Gestational Trophoblastic Neoplasia GTN Prof Gamze Mocan Kuzey
Gestational Trophoblastic Neoplasia (GTN) Prof. Gamze Mocan Kuzey M. D. Near East University Faculty of Medicine Department of Pathology

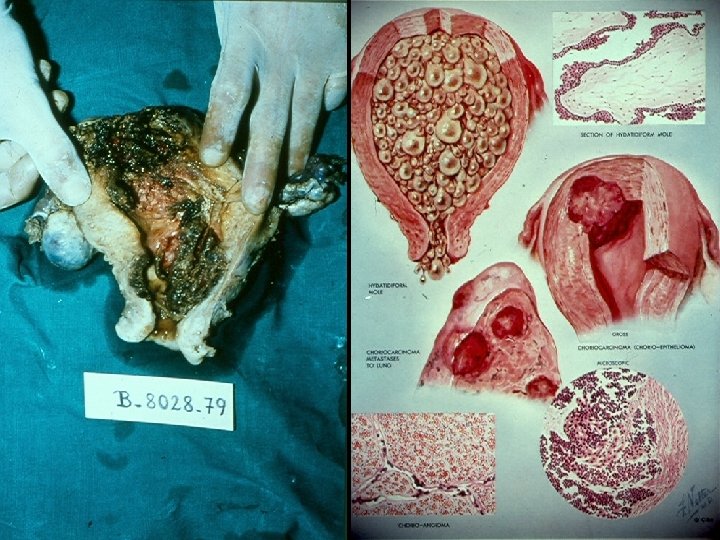
Gestational Trophoblastic Neoplasia (GTN) Ø n n Proliferation of pregnancy-associated trophoblastic tissue of progressive malignant potential Benign hydatiform mole Invasive mole (chorioadenoma destruens) Placental site trophoblastic tumor (PSTT) Choriocarcinoma

GTN n n n Pathogenesis geographic distribution, dietary, genetic components An accentuation of the hydropic swelling encountered in a blighted ovum (Hertig&Mansell) Cytogenetic studies of moles Ø 90% have 46 XX diploid patterns

GTN n Androgenesis : chromosome banding patterns of cells from molar tissues and parents strongly suggest that the entire chromosome complement of the mole comes from the SPERM n n n 80% of moles → BENIGN 20% of moles → further complications ( + invasive mole) 2 -3% of moles → choriocarcinoma
