GI Topics Appendicitis Diverticulitis Obstruction Mesenteric Ischemia Thomas
GI Topics: Appendicitis Diverticulitis Obstruction Mesenteric Ischemia Thomas Vu Brookdale Emergency Medicine Residency Conference July 1 st, 2020
1. 8 yo. M presents with abd pain, has low grade fever and is tender RLQ. Labs show normal wbc. US performed, no evidence of appendicitis. XR KUB shows constipation. • Provider discharges patient with miralax, diagnosis = constipation. Is this appropriate? 2. 85 yo. M h/o diverticulitis presents with left lower abdominal pain, fever, vomiting, and found to be tachycardic in triage. Labs show WBC 13. 5. • Provider provides dose of IV antibiotics, prescribes oral antibiotics and discharges patient. Is this appropriate? 3. 45 yo. F h/o hysterectomy, cholecystectomy p/w abdominal pain. Found to have a large bowel obstruction, WBC 22, elev lactic acid. • Provider believes it to be secondary to previous abdominal surgeries, orders NG tube, admits to medicine with surgery consult. Is this appropriate?
Appendicitis • Background • Clinical Features • Diagnostics • Management
Appendicitis – Background • 250 -300 K appy’s/year in US • Lifetime risk: 12% M, 25% F • Most Common Ages: 10 -19 yo • 1: 1500 pregnancies (#1 non OB surgical emergency in pregnancy)

Appendicitis – Background • Luminal obstruction of appendix, typically by fecalith • Other causes – lymphatic tissue, gallstone, tumor, parasites • Increased pressures, vascular insufficiency; can lead to perforation • Early – visceral innervation, periumbilical/central abdominal discomfort • Later – parietal peritoneal irritation @ RLQ (Mc. Burney’s)

Quiz 1
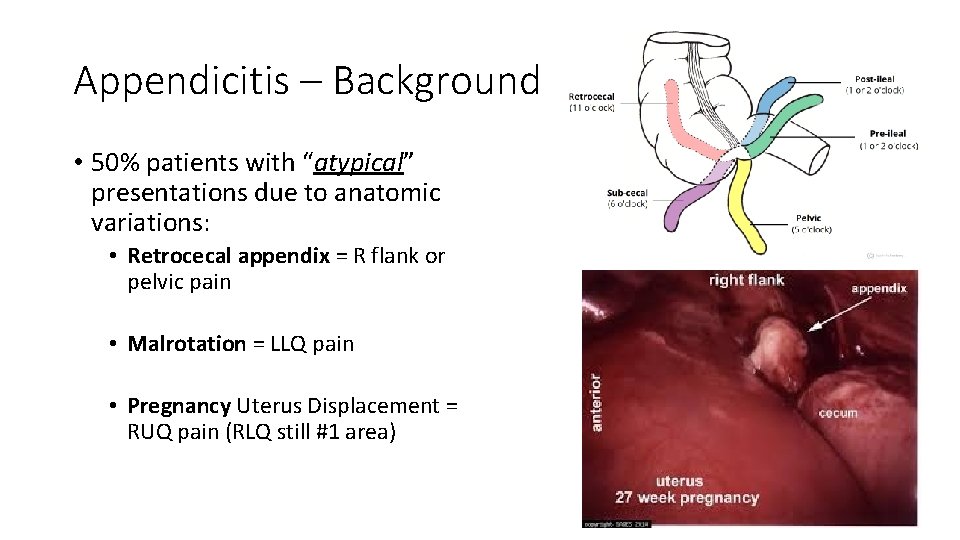
Appendicitis – Background • 50% patients with “atypical” presentations due to anatomic variations: • Retrocecal appendix = R flank or pelvic pain • Malrotation = LLQ pain • Pregnancy Uterus Displacement = RUQ pain (RLQ still #1 area)
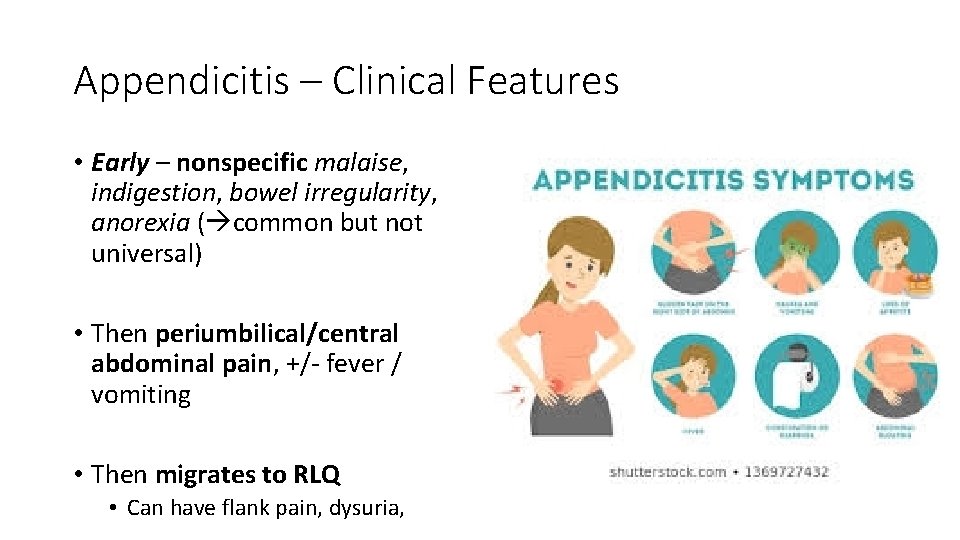
Appendicitis – Clinical Features • Early – nonspecific malaise, indigestion, bowel irregularity, anorexia ( common but not universal) • Then periumbilical/central abdominal pain, +/- fever / vomiting • Then migrates to RLQ • Can have flank pain, dysuria, hematuria if close to urinary tract

Appendicitis – Clinical Features • Worsens with deep inspiration (peritoneal irritation) and movement • Can have pain remittance if perforation (intraluminal obstruction release) • Rebound, involuntary guarding if peritonitis
Quiz 2
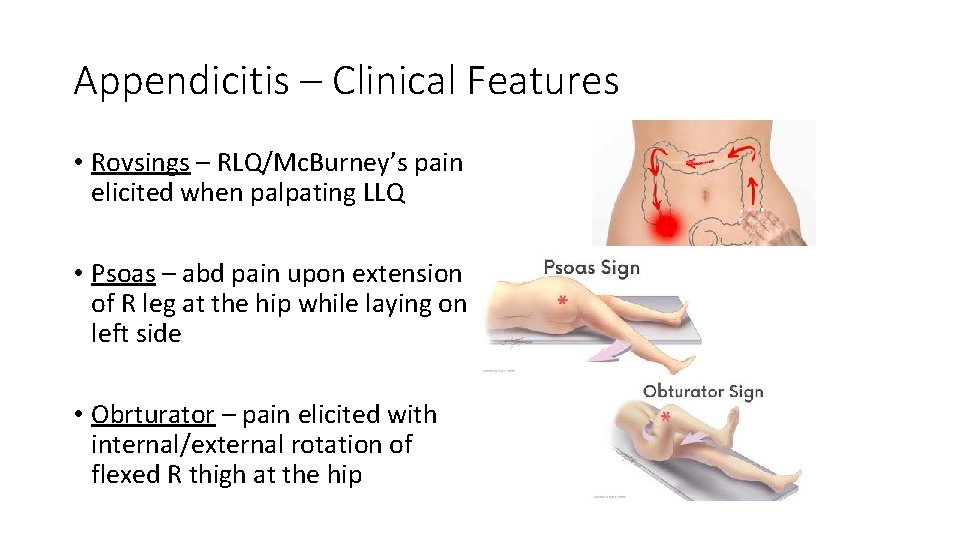
Appendicitis – Clinical Features • Rovsings – RLQ/Mc. Burney’s pain elicited when palpating LLQ • Psoas – abd pain upon extension of R leg at the hip while laying on left side • Obrturator – pain elicited with internal/external rotation of flexed R thigh at the hip

Quiz 3
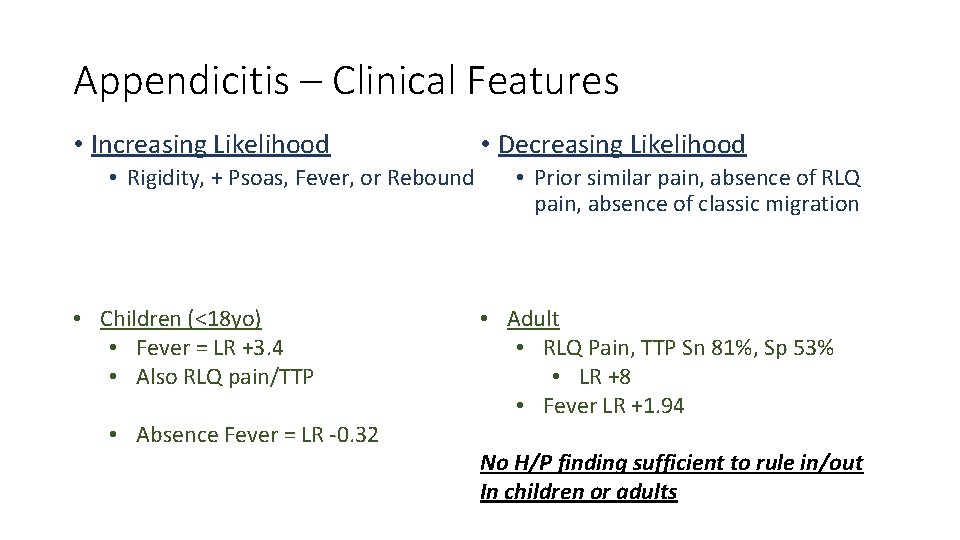
Appendicitis – Clinical Features • Increasing Likelihood • Rigidity, + Psoas, Fever, or Rebound • Children (<18 yo) • Fever = LR +3. 4 • Also RLQ pain/TTP • Absence Fever = LR -0. 32 • Decreasing Likelihood • Prior similar pain, absence of RLQ pain, absence of classic migration • Adult • RLQ Pain, TTP Sn 81%, Sp 53% • LR +8 • Fever LR +1. 94 No H/P finding sufficient to rule in/out In children or adults
Appendicitis – Diagnostics • Still largely a clinical diagnosis • Scoring Systems (Alvarado, Samuel) • Alvarado Sn ~72% compared to clinical judgement 93% of appendicitis as most likely diagnosis

