GI 8 IMAGING AMPULLOMA OF VATERS PAPILLE SERIES


- Slides: 41
GI 8 IMAGING AMPULLOMA OF VATER’S PAPILLE SERIES OF FIFTEEN CASES YAHDI VICHE, R SAOUAB, J EL FENNI, S. CHAOUIR, T. AMIL, A HANINE, B RADOUANE Radiology Service Instruction Military Hospital Mohammed V In collaboration with the visceral surgery service (Sair Pr)
INTRODUCTION q q The ampullomas vatériens = often malignant or benign tumors derived from the intersection area bounded by biliopancreatic tract and the sphincter of Oddi (the last 2 cm of the biliopancreatic junction) Biliary obstruction is early clinical symptoms q The cross-sectional imaging is a great contribution to the diagnosis, staging and monitoring q Early diagnosed , the prognosis is better than pancreatic cancer
OBJECTIVES To report the clinical and epidemiological aspects of ampullomas vatériens in the series. Establish the role and limitations of each imaging system. Describe aspects of imaging ampullomas vatériens. Discuss the differential diagnosis.
MATERIALS AND METHODS Retrospective review of records of ampullomas vatériens explored in the training. During 6 years period [January 2005 - December 2010]. The image system used: - Ultrasound (n: 15) - CT (n: 11) - MRI (n: 4) - Endoscopic retrograde cholangiography (n = 4).
RESULTS 15 cases of ampulla vatériens were detected Their representation are: - 0. 2% of hospitalizations in the department of visceral surgery - 3. 4% of digestive cancers (rank 8) Average age: 68 years [ Between 52 ans and 89 ans] 9 Males and 6 Female
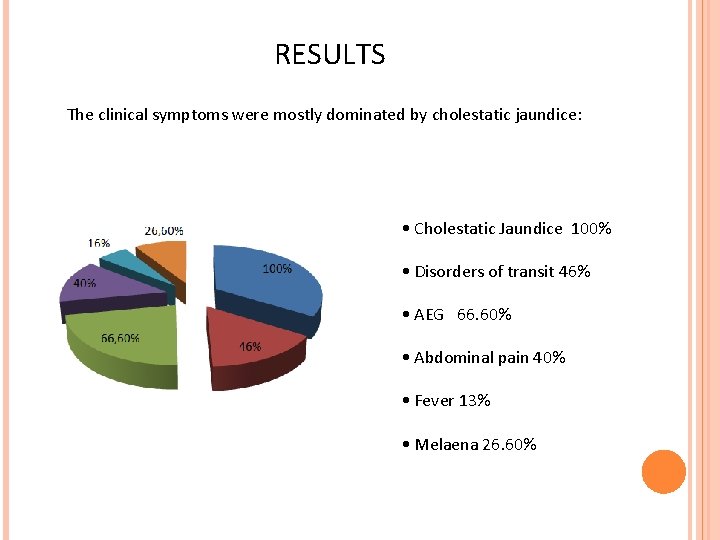
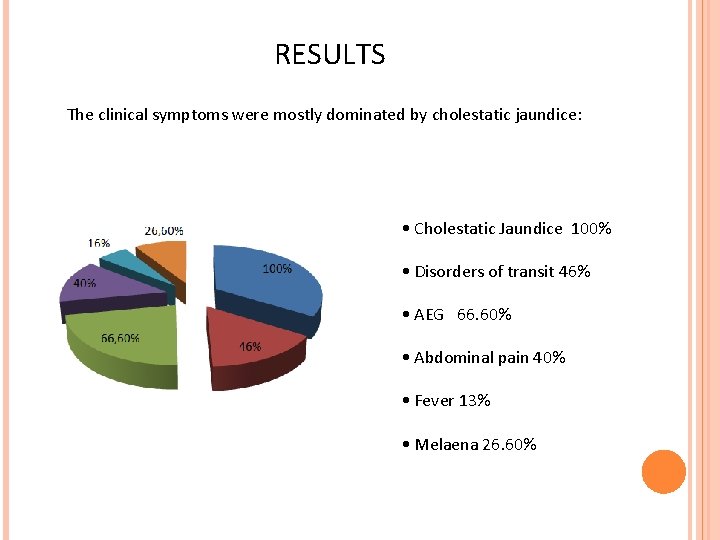
RESULTS The clinical symptoms were mostly dominated by cholestatic jaundice: • Cholestatic Jaundice 100% • Disorders of transit 46% • AEG 66. 60% • Abdominal pain 40% • Fever 13% • Melaena 26. 60%
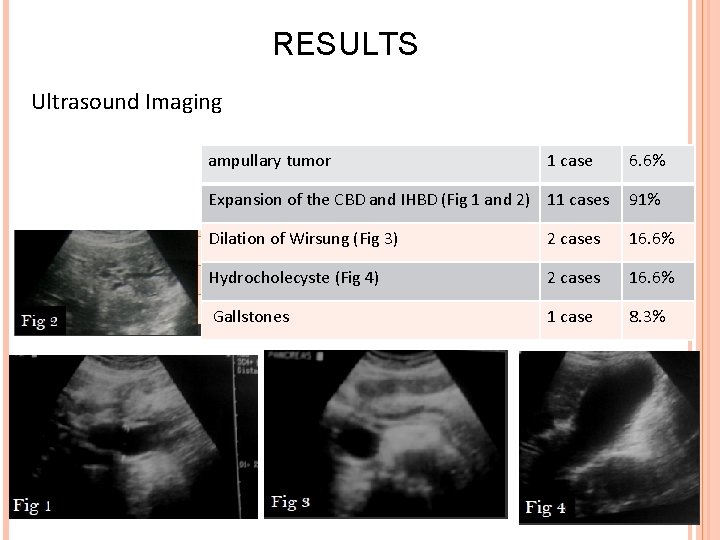
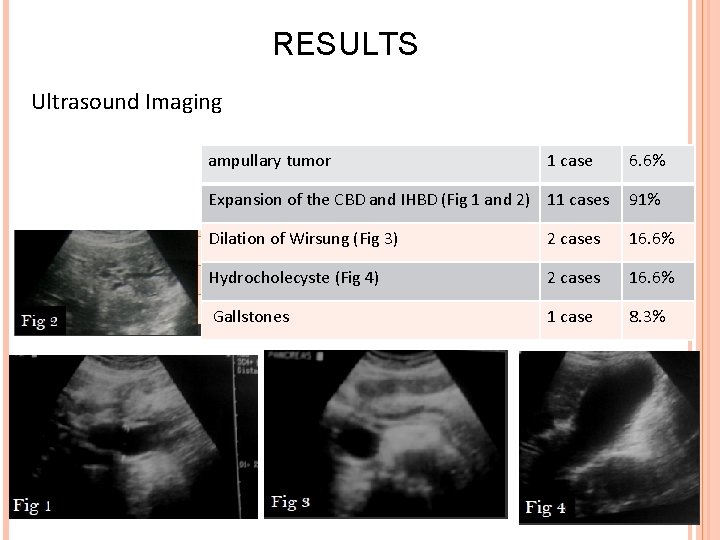
RESULTS Ultrasound Imaging ampullary tumor 1 case 6. 6% Expansion of the CBD and IHBD (Fig 1 and 2) 11 cases 91% Dilation of Wirsung (Fig 3) 2 cases 16. 6% Hydrocholecyste (Fig 4) 2 cases 16. 6% Gallstones 1 case 8. 3%
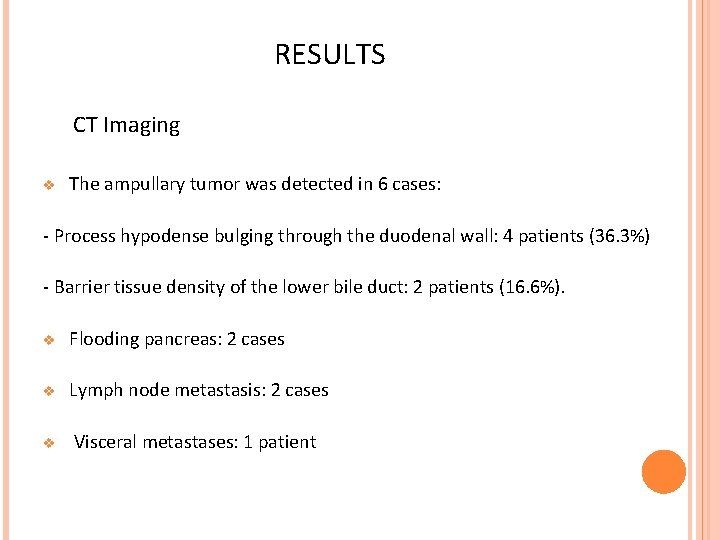
RESULTS CT Imaging v The ampullary tumor was detected in 6 cases: - Process hypodense bulging through the duodenal wall: 4 patients (36. 3%) - Barrier tissue density of the lower bile duct: 2 patients (16. 6%). v Flooding pancreas: 2 cases v Lymph node metastasis: 2 cases v Visceral metastases: 1 patient

RESULTS Case 1: Abdominal CT in axial(a), Reconstruction with frontal (b), C +: Tissue process of duodenal papilla, enhanced homogeneously, causing a dilation of a EHBD.
