GERD and its supraesophageal or extraesophageal manafestations Yousif



- Slides: 59
GERD and its supraesophageal or extraesophageal manafestations Yousif A. Qari Ass. prof, Consultant Gastroenterologist KAUH
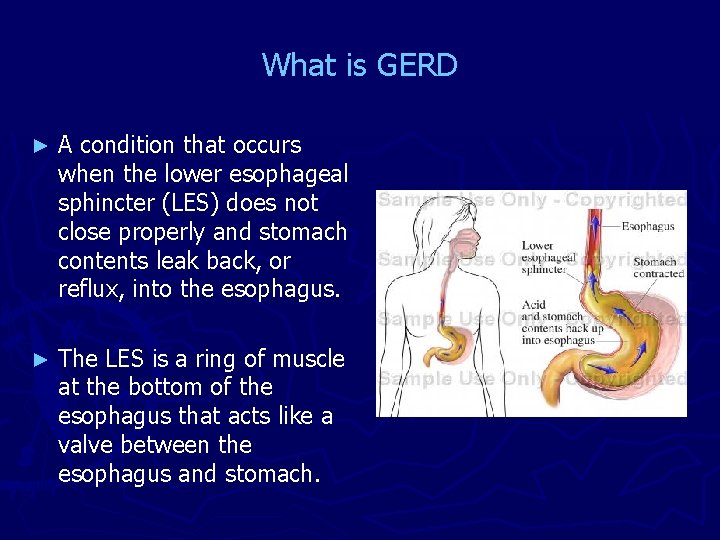
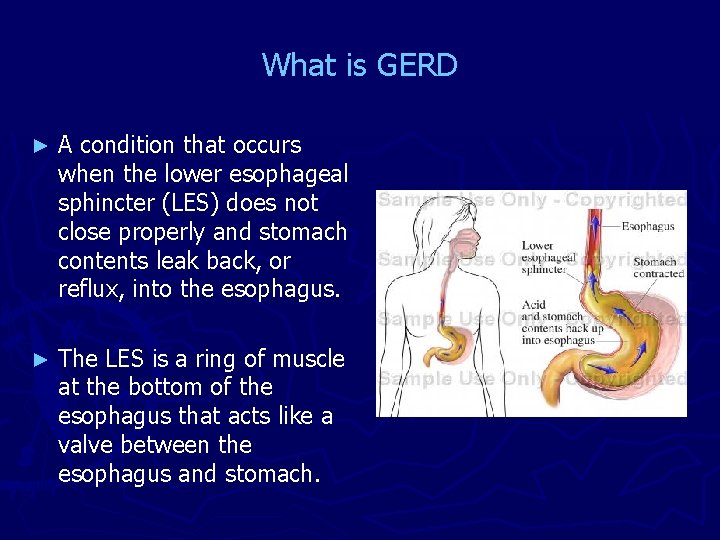
What is GERD ► A condition that occurs when the lower esophageal sphincter (LES) does not close properly and stomach contents leak back, or reflux, into the esophagus. ► The LES is a ring of muscle at the bottom of the esophagus that acts like a valve between the esophagus and stomach.
Prevalence of GERD Approximately 20% of adults have frequent "classic" symptoms of gastroesophageal reflux (GER): ► Heartburn ► Regurgitation.
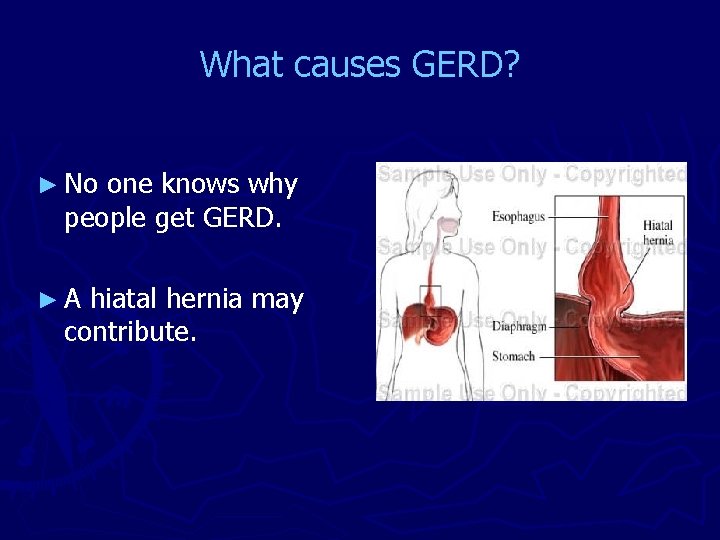
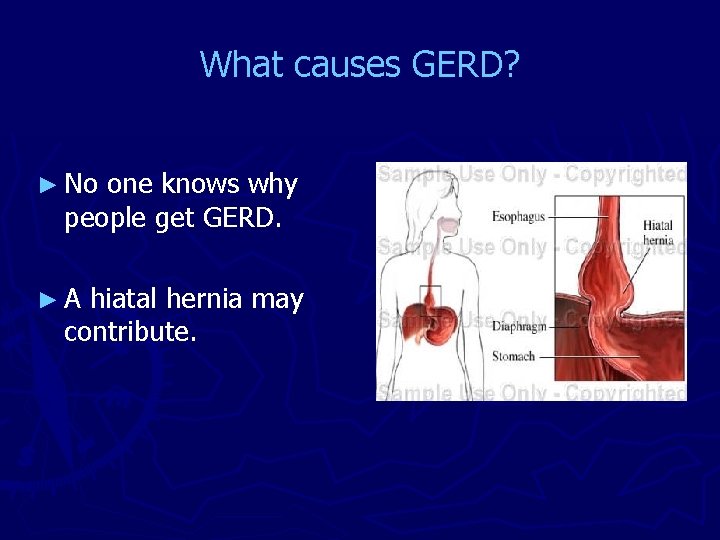
What causes GERD? ► No one knows why people get GERD. ►A hiatal hernia may contribute.
Other factors that may contribute to GERD ► Alcohol use ► Overweight ► Pregnancy ► Smoking
Certain foods can be associated with reflux events Citrus fruits ► Chocolate ► Drinks with caffeine ► Fatty and fried foods ► Garlic and onions ► Mint flavorings ► Spicy foods ► Tomato-based foods, like spaghetti sauce, chili, and pizza ►
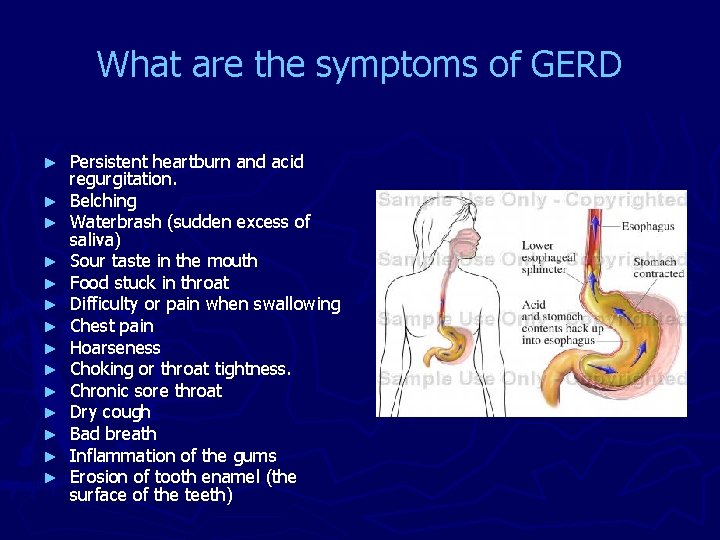
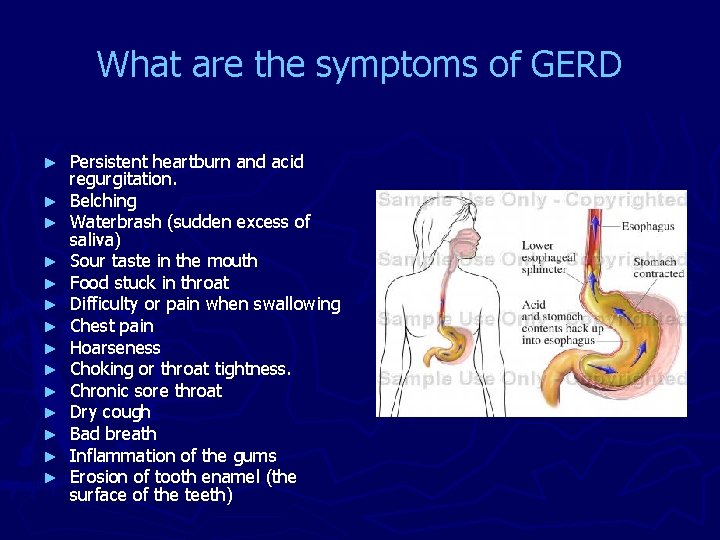
What are the symptoms of GERD ► ► ► ► Persistent heartburn and acid regurgitation. Belching Waterbrash (sudden excess of saliva) Sour taste in the mouth Food stuck in throat Difficulty or pain when swallowing Chest pain Hoarseness Choking or throat tightness. Chronic sore throat Dry cough Bad breath Inflammation of the gums Erosion of tooth enamel (the surface of the teeth)
How is GERD diagnosed? ► Review of symptoms and a complete physical examination, with Special attention to alarming symptoms. § Duration & severity of symptoms § Anemia § Dysphagia (Difficulty in swollowing) § Weight loss
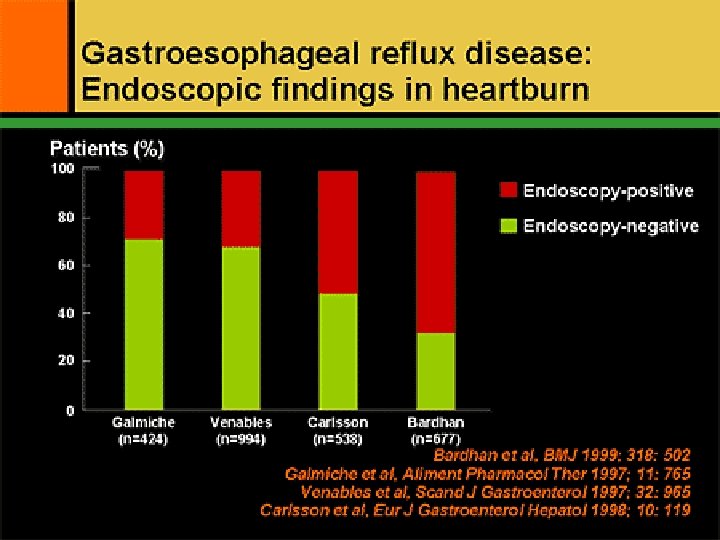
Diagnosis of supraesophageal Reflux 1. Heartburn and regurgitation many of these patients fail to demonstrate the typical symptoms of heartburn and regurgitation 2. The response of symptoms to an empirical trial of antireflux therapy 3. Ambulatory, esophageal p. H monitoring 4. Upper gastrointestinal endoscopy Most do not have esophagitis when looked at endoscopically.
