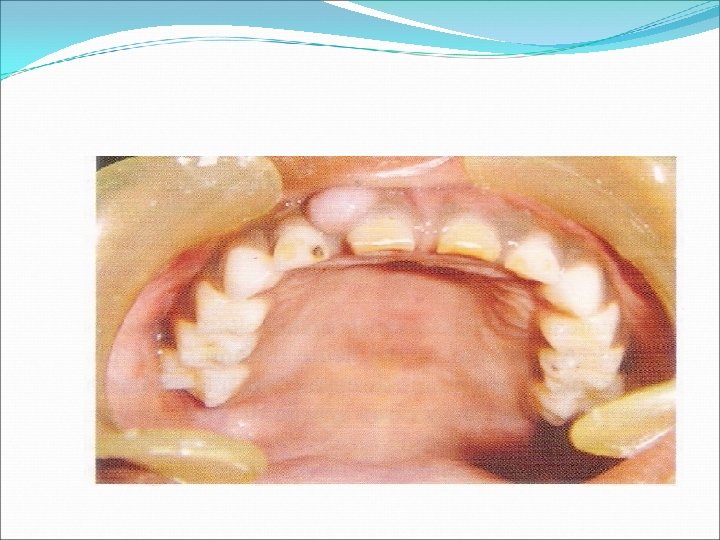
Acute inflammatory Enlargement
Gingival abscess: Localised painful, rapidly expanding lesionsudden onset. Marginal gingiva or interdental gingiva. Initially appears as a red swelling with smooth shiny surface. 24 -48 hrs it becomes fluctuant and pointed. purulent exudate. Adjacent teeth –sensitive
Etiology. Impacted foreign substance. Treatment: Topical LA-incision-drain the pus-cleansed with saline or warm water-gauze pad. Home-warm water rinse.
Viral: Acute herpetic gingivostomatitis 2 types of HSV-1 -upper part of body. HSV-2. -lower part of the body.
Rarely occur before the age of 6 months presence of circulating antibodies. in the infants , derived from the mother. Focal itching , burning or tingling sensations on the lips -1 -7 days. This may be proceeded by stress, strain, oral trauma, pharyngitis, sinusities.
