GETTING UP TO SPEED HOW TO WORK EFFECTIVELY

- Slides: 35
GETTING UP TO SPEED: HOW TO WORK EFFECTIVELY WITH SENIOR ADULTS WITH MENTAL HEALTH AND SUBSTANCE USE DISORDERS Jim Messina, Ph. D. , CCMHC, NCC, DCMHS-T Lecturer Troy University Tampa Bay Site Website Source: http: //coping. us/gerontology. html
What’s the Need for Gerontological Intervention Baby Boomer Focus ■ Following WWII, people around the world settled down to enjoy peace and prosperity and raise families. From 1946 to 1964, the largest generation in history was created: the Baby Boomers (Work. Health. Life, 2019). ■ Because of their sheer numbers, the Boomers radically changed society at every stage of their lives and now that they’re in their 60 s and early 70 s they’re redefining old age and facing some significant mental health challenges. ■ Over 25% of people over 55 experience some form of health issue but many go undiagnosed or untreated (especially men).
The most common mental health issues for people over 50 are: ■ Depression. Risk factors include chronic physical illness and/or pain, diminishing physical functioning, grief and loss, and medications. ■ Anxiety disorders. Traumatic events, social isolation, medical issues, financial concerns and/or impaired memory can increase anxiety in older adults. ■ Dementia. Age, high blood pressure, diabetes, strokes, sedentary lifestyle, head injury, and alcohol abuse are all factors in the development of dementia. After 65, the likelihood of developing some form of dementia increases every five years and by age 85, more than 50 percent of people are affected. ■ Substance abuse or misuse. According to the Institute of Medicine, an estimated 14 to 20 percent of seniors have one or more mental health conditions resulting from misuse or abuse of medications, alcohol or other substances (Work. Health. Life, 2019). ■ Caregiving: is another factor affecting the mental health of many Boomers. Because of advances in medicine and better living conditions, people are living longer and more Boomers find themselves caring for elderly parents, often in their 90 s. Boomers may think they can do it all, even as they enter their senior years, but a lifetime of doing so is putting their physical and certainly mental health at risk (Work. Health. Life, 2019).
Other Issues Facing Baby Boomers ■ One of the central issues that the elderly must cope with is loss. Most people get their first experience with death as children. However, people deal with death much more frequently in their senior years. Particularly difficult are the losses of spouse and lifelong friends (Careers in Psychology, 2019). Other losses aging Baby Boomers face are: ■ Physical impairment impacting mobility ■ Impairments in hearing and vision ■ worsening of overall health ■ If they live long enough, many individuals also deal with the loss of independence and, to some degree, dignity (Careers in Psychology, 2019). A recent study found that One in two women and one in three men will develop dementia, stroke or parkinsonism during their life. These findings strengthen the call for prioritizing the focus on preventive interventions at population level which could substantially reduce the burden of common neurological diseases in the ageing Baby Boomer population (Licher et al. , 2019).
The stages of aging for Baby Boomers First Stage. Independence: In the first stage, they are generally self-reliant and sufficient. They still have the ability to manage simple health problems, chronic ailments and disabilities. They can rely on Their own capabilities and do not need help from loved ones. Second Stage. Interdependence: This is the stage in Baby Boomers’ older adult lives when they are in need of help with basic tasks such as cleaning, doing house chores and other menial tasks. The importance of interdependence is important. This stage may be difficult but nowadays, there are increasingly more options coming up as more and more boomers are finding themselves in the same predicament. Usually, hiring caregivers and domestic helpers may be an option. Group homes and communes are also convenient. Looking for independent living facilities and homes that have strict security, clean rooms, decent meals, laundry services and cleaning service is also highly recommended. Third Stage. Dependence: This stage is when Baby Boomers are in dire need of others to help them with basic daily living activities such as dressing, preparing meals, bathing, grooming, driving, cleaning, shopping and even walking. Boomers can consider continuingcare retirement community in the stage of dependence. These kinds of facilities offer different living arrangements for different people needing care in all stages of their lives.
The stages of aging for Baby Boomers Fourth Stage. Crisis Management: This is the stage where Baby Boomers may be in need of greater care and they may find themselves gravely dependent on health professionals and medical institutions to provide their medical necessities. For older adults who already have chronic ailments early in life or those with a family disposition to certain ailments related to aging, preparing for a crisis in the last stages of their life should be planned well. They must be prepared financially for this, most especially if they are living alone. Cognitive impairments may debilitate them in making decisions for themselves once the crisis starts. Fifth Stage. Institutional Care: The last stage is when Baby Boomers may be in need of extensive medical and personal care. This type of care may be provided by a nursing home or a hospice. Before this period, it is best that they have already prepared a “Durable Medical Power of Attorney” that will make legal decisions about their medical care needs. This will be especially helpful when they may be incapable of communicating or understanding what’s happening around them. The Durable Medical Power of Attorney will make a trusted person (preferably someone they chose) be in charge of overseeing their medical care and make proper health care decisions for them. It includes making decisions on their tests, medications, hydration, nourishment, doctors, hospitals, surgery and rehabilitation facilities they need. (Senior. Living. org, 2018)
Historical Perspective ■ Researchers In 2002 after pointing out that at least one in five people over the age of 65 suffers from a mental disorder and that by 2030 the number of persons with psychiatric disorders in this older group will equal or exceed the number with such disorders in younger age groups (age 18 to 29 or age 30 to 44). And concluding that despite the growing requirement for mental health services for older persons, there is substantial unmet need. These researchers concluded that there is a clear and urgent demographic imperative to address the emerging public health problem of the mental disorders of aging (Bartels, et al. , 2002). ■ In 2007, it was recognized that It cannot be assumed that older adults respond to psychological treatments in the same manner as their younger counterparts. It was around 2007 that there been enough data collected and criteria developed to allow researchers to perform broad reviews of the geropsychology literature to identify specific psychological treatments having the strongest evidence to support their use (Yon & Scogin, 2007). These writers cautioned that not only must the treatment’s merit be considered, but clinicians’ expertise and clients’ values and preferences should be taken into account as well. They concluded that once informed about such treatments, practitioners will have a variety of solid treatments to offer their clients, thus patient choice can be taken into account (Yon & Scogin, 2007). ■ Major barriers limiting practitioners’ implementation of therapeutic interventions with older adults who live in the community either alone or with caregivers included time restraints, costs, and organizational hindrances. Perceived barriers to implementing interventions on behalf of caregivers also included time restraints and the complexity of new interventions. Because both practitioners and caregivers identified time restraints as key obstacles to implementation, issues such as the length of program training, the frequency of intervention delivery, and the time needed to learn documentation procedures were considered in a 2018 report (Juckett & Robinson, 2018).
Predictions about Baby Boomer In reviewing the future needs of the aging Baby Boomers (born between 1946 and 1967), a Bump review was made of the economic and demographic data in 2002 with a simulation of projected socioeconomic and demographic patterns in the year 2030. The results of this study found that there would be real challenges especially in providing for long-term care services for this aging population which numbers close to 61 million people (Knickman & Snell, 2002). This study concluded the following: The real challenges of caring for the elderly in 2030 will involve: 1. Making sure society develops payment and insurance systems for long-term care that work better than existing ones, 2. Taking advantage of advances in medicine and behavioral health to keep the elderly as healthy and active as possible, 3. Changing the way society organizes community services so that care is more accessible, 4. Altering the cultural view of aging to make sure all ages are integrated into the fabric of community life (Knickman & Snell, 2002).
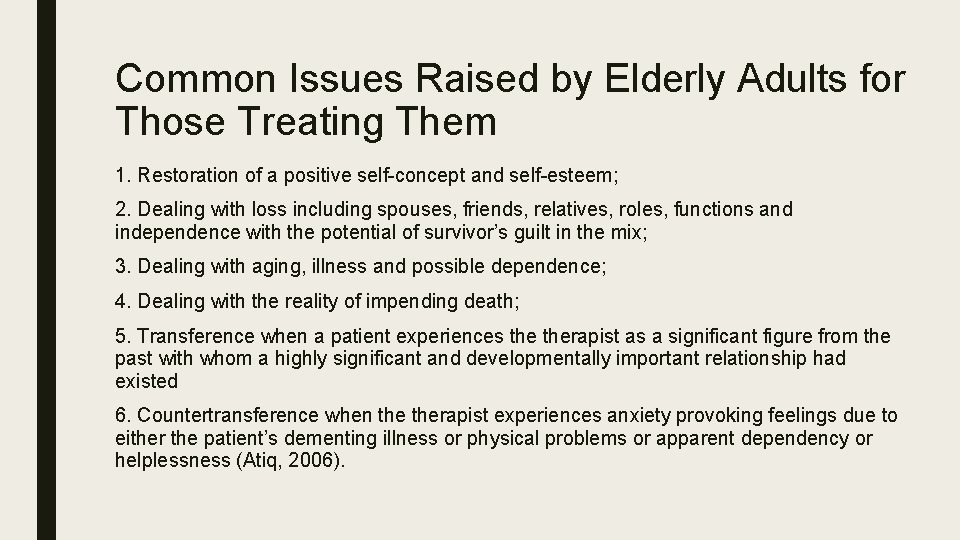
Common Issues Raised by Elderly Adults for Those Treating Them 1. Restoration of a positive self-concept and self-esteem; 2. Dealing with loss including spouses, friends, relatives, roles, functions and independence with the potential of survivor’s guilt in the mix; 3. Dealing with aging, illness and possible dependence; 4. Dealing with the reality of impending death; 5. Transference when a patient experiences therapist as a significant figure from the past with whom a highly significant and developmentally important relationship had existed 6. Countertransference when therapist experiences anxiety provoking feelings due to either the patient’s dementing illness or physical problems or apparent dependency or helplessness (Atiq, 2006).