Appendicitis – Diagnostics Labs • WBC • Increase may be earliest marker of inflammation • Normal not uncommon, some also leukopenic • No clear consensus on utility • ESR / CRP • Not high enough Sn / Sp • Combined WBC + CRP: Sn 98% but not Sp • Adjunts: UA, Upreg

Quiz 4
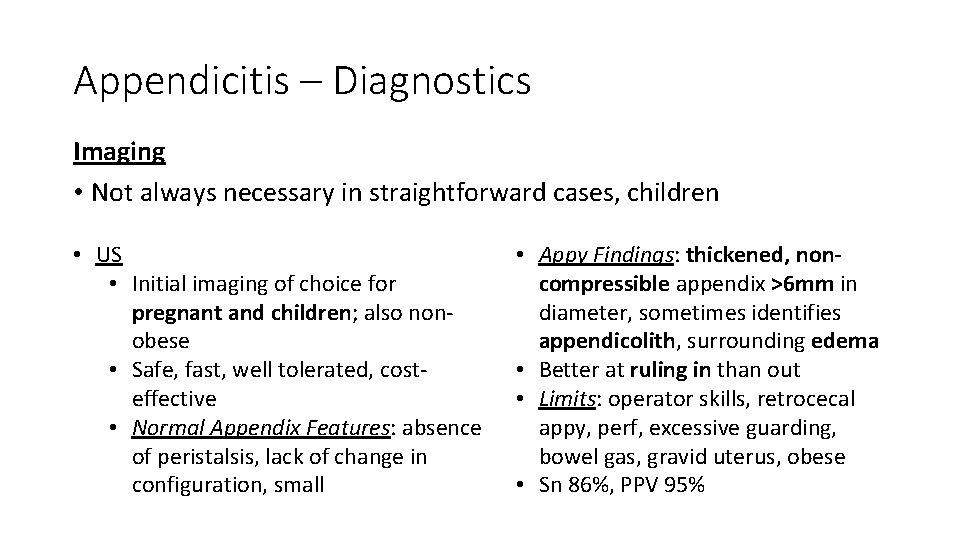
Appendicitis – Diagnostics Imaging • Not always necessary in straightforward cases, children • US • Initial imaging of choice for pregnant and children; also nonobese • Safe, fast, well tolerated, costeffective • Normal Appendix Features: absence of peristalsis, lack of change in configuration, small • Appy Findings: thickened, noncompressible appendix >6 mm in diameter, sometimes identifies appendicolith, surrounding edema • Better at ruling in than out • Limits: operator skills, retrocecal appy, perf, excessive guarding, bowel gas, gravid uterus, obese • Sn 86%, PPV 95%
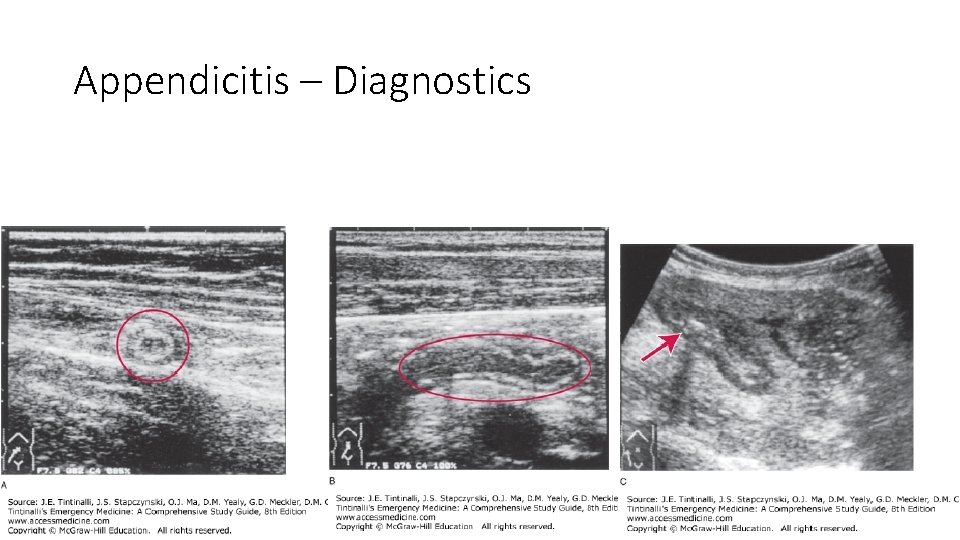
Appendicitis – Diagnostics
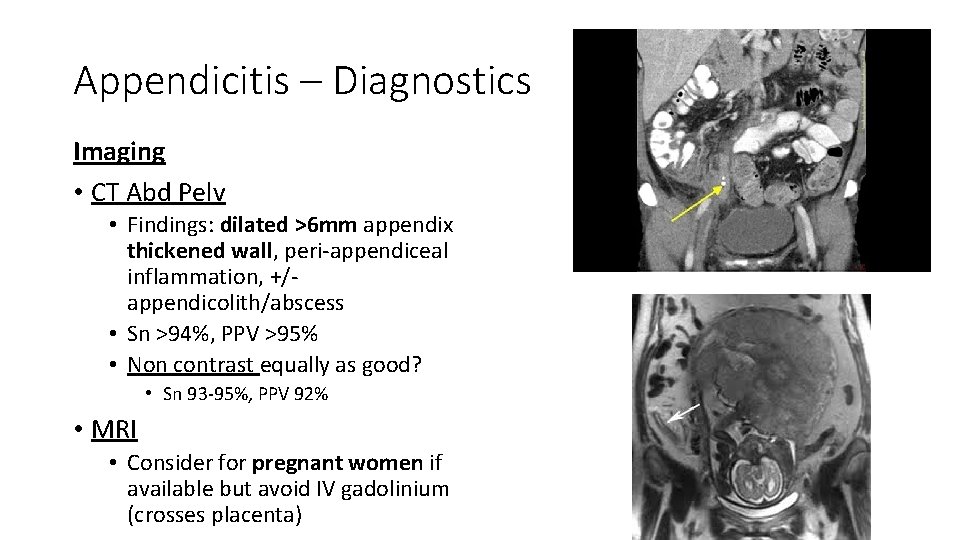
Appendicitis – Diagnostics Imaging • CT Abd Pelv • Findings: dilated >6 mm appendix thickened wall, peri-appendiceal inflammation, +/appendicolith/abscess • Sn >94%, PPV >95% • Non contrast equally as good? • Sn 93 -95%, PPV 92% • MRI • Consider for pregnant women if available but avoid IV gadolinium (crosses placenta)

Quiz
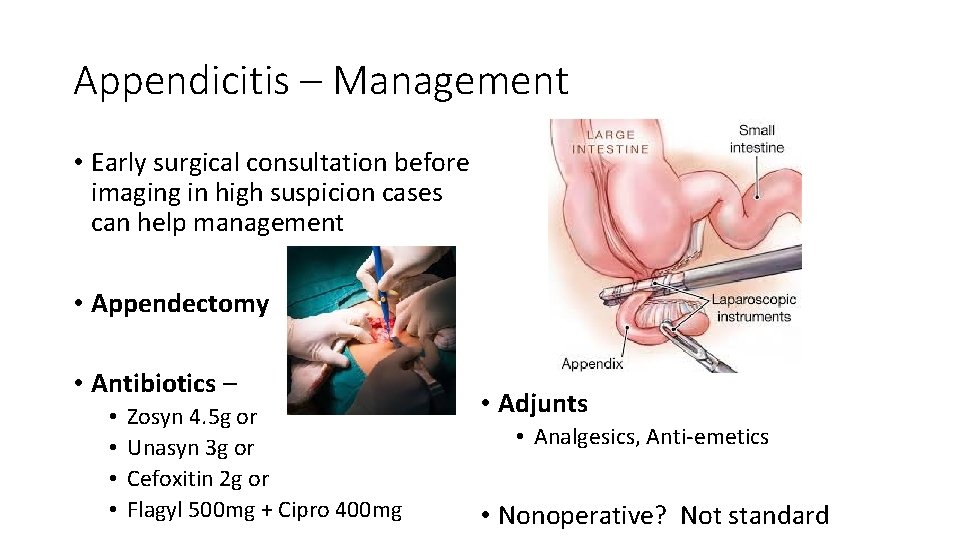
Appendicitis – Management • Early surgical consultation before imaging in high suspicion cases can help management • Appendectomy • Antibiotics – • • Zosyn 4. 5 g or Unasyn 3 g or Cefoxitin 2 g or Flagyl 500 mg + Cipro 400 mg • Adjunts • Analgesics, Anti-emetics • Nonoperative? Not standard
Appendicitis – Management Disposition: • Surgery if diagnosed • Can be same-day surgery and discharge without admission • Not clear diagnosis but suspicion stays high, extended ED or hospital stay with serial exams • Alternatively if stable & reliable can be d/c if scheduled return to ED or PCP (w/in 12 hrs) • Able to tolerate pain and PO • Special considerations: Pregnant women, children

