GETTING TO KNOW SIRS DR AKINWUNMI AKINWUNTAN M



- Slides: 15
GETTING TO KNOW SIRS DR. AKINWUNMI AKINWUNTAN M. B; BS(Ib), MHSc (Ib), FMCOG, FWACS
BACKGROUND • Localized inflammation is a physiological protective response which is generally tightly controlled by the body at the site of injury • Loss of this local control or an overly activated response results in an exaggerated systemic response which is clinically identified as Systemic Inflammatory Response Syndrome (SIRS) 9/16/2020 2
DEFINITION • Is an inflammatory state affecting the whole body, frequently a response of the immune system to infection, but not necessarily so ICD-10 • The active pathways leading to such pathophysiology may include fibrin deposition, platelet aggregation, coagulopathies and leukocyte liposomal release • First described in 1983 – Dr. William Nelson 9/16/2020 3
CAUSES OF SIRS • INFECTIONS • NON – INFECTIONS Trauma, Burns, Pancreatitis, Ischemia, and Hemorrhage – Other causes include: – Complications of surgery – Adrenal insufficiency – Pulmonary embolism – Complicated aortic aneurysm – Cardiac tamponade – Anaphylaxis – Drug overdose – Polypropylene Mesh Surgical Implant 9/16/2020 4
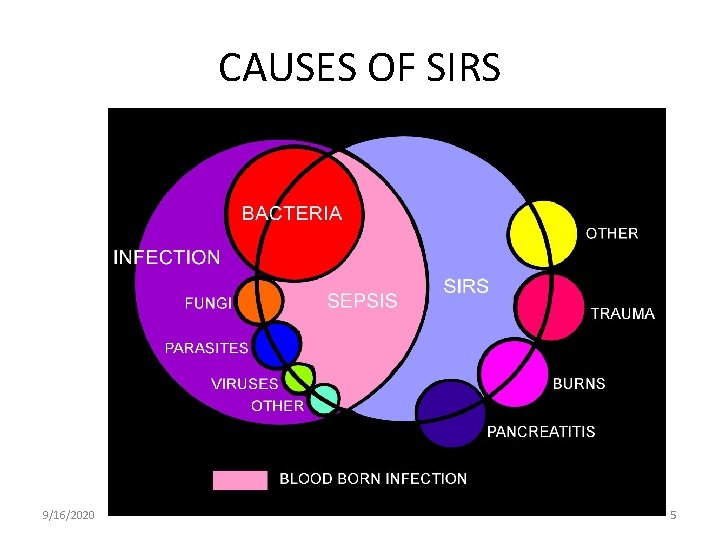
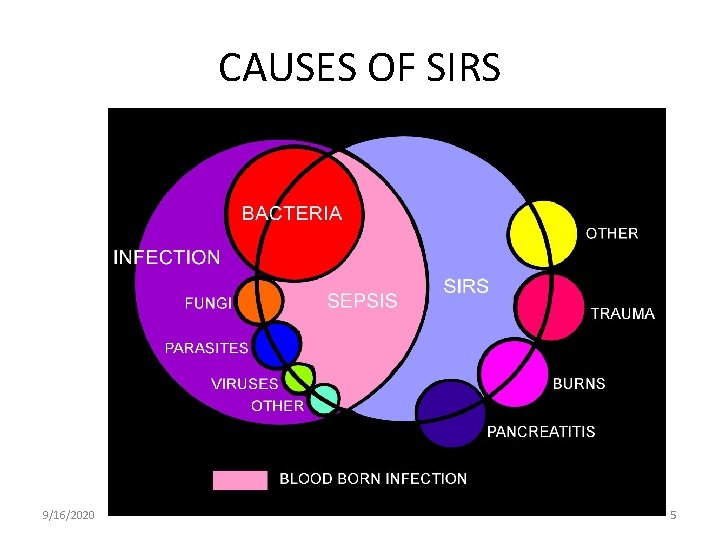
CAUSES OF SIRS 9/16/2020 5
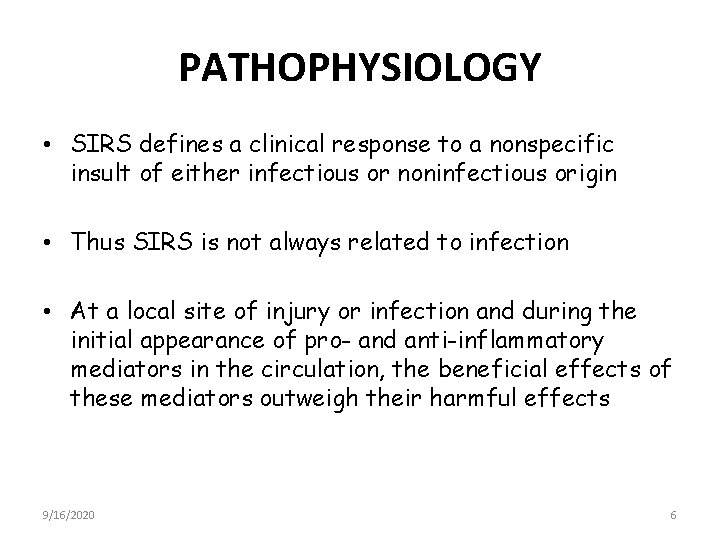
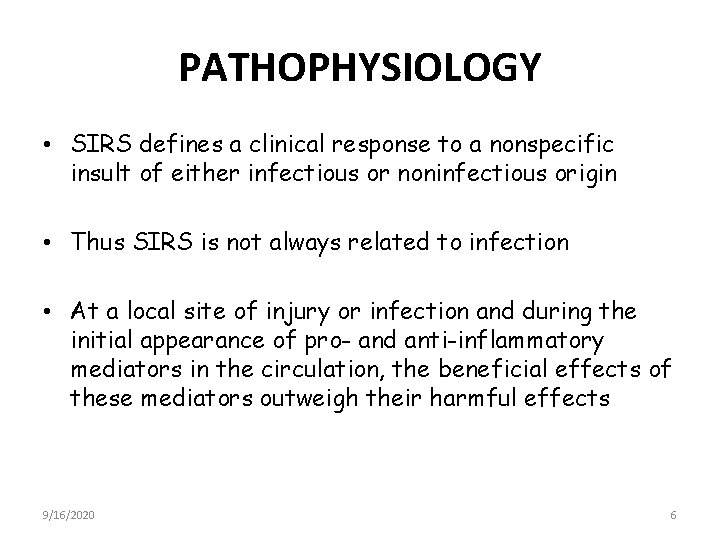
