Geriatric Medicine Gary Winzelberg MD MPH Inpatient Medicine
Geriatric Medicine Gary Winzelberg, MD MPH Inpatient Medicine Clerkship
Ms. IM • 87 yo woman, Holocaust survivor • “Positive” cardiac stress test, elective catheterization, no intervention • Pre-meds: diphenhydramine 25 mg, diazepam 5 mg • Post-cath: somnolent, agitated, taking off clothes • Neurology consult • “Cause is atypical response to sedatives and benzodiazepines which is fairly normal in the elderly”
IM (2) • Admitted to hospital (vs discharged home) • Next morning: somnolent, will not respond to commands, occasionally opens eyes and occasionally verbalizes • Neurology follow-up • Benadryl and valium should have been out of the patient's system at this point…In 24 hours if unchanged recommend lumbar puncture and MRI brain.
IM (3) • Geriatrics: transition to health center at IM’s retirement community • Return to baseline mental status, cognitive function over 72 hours • Take Home points: – Preventable hospitalization – IM’s response was more typical than atypical – Pre-medicate 87 year old patients differently – Hospitals are dangerous places for older adults
IM Follow-Up • Age 90 – Fall, subararchnoid hemorrhage – Fall, right humerus & right hip fractures • Age 91 – Lives in assisted living – Ambulates independently with walker – Independent in activities of daily living
Objectives • To present medical student geriatric competencies • To discuss older adults’ diagnostic challenges • To identify potential hazards of hospitalization • To understand strategies re: delirium – Diagnosis – Prevention – Evaluation – Management
Who is a geriatric patient? • • Age Chronic diseases Functional limitations (ADLs, IADLs) Cognitive impairment Frailty Multidisciplinary assessment/service needs Goals of care
Minimum Geriatric Competencies • • Medication management Cognitive and Behavioral Disorders Self-Care Capacity Falls, Balance, Gait Disorders Health Care Planning and Promotion Atypical Presentation of Disease Palliative Care Hospital Care for Elders Leipzig RM et al. Academic Medicine 2009
Today’s Session #17: identify at least 3 physiologic changes of aging for each organ system and their impact on the patient #22: identify potential hazards of hospitalization #5: formulate a ddx for patient with delirium #6: in a patient with delirium, urgently initiate a diagnostic workup to determine the root cause #8: develop an evaluation and nonpharmacologic management plan for agitated demented or delirious patients #22: explain the risks, indications, alternatives and contraindications for Foley catheter use
Diagnostic/Treatment Challenges (& Opportunities) • Gradual decline in physiological reserve • Increased heterogeneity with aging – Genetic, lifestyle, environmental differences • Disease often presents at an earlier stage – Delirium with mild hypercalcemia – Urinary retention with mild BPH – Treatment may be simple – Drug side effects at lower doses Resnick NM. Marcantonio ER. How should clinical care of the aged differ? Lancet 1997; 350: 1157 -58
