Getting Paid Jon HarrisShapiro Nancy Nager Wendy Wright



- Slides: 42
Getting Paid Jon Harris-Shapiro Nancy Nager Wendy Wright Lorraine Bock - Moderator 1
Objectives At the completion of this session the learner will: • Be able to identify the various payors available to contract with, including commercial, government, and private. • Be familiar with the various payment models available to nurse practitioners who operate their own practice. • Discuss future payment models that are outcomes-based, including MIPS and MACRA, and how nurse practitioners can benefit from these types of payment models. • Evaluate the costs and benefits of data capabilities required to participate in outcomes-driven payment models 2
Insurance Credentialing/FFS Nancy Nager
Insurance Credentialing • Definition: Insurance Credentialing (sometimes referred to as “medical credentialing” or “provider enrollment”) is the process of becoming affiliated with an insurance company so that you (the medical provider) can accept third party reimbursement. • Application: The process of getting on insurance panels (if you’re taking a DIY approach) can be both challenging and lengthy. It generally takes between 3 -4 months to submit the necessary paperwork, add supplementary documentation, and correspond with insurance companies’ credentialing departments, before getting approved to join an insurance panel.
Insurance Panels • Filling and Closing: Unfortunately for some, insurance panels are becoming increasingly full, meaning the process of getting on insurance panels is becoming more difficult everyday as insurance companies close provider networks and make the barrier for physicians, counselors or any health professionals higher and more difficult to climb. 5