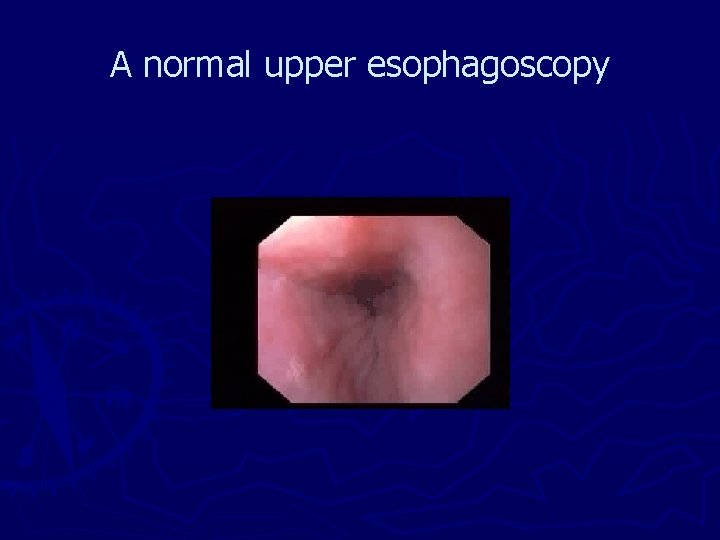
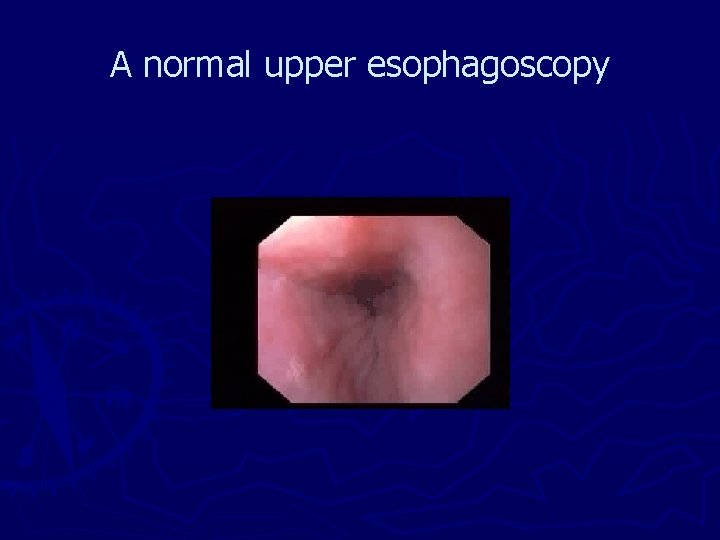
A normal upper esophagoscopy

The Los Angeles Classification System for the endoscopic assessment of reflux oesophagitis GRADE A: One or more mucosal breaks no longer than 5 mm, non of which extends between the tops of the mucosal folds
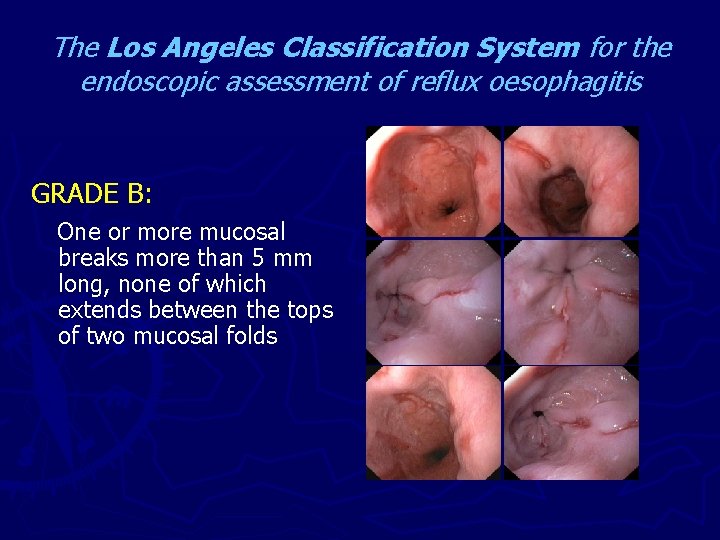
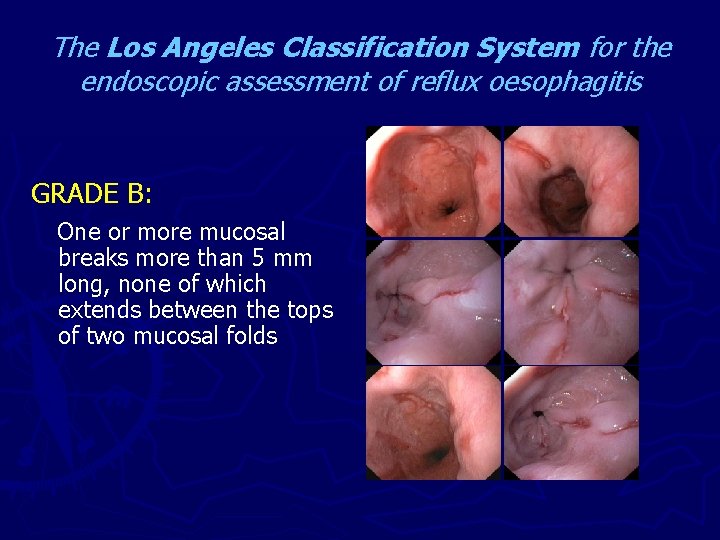
The Los Angeles Classification System for the endoscopic assessment of reflux oesophagitis GRADE B: One or more mucosal breaks more than 5 mm long, none of which extends between the tops of two mucosal folds
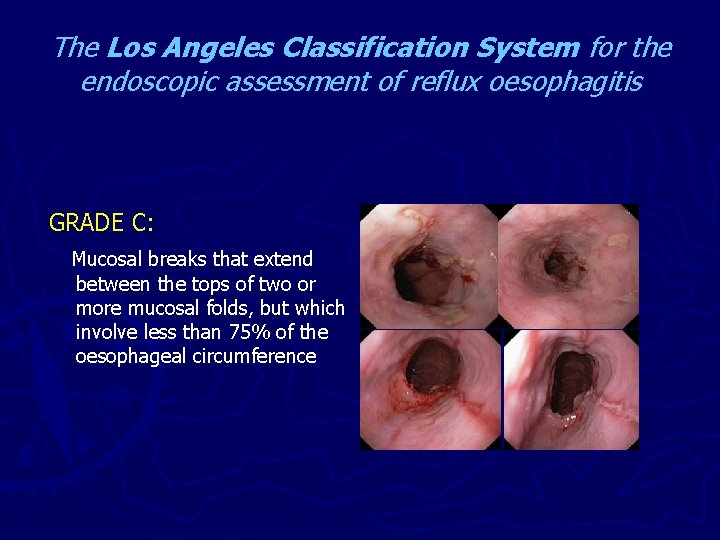
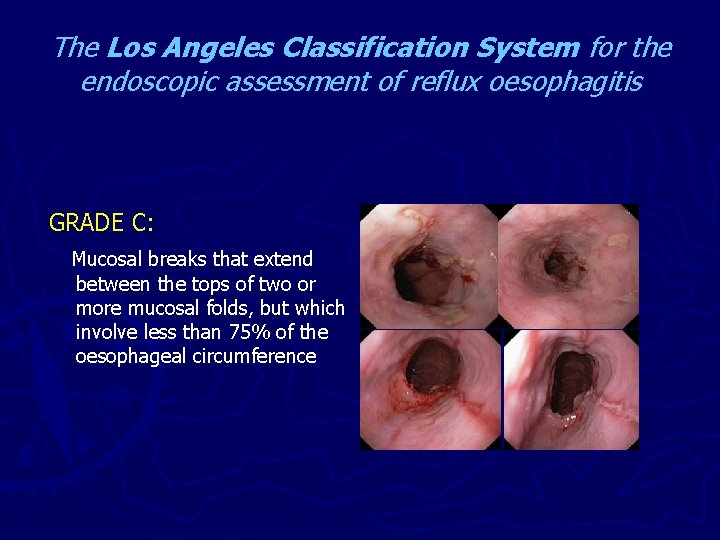
The Los Angeles Classification System for the endoscopic assessment of reflux oesophagitis GRADE C: Mucosal breaks that extend between the tops of two or more mucosal folds, but which involve less than 75% of the oesophageal circumference
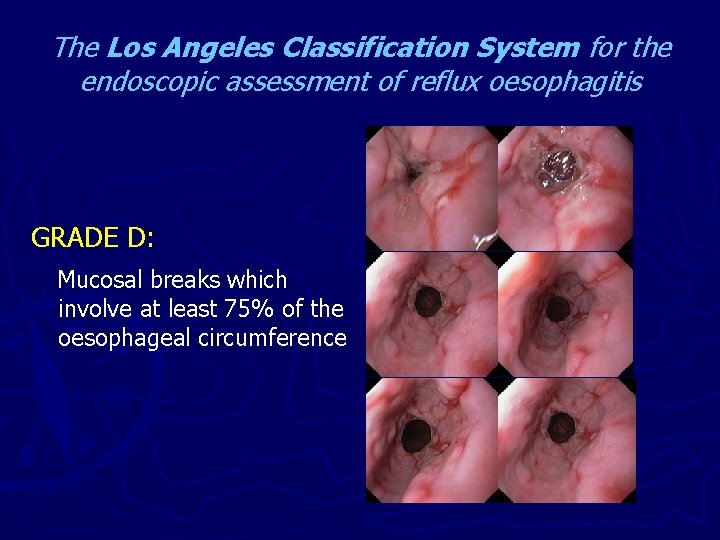
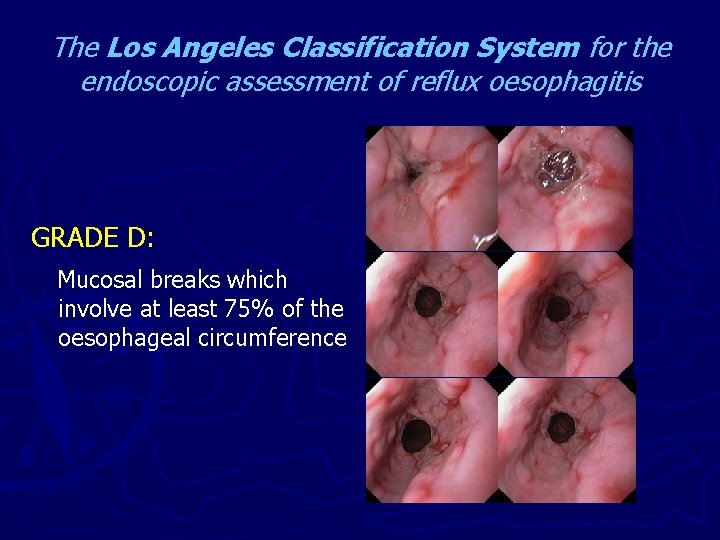
The Los Angeles Classification System for the endoscopic assessment of reflux oesophagitis GRADE D: Mucosal breaks which involve at least 75% of the oesophageal circumference
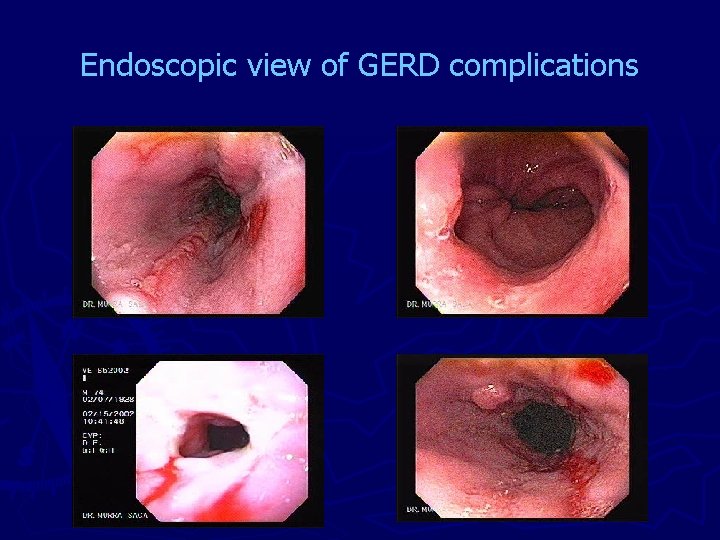
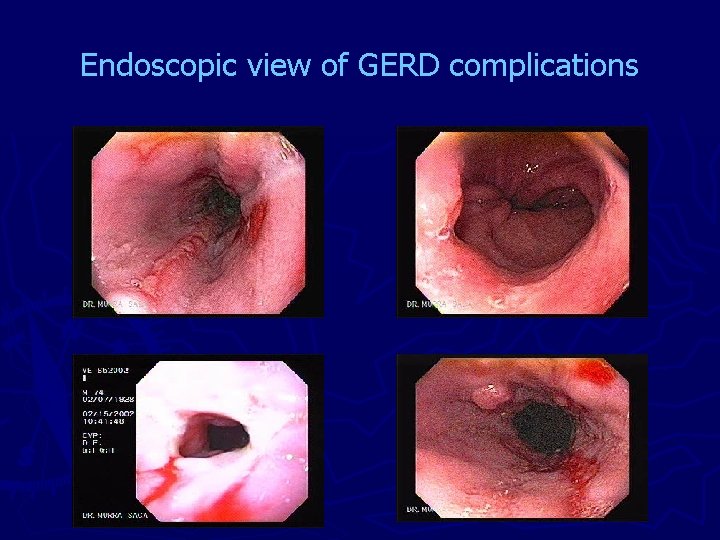
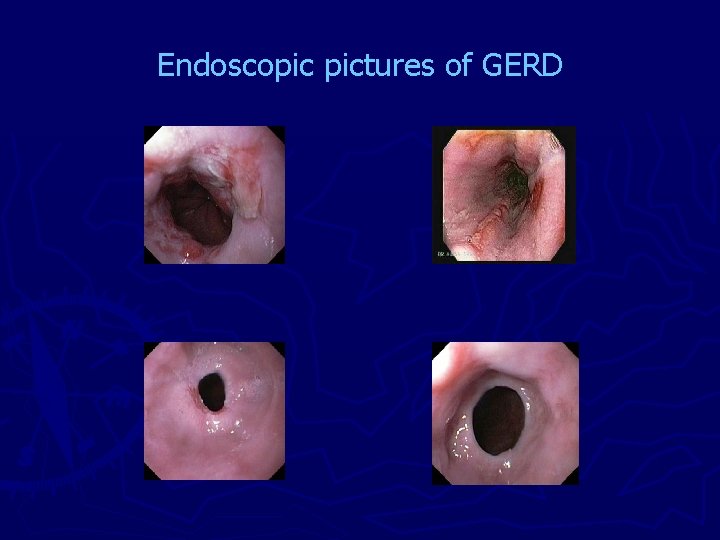
Endoscopic view of GERD complications
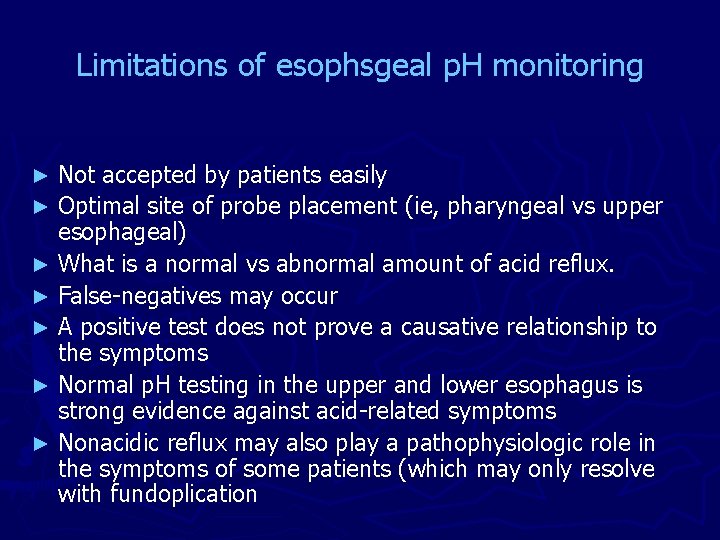