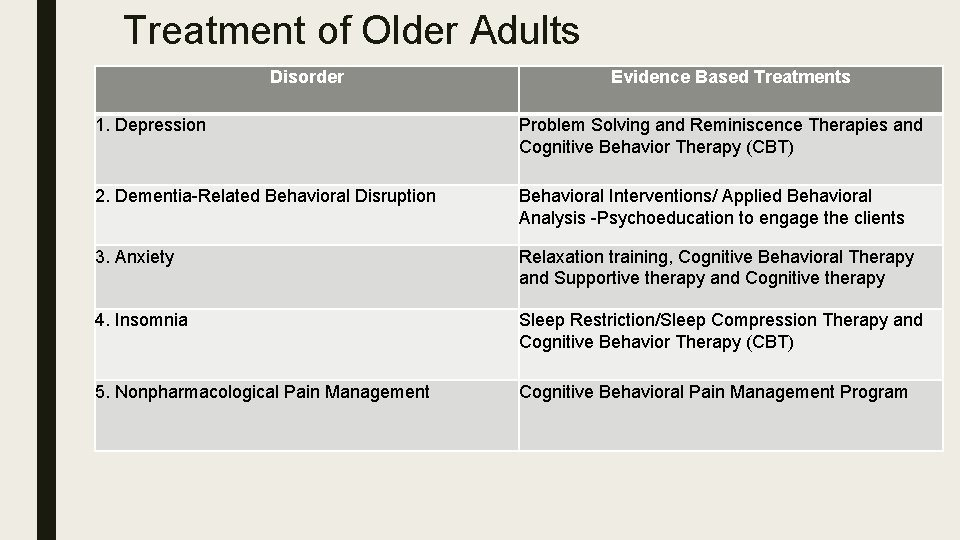
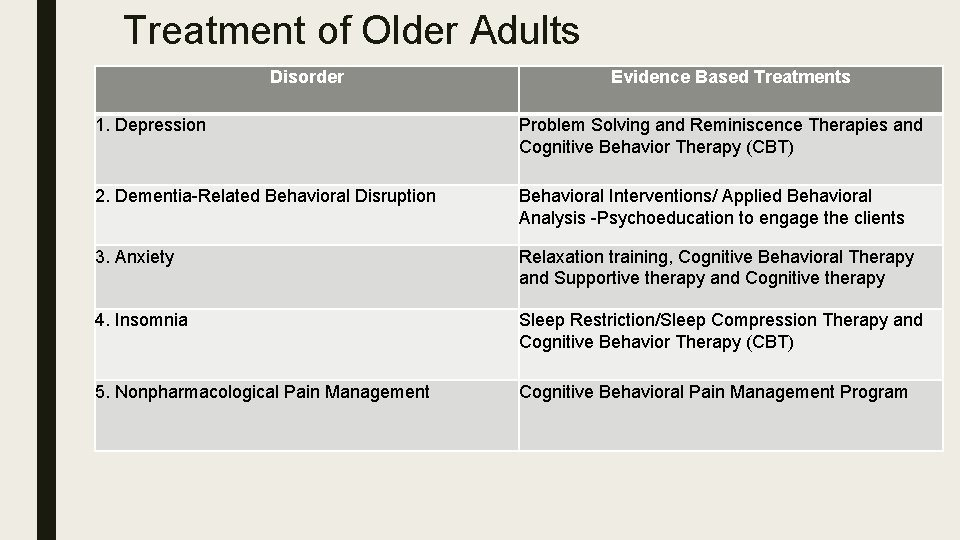
Treatment of Older Adults Disorder Evidence Based Treatments 1. Depression Problem Solving and Reminiscence Therapies and Cognitive Behavior Therapy (CBT) 2. Dementia-Related Behavioral Disruption Behavioral Interventions/ Applied Behavioral Analysis -Psychoeducation to engage the clients 3. Anxiety Relaxation training, Cognitive Behavioral Therapy and Supportive therapy and Cognitive therapy 4. Insomnia Sleep Restriction/Sleep Compression Therapy and Cognitive Behavior Therapy (CBT) 5. Nonpharmacological Pain Management Cognitive Behavioral Pain Management Program
What works well with Older Adults A report in 2004 found that between 1985 and 2004 there was emerging evidence of efficacious psychosocial interventions for older individuals and their families. They concluded that the most consistent support was found for treatments employing: 1. Cognitive-behavioral focused on dealing with depression and other emotional concerns 2. Problem solving focused on improving activities of daily living 3. Reminiscence therapies which is focused on improved coping, lowering anxiety, lessening depression; increasing life satisfaction and higher well-being (Cummings, Kropf, Cassie & Bride, 2004).
IMPACT (Improving Mood—Promoting Access to Collaborative Treatment) ■ A large body of evidence demonstrated IMPACTs effectiveness for treating late-life depression in clients enrolled in a clinical research study, but little was known about how well the collaborative care model translates into treatment provided in a public mental health setting ■ In 2015 it was found that depression severity decreases for 85% of the clients in a public health setting. ■ IMPACT provides older adults with problem solving therapy and antidepressant medications in the public health care setting. ■ Services were delivered by a treatment team consisting of the primary care physician, a consulting psychiatrist, and a depression care specialist (Peukunas & Hahn-Smith, 2015).
Latest Findings on Effective Treatment of Senior In 2019 a study provided the following recommended lifestyle changes which can delay or Adults prevent the onset of Alzheimer’s Disease (AD): ■ Higher levels of physical exercise in cognitively intact older adults are linked with reduced brain amyloid beta deposits ■ Mentally stimulating activities were found to be associated with a reduced risk of developing AD in a cohort of cognitively intact older adults ■ Random Controlled Treatment studies have found that mindfulness-based interventions can modulate inflammatory processes implicated in AD ■ The Mediterranean and DASH diets are associated with better cognitive function and slower cognitive decline ■ Despite some evidence of the benefit of alcohol, non-drinkers should not be advised to begin drinking ■ A multi-domain approach for lifestyle modification should be strongly recommended to cognitively intact older patients The final conclusion of this study was to advise patients that pursuing a healthy lifestyle is a key to delaying or preventing Alzheimer’s disease. This involves managing cardiovascular risk factors and a combination of staying physically, mentally, socially, and spiritually active, in addition to adhering to a healthy diet such as the Mediterranean diet (Khoury, Shoch, Nair, Paracha & Grosberg, 2019).
Dealing with Late-Life Suicide is a tragic, traumatic loss, and one of the most emotionally devastating events families, friends, and communities experience. Suicide claims more than 800, 000 lives every year, and some of the highest rates of suicide in the United States and globally are among older adults (Bucher & Ingram, 2018). The first issue is assessment for late life suicide in older adults which involves an interview with the individual which looks at the following factors: ■ Identification of risk factors, diagnosed medical problems, medications, functional status, nutritional status, personal and family psychiatric history, alcohol or drug use, thorough physical and neurological examination ■ Cognitive functioning mental status examination, including changes in cognition over time; educational level ■ Psychological strengths and symptomatology, coping skills, spirituality, sexuality, suicidal ideation, past attempts at suicide ■ Quality and quantity of social support, fi nancial status, legal history, potential for elder abuse ■ Time course /duration and severity of depressive symptoms to differentiate type of depression (Bucher & Ingram, 2018).