Top US Based Health Insurers • • • 1. Unitedhealth 2. Kaiser Foundations 3. Wellpoint Inc. 4. Aetna 5. Humana 6. Health Care Service Corporation (HCSC) 7. Cigna 8. Highmark 9. Blue Shield of California 10. Independence Blue Cross Group 6
NPI and CAQH • A National Provider Identifier or NPI is a unique 10 -digit identification number issued to health care providers in the United States by the Centers for Medicare and Medicaid Services (CMS). • Council for Affordable Quality Healthcare. It is essentially an online database that stores provider information. This information is granted to health insurance companies to make acquiring provider information more efficient. 7
Fee for Service • Fee-for-service (FFS) is a payment model where services are unbundled and paid for separately. In health care, it gives an incentive for physicians to provide more treatments because payment is dependent on the quantity of care, rather than quality of care. • It includes tests, procedure, visits or other health care services • Payments are issued only after the services are provided
FFS and Health Care Costs • If bills are paid under FFS by a third party, patients (along with doctors) have no incentive to consider the cost of treatment • Declining reimbursement and regulatory changes are increasing costs and decreasing revenue • What to do: While most practices have succumbed to the need to see more patients and increase FFS procedures to maintain revenue, more physicians are looking to alternate practice models as a better solution. In addition to value-based reimbursement models, such as pay-forperformance programs and accountable care organizations, there is a resurgence of interest in concierge and direct-pay practice models. When patients have greater access to their physicians and physicians have more time to spend with patients, utilization of services such as imaging and testing declines thus helping physicians to reduce costs. .