Importance of GTN n n Benign mole – common complication of gestation, one in every 2000 pregnancies Monitoring the circulating levels of HCG n n Determination of the early development of the more malignant forms Once a dreaded and fatal complication n Choriocarcinoma – highly responsive to chemotherapy
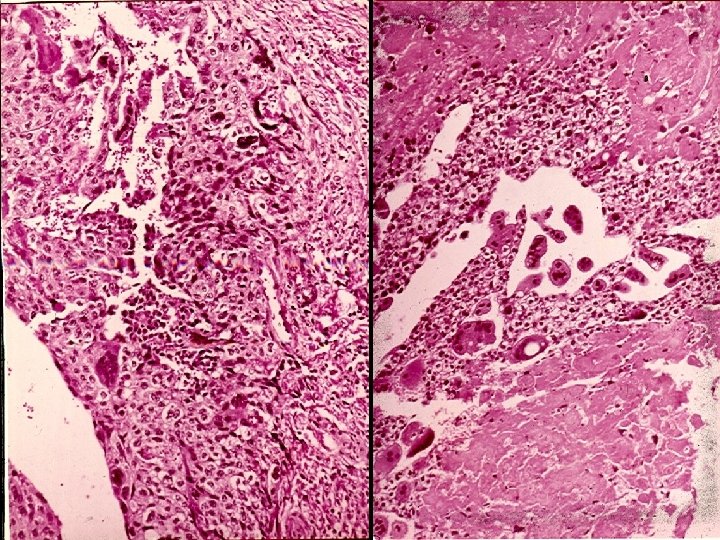
Mole Hydatiform n n Hydropic swelling of chorionic villi Absence or inadequate development of vascularization of villi Variable degrees of hyperplasia and anaplasia of the chorionic epithelium Thin layer of chorionic epithelium n n Cytotrophoblast Syncytial trophoblast
Incomplete mole (Partial Mole) n n n n Diffuse & massive villous edema (in some villi) No trophoblastic proliferation Focal slight trophoblastic proliferation Fetus is present or in specimens from Spontaneous abortions amnion is present Triploid karyotype Rarely followed by choriocarcinoma Absence of atypia HCG staining in tissue is weak



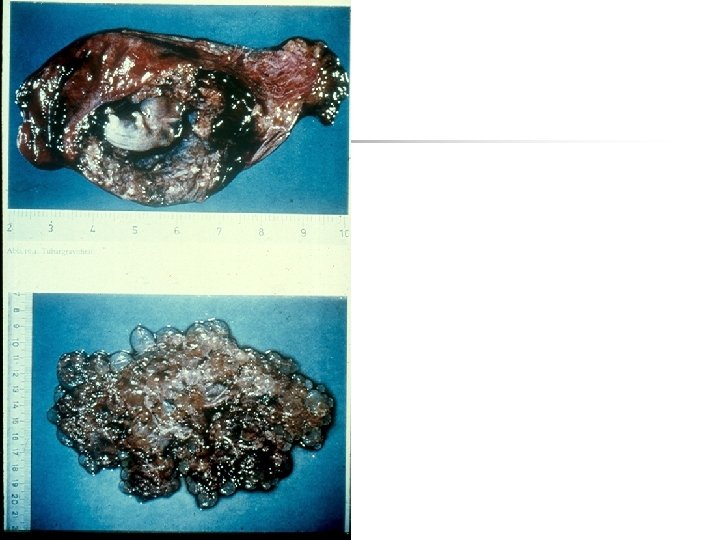
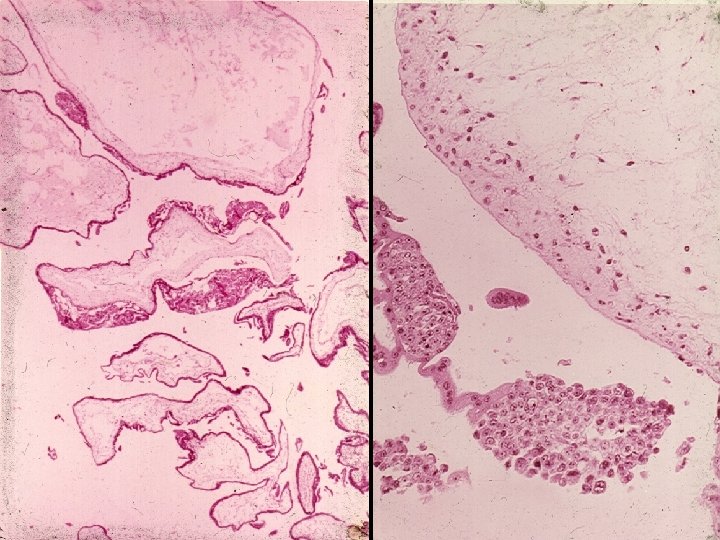

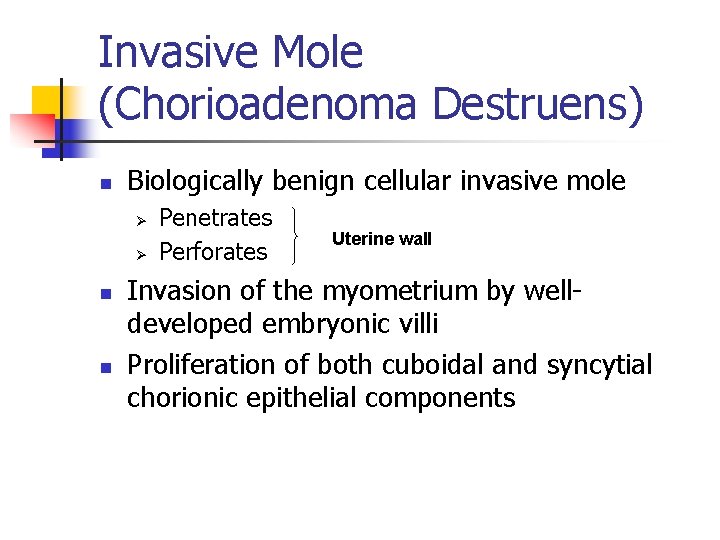