Quiz
Welcome to Brookdale Dr. Rebecca Siegel!
Quiz
Welcome to Brookdale Dr. Bahar Pourshariati!
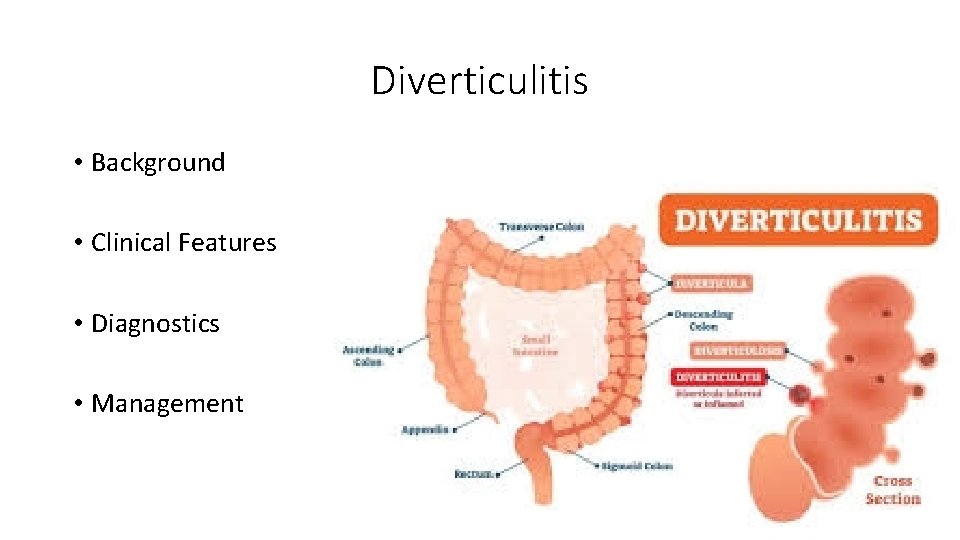
Diverticulitis • Background • Clinical Features • Diagnostics • Management
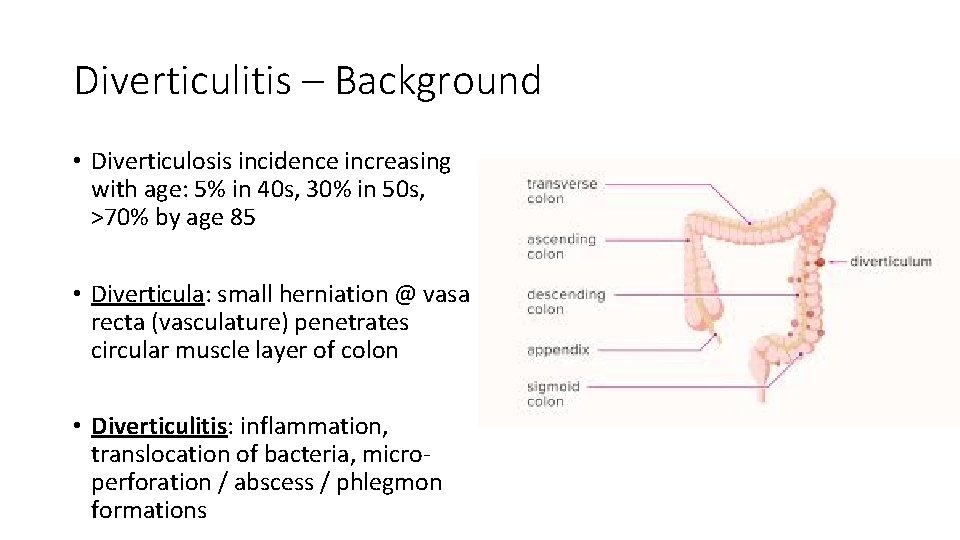
Diverticulitis – Background • Diverticulosis incidence increasing with age: 5% in 40 s, 30% in 50 s, >70% by age 85 • Diverticula: small herniation @ vasa recta (vasculature) penetrates circular muscle layer of colon • Diverticulitis: inflammation, translocation of bacteria, microperforation / abscess / phlegmon formations
Diverticulitis – Background • Most common bacteria – Bacteroides, Peptostreptococcus, Clostridium, Fusobacterium, E coli & other G neg rods • Altered bowel motility leads to high intraluminal colonic pressures, diverticula formation • Risk factors: smoking, obesity, lack of active lifestyle • US almost exclusively left-sided desc/sigmoid colon

Quiz 5

Diverticulitis – Clinical Features • Classic – LLQ, fever, leukocytosis • RLQ can be in Asian populations • Intermittent or constant • Change in bowel habits (diarrhea or constipation), n/v, anorexia, urinary sx • TTP mild to moderate, or peritonitis with rebound/guarding

Quiz 6
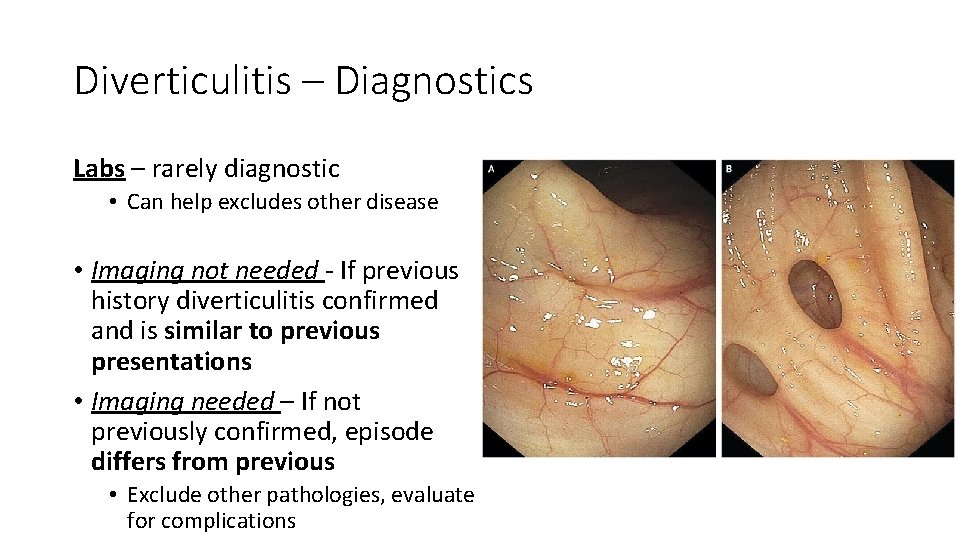
Diverticulitis – Diagnostics Labs – rarely diagnostic • Can help excludes other disease • Imaging not needed - If previous history diverticulitis confirmed and is similar to previous presentations • Imaging needed – If not previously confirmed, episode differs from previous • Exclude other pathologies, evaluate for complications
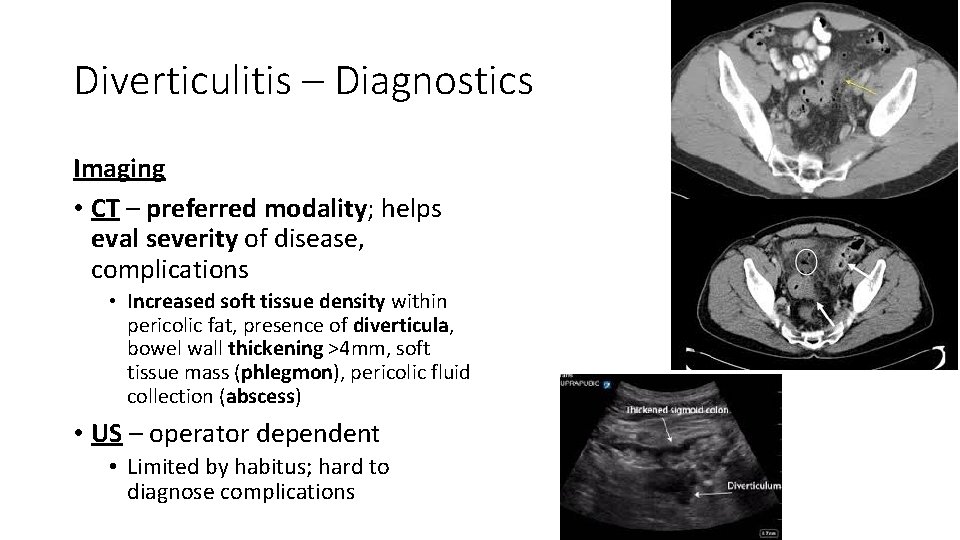
Diverticulitis – Diagnostics Imaging • CT – preferred modality; helps eval severity of disease, complications • Increased soft tissue density within pericolic fat, presence of diverticula, bowel wall thickening >4 mm, soft tissue mass (phlegmon), pericolic fluid collection (abscess) • US – operator dependent • Limited by habitus; hard to diagnose complications
Diverticulitis – Management