Diagnostic/Treatment Challenges (2) • Symptoms occur earlier, but patients delay care – Perceptions of “normal” aging • Disease presentation depends on most vulnerable organ system (weakest link) – How is UTI associated with delirium? • Abnormal findings in a younger person may be common (and not harmful) in older adults – Bacteriuria
Diagnostic/Treatment Challenges (3) • Symptoms from multiple cause (inverse Occum’s razor) – Syncope • Multiple homeostatic mechanisms compromised, multiple abnormalities amenable to treatment – Falls
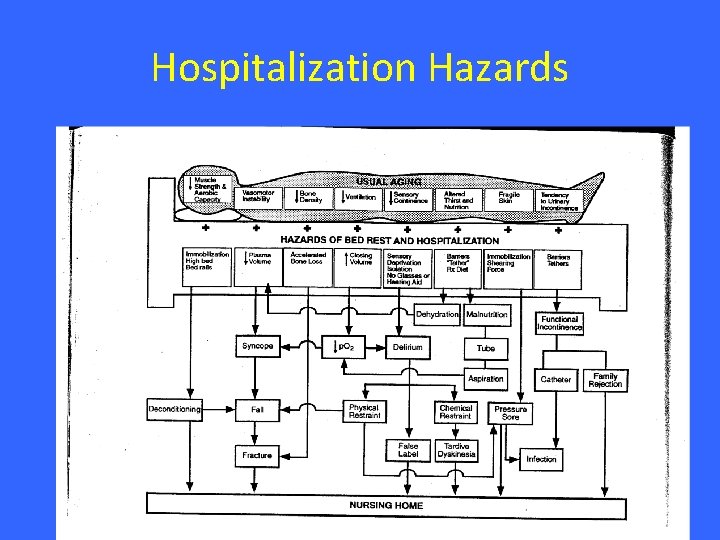
Hospitalization Hazards

Hospitalization Risks • Delirium • Infection – UTI, pneumonia, C diff • Pressure ulcers • Malnutrition • Nursing home placement
Nursing Homes • ? live permanently: > 50% hospitalized older adults “very unwilling” or “rather die” Mattimore TJ, JAGS 1997 • Infrequent physician visits • Decreased likelihood of returning to community within 30 days if discharged from hospital with delirium Marcantonio ER et al, JAGS 2005
Mrs. W History • 89 year old woman transferred from AL facility • CC: fever, lethargy (very quiet, not usual self) • HPI: Few days of diarrhea, cough, weakness, decreased PO intake, left hip pain • PMH: CRI, HTN, DM, CAD, h/o CVA • Meds: insulin, furosemide, atenolol, asa, plavix, amlodipine, doxazocin, isordil, nexium, calcium, nephrovite, fe, vitamin d, shohl’s • ROS: headache, nausea & emesis x 1, dizziness x 1 month
Mrs. W Exam • • • General: lethargic, difficult to engage VS: T 38, 142/90, HR 92, O 2 sat 94% ra Lungs: bibasilar crackles Heart: RRR, S 1/S 2, II/VI SEM at USB Ext: pain with external rotation left leg Neuro: difficulty following commands
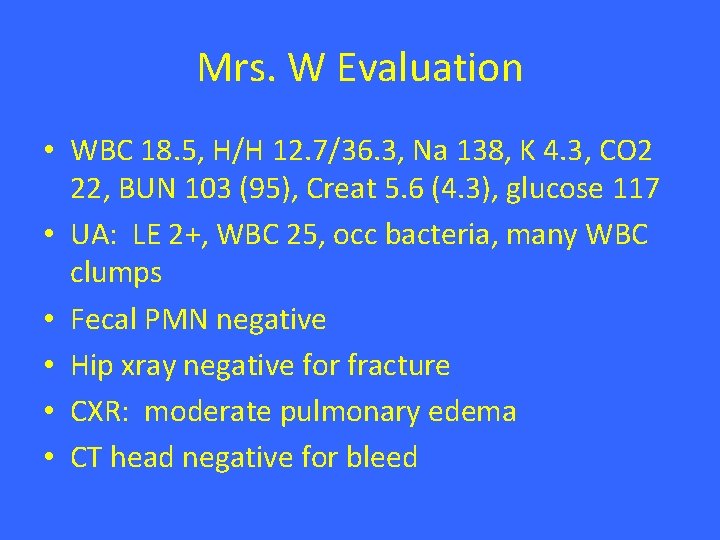
Mrs. W Evaluation • WBC 18. 5, H/H 12. 7/36. 3, Na 138, K 4. 3, CO 2 22, BUN 103 (95), Creat 5. 6 (4. 3), glucose 117 • UA: LE 2+, WBC 25, occ bacteria, many WBC clumps • Fecal PMN negative • Hip xray negative for fracture • CXR: moderate pulmonary edema • CT head negative for bleed
DDX • Impression: • 89 year old woman with CRI, DM, CAD admitted with fever, lethargy and associated delirium. Most likely etiologies include… • DDX:
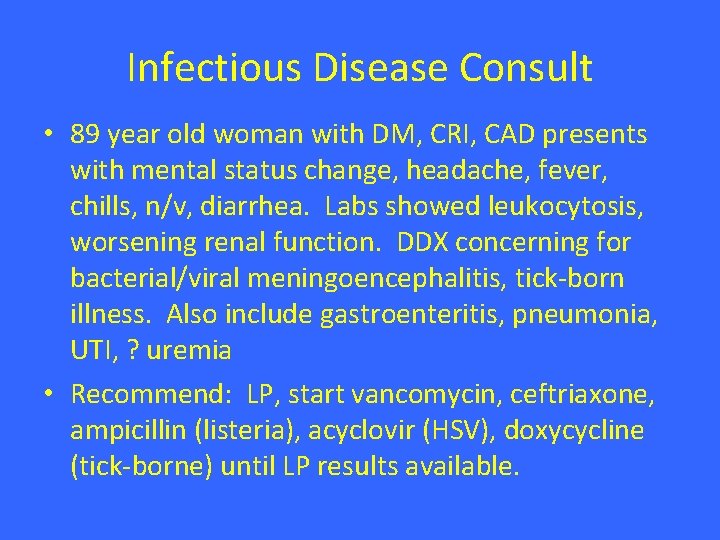
Infectious Disease Consult • 89 year old woman with DM, CRI, CAD presents with mental status change, headache, fever, chills, n/v, diarrhea. Labs showed leukocytosis, worsening renal function. DDX concerning for bacterial/viral meningoencephalitis, tick-born illness. Also include gastroenteritis, pneumonia, UTI, ? uremia • Recommend: LP, start vancomycin, ceftriaxone, ampicillin (listeria), acyclovir (HSV), doxycycline (tick-borne) until LP results available.