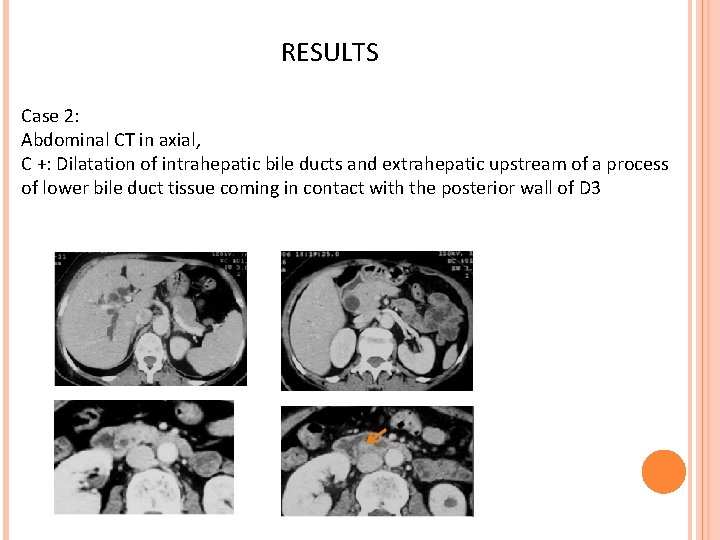
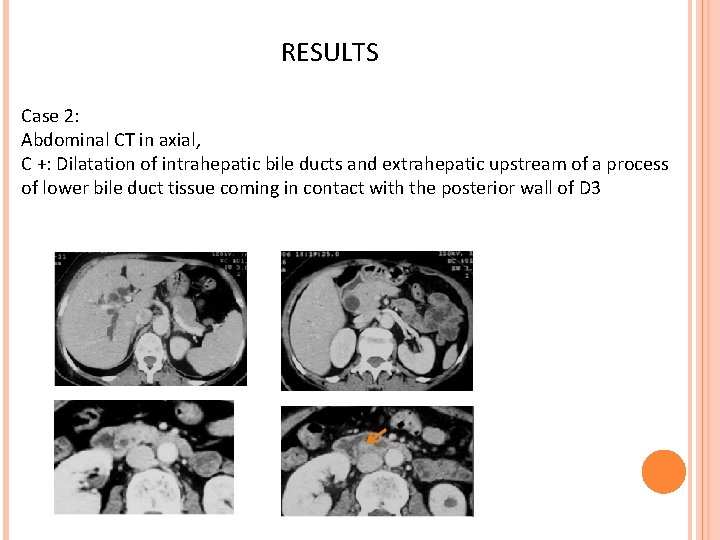
RESULTS Case 2: Abdominal CT in axial, C +: Dilatation of intrahepatic bile ducts and extrahepatic upstream of a process of lower bile duct tissue coming in contact with the posterior wall of D 3
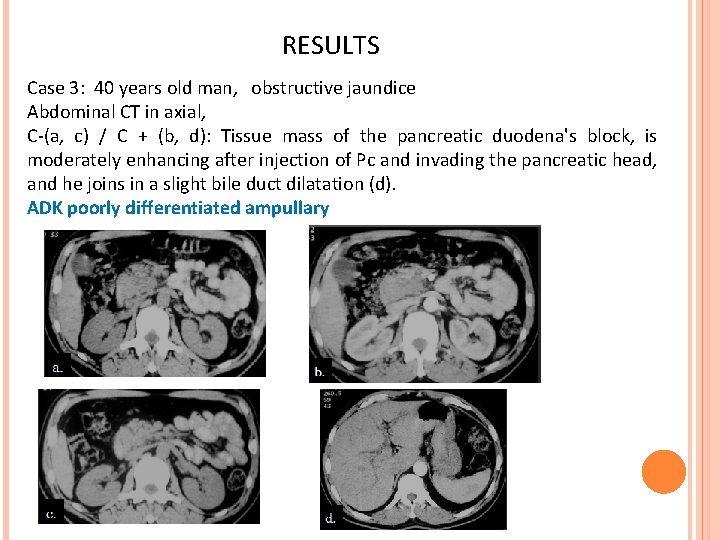
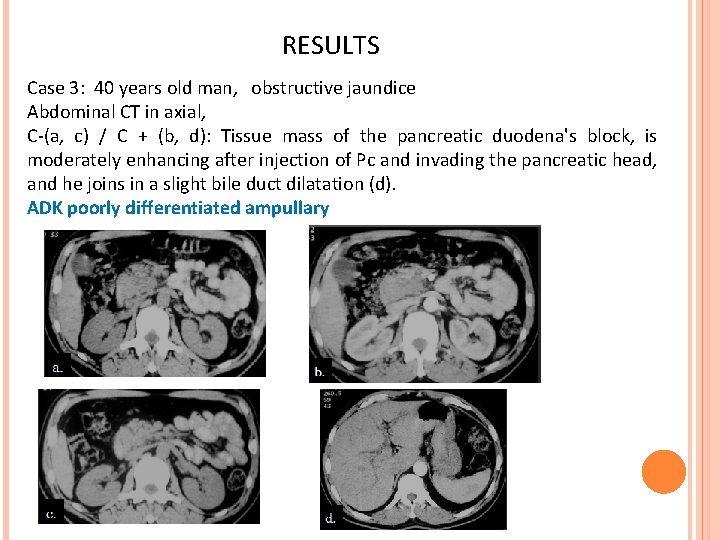
RESULTS Case 3: 40 years old man, obstructive jaundice Abdominal CT in axial, C-(a, c) / C + (b, d): Tissue mass of the pancreatic duodena's block, is moderately enhancing after injection of Pc and invading the pancreatic head, and he joins in a slight bile duct dilatation (d). ADK poorly differentiated ampullary
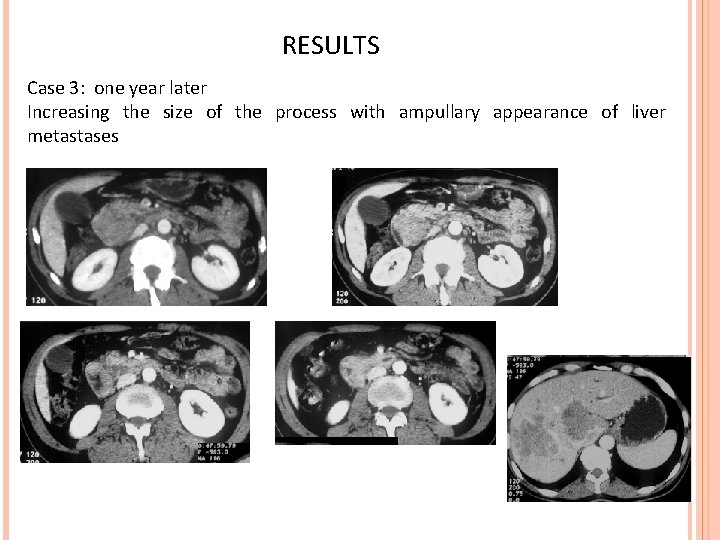
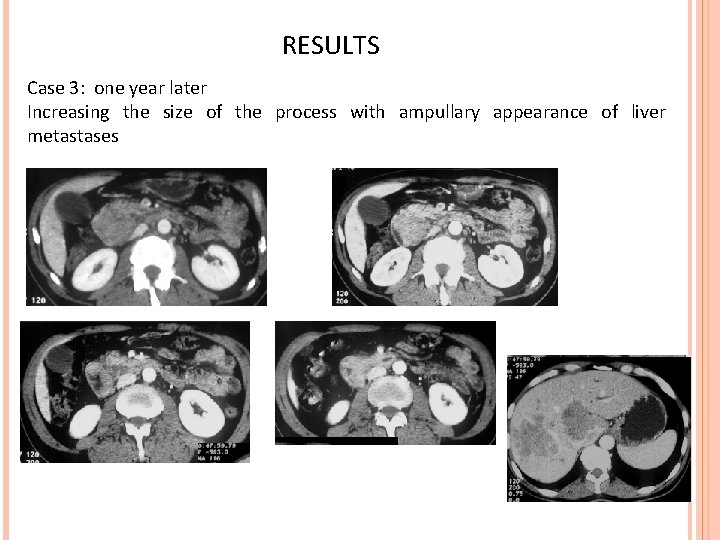
RESULTS Case 3: one year later Increasing the size of the process with ampullary appearance of liver metastases
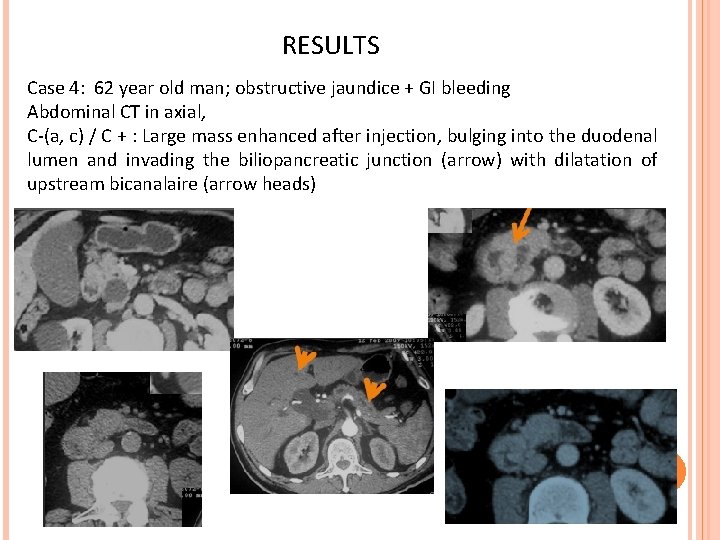
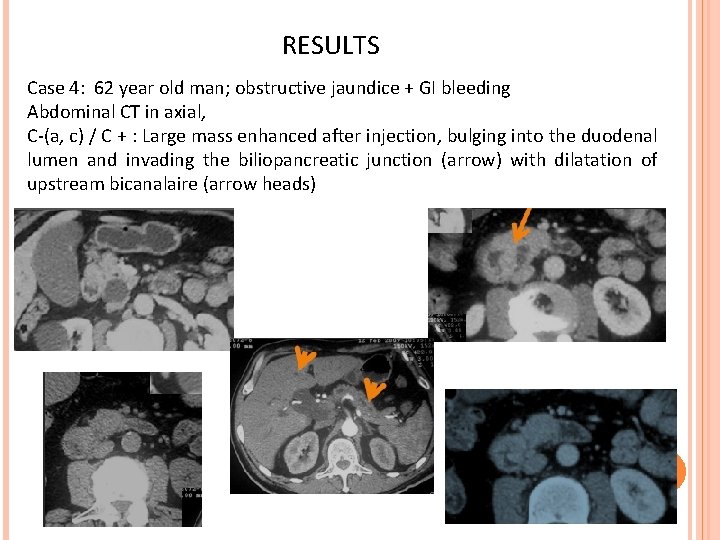
RESULTS Case 4: 62 year old man; obstructive jaundice + GI bleeding Abdominal CT in axial, C-(a, c) / C + : Large mass enhanced after injection, bulging into the duodenal lumen and invading the biliopancreatic junction (arrow) with dilatation of upstream bicanalaire (arrow heads)
