GI MOTILITY GI smooth muscles are unitary type





- Slides: 46
GI MOTILITY
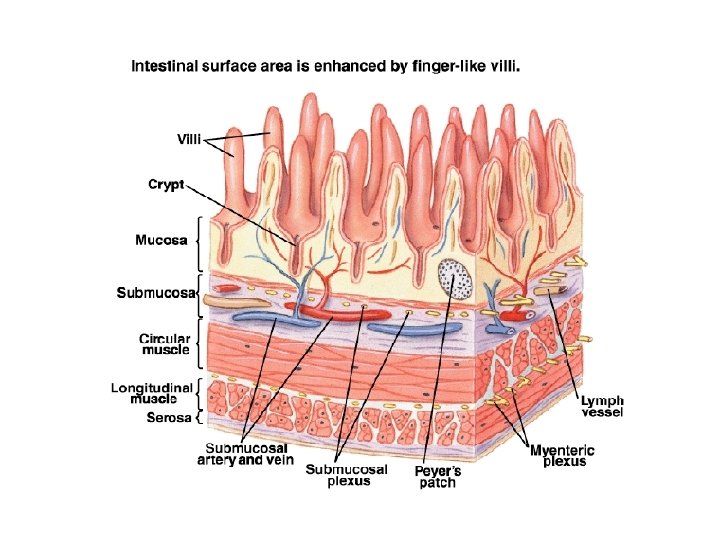
• GI smooth muscles are unitary type • Have numerous gap junctions- synctial nature of smooth muscle. • Pacemaker tissue-interstitial cells of Cajal. • Contract spontaneously without external neural innervation. • Contract when stretched
BASIC ELECTRICAL RHYTHM AND SLOW WAVES • Electrical slow waves are wide spontaneous rhythmic fluctuations in the membrane potential ranging between -65 to -45 m. V. • PHASES
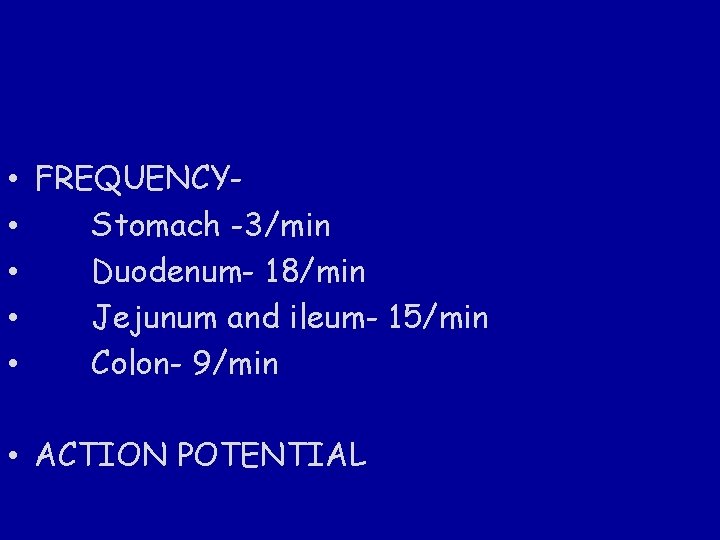
• FREQUENCY • Stomach -3/min • Duodenum- 18/min • Jejunum and ileum- 15/min • Colon- 9/min • ACTION POTENTIAL
Functions: • Mixing of food • Spreading of chyme • Propulsive movement
Types of movement: 1. Rhythmic segmental movements 2. Peristalsis 3. Migratory motor complex
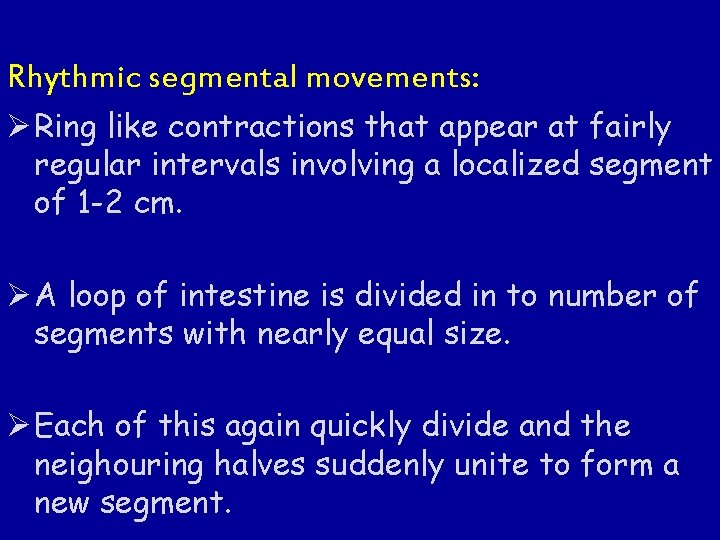
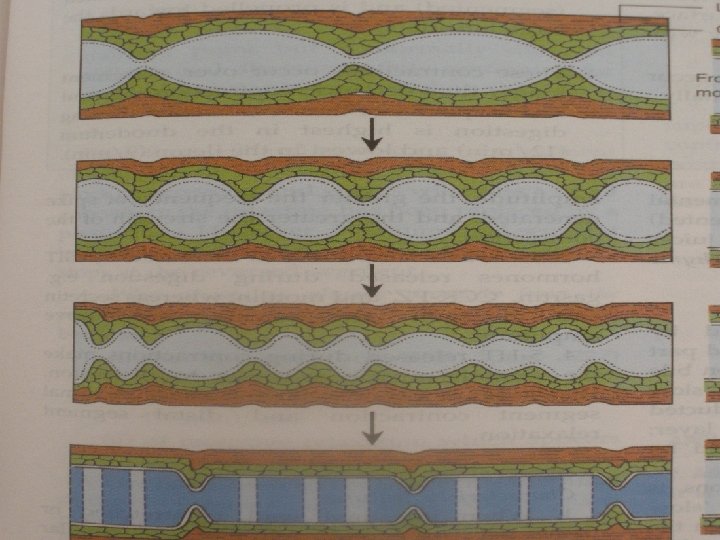
