Generation of HLA universal platelets for regenerative applications

- Slides: 32
Generation of HLA universal platelets for regenerative applications Constança Figueiredo Institute for Transfusion Medicine, Hannover Medical School, Hannover, Germany
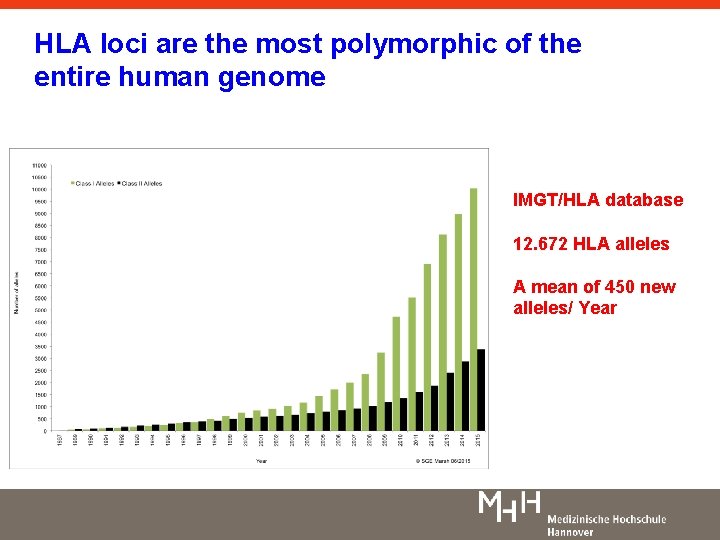
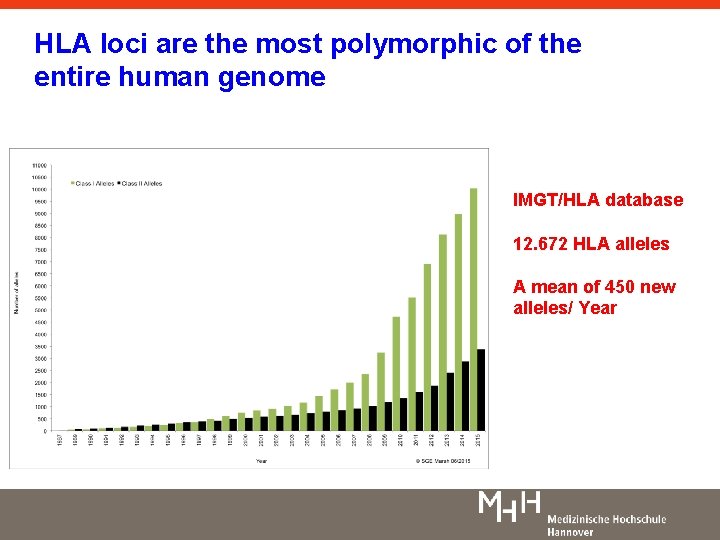
HLA loci are the most polymorphic of the entire human genome IMGT/HLA database 12. 672 HLA alleles A mean of 450 new alleles/ Year
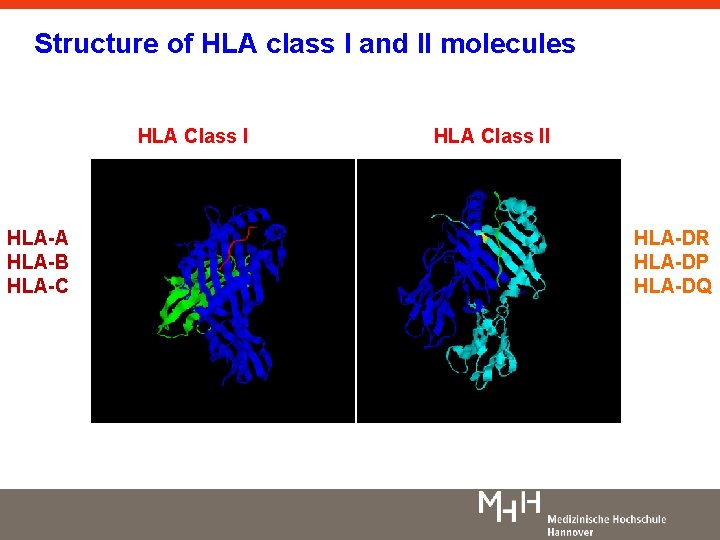
