Getting to Zero in San Francisco Consortium Zero





















- Slides: 51

“Getting to Zero” in San Francisco Consortium Zero new HIV infections Zero HIV deaths Zero stigma and discrimination Photo by Jim Herd
Agenda 1. 2. 3. 4. Welcome & Overview Update on Funding SF HIV Epidemiology Data Committee updates – – Pr. EP RAPID Ending Stigma Retention & Re‐engagement 5. Panel Discussion: HIV Navigation 6. Thank you Will Hagerty
Getting to Zero SF: What are we? • Multi-sector independent consortium– operates under principles of collective impact: “Commitment of groups from different sectors to a common agenda to solve a specific problem. ” • Vision Become the first municipal jurisdiction in the United States to achieve the UNAIDS vision of “Getting to Zero”

GTZ reach since last meeting • Government § SF part of FTCI launch and website § Updates with DPH Director Barbara Garcia and Senator Feinstein § Health Commission presentation 9/22 § Update to National Institutes of Health and DC City efforts • Conferences- Community and Scientific – Adherence 2016, May 9 -11 – AIDS 2016, July 18 -22 – USCA, Sept 15 -18 • Media • Collaborations § § § Meeting with representatives from South African representative, England Modeling Paris/London/Amsterdam Collaboration § § § § PBS News. Hour HIV plus Takepart Bay Area Reporter Star Observer (AU) San Francisco Chronicle KGO-TV San Francisco/abc 7 news
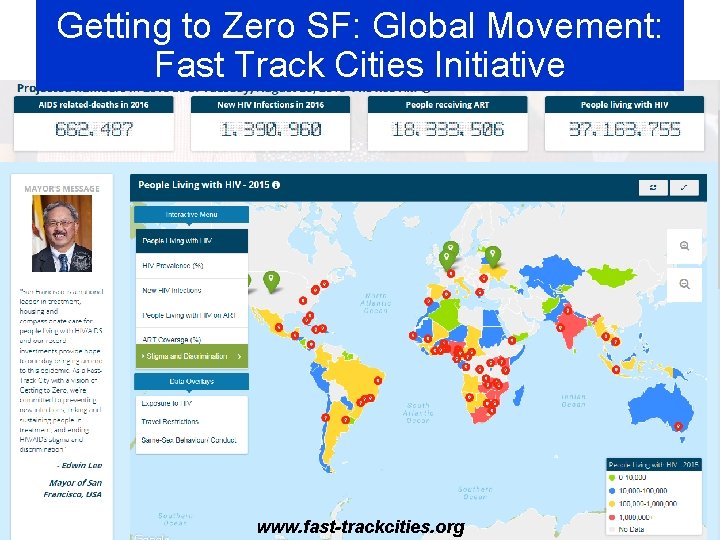
Getting to Zero SF: Global Movement: Fast Track Cities Initiative www. fast-trackcities. org

Update on Funding
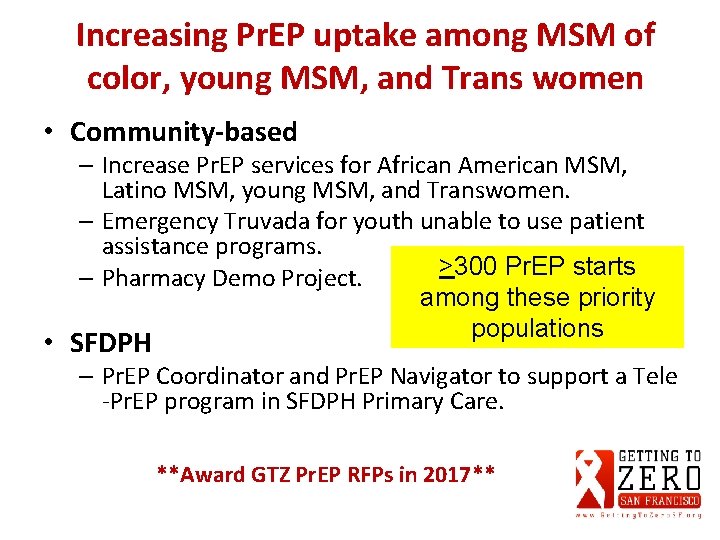
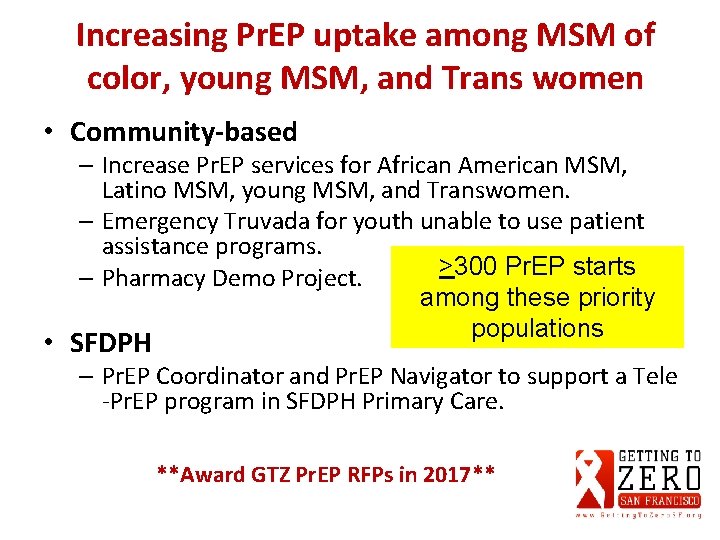
Increasing Pr. EP uptake among MSM of color, young MSM, and Trans women • Community-based – Increase Pr. EP services for African American MSM, Latino MSM, young MSM, and Transwomen. – Emergency Truvada for youth unable to use patient assistance programs. >300 Pr. EP starts – Pharmacy Demo Project. among these priority populations • SFDPH – Pr. EP Coordinator and Pr. EP Navigator to support a Tele ‐Pr. EP program in SFDPH Primary Care. **Award GTZ Pr. EP RFPs in 2017**

