GETTING THE FLUIDS RIGHT IN SEPSIS ITS TIME


- Slides: 58
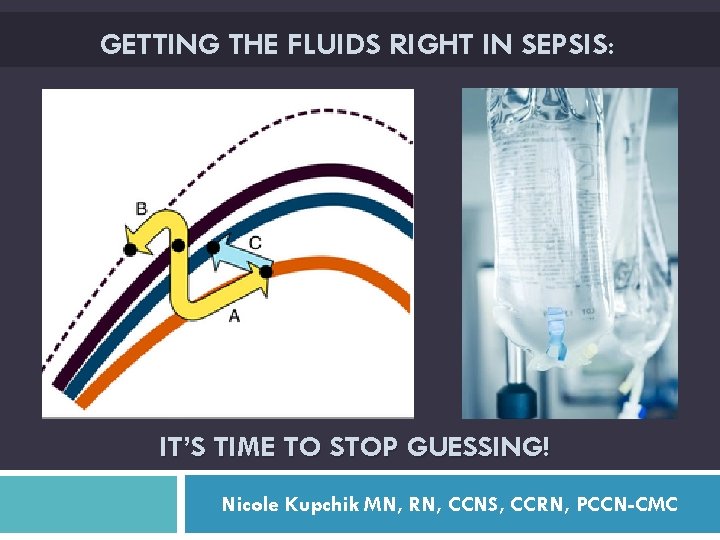
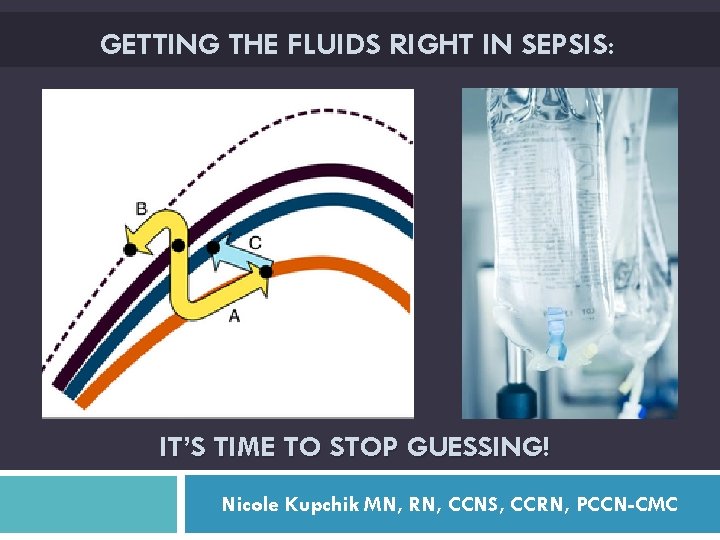
GETTING THE FLUIDS RIGHT IN SEPSIS: IT’S TIME TO STOP GUESSING! Nicole Kupchik MN, RN, CCNS, CCRN, PCCN-CMC
Objectives: Discuss the latest Sepsis Guidelines & CMS Core Measure recommendations regarding fluid resuscitation Discuss the timing, type & amount of fluid to use in resuscitation Describe the concept of fluid responsiveness & stroke volume optimization
Disclosures Speaker’s Bureau: Physio-Control (Stryker) Saxe Communications (webinars) La Jolla Pharmaceuticals Consultant: Physio-Control (Stryker) Baxter Healthcare Medivance/Bard (past)
58 year old with productive cough, fever & chills Vitals: HR 115 BP 94/46 (62) RR 16 O 2 sat 91%; placed on 4 L NC Temp 38. 6˚C Patient is really drowsy, difficult to keep attention What would you like to do?
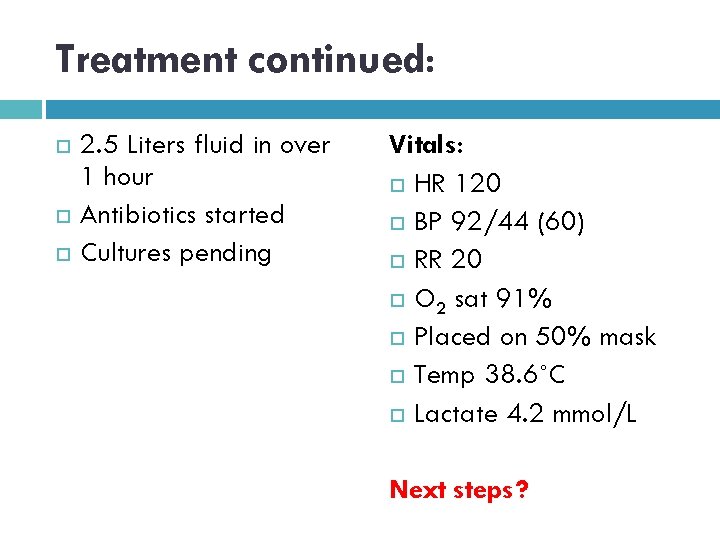
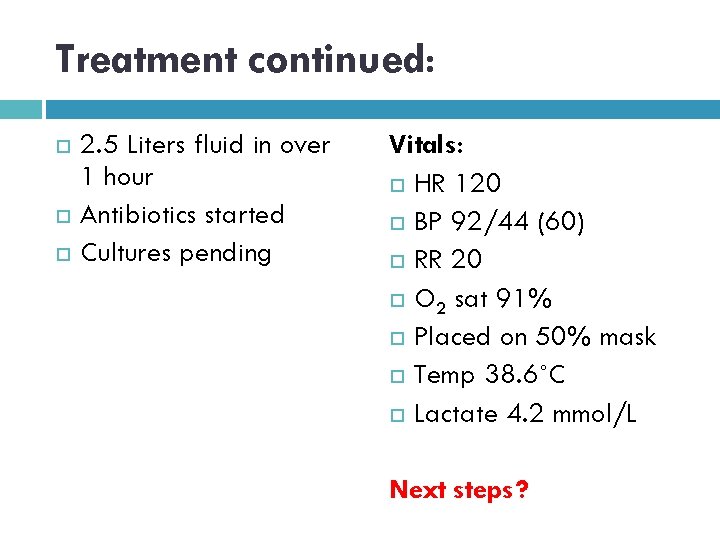
Treatment continued: 2. 5 Liters fluid in over 1 hour Antibiotics started Cultures pending Vitals: HR 120 BP 92/44 (60) RR 20 O 2 sat 91% Placed on 50% mask Temp 38. 6˚C Lactate 4. 2 mmol/L Next steps?
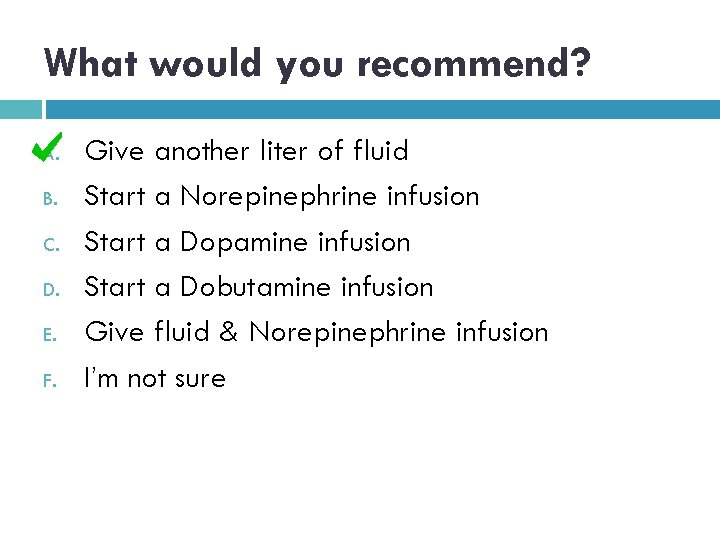
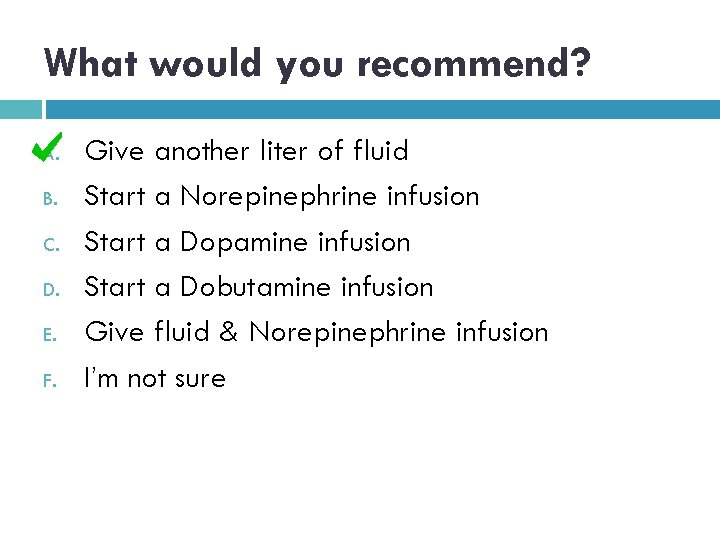
What would you recommend? A. B. C. D. E. F. Give another liter of fluid Start a Norepinephrine infusion Start a Dopamine infusion Start a Dobutamine infusion Give fluid & Norepinephrine infusion I’m not sure
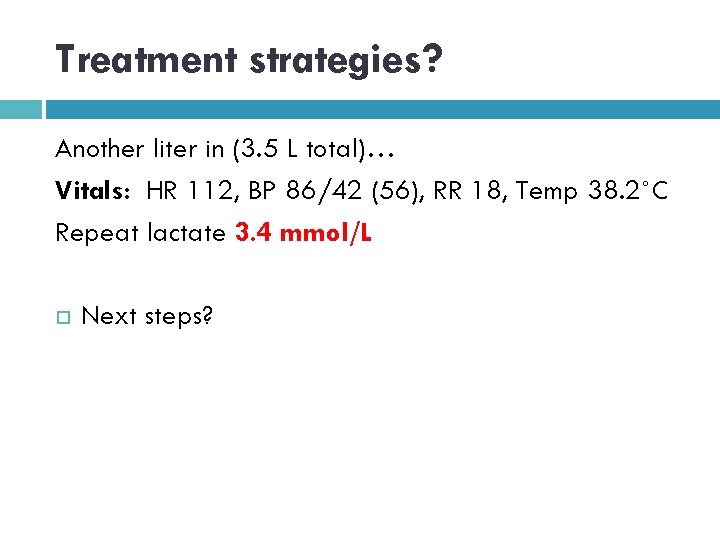
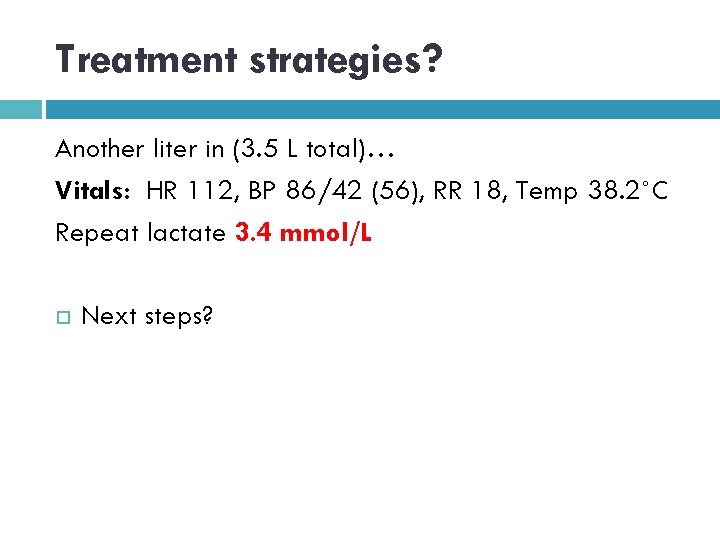
Treatment strategies? Another liter in (3. 5 L total)… Vitals: HR 112, BP 86/42 (56), RR 18, Temp 38. 2˚C Repeat lactate 3. 4 mmol/L Next steps?