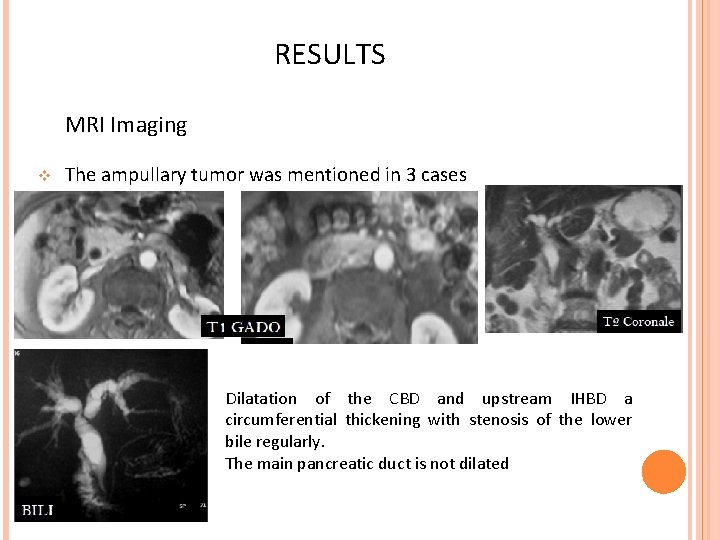
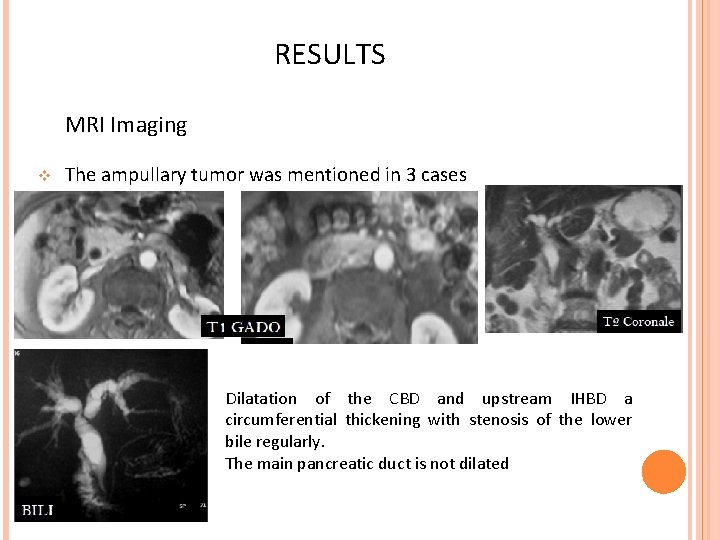
RESULTS MRI Imaging v The ampullary tumor was mentioned in 3 cases Dilatation of the CBD and upstream IHBD a circumferential thickening with stenosis of the lower bile regularly. The main pancreatic duct is not dilated
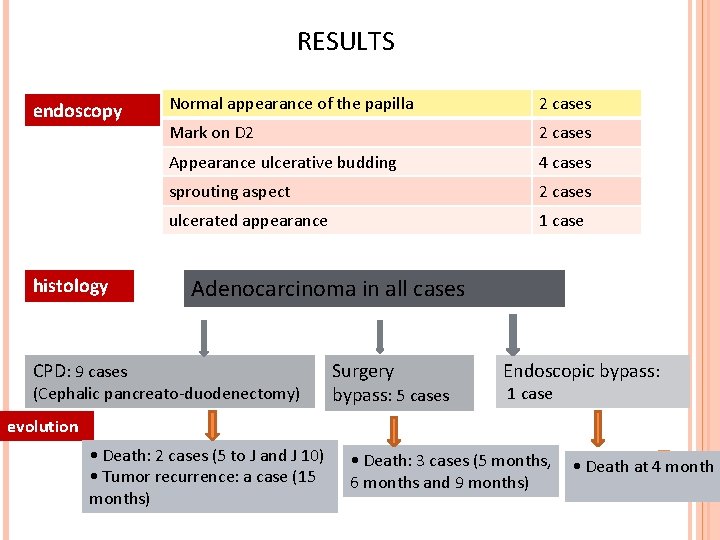
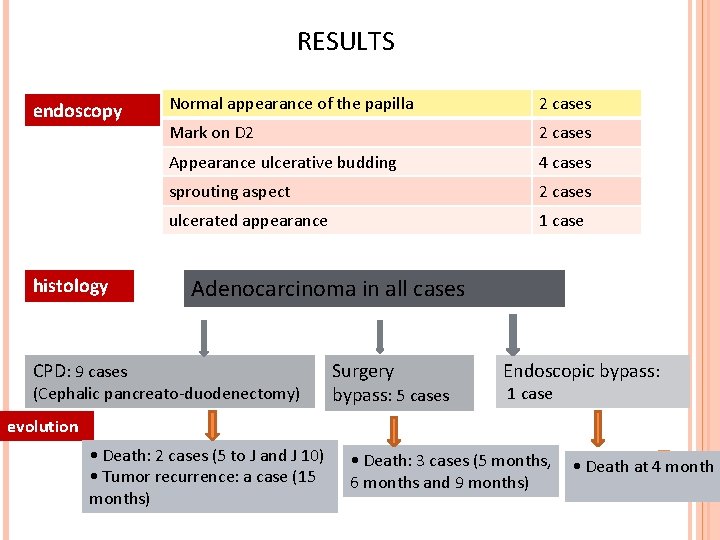
RESULTS endoscopy histology Normal appearance of the papilla 2 cases Mark on D 2 2 cases Appearance ulcerative budding 4 cases sprouting aspect 2 cases ulcerated appearance 1 case Adenocarcinoma in all cases CPD: 9 cases (Cephalic pancreato-duodenectomy) Surgery bypass: 5 cases Endoscopic bypass: 1 case evolution • Death: 2 cases (5 to J and J 10) • Tumor recurrence: a case (15 months) • Death: 3 cases (5 months, 6 months and 9 months) • Death at 4 month

DISCUSSION
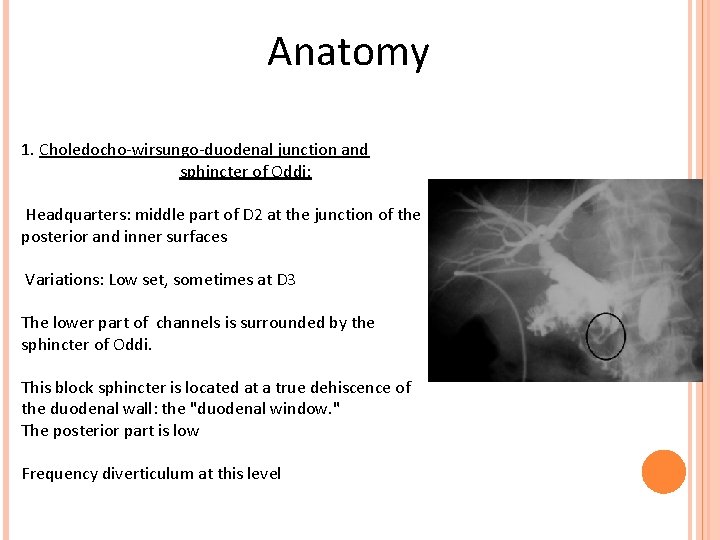
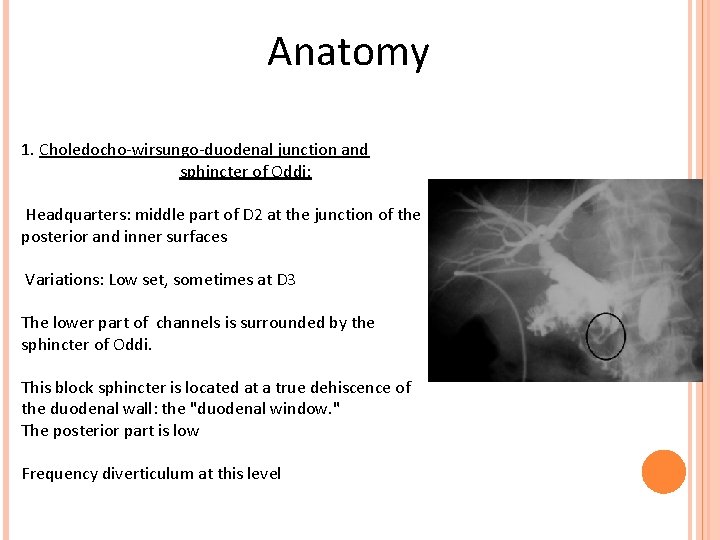
Anatomy 1. Choledocho-wirsungo-duodenal junction and sphincter of Oddi: Headquarters: middle part of D 2 at the junction of the posterior and inner surfaces Variations: Low set, sometimes