Invasive Mole (Chorioadenoma Destruens) n Biologically benign cellular invasive mole Ø Ø n n Penetrates Perforates Uterine wall Invasion of the myometrium by welldeveloped embryonic villi Proliferation of both cuboidal and syncytial chorionic epithelial components
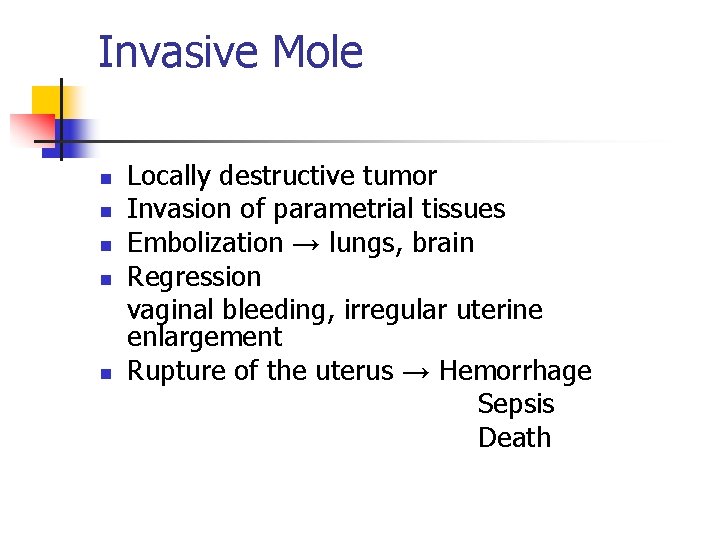
Invasive Mole n n n Locally destructive tumor Invasion of parametrial tissues Embolization → lungs, brain Regression vaginal bleeding, irregular uterine enlargement Rupture of the uterus → Hemorrhage Sepsis Death


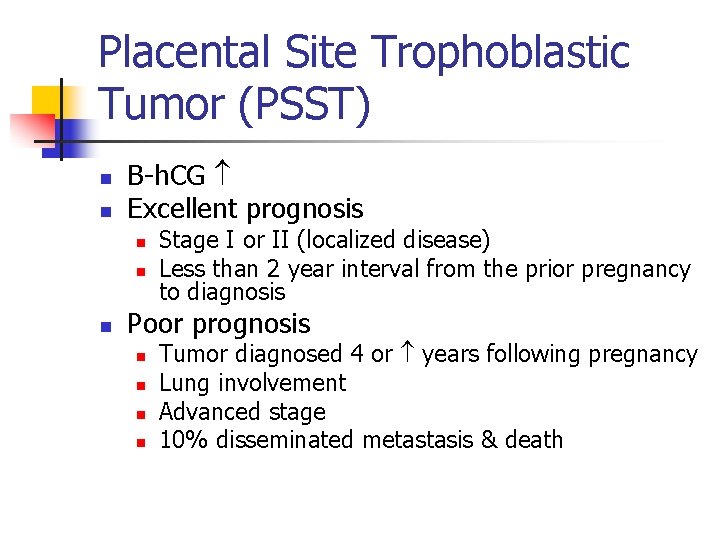
Placental Site Trophoblastic Tumor (PSST) n n Β-h. CG Excellent prognosis n n n Stage I or II (localized disease) Less than 2 year interval from the prior pregnancy to diagnosis Poor prognosis n n Tumor diagnosed 4 or years following pregnancy Lung involvement Advanced stage 10% disseminated metastasis & death
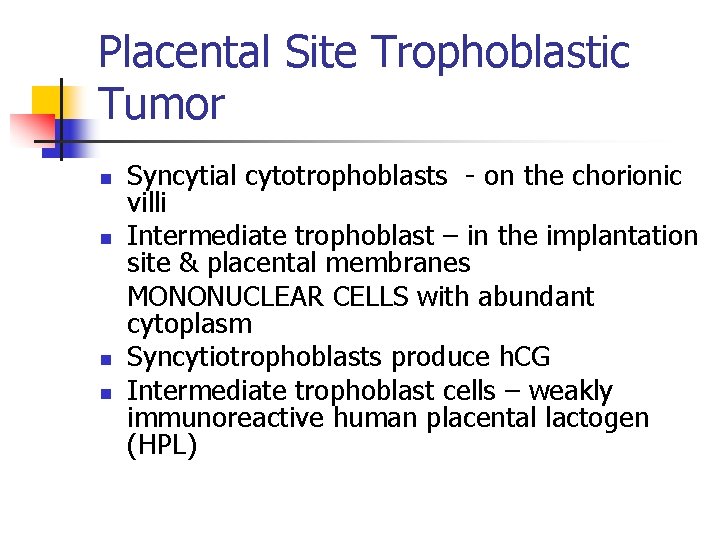
Placental Site Trophoblastic Tumor n n Syncytial cytotrophoblasts - on the chorionic villi Intermediate trophoblast – in the implantation site & placental membranes MONONUCLEAR CELLS with abundant cytoplasm Syncytiotrophoblasts produce h. CG Intermediate trophoblast cells – weakly immunoreactive human placental lactogen (HPL)