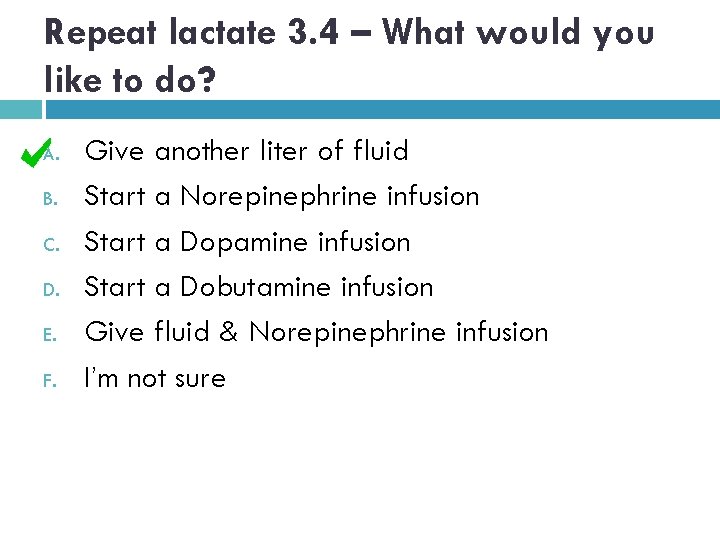
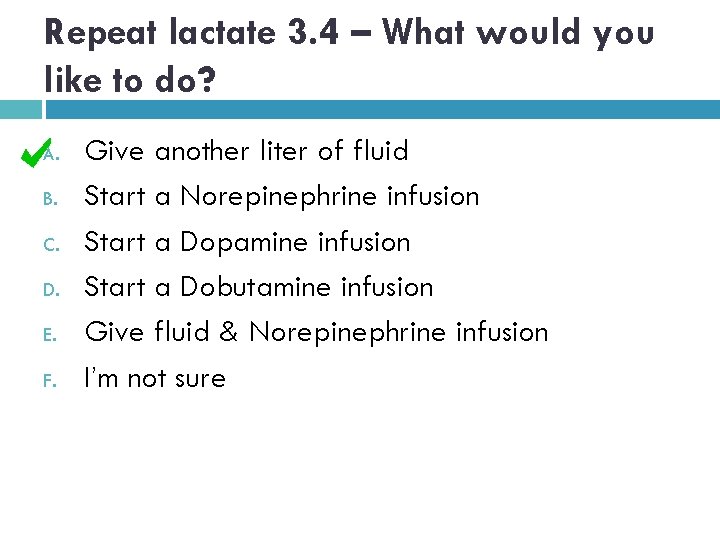
Repeat lactate 3. 4 – What would you like to do? A. B. C. D. E. F. Give another liter of fluid Start a Norepinephrine infusion Start a Dopamine infusion Start a Dobutamine infusion Give fluid & Norepinephrine infusion I’m not sure
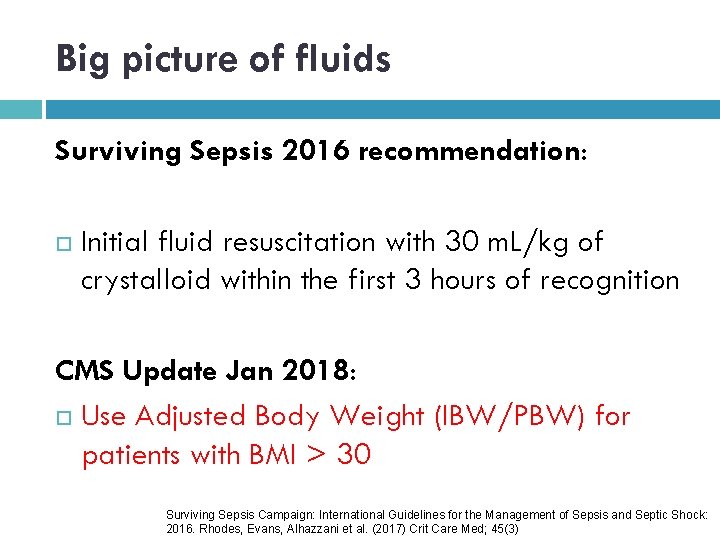
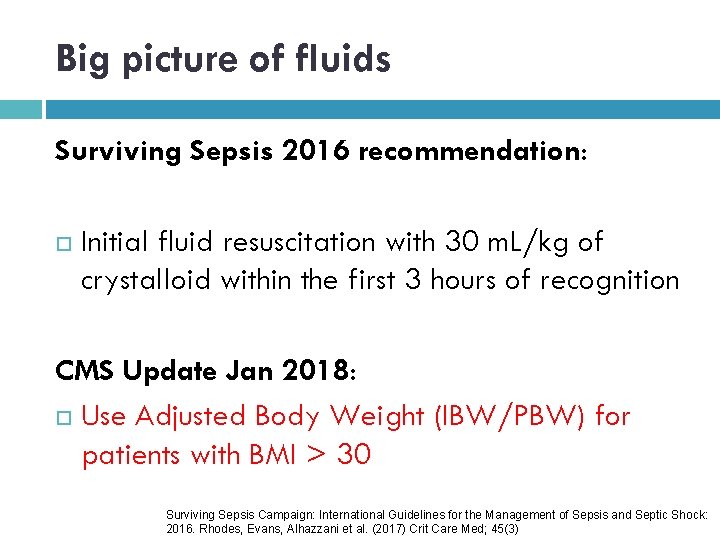
Big picture of fluids Surviving Sepsis 2016 recommendation: Initial fluid resuscitation with 30 m. L/kg of crystalloid within the first 3 hours of recognition CMS Update Jan 2018: Use Adjusted Body Weight (IBW/PBW) for patients with BMI > 30 Surviving Sepsis Campaign: International Guidelines for the Management of Sepsis and Septic Shock: 2016. Rhodes, Evans, Alhazzani et al. (2017) Crit Care Med; 45(3)
Which fluid would you expect to hang at your institution? A. B. C. D. 0. 9% Saline Lactated Ringers (LR) Plasma-Lyte A Albumin 5%
How many liters of saline are administered in the US every year? A. B. C. D. E. 20, 000 200, 000 2 million 200 million
Which fluid?
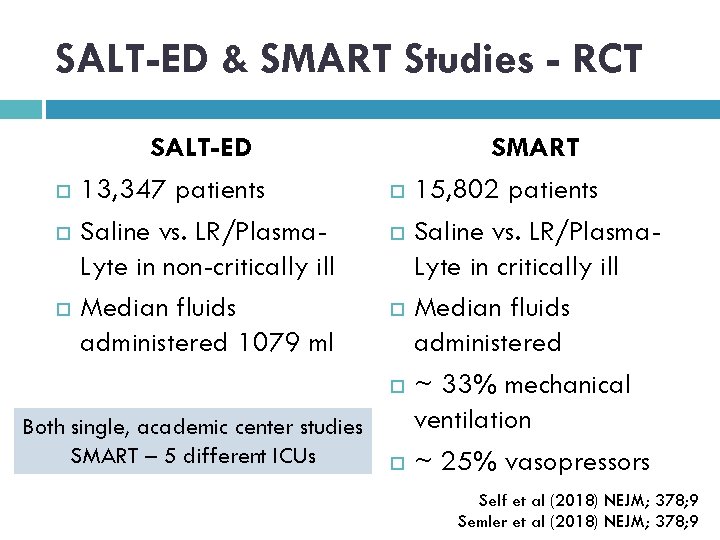
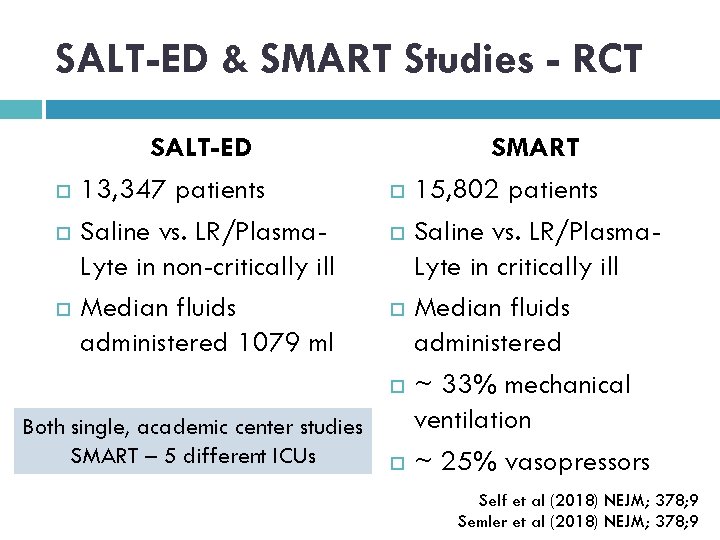
SALT-ED & SMART Studies - RCT SALT-ED 13, 347 patients Saline vs. LR/Plasma. Lyte in non-critically ill Median fluids administered 1079 ml Both single, academic center studies SMART – 5 different ICUs SMART 15, 802 patients Saline vs. LR/Plasma. Lyte in critically ill Median fluids administered ~ 33% mechanical ventilation ~ 25% vasopressors Self et al (2018) NEJM; 378; 9 Semler et al (2018) NEJM; 378; 9
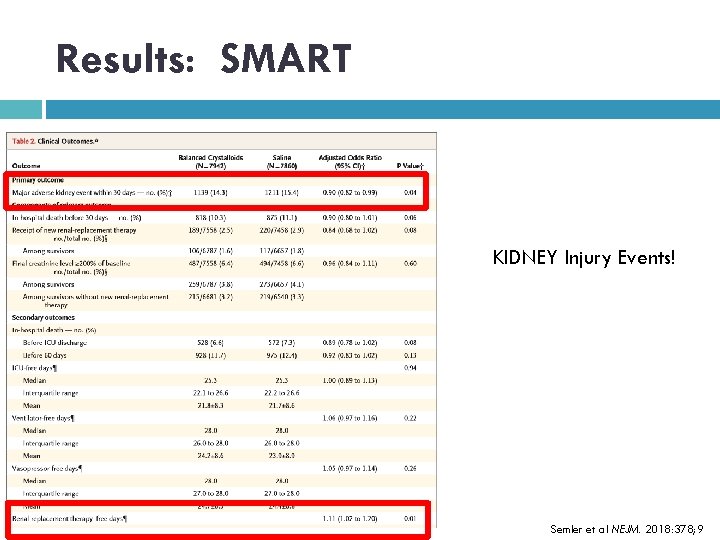
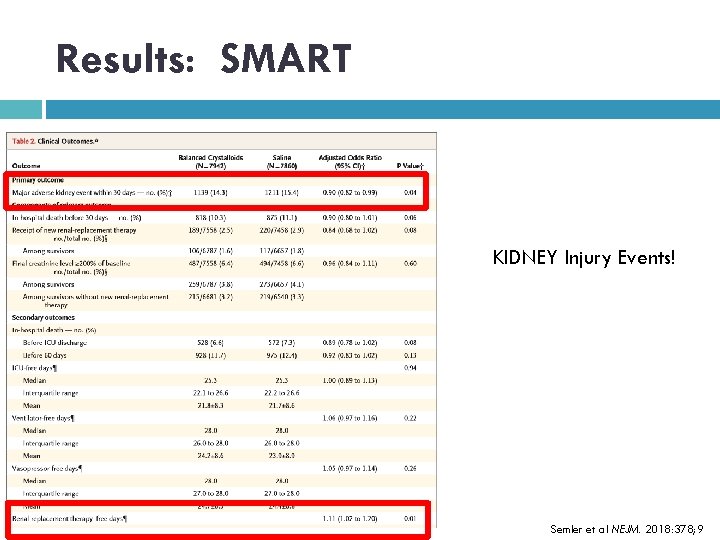
Results: SMART KIDNEY Injury Events! Semler et al NEJM. 2018: 378; 9
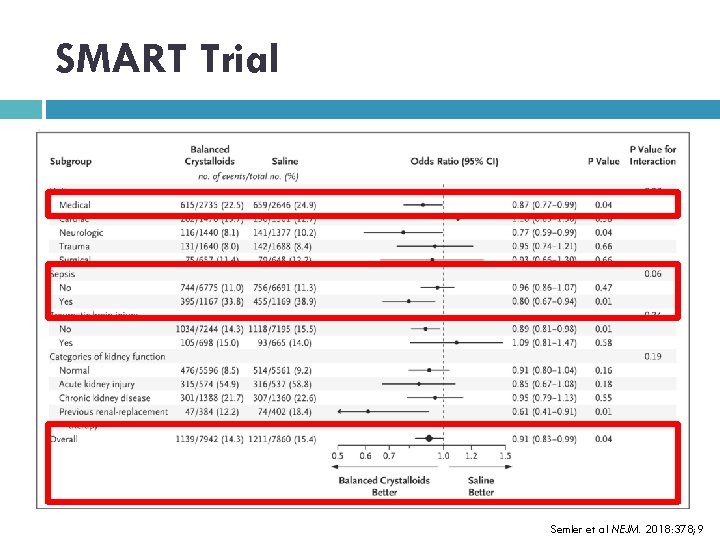
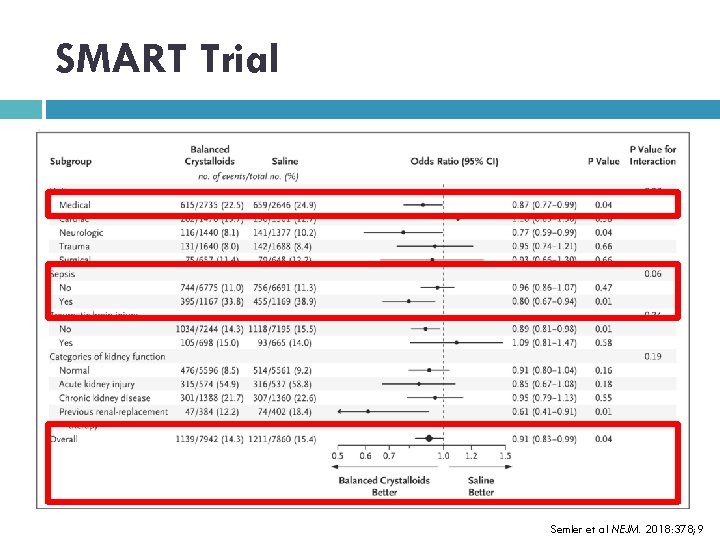
SMART Trial Semler et al NEJM. 2018: 378; 9
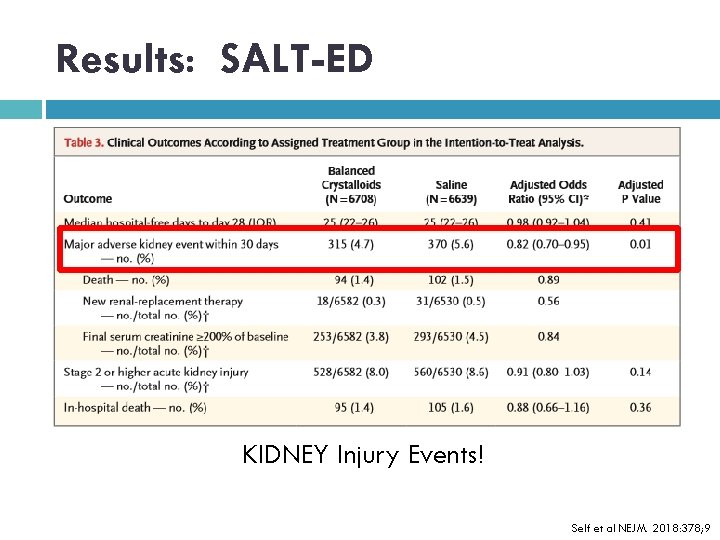
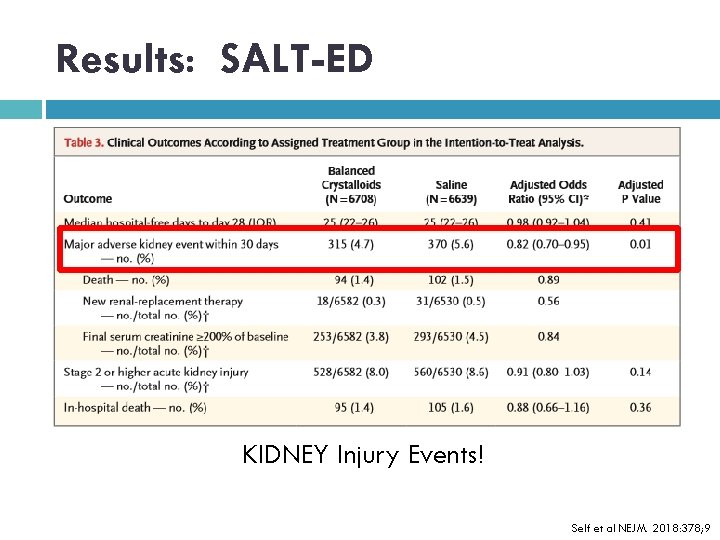
Results: SALT-ED KIDNEY Injury Events! Self et al NEJM. 2018: 378; 9
Who’s thinking, so what? ? ? 1% = 50, 000 - 70, 000 lives saved per year A reduction of over 100, 000 cases of AKI
Are all fluids created equal? !