at D 3 The lower part of channels is surrounded by the sphincter of Oddi. This block sphincter is located at a true dehiscence of the duodenal wall: the "duodenal window. " The posterior part is low Frequency diverticulum at this level
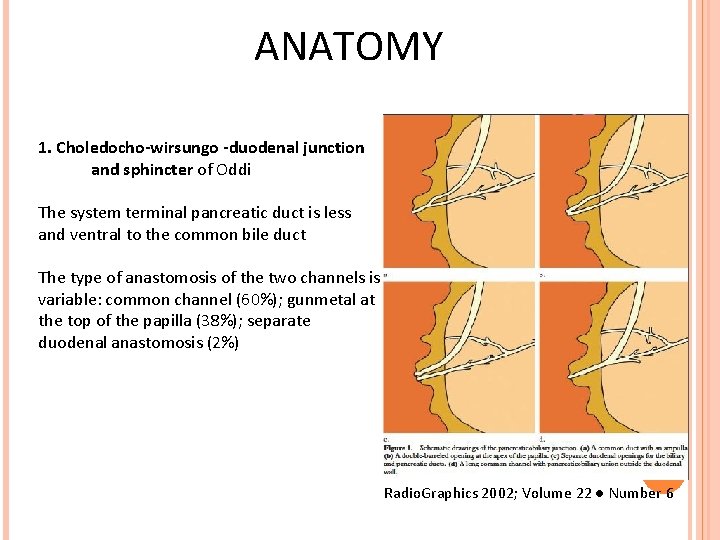
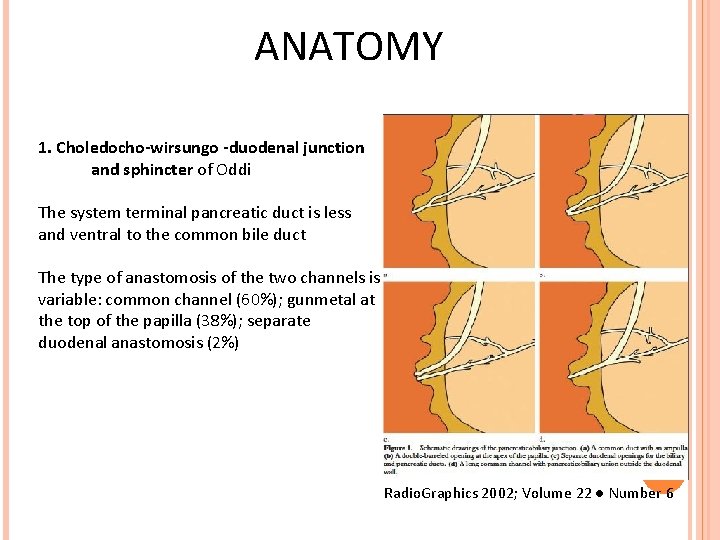
ANATOMY 1. Choledocho-wirsungo -duodenal junction and sphincter of Oddi The system terminal pancreatic duct is less and ventral to the common bile duct The type of anastomosis of the two channels is variable: common channel (60%); gunmetal at the top of the papilla (38%); separate duodenal anastomosis (2%) Radio. Graphics 2002; Volume 22 ● Number 6
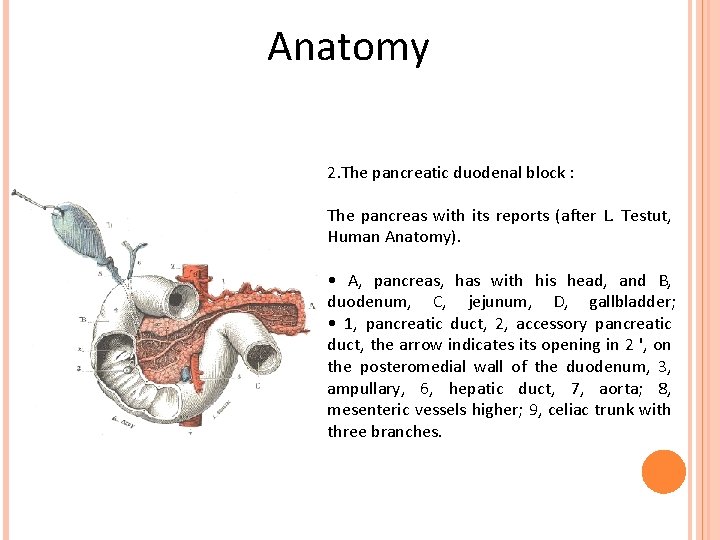
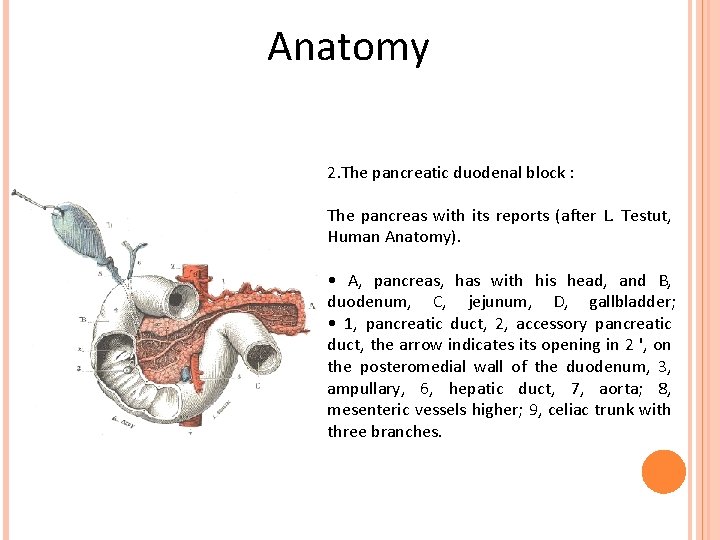
Anatomy 2. The pancreatic duodenal block : The pancreas with its reports (after L. Testut, Human Anatomy). • A, pancreas, has with his head, and B, duodenum, C, jejunum, D, gallbladder; • 1, pancreatic duct, 2, accessory pancreatic duct, the arrow indicates its opening in 2 ', on the posteromedial wall of the duodenum, 3, ampullary, 6, hepatic duct, 7, aorta; 8, mesenteric vessels higher; 9, celiac trunk with three branches.
