Gestational Trophoblastic Disease GTD Part I Molar Pregnancy
Gestational Trophoblastic Disease (GTD) Part I : Molar Pregnancy • Dr. Mohamed El Sherbiny MD Ob. & Gyn. Senior Consultant • Damietta, Egypt
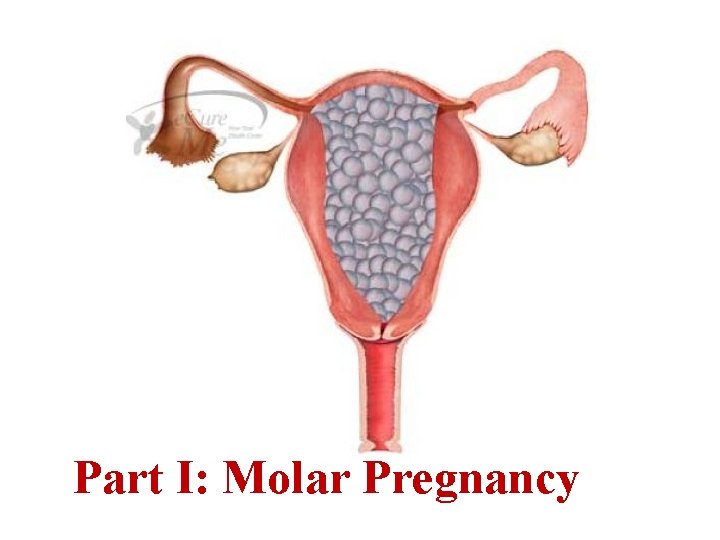
Part I: Molar Pregnancy
Definitions Gestational Trophoblastic Disease (GTD) It is a spectrum of trophoblastic diseases that includes: Complete molar pregnancy Partial molar pregnancies Invasive mole Choriocarcinoma Placental site trophoblastic tumour The last 2 may follow abortion, ectopic or normal pregnancy. RCOG Guideline No. 38. 2010
Definitions Gestational Trophoblastic Neoplasia (GTN) =Malignant Gestational Trophoblastic Disease It is a spectrum of trophoblastic diseases that develops malignant sequelae. GTN includes: Persistent post molar GTD Invasive mole Choriocarcinoma Placental site trophoblastic tumour The last 2 may follow abortion, ectopic or normal pregnancy. Disaia &Creasman Clinical Gynecological Oncology 2007 Cunningham et al Williams Obsterics 23 rd , 2010
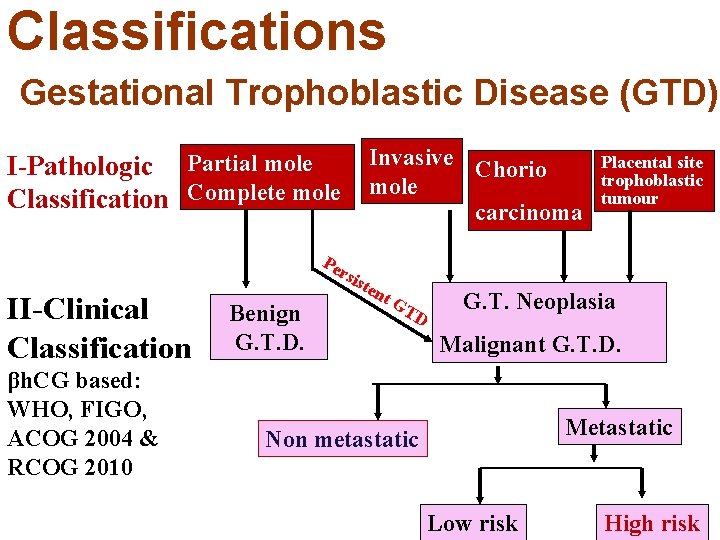
Classifications Gestational Trophoblastic Disease (GTD) Invasive Chorio I-Pathologic Partial mole Complete mole Classification carcinoma Placental site trophoblastic tumour Pe II-Clinical Classification βh. CG based: WHO, FIGO, ACOG 2004 & RCOG 2010 rsi ste Benign G. T. D. nt GT D G. T. Neoplasia Malignant G. T. D. Metastatic Non metastatic Low risk High risk
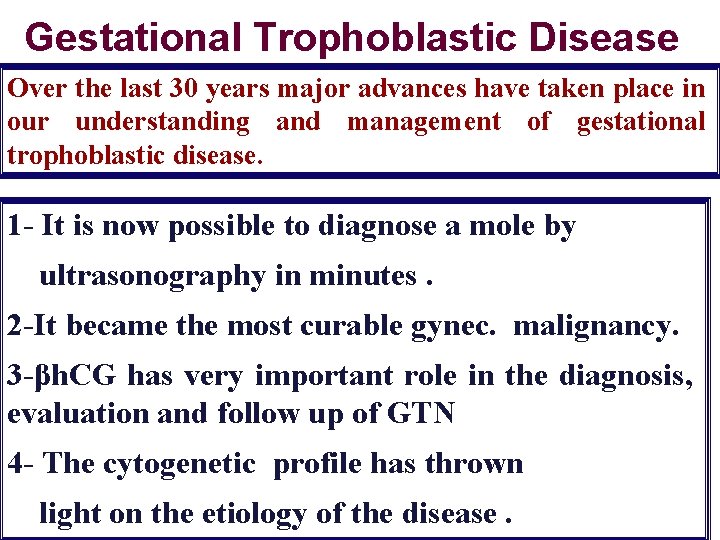
Gestational Trophoblastic Disease Over the last 30 years major advances have taken place in our understanding and management of gestational trophoblastic disease. 1 - It is now possible to diagnose a mole by ultrasonography in minutes. 2 -It became the most curable gynec. malignancy. 3 -βh. CG has very important role in the diagnosis, evaluation and follow up of GTN 4 - The cytogenetic profile has thrown light on the etiology of the disease.
Hydatidiform Mole - (H. MOLE) = Vesicular Mole
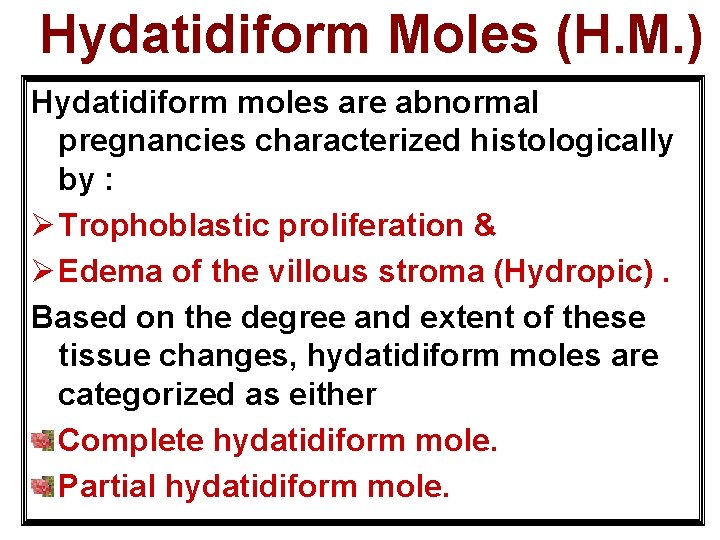
Hydatidiform Moles (H. M. ) Hydatidiform moles are abnormal pregnancies characterized histologically by : Ø Trophoblastic proliferation & Ø Edema of the villous stroma (Hydropic). Based on the degree and extent of these tissue changes, hydatidiform moles are categorized as either Complete hydatidiform mole. Partial hydatidiform mole.
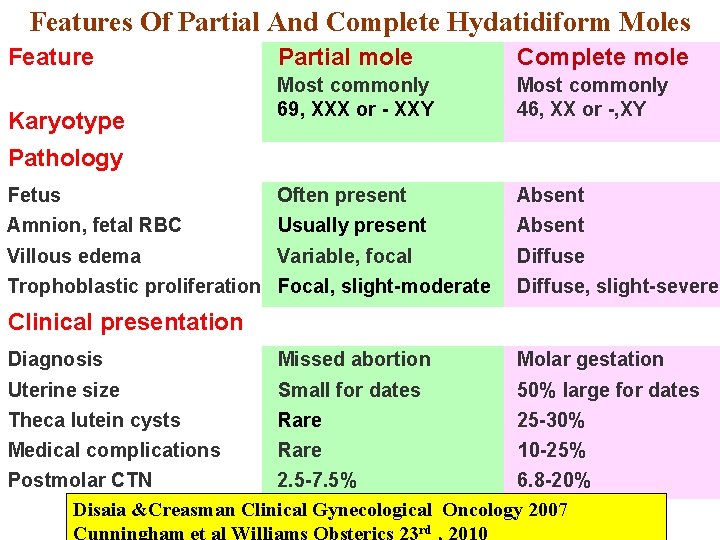
Features Of Partial And Complete Hydatidiform Moles Feature Partial mole Complete mole Most commonly 69, XXX or - XXY Most commonly 46, XX or -, XY Fetus Often present Absent Amnion, fetal RBC Usually present Absent Villous edema Variable, focal Diffuse Karyotype Pathology Trophoblastic proliferation Focal, slight-moderate Diffuse, slight-severe Clinical presentation Diagnosis Missed abortion Molar gestation Uterine size Small for dates 50% large for dates Theca lutein cysts Rare 25 -30% Medical complications Rare 10 -25% Postmolar CTN 2. 5 -7. 5% 6. 8 -20% Disaia &Creasman Clinical Gynecological Oncology 2007 rd