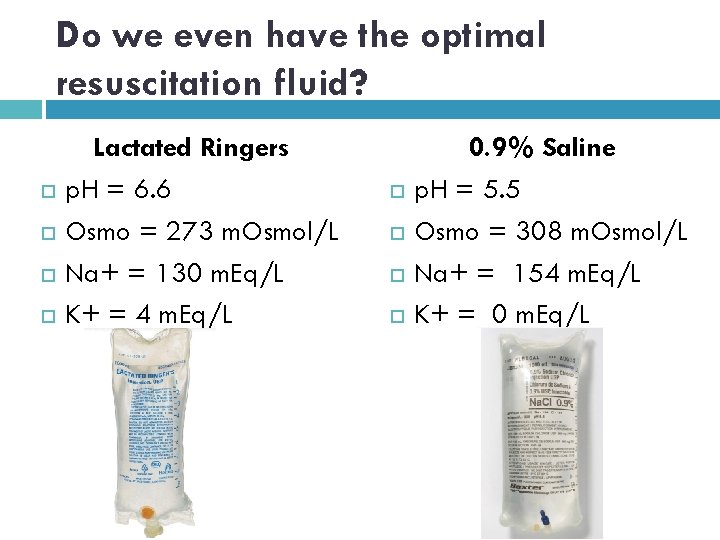
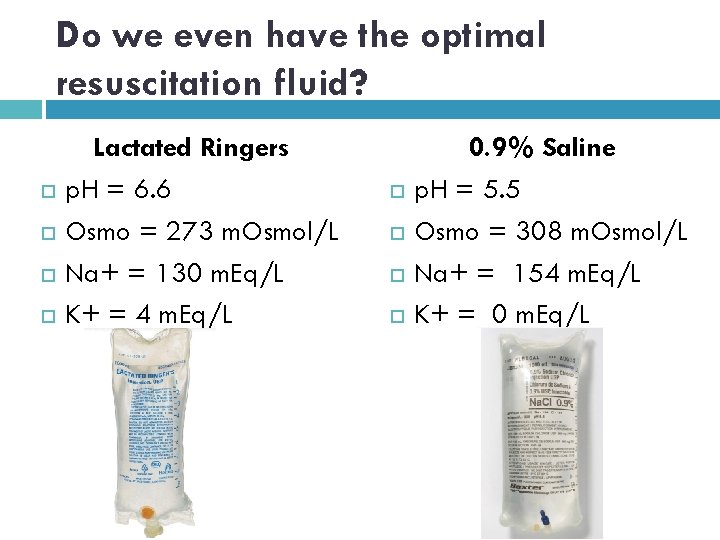
Do we even have the optimal resuscitation fluid? Lactated Ringers p. H = 6. 6 Osmo = 273 m. Osmol/L Na+ = 130 m. Eq/L K+ = 4 m. Eq/L 0. 9% Saline p. H = 5. 5 Osmo = 308 m. Osmol/L Na+ = 154 m. Eq/L K+ = 0 m. Eq/L
Sodium Anybody? . . . Anybody? = 1 liter “Normal Saline”
Hyperchloremia Reduces renal blood flow Reduces glomerular filtration Has been shown as an independent risk factor for hospital mortality Hyperchloremic metabolic acidosis Increases risk for lung injury Neyra JA et al. (2015) Association of hyperchloremia with hospital mortality in critically ill septic patients. Crit Care Med. 43(9): 1938 -1944.
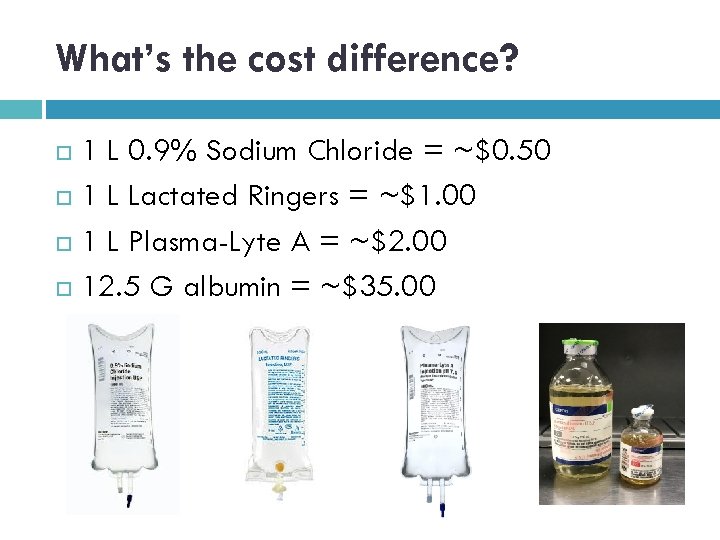
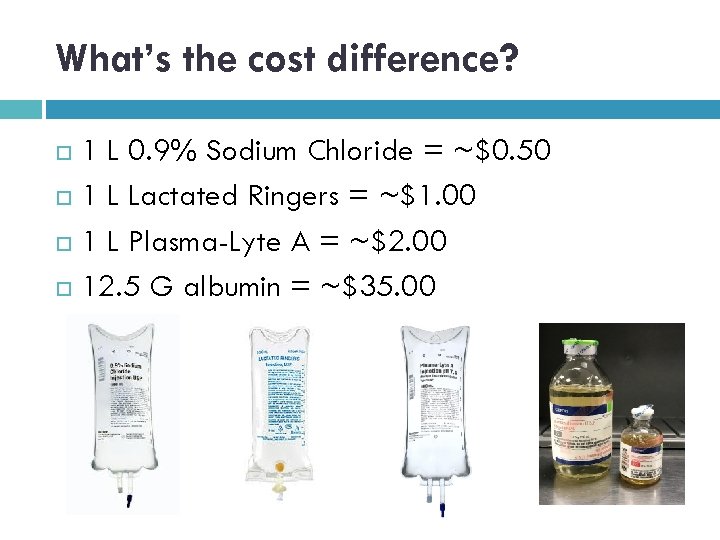
What’s the cost difference? 1 L 0. 9% Sodium Chloride = ~$0. 50 1 L Lactated Ringers = ~$1. 00 1 L Plasma-Lyte A = ~$2. 00 12. 5 G albumin = ~$35. 00
How do you know if your patient is a fluid responder? OR
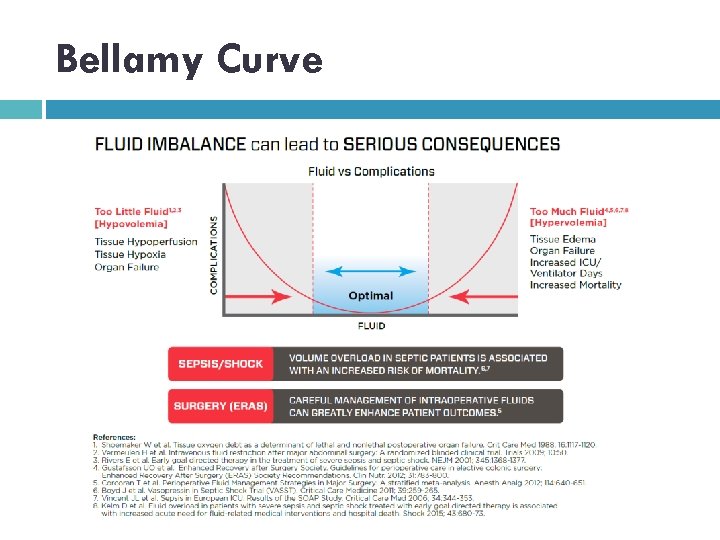
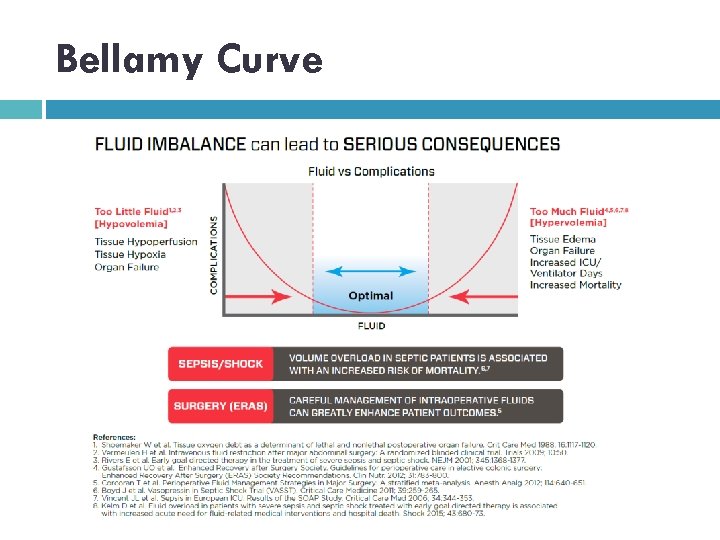
Bellamy Curve
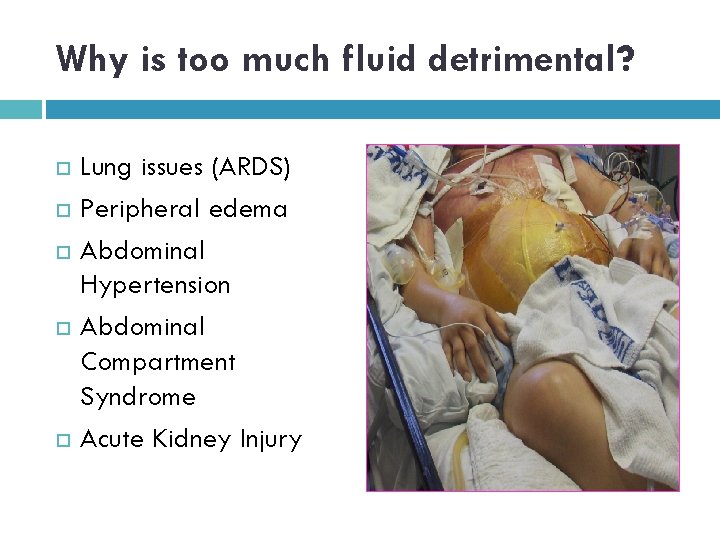
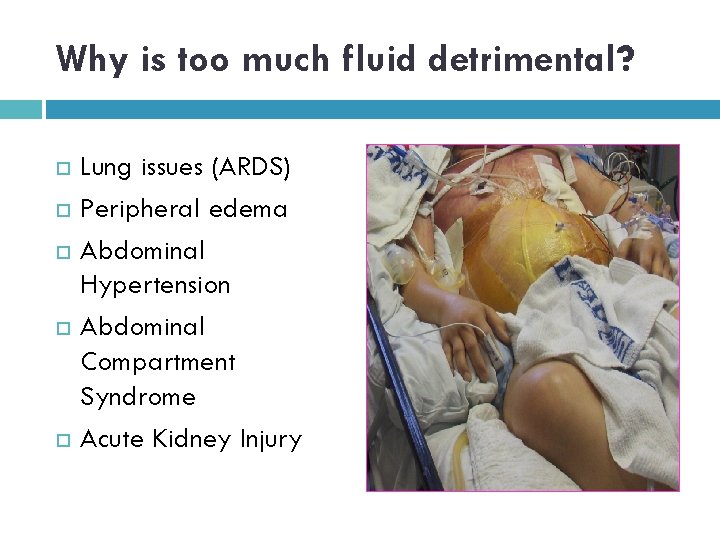
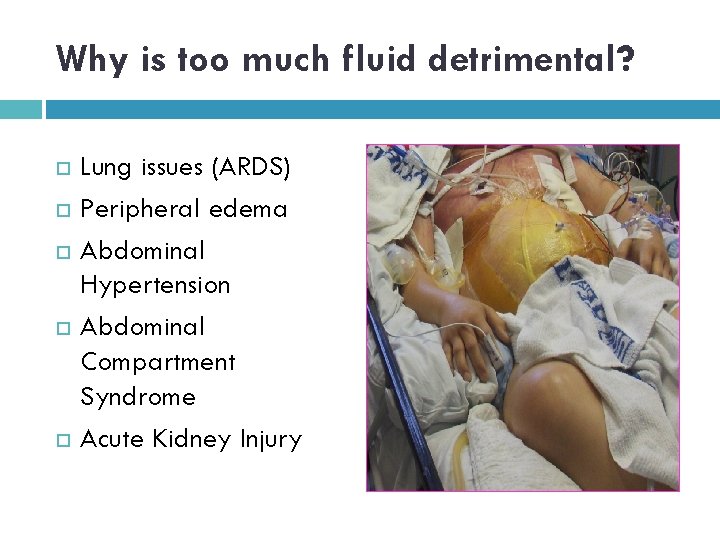
Why is too much fluid detrimental? Lung issues (ARDS) Peripheral edema Abdominal Hypertension Abdominal Compartment Syndrome Acute Kidney Injury
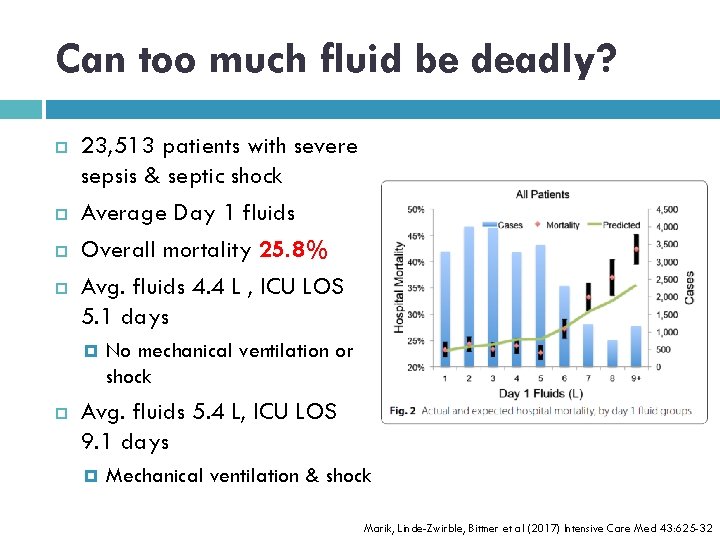
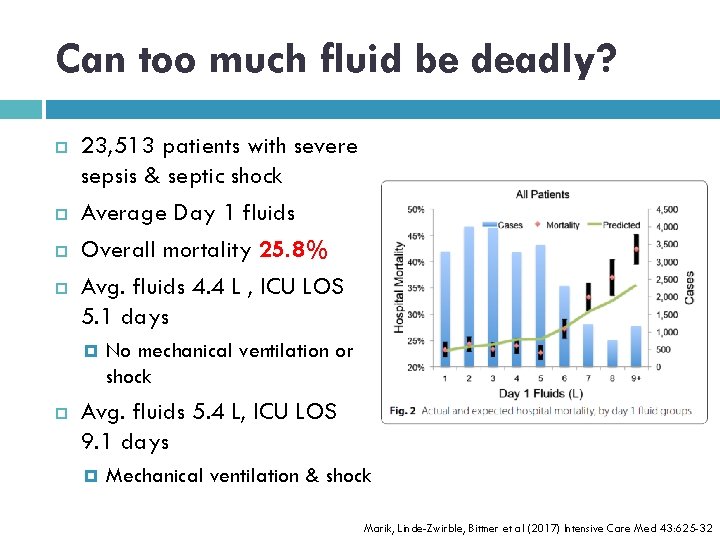
Can too much fluid be deadly? 23, 513 patients with severe sepsis & septic shock Average Day 1 fluids Overall mortality 25. 8% Avg. fluids 4. 4 L , ICU LOS 5. 1 days No mechanical ventilation or shock Avg. fluids 5. 4 L, ICU LOS 9. 1 days Mechanical ventilation & shock Marik, Linde-Zwirble, Bittner et al (2017) Intensive Care Med 43: 625 -32