PATHOPHYSIOLOGY • SIRS defines a clinical response to a nonspecific insult of either infectious or noninfectious origin • Thus SIRS is not always related to infection • At a local site of injury or infection and during the initial appearance of pro- and anti-inflammatory mediators in the circulation, the beneficial effects of these mediators outweigh their harmful effects 9/16/2020 6
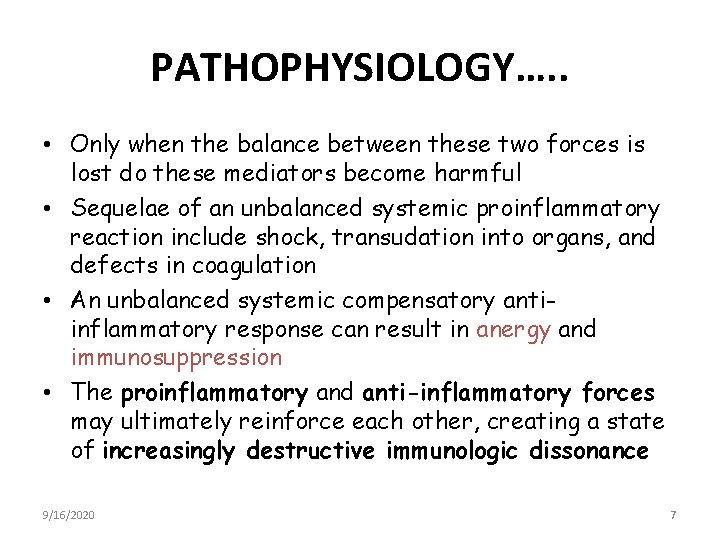
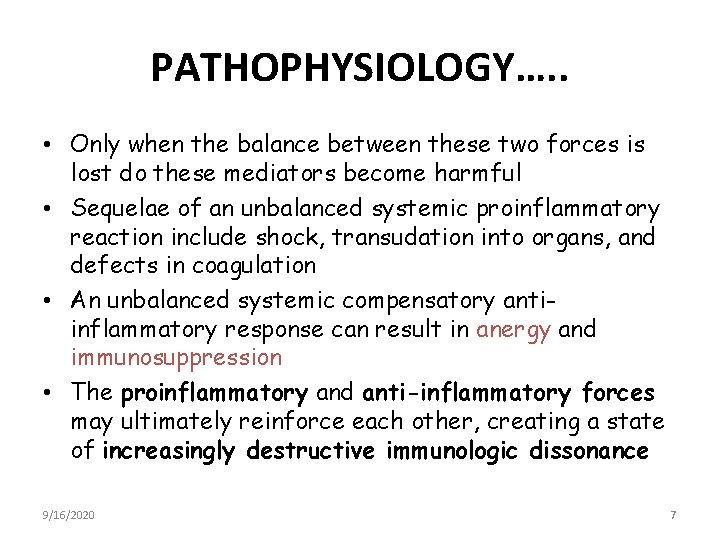
PATHOPHYSIOLOGY…. . • Only when the balance between these two forces is lost do these mediators become harmful • Sequelae of an unbalanced systemic proinflammatory reaction include shock, transudation into organs, and defects in coagulation • An unbalanced systemic compensatory antiinflammatory response can result in anergy and immunosuppression • The proinflammatory and anti-inflammatory forces may ultimately reinforce each other, creating a state of increasingly destructive immunologic dissonance 9/16/2020 7
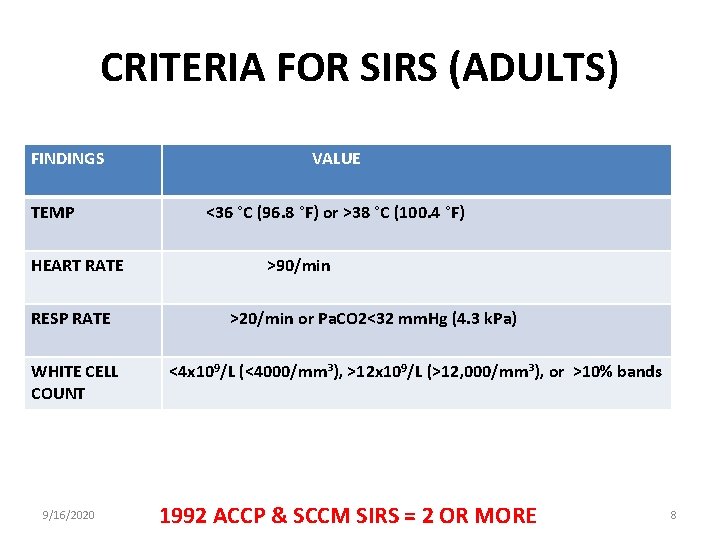
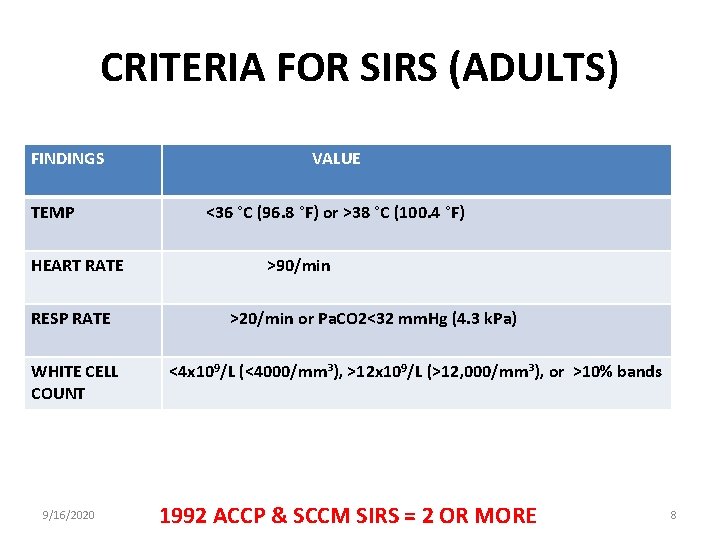
CRITERIA FOR SIRS (ADULTS) FINDINGS VALUE TEMP <36 °C (96. 8 °F) or >38 °C (100. 4 °F) HEART RATE >90/min RESP RATE >20/min or Pa. CO 2<32 mm. Hg (4. 3 k. Pa) WHITE CELL COUNT <4 x 109/L (<4000/mm³), >12 x 109/L (>12, 000/mm³), or >10% bands 9/16/2020 1992 ACCP & SCCM SIRS = 2 OR MORE 8
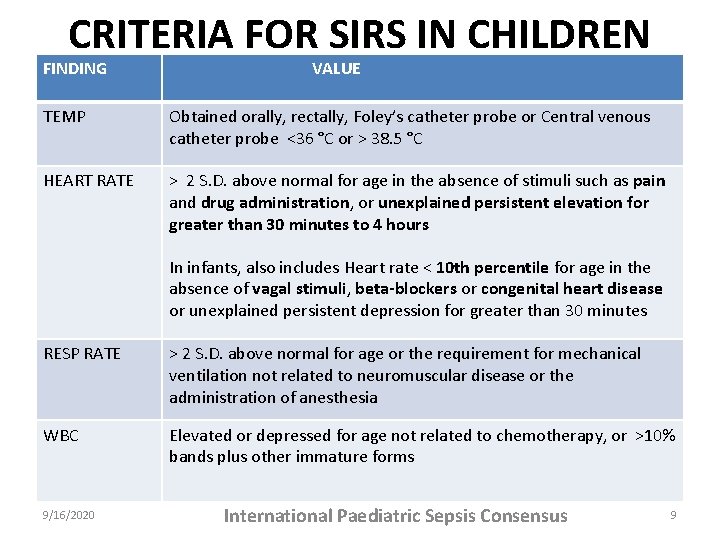
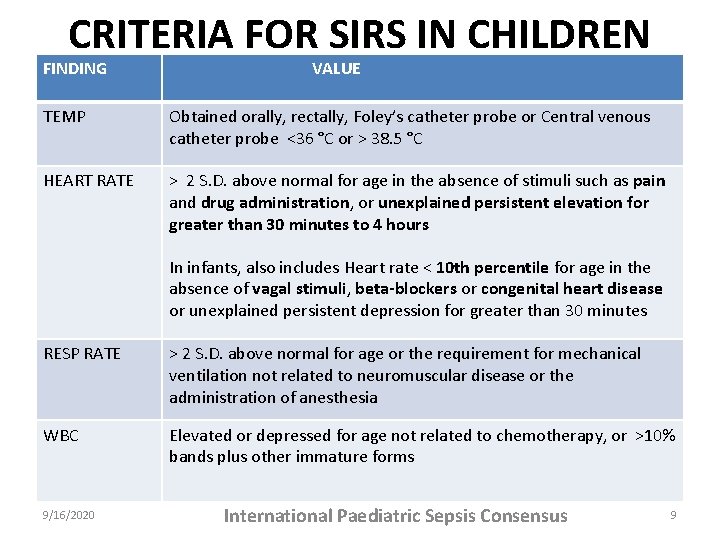