Preparing for Payment Reform: Sustainability in NP Owned or Managed Clinics Wendy L. Wright, MS, RN, APRN, FNP, FAAN Wright, 2016 10
My NP Owned Clinics From 7 patients in 2007 to 5000 patients in 2016 Wright, 2016 11
Nurse-Owned or Managed Clinics • Unique position • Compete with other MD or Hospital Owned practices • Bring something different to market place • Must still be sustainable • NPs see 10 -12 patients per day – Comprehensive care model – Telehealth division – Long-term care facility/home care division Wright, 2016 12

Ah-h different kind of care Nurse practitioners are partners with their patients By Kathleen Baglio Humphreys and Susan Lunt Childress Front page article Cabinet Press Amherst, New Hampshire Photo by Kathleen Baglio Humphreys Nurse practitioner Wendy Wright shows Benjamin Egan, 3, of Manchester how to ‘open wide. ’ Wright is co-owner of Wright & Associates Family Healthcare, a new nurse-only practice. Wright, 2016 13
Challenges Continue to Face Our Profession Wright, 2016 14
The Future: Wright, 2016 15
We are working to modify ACO language Wright, 2016 16
Background • Patient Protection & Affordable Care Act signed March 30, 2010 (Affordable Care Act) • Section 3022 required Secretary to: – Establish the Medicare Shared Savings Program – Intended to encourage the development of ACO’s within Medicare – Purpose of cost-savings and quality care delivery while avoiding duplication of services http: //www. aanp. org/images/documents/federal-legislation/Final%20 Rule. ACO. pdf accessed 08 -30 -2014 Wright, 2016 17
What Have We Done in New Hampshire? Wright, 2016 18