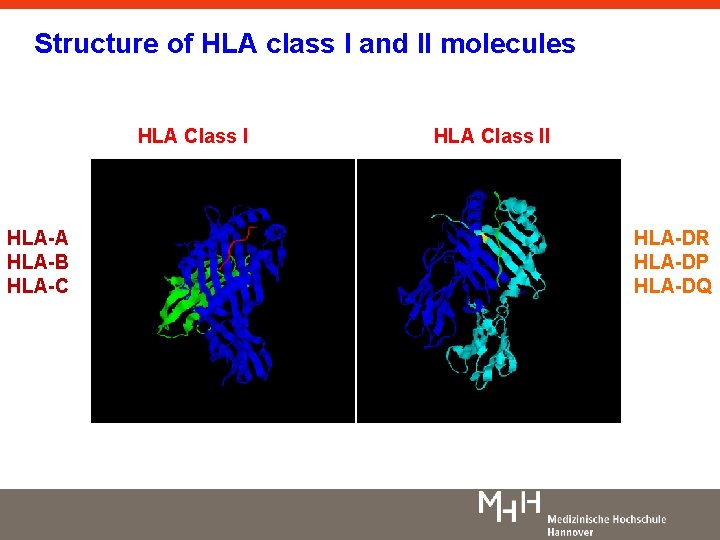
Structure of HLA class I and II molecules HLA Class I HLA-A HLA-B HLA-C HLA Class II HLA-DR HLA-DP HLA-DQ
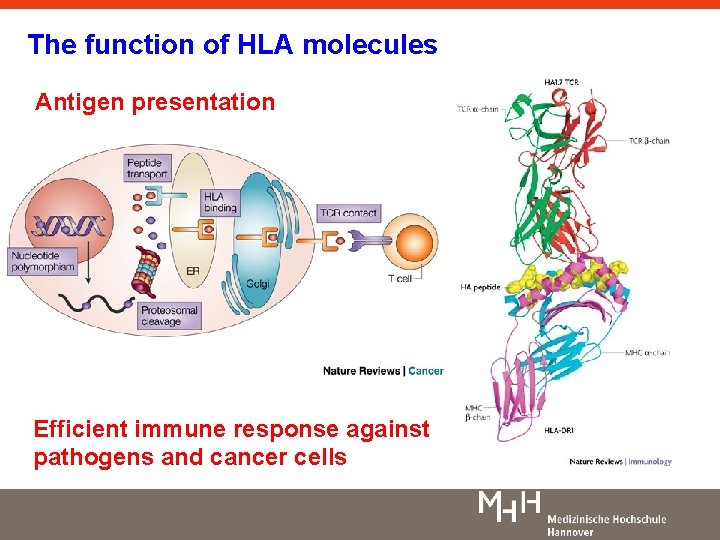
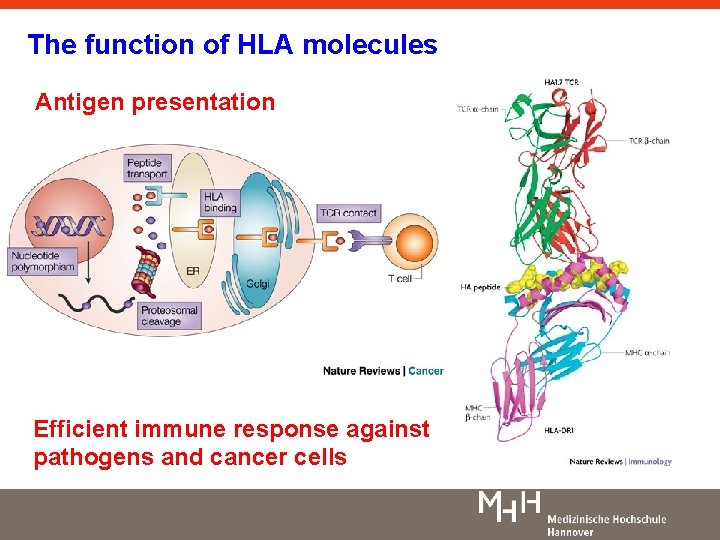
The function of HLA molecules Antigen presentation Efficient immune response against pathogens and cancer cells
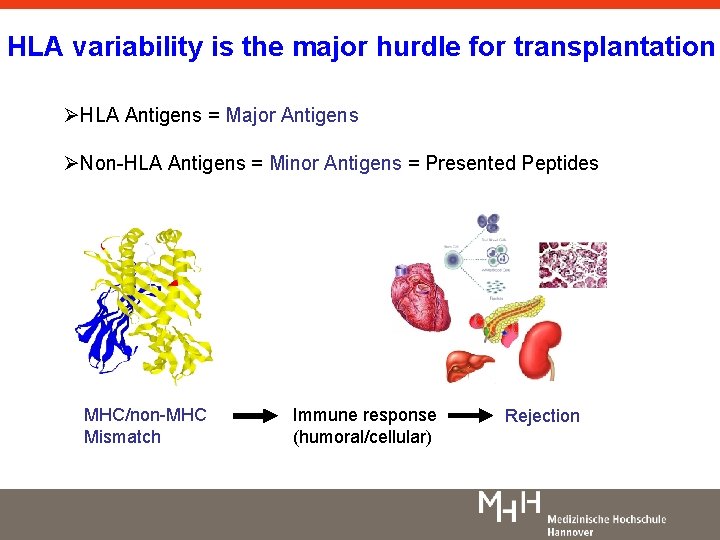
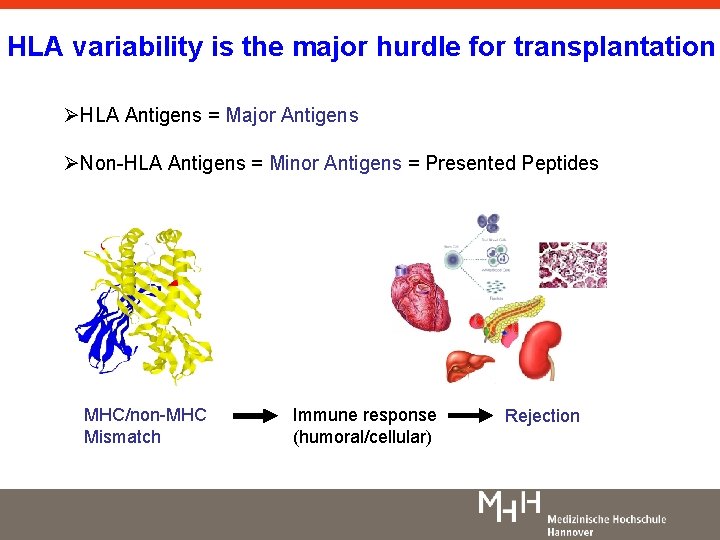
HLA variability is the major hurdle for transplantation ØHLA Antigens = Major Antigens