Quiz 7
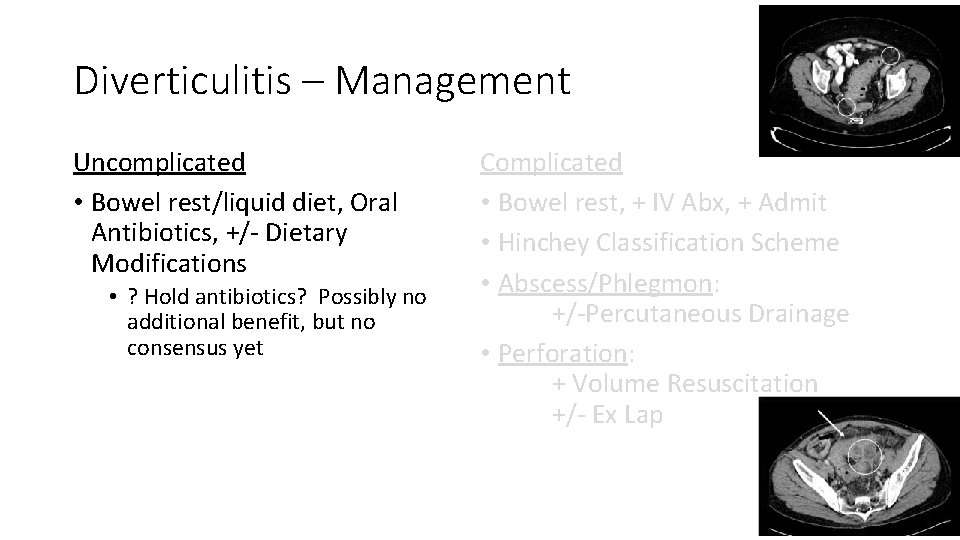
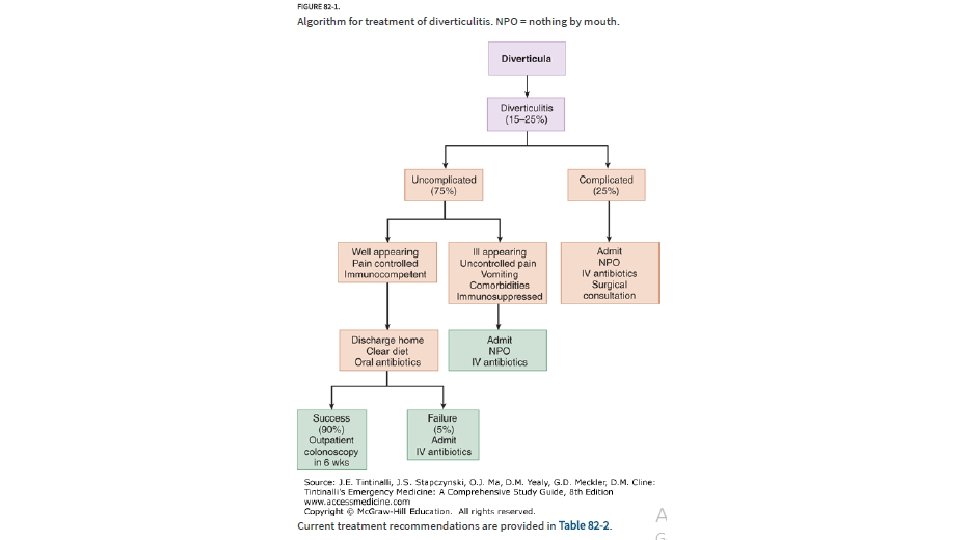
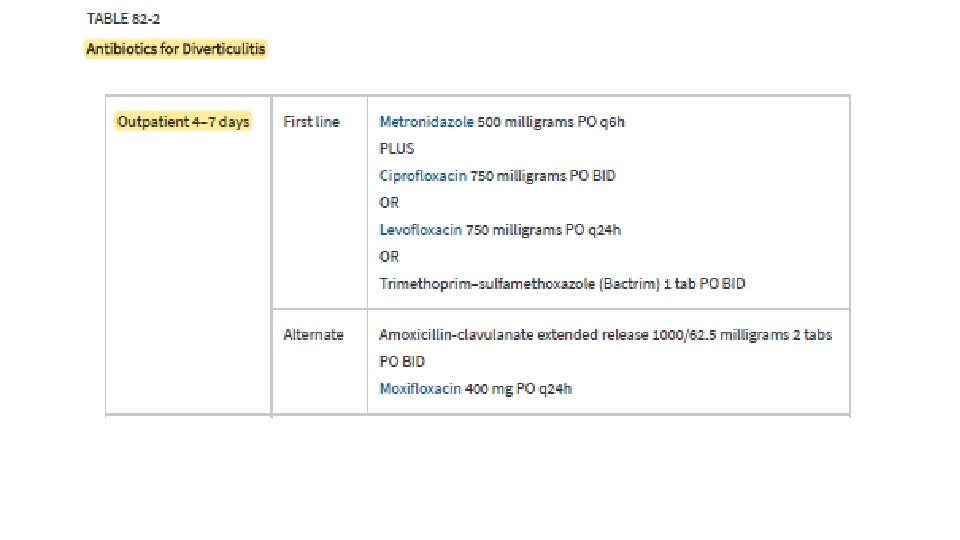
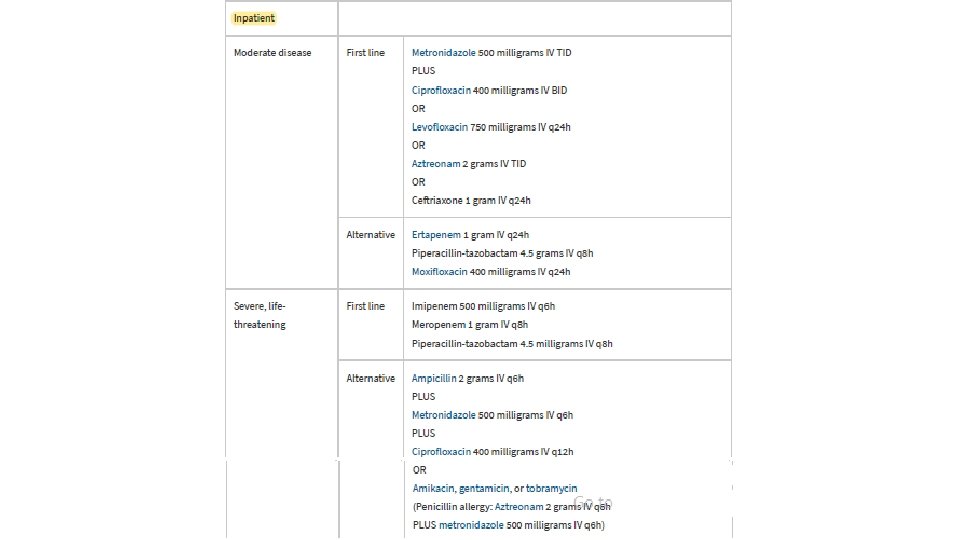
Diverticulitis – Management Uncomplicated • Bowel rest/liquid diet, Oral Antibiotics, +/- Dietary Modifications • ? Hold antibiotics? Possibly no additional benefit, but no consensus yet Complicated • Bowel rest, + IV Abx, + Admit • Hinchey Classification Scheme • Abscess/Phlegmon: +/-Percutaneous Drainage • Perforation: + Volume Resuscitation +/- Ex Lap
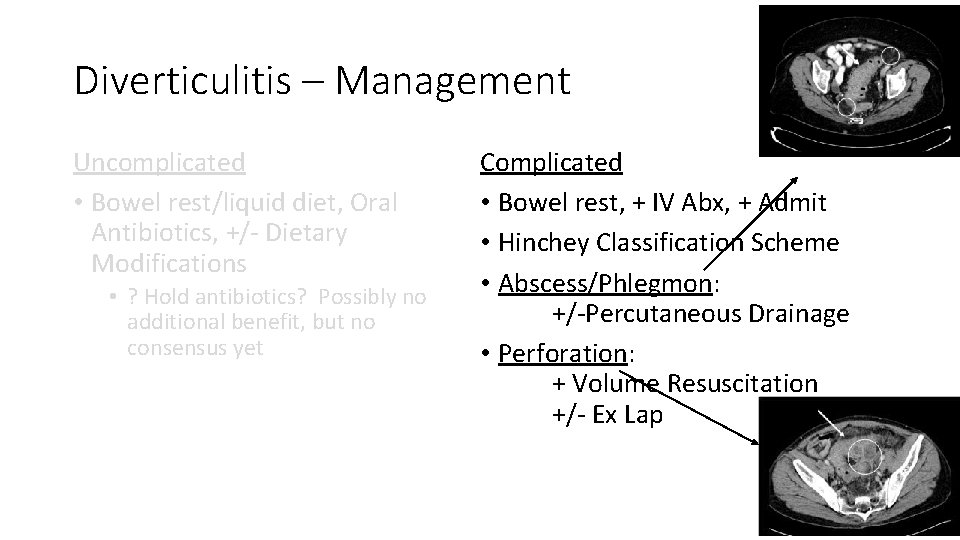
Diverticulitis – Management Uncomplicated • Bowel rest/liquid diet, Oral Antibiotics, +/- Dietary Modifications • ? Hold antibiotics? Possibly no additional benefit, but no consensus yet Complicated • Bowel rest, + IV Abx, + Admit • Hinchey Classification Scheme • Abscess/Phlegmon: +/-Percutaneous Drainage • Perforation: + Volume Resuscitation +/- Ex Lap
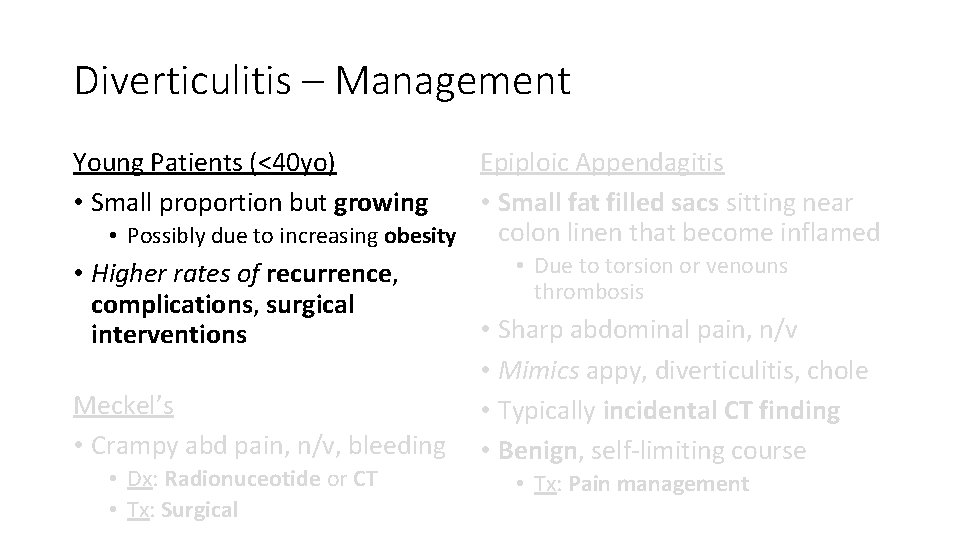
Diverticulitis – Management Epiploic Appendagitis • Small fat filled sacs sitting near colon linen that become inflamed • Possibly due to increasing obesity • Due to torsion or venouns • Higher rates of recurrence, thrombosis complications, surgical • Sharp abdominal pain, n/v interventions • Mimics appy, diverticulitis, chole Meckel’s • Typically incidental CT finding • Crampy abd pain, n/v, bleeding • Benign, self-limiting course Young Patients (<40 yo) • Small proportion but growing • Dx: Radionuceotide or CT • Tx: Surgical • Tx: Pain management
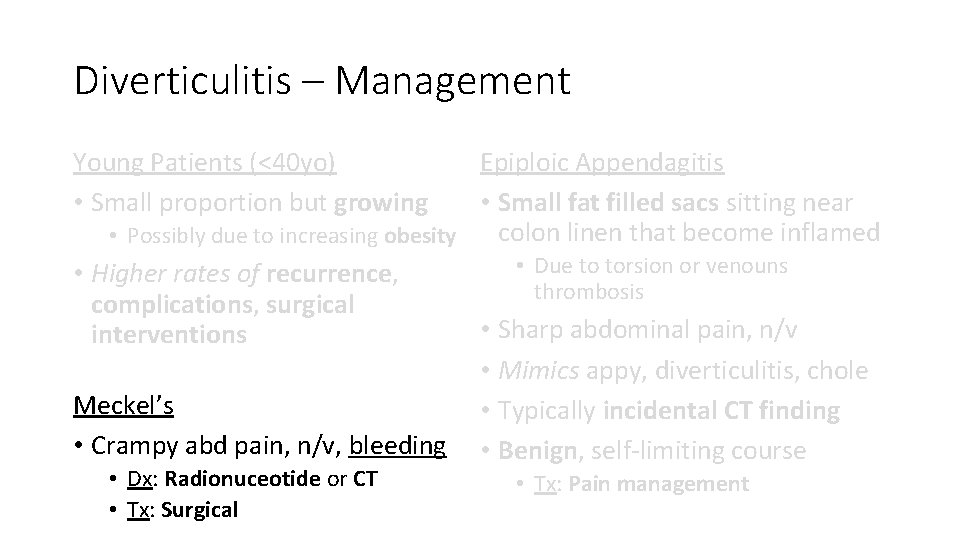
Diverticulitis – Management Epiploic Appendagitis • Small fat filled sacs sitting near colon linen that become inflamed • Possibly due to increasing obesity • Due to torsion or venouns • Higher rates of recurrence, thrombosis complications, surgical • Sharp abdominal pain, n/v interventions • Mimics appy, diverticulitis, chole Meckel’s • Typically incidental CT finding • Crampy abd pain, n/v, bleeding • Benign, self-limiting course Young Patients (<40 yo) • Small proportion but growing • Dx: Radionuceotide or CT • Tx: Surgical • Tx: Pain management
Diverticulitis – Management Epiploic Appendagitis • Small fat filled sacs sitting near colon linen that become inflamed • Possibly due to increasing obesity • Due to torsion or venouns • Higher rates of recurrence, thrombosis complications, surgical • Sharp abdominal pain, n/v interventions • Mimics appy, diverticulitis, chole Meckel’s • Typically incidental CT finding • Crampy abd pain, n/v, bleeding • Benign, self-limiting course Young Patients (<40 yo) • Small proportion but growing • Dx: Radionuceotide or CT • Tx: Surgical • Tx: Pain management

