Genetic predisposition to gastric cancer AnneMarie Gerdes Klinisk



- Slides: 14
Genetic predisposition to gastric cancer Anne-Marie Gerdes Klinisk Genetisk Klinik
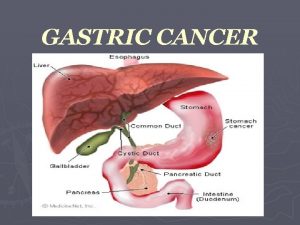
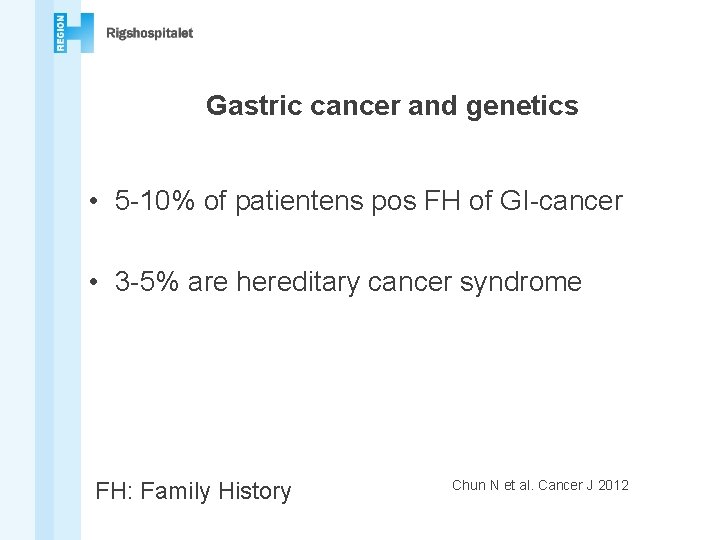
Gastric cancer and genetics • 5 -10% of patientens pos FH of GI-cancer • 3 -5% are hereditary cancer syndrome FH: Family History Chun N et al. Cancer J 2012
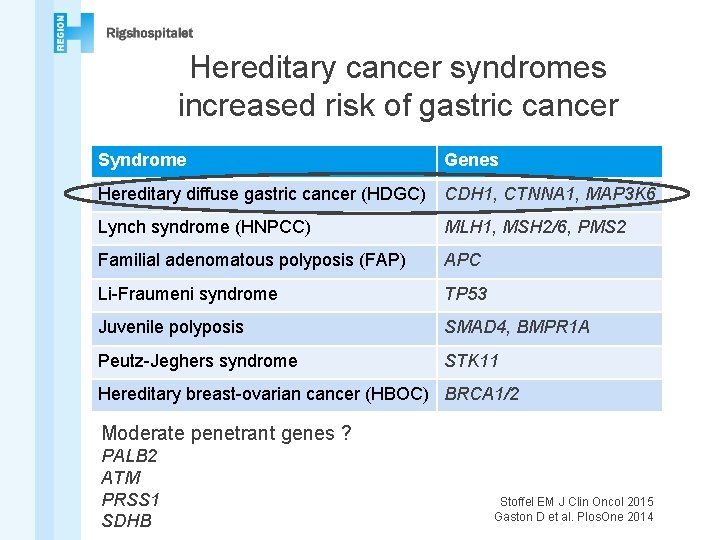
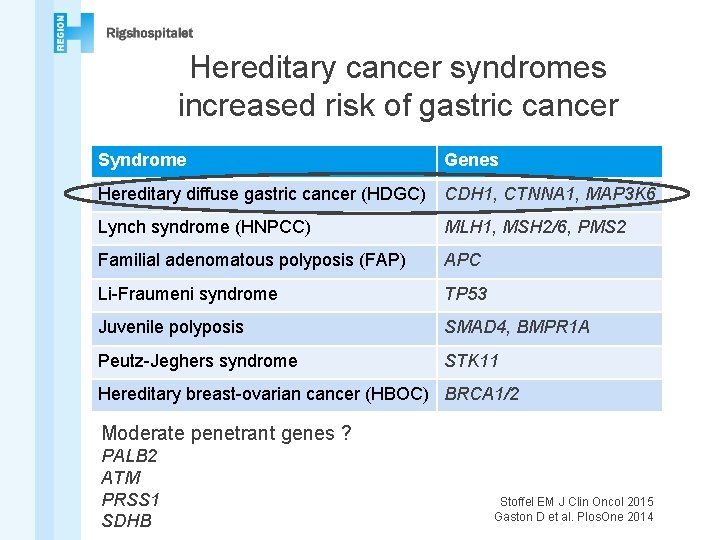
Hereditary cancer syndromes increased risk of gastric cancer Syndrome Genes Hereditary diffuse gastric cancer (HDGC) CDH 1, CTNNA 1, MAP 3 K 6 Lynch syndrome (HNPCC) MLH 1, MSH 2/6, PMS 2 Familial adenomatous polyposis (FAP) APC Li-Fraumeni syndrome TP 53 Juvenile polyposis SMAD 4, BMPR 1 A Peutz-Jeghers syndrome STK 11 Hereditary breast-ovarian cancer (HBOC) BRCA 1/2 Moderate penetrant genes ? PALB 2 ATM PRSS 1 SDHB Stoffel EM J Clin Oncol 2015 Gaston D et al. Plos. One 2014