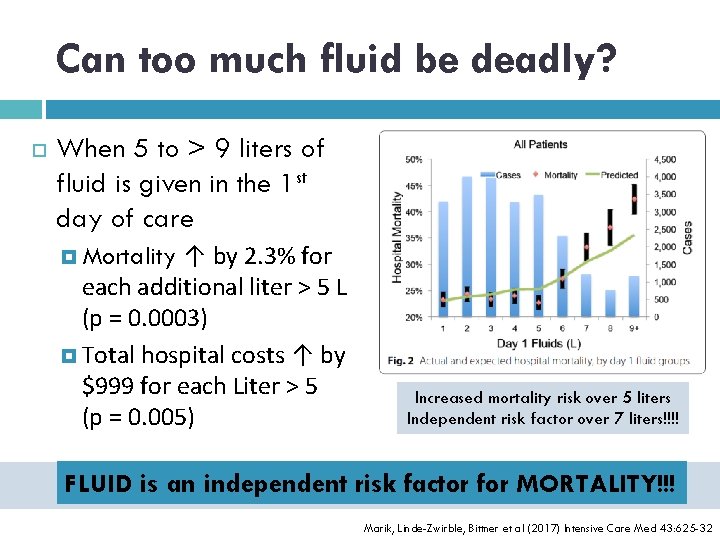
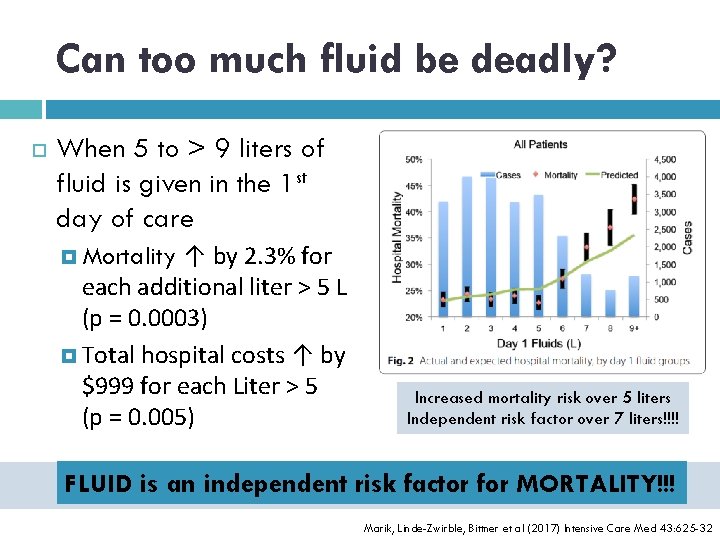
Can too much fluid be deadly? When 5 to > 9 liters of fluid is given in the 1 st day of care ↑ by 2. 3% for each additional liter > 5 L (p = 0. 0003) Total hospital costs ↑ by $999 for each Liter > 5 (p = 0. 005) Mortality Increased mortality risk over 5 liters Independent risk factor over 7 liters!!!! FLUID is an independent risk factor for MORTALITY!!! HOLY WOWZERS!!!!! Marik, Linde-Zwirble, Bittner et al (2017) Intensive Care Med 43: 625 -32
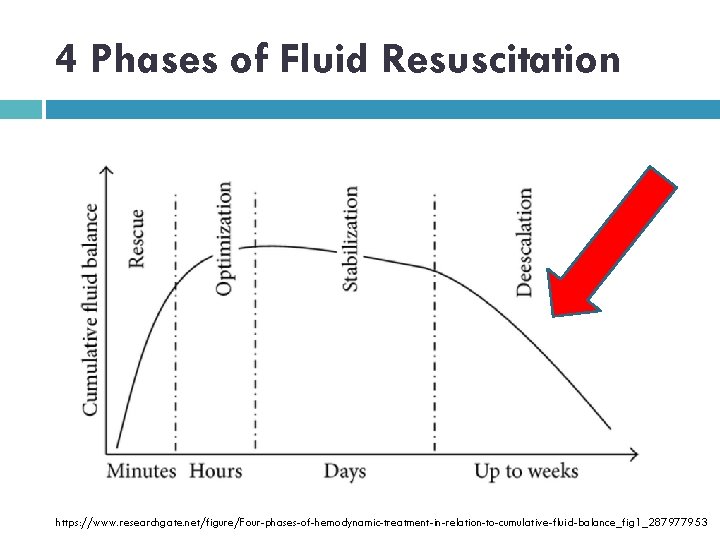
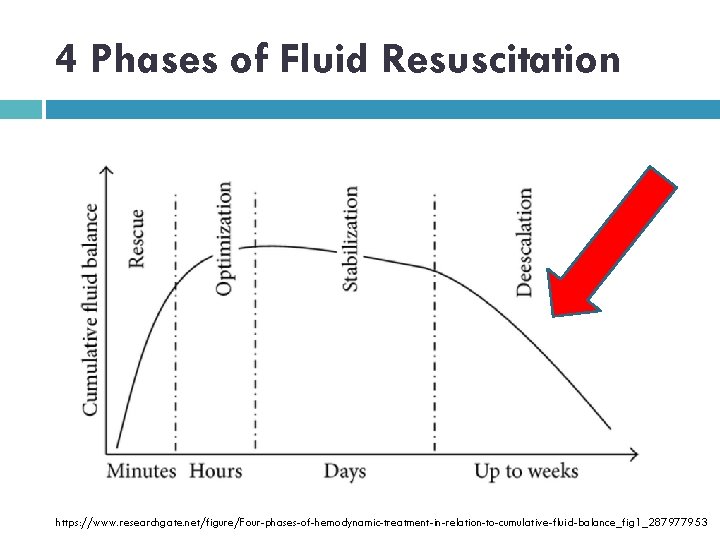
4 Phases of Fluid Resuscitation https: //www. researchgate. net/figure/Four-phases-of-hemodynamic-treatment-in-relation-to-cumulative-fluid-balance_fig 1_287977953
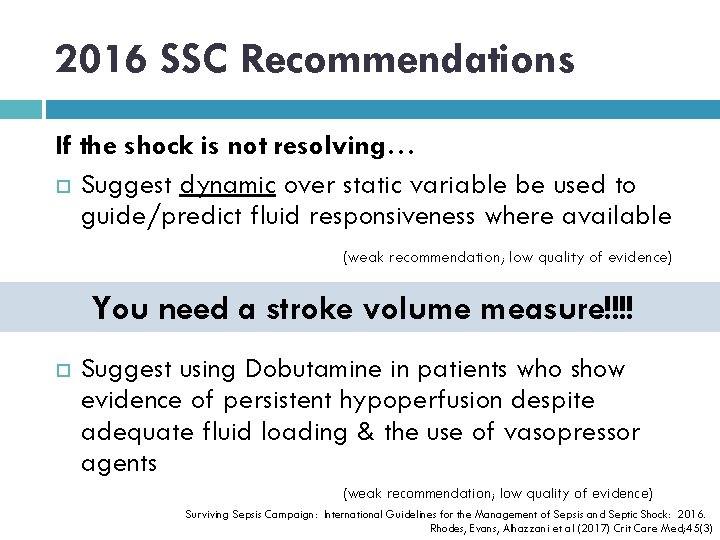
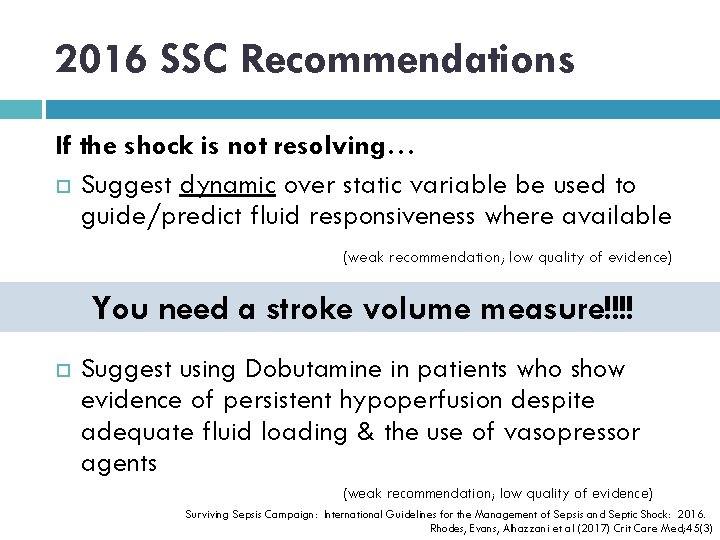
2016 SSC Recommendations If the shock is not resolving… Suggest dynamic over static variable be used to guide/predict fluid responsiveness where available (weak recommendation; low quality of evidence) You need a stroke volume measure!!!! Suggest using Dobutamine in patients who show evidence of persistent hypoperfusion despite adequate fluid loading & the use of vasopressor agents (weak recommendation; low quality of evidence) Surviving Sepsis Campaign: International Guidelines for the Management of Sepsis and Septic Shock: 2016. Rhodes, Evans, Alhazzani et al (2017) Crit Care Med; 45(3)
Is STROKE VOLUME the 6 th vital sign?