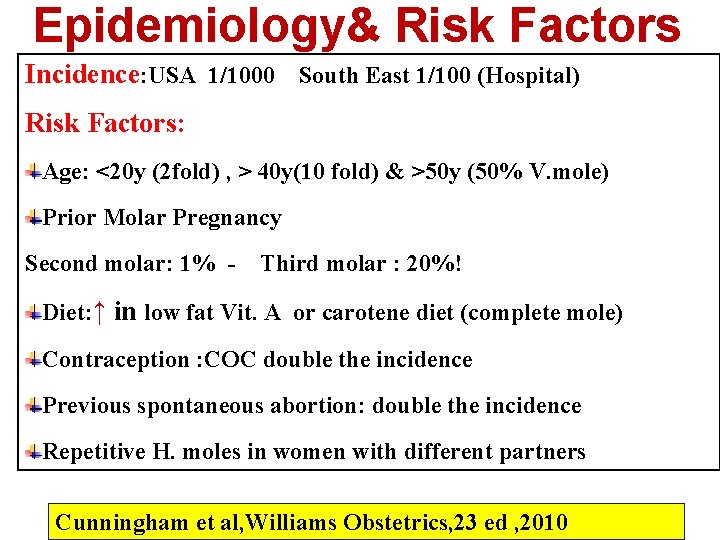
Epidemiology& Risk Factors Incidence: USA 1/1000 South East 1/100 (Hospital) Risk Factors: Age: <20 y (2 fold) , > 40 y(10 fold) & >50 y (50% V. mole) Prior Molar Pregnancy Second molar: 1% - Third molar : 20%! Diet: ↑ in low fat Vit. A or carotene diet (complete mole) Contraception : COC double the incidence Previous spontaneous abortion: double the incidence Repetitive H. moles in women with different partners Cunningham et al, Williams Obstetrics, 23 ed , 2010
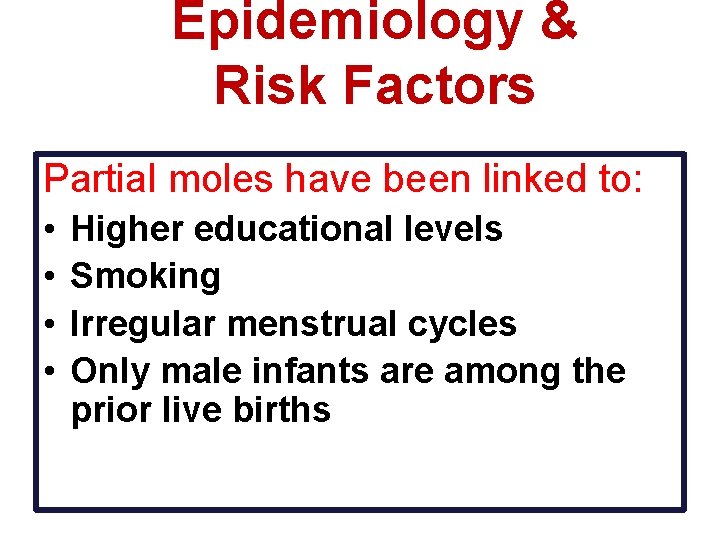
Epidemiology & Risk Factors Partial moles have been linked to: • • Higher educational levels Smoking Irregular menstrual cycles Only male infants are among the prior live births
Karyotype
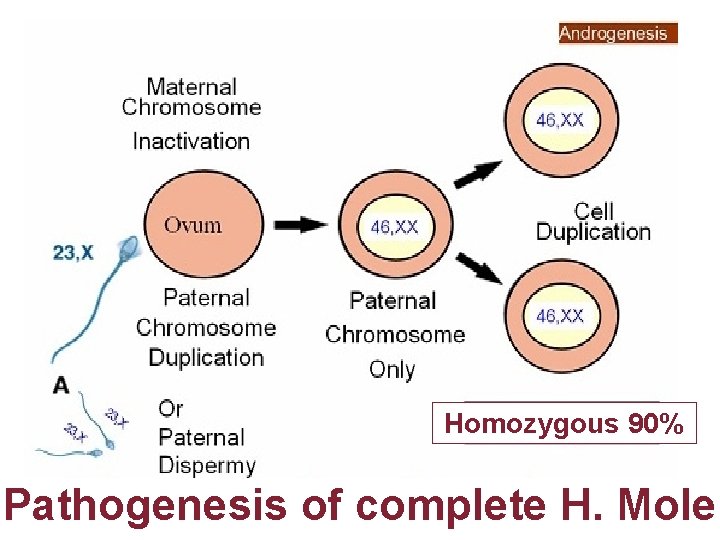
Homozygous 90% Pathogenesis of complete H. Mole
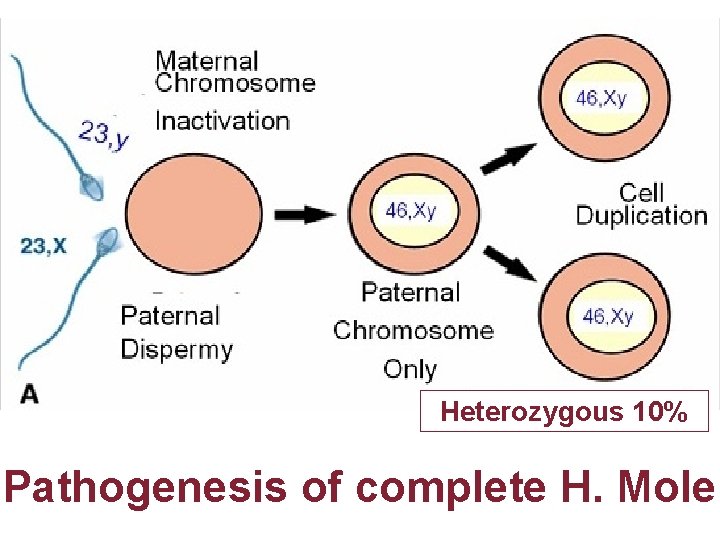
Heterozygous 10% Pathogenesis of complete H. Mole
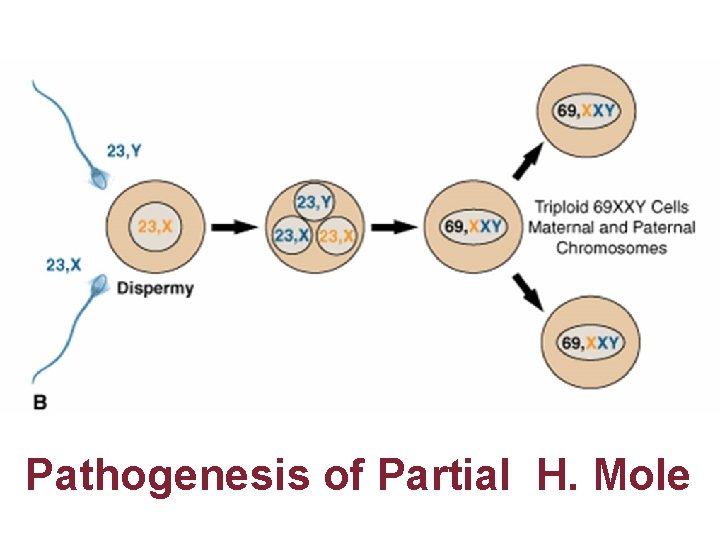
Pathogenesis of Partial H. Mole
Pathology of Molar Pregnancy
Complete H. Mole Microscopically Enlarged, edematous villi and abnormal trophoblastic proliferation that diffusely involve the entire villi No fetal tissue, RBCs or amnion are produced Macroscopically, these microscopic changes transform the chorionic villi into clusters of vesicles with variable dimensions “ like bunch of grapes" No fetal or embryonic tissue are produced Uterine enlargement in excess of gestational age. Theca-lutein cyst associated in 30%
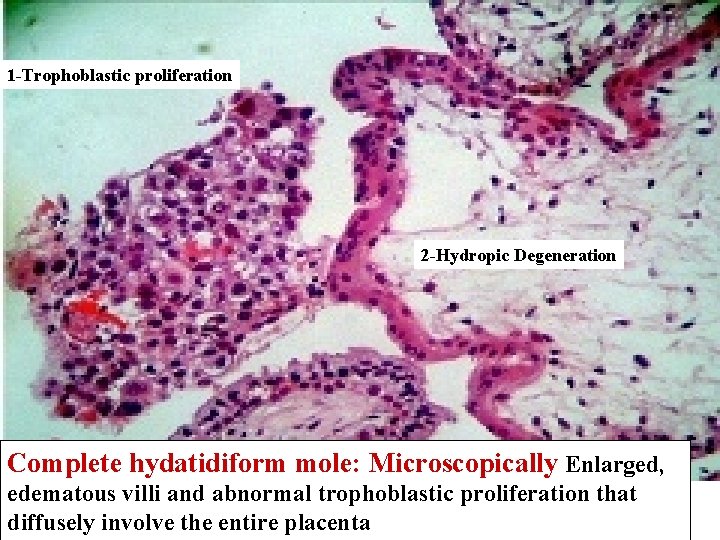
1 -Trophoblastic proliferation 2 -Hydropic Degeneration Complete hydatidiform mole: Microscopically Enlarged, edematous villi and abnormal trophoblastic proliferation that diffusely involve the entire placenta
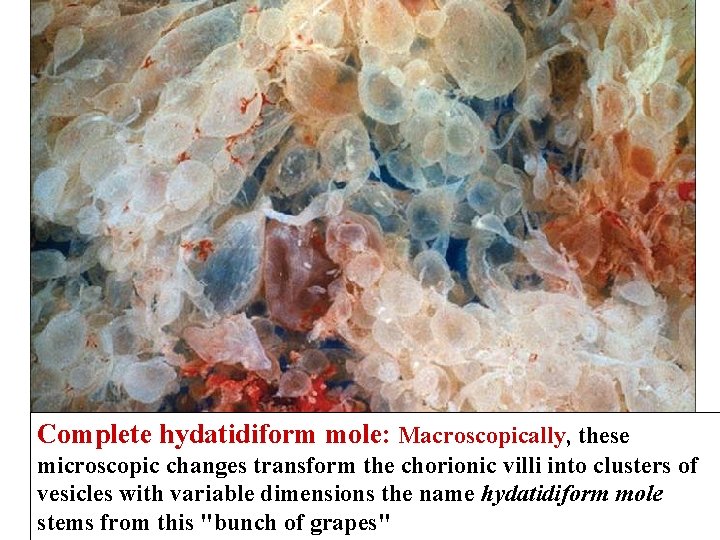
Complete hydatidiform mole: Macroscopically, these microscopic changes transform the chorionic villi into clusters of vesicles with variable dimensions the name hydatidiform mole stems from this "bunch of grapes"

Complete Hydatiform Mole Uterine wall
Pathogenesis of Choriocarcinoma –Aneuploidy –(Not a multiplication of 23 chromosome )
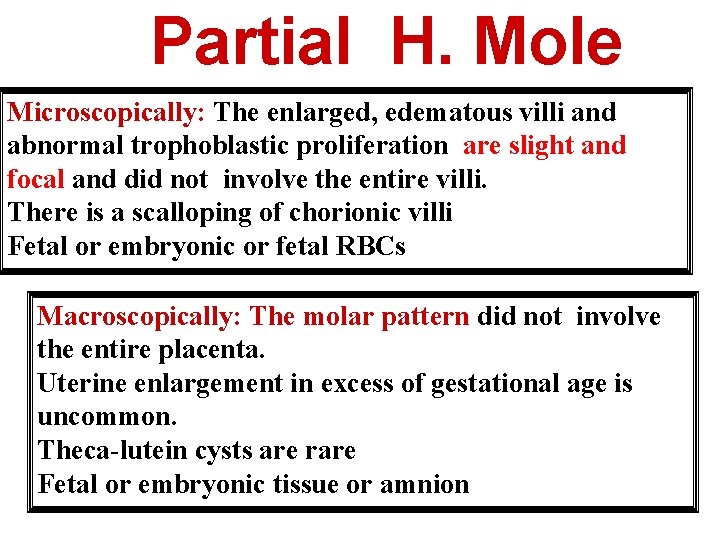
Partial H. Mole Microscopically: The enlarged, edematous villi and abnormal trophoblastic proliferation are slight and focal and did not involve the entire villi. There is a scalloping of chorionic villi Fetal or embryonic or fetal RBCs Macroscopically: The molar pattern did not involve the entire placenta. Uterine enlargement in excess of gestational age is uncommon. Theca-lutein cysts are rare Fetal or embryonic tissue or amnion
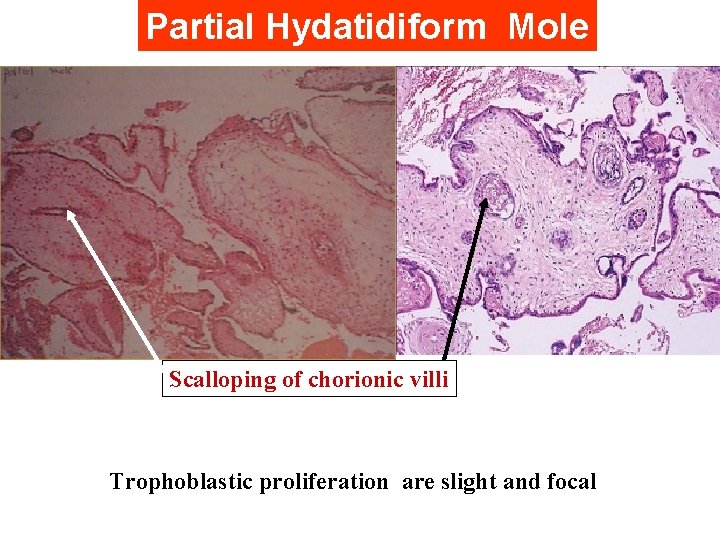
Partial Hydatidiform Mole Scalloping of chorionic villi Trophoblastic proliferation are slight and focal
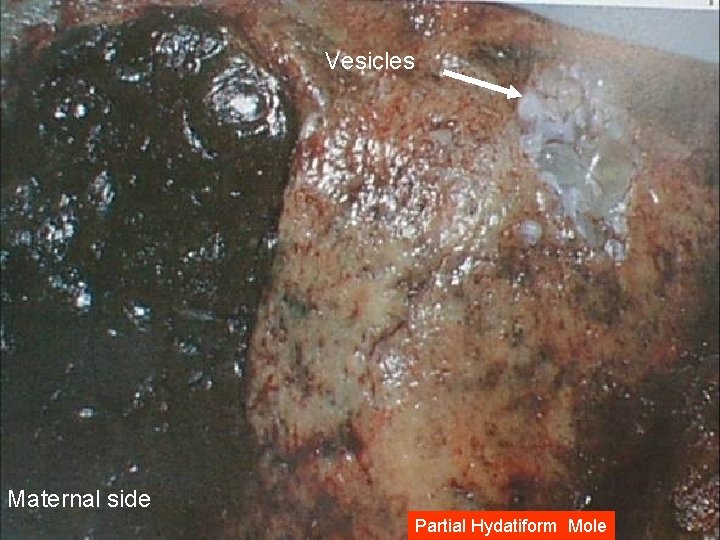
Vesicles Maternal side Partial Hydatiform Mole
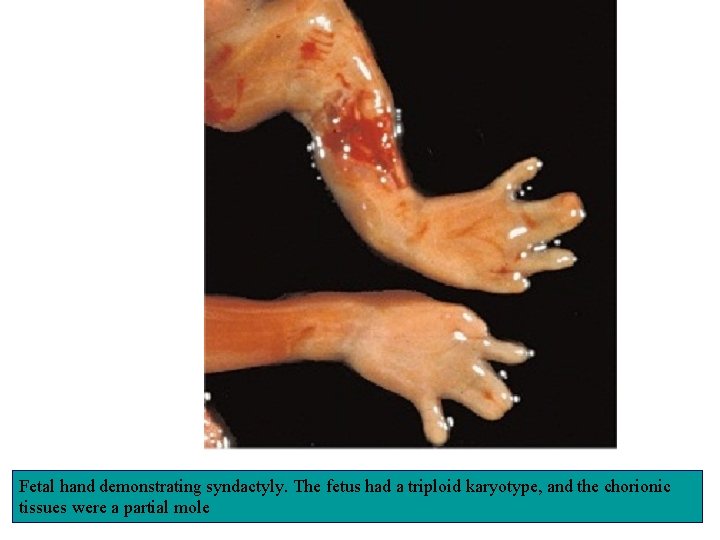
Fetal hand demonstrating syndactyly. The fetus had a triploid karyotype, and the chorionic tissues were a partial mole
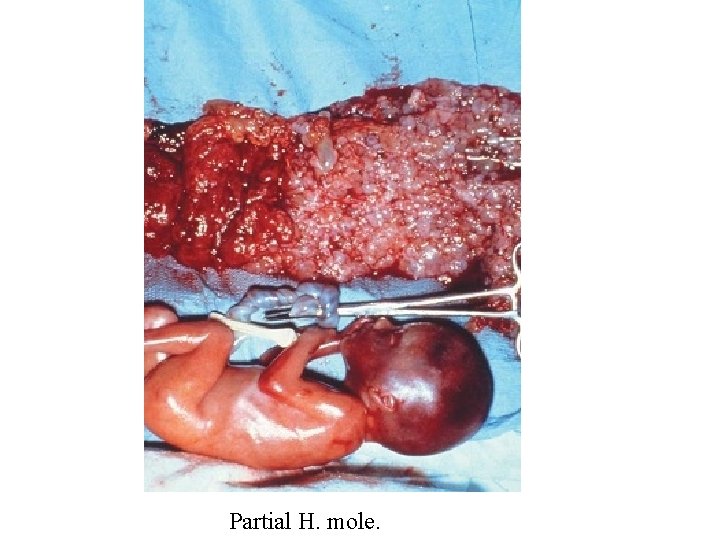
Partial H. mole.