Quiz
Welcome to Brookdale Dr. Rasheeda Rickman!

Quiz
Welcome to Brookdale Dr. Bannet Muhoozi!
Obstruction • Background • Clinical Features • Diagnostics • Management
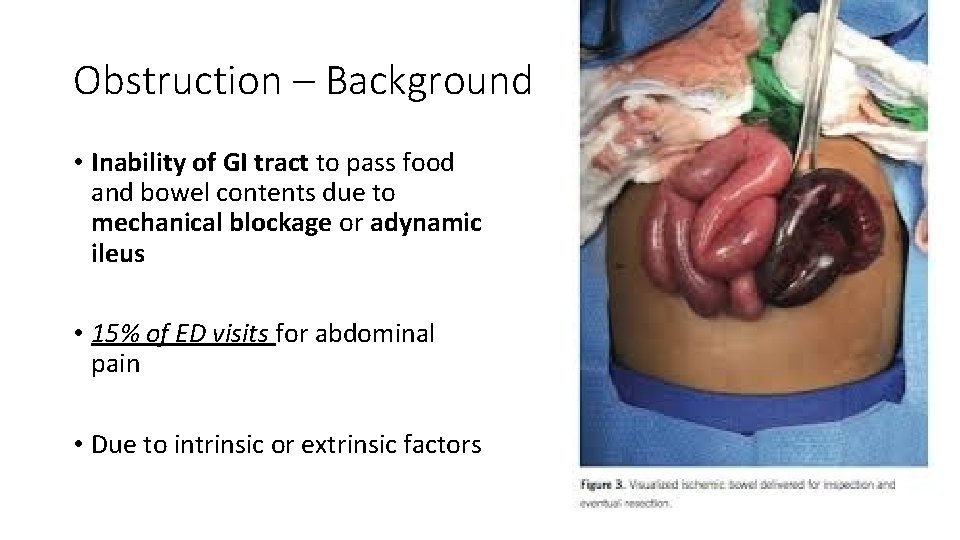
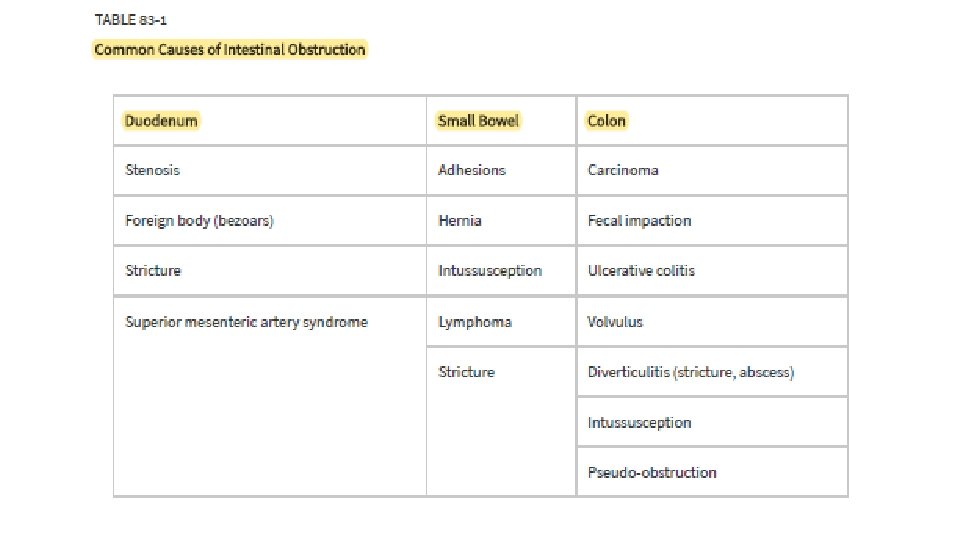
Obstruction – Background • Inability of GI tract to pass food and bowel contents due to mechanical blockage or adynamic ileus • 15% of ED visits for abdominal pain • Due to intrinsic or extrinsic factors
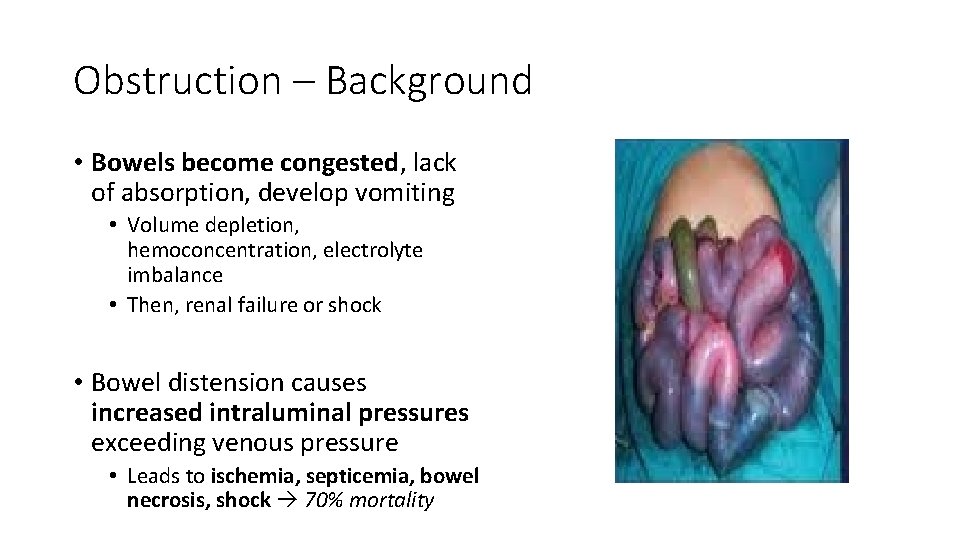
Obstruction – Background • Bowels become congested, lack of absorption, develop vomiting • Volume depletion, hemoconcentration, electrolyte imbalance • Then, renal failure or shock • Bowel distension causes increased intraluminal pressures exceeding venous pressure • Leads to ischemia, septicemia, bowel necrosis, shock 70% mortality
Quiz 8
Obstruction – Background Small Bowel Obstruction • 4 x more common than LBO Large Bowel Obstruction • #1 Adhesions (weeks to months, • #1 Neoplasms years after surgery) • Rarely adhesions • #2 Hernia Incarceration • Other: Diverticulitis (Excess Edema), Sigmoid Volvulus • Other: Cancer, Polyps, Bariatric (Elderly, Bedridden, Psych, or on surgery, Gallstones, Anticholinergics) Lymphomas/Intussusception, Bezoars, Radiation Enteritis, Trauma
Obstruction – Background Small Bowel Obstruction • 4 x more common than LBO Large Bowel Obstruction • #1 Adhesions (weeks to months, • #1 Neoplasms years after surgery) • Rarely adhesions • #2 Hernia Incarceration • Other: Diverticulitis (Excess Edema), Sigmoid Volvulus • Other: Cancer, Polyps, Bariatric (Elderly, Bedridden, Psych, or on surgery, Gallstones, Anticholinergics) Lymphomas/Inutssusception, Bezoars, Radiation Enteritis, Trauma