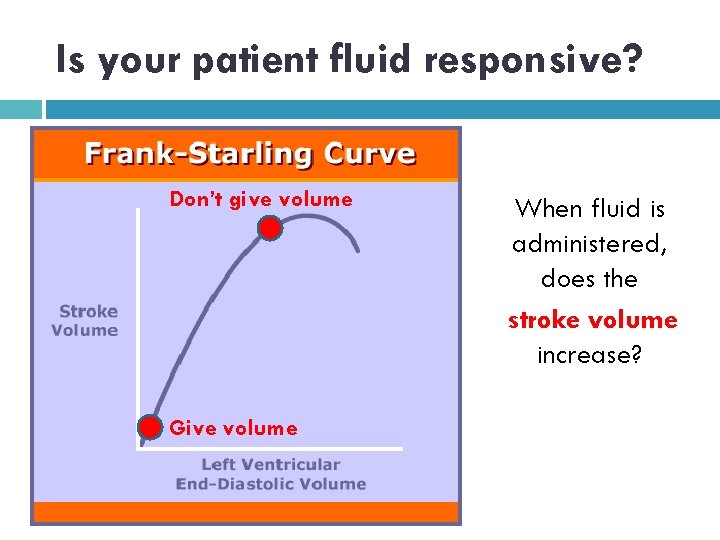
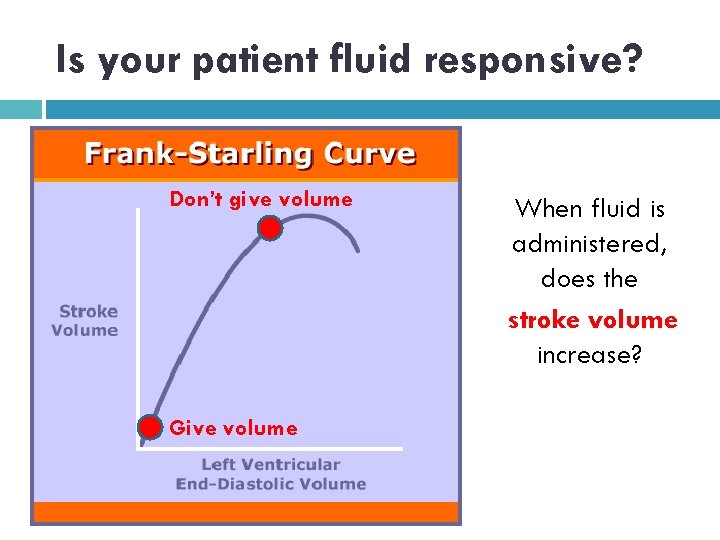
Is your patient fluid responsive? Don’t give volume Give volume When fluid is administered, does the stroke volume increase?
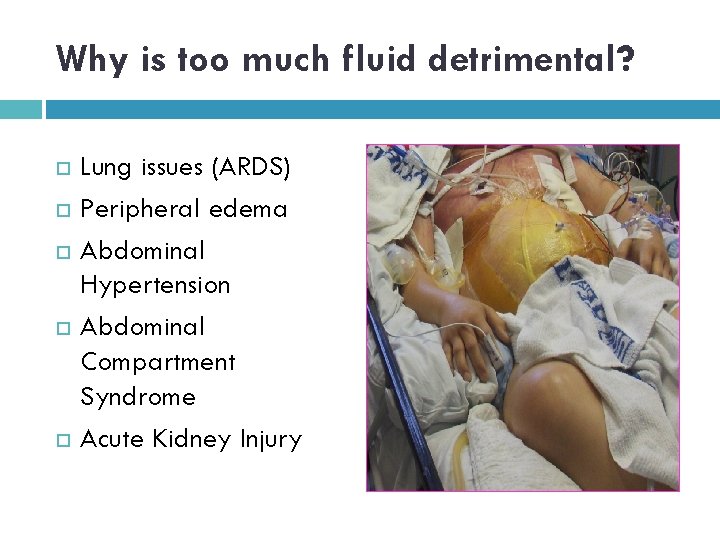
Why is too much fluid detrimental? Lung issues (ARDS) Peripheral edema Abdominal Hypertension Abdominal Compartment Syndrome Acute Kidney Injury
In Sepsis, when should a pressor be started?
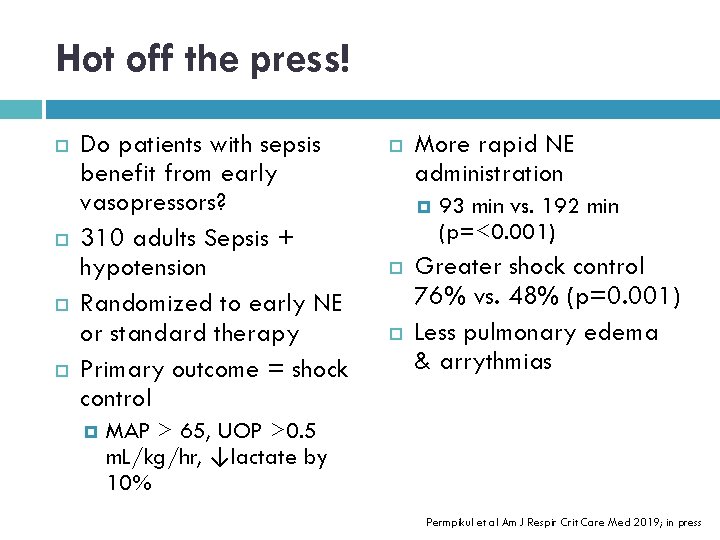
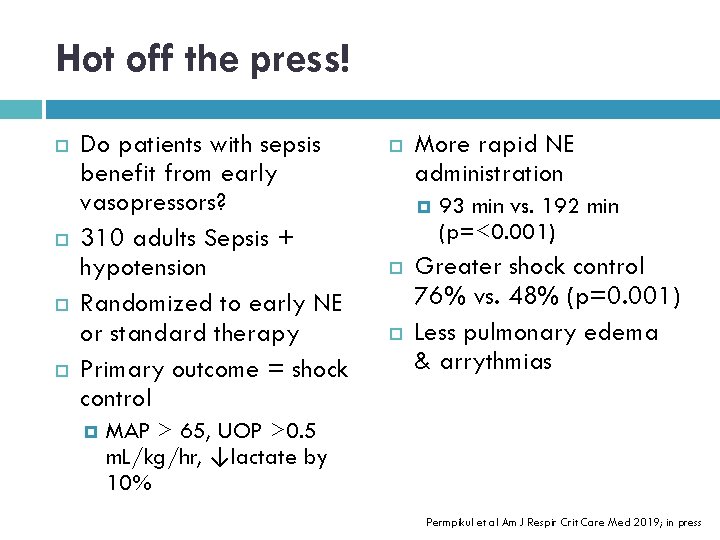
Hot off the press! Do patients with sepsis benefit from early vasopressors? 310 adults Sepsis + hypotension Randomized to early NE or standard therapy Primary outcome = shock control More rapid NE administration 93 min vs. 192 min (p=<0. 001) Greater shock control 76% vs. 48% (p=0. 001) Less pulmonary edema & arrythmias MAP > 65, UOP >0. 5 m. L/kg/hr, ↓lactate by 10% Permpikul et al Am J Respir Crit Care Med 2019; in press
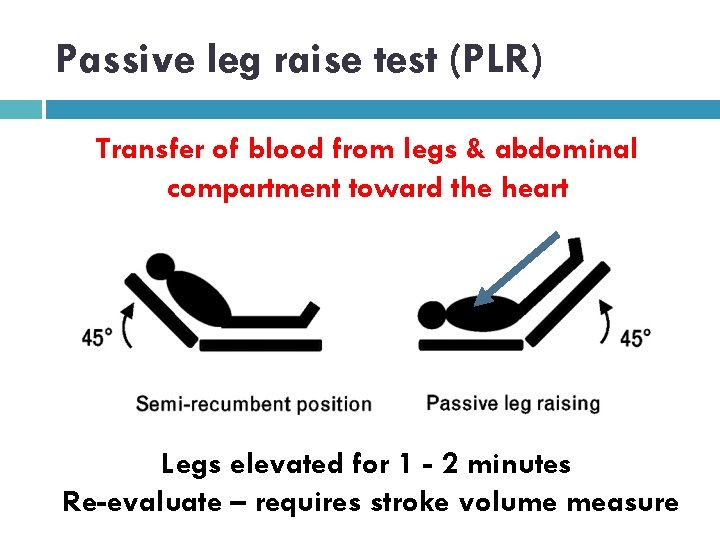
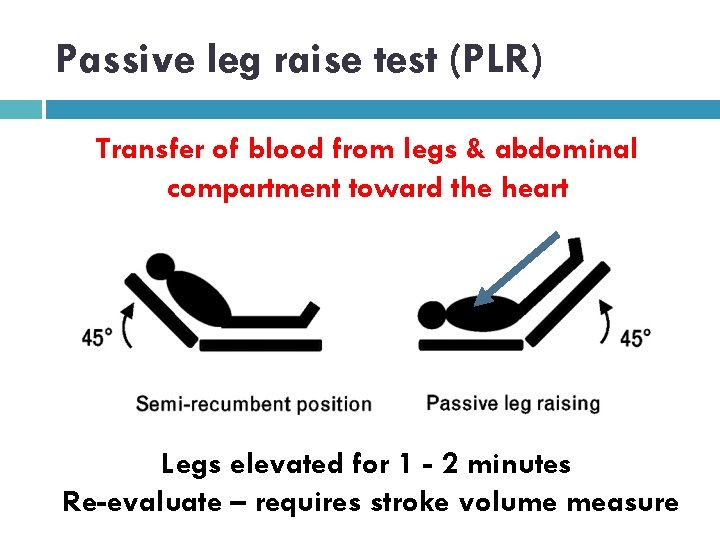
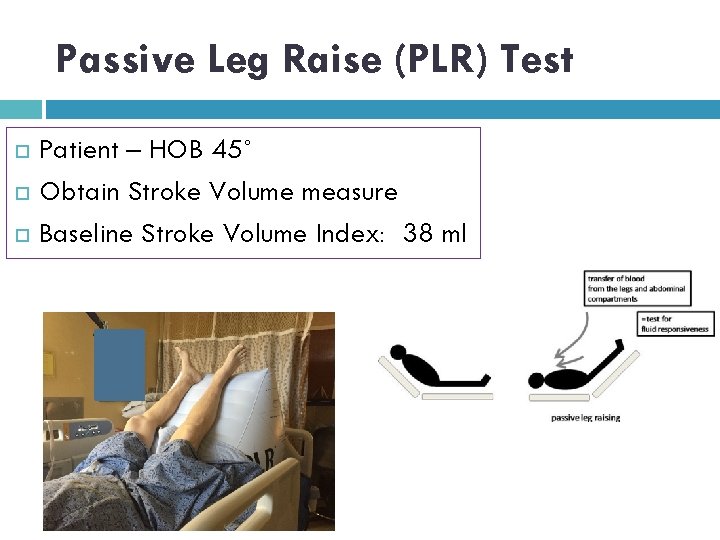
Passive leg raise test (PLR) Transfer of blood from legs & abdominal compartment toward the heart Legs elevated for 1 - 2 minutes Re-evaluate – requires stroke volume measure
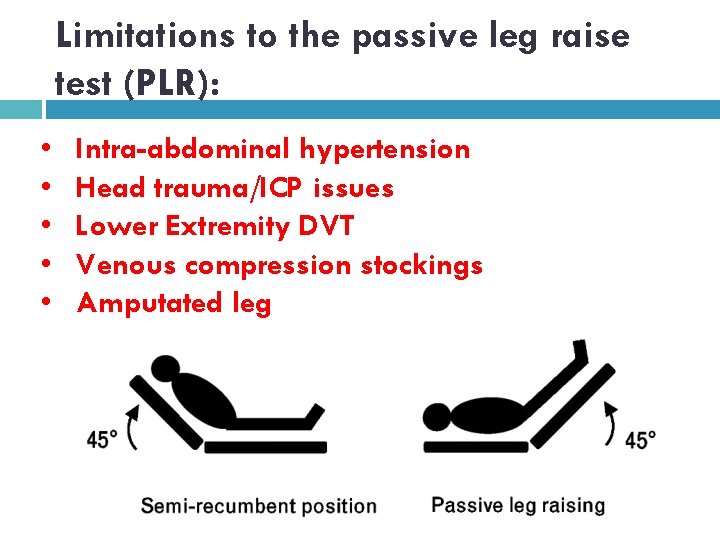
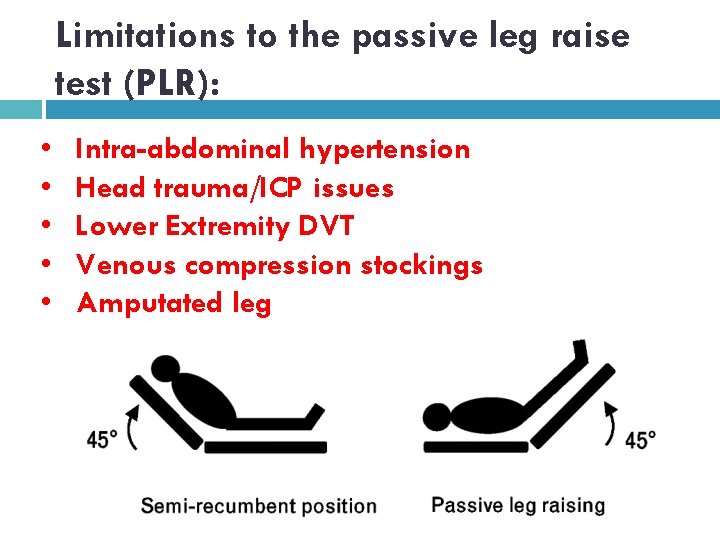
Limitations to the passive leg raise test (PLR): • • • Intra-abdominal hypertension Head trauma/ICP issues Lower Extremity DVT Venous compression stockings Amputated leg
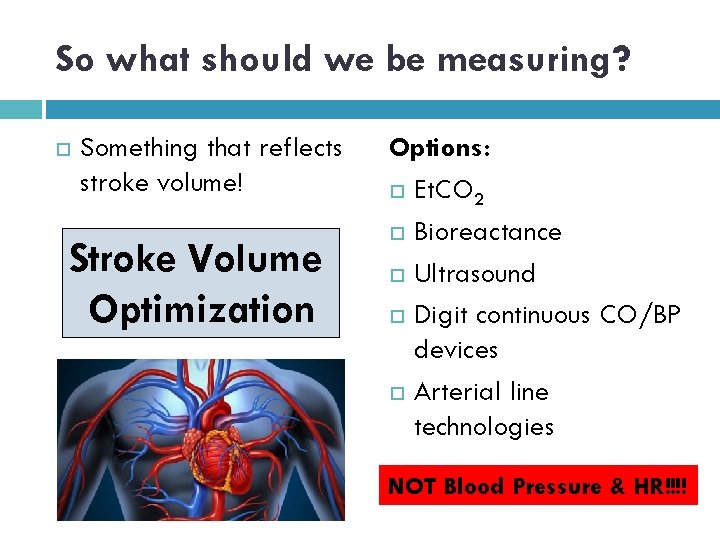
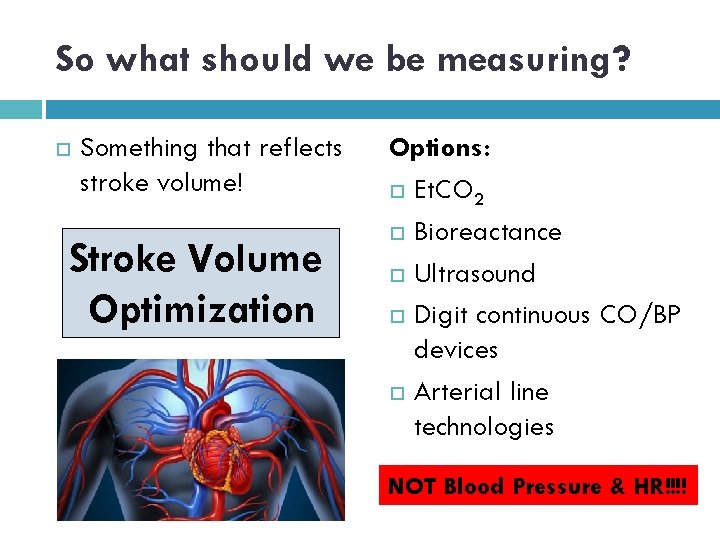
So what should we be measuring? Something that reflects stroke volume! Stroke Volume Optimization Options: Et. CO 2 Bioreactance Ultrasound Digit continuous CO/BP devices Arterial line technologies NOT Blood Pressure & HR!!!!