Project Pride (funded by CDC) • Increase user knowledge and interest in Pr. EP – Social marketing campaign, Popular Opinion Leader • Increase linkage of focus populations to Pr. EP – City‐wide Pr. EP coordinator and navigator using innovative social media strategies – “Data‐to‐Pr. EP”– use of STI surveillance to link patients diagnosed with rectal STIs and syphilis to Pr. EP – Pr. EP navigators Group: share best practices • Increase primary care provider engagement in Pr. EP – Public Health Detailing
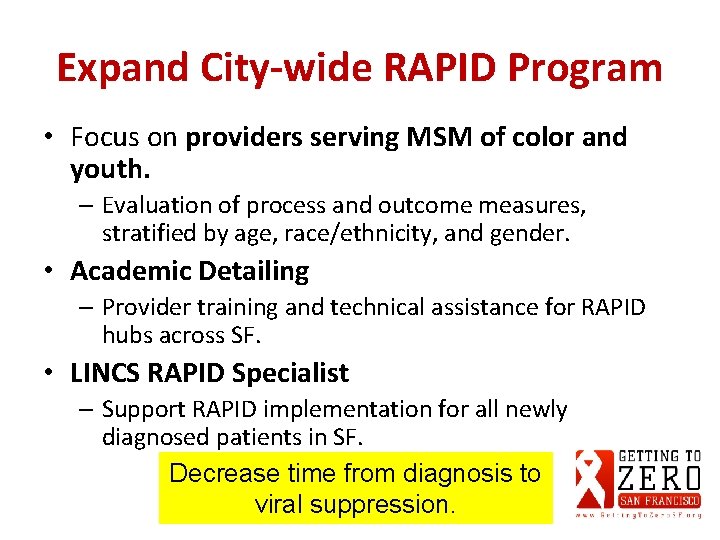
Expand City-wide RAPID Program • Focus on providers serving MSM of color and youth. – Evaluation of process and outcome measures, stratified by age, race/ethnicity, and gender. • Academic Detailing – Provider training and technical assistance for RAPID hubs across SF. • LINCS RAPID Specialist – Support RAPID implementation for all newly diagnosed patients in SF. Decrease time from diagnosis to viral suppression.
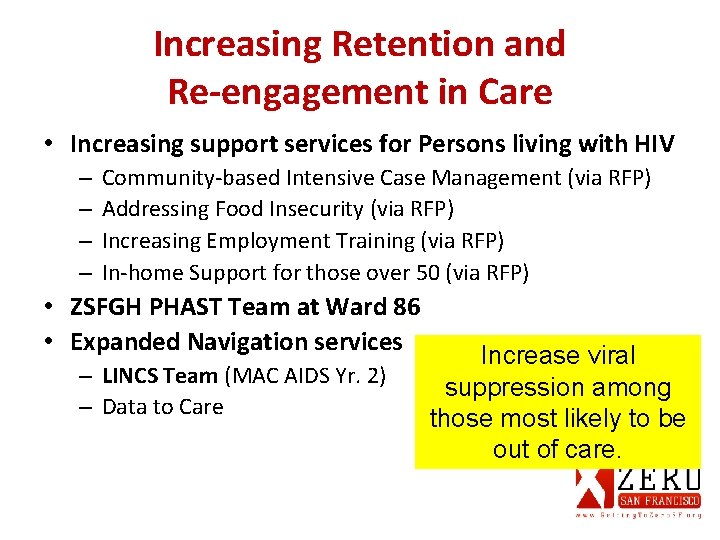
Increasing Retention and Re-engagement in Care • Increasing support services for Persons living with HIV – – Community‐based Intensive Case Management (via RFP) Addressing Food Insecurity (via RFP) Increasing Employment Training (via RFP) In‐home Support for those over 50 (via RFP) • ZSFGH PHAST Team at Ward 86 • Expanded Navigation services – LINCS Team (MAC AIDS Yr. 2) – Data to Care Increase viral suppression among those most likely to be out of care.
Addressing Stigma • Develop an anti-stigma initiative (via RFP) – Stigma is an important barrier for HIV prevention, care, and treatment. – Create an initiative with sustainable impact on the community and providers. – Representation from disproportionally impacted communities: young MSM and MSM >50; MSM of color; and women at risk. Increase capacity to address HIVrelated stigma in SF.

Requests for Proposals (RFPs) • 22‐ 2016: Support Services and Program Coordination for HIV‐positive Adults Age 50 and Older (here) • 23‐ 2016: Communications Support and Capacity‐Building for HIV Frontline Workers Group (here)
Requests for Proposals (RFPs) • 24‐ 2016: Getting to Zero: Community‐Based Intensive Case Management Services for HIV‐positive Clients with Complex Needs (here) • 25‐ 2016: G 2 Z: Community‐Based Intensive Pre‐Exposure Prophylaxis (Pr. EP) Services (here)
HIV Epidemiology Annual Report 2015

HIV Epidemiology Annual Report 2015 Susan Scheer, Ph. D, MPH Director HIV Epidemiology Section susan. scheer@sfdph. org
Outline v Key highlights from the recently released HIV Epidemiology Section 2015 Annual Report including trends in key indicators § Encouraging trends on the population level § Overall declines in new HIV diagnoses § Declines in deaths and late diagnoses § Care and treatment items along the HIV care continuum § Not all San Franciscans have experienced the same improvements; significant health disparities identified § By race/ethnicity, particularly African‐Americans, in treatment and care outcomes, survival and new diagnoses § Gender disparities in survival and viral suppression § People experiencing homelessness have very low engagement care and viral suppression
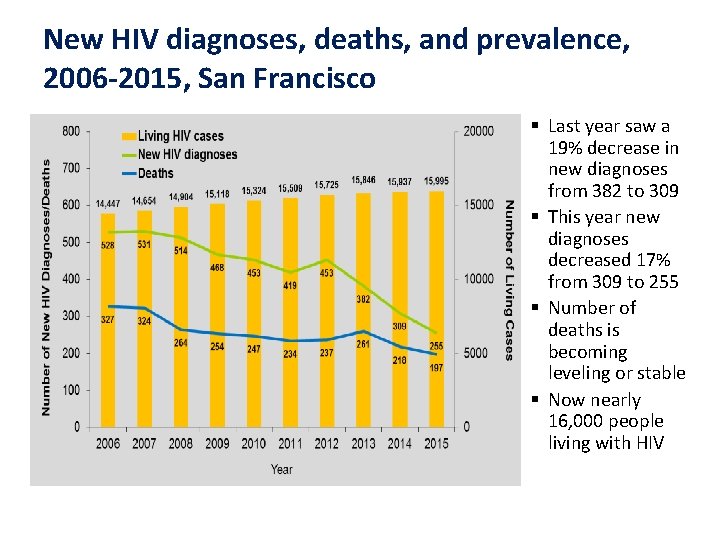
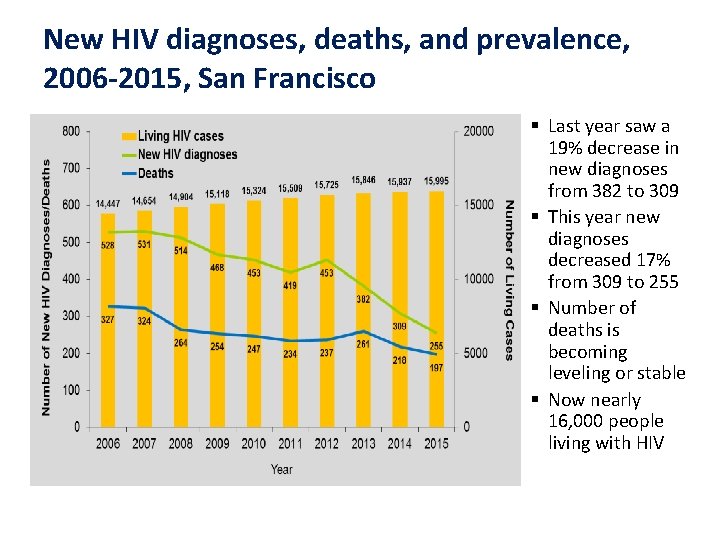
New HIV diagnoses, deaths, and prevalence, 2006 -2015, San Francisco § Last year saw a 19% decrease in new diagnoses from 382 to 309 § This year new diagnoses decreased 17% from 309 to 255 § Number of deaths is becoming leveling or stable § Now nearly 16, 000 people living with HIV