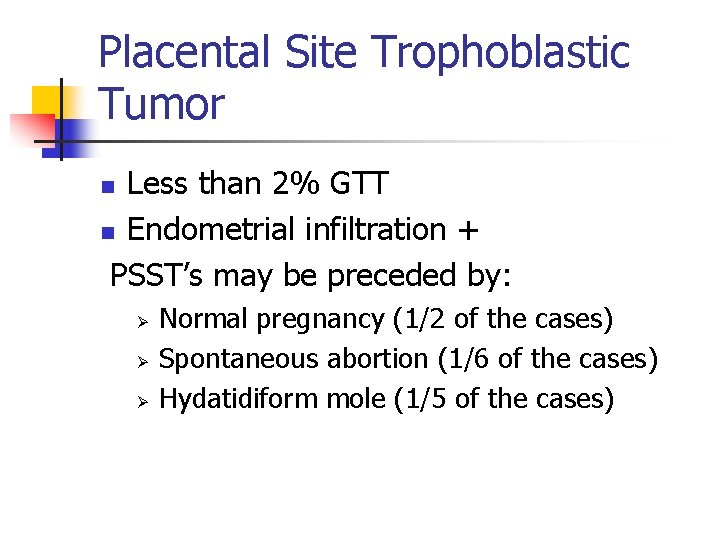
Placental Site Trophoblastic Tumor Less than 2% GTT n Endometrial infiltration + PSST’s may be preceded by: n Ø Ø Ø Normal pregnancy (1/2 of the cases) Spontaneous abortion (1/6 of the cases) Hydatidiform mole (1/5 of the cases)
Placental Site Trophoblastic Tumor n Intermediate trophoblasts compose the placental site trophoblasts & residual plasental site (implantation site nodule) following pregnancy → may give rise to PSTT’s
Differential diagnosis Ø n n Normal exaggerated placental implantation site trophoblasts Mel-Cam Ki-67 Biomarkers that detect trophoblastic cell proliferation
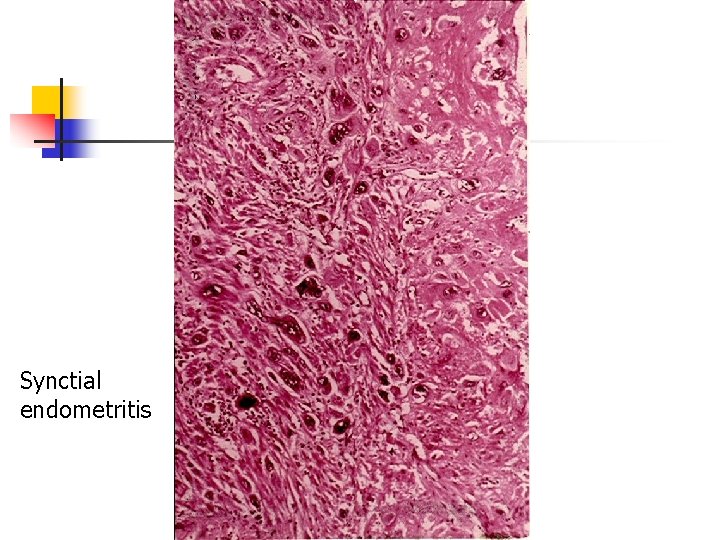
Synctial endometritis
Choriocarcinoma n Uncommon condition n n n 1/20, 000 – 30, 000 pregnancies in USA 1/2500 pregnancies in Asian & African countries 50% arise in hydatiform moles 25% arise in previous abortions 22% arise in normal pregnancies The rest in ectopic pregnancies, genital and extragenital teratomas Ø Occurence in males