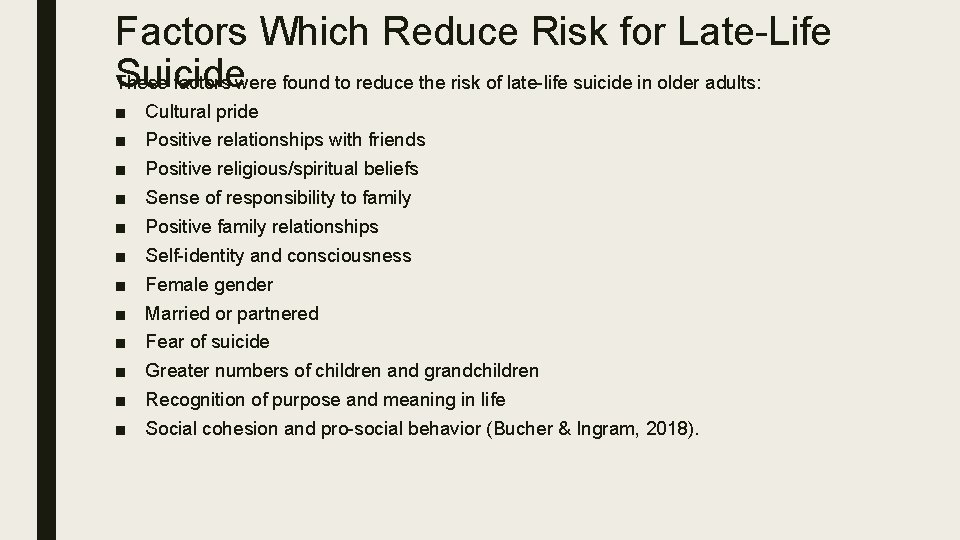
Factors Which Reduce Risk for Late-Life Suicide These factors were found to reduce the risk of late-life suicide in older adults: ■ ■ ■ Cultural pride Positive relationships with friends Positive religious/spiritual beliefs Sense of responsibility to family Positive family relationships Self-identity and consciousness Female gender Married or partnered Fear of suicide Greater numbers of children and grandchildren Recognition of purpose and meaning in life Social cohesion and pro-social behavior (Bucher & Ingram, 2018).
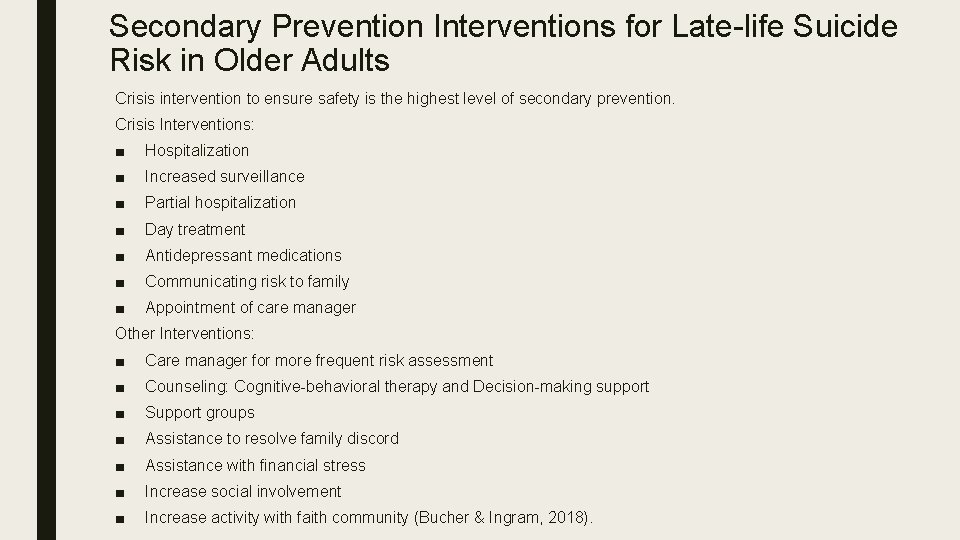
Secondary Prevention Interventions for Late-life Suicide Risk in Older Adults Crisis intervention to ensure safety is the highest level of secondary prevention. Crisis Interventions: ■ Hospitalization ■ Increased surveillance ■ Partial hospitalization ■ Day treatment ■ Antidepressant medications ■ Communicating risk to family ■ Appointment of care manager Other Interventions: ■ Care manager for more frequent risk assessment ■ Counseling: Cognitive-behavioral therapy and Decision-making support ■ Support groups ■ Assistance to resolve family discord ■ Assistance with financial stress ■ Increase social involvement ■ Increase activity with faith community (Bucher & Ingram, 2018).
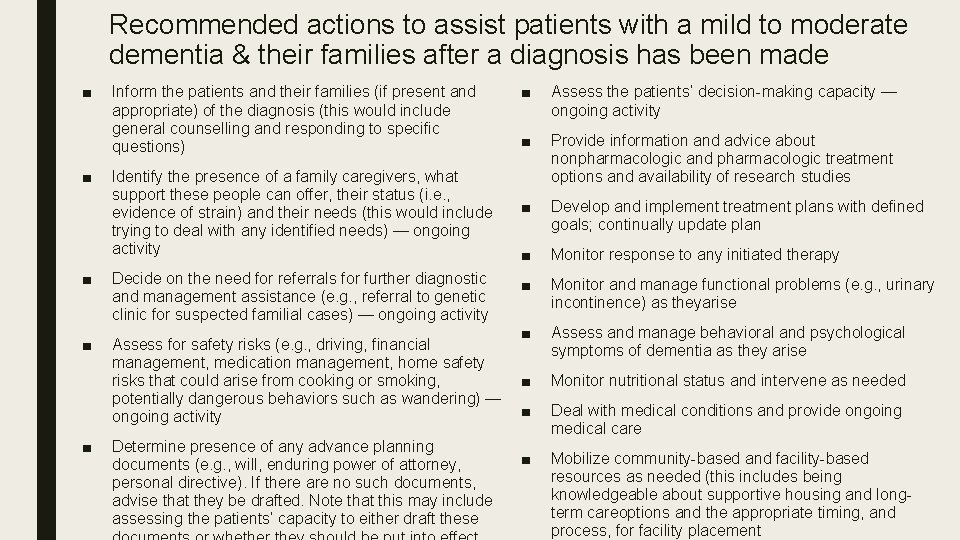
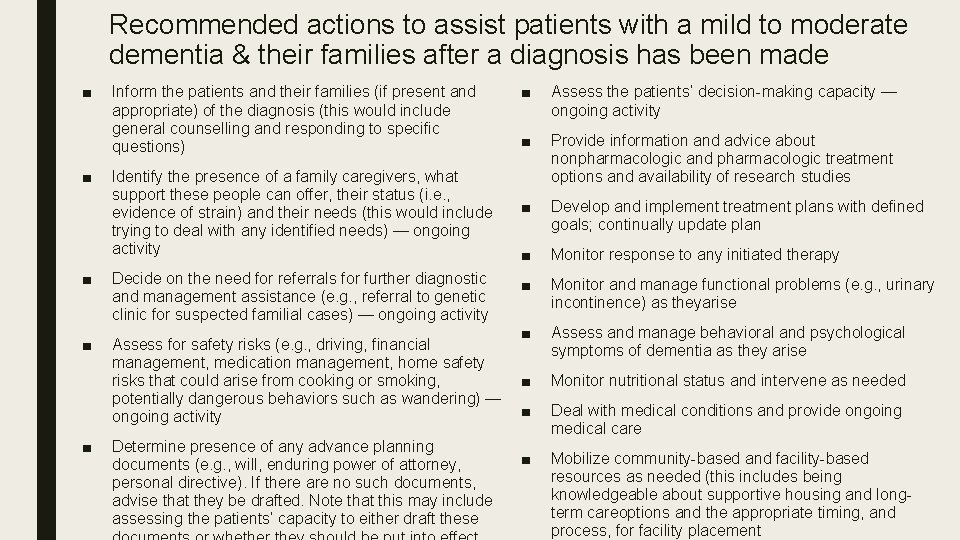
Recommended actions to assist patients with a mild to moderate dementia & their families after a diagnosis has been made ■ ■ Inform the patients and their families (if present and appropriate) of the diagnosis (this would include general counselling and responding to specific questions) Identify the presence of a family caregivers, what support these people can offer, their status (i. e. , evidence of strain) and their needs (this would include trying to deal with any identified needs) — ongoing activity ■ Decide on the need for referrals for further diagnostic and management assistance (e. g. , referral to genetic clinic for suspected familial cases) — ongoing activity ■ Assess for safety risks (e. g. , driving, financial management, medication management, home safety risks that could arise from cooking or smoking, potentially dangerous behaviors such as wandering) — ongoing activity ■ Determine presence of any advance planning documents (e. g. , will, enduring power of attorney, personal directive). If there are no such documents, advise that they be drafted. Note that this may include assessing the patients’ capacity to either draft these ■ Assess the patients’ decision-making capacity — ongoing activity ■ Provide information and advice about nonpharmacologic and pharmacologic treatment options and availability of research studies ■ Develop and implement treatment plans with defined goals; continually update plan ■ Monitor response to any initiated therapy ■ Monitor and manage functional problems (e. g. , urinary incontinence) as theyarise ■ Assess and manage behavioral and psychological symptoms of dementia as they arise ■ Monitor nutritional status and intervene as needed ■ Deal with medical conditions and provide ongoing medical care ■ Mobilize community-based and facility-based resources as needed (this includes being knowledgeable about supportive housing and longterm careoptions and the appropriate timing, and process, for facility placement

4 Reminiscence Therapy Activities 1. Listen to their favorite music: Music helps people reminisce and relate to emotions and past experiences. That’s why it’s often recommended for those with Alzheimer’s or dementia. Music can even reach seniors with very advanced dementia. You can play their favorite songs, have a little sing-along, or play music on simple instruments like shakers, bells, tambourines, or a do it yourself drum. 2. Look through photos or keepsakes: Pictures or keepsakes that bring back memories are another excellent way to reminisce. Photos of family, friends, and important life events are always good choices. Photos of things that remind them of favorite hobbies are also great. For example, someone who loves to garden might enjoy looking at a gardening magazine or plant catalog. Someone who loved to cook might like a gourmet magazine with beautiful food photos. The same goes for sports, crafts, historical events, etc. 3. Smell familiar scents and taste favorite foods: Smell is a powerful way to access memories. You could create scent cards or jars with smells that remind them of favorite foods (use spices) or a location like a pine forest near their childhood home (use fresh pine needles or pine scented sticks). Taste is another way to evoke fond memories. Maybe they always made a special dish for holiday celebrations – the facilitator could make it for them and reminisce while eating together. Or maybe the facilitator could recreate a favorite snack they made for as a treat when their children were young. 4. Enjoy tactile activities like painting, pottery, or other crafts: Touch can also remind someone of the past. Familiar tactile activities like drawing, painting, pottery, knitting, sewing, or other crafts can spark old memories. Even if they can’t participate in these hobbies anymore, doing things like touching paintbrushes, swirling watercolors, scribbling with drawing chalk, squeezing yarn, or playing with fabrics can evoke strong memories. Another way to use touch is through objects. Maybe wearing or handling favorite pieces of jewelry or accessories (like a watch or a necklace) would bring up memories of significant life events. Other ideas would be to bring out a significant piece of clothing (maybe a dress or suit) that they used to love or wear to important events.