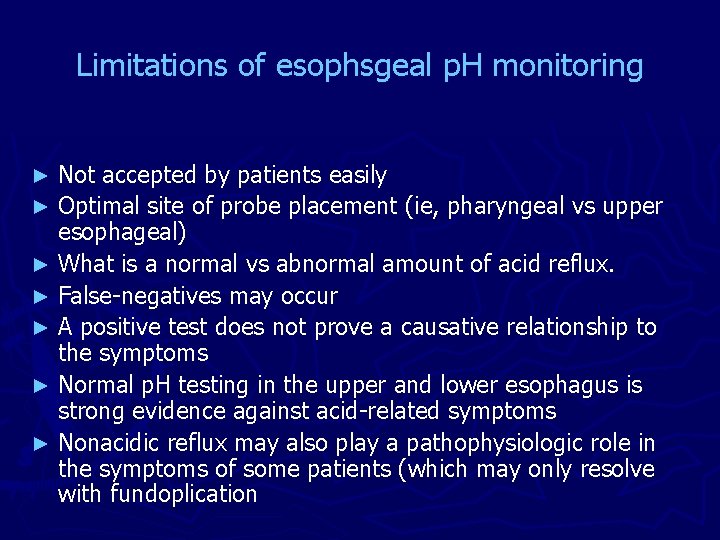
Limitations of esophsgeal p. H monitoring Not accepted by patients easily ► Optimal site of probe placement (ie, pharyngeal vs upper esophageal) ► What is a normal vs abnormal amount of acid reflux. ► False-negatives may occur ► A positive test does not prove a causative relationship to the symptoms ► Normal p. H testing in the upper and lower esophagus is strong evidence against acid-related symptoms ► Nonacidic reflux may also play a pathophysiologic role in the symptoms of some patients (which may only resolve with fundoplication ►
Catheter-Free p. H-Monitoring System BRAVO Catheter-Free ph Testing ► Bravo can be placed during endoscopy ► Allows 24 -hour or 48 -hour p. H monitoring to record more clinical data ► Patients maintain normal diet and routine activities ► Minimizes throat and nasal discomfort associated with transnasal catheters ► Transmits data to pager-sized reciever ► Uploads easily to p. H analysis software 1. C, De. Meester T, Peters J, et al. Clinical evaluation of the BRAVOTM probe - a catheter-free ambulatory esophageal p. H monitoring system. Gastroenterology. 2001; 120: A-35. [Abstract #177]
Catheter-Free p. H-Monitoring System ► In a controlled study of only 7 asymptomatic subjects § the small amounts of measured acid reflux appeared comparable to that obtained with the conventional p. H probe. ► Additional head-to-head trials of the micro-probe and conventional catheter systems are needed in symptomatic patients to determine the accuracy, reliability, and patient acceptance of this technique.