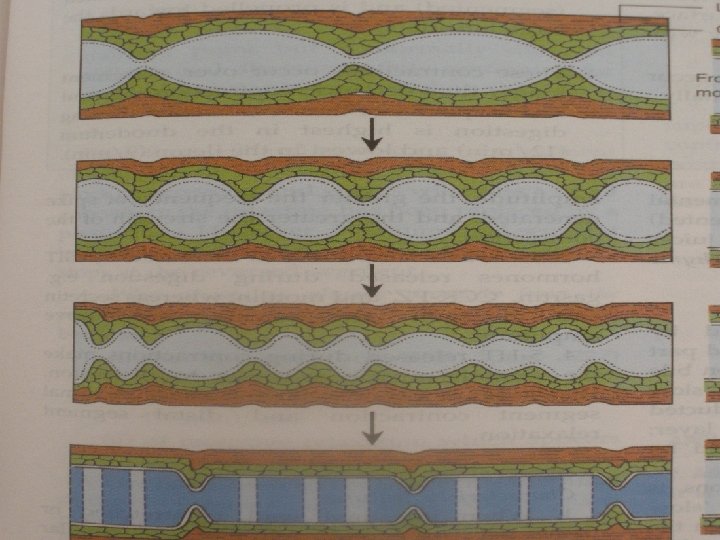
Rhythmic segmental movements: Ø Ring like contractions that appear at fairly regular intervals involving a localized segment of 1 -2 cm. Ø A loop of intestine is divided in to number of segments with nearly equal size. Ø Each of this again quickly divide and the neighouring halves suddenly unite to form a new segment.
Duodenum= 18/min Jejunum = 15/min Ileum = 12/min Myogenic in Orgin
Function : Agitation of intestinal contents. • Cut the larger food particles in to smaller one. • Mixing of the food with the intestinal and other digestive juices. • Changing the layer of food in contact with the mucosa thus facilitating absorption.
Pendular movement: Side to side swaying movements accompanied by lengthening and shortening of the intestine. One entire loop of intestine is involved. Function: Similar to that of rhythmic segmental contraction.