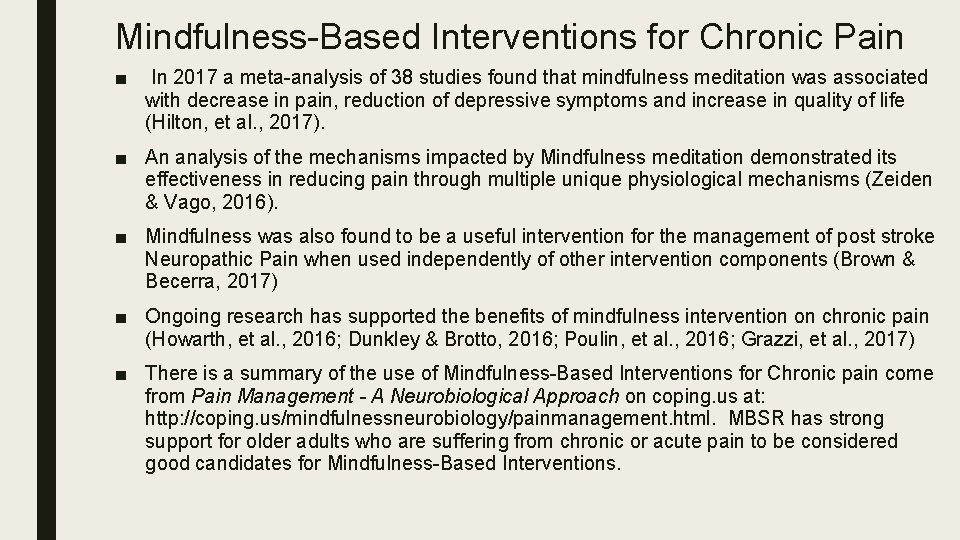
Mindfulness-Based Interventions for Chronic Pain ■ In 2017 a meta-analysis of 38 studies found that mindfulness meditation was associated with decrease in pain, reduction of depressive symptoms and increase in quality of life (Hilton, et al. , 2017). ■ An analysis of the mechanisms impacted by Mindfulness meditation demonstrated its effectiveness in reducing pain through multiple unique physiological mechanisms (Zeiden & Vago, 2016). ■ Mindfulness was also found to be a useful intervention for the management of post stroke Neuropathic Pain when used independently of other intervention components (Brown & Becerra, 2017) ■ Ongoing research has supported the benefits of mindfulness intervention on chronic pain (Howarth, et al. , 2016; Dunkley & Brotto, 2016; Poulin, et al. , 2016; Grazzi, et al. , 2017) ■ There is a summary of the use of Mindfulness-Based Interventions for Chronic pain come from Pain Management - A Neurobiological Approach on coping. us at: http: //coping. us/mindfulnessneurobiology/painmanagement. html. MBSR has strong support for older adults who are suffering from chronic or acute pain to be considered good candidates for Mindfulness-Based Interventions.
Frailty of Elderly Frailty is an age-related state of decreased physiological reserves characterized by an increased risk of poor clinical outcomes. Evidence supporting the malleability of frailty, its prevention and treatment, was researched in 2018. Results looked for included: 1. Cognition, quality of life, activities of daily living, caregiver burden, functional capacity, depression and other mental health-related outcomes, self-perceived health and social engagement; 2. Drugs and prescriptions, analytical parameters, adverse outcomes and comorbidities; 3. Costs, and/or costs relative to benefits and/or savings associated with implementing the interventions for frailty. The findings were that physical exercise programs were shown to be generally effective for reducing or postponing frailty but only when conducted in groups. Favorable effects on frailty indicators were also observed after the interventions, based on physical exercise with supplementation, supplementation alone, cognitive training and combined treatment (Apostolo, et al. , 2018).
Increase Physical Activity in Older Adults In the 2018 U. S. Department of Health and Human Services Physical Activity Guidelines for Americans, its key guidelines for adults also apply to older adults they are: ■ Adults should move more and sit less throughout the day. Some physical activity is better than none. Adults who sit less and do any amount of moderate-to-vigorous physical activity gain some health benefits. ■ For substantial health benefits, adults should do at least 150 minutes (2 hours and 30 minutes) to 300 minutes (5 hours) a week of moderate-intensity, or 75 minutes (1 hour and 15 minutes) to 150 minutes (2 hours and 30 minutes) a week of vigorous-intensity aerobic physical activity, or an equivalent combination of moderate- and vigorous-intensity aerobic activity. Preferably, aerobic activity should be spread throughout the week. ■ Additional health benefits are gained by engaging in physical activity beyond the equivalent of 300 minutes (5 hours) of moderate-intensity physical activity a week. ■ Adults should also do muscle-strengthening activities of moderate or greater intensity and that involve all major muscle groups on 2 or more days a week, as these activities provide additional health benefits In addition to the adult guidelines, the following key guidelines are just for older adults: ■ As part of their weekly physical activity, older adults should do multicomponent physical activity that includes balance training as well as aerobic and muscle-strengthening activities. ■ Older adults should determine their level of effort for physical activity relative to their level of fitness. ■ Older adults with chronic conditions should understand whether and how their conditions affect their ability to do regular physical activity safely. ■ When older adults cannot do 150 minutes of moderate-intensity aerobic activity a week because of chronic conditions, they should be as physically active as their abilities and conditions allow (US HHS,
Independent vs Supervised Living Conditions for Frail Elderly In working in geriatric rehabilitation settings which serve frail geriatric patients who are over 80 years of age The goal of rehabilitation treatment in this population is to help patients ■ maximize their functional independence and ■ regain autonomy to the greatest extent possible to safely resume independent living. These Seniors are typically evaluated in rehabilitation centers post-acute hospitalization for ■ stroke, ■ orthopedic injury, ■ Parkinson’s disease or other functional deconditioning. The discharge goals were to either 1. return home, 2. return home with support services, 3. go to a residential placement or long-term care placement. The majority of these frail patients went home on their own or home with support services at that time (Patrick, Leclerc & Perugini, 2003).