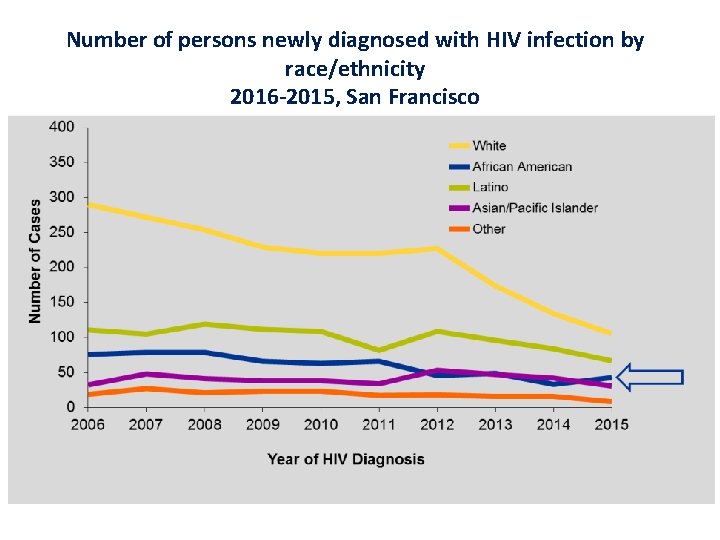
Among women, # stable, %↑ In all races, # ↓ except AA, # stable, %↑ Most new dx in ages 30 -39 60% PLWH >50; ⅟₄ >60 years MSM dis- proportionately affected
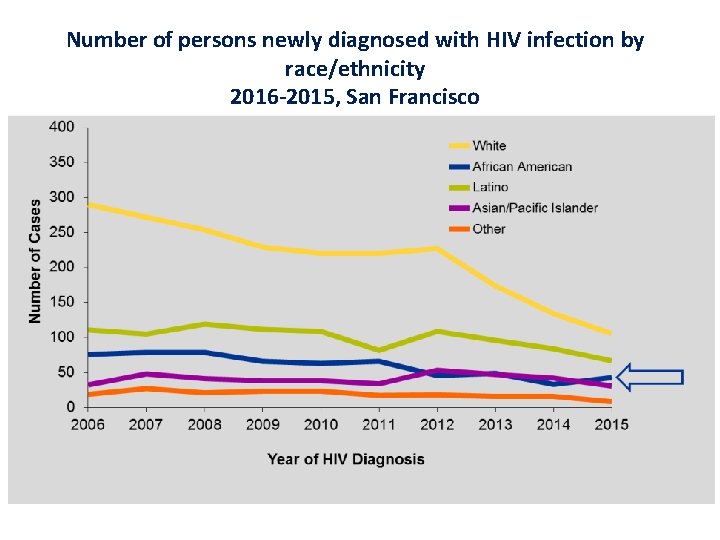
Number of persons newly diagnosed with HIV infection by race/ethnicity 2016 -2015, San Francisco

Annual Rates of men newly diagnosed with HIV Infection per 100, 000 population by Race/ethnicity, 2006 -2015, SF Rates 2015 140 AA 83 Latino 52 White 24 Other