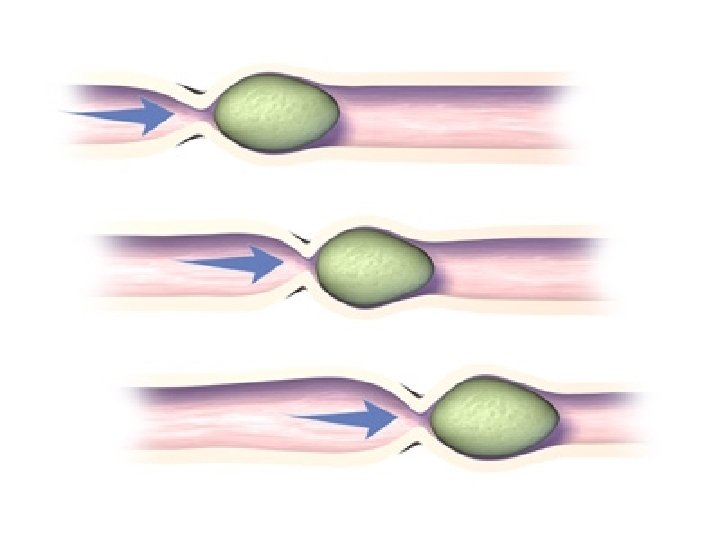
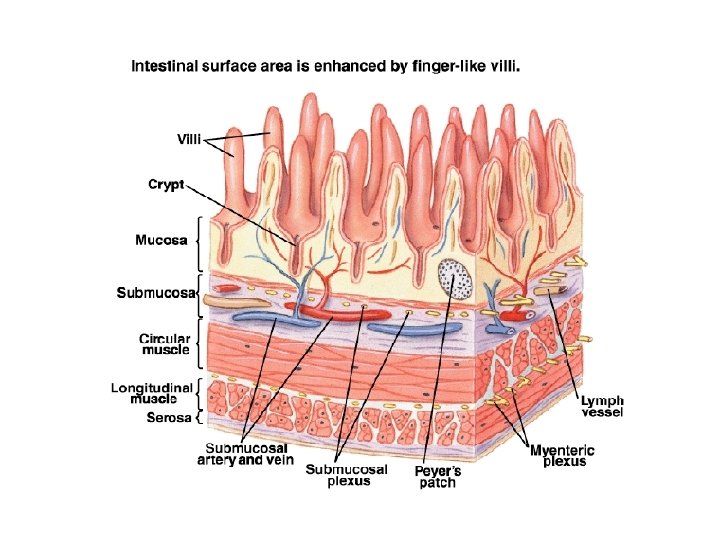
Peristalsis: • It is defined as a wave of contraction preceded by a wave of relaxation that travels aborally. • It is neurogenic and depends on Myenteric plexus. • When the intestine is stretched due to the presence of food, a contraction above and relaxation below appears. (MYENTERIC REFLEX)

Law of intestine- propogation of ring of contraction in aboral direction. Rush peristalsis Antiperistalsis
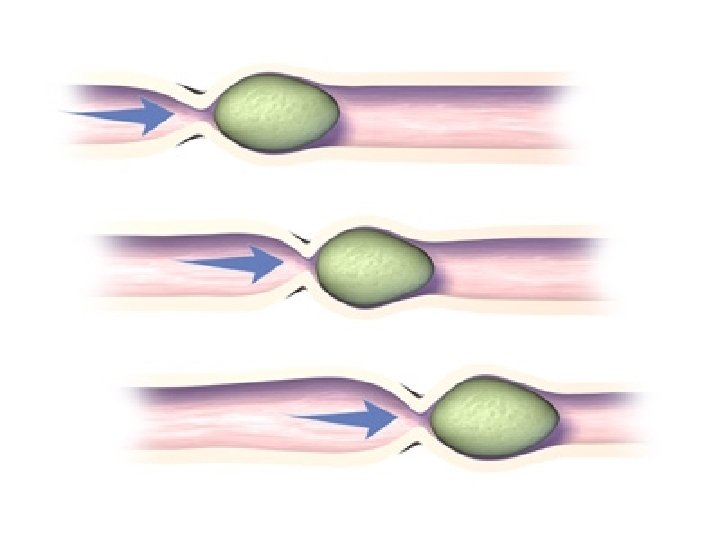
• The rate of movement is 2 -12 cm/sec. • Faster in the proximal part and slower in the terminal part. Functions: • Progression of the chyme towards the ileocaecal valve. • Spreading of the chyme along the intestine.