How is GERD treated? ► Lifestyle Changes ► Medications ► Surgery ► Endoscopic options
Lifestyle Changes If you smoke, stop. ► Do not drink alcohol. ► Lose weight if needed. ► Eat small meals. ► Wear loose-fitting clothes. ► Avoid lying down for 3 hours after a meal. ► Raise the head of your bed 6 to 8 inches by putting blocks of wood under the bedposts-just using extra pillows will not help. ►

Medications ► Antacids: § § Maalox, Mylanta Pepto-Bismol Rolaids ► Foaming agents ► H 2 blockers § Gaviscon § § Cimetidine (Tagamet ) Famotidine (Pepcid) Nizatidine (Axid) Ranitidine (Zantac 75) Magnesium salt can lead to diarrhea, and aluminum salts can cause constipation

Medications ► Proton pump inhibitors § § § ► omeprazole (Prilosec) lansoprazole (Prevacid) pantoprazole (Protonix) rabeprazole (Aciphex) esomeprazole (Nexium) Prokinetics § § § Bethanechol (Urecholine) Metoclopramide (Primpran) Domperidone (Motilium)
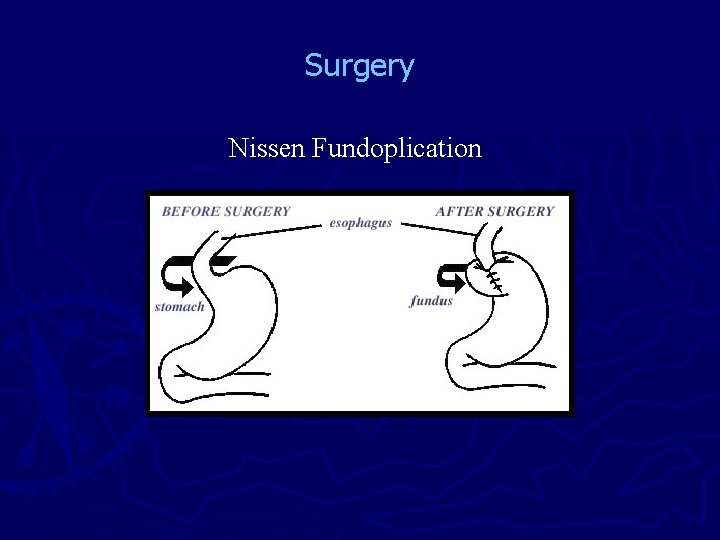
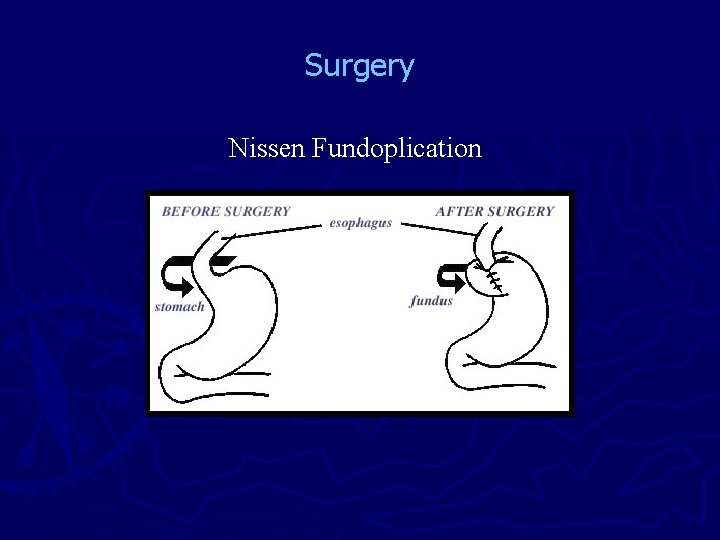
Surgery Nissen Fundoplication
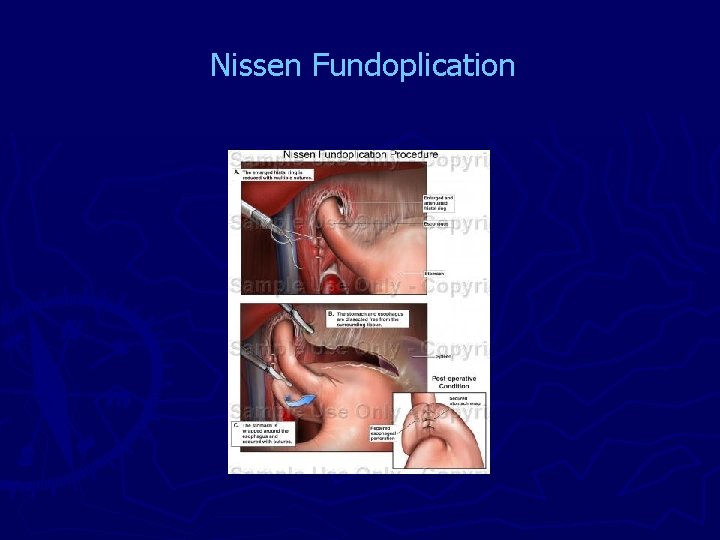
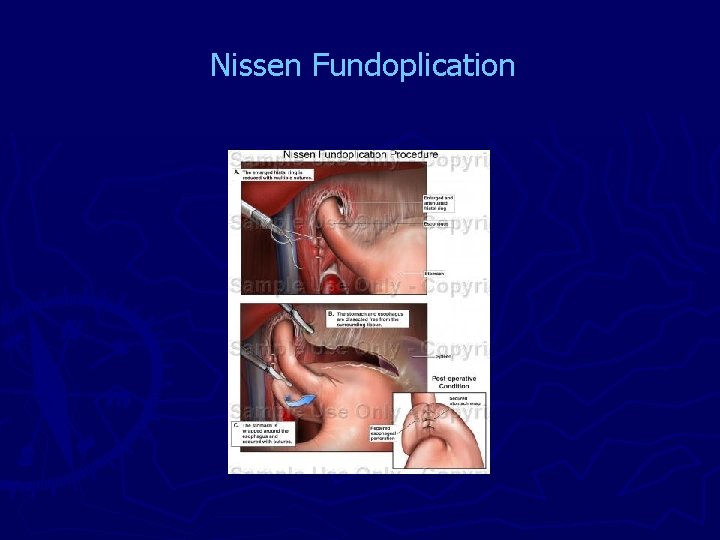
Nissen Fundoplication
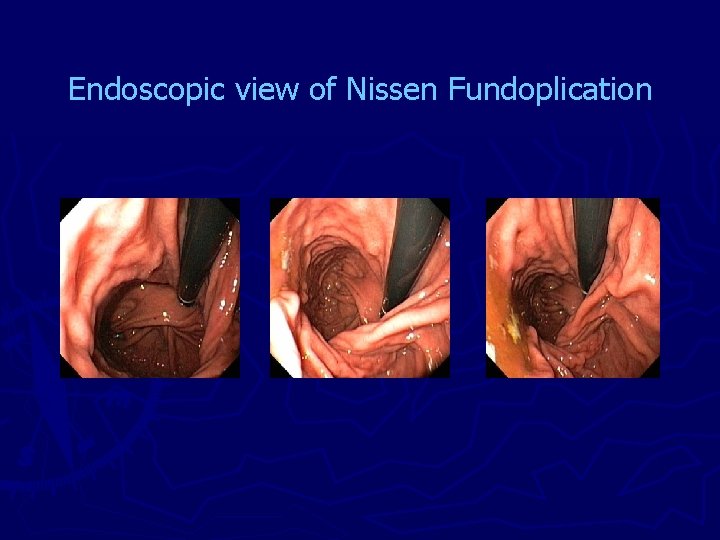
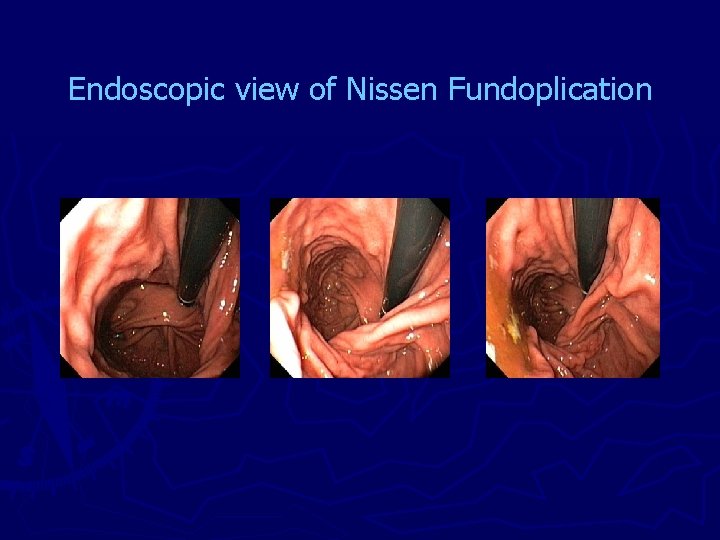