Annual Rates of women newly diagnosed with HIV Infection per 100, 000 population by Race/ethnicity, 2006 -2015, SF Rates 2015 31 AA 8 Latina 5 White 2 Other
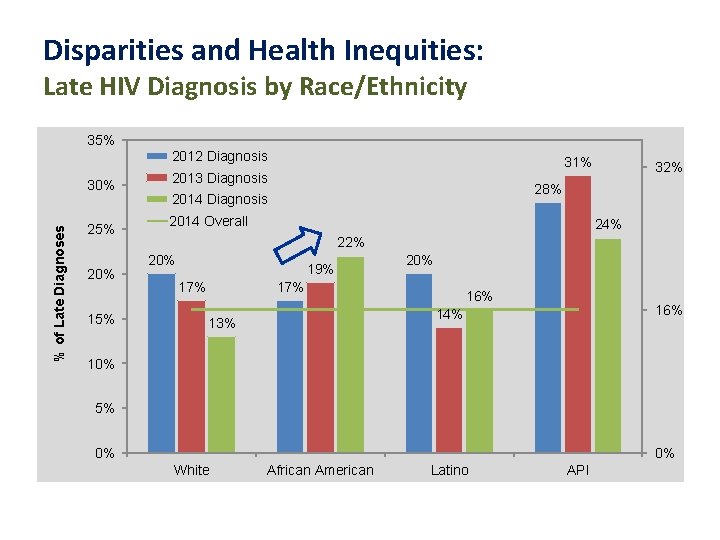
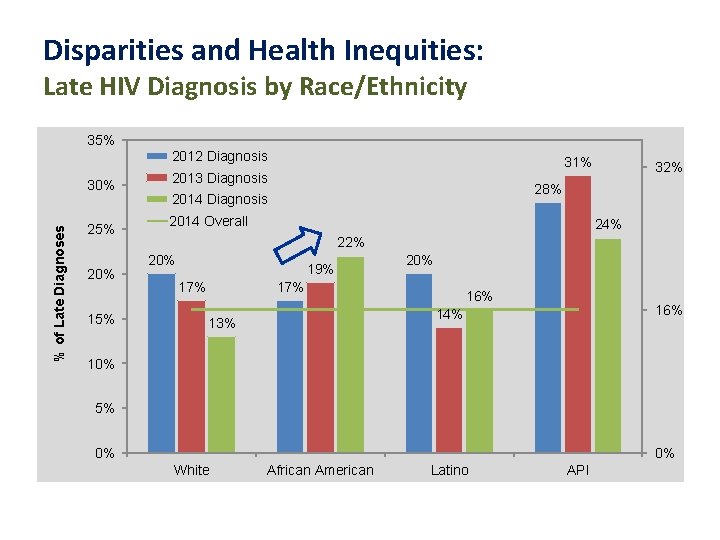
Disparities and Health Inequities: Late HIV Diagnosis by Race/Ethnicity 35% 2012 Diagnosis % of Late Diagnoses 30% 25% 20% 15% 31% 2013 Diagnosis 32% 28% 2014 Diagnosis 2014 Overall 24% 22% 20% 19% 17% 20% 17% 16% 14% 13% 10% 5% 0% 0% White African American Latino API
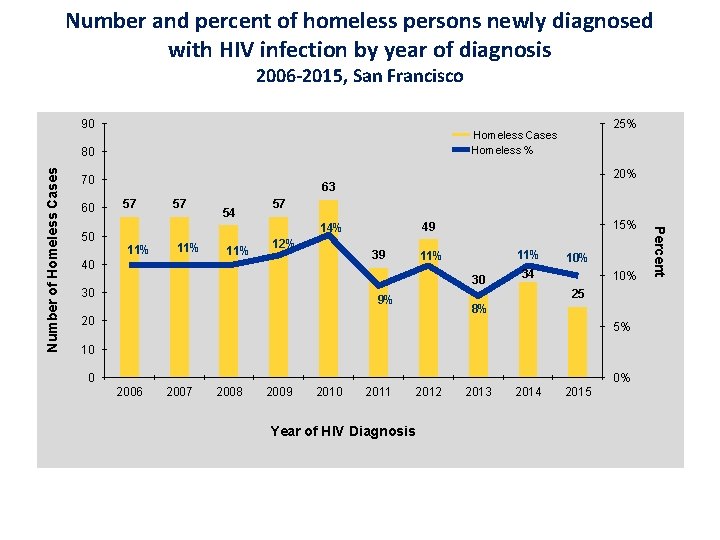
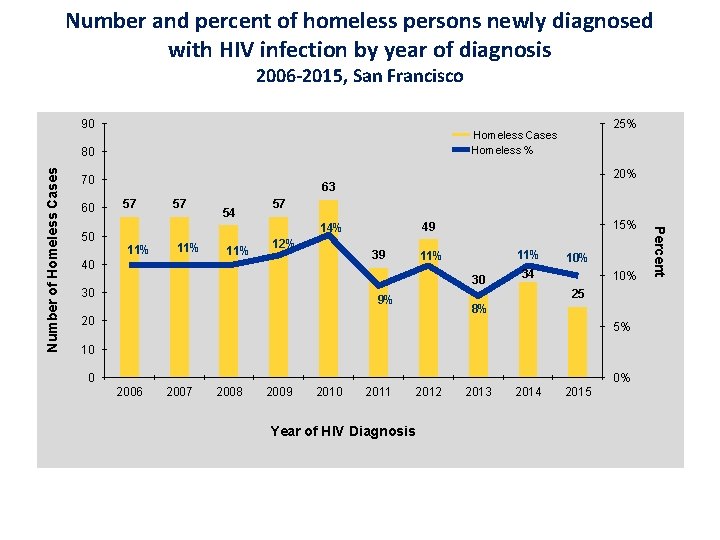
Number and percent of homeless persons newly diagnosed with HIV infection by year of diagnosis 2006 -2015, San Francisco 90 70 50 20% 63 57 57 54 57 11% 11% 12% 39 40 15% 49 14% 11% 30 30 10% 34 10% 25 9% 8% 20 5% 10 0 0% 2006 2007 2008 2009 2010 2011 2012 Year of HIV Diagnosis 2013 2014 2015 Percent Number of Homeless Cases 80 60 25% Homeless Cases Homeless %