Migratory motor complex They are electomechanical waves. This occurs when the food is absent in the small intestine. Takes Orgin in the stomach and spreads towards the ileum. Every 90 min Housekeeper of small intestine or sweeper of GIT
Function: • It helps to clear off any food residue that remains after previous meal. • Inhibits the migration of colon bacteria in to the distal ileum • Keeps the GIT ready for next meal.
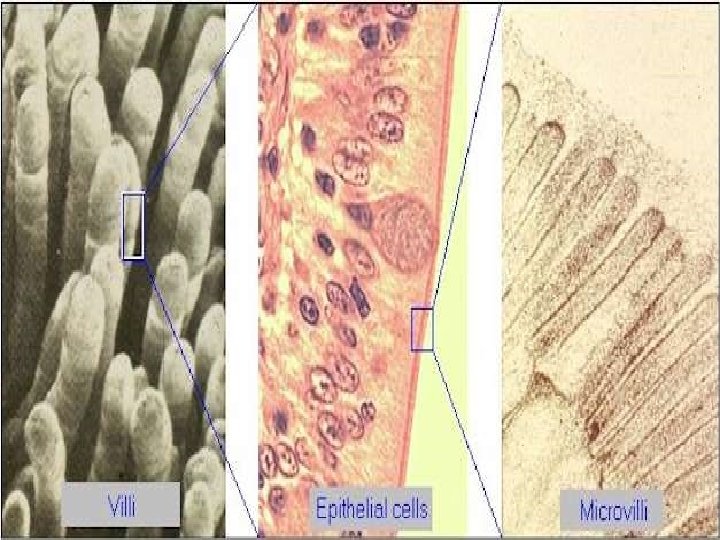
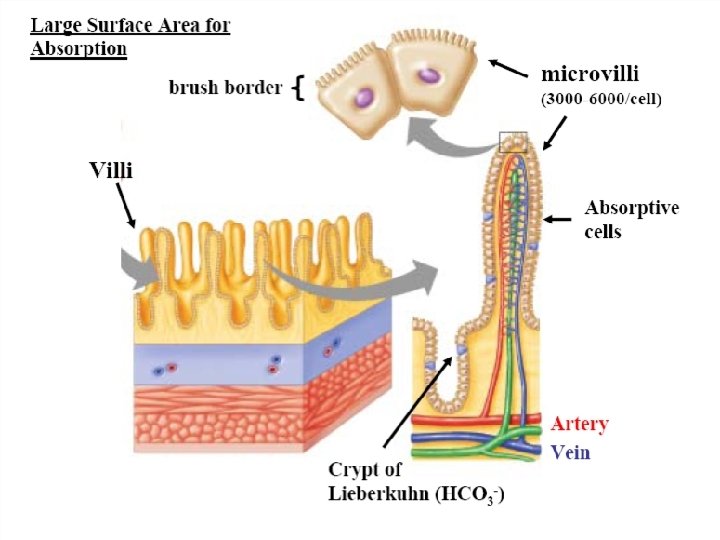
In addition in small intestine Movements of Villi: They are initiated by local nervous reflexes that occurs in response to the chyme in the small intestine. Helps in emptying central lacteals of villi. 1. Lashing movements 2. Lengthening and shortening movements