Quiz
• Coronal views
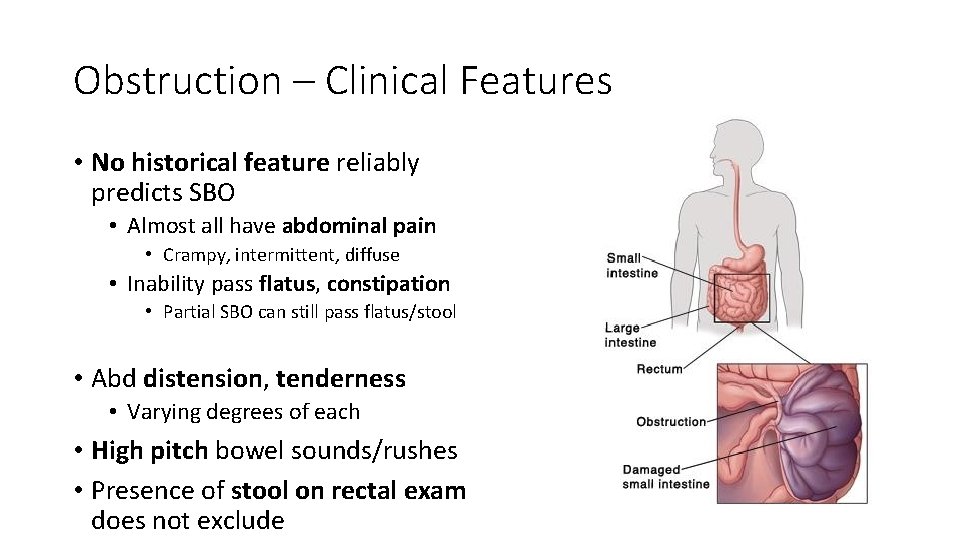
Obstruction – Clinical Features • No historical feature reliably predicts SBO • Almost all have abdominal pain • Crampy, intermittent, diffuse • Inability pass flatus, constipation • Partial SBO can still pass flatus/stool • Abd distension, tenderness • Varying degrees of each • High pitch bowel sounds/rushes • Presence of stool on rectal exam does not exclude
Obstruction – Diagnostics Labs • Screening CBC and Chem • Very elevated WBC can suggest bowel gangrene, abscess, peritonitis, mesenteric vascular occlusion • Chem – can show vol depletion • Procalcitonin – may predict bowel ischemia
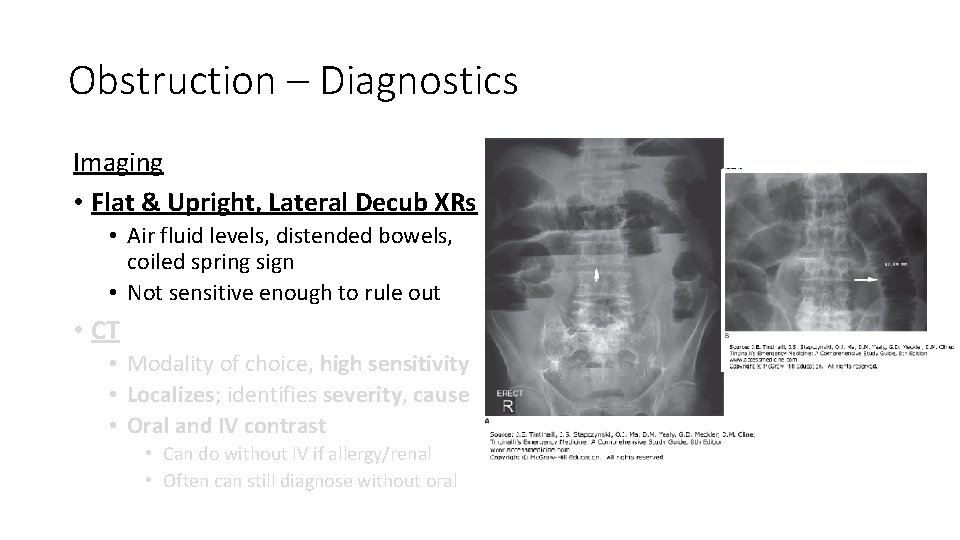
Obstruction – Diagnostics Imaging • Flat & Upright, Lateral Decub XRs • Air fluid levels, distended bowels, coiled spring sign • Not sensitive enough to rule out • CT • Modality of choice, high sensitivity • Localizes; identifies severity, cause • Oral and IV contrast • Can do without IV if allergy/renal • Often can still diagnose without oral
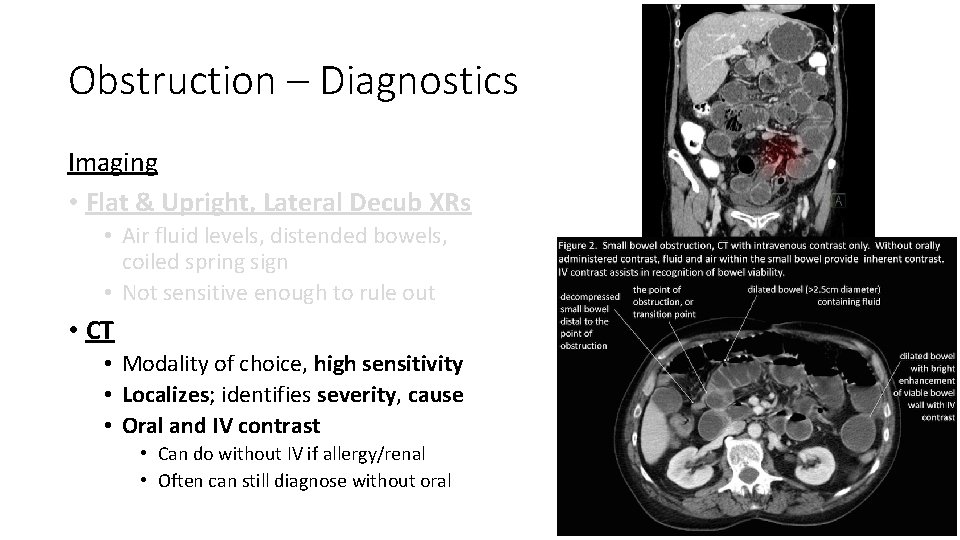
Obstruction – Diagnostics Imaging • Flat & Upright, Lateral Decub XRs • Air fluid levels, distended bowels, coiled spring sign • Not sensitive enough to rule out • CT • Modality of choice, high sensitivity • Localizes; identifies severity, cause • Oral and IV contrast • Can do without IV if allergy/renal • Often can still diagnose without oral

Quiz 9
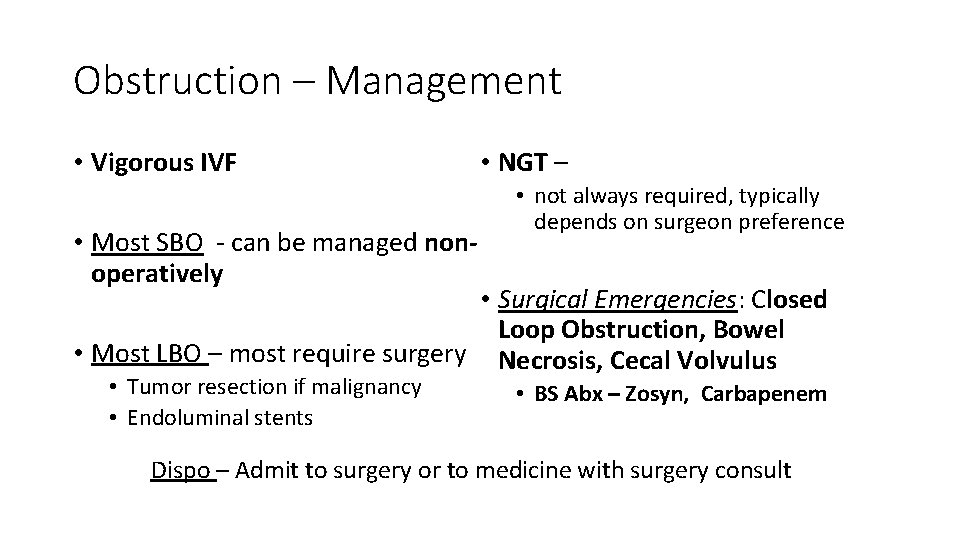
Obstruction – Management • Vigorous IVF • Most SBO - can be managed nonoperatively • NGT – • not always required, typically depends on surgeon preference • Surgical Emergencies: Closed Loop Obstruction, Bowel • Most LBO – most require surgery Necrosis, Cecal Volvulus • Tumor resection if malignancy • Endoluminal stents • BS Abx – Zosyn, Carbapenem Dispo – Admit to surgery or to medicine with surgery consult

Quiz
Welcome (Back) to Brookdale Dr. Amy Plasencia!