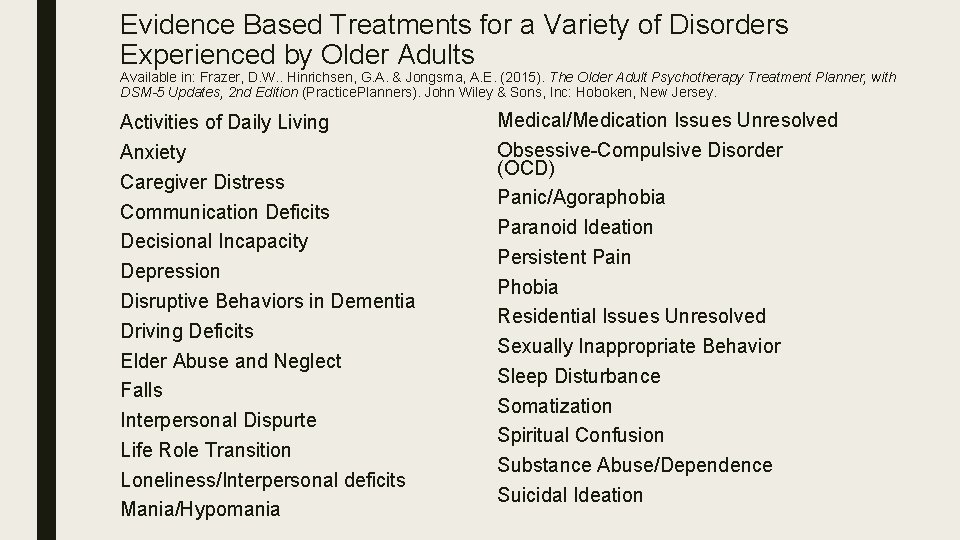
Evidence Based Treatments for a Variety of Disorders Experienced by Older Adults Available in: Frazer, D. W. . Hinrichsen, G. A. & Jongsma, A. E. (2015). The Older Adult Psychotherapy Treatment Planner, with DSM-5 Updates, 2 nd Edition (Practice. Planners). John Wiley & Sons, Inc: Hoboken, New Jersey. Activities of Daily Living Anxiety Caregiver Distress Communication Deficits Decisional Incapacity Depression Disruptive Behaviors in Dementia Driving Deficits Elder Abuse and Neglect Falls Interpersonal Dispurte Life Role Transition Loneliness/Interpersonal deficits Mania/Hypomania Medical/Medication Issues Unresolved Obsessive-Compulsive Disorder (OCD) Panic/Agoraphobia Paranoid Ideation Persistent Pain Phobia Residential Issues Unresolved Sexually Inappropriate Behavior Sleep Disturbance Somatization Spiritual Confusion Substance Abuse/Dependence Suicidal Ideation
Ethical Consideration in Work with Senior The process of capacity assessment is dominated by a fundamental tension between two core ethical Adults principles: autonomy (self-determination) and protection (beneficence). What should clinicians do when an older adult, particularly one who is frail, vulnerable, dementing, or eccentric, begins to make decisions that put the elder or others in danger, or that are inconsistent with the person’s long-held values? At what point does decision making that is affected by a neuropsychiatric disease process no longer represent ‘‘competent’’ decision making? These are some of the essential, and perplexing, questions of clinical capacity assessment (Moye & Marson, 2007). The term capacity refers to a dichotomous (yes or no) judgment by a clinician or other professional as to whether an individual can perform a specific task (such as driving or living independently) or make a specific decision (such as consenting to health care or changing a will). There at least eight major capacity