Choriocarcinoma n n n Epithelial malignancy of trophoblastic cells Derived from any form of previous normal or abnormal pregnancy Most cases arise in the uterus Ectopic pregnancies – extrauterine sites of origin One of the most rapidly invasive widely metastasizing malignancies
Choriocarcinoma Ø Ø 1/40 hydatiform moles → choriocarcinoma 1/150, 000 normal pregnancies → choriocarcinoma
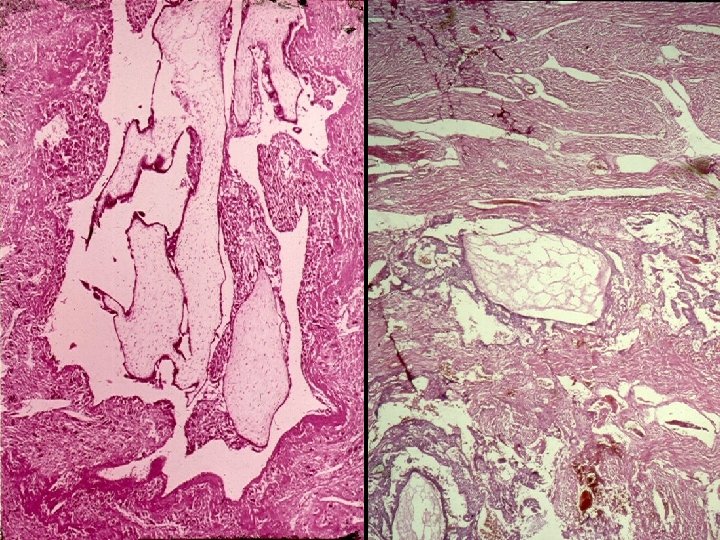
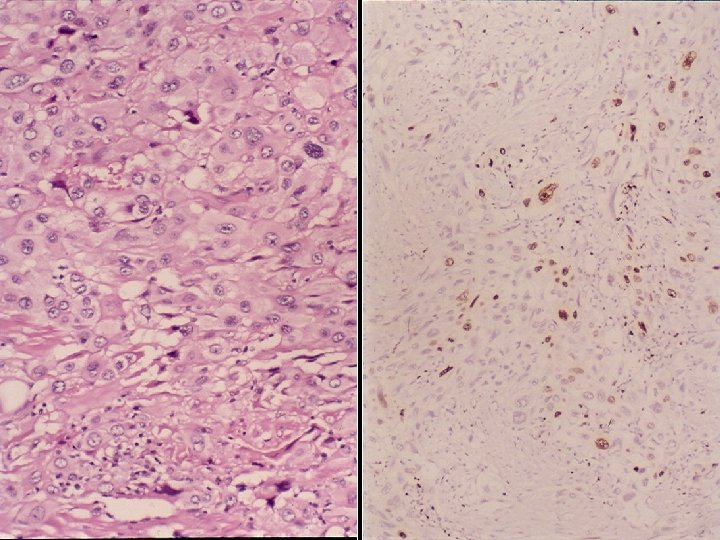
Morphology n n n Epithelial, cellular Chorionic villi (-) Abnormal proliferation of cytotrophoblast & syncytial trophoblast n n n n n Anaplasia Abnormal mitoses (+) Invasion of the myometrium Penetration of blood vessels & lymphatics Extension out (uterine serosa, adjacent structures) Hemorrhage Ischemic necrosis, cystic softening Secondary inflammatory infiltration Metastases: lungs, bone marrow, liver, vagina, brain, kidney HCG titers to levels above those encountered in moles. SUCH EXTREME ELEVATIONS → DIAGNOSIS OF CHORIOCARCINOMA
- Slides: 31