Epidemiology The ampullary vatérien is a rare tumor: 0. 02 to 5% of gastrointestinal tumors Peak age between 50 and 70 years with slight male predominance Predisposing factors: Familial adenomatous polyposis (ampullary adenoma in 50% of cases) Gardner's syndrome Van Recklinghausen's disease The association with cholelithiasis is found in 8 -20% depending on the series
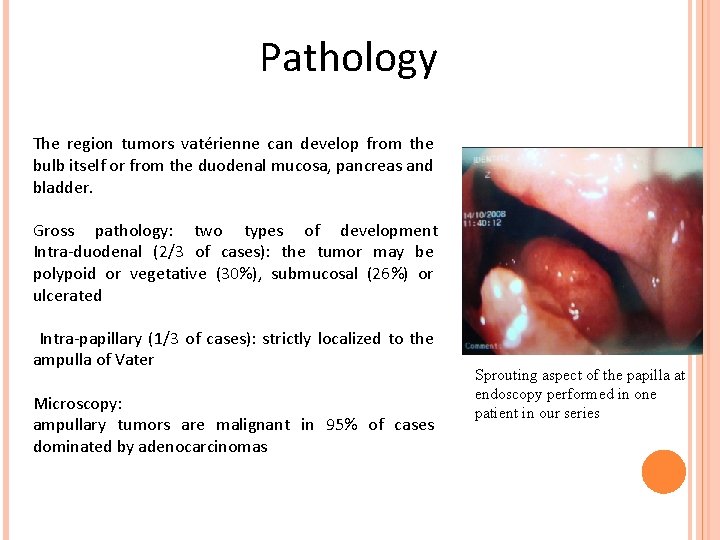
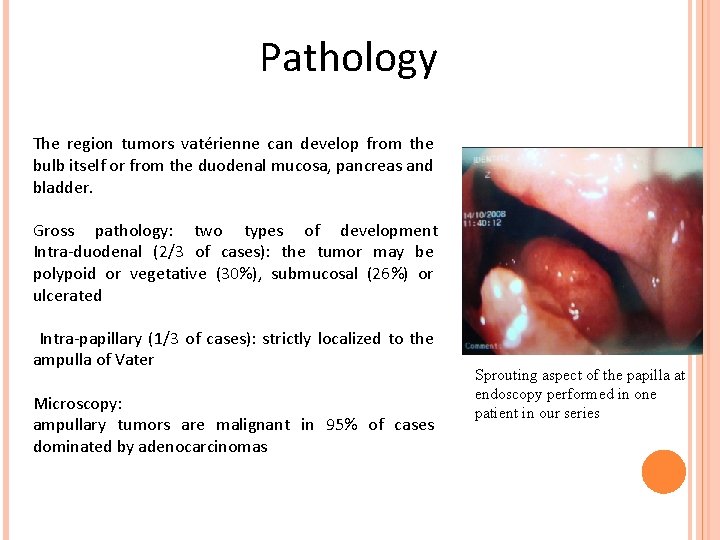
Pathology The region tumors vatérienne can develop from the bulb itself or from the duodenal mucosa, pancreas and bladder. Gross pathology: two types of development Intra-duodenal (2/3 of cases): the tumor may be polypoid or vegetative (30%), submucosal (26%) or ulcerated Intra-papillary (1/3 of cases): strictly localized to the ampulla of Vater Microscopy: ampullary tumors are malignant in 95% of cases dominated by adenocarcinomas Sprouting aspect of the papilla at endoscopy performed in one patient in our series
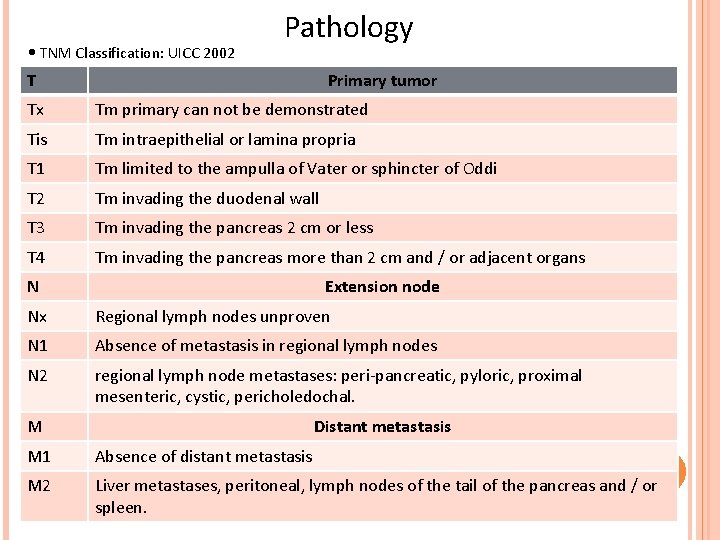
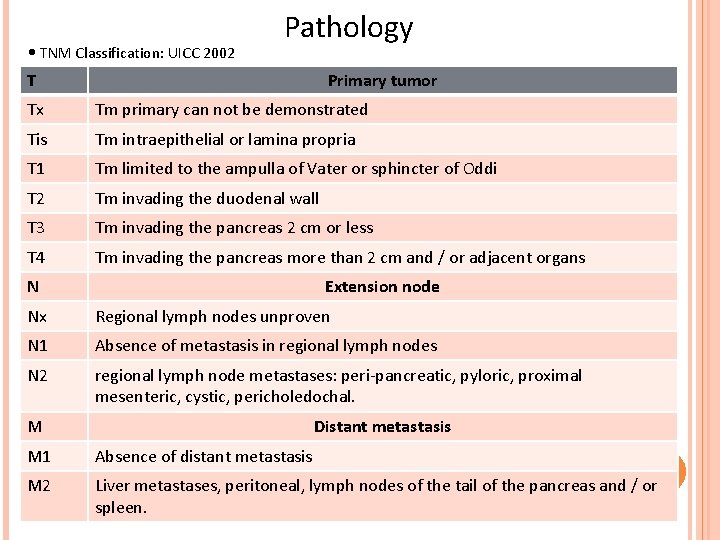
• TNM Classification: UICC 2002 Pathology T Primary tumor Tx Tm primary can not be demonstrated Tis Tm intraepithelial or lamina propria T 1 Tm limited to the ampulla of Vater or sphincter of Oddi T 2 Tm invading the duodenal wall T 3 Tm invading the pancreas 2 cm or less T 4 Tm invading the pancreas more than 2 cm and / or adjacent organs N Extension node Nx Regional lymph nodes unproven N 1 Absence of metastasis in regional lymph nodes N 2 regional lymph node metastases: peri-pancreatic, pyloric, proximal mesenteric, cystic, pericholedochal. M Distant metastasis M 1 Absence of distant metastasis M 2 Liver metastases, peritoneal, lymph nodes of the tail of the pancreas and / or spleen.
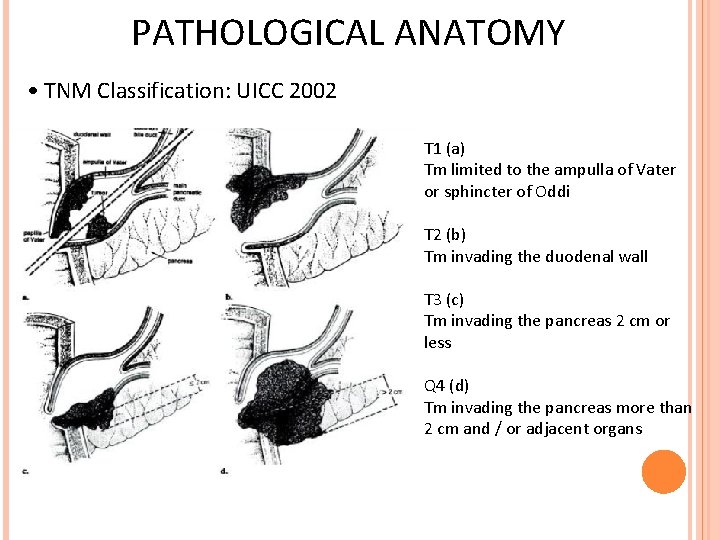
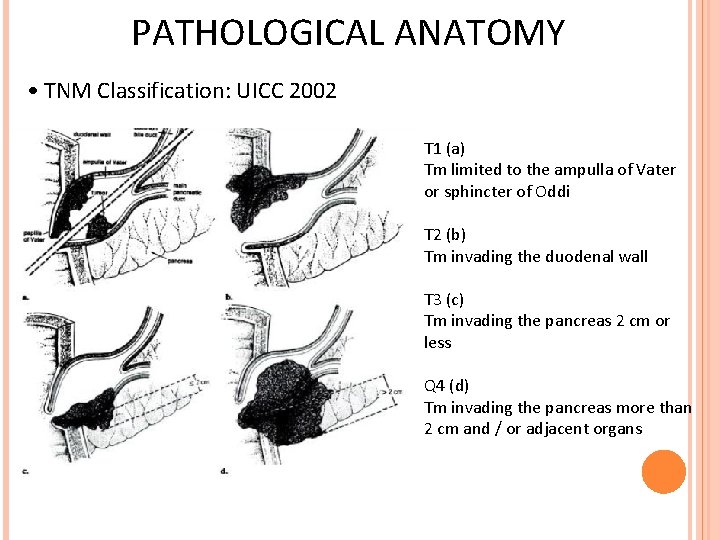
PATHOLOGICAL ANATOMY • TNM Classification: UICC 2002 T 1 (a) Tm limited to the ampulla of Vater or sphincter of Oddi T 2 (b) Tm invading the duodenal wall T 3 (c) Tm invading the pancreas 2 cm or less Q 4 (d) Tm invading the pancreas more than 2 cm and / or adjacent organs
Clinical The obstructive jaundice: it is the sign most frequently revealing and often constant, found in 70 -80% of cases GI bleeding: Sx evocative but inconstant (6% of cases), melaena, anemia Other: abdominal pain, transit disorders, IGC
1. Échographie: Imagery Review of first-line before a cholestatic jaundice Interest: Confirm the dilated bile ducts in 100% of cases with hydrocholecyste Specify the level of obstruction in 90% of cases View ampullary tumor in 25% of cases especially if the tumor size> 2 cm To identify liver metastases Limits: Tumors <2 cm The nodal The interposition gas or obesity + + +
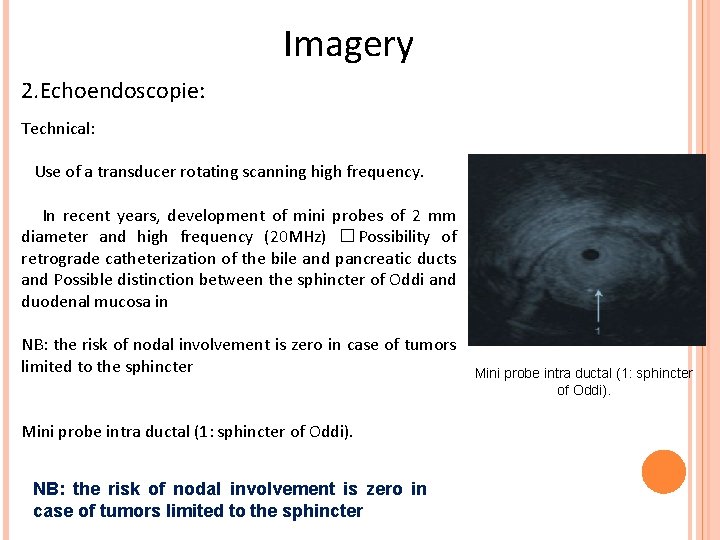
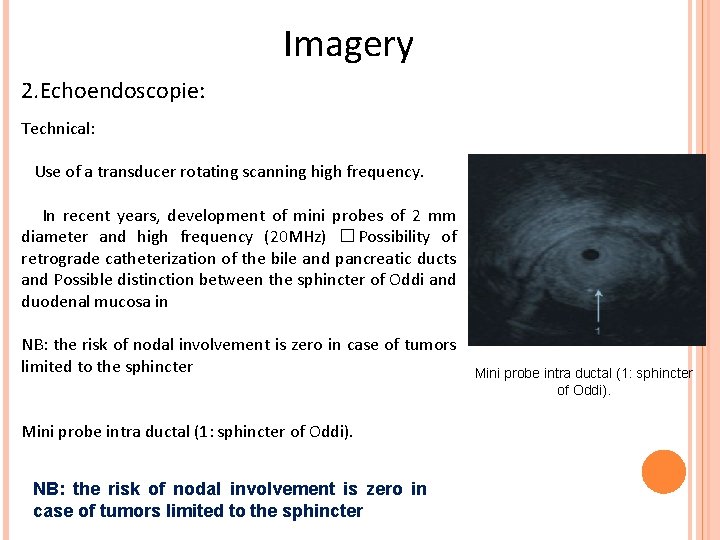
Imagery 2. Echoendoscopie: Technical: Use of a transducer rotating scanning high frequency. In recent years, development of mini probes of 2 mm diameter and high frequency (20 MHz) � Possibility of retrograde catheterization of the bile and pancreatic ducts and Possible distinction between the sphincter of Oddi and duodenal mucosa in NB: the risk of nodal involvement is zero in case of tumors limited to the sphincter Mini probe intra ductal (1: sphincter of Oddi).