domains of relevance to older adults with neuropsychiatric illness. ■ 1. Independent living, ■ 2. General financial management and ■ 3. Driving, require a broad set of cognitive and procedural skills and are frequently subject to judicial review. Other capacities, ■ 4. Treatment consent, ■ 5. Testamentary capacity (wills), ■ 6. Research consent, ■ 7. Sexual consent, and ■ 8. Voting are generally narrower in scope, focusing on one or a small number of specific decisions requiring an underlying set of cognitive abilities. These narrow capacities, although technically legal capacities, are rarely subject to judicial review (Moye & Marson, 2007).
ELDERLY AND SUDS Jim Messina, Ph. D. , CCMHC, NCC, DCMHS-T
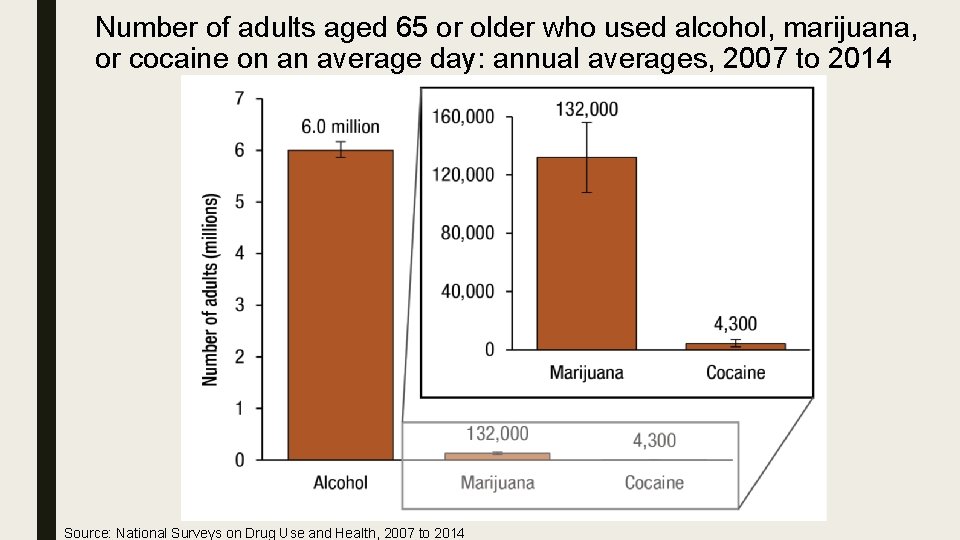
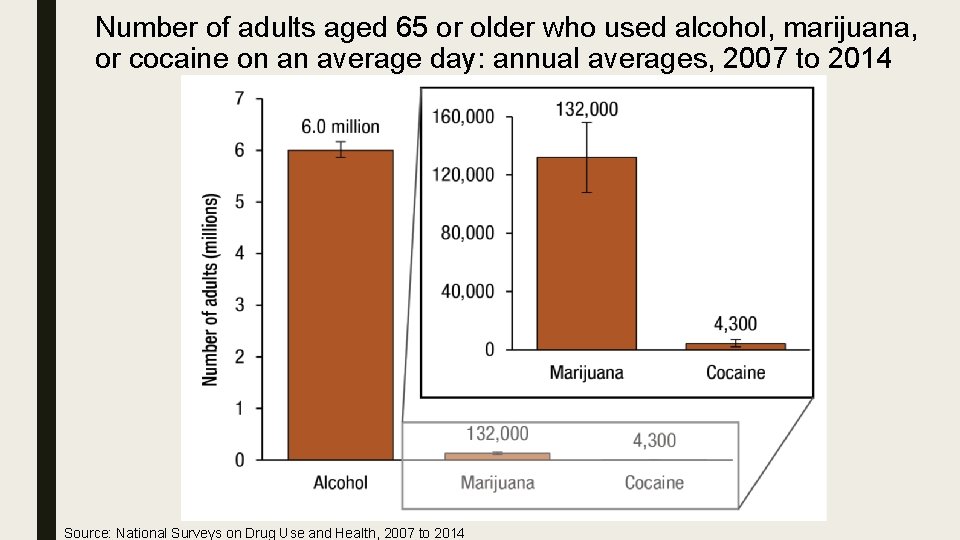
Number of adults aged 65 or older who used alcohol, marijuana, or cocaine on an average day: annual averages, 2007 to 2014 Source: National Surveys on Drug Use and Health, 2007 to 2014
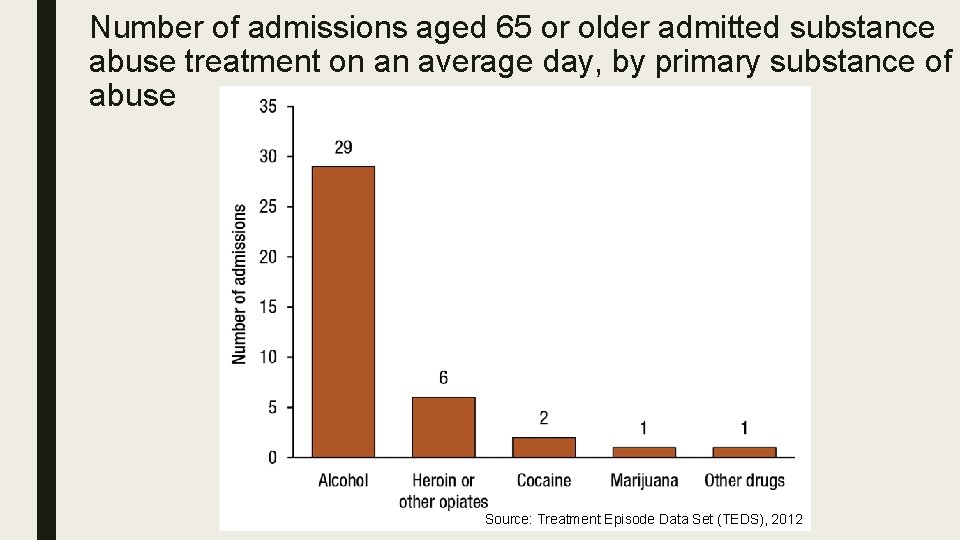
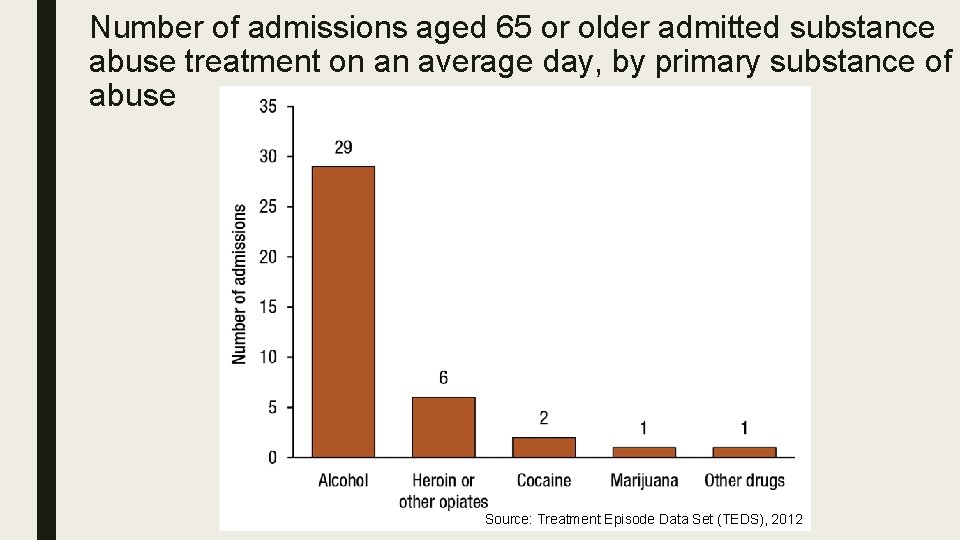
Number of admissions aged 65 or older admitted substance abuse treatment on an average day, by primary substance of abuse Source: Treatment Episode Data Set (TEDS), 2012
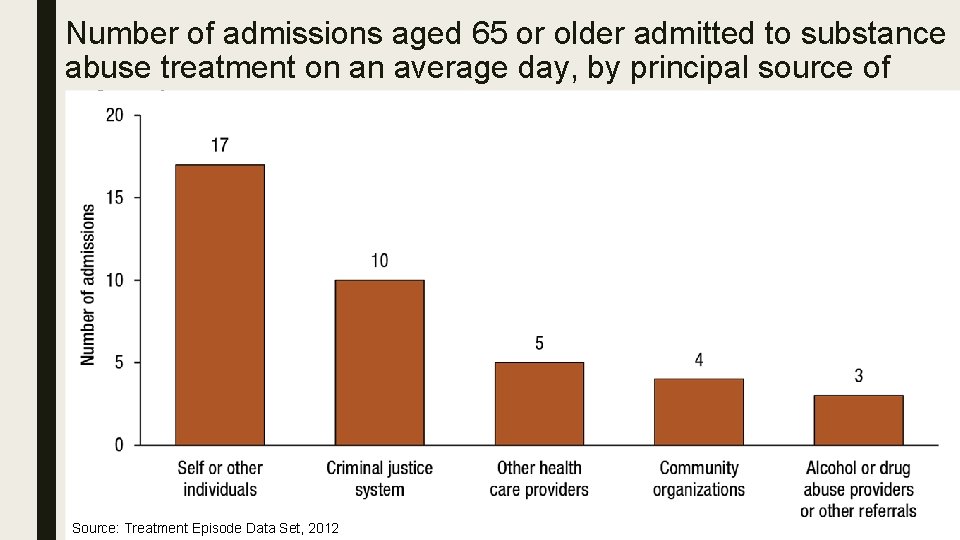
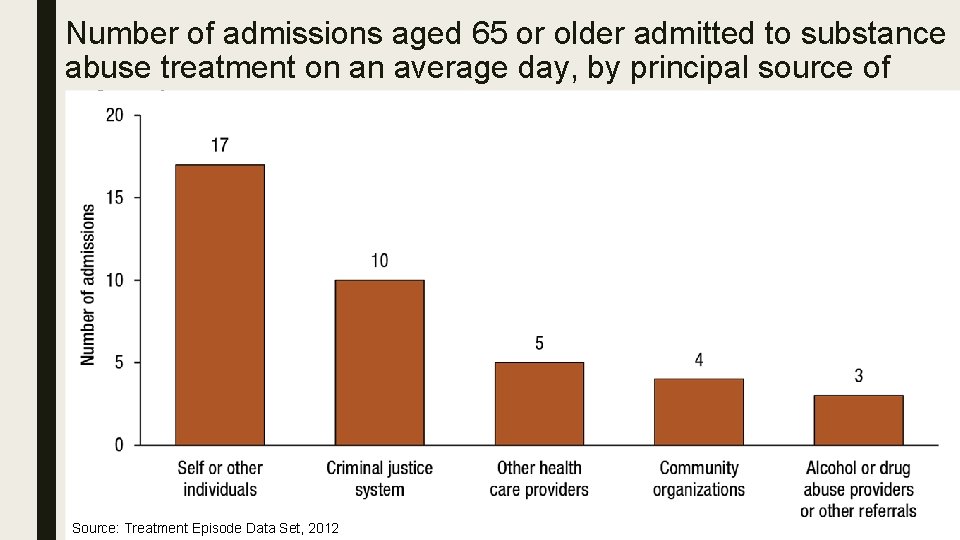
Number of admissions aged 65 or older admitted to substance abuse treatment on an average day, by principal source of referral Source: Treatment Episode Data Set, 2012
Conclusion Across all data sets, alcohol emerges as a source of concern. ■ TEDS data show that most substance use admissions for people 65 or older were primarily for alcohol. ■ People aged 65 years of older are more sensitive to the effects of alcohol. ■ Alcohol can interact dangerously with medications taken by older adults and may also exacerbate common medical conditions, including stroke, high blood pressure, diabetes, osteoporosis, memory loss, and mood disorders.