Functions: • These movements facilitate the flow of blood and lymph. • Increase absorption

Contraction of muscularis mucosa: contract irregularly Intestinal reflex: 1) Intestino-intestinal reflex 2) Gastroileal reflex

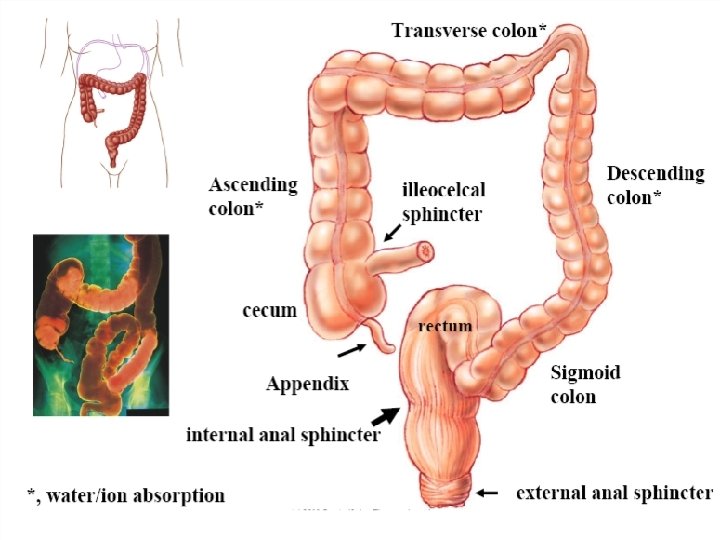
Large intestine:
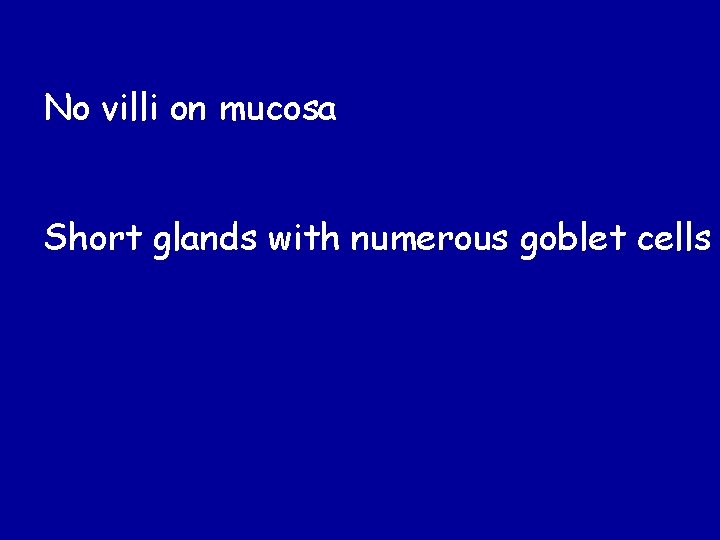
No villi on mucosa Short glands with numerous goblet cells
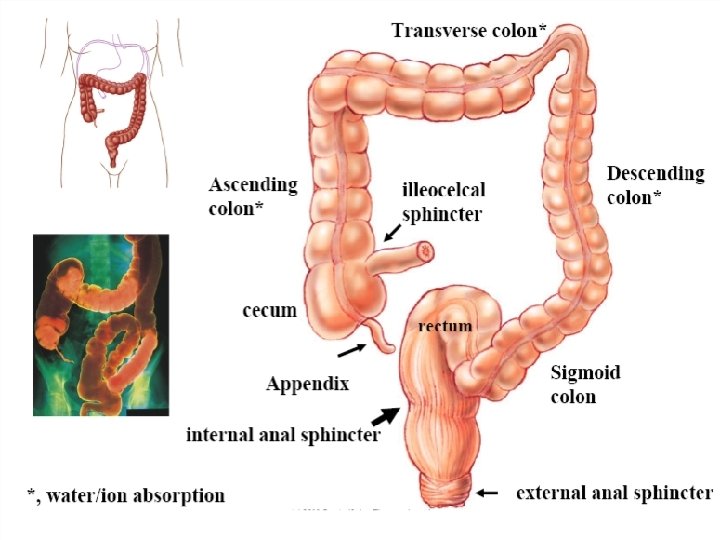
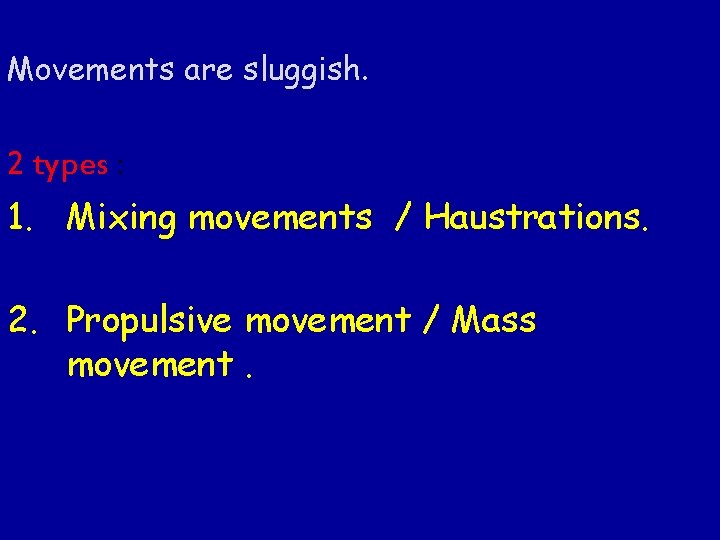
Movements are sluggish. 2 types : 1. Mixing movements / Haustrations. 2. Propulsive movement / Mass movement.