Condition occurs during and immediately after an episode of pneumonia, typhoid and influenza Development of fever , irritability, head ache, pain upon swallowing and regional lymphadenopathy.
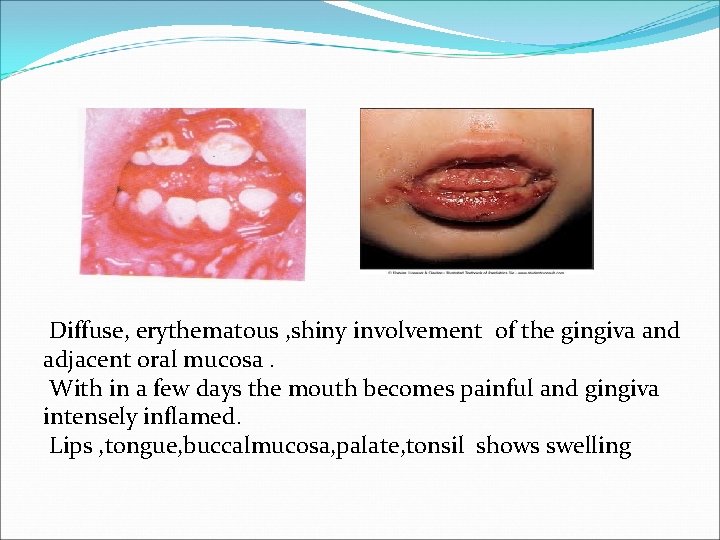
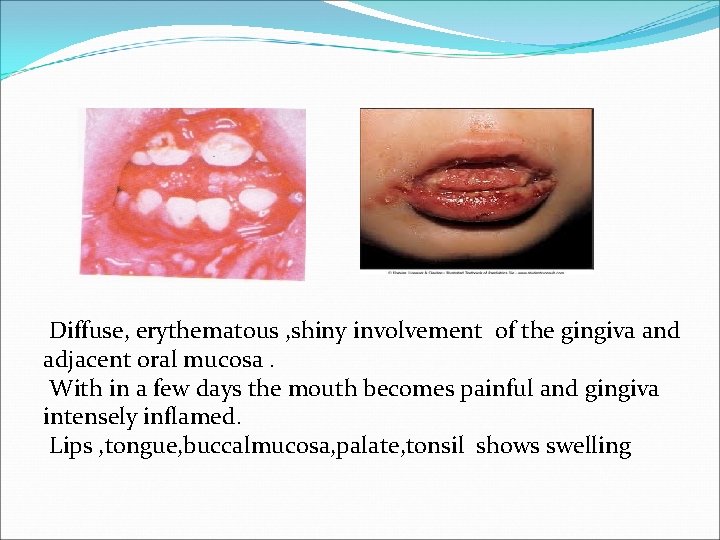
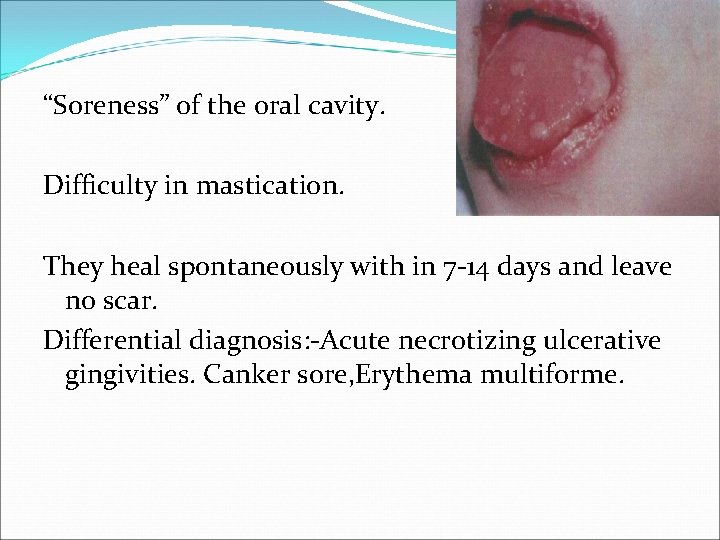
Diffuse, erythematous , shiny involvement of the gingiva and adjacent oral mucosa. With in a few days the mouth becomes painful and gingiva intensely inflamed. Lips , tongue, buccalmucosa, palate, tonsil shows swelling
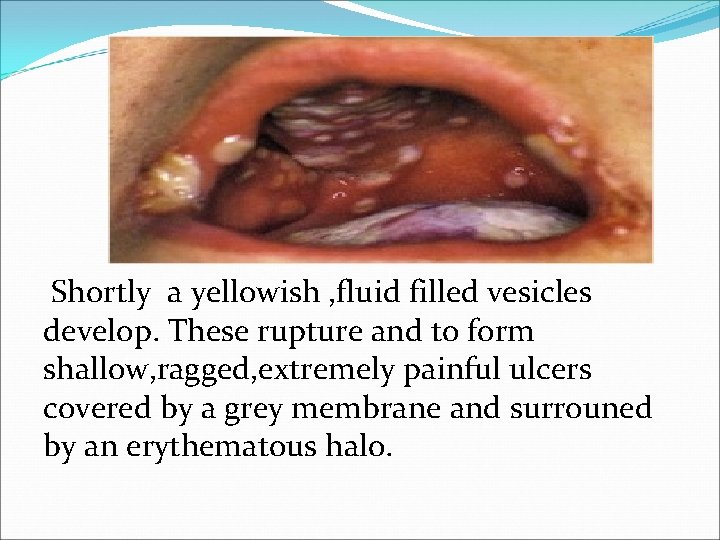
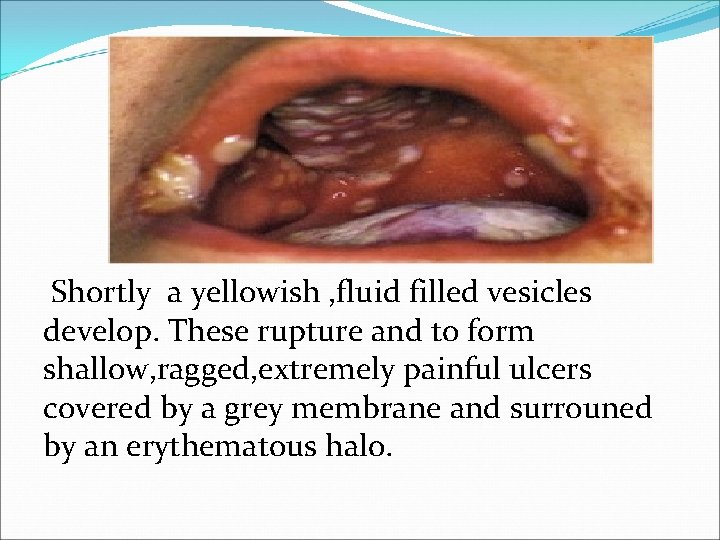
Shortly a yellowish , fluid filled vesicles develop. These rupture and to form shallow, ragged, extremely painful ulcers covered by a grey membrane and surrouned by an erythematous halo.