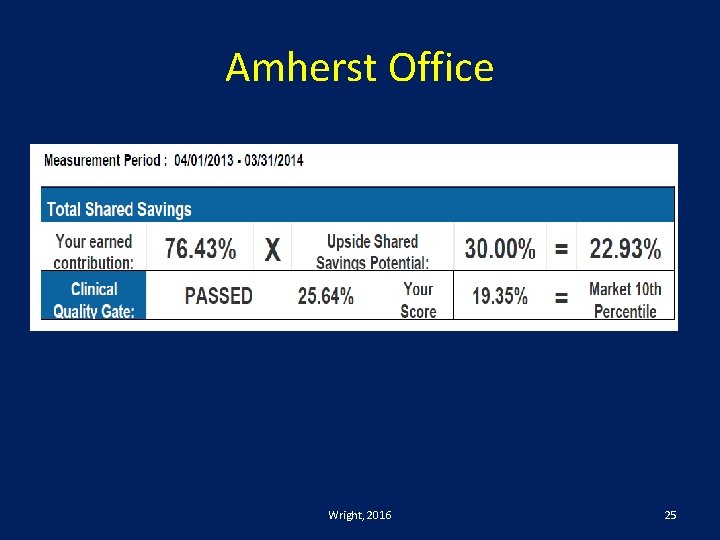
Anthem Patient Shared Savings • Patient Centered Primary Care Program started January 2013 • There are financial incentives within this program: – 1. There is a per member per month fee paid to office based on the collective severity of illness of patients – 2. There is an incentive based on shared savings of cost which is calculated at the end of each year. This incentive is calculated by those practitioners working in a combined risk pool. The larger the risk pool the lower the risk become when there is a catastrophic risk Wright, 2016 19
Sean Lyon APRN • Needs to be given credit for the foresight…. . • He was at the table/on panel • Asked for APRN’s who own their own practice to be grouped together for aggregate data collection • And…. it began what will hopefully be some amazing information about APRNs and our participation in ACO’s Wright, 2016 20
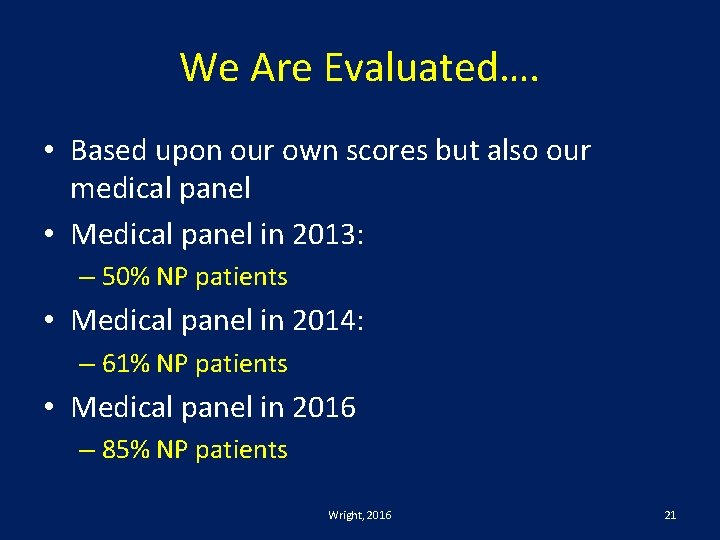
We Are Evaluated…. • Based upon our own scores but also our medical panel • Medical panel in 2013: – 50% NP patients • Medical panel in 2014: – 61% NP patients • Medical panel in 2016 – 85% NP patients Wright, 2016 21
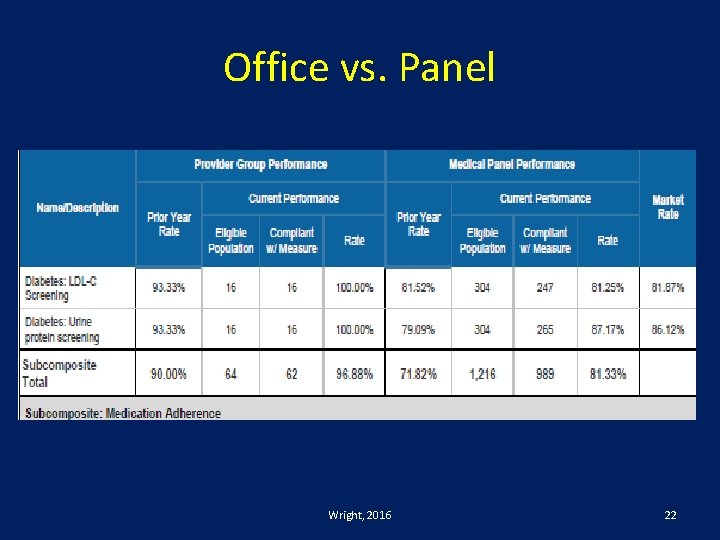
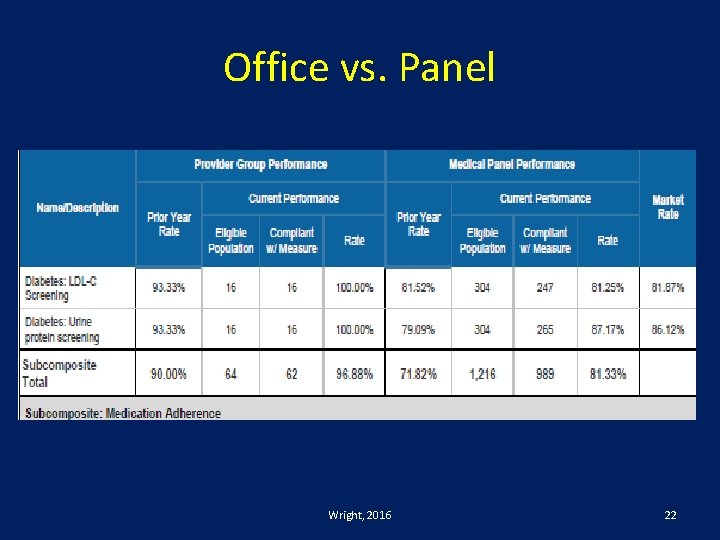
Office vs. Panel Wright, 2016 22
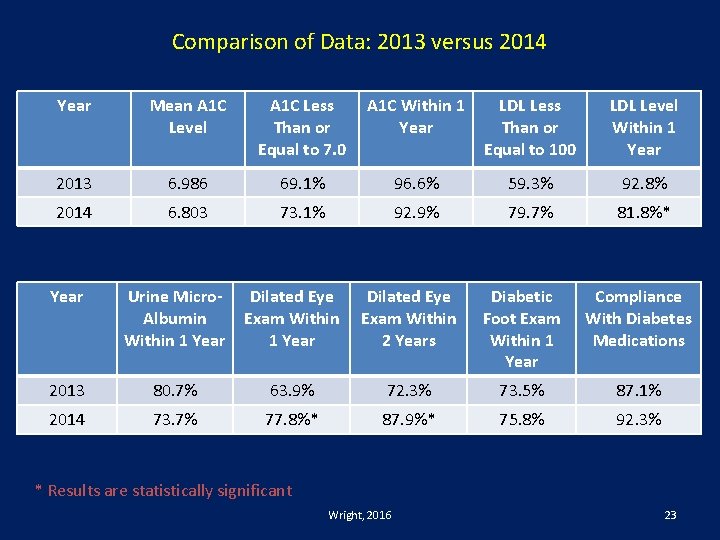
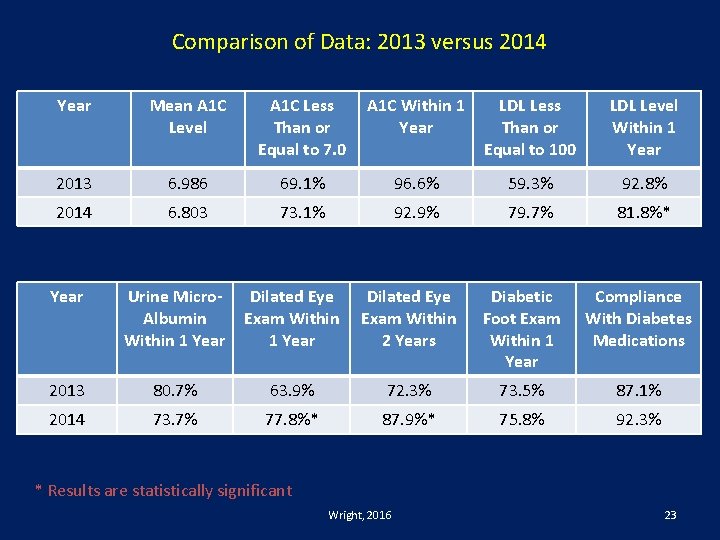
Comparison of Data: 2013 versus 2014 Year Mean A 1 C Level A 1 C Less Than or Equal to 7. 0 A 1 C Within 1 Year LDL Less Than or Equal to 100 LDL Level Within 1 Year 2013 6. 986 69. 1% 96. 6% 59. 3% 92. 8% 2014 6. 803 73. 1% 92. 9% 79. 7% 81. 8%* Year Urine Micro. Albumin Within 1 Year Dilated Eye Exam Within 2 Years Diabetic Foot Exam Within 1 Year Compliance With Diabetes Medications 2013 80. 7% 63. 9% 72. 3% 73. 5% 87. 1% 2014 73. 7% 77. 8%* 87. 9%* 75. 8% 92. 3% * Results are statistically significant Wright, 2016 23