- Haustral contractions - Propulsive movements - Mass peristalsis - Reflex- 1) Colonocolonic reflex 2) Gastrocolic reflex
Mixing movements /Haustrations: • Same as that of segmental movements in small intestine but involve larger segments. • Bag like sac =Haustrations formed.
Mass peristalsis: • Occurs once or twice a day in an adults and several times a day in infants Stimulus: Filling of the stomach /over distention of the colon. - leads to defecation reflex Ø Evacuation of the colon contents.
In Paraplegic patients due to spinal injury voluntary control of defaecation reflux is lost. Initiated by • Scratching the medial side of the thigh/the lower part of anterior abdominal wall. • Introducing an irritating substance in to the rectum(Enema)
Applied aspects: § Constipation - motility is less. § Diarrhoea – motility is more. § Aganglionic megacolon: congenital absence of the ganglionic cells in myenteric and submucosal plexus of a segment of the distal colon. • Faecal matter accumulates in this region. • This area is resected and the portion of the colon above is anastamosed to the colon.

Gastric Empting
- HUNGER CONTRACTION - GASTRIC RELAXATION- 1) receptive relaxation 2) adaptive relaxation 3) feedback relaxation - PERISTALSIS - MIGRATORY MOTOR COMPLEX - REVERSE PERISTALSIS