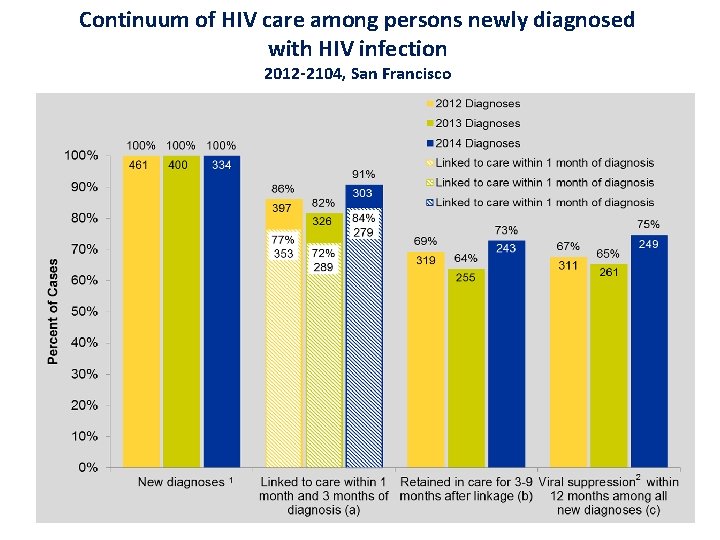
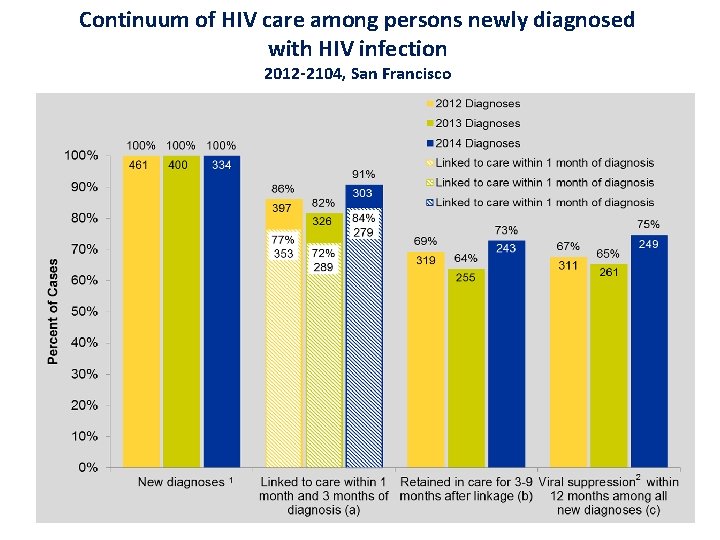
Continuum of HIV care among persons newly diagnosed with HIV infection 2012 -2104, San Francisco
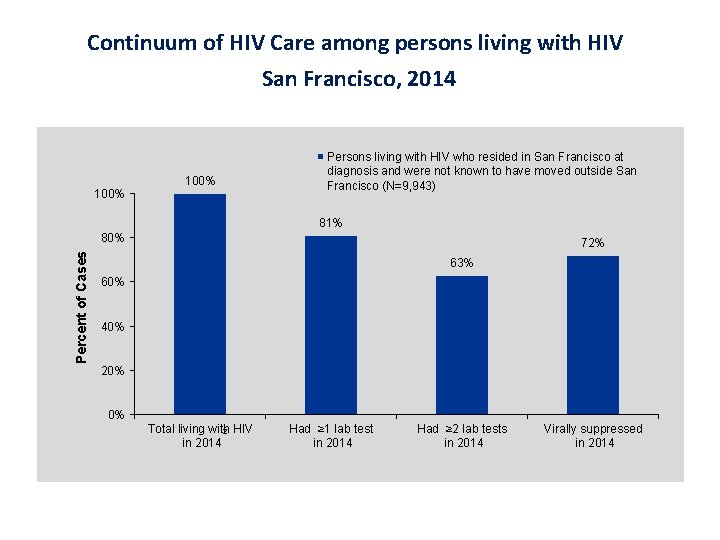
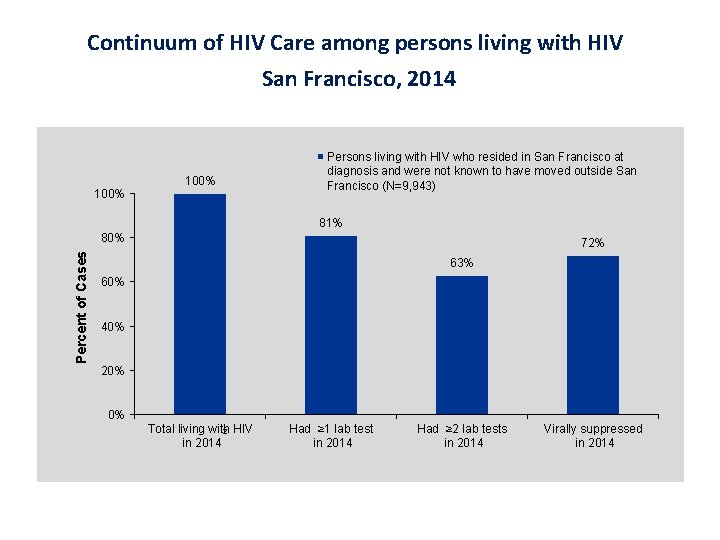
Continuum of HIV Care among persons living with HIV San Francisco, 2014 100% Persons living with HIV who resided in San Francisco at diagnosis and were not known to have moved outside San Francisco (N=9, 943) 81% Percent of Cases 80% 72% 63% 60% 40% 20% 0% Total living with 2 HIV in 2014 Had ≥ 1 lab test in 2014 Had ≥ 2 lab tests in 2014 Virally suppressed in 2014
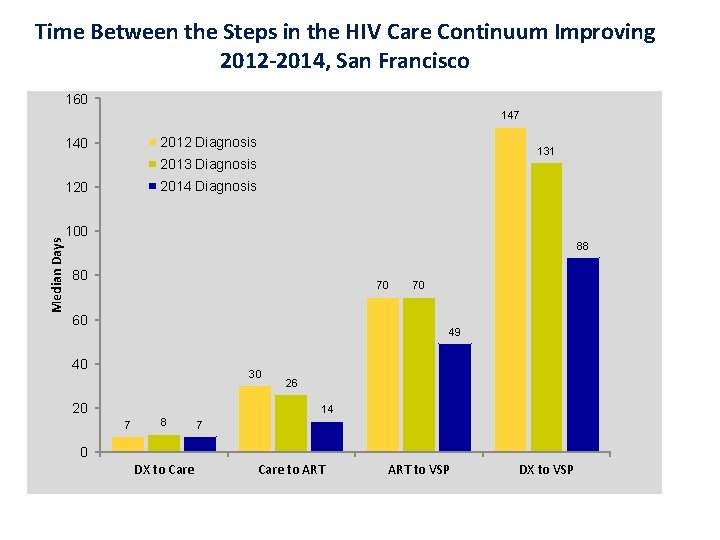
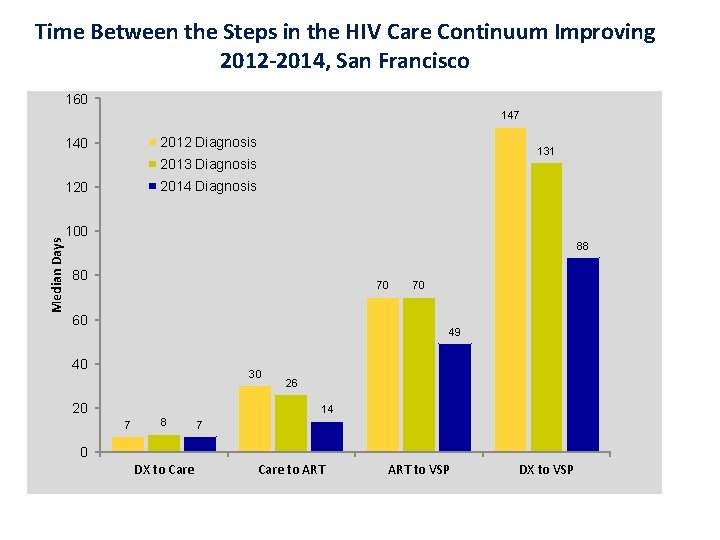
Time Between the Steps in the HIV Care Continuum Improving 2012 -2014, San Francisco 160 147 2012 Diagnosis 140 131 2013 Diagnosis 2014 Diagnosis Median Days 120 100 88 80 70 60 70 49 40 30 20 26 14 7 8 7 0 DX to Care to ART to VSP DX to VSP