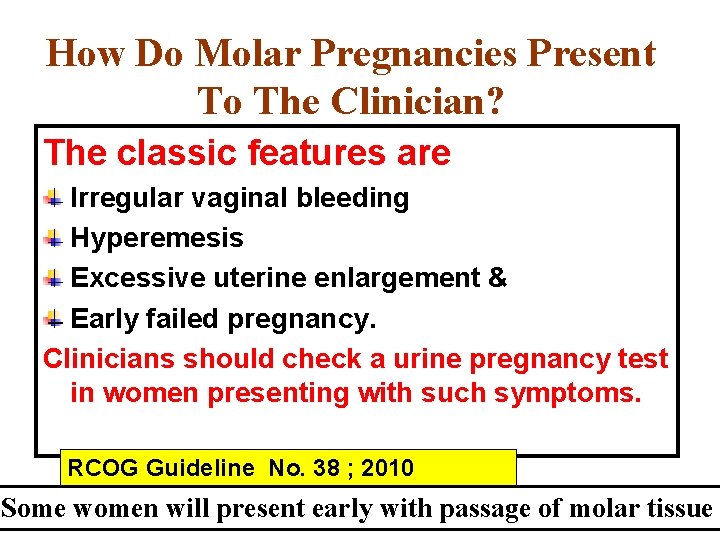
How Do Molar Pregnancies Present To The Clinician? The classic features are Irregular vaginal bleeding Hyperemesis Excessive uterine enlargement & Early failed pregnancy. Clinicians should check a urine pregnancy test in women presenting with such symptoms. RCOG Guideline No. 38 ; 2010 Some women will present early with passage of molar tissue
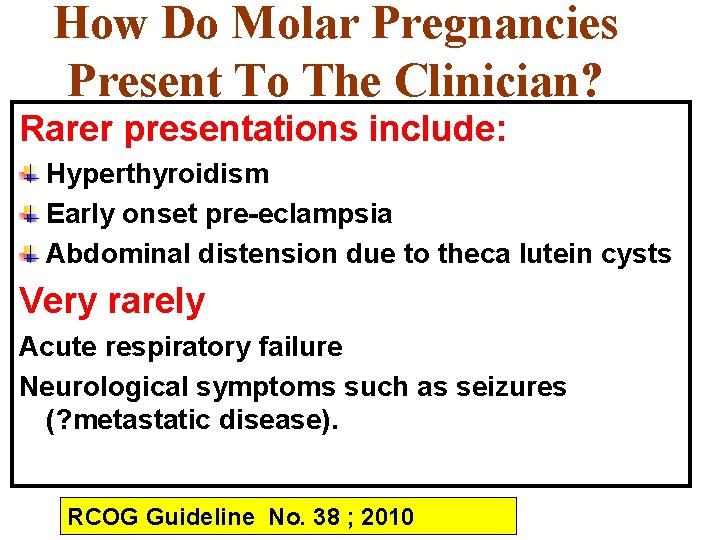
How Do Molar Pregnancies Present To The Clinician? Rarer presentations include: Hyperthyroidism Early onset pre-eclampsia Abdominal distension due to theca lutein cysts Very rarely Acute respiratory failure Neurological symptoms such as seizures (? metastatic disease). RCOG Guideline No. 38 ; 2010
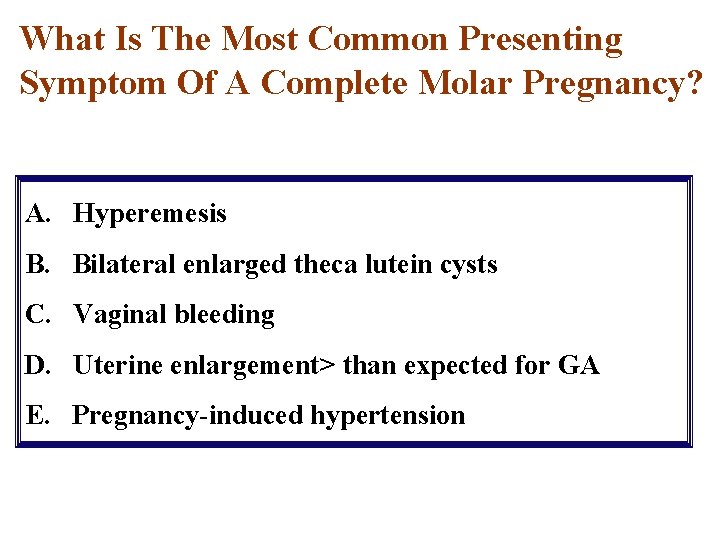
What Is The Most Common Presenting Symptom Of A Complete Molar Pregnancy? A. Hyperemesis B. Bilateral enlarged theca lutein cysts C. Vaginal bleeding D. Uterine enlargement> than expected for GA E. Pregnancy-induced hypertension
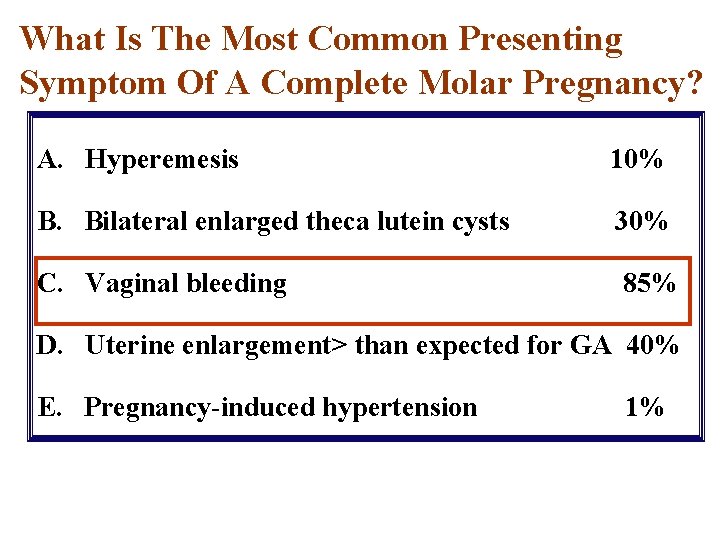
What Is The Most Common Presenting Symptom Of A Complete Molar Pregnancy? A. Hyperemesis 10% B. Bilateral enlarged theca lutein cysts 30% C. Vaginal bleeding 85% D. Uterine enlargement> than expected for GA 40% E. Pregnancy-induced hypertension 1%
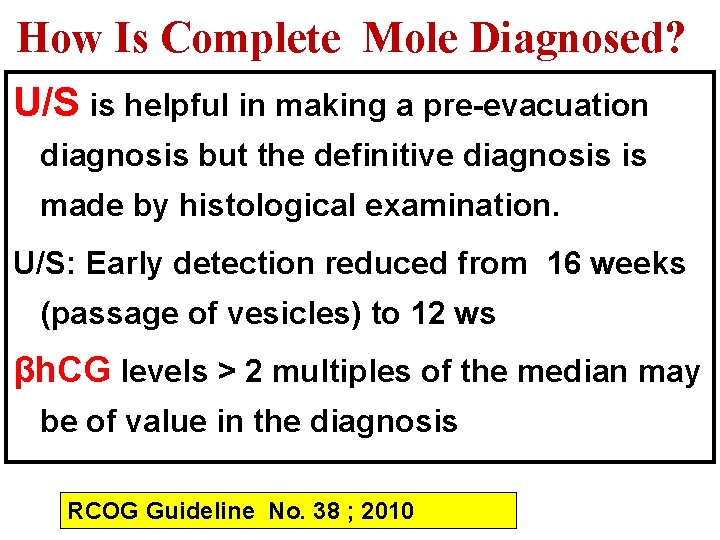
How Is Complete Mole Diagnosed? U/S is helpful in making a pre-evacuation diagnosis but the definitive diagnosis is made by histological examination. U/S: Early detection reduced from 16 weeks (passage of vesicles) to 12 ws βh. CG levels > 2 multiples of the median may be of value in the diagnosis RCOG Guideline No. 38 ; 2010
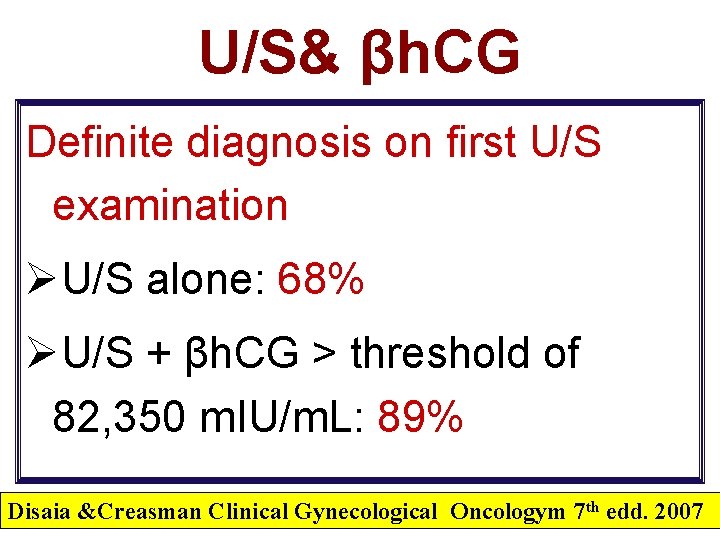
U/S& βh. CG Definite diagnosis on first U/S examination ØU/S alone: 68% ØU/S + βh. CG > threshold of 82, 350 m. IU/m. L: 89% Disaia &Creasman Clinical Gynecological Oncologym 7 th edd. 2007
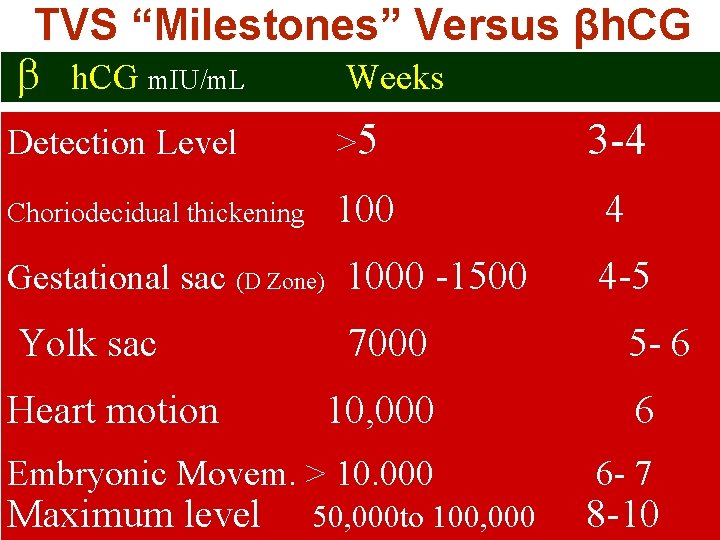
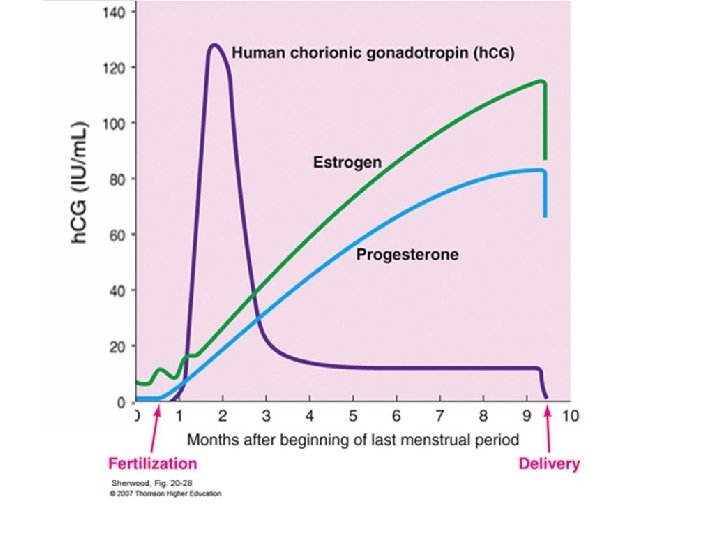
