Getting Knowledge into Action to Support People with

- Slides: 16
Getting Knowledge into Action to Support People with Multiple Conditions Ann. wales@nes. scot. nhs. uk
Knowledge into Action 1. What is Knowledge into Action? 2. Why is it important? 3. What does it involve? 4. How could it help to support people with multiple conditions?
Knowledge-Practice Gap Around 45% of patients do not receive care as recommended in the published evidence. It can take 17 years for published research to become routine practice. AHRQ, 2008 NHS Atlas of Variation – Diabetes 2012.
Knowledge into Action Review What do we need to do differently to get knowledge into routine delivery of care?
Knowledge into Action: New Approaches Key messages: 1. Knowledge comes in many forms. 2. Knowledge is a dynamic process not a product. 3. The evidence highlights several methods that can help to translate knowledge into practice. 4. To achieve change, knowledge needs to be embedded in day to day practice and day to day life.
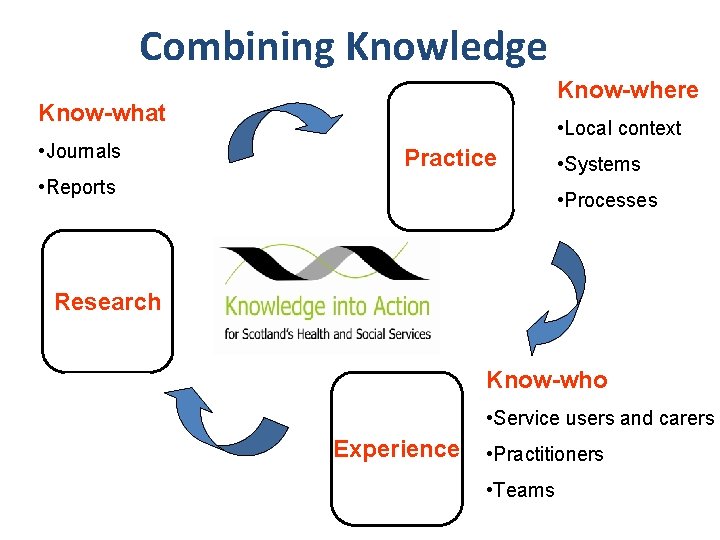
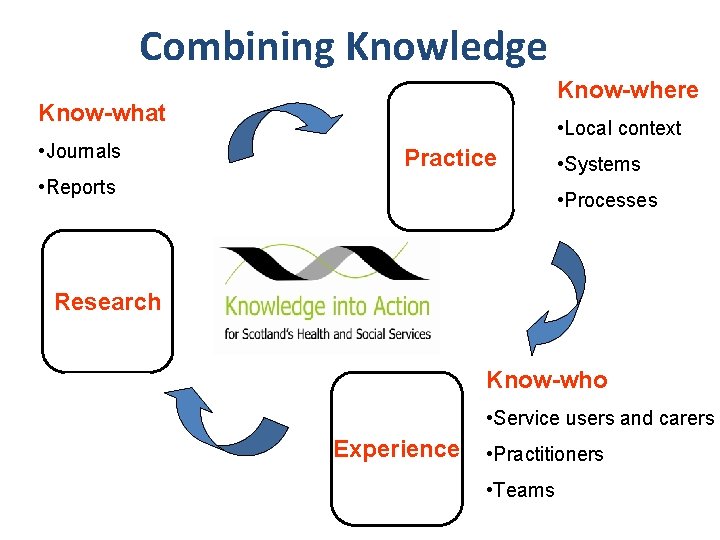
Combining Knowledge Know-where Know-what • Journals • Local context Practice • Reports • Systems • Processes Research Know-who • Service users and carers Experience • Practitioners • Teams
Bridging the Knowledge-Practice Gap
1. Helping people to get personal meaning from health information – “health literacy. ”

2. Sharing experience – e. g. through communities of practice, social networking, support groups.
3. Presenting knowledge in ways that make it quick and easy to use in day to day work and life – e. g. prompts and reminders, mobile apps, pathways, decision aids, visual summaries.
4. Embed all these approaches in day to day practice, individual and community life.
Today’s Question How can these Knowledge into Action approaches support people with multiple conditions?