Quiz
Welcome to Brookdale Dr. Shruti Kamat!
Mesenteric Ischemia • Background • Clinical Features • Diagnostics • Management
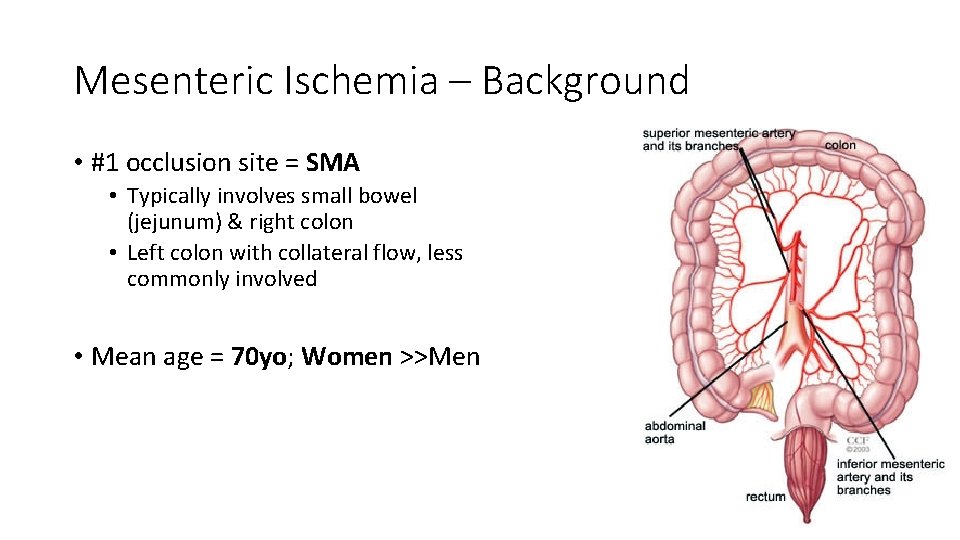
Mesenteric Ischemia – Background • #1 occlusion site = SMA • Typically involves small bowel (jejunum) & right colon • Left colon with collateral flow, less commonly involved • Mean age = 70 yo; Women >>Men
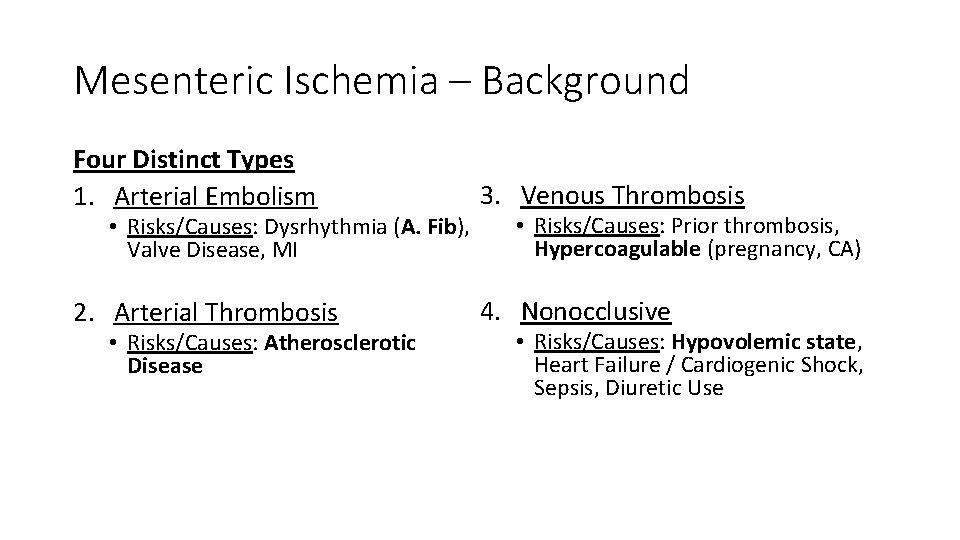
Mesenteric Ischemia – Background Four Distinct Types 1. Arterial Embolism 3. Venous Thrombosis 2. Arterial Thrombosis 4. Nonocclusive • Risks/Causes: Dysrhythmia (A. Fib), Valve Disease, MI • Risks/Causes: Atherosclerotic Disease • Risks/Causes: Prior thrombosis, Hypercoagulable (pregnancy, CA) • Risks/Causes: Hypovolemic state, Heart Failure / Cardiogenic Shock, Sepsis, Diuretic Use

Quiz 10
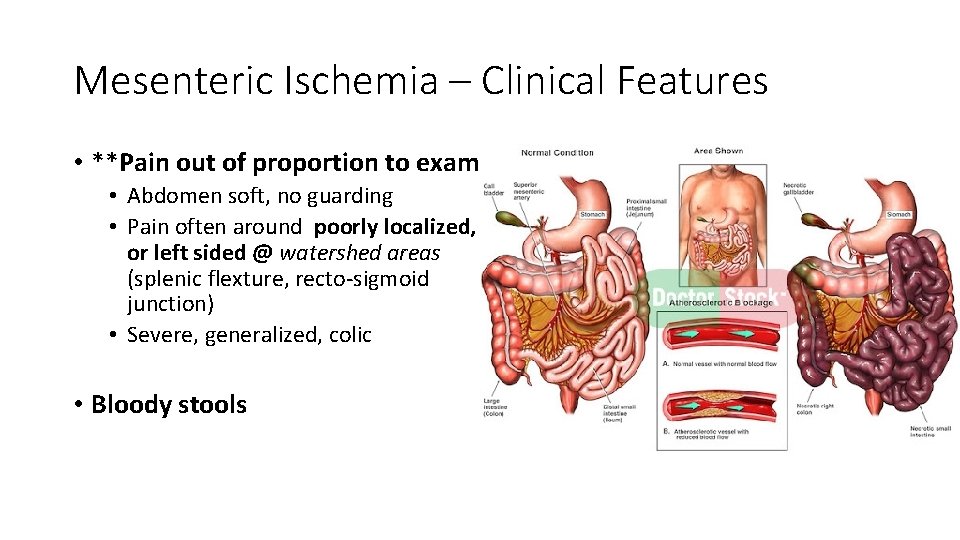
Mesenteric Ischemia – Clinical Features • **Pain out of proportion to exam • Abdomen soft, no guarding • Pain often around poorly localized, or left sided @ watershed areas (splenic flexture, recto-sigmoid junction) • Severe, generalized, colic • Bloody stools
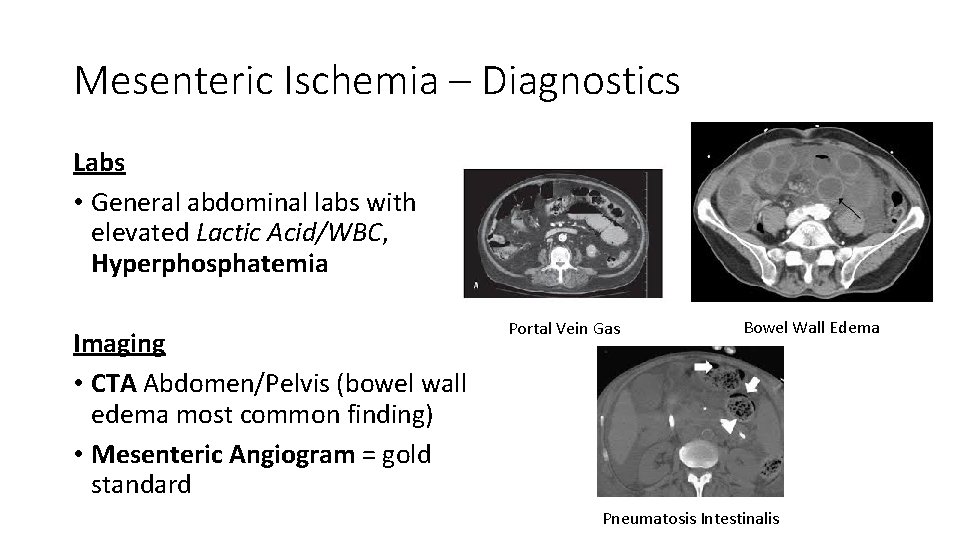
Mesenteric Ischemia – Diagnostics Labs • General abdominal labs with elevated Lactic Acid/WBC, Hyperphosphatemia Imaging • CTA Abdomen/Pelvis (bowel wall edema most common finding) • Mesenteric Angiogram = gold standard Portal Vein Gas Bowel Wall Edema Pneumatosis Intestinalis
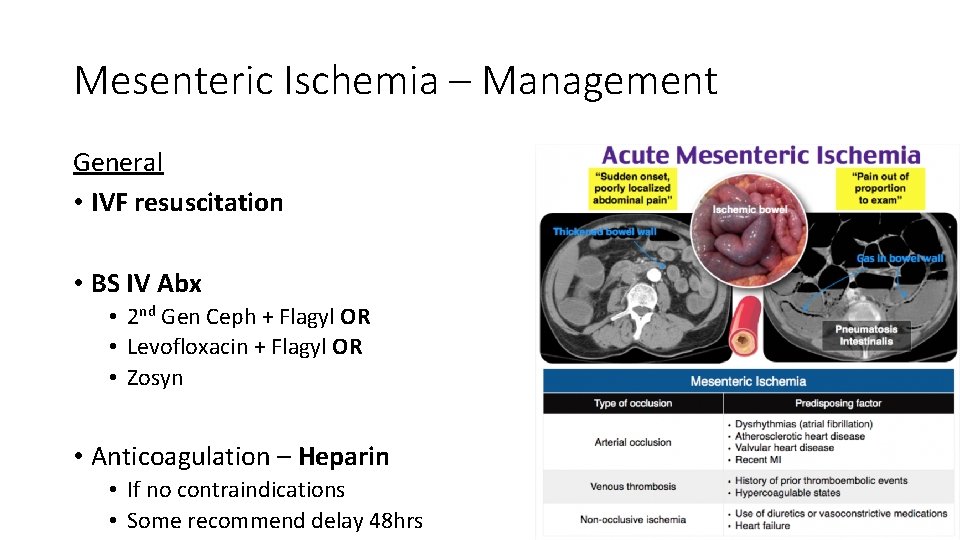
Mesenteric Ischemia – Management General • IVF resuscitation • BS IV Abx • 2 nd Gen Ceph + Flagyl OR • Levofloxacin + Flagyl OR • Zosyn • Anticoagulation – Heparin • If no contraindications • Some recommend delay 48 hrs