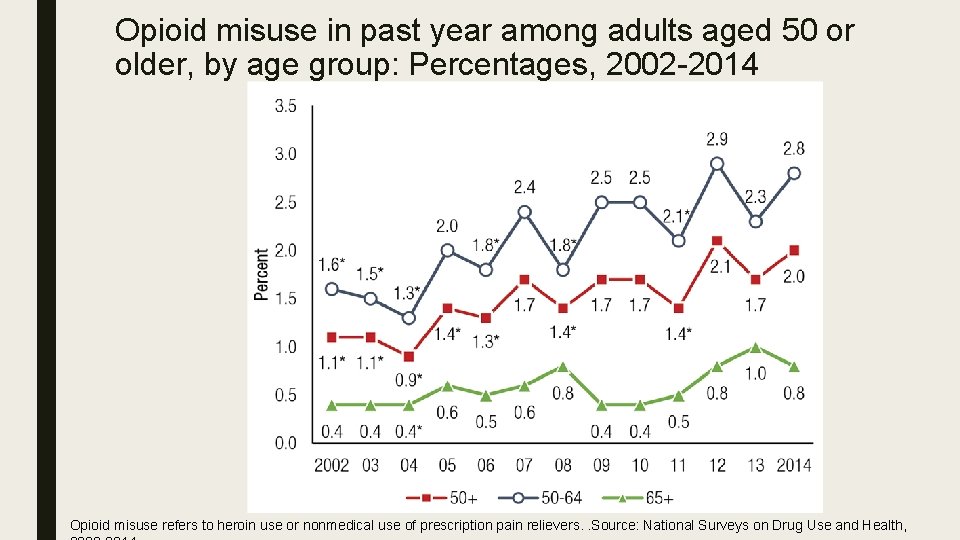
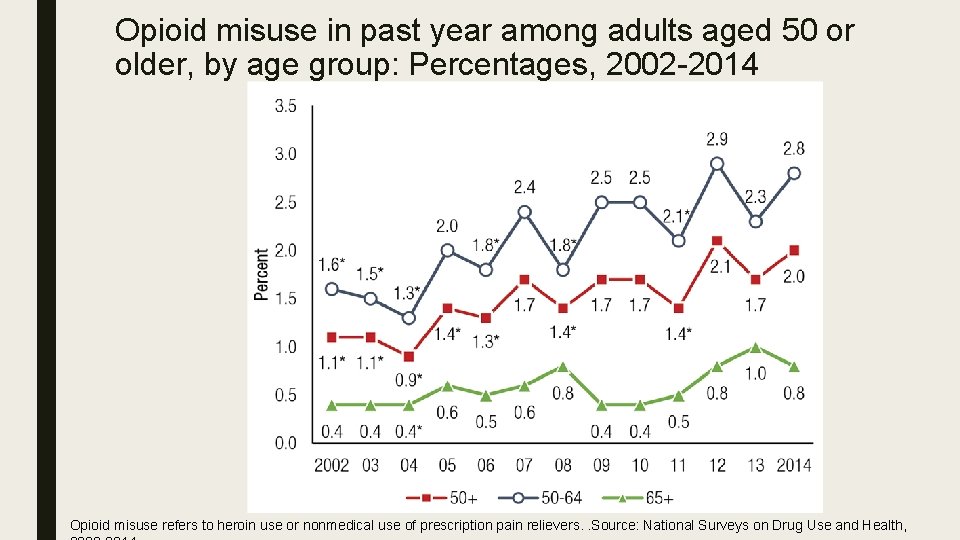
Opioid misuse in past year among adults aged 50 or older, by age group: Percentages, 2002 -2014 Opioid misuse refers to heroin use or nonmedical use of prescription pain relievers. . Source: National Surveys on Drug Use and Health,
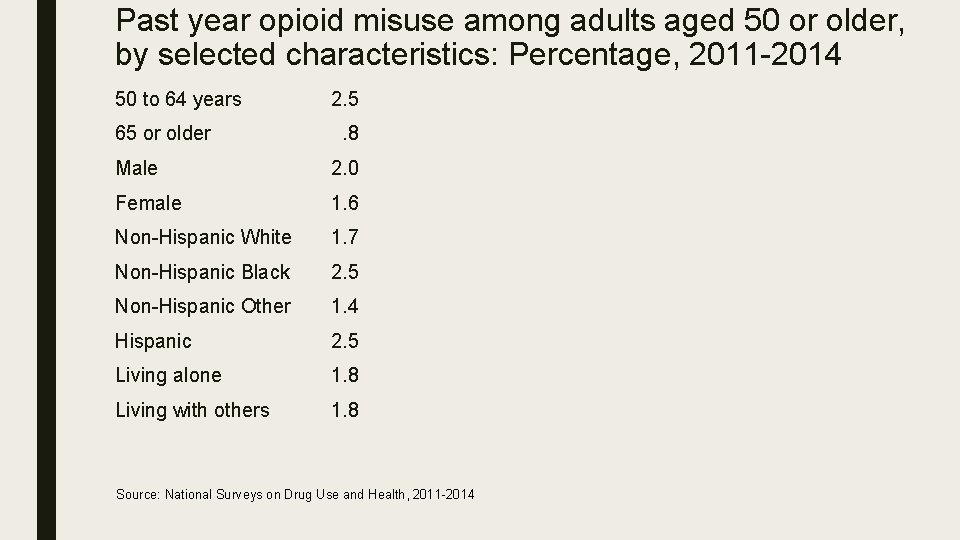
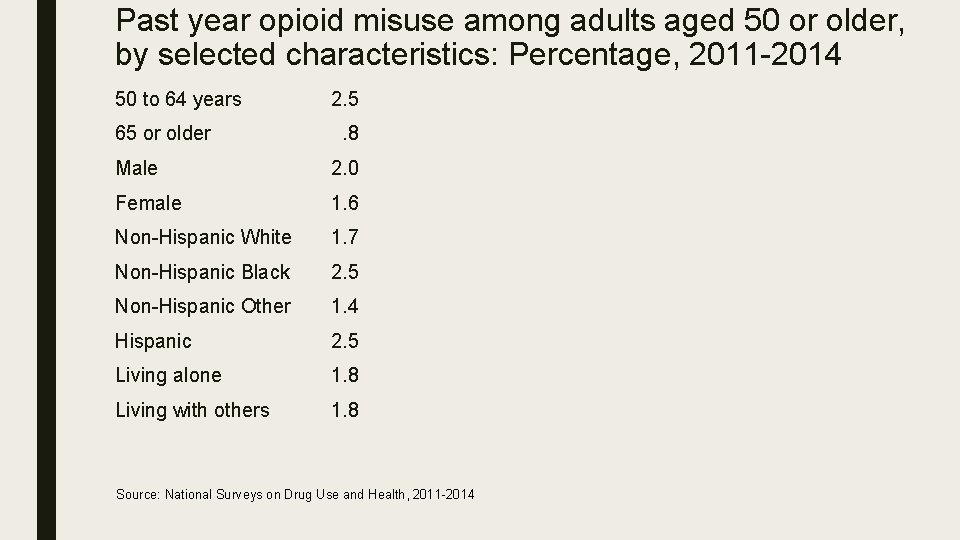
Past year opioid misuse among adults aged 50 or older, by selected characteristics: Percentage, 2011 -2014 50 to 64 years 65 or older 2. 5. 8 Male 2. 0 Female 1. 6 Non-Hispanic White 1. 7 Non-Hispanic Black 2. 5 Non-Hispanic Other 1. 4 Hispanic 2. 5 Living alone 1. 8 Living with others 1. 8 Source: National Surveys on Drug Use and Health, 2011 -2014
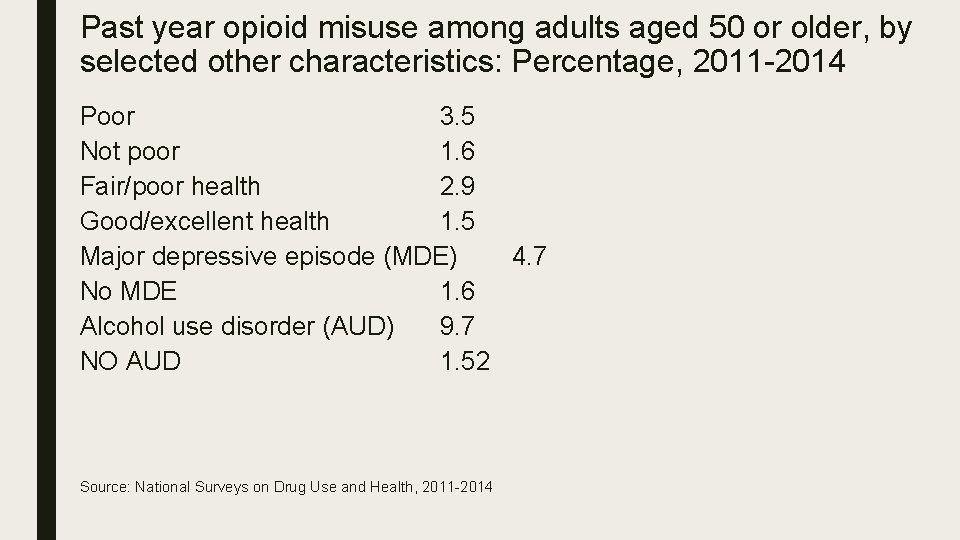
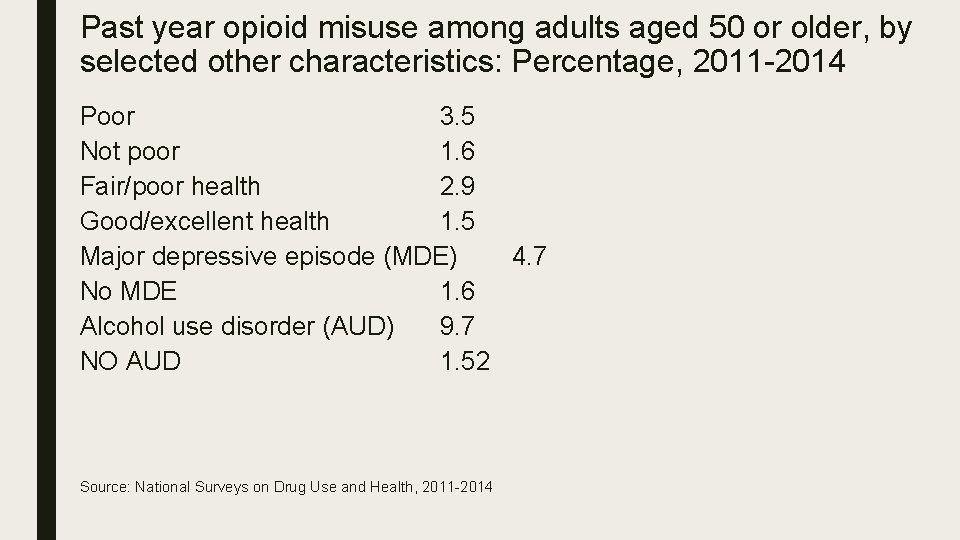
Past year opioid misuse among adults aged 50 or older, by selected other characteristics: Percentage, 2011 -2014 Poor 3. 5 Not poor 1. 6 Fair/poor health 2. 9 Good/excellent health 1. 5 Major depressive episode (MDE) 4. 7 No MDE 1. 6 Alcohol use disorder (AUD) 9. 7 NO AUD 1. 52 Source: National Surveys on Drug Use and Health, 2011 -2014
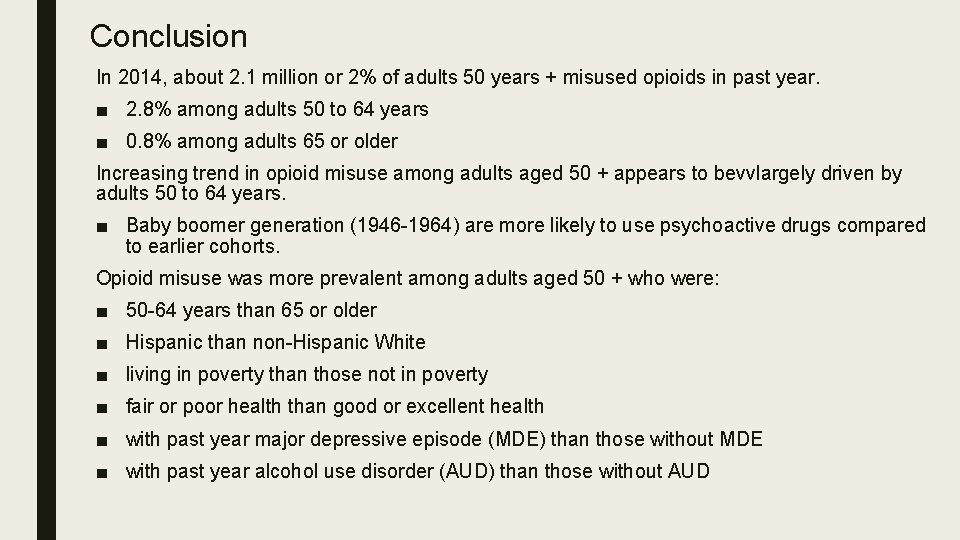
Conclusion In 2014, about 2. 1 million or 2% of adults 50 years + misused opioids in past year. ■ 2. 8% among adults 50 to 64 years ■ 0. 8% among adults 65 or older Increasing trend in opioid misuse among adults aged 50 + appears to bevvlargely driven by adults 50 to 64 years. ■ Baby boomer generation (1946 -1964) are more likely to use psychoactive drugs compared to earlier cohorts. Opioid misuse was more prevalent among adults aged 50 + who were: ■ 50 -64 years than 65 or older ■ Hispanic than non-Hispanic White ■ living in poverty than those not in poverty ■ fair or poor health than good or excellent health ■ with past year major depressive episode (MDE) than those without MDE ■ with past year alcohol use disorder (AUD) than those without AUD
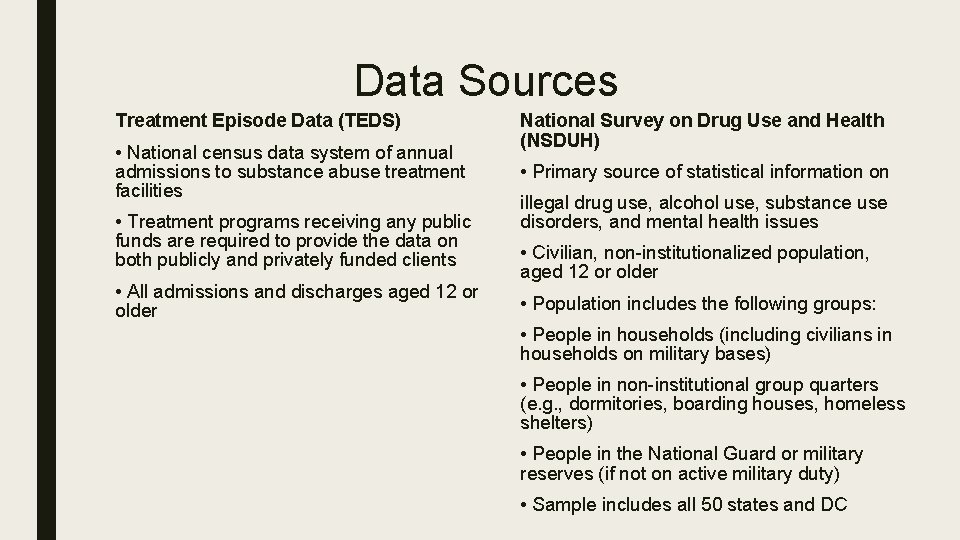