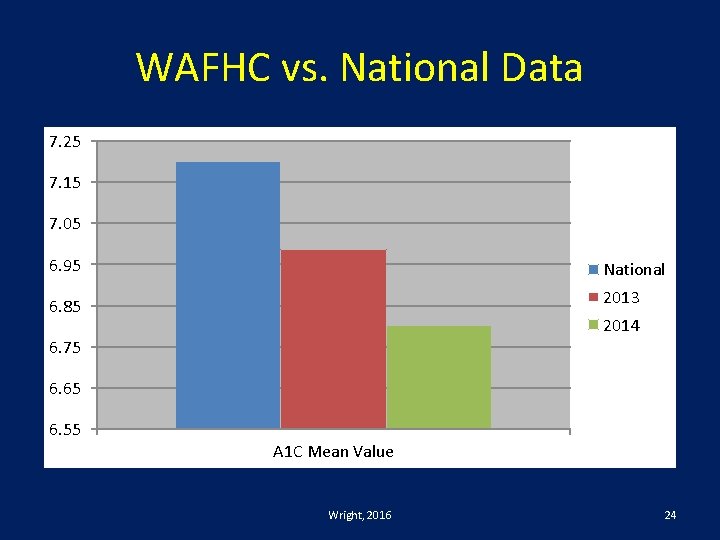
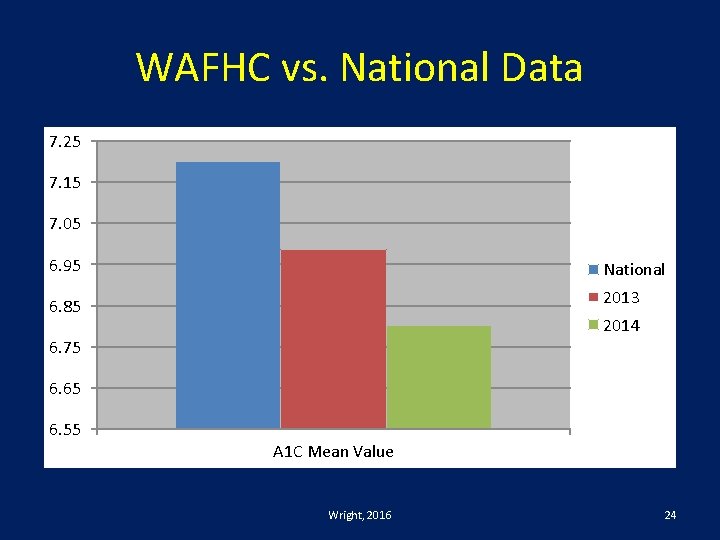
WAFHC vs. National Data 7. 25 7. 15 7. 05 6. 95 National 6. 85 2013 2014 6. 75 6. 65 6. 55 A 1 C Mean Value Wright, 2016 24
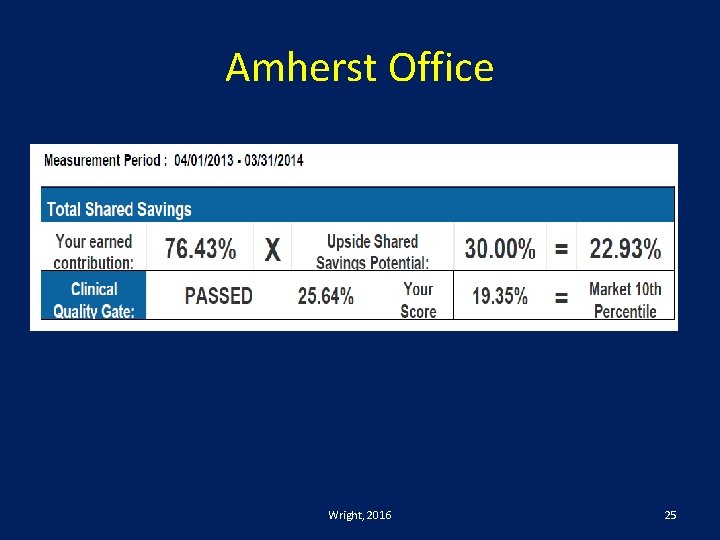
Amherst Office Wright, 2016 25
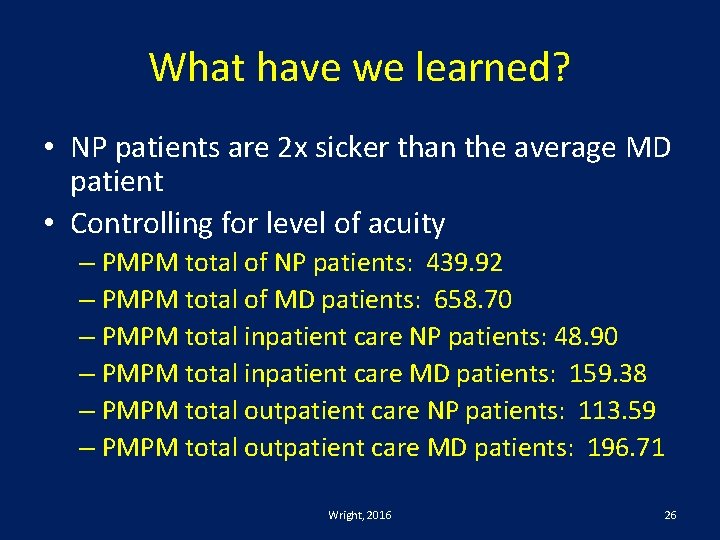
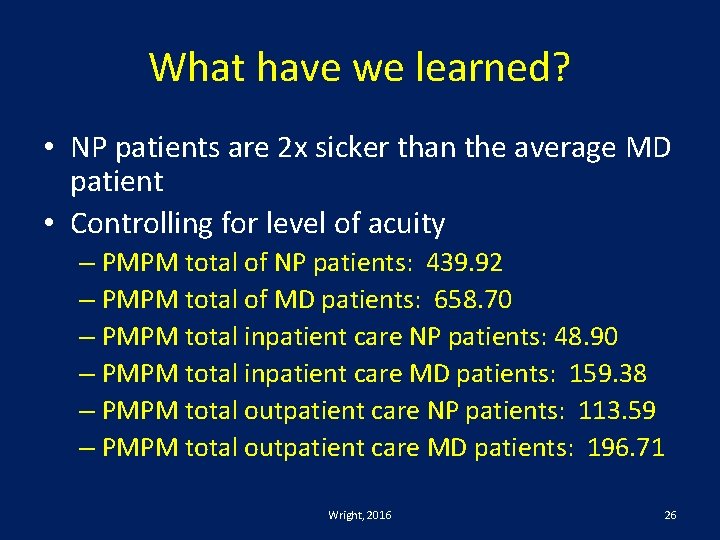
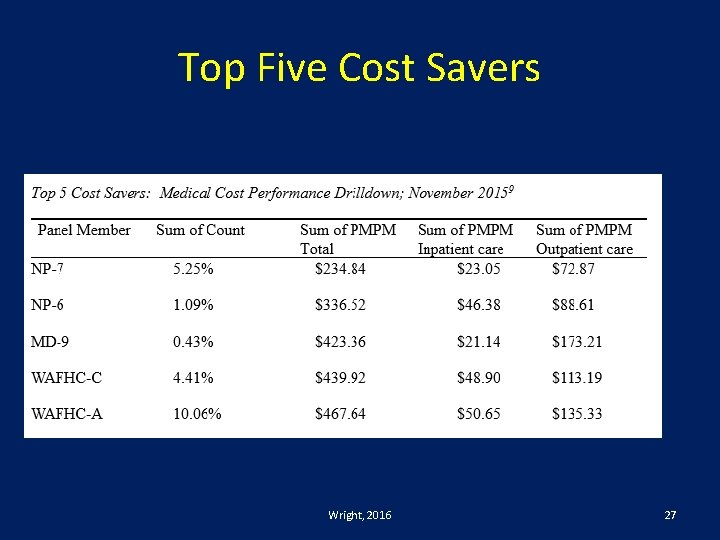
What have we learned? • NP patients are 2 x sicker than the average MD patient • Controlling for level of acuity – PMPM total of NP patients: 439. 92 – PMPM total of MD patients: 658. 70 – PMPM total inpatient care NP patients: 48. 90 – PMPM total inpatient care MD patients: 159. 38 – PMPM total outpatient care NP patients: 113. 59 – PMPM total outpatient care MD patients: 196. 71 Wright, 2016 26
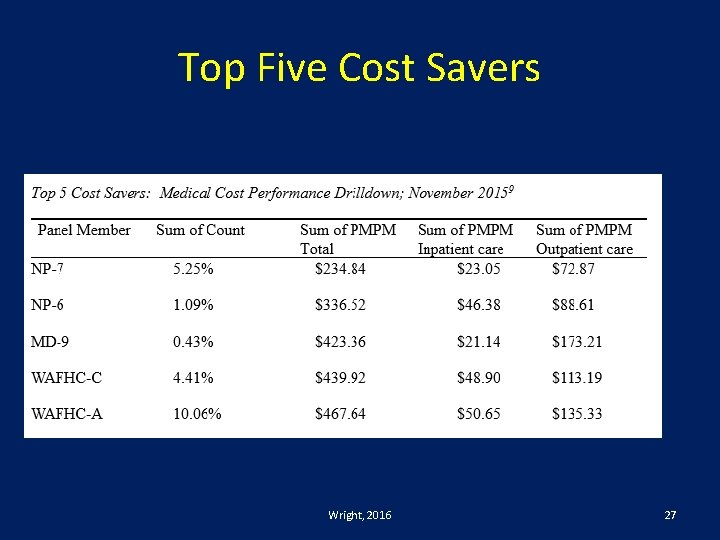
Top Five Cost Savers Wright, 2016 27
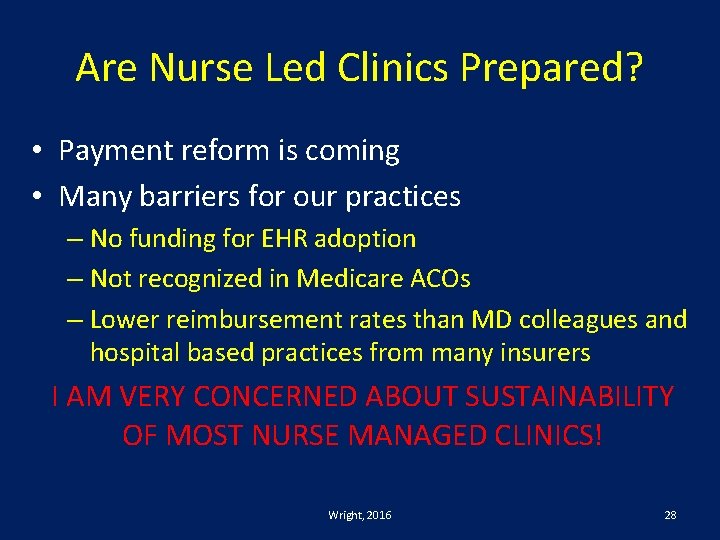
Are Nurse Led Clinics Prepared? • Payment reform is coming • Many barriers for our practices – No funding for EHR adoption – Not recognized in Medicare ACOs – Lower reimbursement rates than MD colleagues and hospital based practices from many insurers I AM VERY CONCERNED ABOUT SUSTAINABILITY OF MOST NURSE MANAGED CLINICS! Wright, 2016 28

Complacency is not an option! Wright, 2016 29
Are you prepared for payment reform? Wright, 2017 30
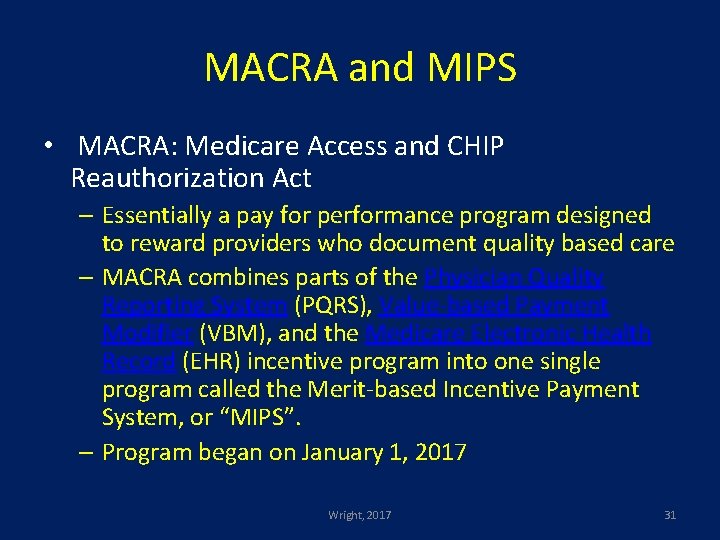
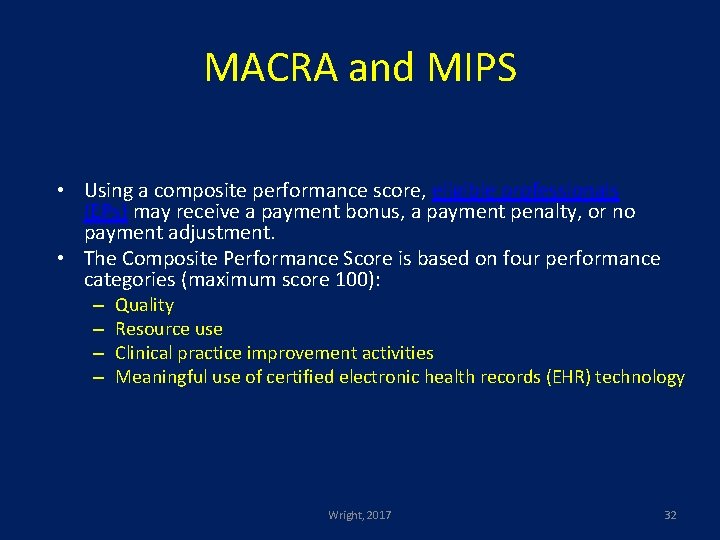
MACRA and MIPS • MACRA: Medicare Access and CHIP Reauthorization Act – Essentially a pay for performance program designed to reward providers who document quality based care – MACRA combines parts of the Physician Quality Reporting System (PQRS), Value-based Payment Modifier (VBM), and the Medicare Electronic Health Record (EHR) incentive program into one single program called the Merit-based Incentive Payment System, or “MIPS”. – Program began on January 1, 2017 Wright, 2017 31