Imagery 2. Echoendoscopie Interest: The visualization of the tumor vatérienne in 90 to 100% of cases Superior sensitivity than other imaging techniques for evaluation of: - The extension of the tumor (T): if malignancy crossing the fourth hypoechoic layer of the duodenal wall (muscularis) - The nodal (N): diagnostic accuracy of 68 to 76% for stage N 1 - The invasion of the vein axis mesocaval door with a sensitivity of 91% and a specificity of 97% Indications: Suspicion of pathology with an ampullary OGDF a cross-sectional imaging and inconclusive Assessment of preoperative extension of ampullary tumors proven choice of TRT (surgical or endoscopic)
3. TDM: Imagery Importance: Sensitivity of 85 to 90% in case of biliary dilatation and specificity of 90%. Technical: Acquisition helical thin sections Ingestion of water + + + Study with and without injection of the PC in arterial and portal venous phase (with 100 cc flow 3 cc/sec) Results: Positive diagnosis: Turgid appearance of the papilla or hypodense heterogeneous process bulging into the duodenal lumen The dilated bile ducts inside and outside the liver associated with dilatation of the pancreatic duct is highly suggestive of the diagnosis Extension: The pancreas, lymph node, peritoneal or hepatic vein thrombosis
Imagery MRI Interest: better contrast resolution and multi planar study Technical: morphological sequences: axial acquisitions SPT 1 and FAT-SAT GADO T 1, T 2 Sp coronal acquisition, 4 mm thick Sequence diffusion and Bili-sequence MRI Results: MRI allows visualization of the ampullary tumor in 93% of cases: Small polypoid lesion, iso or hypo T 1 and T 2, weakly or moderately enhanced after injection protruding into the duodenal lumen Sometimes, a simple engorgement of the papilla Irregular thickening of the biliopancreatic junction The bili-MRI appreciate the topography and the length of the obstacle. Frank said in a ruling "pellet shells" referred to the diagnosis.
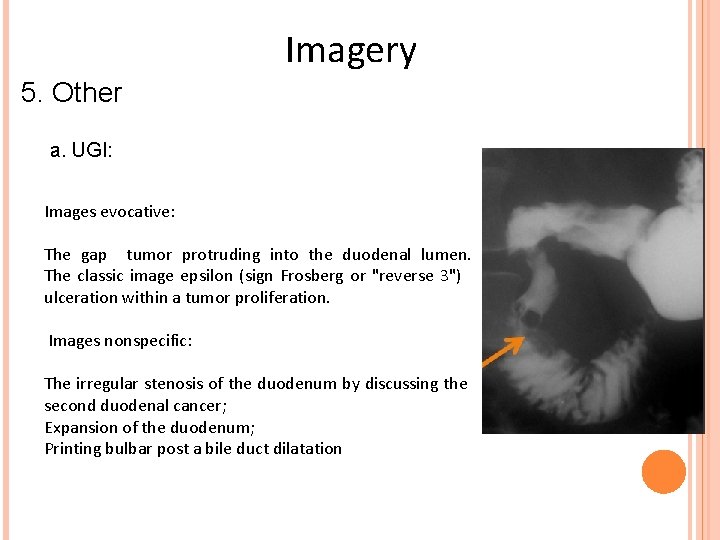
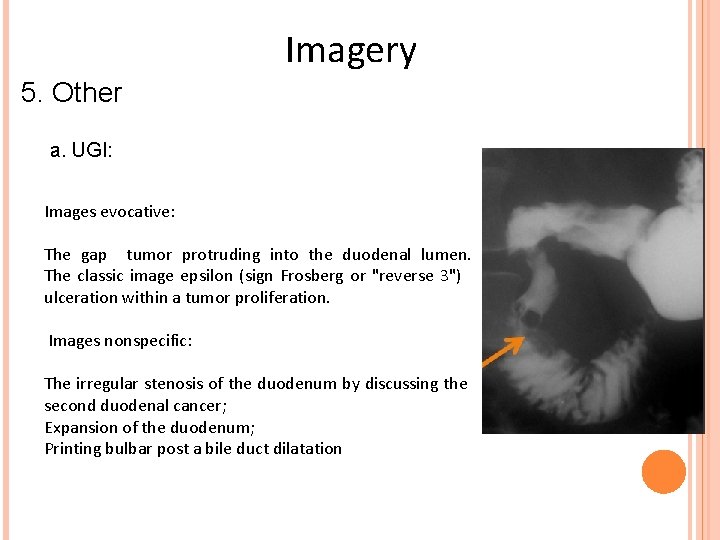
Imagery 5. Other a. UGI: Images evocative: The gap tumor protruding into the duodenal lumen. The classic image epsilon (sign Frosberg or "reverse 3") ulceration within a tumor proliferation. Images nonspecific: The irregular stenosis of the duodenum by discussing the second duodenal cancer; Expansion of the duodenum; Printing bulbar post a bile duct dilatation
Imagery 5. Other: b. Cholangiographie Retrograde Endoscopic (ERCP) It allows: To objectify stricture or bile duct or ampullary gap in intra papillary forms that go unnoticed at duodenoscopy. To complete the review by a wirsungographie possible.
Differential Diagnosis Neoplastic causes: Cancer of the pancreas head The lower bile duct Cholangiocarcinoma Cancer duodenal Non-neoplastic causes: Lithiasis of the CBD; Barrier parasite: cyst, roundworms or flukes. Sclerosing cholangitis; Pancreatitis Inflammatory stenosis of the bile duct. Sphincter of Oddi dysfunction: about 5% of patients suspected of having a DSO have an ampullary; Diverticulum juxta-ampullary: lithiasis and thus promotes misdiagnosis. Benign papilla 'forced' migration after gallstone.