- HUNGER CONTRACTION Stomach empty- contractions Longer duration vigorous contractions Associated with pyloric relaxation
RECEPTIVE RELAXATION: - In response to chewing and swallowing of food - Intra gastric pressure does not rise ADAPTIVE RELAXATION: in response to food in stomach FEEDBACK RELAXATION: Inresponse to food in duodenum
- PERISTALSIS: - Half an hour after gastric filling. - Pacemaker in middle of stomach in greater curvature - Pylorus is closed - Pushes food into antrum - Helps in mixing of food. - MIGRATORY MOTOR COMPLEX - REVERSE PERISTALSIS
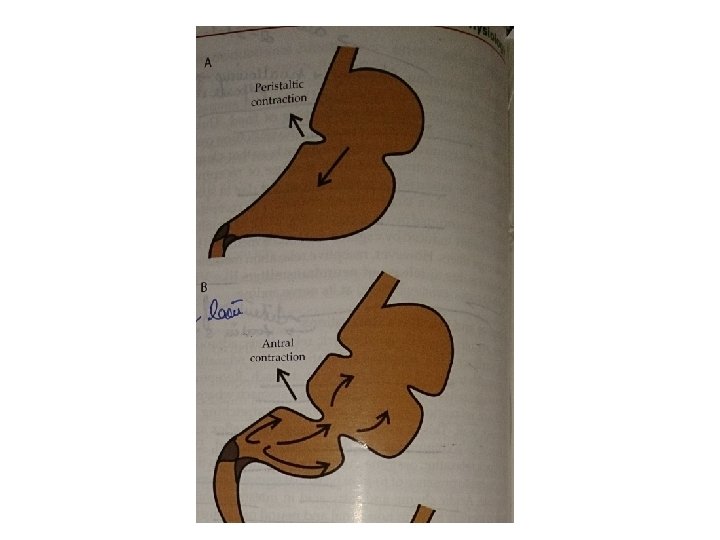
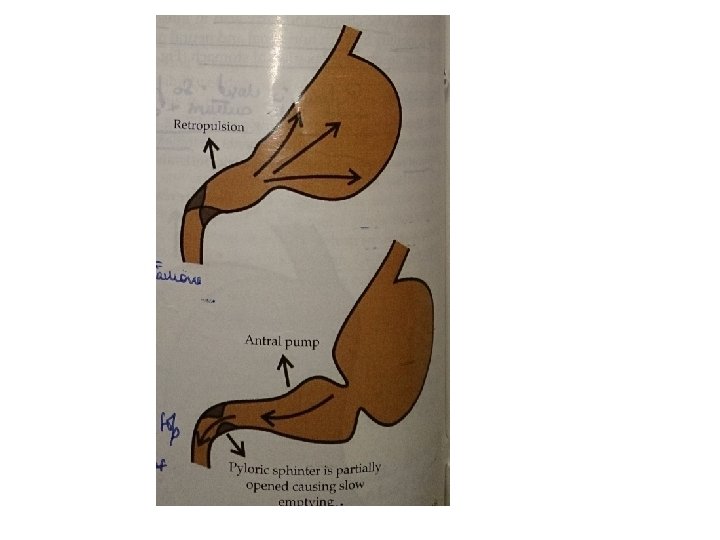
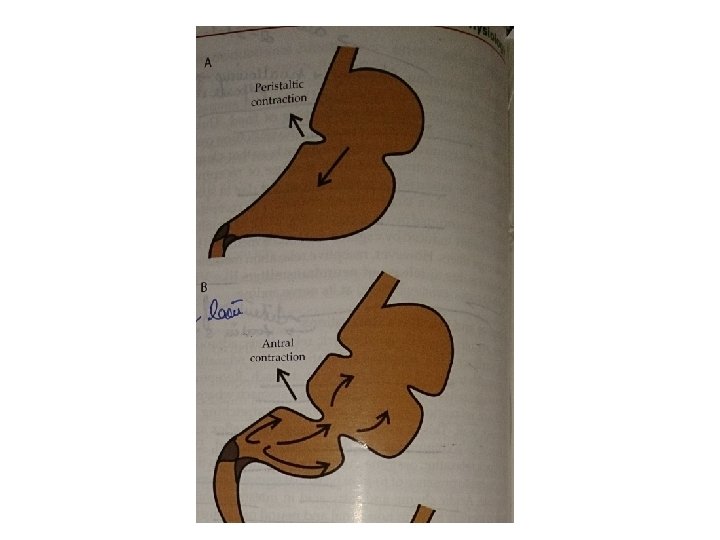
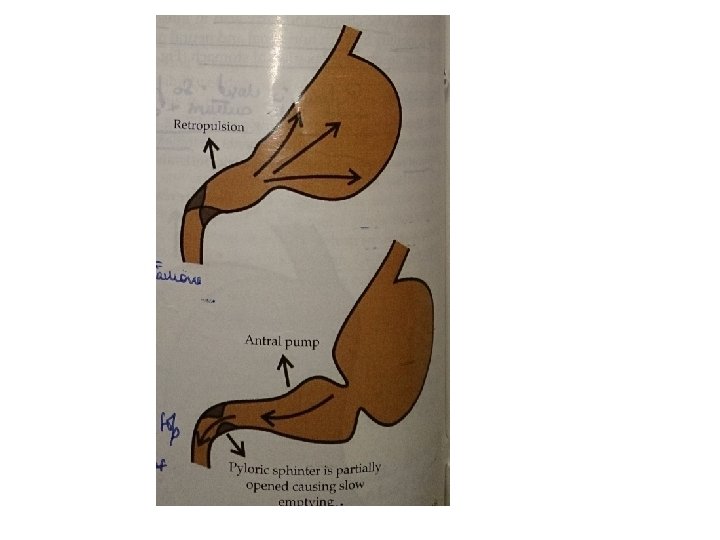
GASRTIC EMPTYING: Peristaltic contraction Antral contraction Retropulsion
The rate at which substances leaves the stomach and enters the duodenum. Regulated by: • • Stomach factors. Duodenal factors. Neural factors. Hormonal factors

Stomach factors: 1. Volume of gastric contents: Increase in gastric content facilitates gastric emptying. 2. Consistency of food: • Liquids-Semisolids-Solids • Chemical composition: • Carbohydrates-proteins-fats.