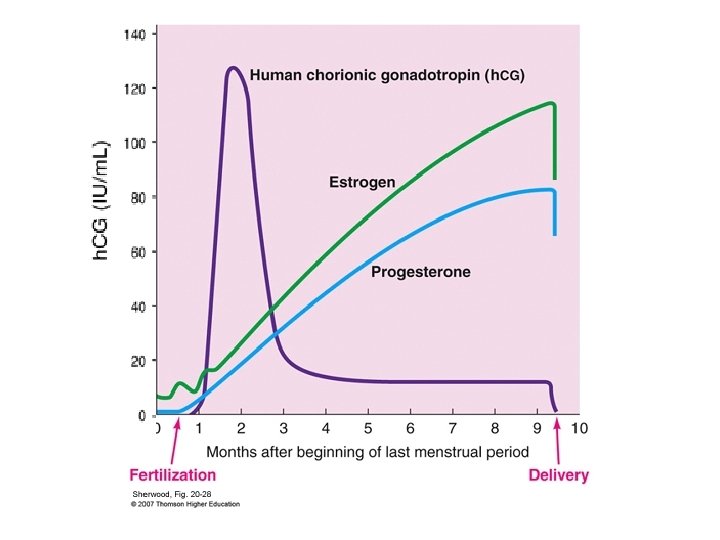
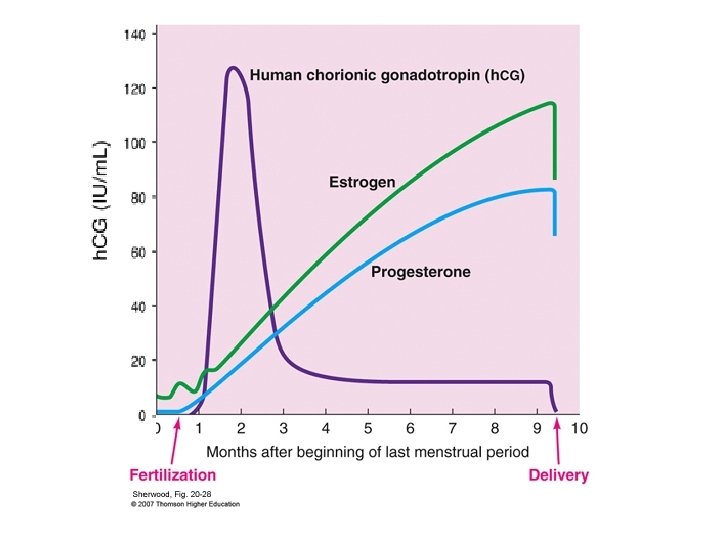
TVS “Milestones” Versus βh. CG m. IU/m. L Weeks Detection Level >5 3 -4 Choriodecidual thickening 100 Gestational sac (D Zone) 1000 -1500 Yolk sac Heart motion 7000 4 4 -5 5 - 6 10, 000 6 Embryonic Movem. > 10. 000 6 - 7 Maximum level 50, 000 to 100, 000 8 -10
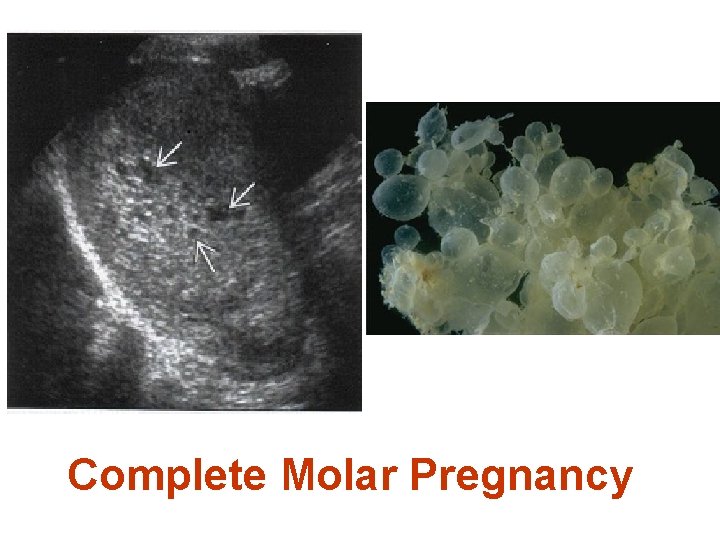
Complete Molar Pregnancy
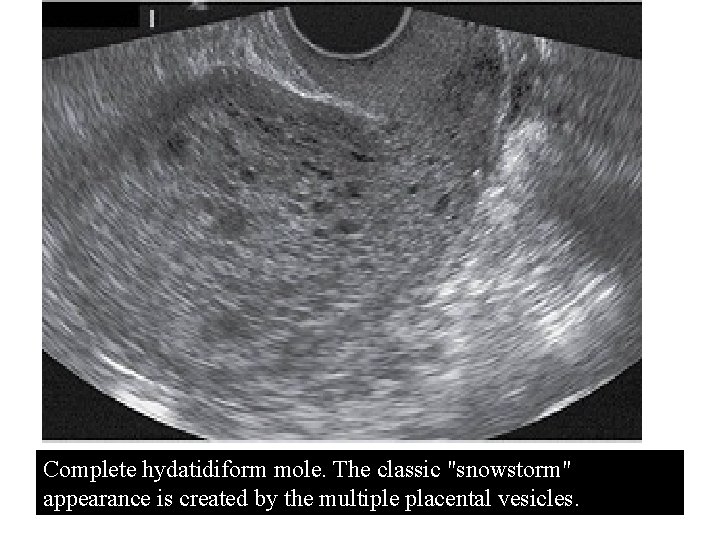
Complete hydatidiform mole. The classic "snowstorm" appearance is created by the multiple placental vesicles.
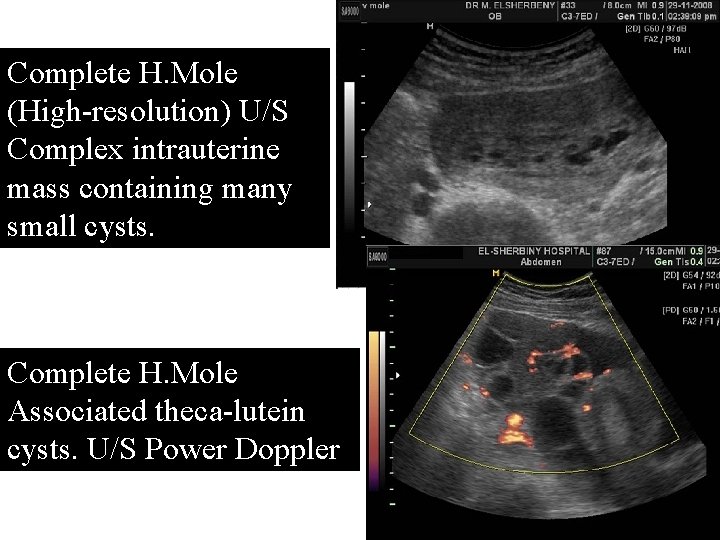
Complete H. Mole (High-resolution) U/S Complex intrauterine mass containing many small cysts. Complete H. Mole Associated theca-lutein cysts. U/S Power Doppler
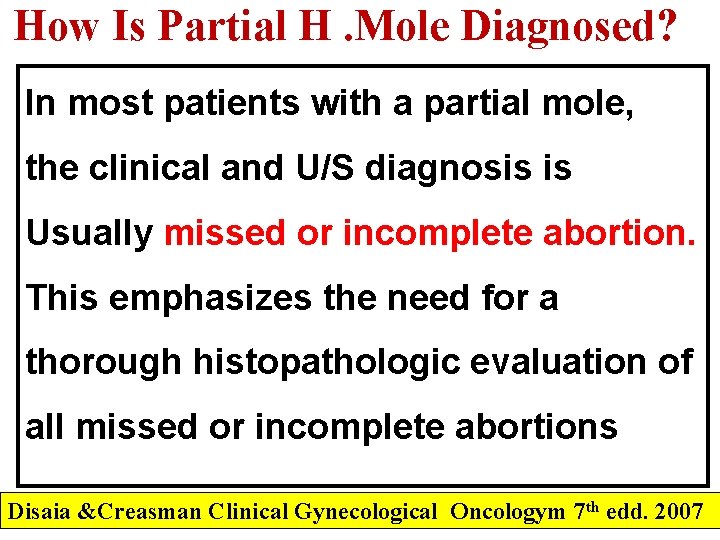
How Is Partial H. Mole Diagnosed? In most patients with a partial mole, the clinical and U/S diagnosis is Usually missed or incomplete abortion. This emphasizes the need for a thorough histopathologic evaluation of all missed or incomplete abortions Disaia &Creasman Clinical Gynecological Oncologym 7 th edd. 2007
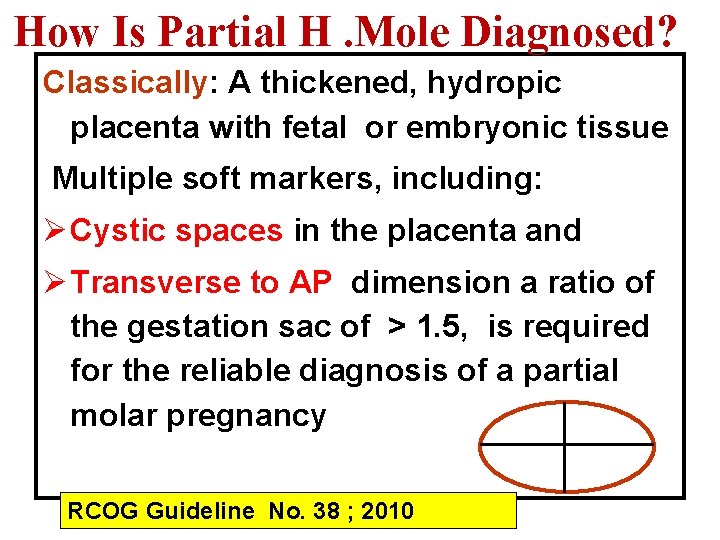
How Is Partial H. Mole Diagnosed? Classically: A thickened, hydropic placenta with fetal or embryonic tissue Multiple soft markers, including: Ø Cystic spaces in the placenta and Ø Transverse to AP dimension a ratio of the gestation sac of > 1. 5, is required for the reliable diagnosis of a partial molar pregnancy RCOG Guideline No. 38 ; 2010
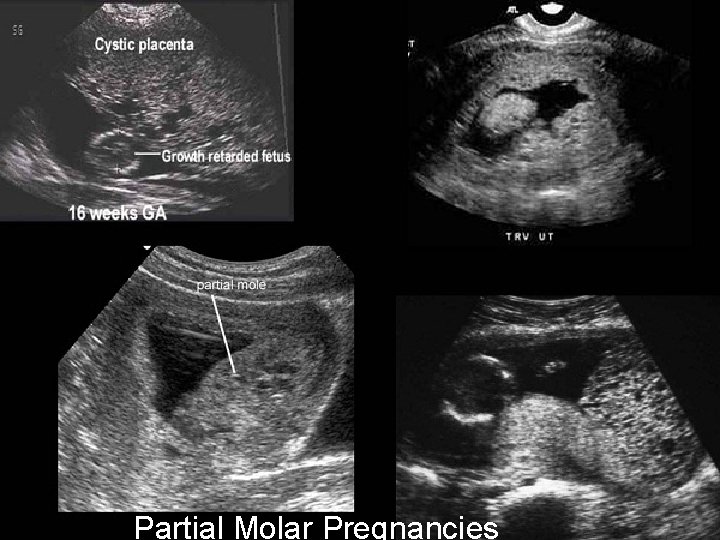
Partial Molar Pregnancies
Case Scenario 1 A 24 -year-old 2 nd Gravida , Para 1 woman at 8 Ws GA (Blood group: O, negative) complains of: 1 -Worsening nausea, and vomiting over the last 2 weeks which is unlike her prior pregnancy. 2 -Irregular vaginal bleeding over the last 7 days She denies any abdominal or back cramps. What does the differential diagnosis include for this patient?