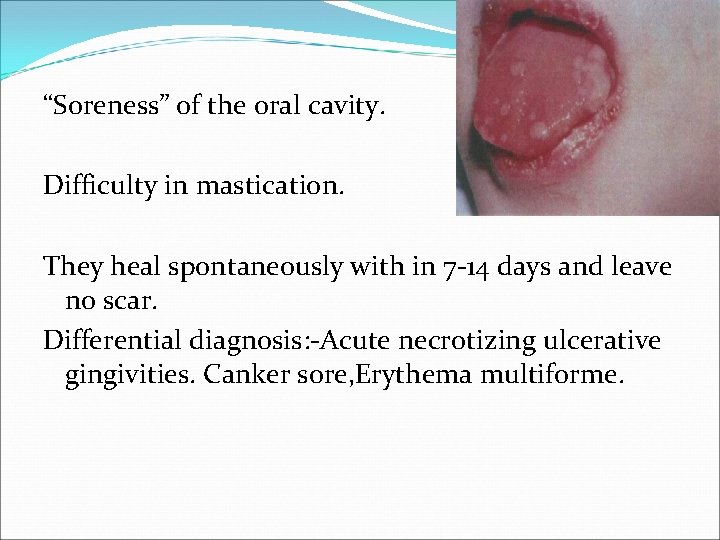
“Soreness” of the oral cavity. Difficulty in mastication. They heal spontaneously with in 7 -14 days and leave no scar. Differential diagnosis: -Acute necrotizing ulcerative gingivities. Canker sore, Erythema multiforme.
Treatment: Application of mild topical anaesthetic – Dicyclomine HCL(0. 5%) before mealtime. Lidocaine -topical LA. -tell them to hold it in mouth for 2 -3 minutes. Vitamin supplement. Acyclovir. (Zovirax)
Acute necrotising ulcerative gingivities: Trenchmouth, vincent’s angina or stomatitis. Etiology: -Fusiform bacilli, spirocheates. Local factors-over hangingrestoration, malocclusion. Systemic factors-stress. Nutritional deficiency-Vitamin. B , Vitamin. C. Debilitating diseases. Down’syndrome, AIDS, diabetes

C/f: Primary diagnostic signs: -gingival bleeding. Interdental ulceration and necrosis. Blunting and cratering of gingiva. Elevated temperature.
Secondary diagnostic feature. Pseudomembrane. Fetid odor. Bad taste-mandibular anteriors. Wooden sensation of teeth.
Severe cases systemic complications-high fever, lymphadenopathy, increased pulse rate, anorexia. Treatment: Local debridement , sub gingival curettage. Mild oxygenating solutions.
Penicillins/erythromycin, metranidazole. NSAIDS. Fluid consumption. Bed rest.
Drug induced gingival hyperplasia: Phenytoin, cyclosporine, nifedipine. c/f: 2 -3 weeks after initiation of phenytoin therapy. Painless enlargement of interproximal gingiva. Buccal and ant. segment more than lingual and posterior.
Gingiva -pink and firm unless infected. No bleeding. Interdental lobulations-clefting-pseudopockets. Difficulty in mastication, speech. Treatment: - maintenance of oral hygiene. Change of drug or drug dossage. Surgical excision.

Scorbutic gingivitis: Vit c deficiency. Marginal and papillae. Bluish red, soft, friable shiny surface. Spontaneous bleeding on slight touch. In infants the enlarged tissue may cover clinical crown.