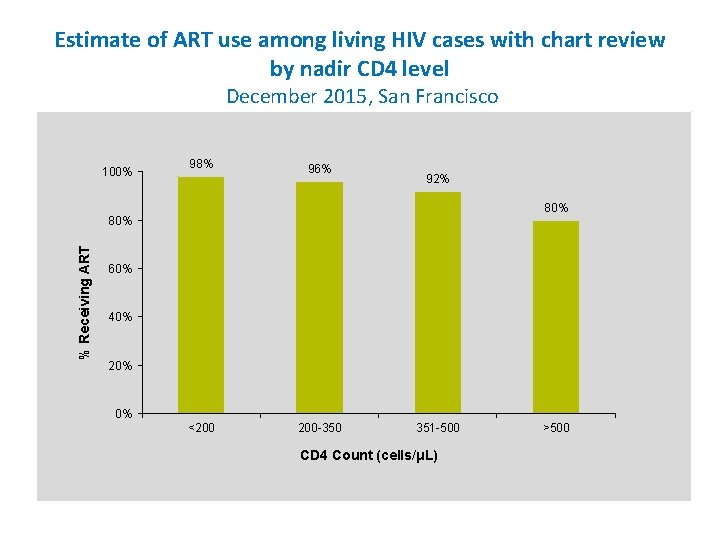
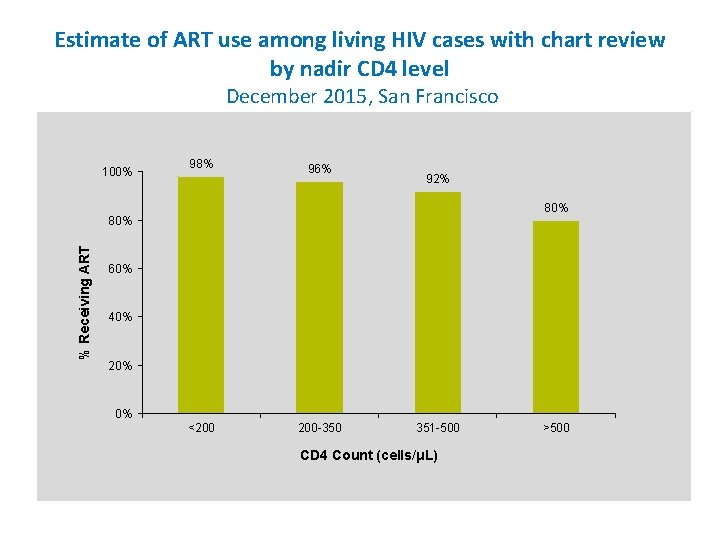
Estimate of ART use among living HIV cases with chart review by nadir CD 4 level December 2015, San Francisco 100% 98% 96% 92% 80% % Receiving ART 80% 60% 40% 20% 0% <200 200 -350 351 -500 CD 4 Count (cells/μL) >500
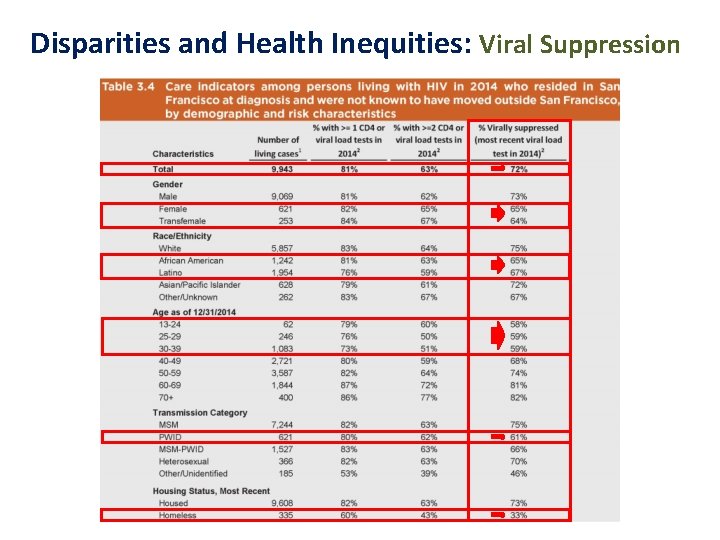
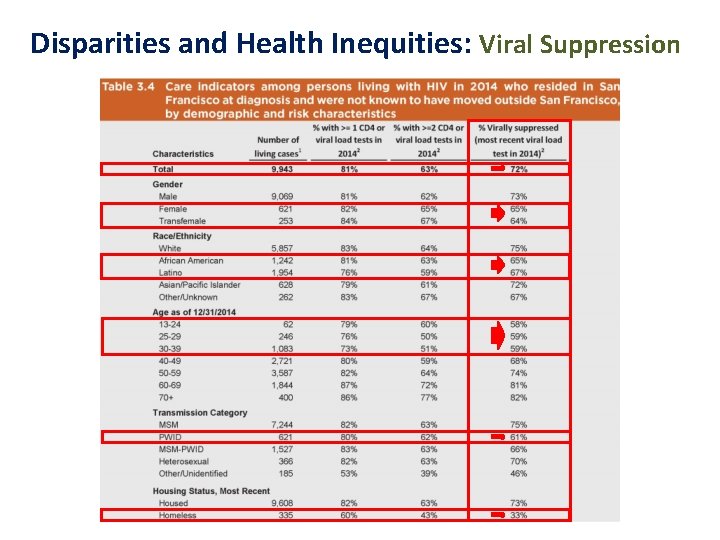
Disparities and Health Inequities: Viral Suppression
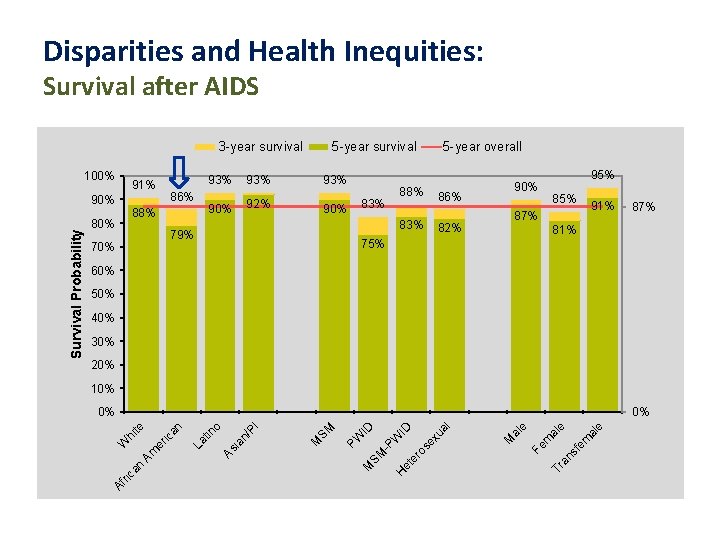
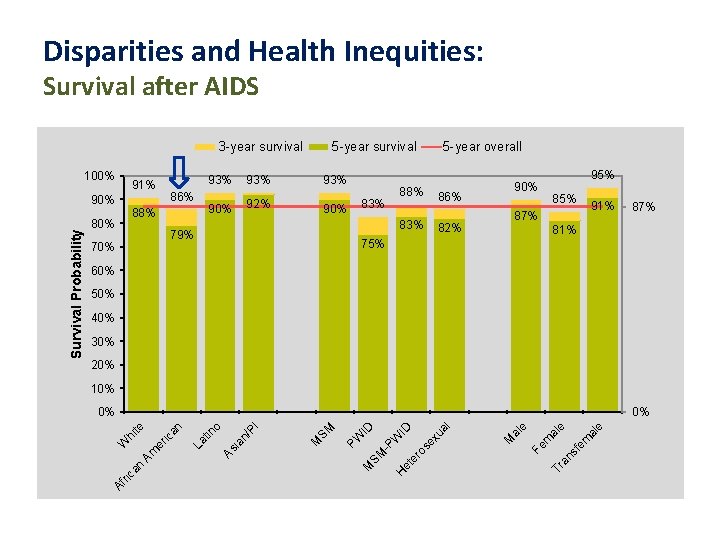
Disparities and Health Inequities: Survival after AIDS 3 -year survival 100% 91% 86% 88% 80% 93% 90% 92% 93% 90% 70% 5 -year overall 88% 83% 79% 95% 90% 86% 85% 91% 87% 82% 87% 81% 75% 60% 50% 40% 30% 20% 10% al e fe m an s Tr Fe m al e e al M ex ua l er os et H SM -P W ID ID PW M I SM M tin n/ P ia As er Am n La hi te W ca o 0% ic an 0% Af ri Survival Probability 90% 93% 5 -year survival