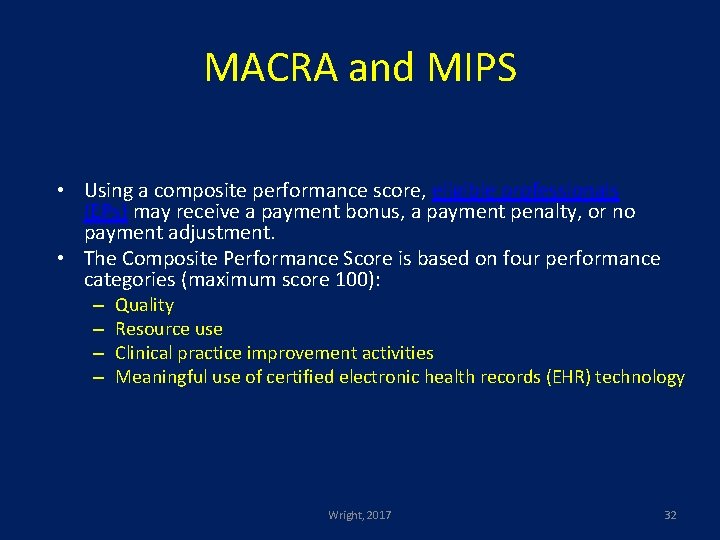
MACRA and MIPS • Using a composite performance score, eligible professionals (EPs) may receive a payment bonus, a payment penalty, or no payment adjustment. • The Composite Performance Score is based on four performance categories (maximum score 100): – – Quality Resource use Clinical practice improvement activities Meaningful use of certified electronic health records (EHR) technology Wright, 2017 32
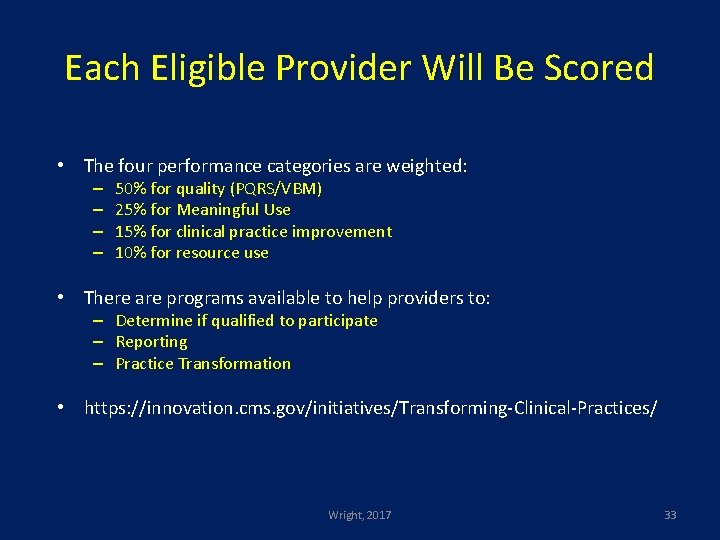
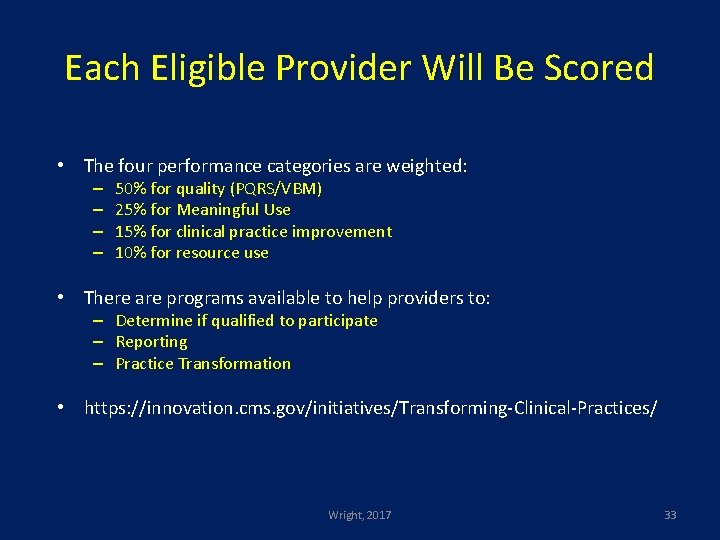
Each Eligible Provider Will Be Scored • The four performance categories are weighted: – – 50% for quality (PQRS/VBM) 25% for Meaningful Use 15% for clinical practice improvement 10% for resource use • There are programs available to help providers to: – Determine if qualified to participate – Reporting – Practice Transformation • https: //innovation. cms. gov/initiatives/Transforming-Clinical-Practices/ Wright, 2017 33
Outcomes Based Payment & Data Collection: Building the Infrastructure Jon Harris-Shapiro 34
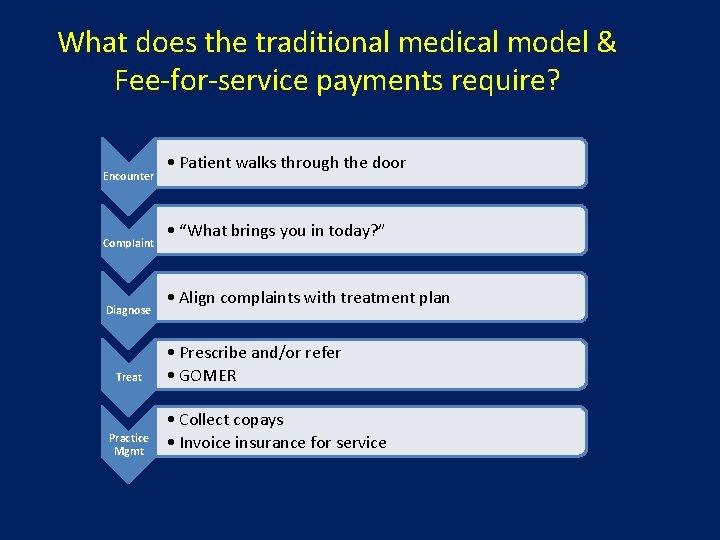
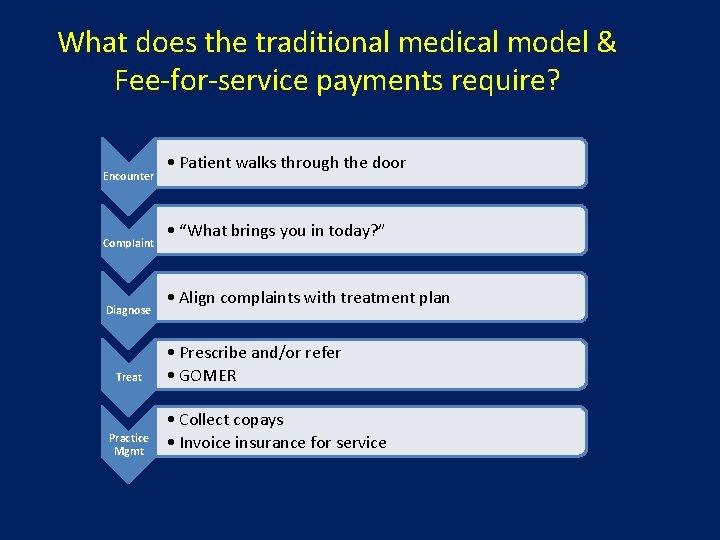
What does the traditional medical model & Fee-for-service payments require? Encounter Complaint Diagnose Treat Practice Mgmt • Patient walks through the door • “What brings you in today? ” • Align complaints with treatment plan • Prescribe and/or refer • GOMER • Collect copays • Invoice insurance for service
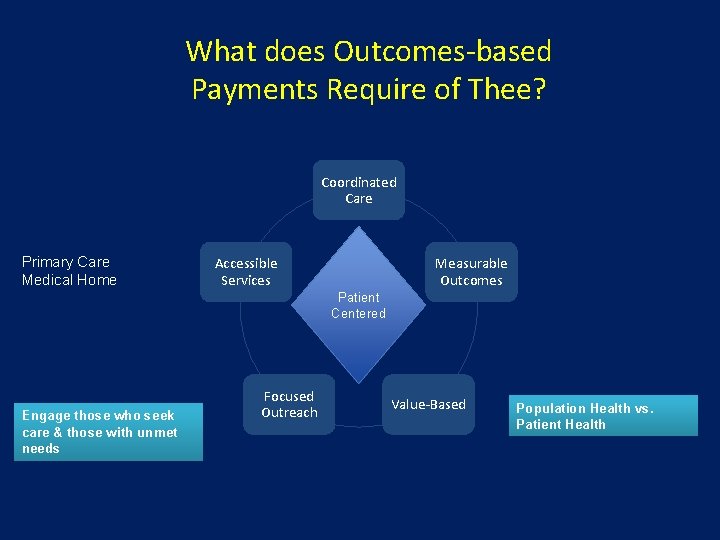
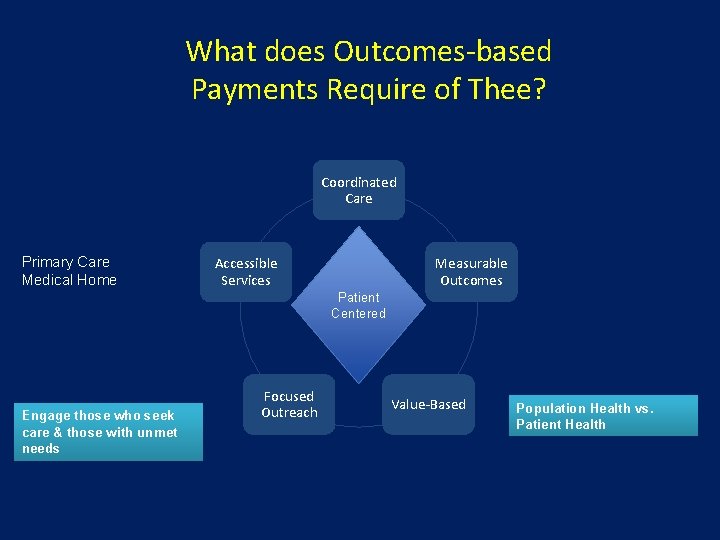