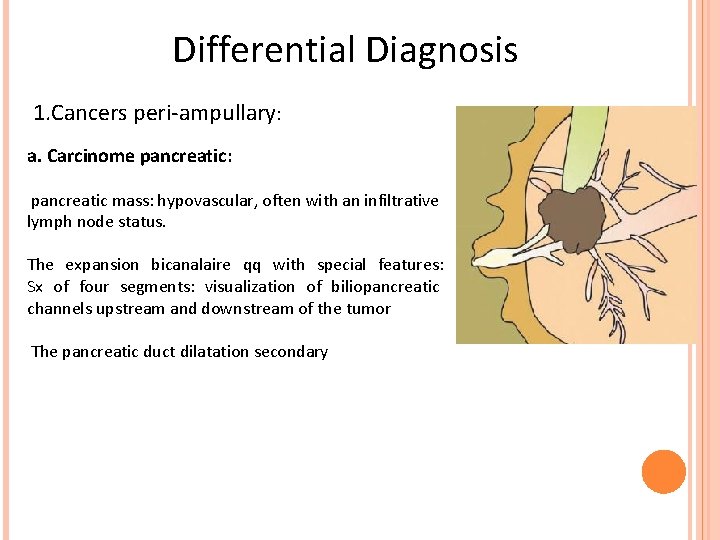
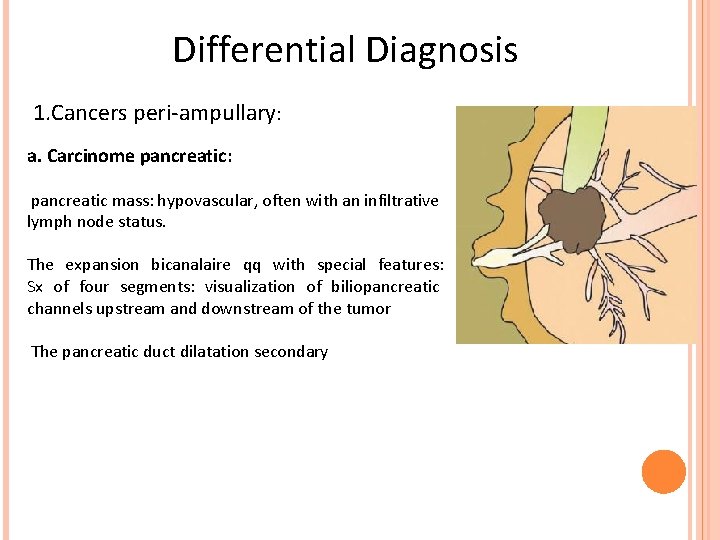
Differential Diagnosis 1. Cancers peri-ampullary: a. Carcinome pancreatic: pancreatic mass: hypovascular, often with an infiltrative lymph node status. The expansion bicanalaire qq with special features: Sx of four segments: visualization of biliopancreatic channels upstream and downstream of the tumor The pancreatic duct dilatation secondary
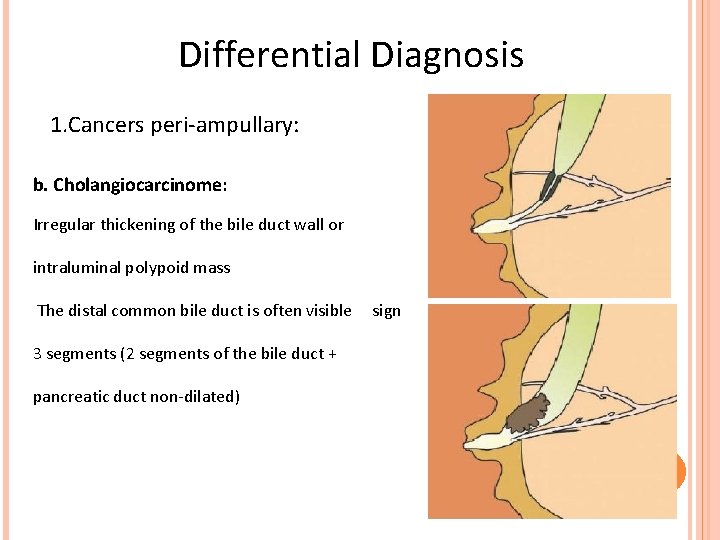
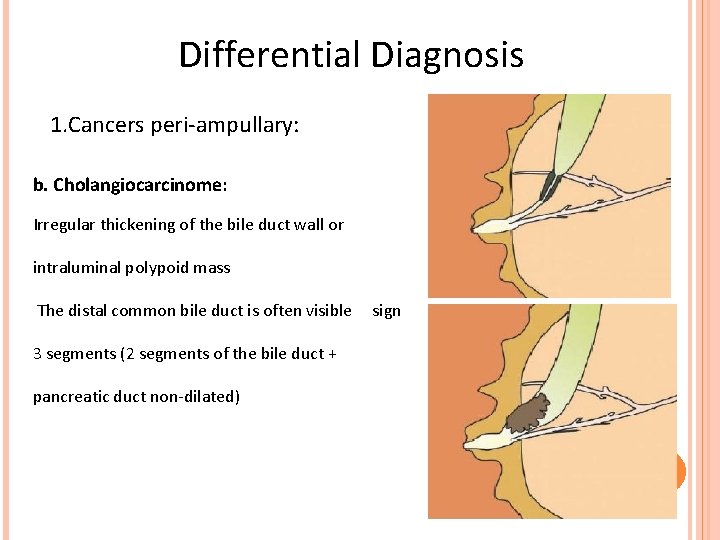
Differential Diagnosis 1. Cancers peri-ampullary: b. Cholangiocarcinome: Irregular thickening of the bile duct wall or intraluminal polypoid mass The distal common bile duct is often visible 3 segments (2 segments of the bile duct + pancreatic duct non-dilated) sign
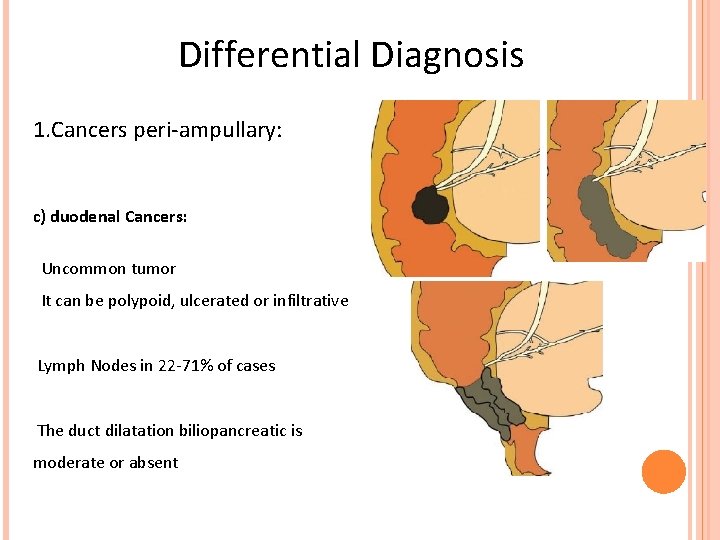
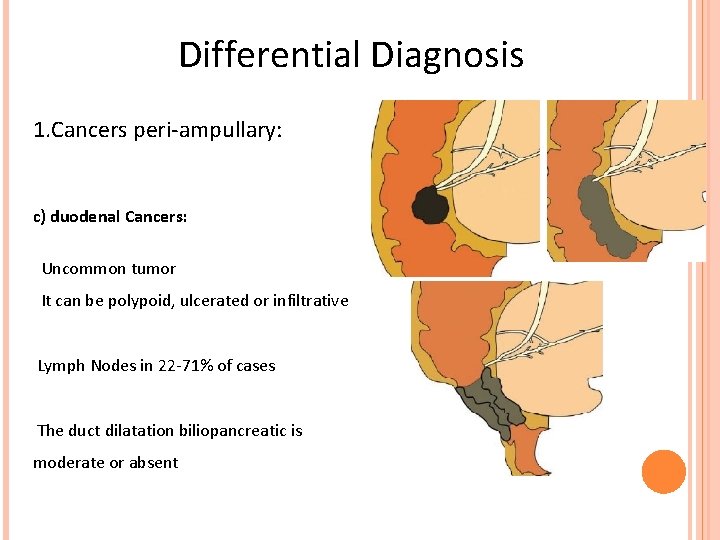
Differential Diagnosis 1. Cancers peri-ampullary: c) duodenal Cancers: Uncommon tumor It can be polypoid, ulcerated or infiltrative Lymph Nodes in 22 -71% of cases The duct dilatation biliopancreatic is moderate or absent
Differential Diagnosis 2. Papillary inflammation: Multiple causes: passage + + + gallstones, cholangitis, pancreatitis or acute infectious (parasitic) Swollen appearance of the papilla with homogeneous enhancement 3. Tumeur intra ductal papillary mucinous pancreas (IPMT): Papillary epithelial proliferation, benign or malignant mucin-producing ductal dilatation Peak age of 60 years with male predominance Imaging: papilla large (> 10 mm) with multicystic dilatation of the pancreatic duct and mural nodules
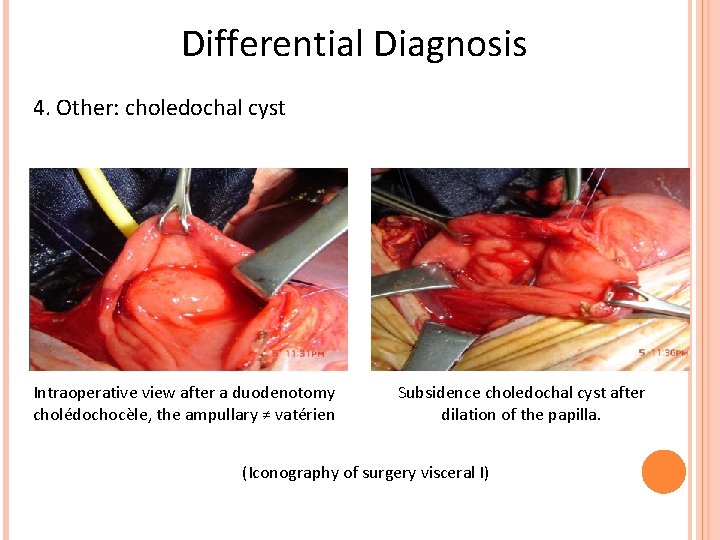
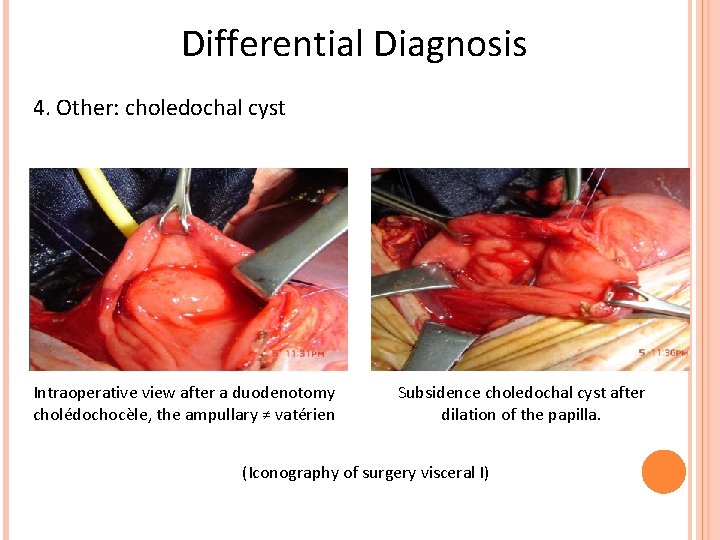
Differential Diagnosis 4. Other: choledochal cyst Intraoperative view after a duodenotomy cholédochocèle, the ampullary ≠ vatérien Subsidence choledochal cyst after dilation of the papilla. (Iconography of surgery visceral I)
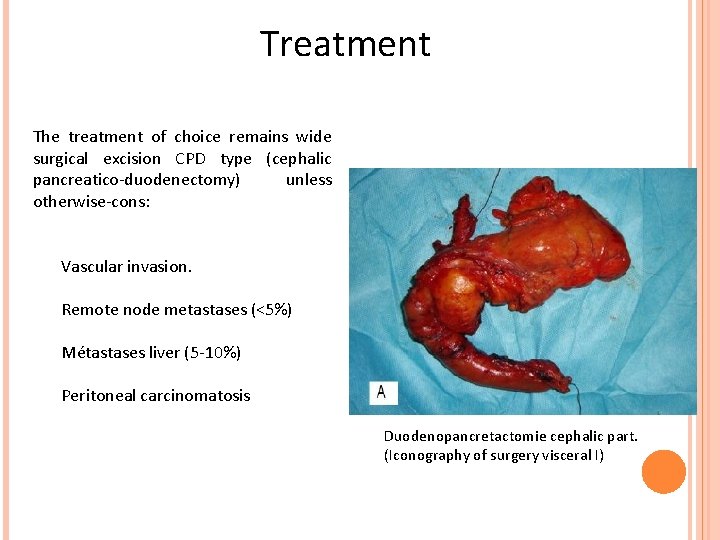
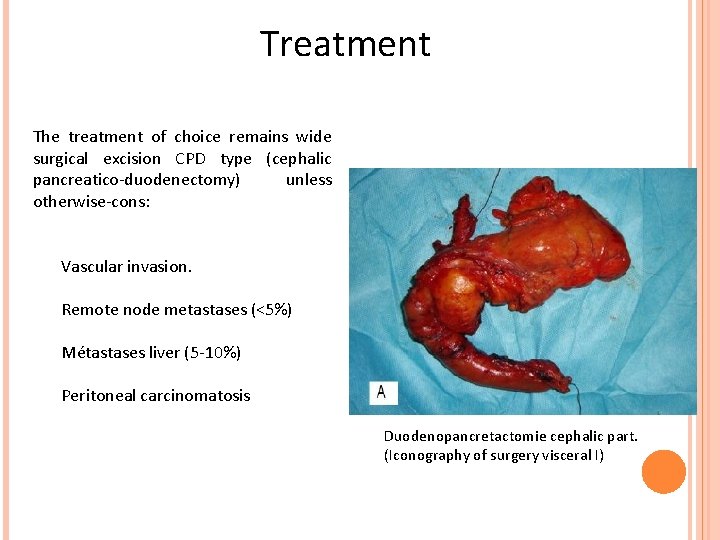
Treatment The treatment of choice remains wide surgical excision CPD type (cephalic pancreatico-duodenectomy) unless otherwise-cons: Vascular invasion. Remote node metastases (<5%) Métastases liver (5 -10%) Peritoneal carcinomatosis Duodenopancretactomie cephalic part. (Iconography of surgery visceral I)
Treatment Other methods: The endoscopic ampullectomy Tm small ampullary benign or malignant is not invading the submucosa duodenal Endoscopic sphincterotomy palliative therapy diagnostic, therapeutic preoperative or Biliary drainage + / - stent grafts: Tm locally advanced Radio-chemotherapy: adjuvant TRT after surgical resection or as palliative
Evolution and prognosis The prognosis is better compared to other peri-ampullary cancers. It is mainly related to nodal involvement. The prognosis is greatly improved by early treatment attitude and thoughtful. The average survival to 5 years is directly related to tumor stage and nodal involvement.