Number of STD diagnoses among persons living with HIV by year of STD diagnosis 2010‐ 2014, San Francisco 1400 No. of Cases w/ STD 1200 Non-MSM 17 1000 24 26 30 32 800 600 400 907 960 2011 1, 086 1, 149 1, 188 2013 2014 200 0 2012 Year of STD Diagnosis
Summary v Positive trends: new diagnoses, late diagnoses and care & treatment outcomes v Significant health disparities. Not all San Franciscans experiencing the same improvements v African‐Americans, in particular, experiencing health inequities: § disproportionately diagnosed; poorer treatment and care outcomes, poorer survival v Other population groups also experiencing disparities: § Latinos most likely to uninsured at diagnosis and less likely to be engaged in care and virally suppressed § Women and transwomen are less likely to achieve viral suppression § Persons experiencing homelessness are less engaged in care and virally suppressed § Asians are most likely to be diagnosed late § Women and PWID have poorer survival § Younger people less engaged in care and virally suppressed v Disparities in our most vulnerable populations will need to be addressed to achieve the goal of Zero New Infections for all San Franciscans

Questions

GTZ Committee Updates
GTZ Pr. EP Committee Co-Chairs: Al Liu & Robert Grant Pr. EP User Subcommittee Co-chairs: Pierre Crouch & Stephanie Goss Pr. EP Provider Subcommittee Co-chairs: Tracey Packer & Stephanie Cohen Pr. EP Metrics Subcommittee Chair: Susan Scheer Members: Oliver Bacon, Halvard Bagoien, Jackson Bowman, Susan Buchbinder, Jim Dilley, Edvard Engesaeth, Jonathan Fuchs, Jesus Gaeta, Jayne Gagliano, Ruben Gamundi, Hans Gangeskar, Ron Goldschmidt, Robert Grant, Brad Hare, Geoff Hart‐Cooper, Jen Hecht, Mike Hickey, Anne Hirozawa, Alison Hughes, Cait Koss, Skot Land, Montica Levy, Paul Marcelin, Julia Marcus, Erick Martinez, John Melichar, Gavin Morrow‐Hall, Austin Nation, Trang Nguyen, Miranda Nordell, Sergio Paz, Susan Philip, Greg Rebchook, Michael Reyes, Hyman Scott, Matt Sharp, Miriam Sheinbein, Lisa Stern, Eric Tang, Adam Taylor, EB Troast, Paul Urban, Dana van Gorder, Jonathan Volk, Shannon Weber, Sophy Wong
Updates & Recent Activities (since March 2016) • 2 transgender Pr. EP demonstration projects funded by CHRP [UCSF, SFDPH] (April) • Presented on GTZ Pr. EP activities at Adherence 2016 meeting (May) • Updated SFHN Pr. EP guidelines published (May) • Hired Pr. EP navigators through Campos RFP • Scale up of Pr. EP services at Mission Neighborhood Health Center and CHPY (Cole/Larkin) • Coordinated monthly city‐wide Pr. EP navigator meetings (ongoing) • Provided Pr. EP trainings to >50 clinical providers and >150 front‐line staff since March 2016 • Launch of E‐referral system for Pr. EP consultation (Sept) • Awarded 2 NIH supplements to evaluate Pr. EP cascade and Pr. EP retention in SF (Sept)

Our new citywide Pr. EP team Montica Levy Citywide Pr. EP Coordinator Miranda Nordell SFHN Lead Pr. EP Navigator Michael Barajas Citywide Pr. EP Navigator Alyson Decker, NP Pr. EP Academic Detailing
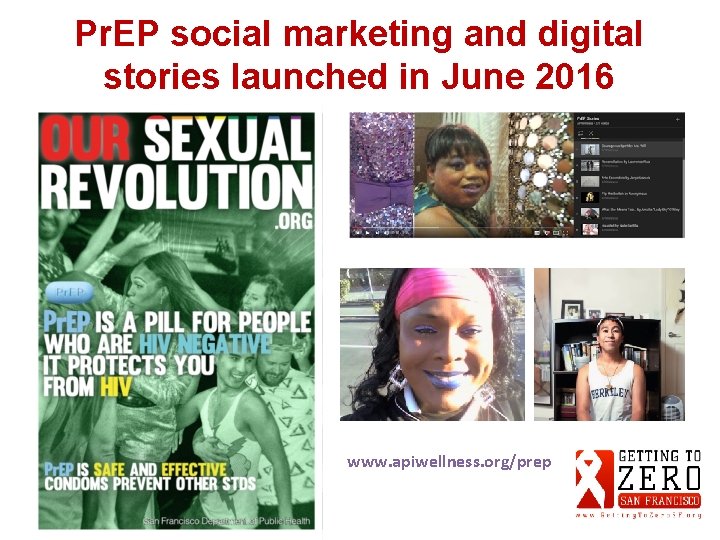
Pr. EP social marketing and digital stories launched in June 2016 www. apiwellness. org/prep