IVC collapse to predict fluid responsiveness?
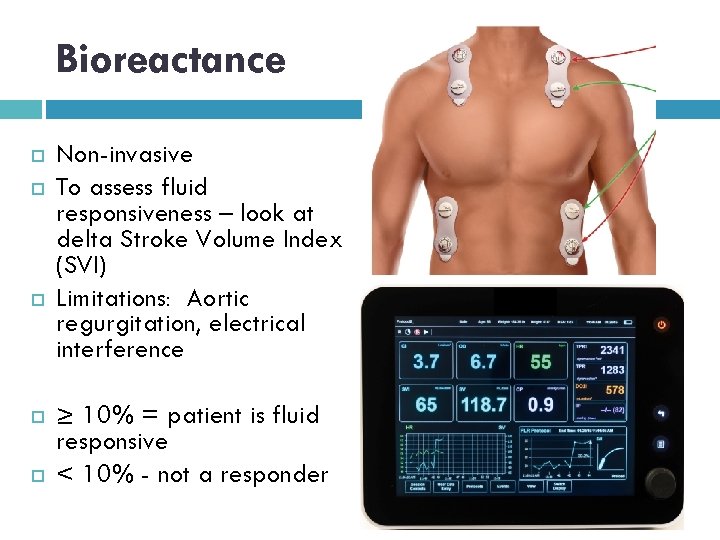
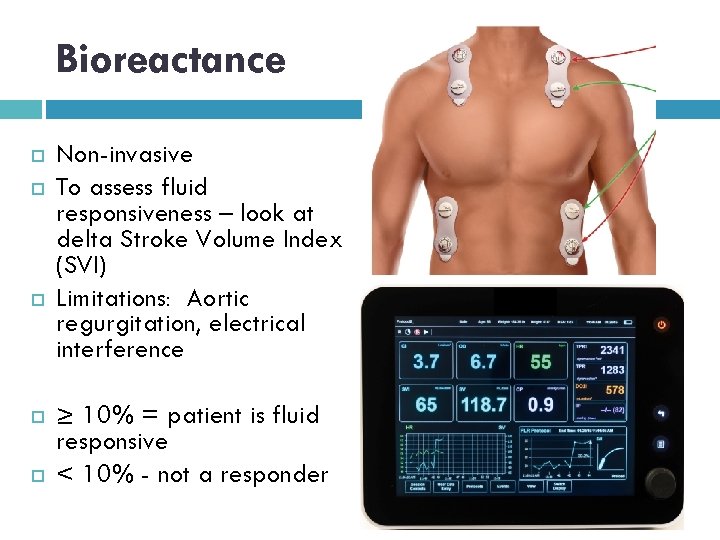
Bioreactance Non-invasive To assess fluid responsiveness – look at delta Stroke Volume Index (SVI) Limitations: Aortic regurgitation, electrical interference ≥ 10% = patient is fluid responsive < 10% - not a responder

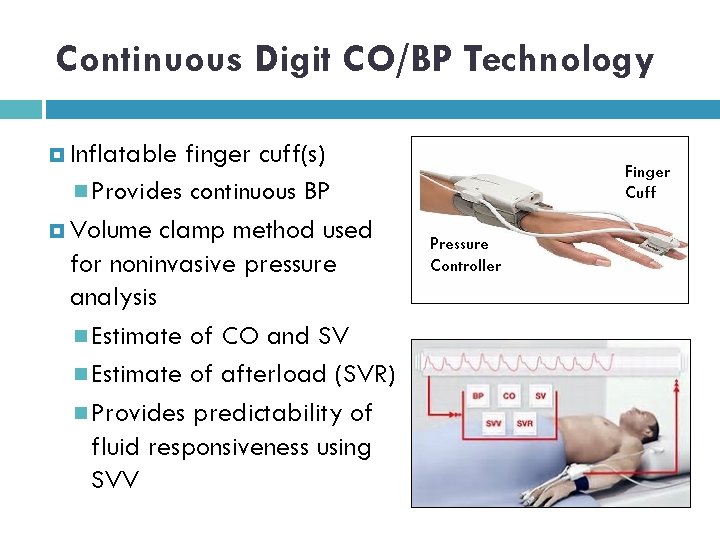
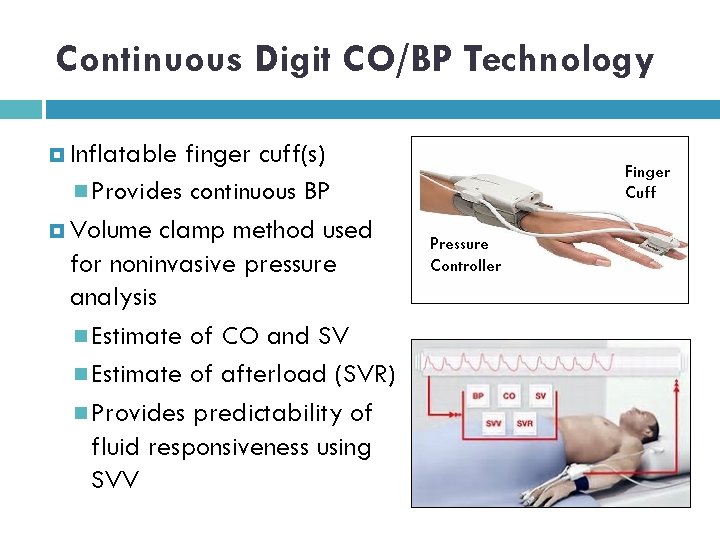
Continuous Digit CO/BP Technology Inflatable finger cuff(s) Provides continuous BP Volume clamp method used for noninvasive pressure analysis Estimate of CO and SV Estimate of afterload (SVR) Provides predictability of fluid responsiveness using SVV Finger Cuff Pressure Controller
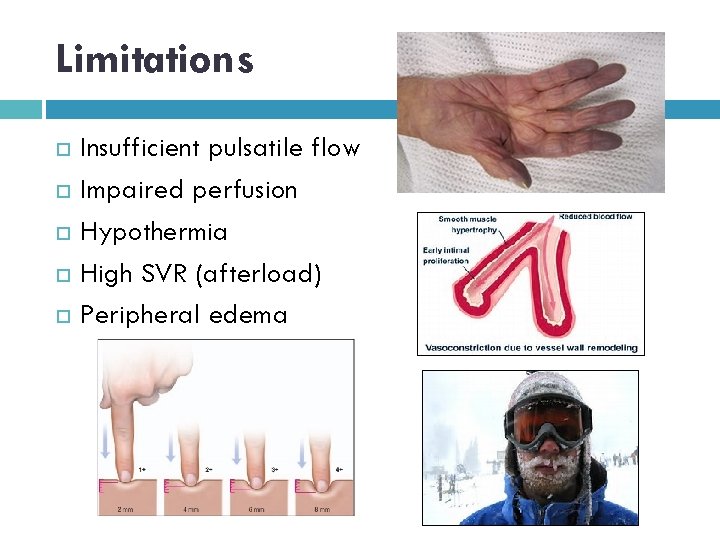
Limitations Insufficient pulsatile flow Impaired perfusion Hypothermia High SVR (afterload) Peripheral edema
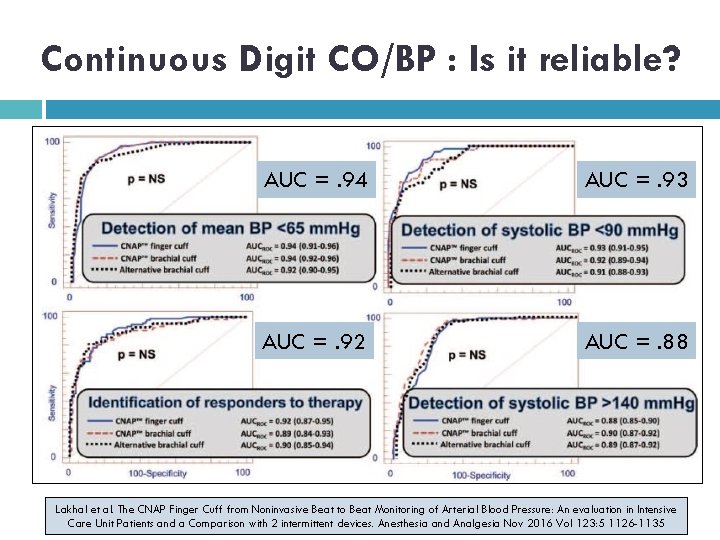
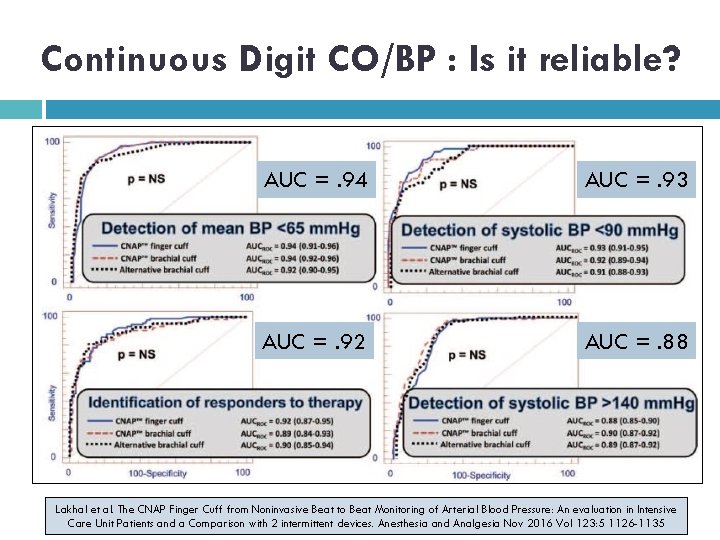
Continuous Digit CO/BP : Is it reliable? AUC =. 94 AUC =. 93 AUC =. 92 AUC =. 88 Lakhal et al. The CNAP Finger Cuff from Noninvasive Beat to Beat Monitoring of Arterial Blood Pressure: An evaluation in Intensive Care Unit Patients and a Comparison with 2 intermittent devices. Anesthesia and Analgesia Nov 2016 Vol 123: 5 1126 -1135
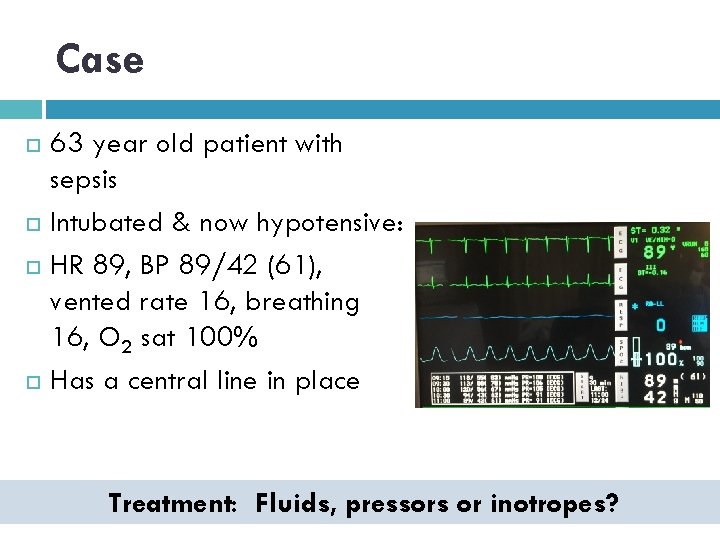
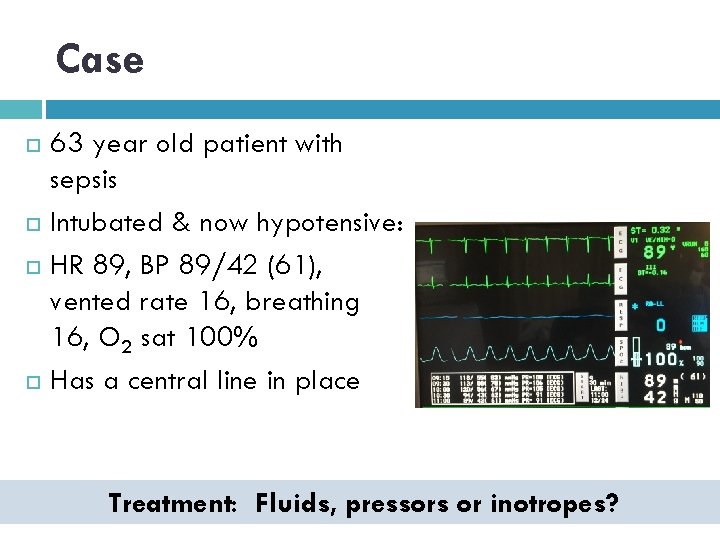
Case 63 year old patient with sepsis Intubated & now hypotensive: HR 89, BP 89/42 (61), vented rate 16, breathing 16, O 2 sat 100% Has a central line in place Treatment: Fluids, pressors or inotropes?