Treatment: Oral prophylaxis. Vitamin C tablets, citrus fruits.
Periodontal diseases in children: Pre-pubertal periodontitis. Localized aggressive periodontitis. Generalized aggressive periodontitis.
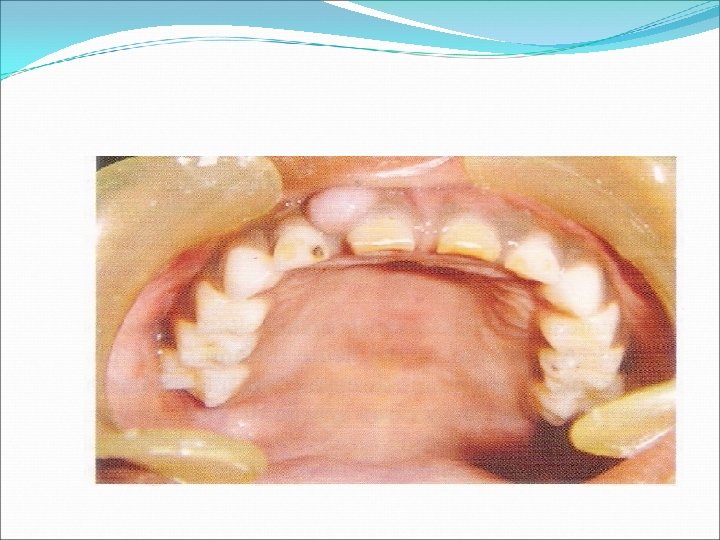
Pre-pubertal periodontitis: Normally it is generalized. But in children –localized. Loss of attachment and alveolar bone lossdeciduous dentition-molar and incisor region. Minimal plaque accumulation and gingival inflammation seen.
Seen after the eruption of the primary teeth. Premature loss of teeth common. All teeth may be lost by 3 yrs of age. Treatment: -. oral prophylaxis. Removal of severely mobile tooth.
Dental curettage. Broad spectrum antibiotics
Localized aggressive periodontitis: (localized Juvenile periodontitis) Actinobacillus actinomycetem comitans, bacterioides and spirochetes. Functional defects of neutrophils and monocytes. More in females. 10 -15 yrs.
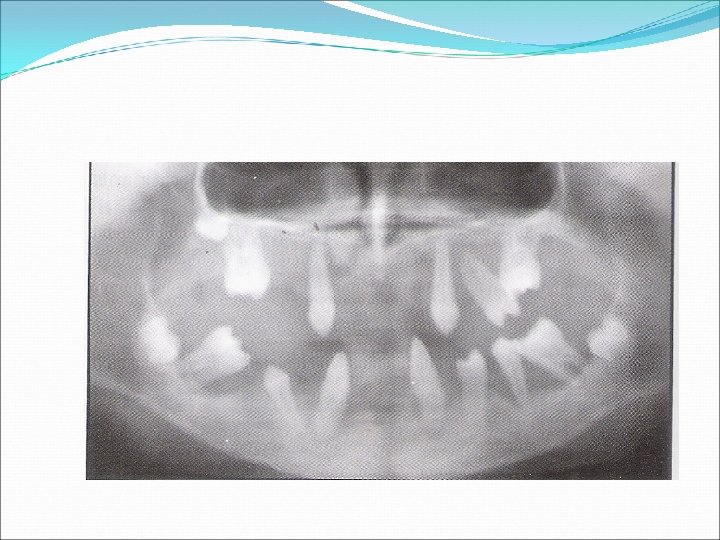
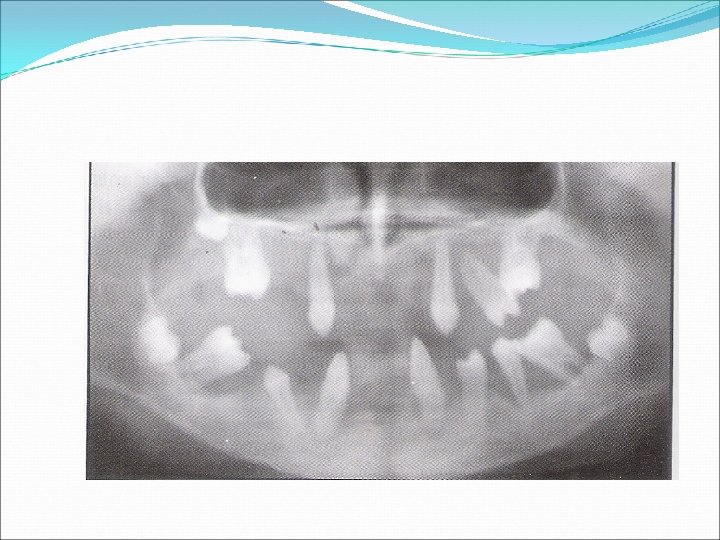
c/f: Rapid and severe bone loss around permanent incisors and first permanent molars. Attachment loss is rapid at 3 times the rate of chronic periodontitis. (1 -4 mm/yr). R/f –Angular bone defects on incisors and arc shaped bone defects on affected permanent molars.