Pr. EP Committee Plans – next 6 months User Provider • Expand Pr. EP ambassador program, specific outreach to African‐ American MSM, youth • Looking for volunteers for Folsom/Castro Fairs • Investigate strategies to increase Pr. EP access for homeless • Launch Pr. EP Demo project in transgender women and men • Launch academic detailing program, with focus on clinics serving prioritized populations • Work to establish Truvada medication access program for youth and pharmacy delivered Pr. EP program in Mission • Establish quarterly mtgs of community of practice of Pr. EP providers: Next mtg November 9 Measurement • Update metrics, from community‐based surveys and medical providers, every 3 months (posted to GTZ website) • Establish Pr. EP cascade measures and begin measurement in transgender cohort in SF • Launch study to evaluate reasons for poor retention in Pr. EP programs GTZ Pr. EP RFP for 2016 -2017
G 2 Z RAPID Committee

Progress since Last Meeting • New RAPID protocol with updated linkage algorithm • Additional RAPID clinics enrolled – Larkin – Private Offices – FHC • 2 Detailing/outreach specialists hired • $$ for RAPID navigation specialist • Inclusion of RAPID indicators in Surveillance Data

Lesson Learned: 2016 1. Provider acceptance high 2. Greatest challenge: linkage/insurance navigation – Uninsured but non‐Medi. Cal/HSF eligible are most challenging 3. Disparities a challenge – Race/ethnicity – Homelessness
RAPID Goals for 2016 -17 1. Systematic RAPID detailing of all HIV providers § G 2 Z funding for 1 year of detailing assistance 2. RAPID linkage § Navigation “bootcamp” for navigators/test sites § Bridging RAPID ART site to care for difficult‐to‐link patients ? ? using Ryan White (A) funds while they are being navigated? ? § G 2 Z funding a RAPID navigator to work with LINCS 3. Shorten time from diagnosis to care, care to ART, diagnosis to viral suppression: goal is 56 days +5 from diagnosis to suppression 4. A plan to address disparities in ART
Co‐Chairs Austin Padilla, Wayne Steward Members Tez Anderson, Samuel Berston, Jonathan Gomez, Stephanie Goss, Robert Grant, Alison Hughes, Brandon Ivory, Shaddai Martinez‐Cuestas, Mark Molnar, Thomas Muyunga, Jenna Rapues, Armando Rodriguez, Ashley Rojas, Will Vincent, Lance Toma
Upcoming Committee Meeting Tuesday, October 4, 6 p San Francisco City Hall, Room 270 *Security requires people with backpacks to enter through the loading dock entrance on Grove Street
Retention & Re‐engagement • • • • Amanda Newstetter/bay area aetc Andy Scheer/sfdph sf city clinic (co‐chair) Austin Padilla (Stigma Committee rep. ) Beth Mazie/prc Bill Hirsh/alrp + hapn Chip Supanich/hiv planning council Chuan Teng/prc Dana Van Gorder/project inform Darpun Sachdev/sfdph lincs navigation Dave Jordan/shanti + hhspn Dean Goodwin/sfdph hhs Edwin Charlebois/ucsf caps (co‐chair) Erin Antunez/sfdph lincs navigation Eva Mureithi/ucsf w 86 • • • • Gale Sandoval/ifr Hyman Scott/dph Joanna Eveland/tom waddell Joe Ramirez‐Forcier/prc Julie Lifshay/sfaf Kat Christopoulos/ucsf w 86 Kate Darling/ucsf Kate Franza/api wellness Kristi Dizon/ahf Linda Walubengo/catholic charities Lori Thoemmes/ucsf ahp Marc Vincent/ucsf Monica Gandhi/ucsf w 86 Susan Scheer/sfdph Tracey Packer/sdfph

Updates & Recent Activities • MAC AIDS Fund, LINCS Lessons Learned – Clinic‐based and Surveillance‐derived data effective in locating and re‐engaging Pts in care; in 9‐month period, 120 clinic‐based referrals enrolled in LINCS – Navigation increases viral suppression, supporting Tas. P biomedical intervention – Approx 1/3 of Pts are homeless and 1/2 substance‐using; more support needed to address these issues • MAC AIDS Fund, Current Practices Survey – DPH/Public/Private providers surveyed: majority use pre‐appointment reminders (phone/voicemail/SMS) & do missed visit follow‐up – Few clinics pass on out‐of‐care patient info to the DPH for re‐engagement in care – Clinics willing to develop links to programs for Pr. EP and RAPID ART start – Clinics interested in support with linkage to MH & SU tx resources Metrics Development: Work group formed, met, goal‐setting commenced • • Retention & Re‐Engagement Toolkit: Content developed; funding secured; moving on to design & distribution phase • RFP Development: Intensive Case Mgmt, Communications, Frontline Workers, Aging Services RFP’s released

Committee Plans – next 6 months • MAC AIDS Fund Renewal, LINCS Y 2: – Develop novel approaches for clients who use substances – Continue data‐to‐care efforts in collaboration w/ DPH Surveillance & clinics • MAC AIDS Fund Renewal, Best Practices Y 2: – Optimize and evaluate R&R package – Finalize & disseminate findings • Metrics: – Establish and obtain preliminary measures, review – ID measures currently not being evaluated R&R Toolkit: Finalize design; academic detailing to practices; group trainings • • RFP Initiatives: Support implementation • Pharmacy Workgroup: Convene workgroup for leveraging pharmacies for retention & re‐engagement collaboration • GTZ Cross‐Committee Collaboration: on MH, SU, housing, benefits navigation, and other issues that impact retention in treatment and prevention interventions

HIV Navigation Panel
GTZ Navigation Panel • LINCS Navigator, Nora Anderson • LINCS Navigation patient, Robert • SF AIDS Foundation Navigator, Naomi Prochovnick • LINCS Program Coordinator, Erin Antunez

HIV Navigation Community Discussion