What Does The Differential Diagnosis Include For This Patient? The differential diagnosis of bleeding with early pregnancy and progressive vomiting are: Multiple pregnancy. Hydatidiform mole. Threatened abortion. Ectopic pregnancy.
Which Diagnostic Test Would Be Most Useful? The most useful diagnostic test is : U/S
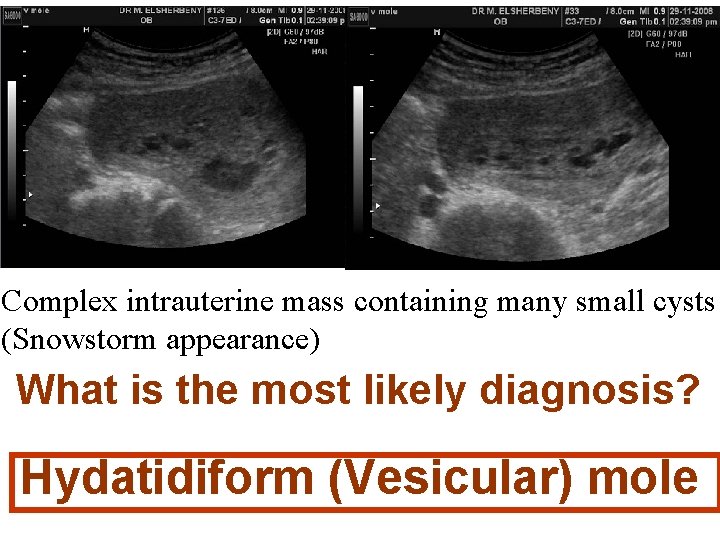
Complex intrauterine mass containing many small cysts (Snowstorm appearance) What is the most likely diagnosis? Hydatidiform (Vesicular) mole
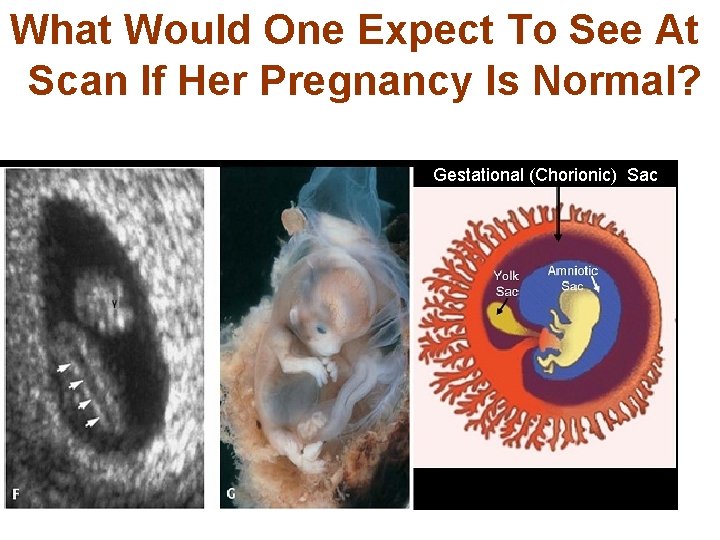
What Would One Expect To See At Scan If Her Pregnancy Is Normal? Gestational (Chorionic) Sac

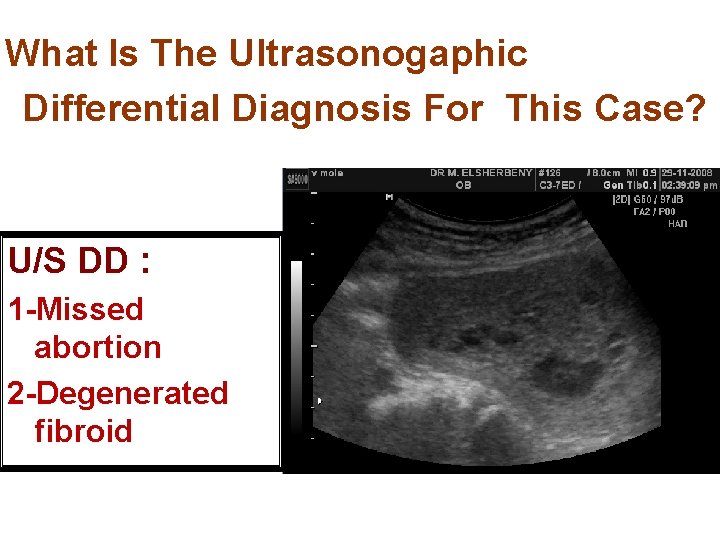
What Is The Ultrasonogaphic Differential Diagnosis For This Case? U/S DD : 1 -Missed abortion 2 -Degenerated fibroid
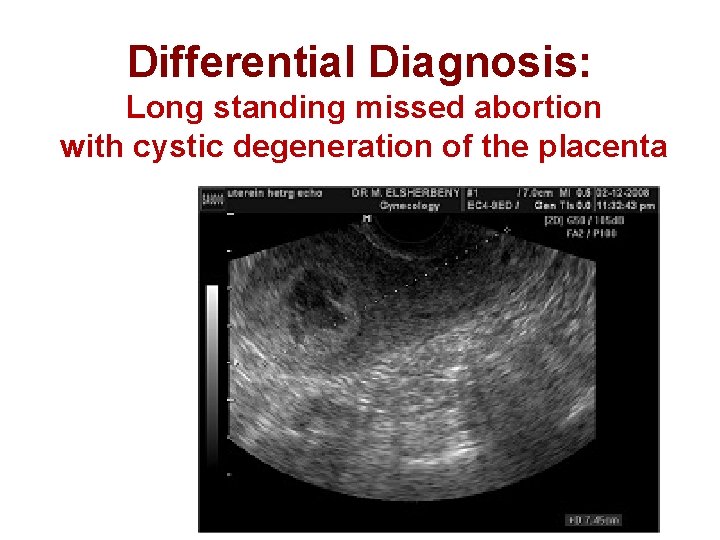
Differential Diagnosis: Long standing missed abortion with cystic degeneration of the placenta
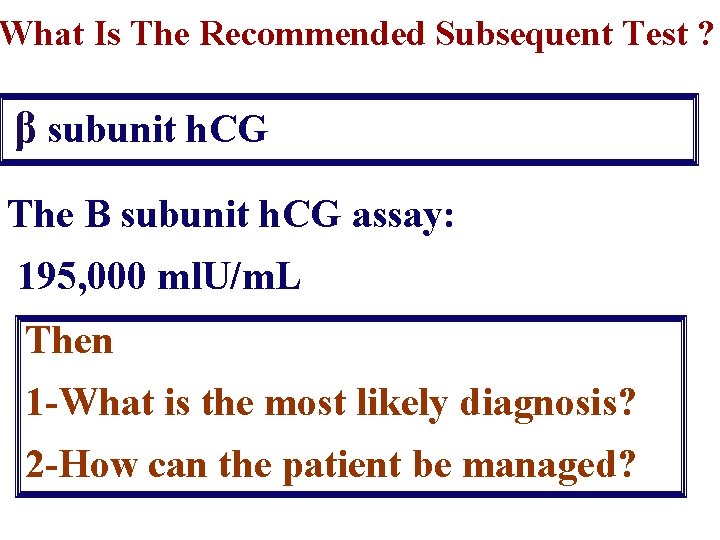
What Is The Recommended Subsequent Test ? β subunit h. CG The B subunit h. CG assay: 195, 000 ml. U/m. L Then 1 -What is the most likely diagnosis? 2 -How can the patient be managed?
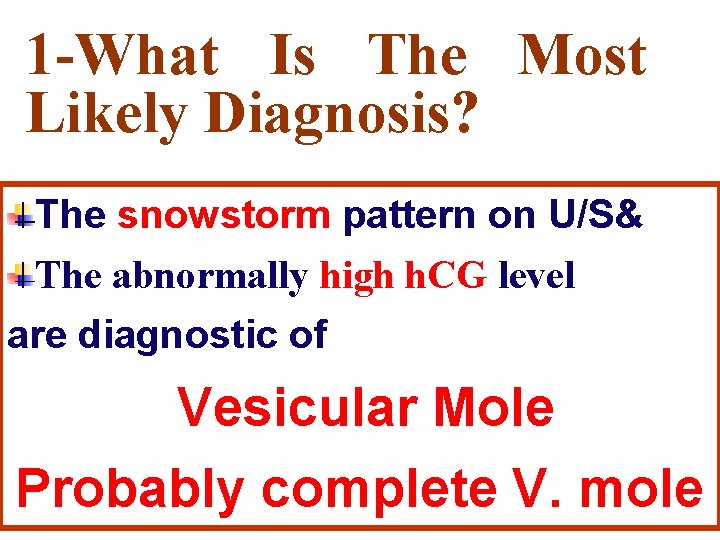
1 -What Is The Most Likely Diagnosis? The snowstorm pattern on U/S& The abnormally high h. CG level are diagnostic of Vesicular Mole Probably complete V. mole
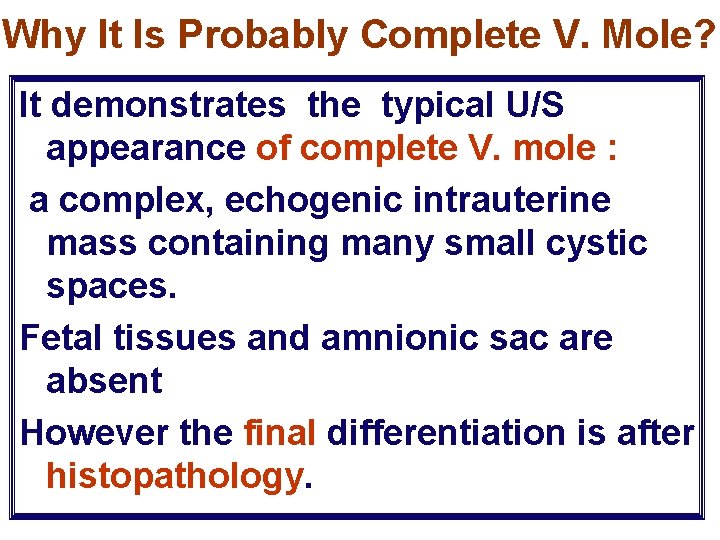
Why It Is Probably Complete V. Mole? It demonstrates the typical U/S appearance of complete V. mole : a complex, echogenic intrauterine mass containing many small cystic spaces. Fetal tissues and amnionic sac are absent However the final differentiation is after histopathology.