CRITERIA FOR SIRS IN CHILDREN FINDING VALUE TEMP Obtained orally, rectally, Foley’s catheter probe or Central venous catheter probe <36 °C or > 38. 5 °C HEART RATE > 2 S. D. above normal for age in the absence of stimuli such as pain and drug administration, or unexplained persistent elevation for greater than 30 minutes to 4 hours In infants, also includes Heart rate < 10 th percentile for age in the absence of vagal stimuli, beta-blockers or congenital heart disease or unexplained persistent depression for greater than 30 minutes RESP RATE > 2 S. D. above normal for age or the requirement for mechanical ventilation not related to neuromuscular disease or the administration of anesthesia WBC Elevated or depressed for age not related to chemotherapy, or >10% bands plus other immature forms 9/16/2020 International Paediatric Sepsis Consensus 9
• Note that SIRS criteria are non-specific and must be interpreted carefully within the clinical context • These criteria exist primarily for the purpose of more objectively classifying critically ill patients so that future clinical studies may be more rigorous and more easily reproducible • As an alternative, when two or more of the systemic inflammatory response syndrome criteria are met without evidence of infection, patients may be diagnosed simply with "SIRS. “ • Patients with SIRS and acute organ dysfunction may be termed "severe SIRS" 9/16/2020 10
COMPLICATION • SIRS SEPSIS SEVERE SEPSIS SEPTIC SHOCK MULTIPLE ORGAN DYSFUNCTION SYNDROME (MODS) • • Acute lung injury Acute kidney injury Shock Anaemia GI Bleeding DIC Multiple Organ Dysfunction Syndrome 9/16/2020 11