But little amount of plaque or inflammation seen. Treatment: -scaling and root planing. Metronidazole +Amoxicillin or Tetracyclines. Extraction of mobile tooth.
Generalized aggressive periodontitis: (Generalized juvenile periodontitis) Seen at puberty. Affects the entire dentition. Generalized interproximal attachment loss (3 mm). At least three permanent teeth other than first molar and incisors involved.
Porphyromonas gingivalis, prevotella intermedia, actinobacillus actinomycetem comitans. Treatment: -oral prophylaxis Dental curettage Removal of extraction of mobile teeth. Antibiotics.
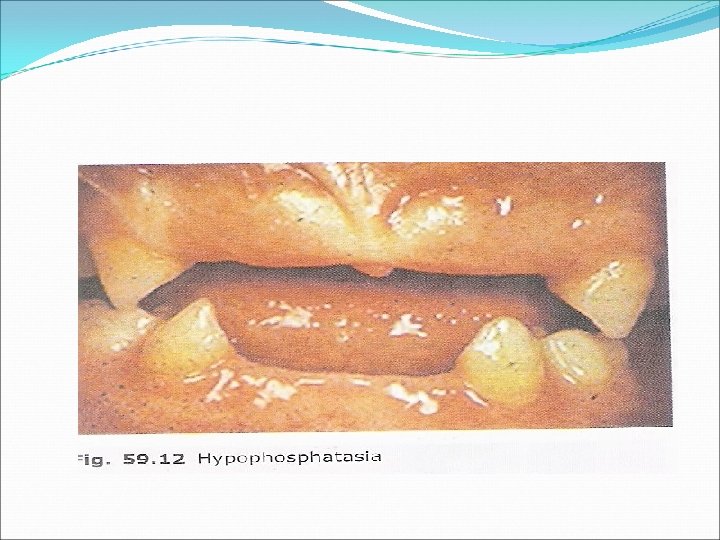
Hypophosphatasia: Genetic disorder. Deficient or defective serum alkaline phosphatase. Premature loss of deciduous teeth to severe bone abnormalities leading to neonatal death. Mild form-early loss of primary teeth-lower incisors.