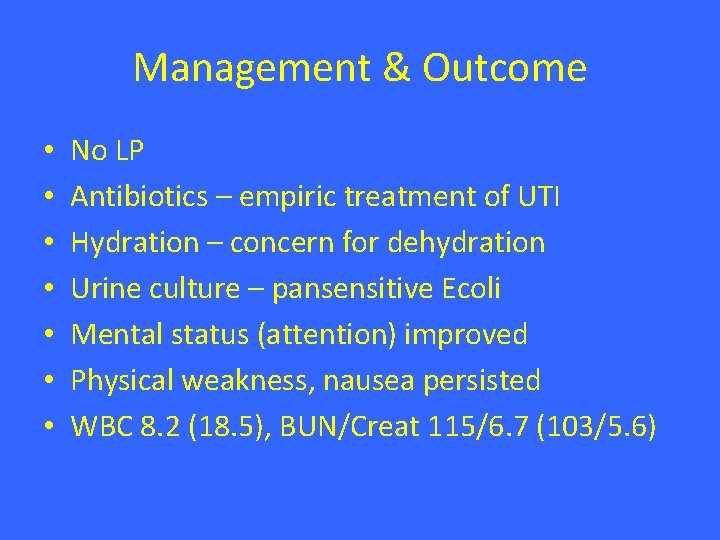
Management & Outcome • • No LP Antibiotics – empiric treatment of UTI Hydration – concern for dehydration Urine culture – pansensitive Ecoli Mental status (attention) improved Physical weakness, nausea persisted WBC 8. 2 (18. 5), BUN/Creat 115/6. 7 (103/5. 6)
Delirium • • • Spectrum: hypoactive – agitated Common Costly Morbidity & mortality Preventable
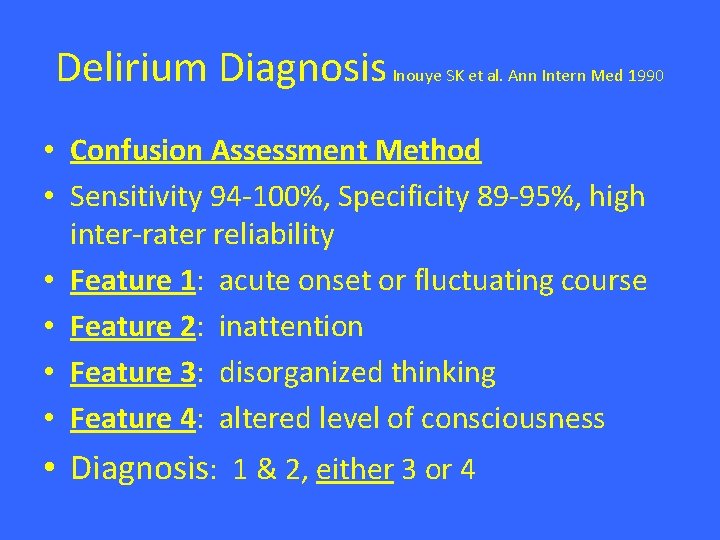
Delirium Diagnosis Inouye SK et al. Ann Intern Med 1990 • Confusion Assessment Method • Sensitivity 94 -100%, Specificity 89 -95%, high inter-rater reliability • Feature 1: acute onset or fluctuating course • Feature 2: inattention • Feature 3: disorganized thinking • Feature 4: altered level of consciousness • Diagnosis: 1 & 2, either 3 or 4
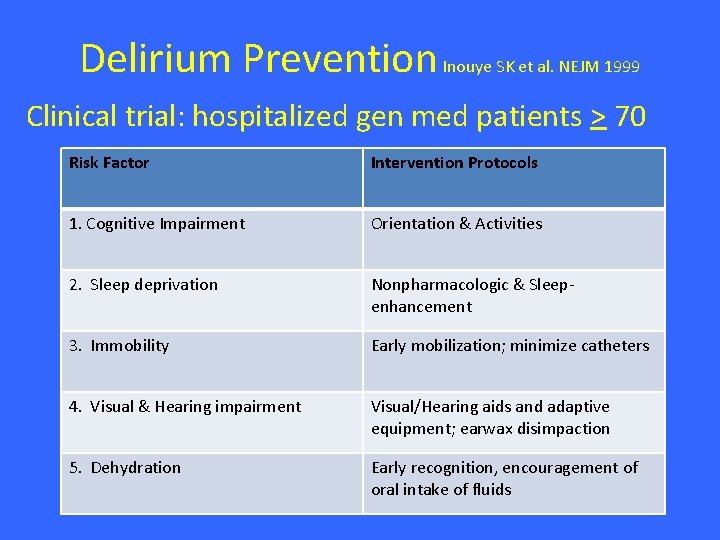
Delirium Prevention Inouye SK et al. NEJM 1999 Clinical trial: hospitalized gen med patients > 70 Risk Factor Intervention Protocols 1. Cognitive Impairment Orientation & Activities 2. Sleep deprivation Nonpharmacologic & Sleepenhancement 3. Immobility Early mobilization; minimize catheters 4. Visual & Hearing impairment Visual/Hearing aids and adaptive equipment; earwax disimpaction 5. Dehydration Early recognition, encouragement of oral intake of fluids
Delirium Prevention Trial Outcomes Intervention group: 10% Usual-care group: 15% OR 0. 60 (0. 39 -0. 92) Intervention group: fewer total number of days with delirium & total number of episodes • No significant differences in delirium severity • 87%: overall rate of intervention adherence • •