Endoscopic view of Nissen Fundoplication
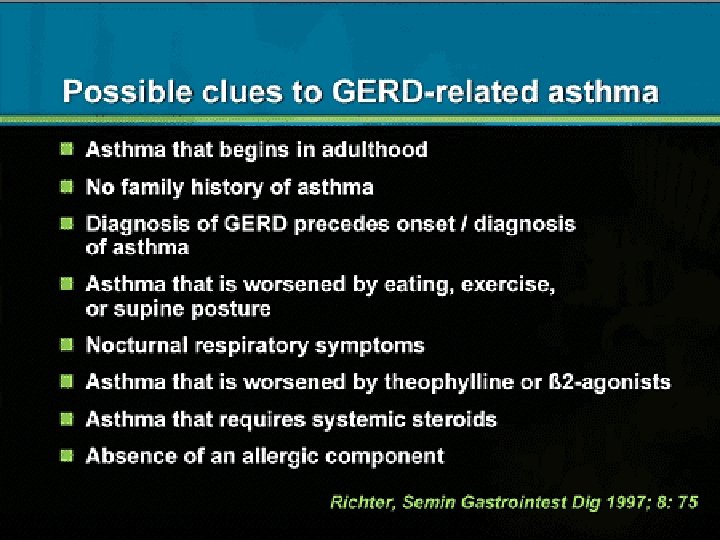
Long-term complications of GERD? Inflammation of the esophagus ► Bleeding or ulcers ► strictures ► Barrett's esophagus and adenoarcinoma ► Supraesphageal manafestations ► § § Asthma chronic cough pulmonary fibrosis ENT manafestations
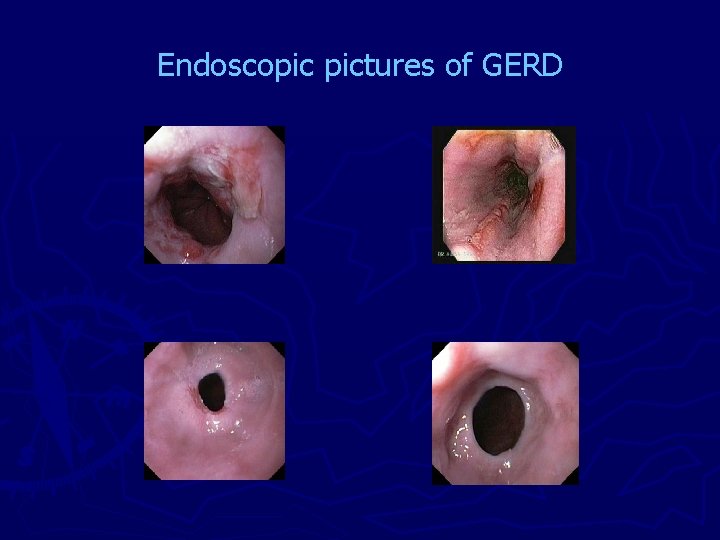
Endoscopic pictures of GERD
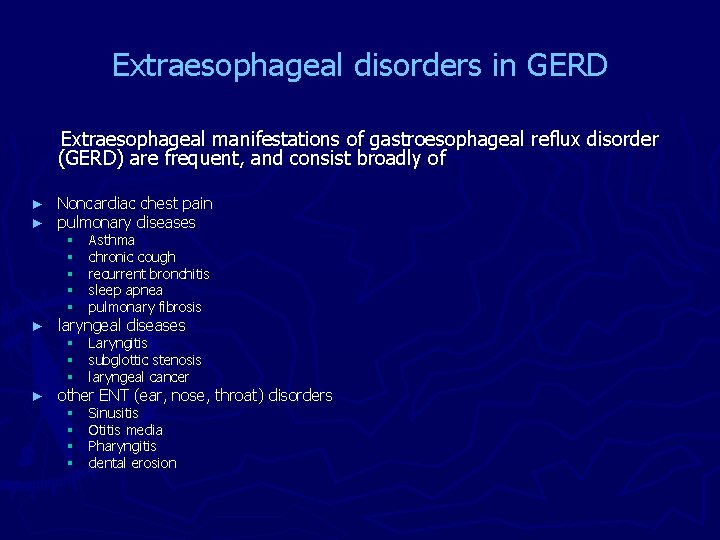
Extraesophageal disorders in GERD Extraesophageal manifestations of gastroesophageal reflux disorder (GERD) are frequent, and consist broadly of ► ► Noncardiac chest pain pulmonary diseases § § § Asthma chronic cough recurrent bronchitis sleep apnea pulmonary fibrosis § § § Laryngitis subglottic stenosis laryngeal cancer § § Sinusitis Otitis media Pharyngitis dental erosion laryngeal diseases other ENT (ear, nose, throat) disorders
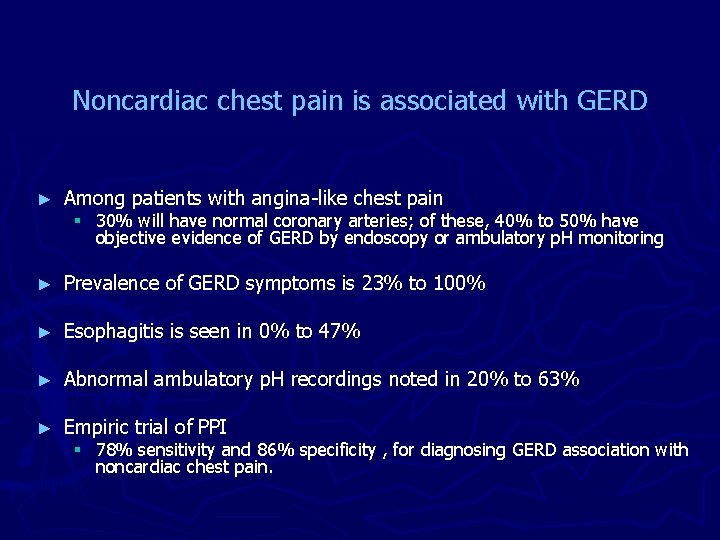
Noncardiac chest pain is associated with GERD ► Among patients with angina-like chest pain ► Prevalence of GERD symptoms is 23% to 100% ► Esophagitis is seen in 0% to 47% ► Abnormal ambulatory p. H recordings noted in 20% to 63% ► Empiric trial of PPI § 30% will have normal coronary arteries; of these, 40% to 50% have objective evidence of GERD by endoscopy or ambulatory p. H monitoring § 78% sensitivity and 86% specificity , for diagnosing GERD association with noncardiac chest pain.