2. hit Tumor cell other mutations
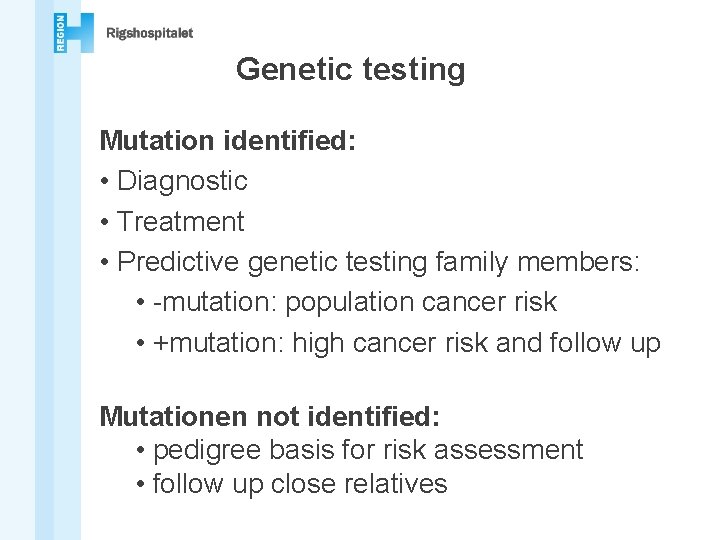
Genetic testing Mutation identified: • Diagnostic • Treatment • Predictive genetic testing family members: • -mutation: population cancer risk • +mutation: high cancer risk and follow up Mutationen not identified: • pedigree basis for risk assessment • follow up close relatives
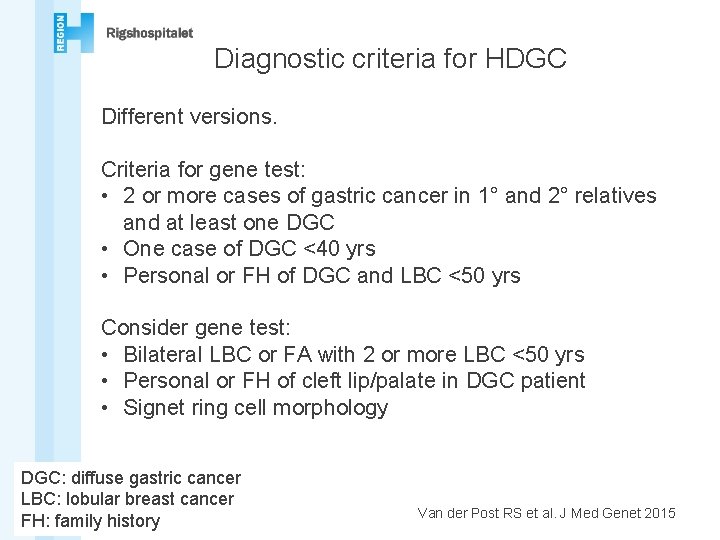
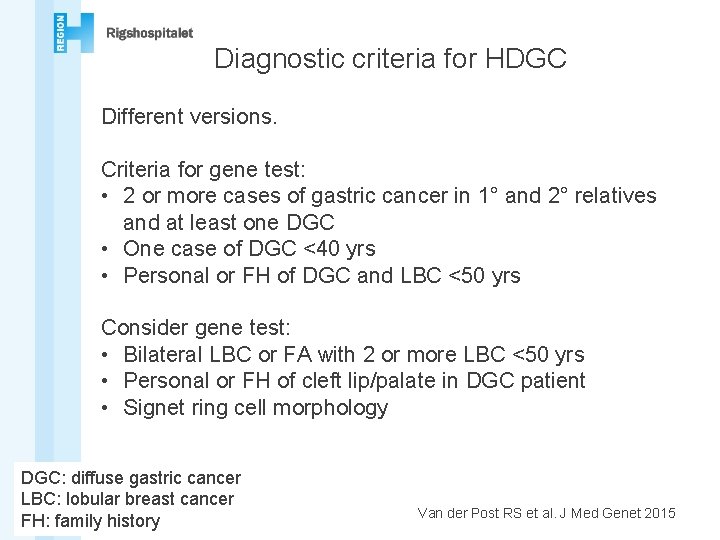
Diagnostic criteria for HDGC Different versions. Criteria for gene test: • 2 or more cases of gastric cancer in 1° and 2° relatives and at least one DGC • One case of DGC <40 yrs • Personal or FH of DGC and LBC <50 yrs Consider gene test: • Bilateral LBC or FA with 2 or more LBC <50 yrs • Personal or FH of cleft lip/palate in DGC patient • Signet ring cell morphology DGC: diffuse gastric cancer LBC: lobular breast cancer FH: family history Van der Post RS et al. J Med Genet 2015
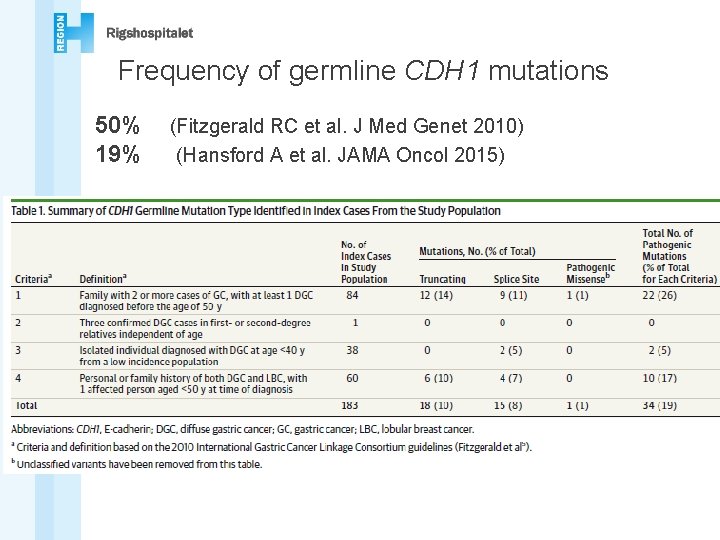
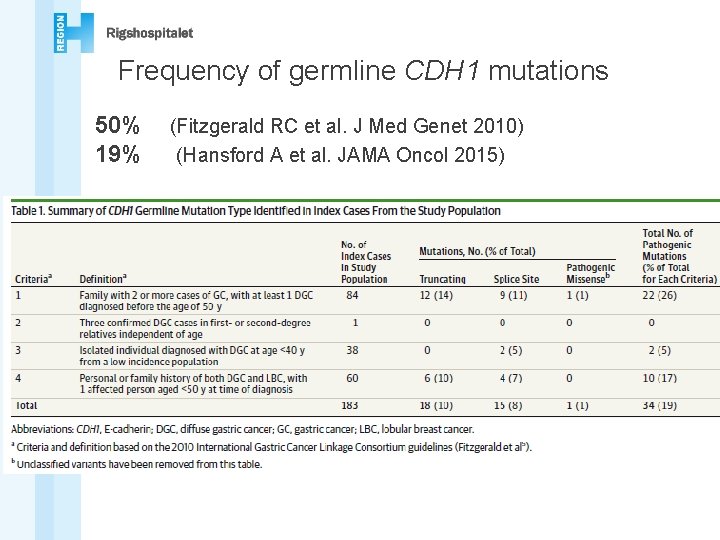
Frequency of germline CDH 1 mutations 50% 19% (Fitzgerald RC et al. J Med Genet 2010) (Hansford A et al. JAMA Oncol 2015)
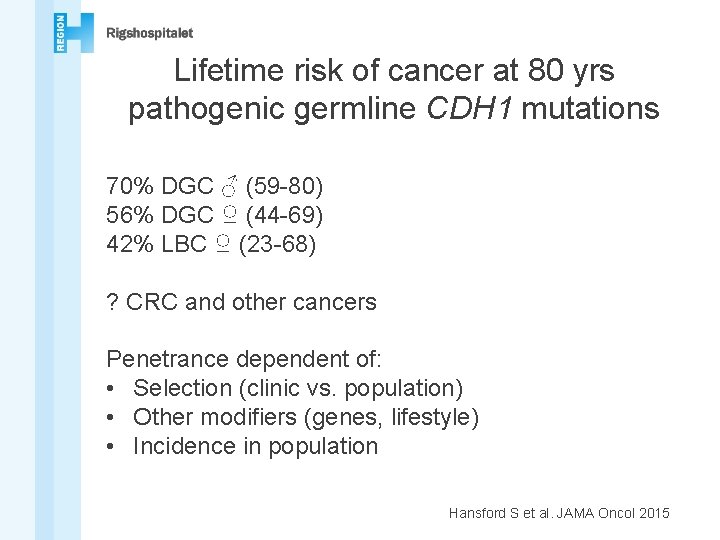
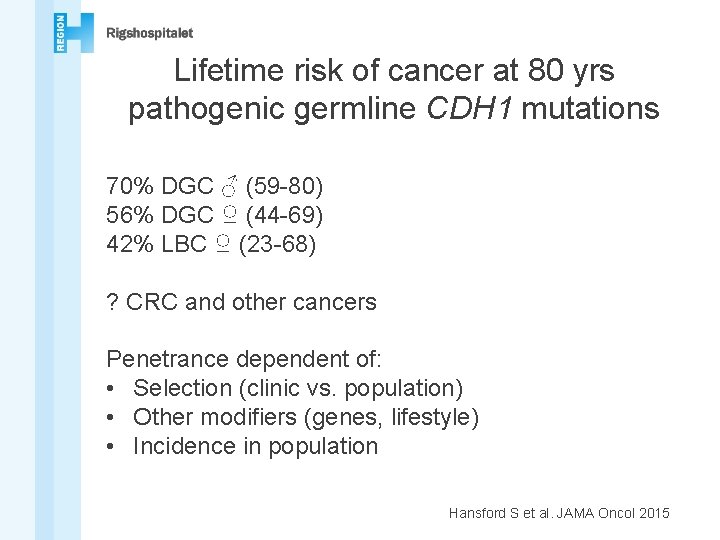
Lifetime risk of cancer at 80 yrs pathogenic germline CDH 1 mutations 70% DGC ♂ (59 -80) 56% DGC ♀ (44 -69) 42% LBC ♀ (23 -68) ? CRC and other cancers Penetrance dependent of: • Selection (clinic vs. population) • Other modifiers (genes, lifestyle) • Incidence in population Hansford S et al. JAMA Oncol 2015

New technology gene test NGS • Genome sequencing (WGS): • Whole genome analyzed Incidental findings Coverage • Exome sequencing: • All genes analyzed • Targeteret sequencing: • Gene panels analyzed Navn (Sidehoved/fod) 10
New technology – more dilemmas • Pathogenic mutation • Normal result • Variant of unknown significance (VUS) • Mutations in other disease causing genes not related to patients symptoms (incidental findings) • Mutations in genes not related to diseases

Incidental findings – good or bad? • High or low disease risk • Uncertainty about size of disease risk • • Disease prevention/treatment possible? Improved survival? At what age will disease be diagnosed? Can the patient actively reduce risk? • Family members? • Genetic discrimination? 13
Therefore we propose that HDGC syndrome may be best defined by mutations in CDH 1 and closely related genes, rather than through clinical criteria that capture families with heterogeneous susceptibility profiles. Hansford S et al. JAMA Oncol 2015