Prevention Trial Dissemination http: //elderlife. med. yale. edu
Delirium Management • Treat the underlying contributing conditions • Address risk factors – Foley, telemetry, nasal cannula • • • Involve family Consider sitter Does the patient need to remain in bed? How important/urgent is the evaluation/tx? Medication options
Delirium Medications • No medications with FDA approval, evaluated in randomized trials • Geriatrics prescribing principle: start low, go slow • Benefits/side effect profile of atypical antipsychotics similar to first generation agents • Haloperidol (advantage PO/IM/IV): 0. 25 -0. 5 mg, max 1 mg/day, prolonged QT interval • Risperidone: 0. 25 -0. 5 mg BID, prolonged QT, increased mortality risk in dementia
Indwelling Urinary Catheters • Risks: infection, bladder weakness, hematuria, discomfort, immobility (1 point restraint S et al. Ann Intern Med 2002 • Indications: retention (+/-), comfort, I/O monitoring (+/-), pressure ulcer management )+/-) • Alternatives: timed voiding with assistance, incontinence care, condom catheters, • Nonpayment for catheter associated UTI Wald HL. Kramer AM. JAMA 2007.
Other Topics • • • Tube feeding in dementia Finucane TE et al. JAMA 1999 Pressure ulcer recognition and prevention Syncope Mendu ML. Arch Intern Med 2009 Goals of care communication Winzelberg GS et al. JAGS 2005 Family communication End of life care – Symptom management – Care options
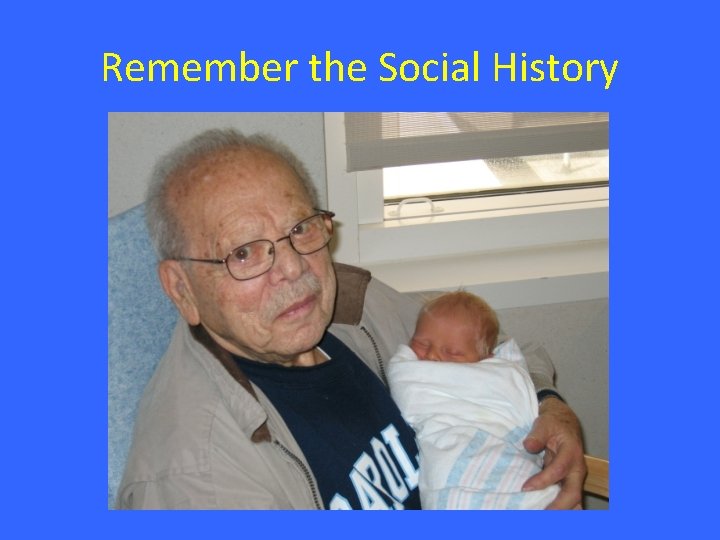
Remember the Social History

- Slides: 32