GERD and Chronic Cough ► Direct mucosal injury and/or ► Triggering vagally mediated mechanisms § Increased airway secretions § Bronchospasm
Nonacid Gastroesophageal Reflux ► Reflux of gastric contents § Food § Nonacidic material. ► Symptoms that fail to respond to aggressive therapy with proton-pump inhibitors may still improve after antireflux surgery ► Traditional p. H testing (which detects reductions in intraesophageal p. H from a baseline of p. H 6 -7) cannot detect nonacidic reflux.
Nonacid Gastroesophageal Reflux ► Nonacidic reflux was seen in both normal (healthy controls) subjects and GERD patients ► Measured by multichannel intraluminal impedance (MII) monitoring ► Accounted for one third of all reflux events ► Occurred more commonly after meals and in recumbency ► Only 4% of nonacidic reflux events were due to bile reflux ► Three fourths of bile reflux episodes occurred in conjunction with acid reflux ► Compared with acid reflux events, nonacidic reflux typically did not extend as far proximally and was cleared more quickly from the esophagus.
importance of nonacidic reflux ► The true importance of nonacidic reflux in the pathogenesis of both esophageal and extraesophageal symptoms remains to be established. ► may be a factor in: § Functional heartburn (ie, heartburn with normal esophageal p. H measurements) § Nonerosive reflux disorders § Extraesophageal disorders, whose symptoms persist despite aggressive proton-pump inhibitor therapy. ► MII may be used to test for nonacidic reflux
GERD and Chronic Cough The mechanisms remain controversial. § Microaspiration § Stimulation of a vagally mediated esophageal-bronchial reflex. That may also involve brainstem centers.
GERD and Chronic Cough ► Establishing a definite cause-and-effect relationship between GER and chronic cough is difficult. A normal esophageal p. H study argues against acid GER as a cause of chronic cough ► An abnormal p. H study does not prove that acid reflux is the cause of chronic cough. ► ► Only a minority of patients with proven GER have improvement of cough after proton-pump inhibitor therapy.
GERD and Chronic Cough Empirical trial of high-dose therapy with PPI § Uncontrolled trials ► 70% to 100% improvement § The only published placebo-controlled trial reported ► 35% response rate.
GERD and Chronic Cough 75 patients with chronic cough prospectively evaluated § GER symptoms in 72% § abnormal p. H testing in 56% (42 of 75) § 20/42 had minimal or no reflux symptoms. ► Omeprazole was given to a subset of patients (n = 55) with either GER symptoms and/or abnormal p. H testing. ► After 3 -6 months, significant improvement was noted 45% ► No symptom or p. H parameter was predictive of improvement. Garrigues V, Bastida G, Bau I, et al. Gastroenterology. 2001; 120: A-430. [Abstract #2195]
GERD and Chronic Cough Conclusions ► ambulatory esophageal p. H testing still is of limited utility in the evaluation of patients with chronic cough. ► A normal p. H study with a low SI (symptom index) , probably excludes acid-related cough, but a positive p. H study does not prove a causal relationship. ► Many clinicians may choose to treat all patients with chronic cough with an empirical trial of high-dose proton-pump inhibitors (eg, omeprazole 40 mg twice daily), even if symptoms of reflux are absent. ► Cough usually responds within 2 weeks of therapy. ► An empirical trial is more cost-effective than formal evaluation with manometry and p. H testing.