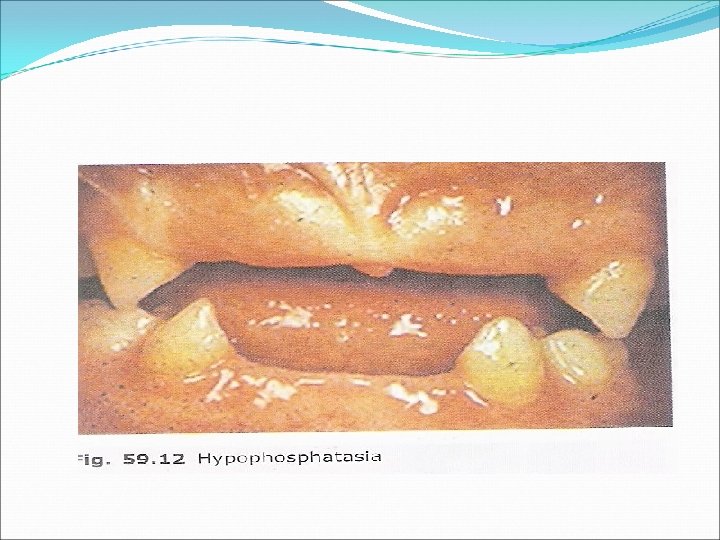
Pulp chambers-abnormally large. Aplasia of root cementum. Permanent teeth are not affected. Treatment: -extraction of mobile primary teeth. Permanent dentition conventional periodontal therapy
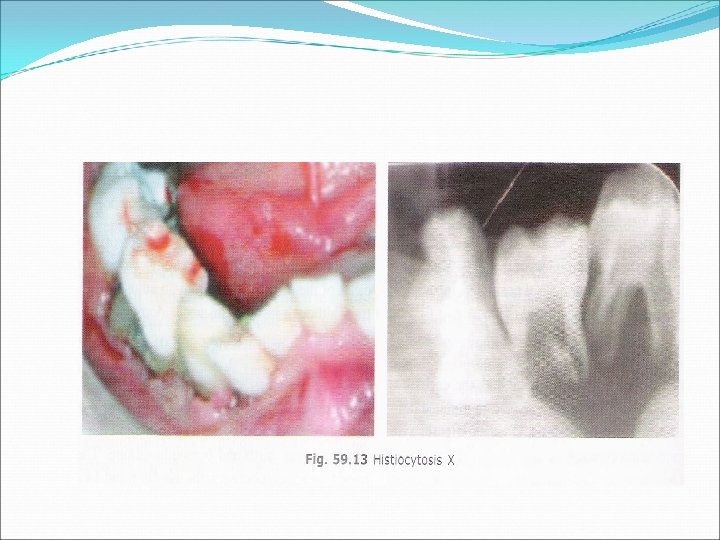
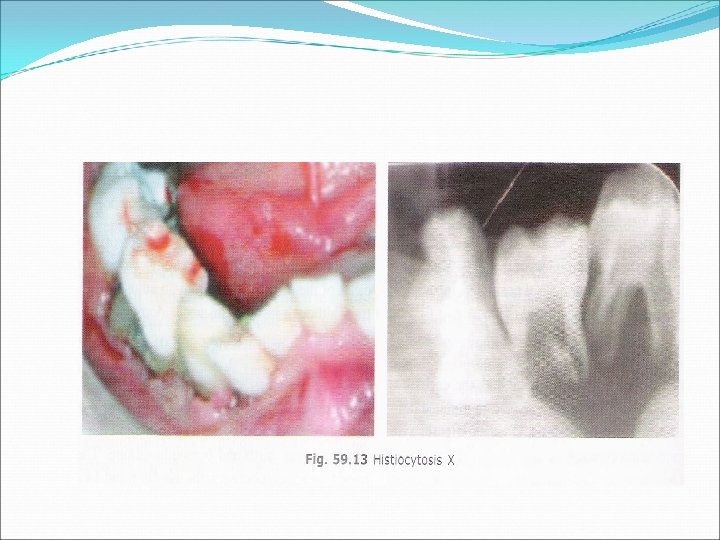
Langerhans cell histiocytosis: -(H. X) Results from disturbances in immunoregulation. Proliferation &dissemination of histiocytecells of Langerhans system Clinical features: Ulcerative necrotizing lesions of gingiva, root exposure, increased mobility of the teeth, halitosis. R/f: -floating teeth. -distruction of alvelor bone
Cyclic neutropenia: Autosomal recessive disorder. Disappearance of neutrophils -3 weeks-after 5 -8 days reappears. C/f: -skin lesions and ear infections. Mucous membrane ulcerations. Severe stomatitis and a profound neutropenia-14 -24 days
Attached papillary and marginal gingiva-enlarged, edematous and erythematous and bleed easily. Cleft formation-marginal gingiva. Bone resorption-extends to the apex. Neutropenic stage-periodontal disase and destruction. Non neutropenic stage-oral health returns.
Normal development & eruption of deciduous teeth Swollen gingiva, migration & mobility of teethexfoliation of teeth. 3 -5 yrs all teeth are lost. Regression of inflammation & gingiva becomes normal.
By age of 13 -14 yrs all Permanent teeth may lost. Treatment: -Antibiotics. Vitamin A -keratinisation of cells.