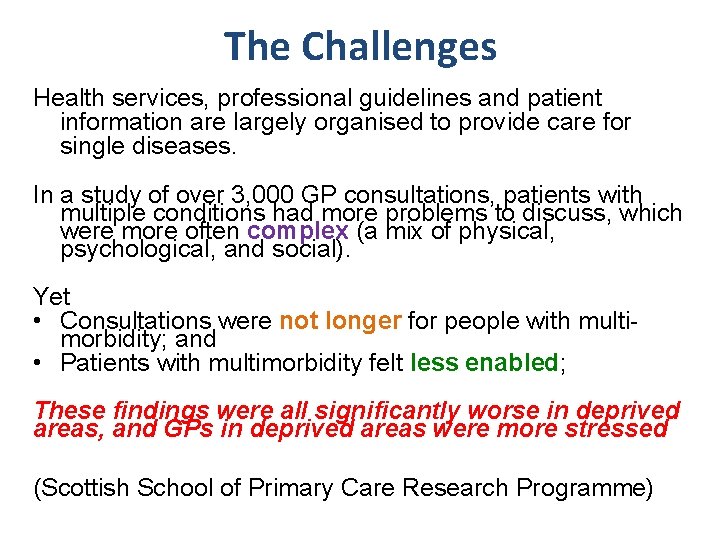
The Challenges Health services, professional guidelines and patient information are largely organised to provide care for single diseases. In a study of over 3, 000 GP consultations, patients with multiple conditions had more problems to discuss, which were more often complex (a mix of physical, psychological, and social). Yet • Consultations were not longer for people with multimorbidity; and • Patients with multimorbidity felt less enabled; These findings were all significantly worse in deprived areas, and GPs in deprived areas were more stressed (Scottish School of Primary Care Research Programme)
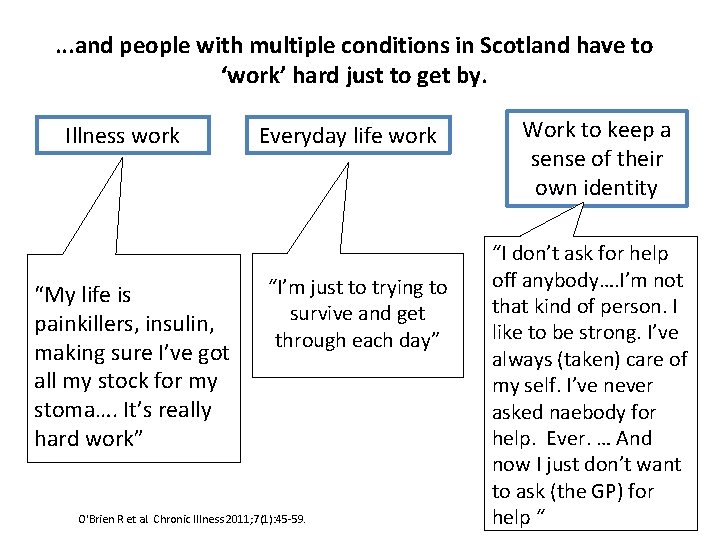
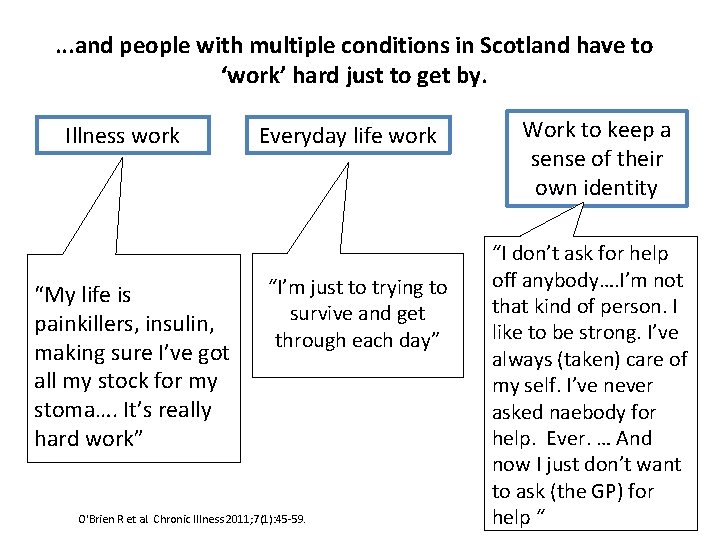
. . . and people with multiple conditions in Scotland have to ‘work’ hard just to get by. Illness work “My life is painkillers, insulin, making sure I’ve got all my stock for my stoma…. It’s really hard work” Everyday life work “I’m just to trying to survive and get through each day” O'Brien R et al. Chronic Illness 2011; 7(1): 45 -59. Work to keep a sense of their own identity “I don’t ask for help off anybody…. I’m not that kind of person. I like to be strong. I’ve always (taken) care of my self. I’ve never asked naebody for help. Ever. … And now I just don’t want to ask (the GP) for help “
Possibilities…. • Enabling people to take more control through understanding and sharing knowledge. • Triggers and prompts for professionals at key points in guidelines and pathways. • Coordinating and connecting community information sources.
Getting Knowledge into Action to Support People with Multiple Conditions Ann. wales@nes. scot. nhs. uk