Laryngopharyngeal reflux ► 81% will have a normal-appearing esophagus ► ► ► 40% may have symptoms of heartburn Symptoms consistent with this diagnosis Dysphonia Globus sensation Throat clearing Halitosis Sore throat Cough. Hoarseness is a majer coplaint in 92% of patients with GERD-related laryngitis § > 50% of patients presenting to ENT specialists with hoarsness will have a component of GERD contributing to their symptoms § § § §
Reflux Laryngitis ► Posterior laryngitis at laryngoscopy is a typical finding of reflux laryngitis ► Niether laryngoscopic findings nor positive p. H studies have been found to be of predictive value in identifying patients likely to respond to proton-pump inhibitors. ► No agreement as to the optimal site of pharyngeal probe placement or normal values of esophagopharyngeal reflux (EPR). ► EPR is also is detected in up to 20% of normal controls.
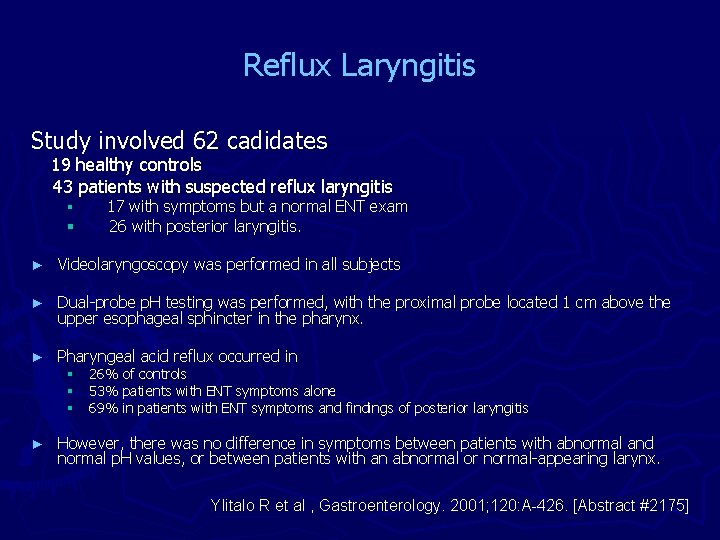
Reflux Laryngitis Study involved 62 cadidates 19 healthy controls 43 patients with suspected reflux laryngitis § § 17 with symptoms but a normal ENT exam 26 with posterior laryngitis. ► Videolaryngoscopy was performed in all subjects ► Dual-probe p. H testing was performed, with the proximal probe located 1 cm above the upper esophageal sphincter in the pharynx. ► Pharyngeal acid reflux occurred in § § § ► 26% of controls 53% patients with ENT symptoms alone 69% in patients with ENT symptoms and findings of posterior laryngitis However, there was no difference in symptoms between patients with abnormal and normal p. H values, or between patients with an abnormal or normal-appearing larynx. Ylitalo R et al , Gastroenterology. 2001; 120: A-426. [Abstract #2175]
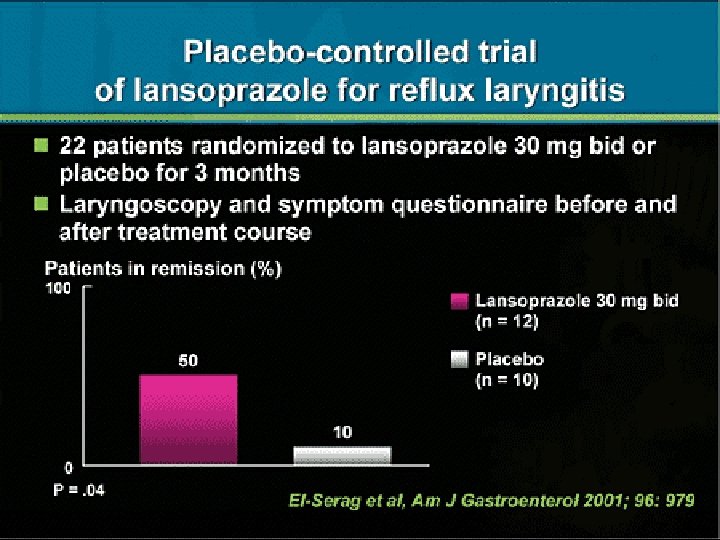
Reflux Laryngitis ► 49 patients with chronic ENT symptoms and abnormal laryngoscopic examination underwent a questionnaire and dual-probe esophageal (not pharyngeal) p. H testing. ► After initial evaluation, patients were treated in an uncontrolled fashion with either § high-dose proton-pump inhibitors § high-dose proton-pump-inhibitor therapy and bedtime ranitidine. § ► At 4 months, improvement was noted in 32 of 49 (65%) of patients treated with proton-pump inhibitors (with or without ranitidine). ► Symptoms, ENT findings, and p. H parameters were not predictive of response to proton-pump inhibitor therapy. 1. Vaezi M et al. Gastroenterology. 2001; 120: A-118. [Abstract #636]
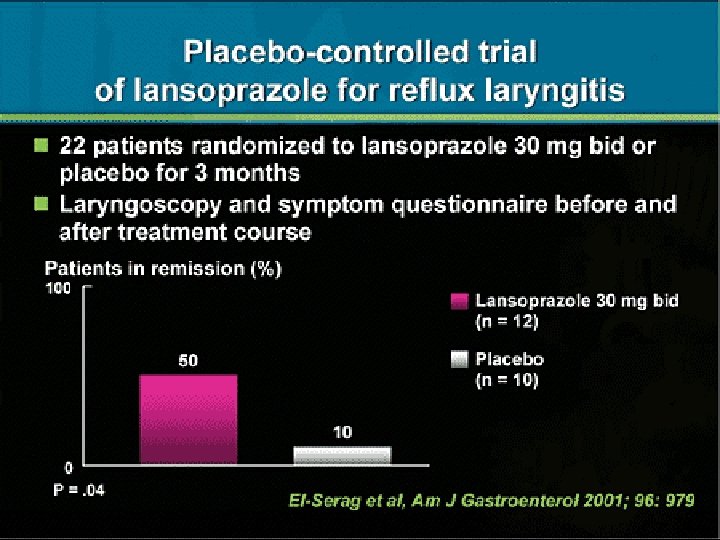
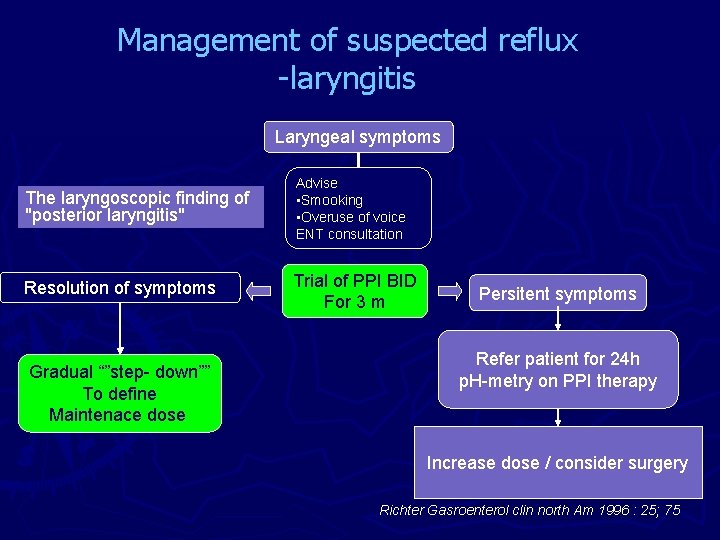
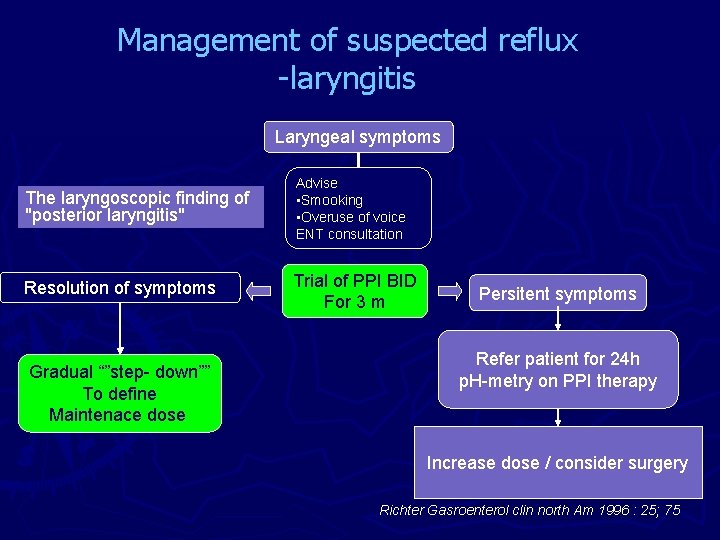
Management of suspected reflux -laryngitis Laryngeal symptoms The laryngoscopic finding of "posterior laryngitis" Advise • Smooking • Overuse of voice ENT consultation Resolution of symptoms Trial of PPI BID For 3 m Gradual “”step- down”” To define Maintenace dose Persitent symptoms Refer patient for 24 h p. H-metry on PPI therapy Increase dose / consider surgery Richter Gasroenterol clin north Am 1996 : 25; 75
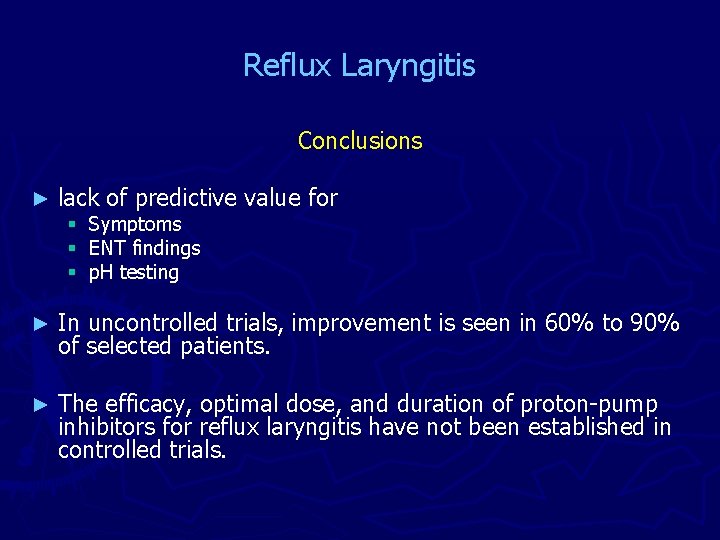
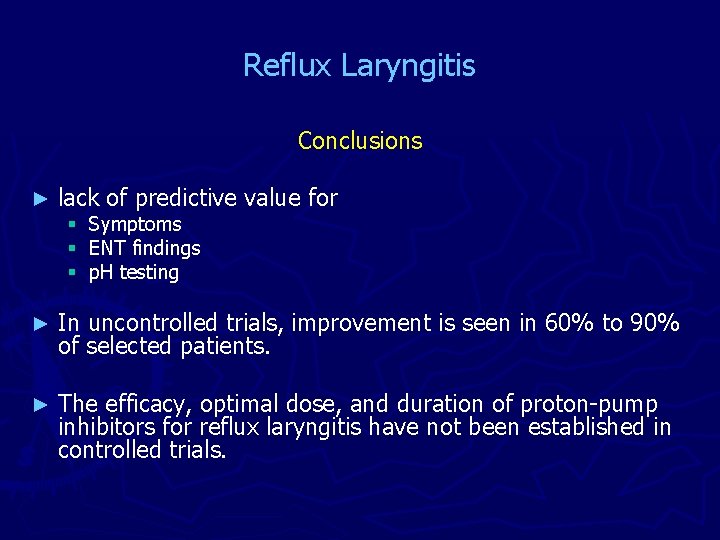
Reflux Laryngitis Conclusions ► lack of predictive value for ► In uncontrolled trials, improvement is seen in 60% to 90% of selected patients. ► The efficacy, optimal dose, and duration of proton-pump inhibitors for reflux laryngitis have not been established in controlled trials. § Symptoms § ENT findings § p. H testing
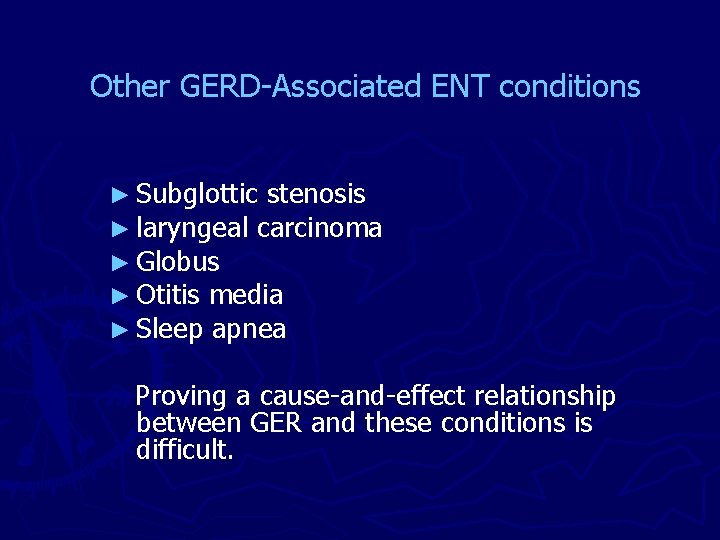
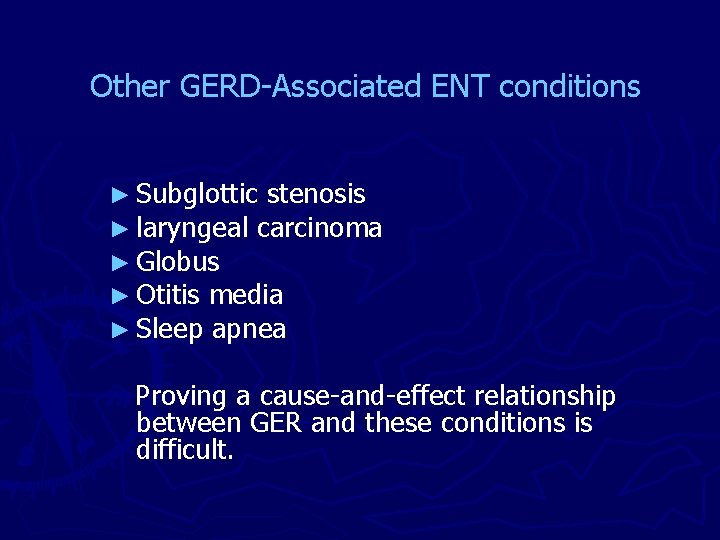
Other GERD-Associated ENT conditions ► Subglottic stenosis ► laryngeal carcinoma ► Globus ► Otitis media ► Sleep apnea Proving a cause-and-effect relationship between GER and these conditions is difficult.