Data Sources Treatment Episode Data (TEDS) • National census data system of annual admissions to substance abuse treatment facilities • Treatment programs receiving any public funds are required to provide the data on both publicly and privately funded clients • All admissions and discharges aged 12 or older National Survey on Drug Use and Health (NSDUH) • Primary source of statistical information on illegal drug use, alcohol use, substance use disorders, and mental health issues • Civilian, non-institutionalized population, aged 12 or older • Population includes the following groups: • People in households (including civilians in households on military bases) • People in non-institutional group quarters (e. g. , dormitories, boarding houses, homeless shelters) • People in the National Guard or military reserves (if not on active military duty) • Sample includes all 50 states and DC
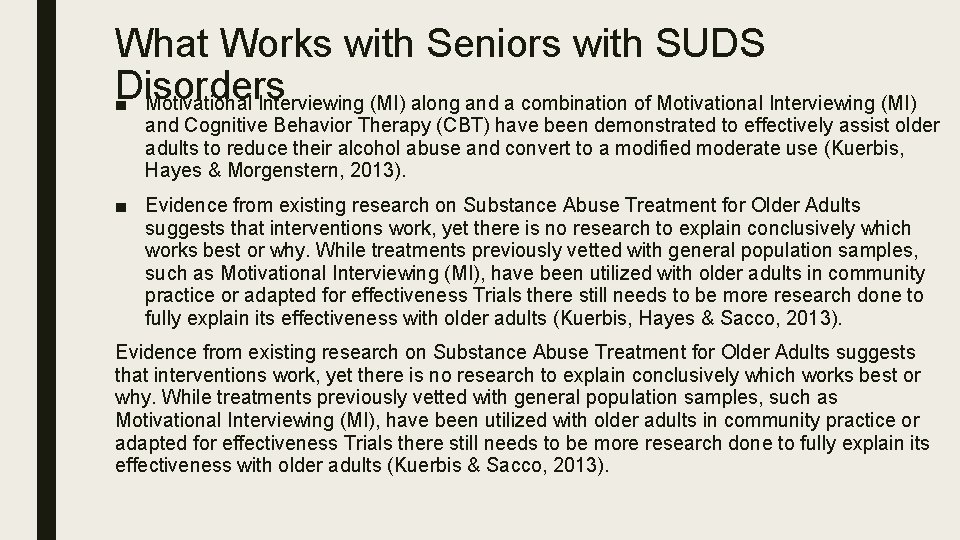
What Works with Seniors with SUDS Disorders ■ Motivational Interviewing (MI) along and a combination of Motivational Interviewing (MI) and Cognitive Behavior Therapy (CBT) have been demonstrated to effectively assist older adults to reduce their alcohol abuse and convert to a modified moderate use (Kuerbis, Hayes & Morgenstern, 2013). ■ Evidence from existing research on Substance Abuse Treatment for Older Adults suggests that interventions work, yet there is no research to explain conclusively which works best or why. While treatments previously vetted with general population samples, such as Motivational Interviewing (MI), have been utilized with older adults in community practice or adapted for effectiveness Trials there still needs to be more research done to fully explain its effectiveness with older adults (Kuerbis, Hayes & Sacco, 2013). Evidence from existing research on Substance Abuse Treatment for Older Adults suggests that interventions work, yet there is no research to explain conclusively which works best or why. While treatments previously vetted with general population samples, such as Motivational Interviewing (MI), have been utilized with older adults in community practice or adapted for effectiveness Trials there still needs to be more research done to fully explain its effectiveness with older adults (Kuerbis & Sacco, 2013).