ØNon-HLA Antigens = Minor Antigens = Presented Peptides MHC/non-MHC Mismatch Immune response (humoral/cellular) Rejection
Standard Strategy to prevent rejection: Immunosuppression Suppression of the recipient’s immune system
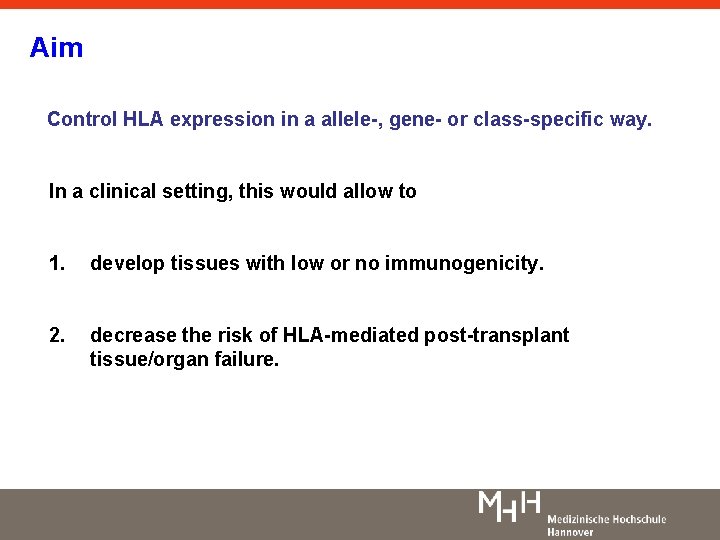
Aim Control HLA expression in a allele-, gene- or class-specific way. In a clinical setting, this would allow to 1. develop tissues with low or no immunogenicity. 2. decrease the risk of HLA-mediated post-transplant tissue/organ failure.