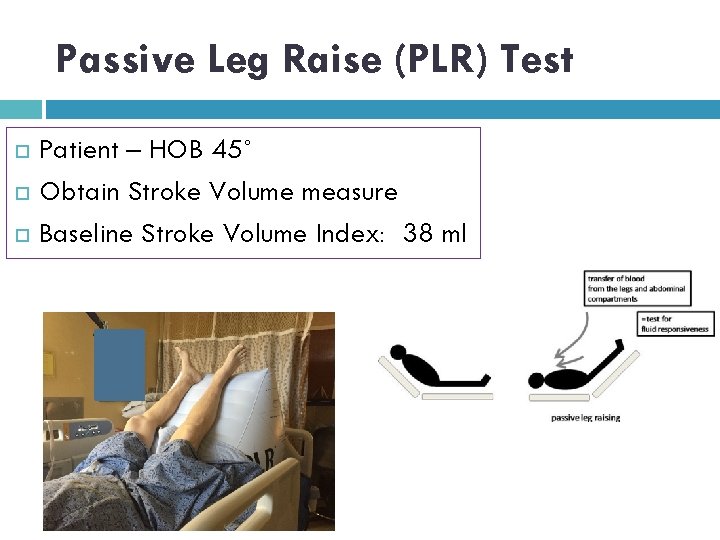
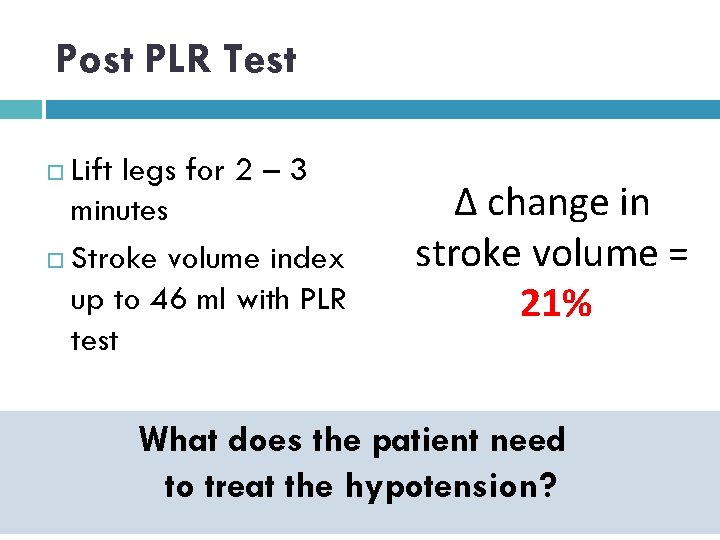
Passive Leg Raise (PLR) Test Patient – HOB 45˚ Obtain Stroke Volume measure Baseline Stroke Volume Index: 38 ml
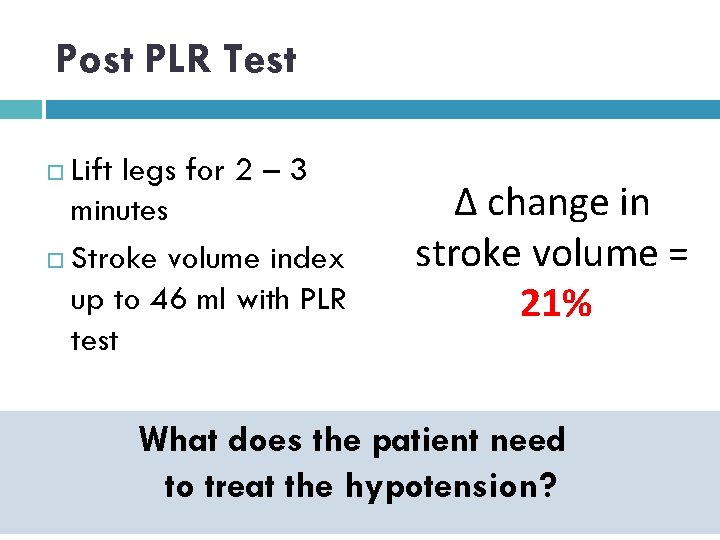
Post PLR Test Lift legs for 2 – 3 minutes Stroke volume index up to 46 ml with PLR test Δ change in stroke volume = 21% What does the patient need to treat the hypotension?
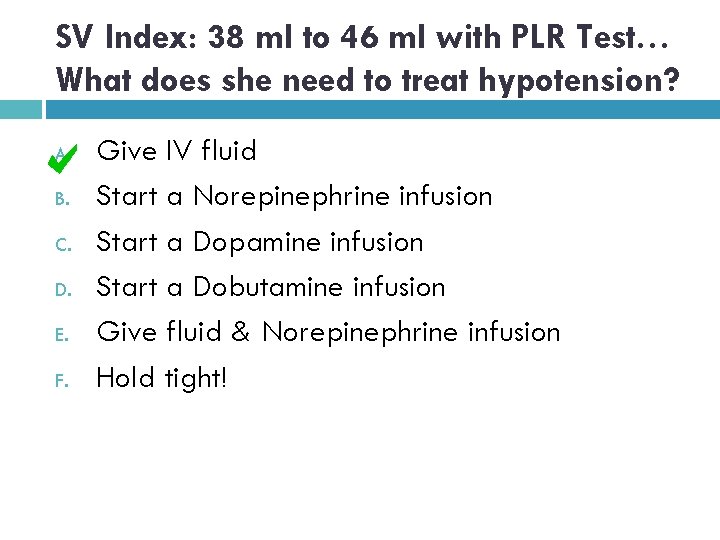
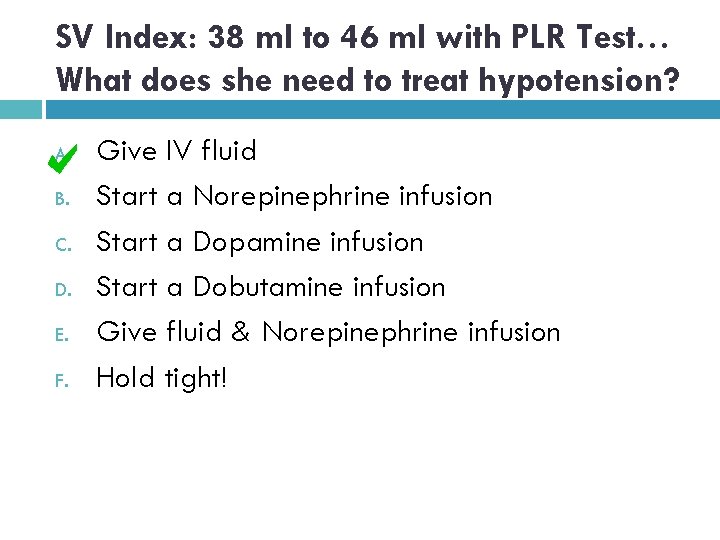
SV Index: 38 ml to 46 ml with PLR Test… What does she need to treat hypotension? A. B. C. D. E. F. Give IV fluid Start a Norepinephrine infusion Start a Dopamine infusion Start a Dobutamine infusion Give fluid & Norepinephrine infusion Hold tight!
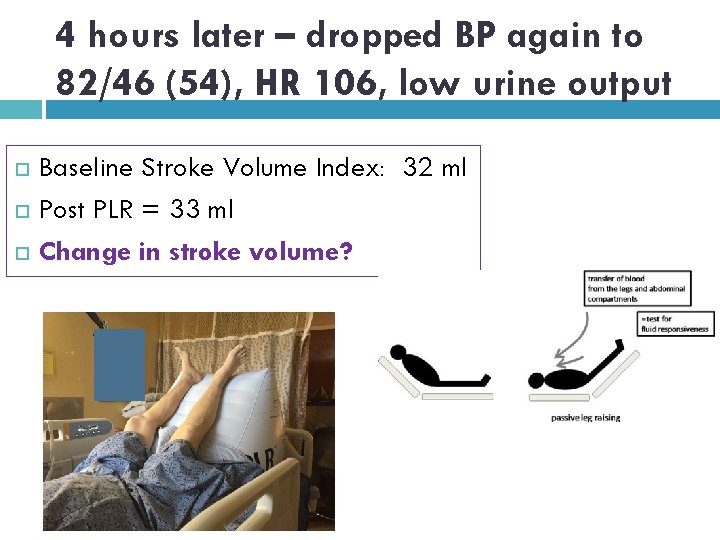
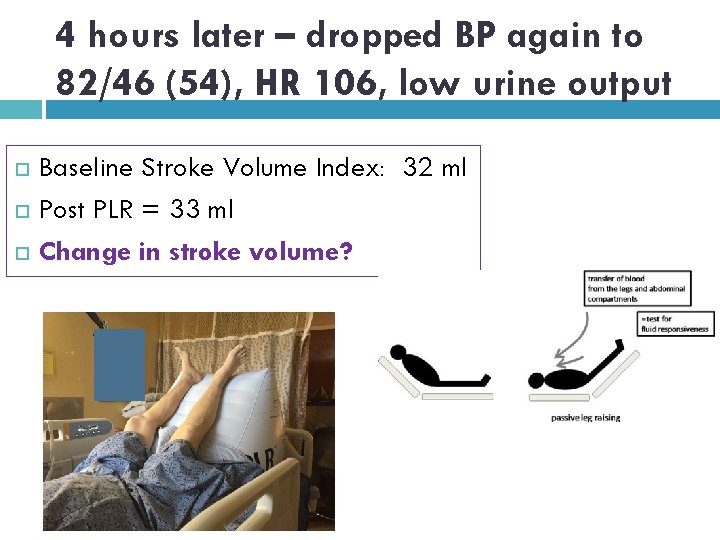
4 hours later – dropped BP again to 82/46 (54), HR 106, low urine output Baseline Stroke Volume Index: 32 ml Post PLR = 33 ml Change in stroke volume?
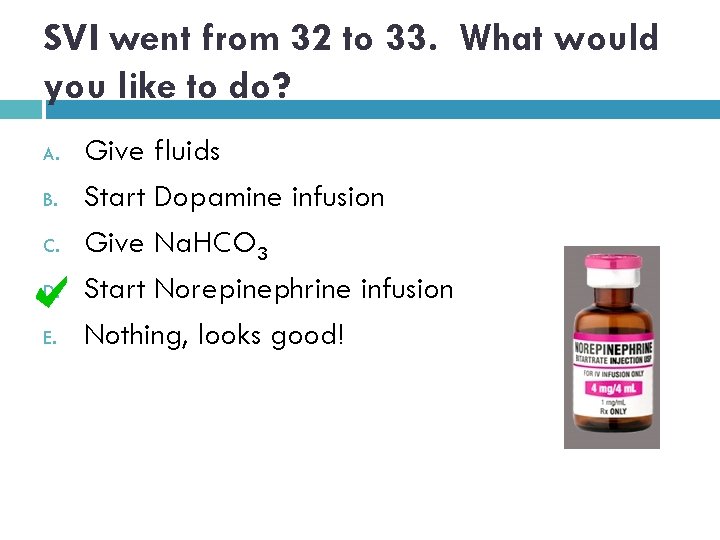
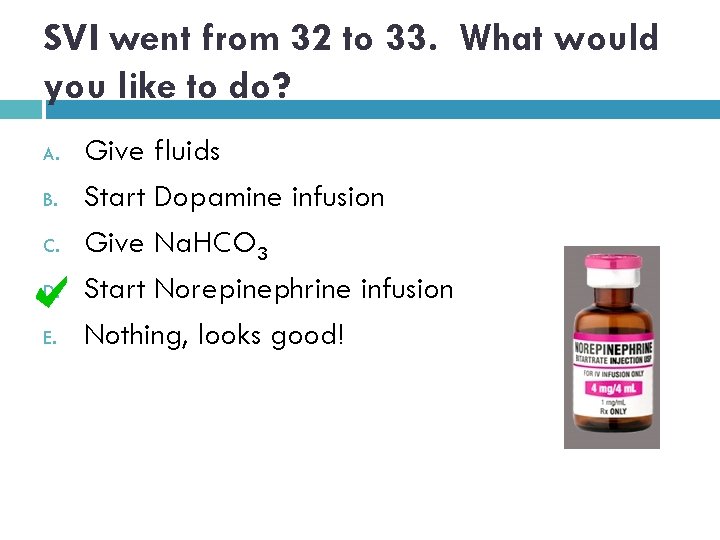
SVI went from 32 to 33. What would you like to do? A. B. C. D. E. Give fluids Start Dopamine infusion Give Na. HCO 3 Start Norepinephrine infusion Nothing, looks good!