What does Outcomes-based Payments Require of Thee? Coordinated Care Primary Care Medical Home Accessible Services Measurable Outcomes Patient Centered Engage those who seek care & those with unmet needs Focused Outreach Value-Based Population Health vs. Patient Health
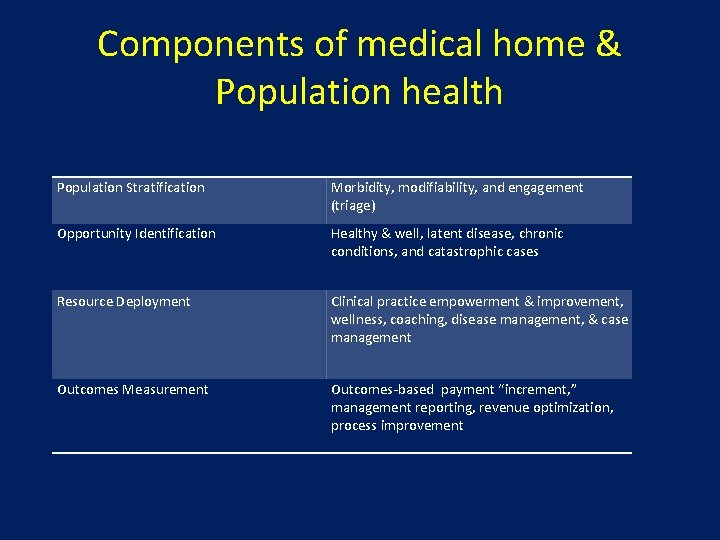
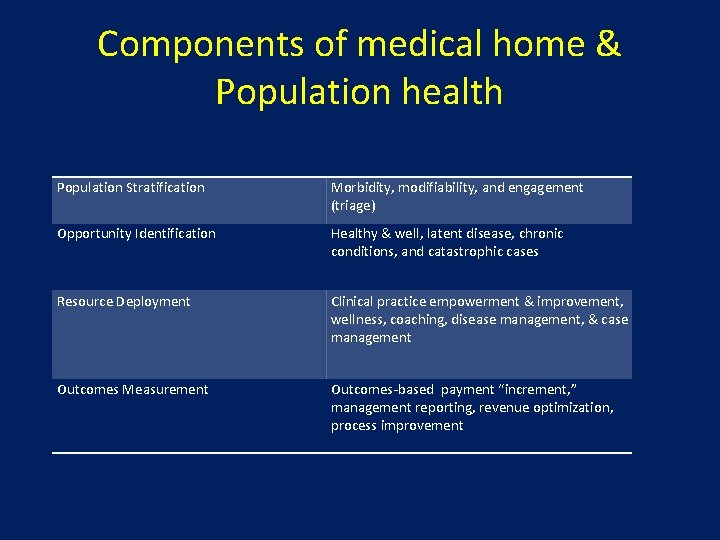
Components of medical home & Population health Population Stratification Morbidity, modifiability, and engagement (triage) Opportunity Identification Healthy & well, latent disease, chronic conditions, and catastrophic cases Resource Deployment Clinical practice empowerment & improvement, wellness, coaching, disease management, & case management Outcomes Measurement Outcomes-based payment “increment, ” management reporting, revenue optimization, process improvement
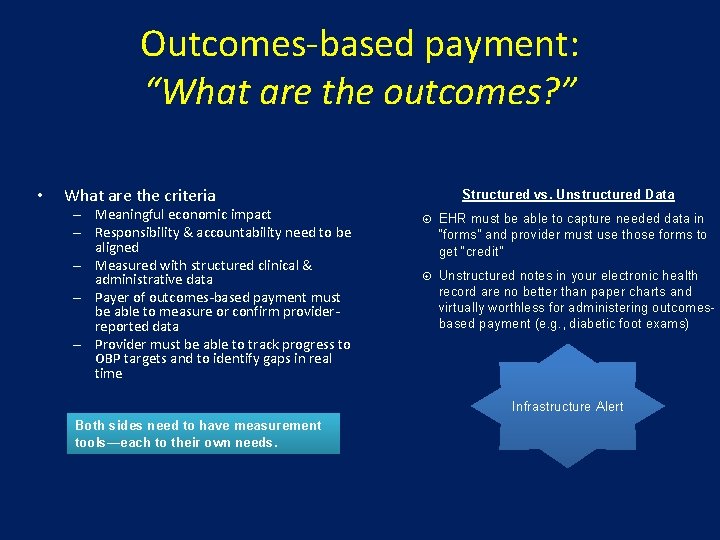
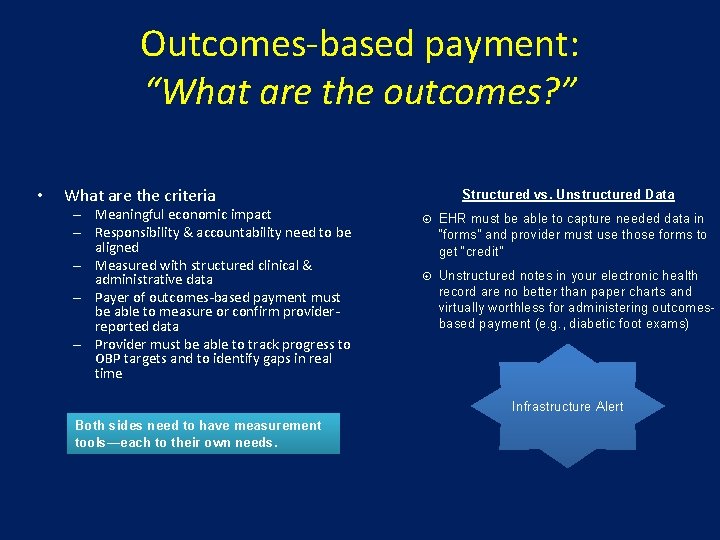
Outcomes-based payment: “What are the outcomes? ” • What are the criteria – Meaningful economic impact – Responsibility & accountability need to be aligned – Measured with structured clinical & administrative data – Payer of outcomes-based payment must be able to measure or confirm providerreported data – Provider must be able to track progress to OBP targets and to identify gaps in real time Structured vs. Unstructured Data EHR must be able to capture needed data in “forms” and provider must use those forms to get “credit” Unstructured notes in your electronic health record are no better than paper charts and virtually worthless for administering outcomesbased payment (e. g. , diabetic foot exams) Infrastructure Alert Both sides need to have measurement tools—each to their own needs.
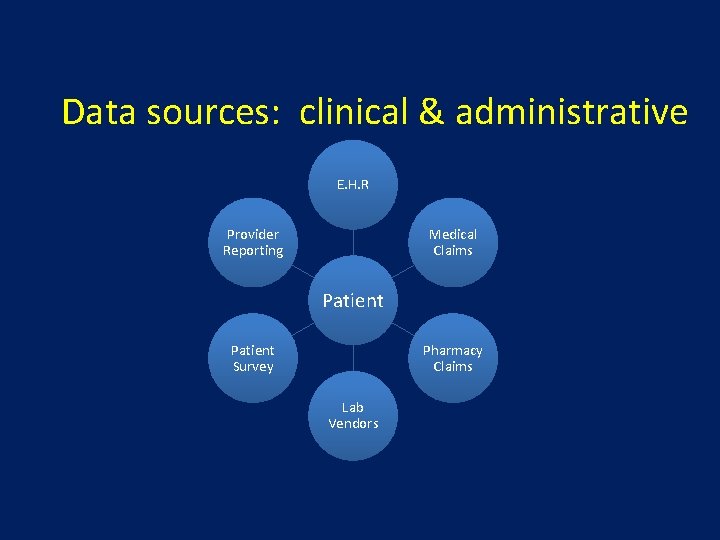
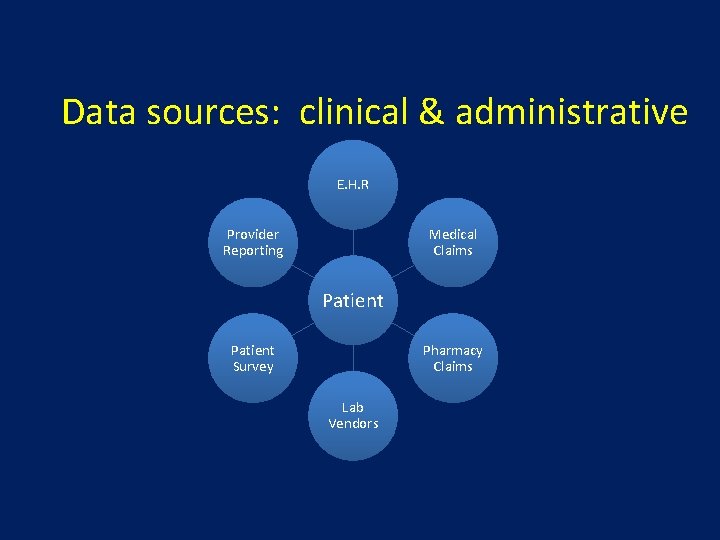