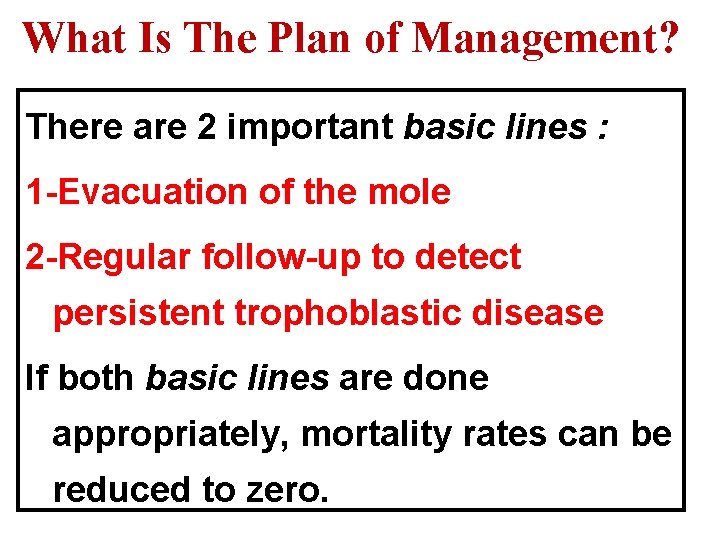
What Is The Plan of Management? There are 2 important basic lines : 1 -Evacuation of the mole 2 -Regular follow-up to detect persistent trophoblastic disease If both basic lines are done appropriately, mortality rates can be reduced to zero.
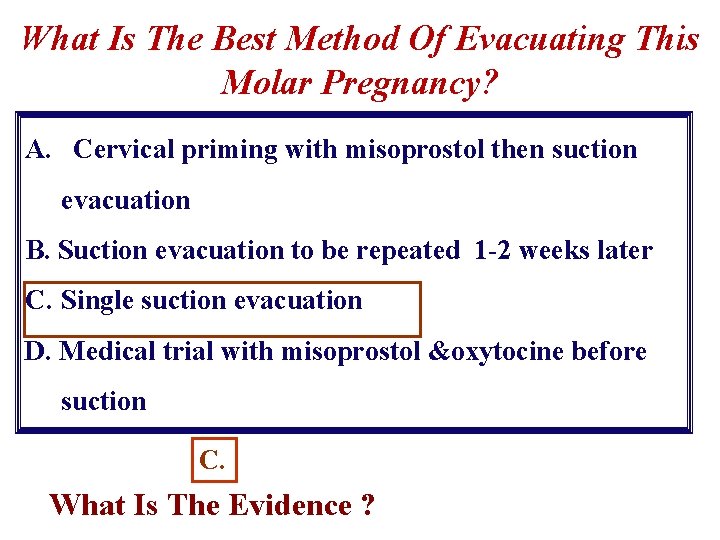
What Is The Best Method Of Evacuating This Molar Pregnancy? A. Cervical priming with misoprostol then suction evacuation B. Suction evacuation to be repeated 1 -2 weeks later C. Single suction evacuation D. Medical trial with misoprostol &oxytocine before suction C. What Is The Evidence ?
What Is The Evidence ? The Management Of Gestational Trophoblastic Disease RCOG Guideline No. 38 ; 2010
What Is The Best Method Of Evacuating A Molar Pregnancy? For Complete mole is: Suction curettage Cervical preparation with prostaglandins or misoprostol , should be avoided to reduce the risk of embolisation (No sufficient studies) RCOG Guideline No. 38 ; 2010
Is That The Same For Partial Mole? For Partial mole: It depends on the fetal parts Small fetal parts : Suction curettage Large fetal parts: Medical (oxytocics) In partial mole the oxytocics is safe , as the hazard to embolise and disseminate trophoblastic tissue is very low Also, the needing for chemotherapy is 0. 1 - 0. 5%. RCOG Guideline No. 38 ; 2010
Can Oxytocic Infusions Be Used During Surgical Evacuation? • The use of oxytocic infusion prior to completion of the evacuation is not recommended (fear of embolisation). • If the woman is experiencing significant haemorrhage prior to evacuation, surgical evacuation should be expedited and the need for oxytocin infusion weighed up against the risk of tumour embolisation. RCOG Guideline No. 38 ; 2010
Should Products Of Conception Be Examined Histologically? Histological examination is indicated in: Failed pregnancies (missed or molar) : All medically or surgical managed cases Products of conception, obtained after all repeat evacuations (post abortive or p. partum) There is no need after therapeutic termination : provided that fetal parts is identified on U/S RCOG Guideline No. 38 ; 2010
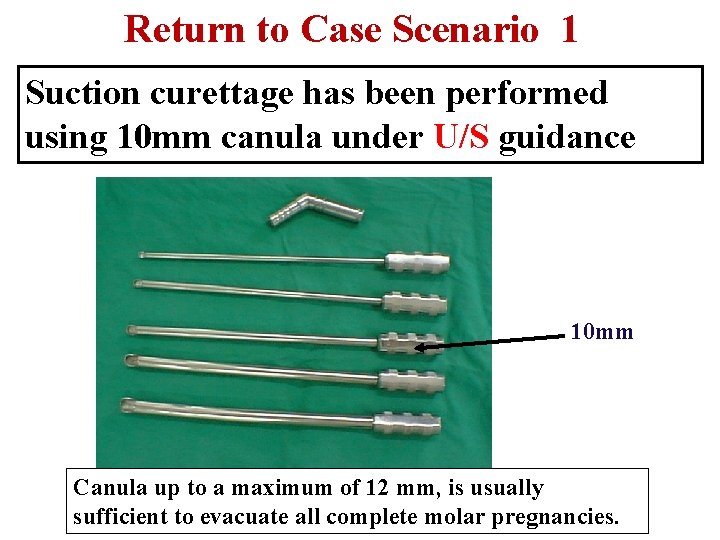
Return to Case Scenario 1 Suction curettage has been performed using 10 mm canula under U/S guidance 10 mm Canula up to a maximum of 12 mm, is usually sufficient to evacuate all complete molar pregnancies.

Other seats of suction curettage
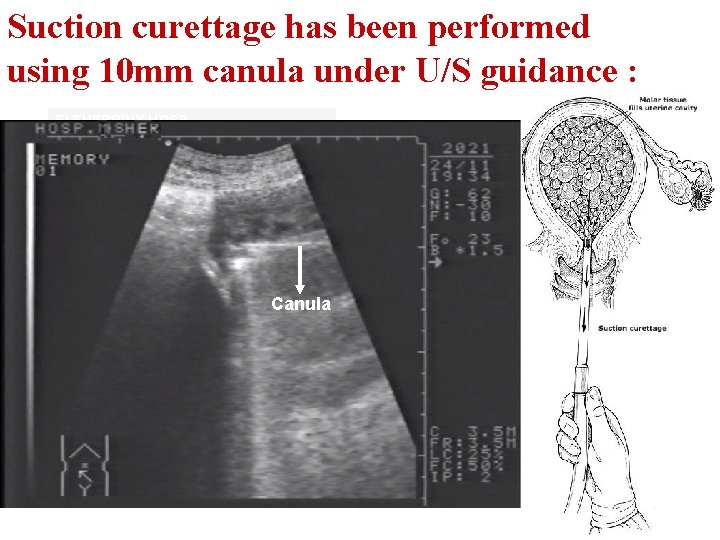
Suction curettage has been performed using 10 mm canula under U/S guidance : El SHERBINY HOSP Canula
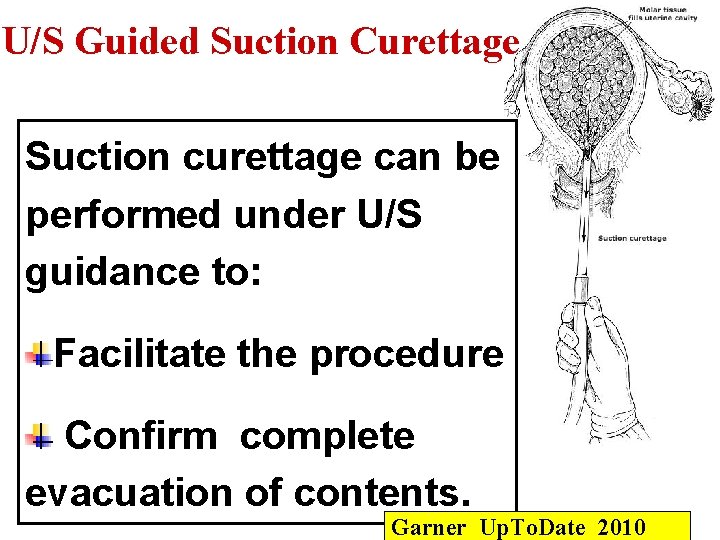
U/S Guided Suction Curettage Suction curettage can be performed under U/S guidance to: Facilitate the procedure Confirm complete evacuation of contents. Garner Up. To. Date 2010

The Molar Content For Histopathological Examination
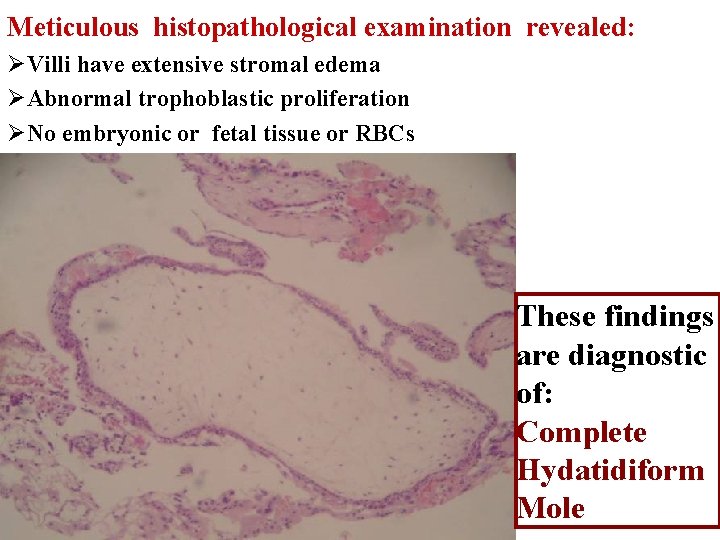
Meticulous histopathological examination revealed: ØVilli have extensive stromal edema ØAbnormal trophoblastic proliferation ØNo embryonic or fetal tissue or RBCs These findings are diagnostic of: Complete Hydatidiform Mole
The Case is Now Confirmed Histopathological As A Complete H. Mole What Is The Most Appropriate Management? A- Surveillance : Weekly then monthly βh. CG B-Hysterectomy C-Transvaginal U/S examination D-Repeated curettage &Biopsy E-Prompt chemotherapy A.