Before & After Using Ni. COM University of Kansas Before & after, severe sepsis/septic shock Fluid guided by NICOM vs. usual care “guessing” 100 patients in NICOM group, 91 patients in usual care 53% of patients needed treatment in NICOM group (if SV Δ > 10%) Latham H, Bengtson CD, Satterwhite L, Stites M, et al (2017) Journal of Critical Care, 42: 42 -46
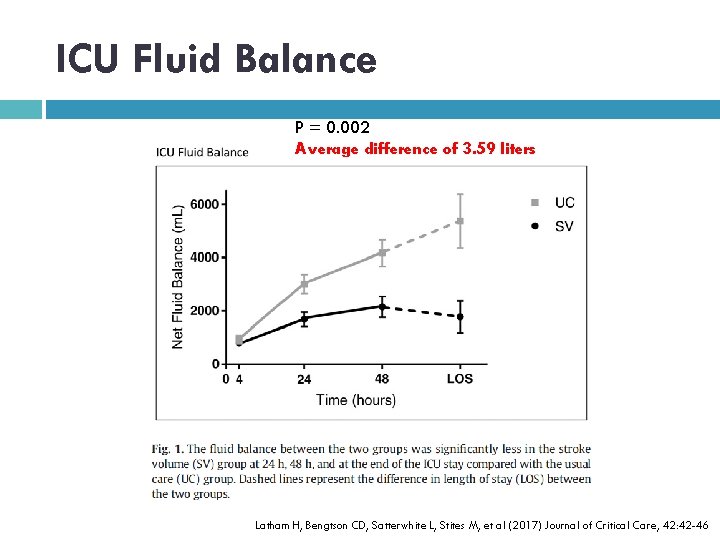
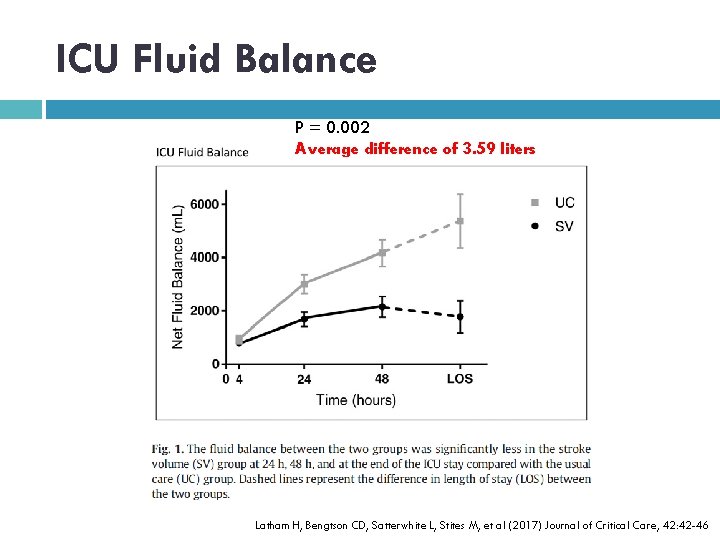
ICU Fluid Balance P = 0. 002 Average difference of 3. 59 liters Latham H, Bengtson CD, Satterwhite L, Stites M, et al (2017) Journal of Critical Care, 42: 42 -46
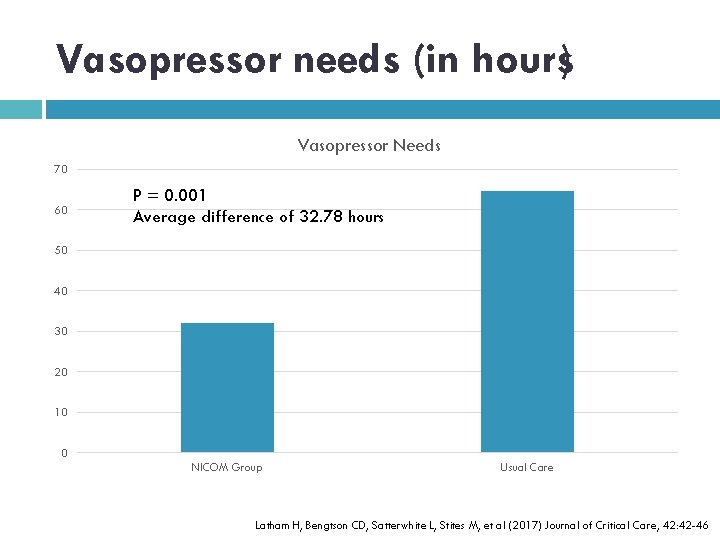
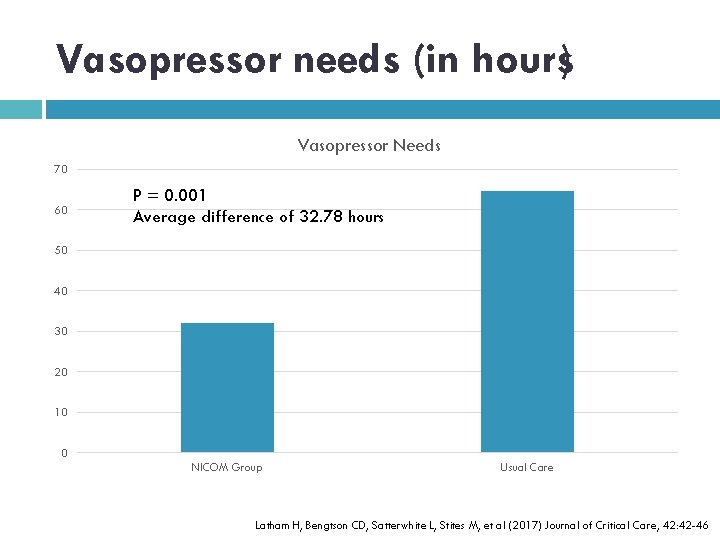
Vasopressor needs (in hours) Vasopressor Needs 70 60 P = 0. 001 Average difference of 32. 78 hours 50 40 30 20 10 0 NICOM Group Usual Care Latham H, Bengtson CD, Satterwhite L, Stites M, et al (2017) Journal of Critical Care, 42: 42 -46
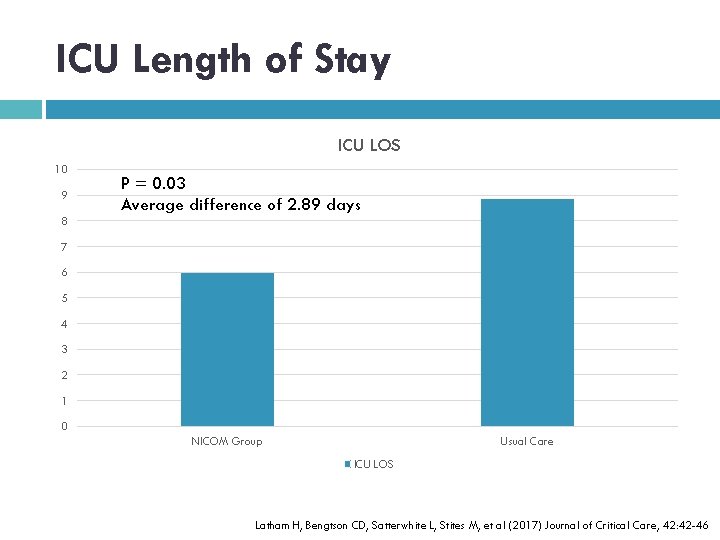
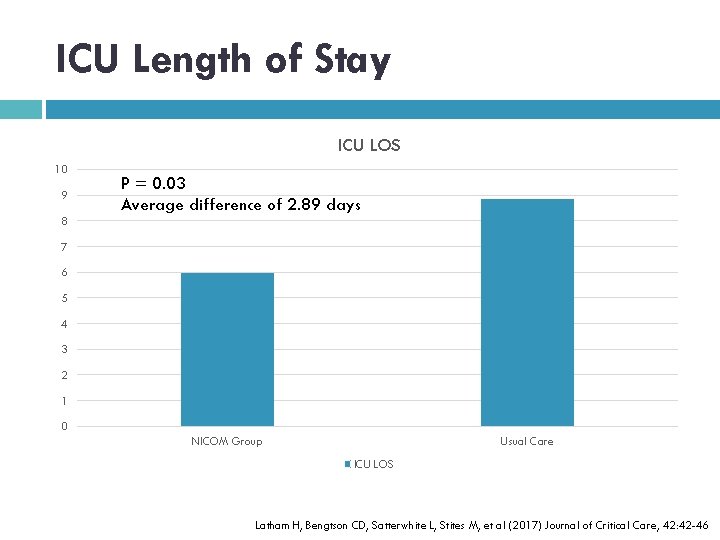
ICU Length of Stay ICU LOS 10 9 P = 0. 03 Average difference of 2. 89 days 8 7 6 5 4 3 2 1 0 NICOM Group Usual Care ICU LOS Latham H, Bengtson CD, Satterwhite L, Stites M, et al (2017) Journal of Critical Care, 42: 42 -46
Need for mechanical ventilation NICOM group less likely to receive mechanical ventilation vs. usual care RR 0. 51 (CI 0. 36 – 0. 72) P = 0. 0001 The chance of being mechanically ventilated was cut in half!!! Latham H, Bengtson CD, Satterwhite L, Stites M, et al (2017) Journal of Critical Care, 42: 42 -46
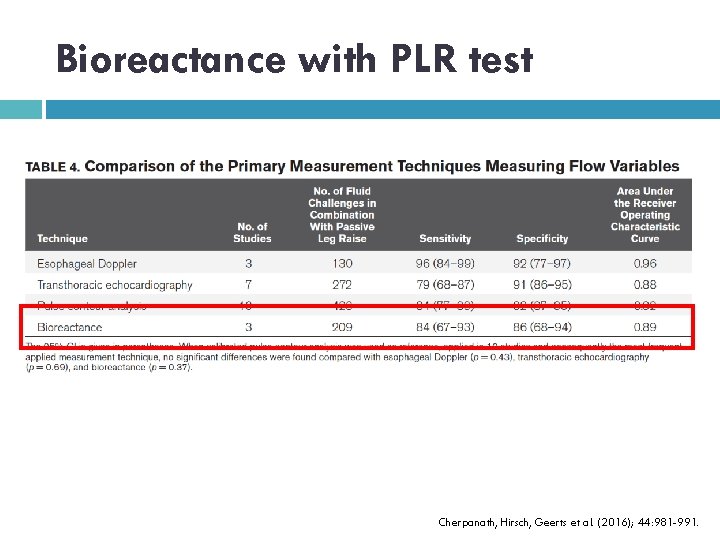
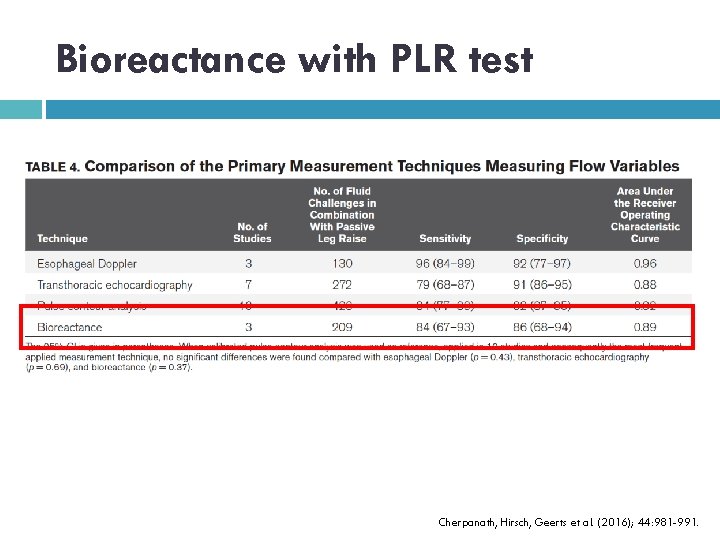
Bioreactance with PLR test Cherpanath, Hirsch, Geerts et al. (2016); 44: 981 -991.
FLUIDS are a DRUG!

Follow me! nkupchik@gmail. com www. nicolekupchikconsulting. com Nicole Kupchik Consulting & Education @nicolekupchik Nicole Kupchik Podcast: Resus 10 (i. Tunes & Stitcher)
In conclusion, FLUIDS are a DRUG!!!! Over resuscitation with fluid is detrimental We need to stop guessing on fluid administration Stroke volume measures can assist in providing optimal fluid resuscitation