GER in Otitis Media ► GER may cause chronic otitis media ► Reflux of gastric contents into the nasopharynx and middle ear might precipitate infections and/or chronic effusions. ► Assessed 50 middle-ear effusions for pepsin and pepsinogen levels using an enzyme-linked immunosorbent assay (ELISA). ► Pepsin and pepsinogen were detected in 41 of 50 effusions (82%) ► provocative observation, but proof of causation is lacking. 1. Tasker A, et al. Gastroenterology. 2001; 120: A-119. [Abstract #638]
GER and Sleep Apnea Obstructive sleep apnea (OSA) ► A condition that occurs as a result of the loss of normal pharyngeal muscle tone while sleeping, which allows the pharynx to collapse during inspiration. ► It is most common in: ► Strong association between OSA and GER was suggested § Obese § anatomically narrowed upper airways due to macroglossia, micrognathia § redundant pharyngeal or tonsillar soft tissue.
GER and Sleep Apnea 101 patients undergoing sleep studies for suspected OSA were evaluated for symptoms of GER § Sleep apnea was diagnosed in 71 of 101 patients § GER symptoms: ► 50% in patients with OSA ► 33% in patients without OSA. § GER symptoms were not related to the severity of OSA. Guda N, et al. Gastroenterology. 2001; 120: A-429. [Abstract #2190]
GER and Sleep Apnea Coclusions ► Observations so far do not prove symptom causality. ► Patients with OSA may be predisposed to GER § § § Obesity sedentary lifestyle alcohol use smoking. Obstructed breathing patterns (with negative intrathoracic pressure) also may predispose to GER ► A controlled trial of GER therapy in patients with OSA is needed. ► Patients with OSA should be assessed for GER symptoms pre- and post-OSA treatment.
Coclusions ► Gastroesophageal reflux is extremely common and may manifest with typical and atypical symptoms. ► At present it is extremely difficult to establish a definite diagnosis of extraesophageal GERD. ► Typical esophageal symptoms (heartburn, regurgitation) may be absent in a large number of patients. ► Neither the type of ENT symptoms nor the ENT findings are of predictive value in determining underlying GER.
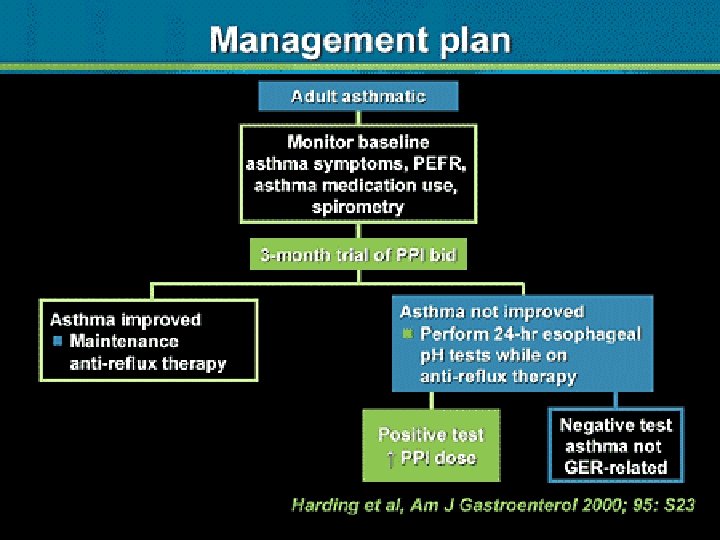
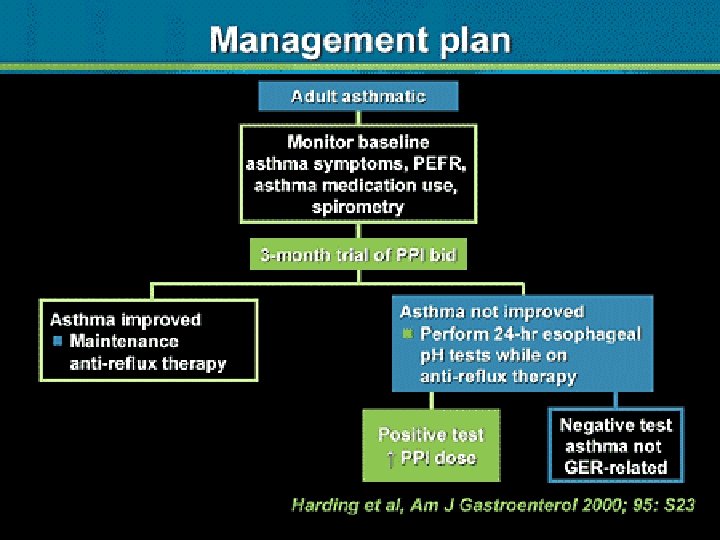
Coclusions ► Although interesting new modalities for reflux testing are available (capsule p. H monitoring, impedance testing) it remains to be seen whether these modalities improve diagnostic accuracy ► Currently, the most cost-effective approach for most patients with suspected reflux-related symptoms is a trial of a high-dose protonpump inhibitor for 3 monthes. ► p. H testing reserved to confirm adequate acid suppression in those with refractory symptoms. ► Although improvement in cough symptoms may be evident within 2 weeks of treatment, improvement in other ENT disorders may require 3 or more months of therapy. ► The place of Fundoplication is yet to be defined
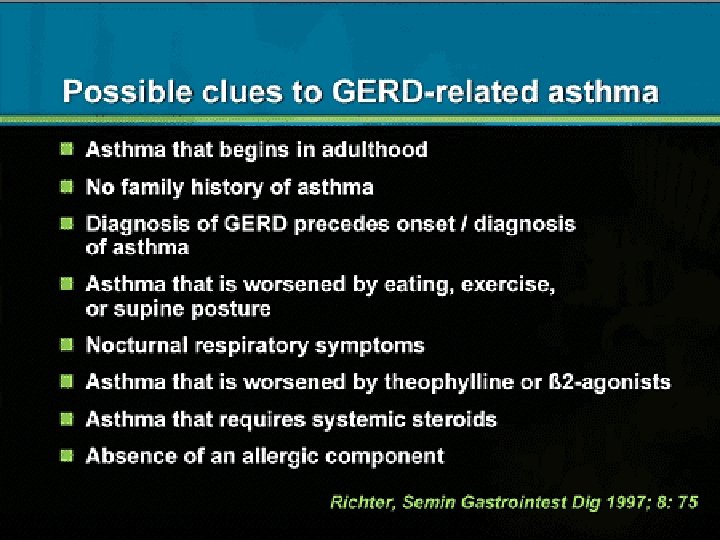
Diagnosis ► The majority of patients with extraesophageal manifestations of GER do not have the classic symptoms of heartburn or regurgitation ► less than 30% have endoscopic evidence of reflux esophagitis ► Twenty-four-hour p. H monitoring has been commonly used to look for evidence of acid reflux into the lower esophagus, upper esophagus, and pharynx. However, this test is not comfortable for most patients
GER and Sleep Apnea 41 consecutive patients with suspected OSA undergoing sleep exams were prospectively evaluated with a GERD symptom questionnaire. § 22/41 enrolled patients, reported heartburn or acid regurgitation. § 17/22 patients with heartburn reported that this symptom awakened them at night. § Regression analysis suggested that GER severity was correlated to the apnea-hypoventilation index.