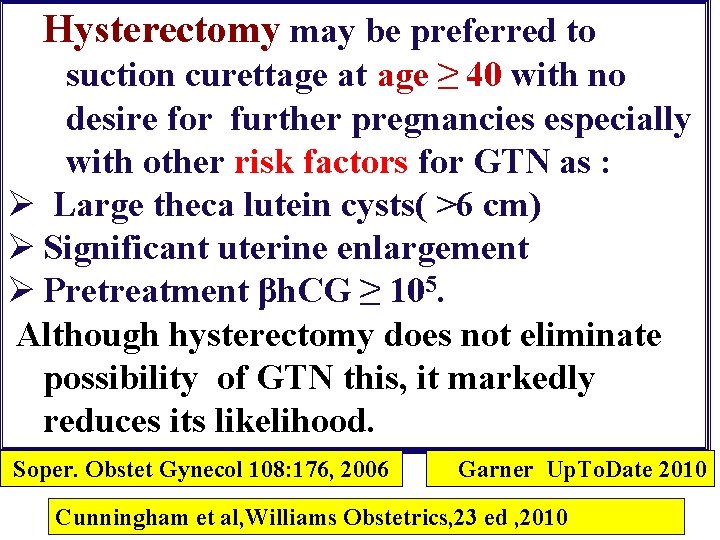
Hysterectomy may be preferred to suction curettage at age ≥ 40 with no desire for further pregnancies especially with other risk factors for GTN as : Ø Large theca lutein cysts( >6 cm) Ø Significant uterine enlargement Ø Pretreatment βh. CG ≥ 105. Although hysterectomy does not eliminate possibility of GTN this, it markedly reduces its likelihood. Soper. Obstet Gynecol 108: 176, 2006 Garner Up. To. Date 2010 Cunningham et al, Williams Obstetrics, 23 ed , 2010
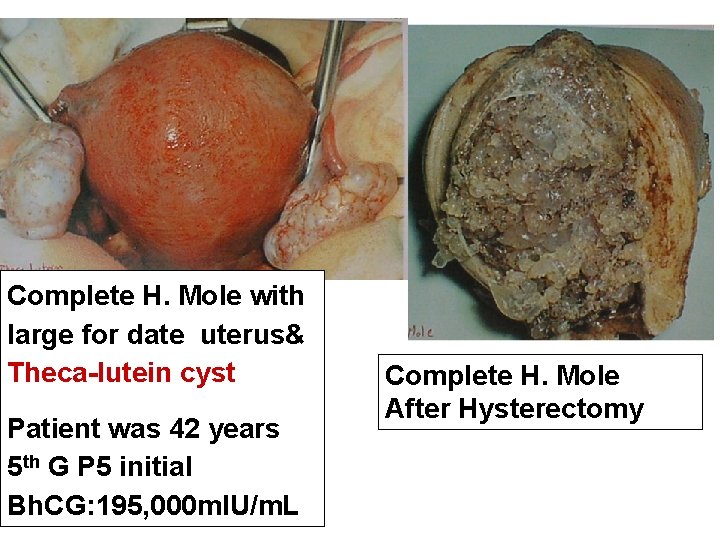
Complete H. Mole with large for date uterus& Theca-lutein cyst Patient was 42 years 5 th G P 5 initial Bh. CG: 195, 000 m. IU/m. L Complete H. Mole After Hysterectomy

Theca-lutein cyst associated with a complete H. mole in >30%
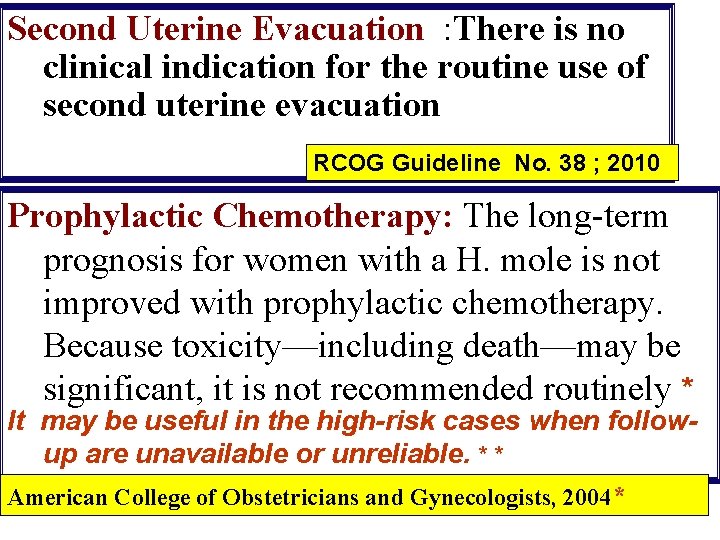
Second Uterine Evacuation : There is no clinical indication for the routine use of second uterine evacuation RCOG Guideline No. 38 ; 2010 Prophylactic Chemotherapy: The long-term prognosis for women with a H. mole is not improved with prophylactic chemotherapy. Because toxicity—including death—may be significant, it is not recommended routinely * It may be useful in the high-risk cases when followup are unavailable or unreliable. * * American College of Obstetricians and Gynecologists, 2004*
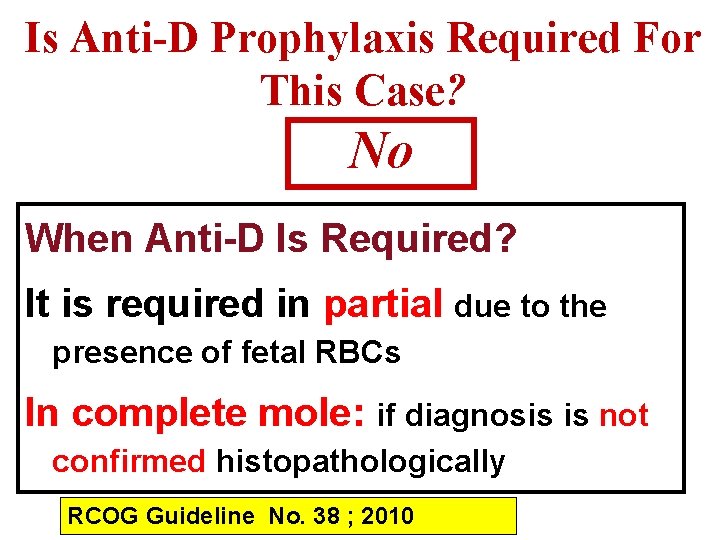
Is Anti-D Prophylaxis Required For This Case? No When Anti-D Is Required? It is required in partial due to the presence of fetal RBCs In complete mole: if diagnosis is not confirmed histopathologically RCOG Guideline No. 38 ; 2010
Post-evacuation Surveillance Why? ØTo determine when pregnancy can be allowed ØTo detect persistent trophoblastic disease (i. e. GTN)
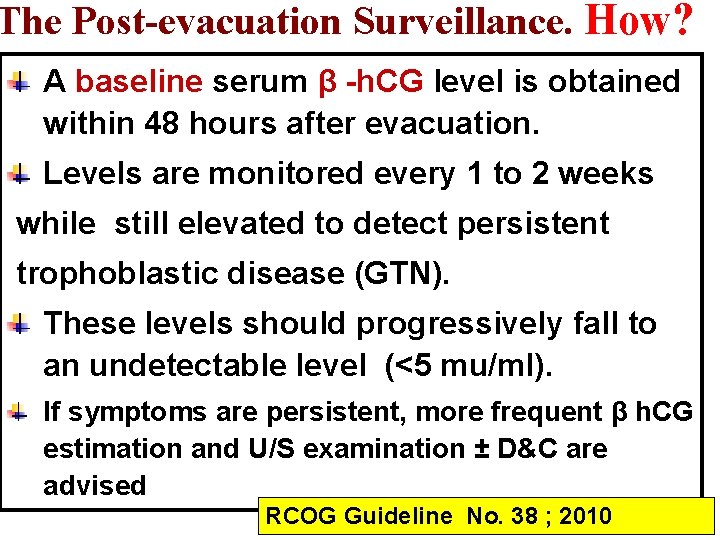
The Post-evacuation Surveillance. How? A baseline serum β -h. CG level is obtained within 48 hours after evacuation. Levels are monitored every 1 to 2 weeks while still elevated to detect persistent trophoblastic disease (GTN). These levels should progressively fall to an undetectable level (<5 mu/ml). If symptoms are persistent, more frequent β h. CG estimation and U/S examination ± D&C are advised RCOG Guideline No. 38 ; 2010
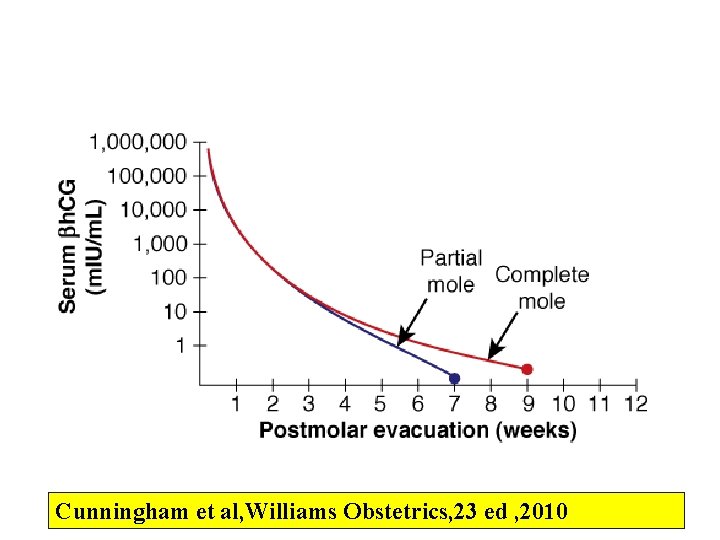
Cunningham et al, Williams Obstetrics, 23 ed , 2010
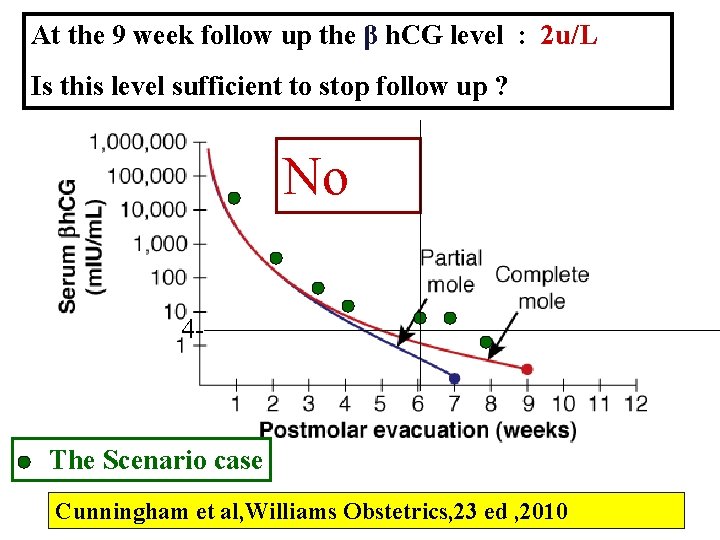
At the 9 week follow up the β h. CG level : 2 u/L Is this level sufficient to stop follow up ? No 4 - The Scenario case Cunningham et al, Williams Obstetrics, 23 ed , 2010
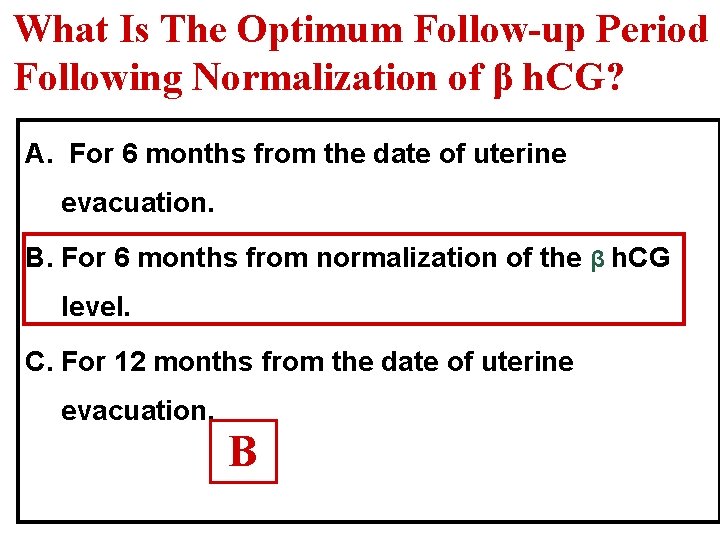
What Is The Optimum Follow-up Period Following Normalization of β h. CG? A. For 6 months from the date of uterine evacuation. B. For 6 months from normalization of the β h. CG level. C. For 12 months from the date of uterine evacuation. B
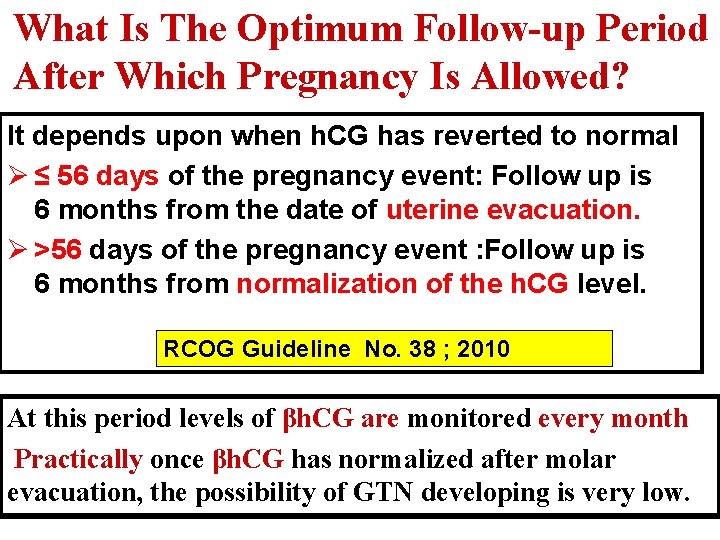
What Is The Optimum Follow-up Period After Which Pregnancy Is Allowed? It depends upon when h. CG has reverted to normal Ø ≤ 56 days of the pregnancy event: Follow up is 6 months from the date of uterine evacuation. Ø >56 days of the pregnancy event : Follow up is 6 months from normalization of the h. CG level. RCOG Guideline No. 38 ; 2010 At this period levels of βh. CG are monitored every month Practically once βh. CG has normalized after molar evacuation, the possibility of GTN developing is very low.