TREATMENT TREAT UNDERLYING PROBLEM OR INCITING CAUSE – Adequate Fluid Replacement for Hypovolemia – Epinephrine/Steroids/Diphenhydramine for anaphylaxis – Selenium, Glutamine, Eicosapentaenoic acid have worked in clinical trials – Vitamin E (Antioxidant)– May be helpful – Removal of implanted mesh(Explantation) 9/16/2020 12

TREATMENT…. . • Long-term antibiotics, when clinically indicated, should be as narrow spectrum as possible to limit the potential for superinfection – This is suggested by a new fever, a change in the white blood cell [WBC] count, or clinical deterioration • Unnecessary vascular catheters and Foley catheters should be removed as soon as possible 9/16/2020 13

CONCLUSION “It is not uncommon in the NICU to be presented with the scenarios of two infants of same gestational age, with similar prenatal and delivery histories, who both have blood cultures positive for group B streptococcus. One infant is active, alert and tolerating feedings. The other is on the ventilator, hypotensive and receiving volume and vasopressor support – and is the sickest child in the nursery. Why, if both infants have the same infection, does the clinical presentation differ? It is believed that, in infants who develop sepsis, the host develops a systemic reaction to the bacteria. This reaction induces the release of substances known as inflammatory mediators, which contribute to the signs and symptoms and to the pathophysiologic sequelae of sepsis” (Carol Botwinski, Neonatal Network vol. 20. No. 5, Aug 2001) 9/16/2020 14

THANK YOU 9/16/2020 15