Conclusion The ampulloma vatérien is a rare tumor, often malignant. Always think before a cholestatic jaundice + GI bleeding. Ultrasound is the first review confirm biliary obstruction and determine the level of obstruction. CT, MRI with MRI-Sq Bili are fundamental for the diagnosis and staging. The echo-endoscopy is a great thing if the cross-sectional imaging is inconclusive
 Der cousin meiner mutter ist mein
Der cousin meiner mutter ist mein Cbd ultrasound
Cbd ultrasound Frc control system
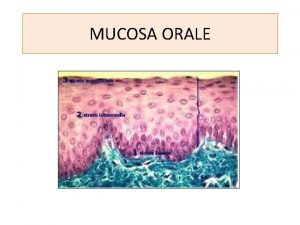
Frc control system Epitelio orale
Epitelio orale Triangle retro molaire
Triangle retro molaire Ligne faîtière dentaire
Ligne faîtière dentaire Sillon gingivo lingual
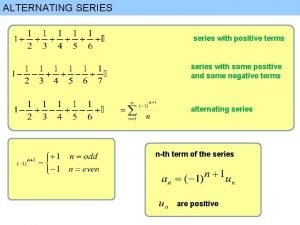
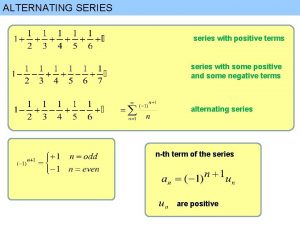
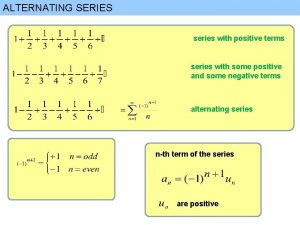
Sillon gingivo lingual Maclaurin series vs taylor series
Maclaurin series vs taylor series Arithmetic series formula
Arithmetic series formula Maclaurin series vs taylor series
Maclaurin series vs taylor series Ibm p series server
Ibm p series server Balmer series lyman series
Balmer series lyman series Voltage shunt feedback amplifier forms
Voltage shunt feedback amplifier forms Taylor series of composite function
Taylor series of composite function Series aiding and series opposing
Series aiding and series opposing Imaging at lafayette surgical specialty hospital
Imaging at lafayette surgical specialty hospital Infinite imaging
Infinite imaging Advantages of paralleling technique
Advantages of paralleling technique Digital imaging artist
Digital imaging artist Kodak 9000 extraoral imaging system
Kodak 9000 extraoral imaging system Study abroad uwe
Study abroad uwe Affordable hyperspectral imaging
Affordable hyperspectral imaging Abbe imaging and spatial filtering experiment
Abbe imaging and spatial filtering experiment Amanda dermer
Amanda dermer Pet imaging
Pet imaging Microsanj
Microsanj Fourier transform in image processing
Fourier transform in image processing Spie medical imaging
Spie medical imaging Nuclear imaging techniques
Nuclear imaging techniques Chapter 39 digital imaging film and radiographs
Chapter 39 digital imaging film and radiographs Hyperspectral imaging
Hyperspectral imaging Astronomy science olympiad 2020
Astronomy science olympiad 2020 Direct imaging subsystem
Direct imaging subsystem Lets person by imaging writing
Lets person by imaging writing Windows image acquisition
Windows image acquisition Almalence
Almalence Cassette construction
Cassette construction Roborio imaging tool
Roborio imaging tool Velocity map imaging
Velocity map imaging Hoglund brain imaging center
Hoglund brain imaging center Spectral imaging
Spectral imaging Enterprise imaging workflow unifier
Enterprise imaging workflow unifier