Data sources: clinical & administrative E. H. R Provider Reporting Medical Claims Patient Survey Pharmacy Claims Lab Vendors
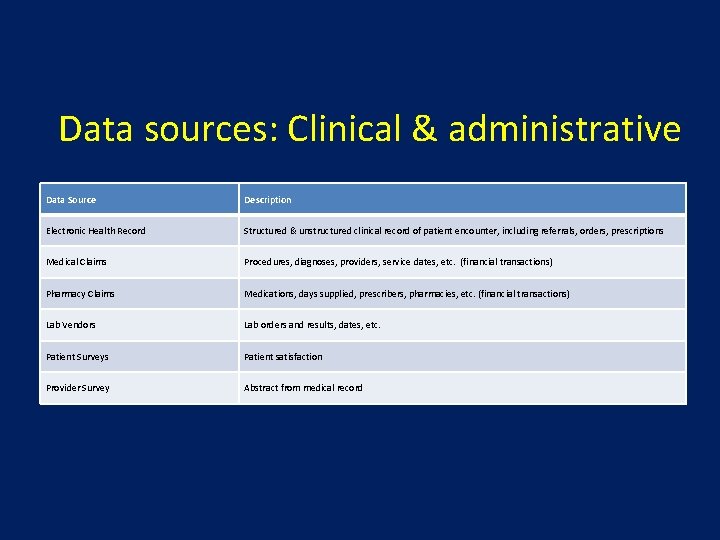
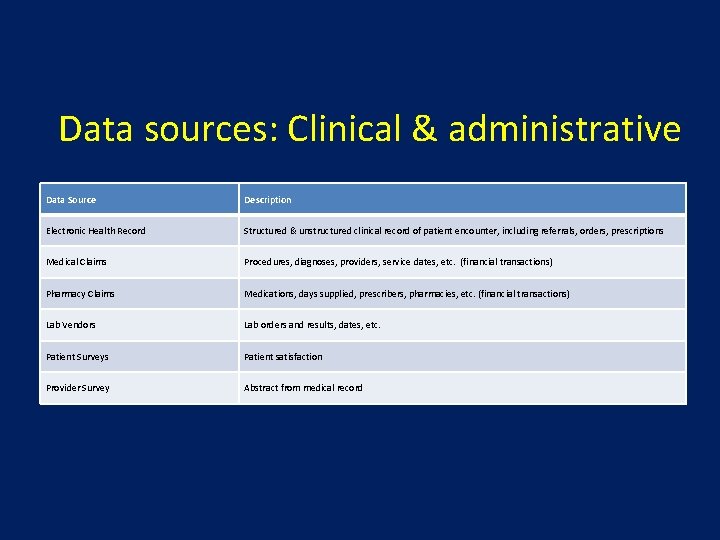
Data sources: Clinical & administrative Data Source Description Electronic Health Record Structured & unstructured clinical record of patient encounter, including referrals, orders, prescriptions Medical Claims Procedures, diagnoses, providers, service dates, etc. (financial transactions) Pharmacy Claims Medications, days supplied, prescribers, pharmacies, etc. (financial transactions) Lab Vendors Lab orders and results, dates, etc. Patient Surveys Patient satisfaction Provider Survey Abstract from medical record
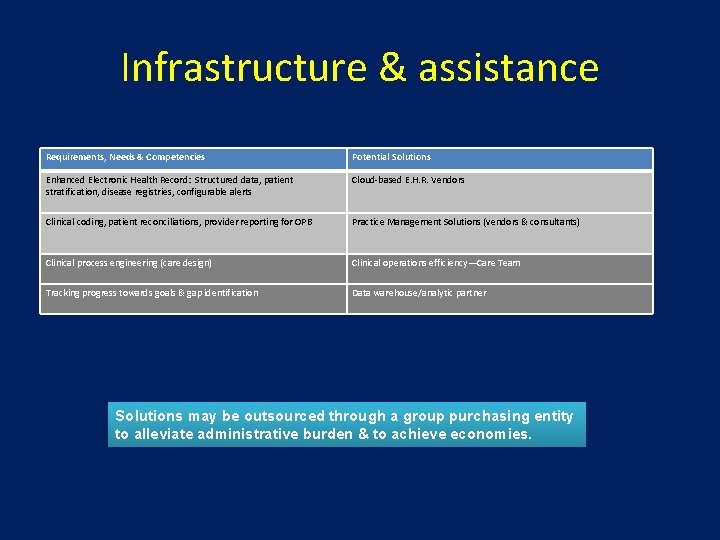
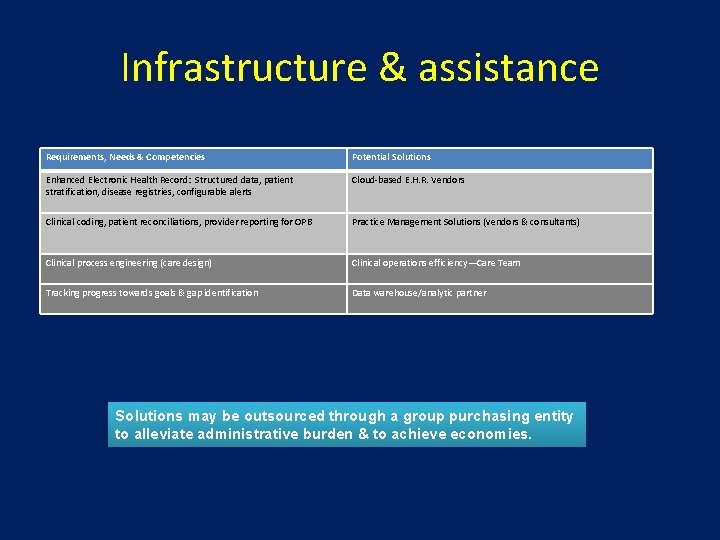
Infrastructure & assistance Requirements, Needs & Competencies Potential Solutions Enhanced Electronic Health Record: Structured data, patient stratification, disease registries, configurable alerts Cloud-based E. H. R. Vendors Clinical coding, patient reconciliations, provider reporting for OPB Practice Management Solutions (vendors & consultants) Clinical process engineering (care design) Clinical operations efficiency—Care Team Tracking progress towards goals & gap identification Data warehouse/analytic partner Solutions may be outsourced through a group purchasing entity to alleviate administrative burden & to achieve economies.
Discussion/Questions • Lorraine Bock – lorrainecrnp@gmail. com – Mobile: 717. 443. 9970 • Jon Harris-Shapiro – jhs@continuancehealthsolutions. com – Direct: 215. 782. 8551 – Office: 908. 781. 7400 – Mobile: 215. 485. 2159 • Nancy Nager – nnager@sbscincorporated. com – Mobile: 617. 332. 4411 • Wendy Wright – wendyarnp@aol. com – Mobile: 603. 490. 0154 42