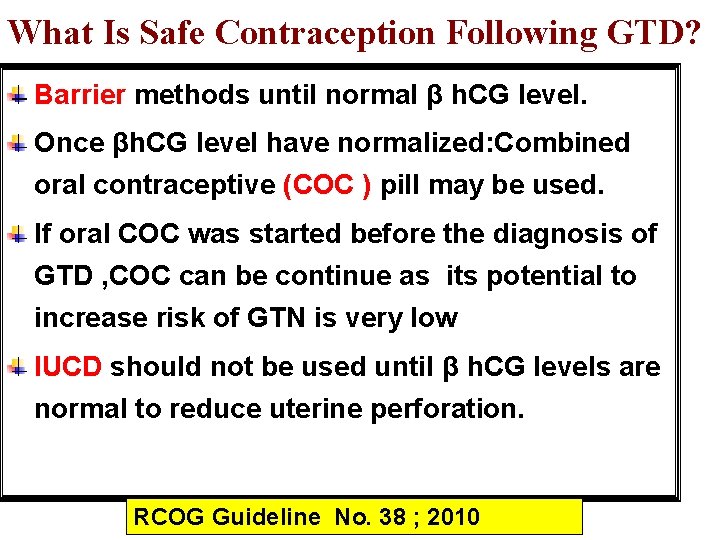
What Is Safe Contraception Following GTD? Barrier methods until normal β h. CG level. Once βh. CG level have normalized: Combined oral contraceptive (COC ) pill may be used. If oral COC was started before the diagnosis of GTD , COC can be continue as its potential to increase risk of GTN is very low IUCD should not be used until β h. CG levels are normal to reduce uterine perforation. RCOG Guideline No. 38 ; 2010

Case Scenario 2 A 34 -year-old woman, married for 7 years 3 rd Gravida , Para 0 at 14 Ws GA. The previous abortions were at 7&8 weeks. She complains of: 1 -Mild vaginal bleeding for 4 days 2 -Nausea, and moderate vomiting Pulse 95/m, Bp 140/85

US scanning revealed What Is The U/S Differential Diagnosis?
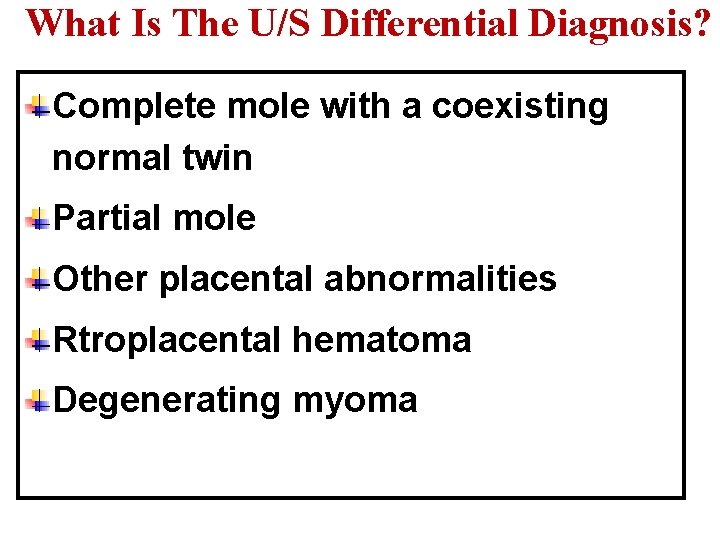
What Is The U/S Differential Diagnosis? Complete mole with a coexisting normal twin Partial mole Other placental abnormalities Rtroplacental hematoma Degenerating myoma

What Are The Required Investigations? Quantities serum β h. CG Free T 4 Protein in urine Rescanning after one week in a tertiary or fetal medicine center for diagnosis & screening.
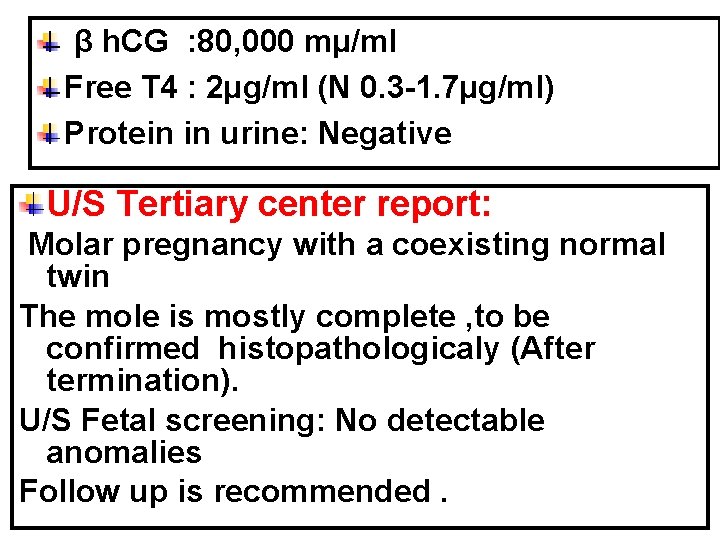
β h. CG : 80, 000 mµ/ml Free T 4 : 2µg/ml (N 0. 3 -1. 7µg/ml) Protein in urine: Negative U/S Tertiary center report: Molar pregnancy with a coexisting normal twin The mole is mostly complete , to be confirmed histopathologicaly (After termination). U/S Fetal screening: No detectable anomalies Follow up is recommended.
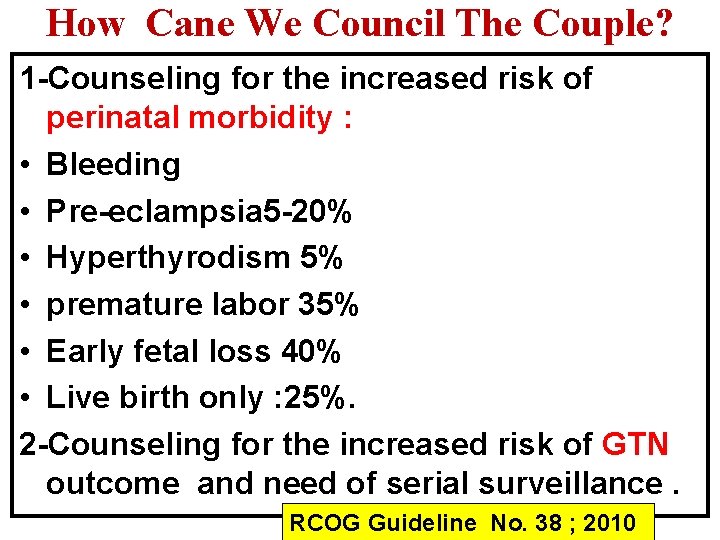
How Cane We Council The Couple? 1 -Counseling for the increased risk of perinatal morbidity : • Bleeding • Pre-eclampsia 5 -20% • Hyperthyrodism 5% • premature labor 35% • Early fetal loss 40% • Live birth only : 25%. 2 -Counseling for the increased risk of GTN outcome and need of serial surveillance. RCOG Guideline No. 38 ; 2010
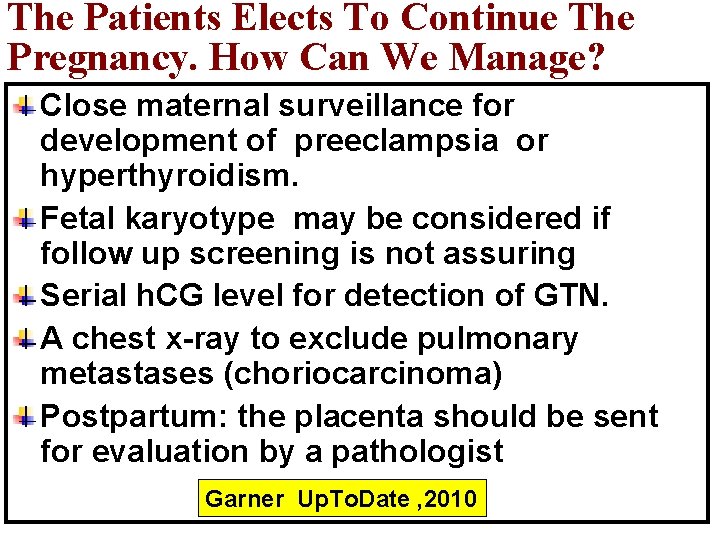
The Patients Elects To Continue The Pregnancy. How Can We Manage? Close maternal surveillance for development of preeclampsia or hyperthyroidism. Fetal karyotype may be considered if follow up screening is not assuring Serial h. CG level for detection of GTN. A chest x-ray to exclude pulmonary metastases (choriocarcinoma) Postpartum: the placenta should be sent for evaluation by a pathologist Garner Up. To. Date , 2010
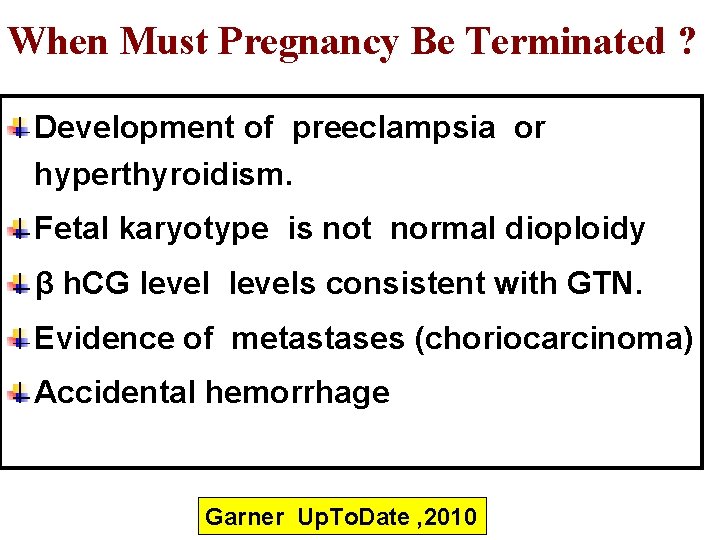
When Must Pregnancy Be Terminated ? Development of preeclampsia or hyperthyroidism. Fetal karyotype is not normal dioploidy β h. CG levels consistent with GTN. Evidence of metastases (choriocarcinoma) Accidental hemorrhage Garner Up. To. Date , 2010

Thank You Egypt
- Slides: 88