3. Acidity: Weak acids and neutral solutions -Strong acids. 4. Osmolar concentration : Higher the Osmolar concentration – slower emptying.
Duodenal factors: 1. Distension of duodenum: Reflexly inhibit gastric emptying. Prevent the overloading of the duodenum with partially digested food. 2. Acid in the duodenum: Reduces the gastric motility mediated through Enterogastrone , CCK-PZ , Secretin , VIP etc
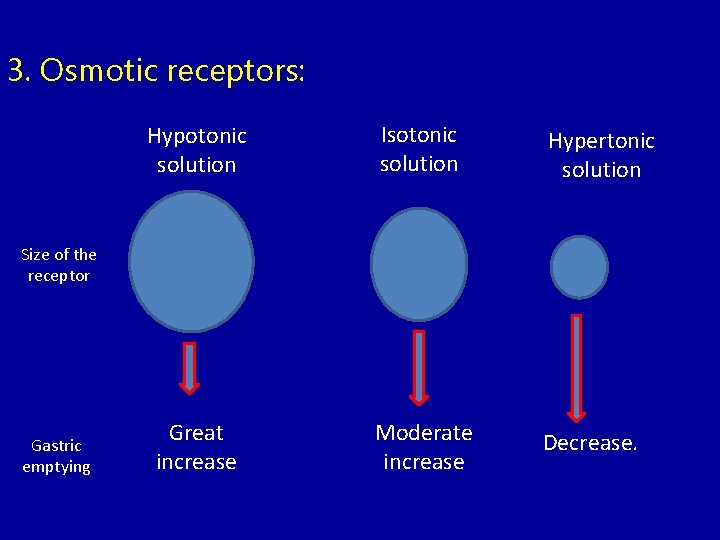
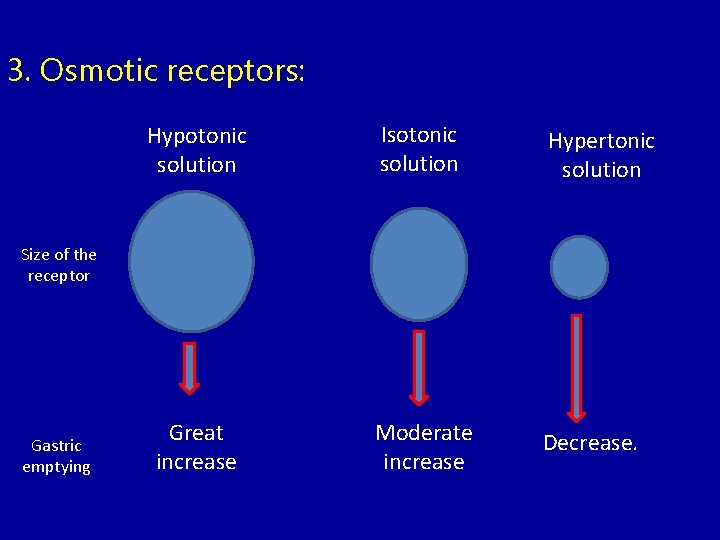
3. Osmotic receptors: Hypotonic solution Isotonic solution Hypertonic solution Great increase Moderate increase Decrease. Size of the receptor Gastric emptying
Neural: Parasympathetic : increase. Sympathetic : decrease. Hormonal: Gastrin –facilitates VIP , CCK-PZ, Secretin etc – decrease. Emotional factors