Quiz 11
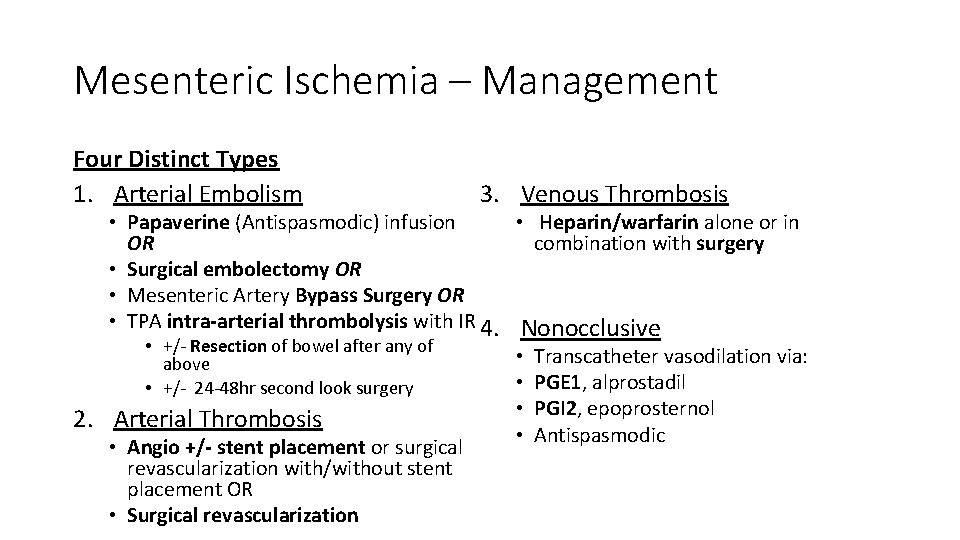
Mesenteric Ischemia – Management Four Distinct Types 1. Arterial Embolism 3. Venous Thrombosis • Papaverine (Antispasmodic) infusion • Heparin/warfarin alone or in OR combination with surgery • Surgical embolectomy OR • Mesenteric Artery Bypass Surgery OR • TPA intra-arterial thrombolysis with IR 4. Nonocclusive • +/- Resection of bowel after any of above • +/- 24 -48 hr second look surgery 2. Arterial Thrombosis • Angio +/- stent placement or surgical revascularization with/without stent placement OR • Surgical revascularization • • Transcatheter vasodilation via: PGE 1, alprostadil PGI 2, epoprosternol Antispasmodic
Mesenteric Ischemia – Management Dispo • Admit with consult of one or more of the following: • IR • Vascular • Surgery

Quiz
Welcome to Brookdale Dr. Abrar Justin Ahmed!

Quiz

Welcome to Brookdale Dr. Brandon Buchel!

Quiz
Welcome to Brookdale Dr. Ama Asare!
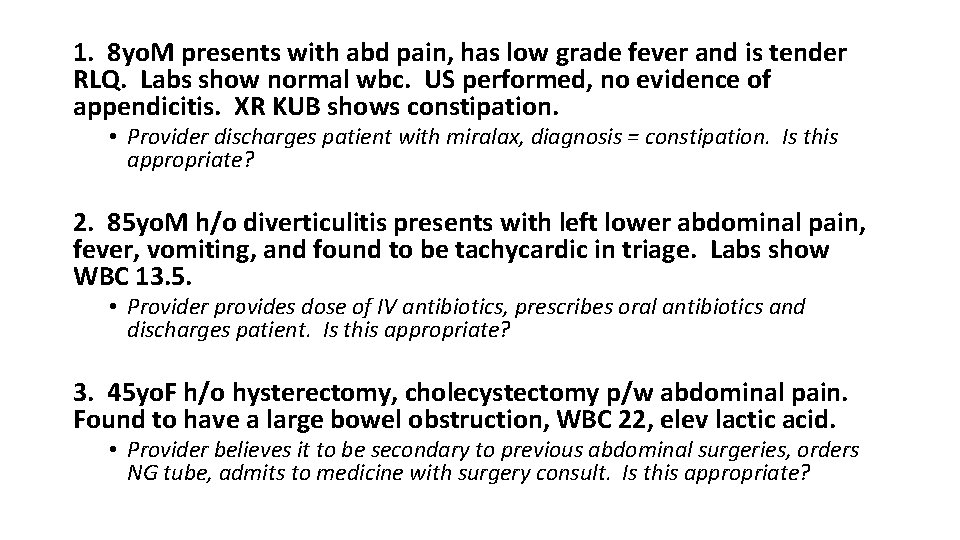
1. 8 yo. M presents with abd pain, has low grade fever and is tender RLQ. Labs show normal wbc. US performed, no evidence of appendicitis. XR KUB shows constipation. • Provider discharges patient with miralax, diagnosis = constipation. Is this appropriate? 2. 85 yo. M h/o diverticulitis presents with left lower abdominal pain, fever, vomiting, and found to be tachycardic in triage. Labs show WBC 13. 5. • Provider provides dose of IV antibiotics, prescribes oral antibiotics and discharges patient. Is this appropriate? 3. 45 yo. F h/o hysterectomy, cholecystectomy p/w abdominal pain. Found to have a large bowel obstruction, WBC 22, elev lactic acid. • Provider believes it to be secondary to previous abdominal surgeries, orders NG tube, admits to medicine with surgery consult. Is this appropriate?
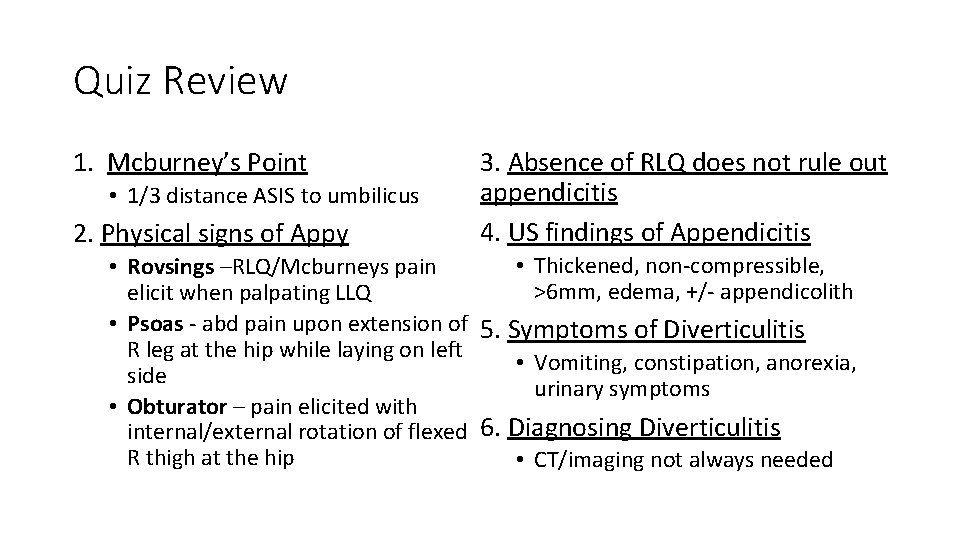
Quiz Review 1. Mcburney’s Point • 1/3 distance ASIS to umbilicus 2. Physical signs of Appy 3. Absence of RLQ does not rule out appendicitis 4. US findings of Appendicitis • Thickened, non-compressible, • Rovsings –RLQ/Mcburneys pain >6 mm, edema, +/- appendicolith elicit when palpating LLQ • Psoas - abd pain upon extension of 5. Symptoms of Diverticulitis R leg at the hip while laying on left • Vomiting, constipation, anorexia, side urinary symptoms • Obturator – pain elicited with internal/external rotation of flexed 6. Diagnosing Diverticulitis R thigh at the hip • CT/imaging not always needed
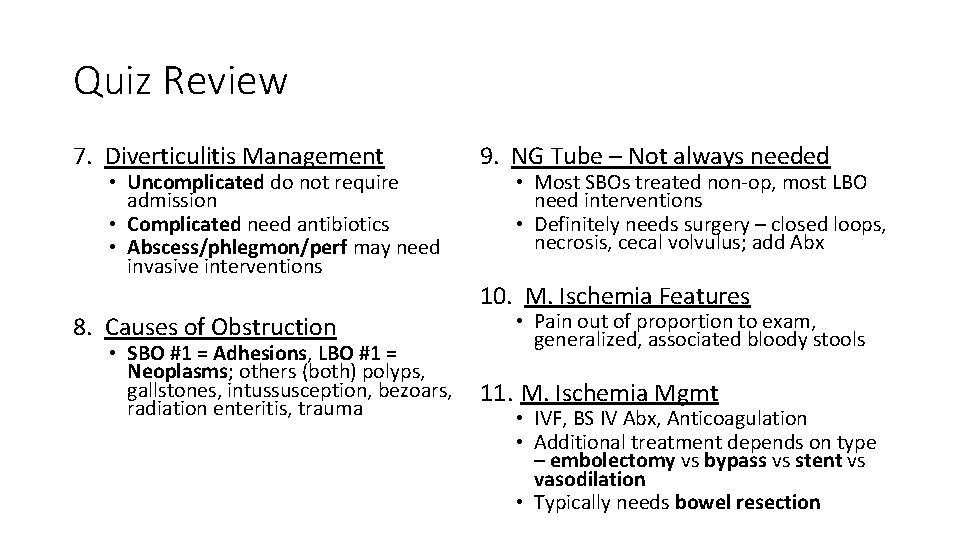
Quiz Review 7. Diverticulitis Management • Uncomplicated do not require admission • Complicated need antibiotics • Abscess/phlegmon/perf may need invasive interventions 9. NG Tube – Not always needed • Most SBOs treated non-op, most LBO need interventions • Definitely needs surgery – closed loops, necrosis, cecal volvulus; add Abx 10. M. Ischemia Features 8. Causes of Obstruction • SBO #1 = Adhesions, LBO #1 = Neoplasms; others (both) polyps, gallstones, intussusception, bezoars, radiation enteritis, trauma • Pain out of proportion to exam, generalized, associated bloody stools 11. M. Ischemia Mgmt • IVF, BS IV Abx, Anticoagulation • Additional treatment depends on type – embolectomy vs bypass vs stent vs vasodilation • Typically needs bowel resection

Quiz
Resources • Tintinalli 8 e Chapter 81 – Acute Appendicitis • Tintinalli 8 e Chapter 82 – Diverticulitis • Tintinalli 8 e Chapter 83 – Bowel Obstruction
- Slides: 89