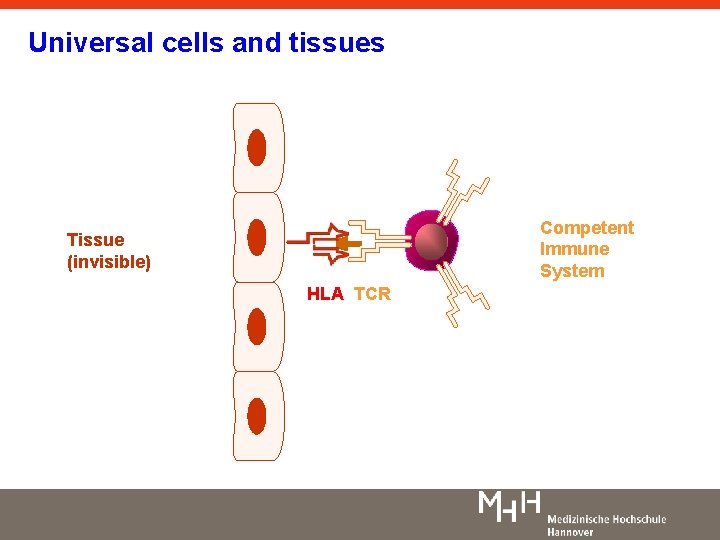
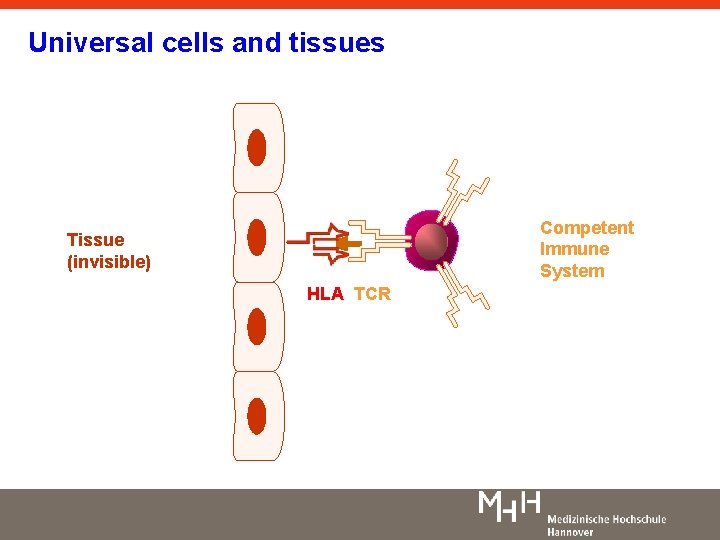
Universal cells and tissues Competent Immune System Tissue (invisible) HLA TCR
Alternative Strategy to prevent rejection: Reducing the organ‘s immunogenicity Reducing the organ’s Immunogenicity
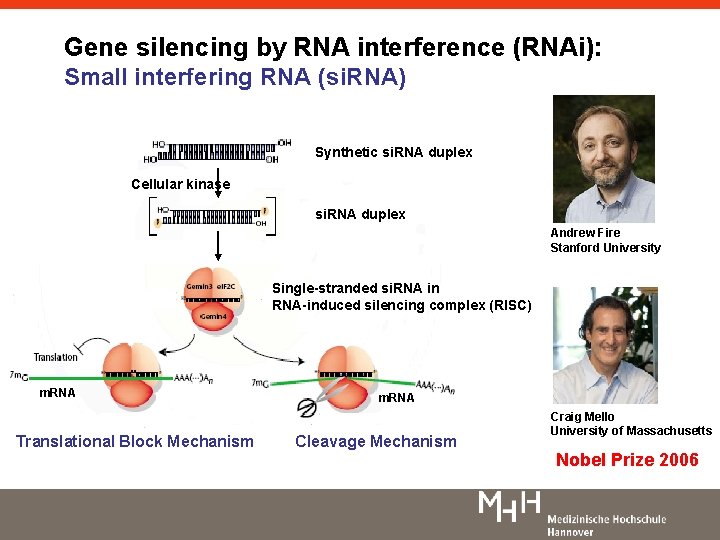
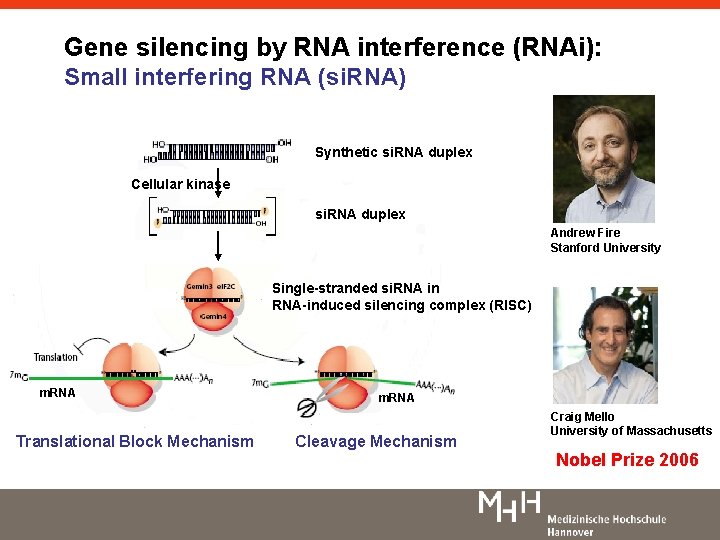
Gene silencing by RNA interference (RNAi): Small interfering RNA (si. RNA) Synthetic si. RNA duplex Cellular kinase si. RNA duplex Andrew Fire Stanford University Single-stranded si. RNA in RNA-induced silencing complex (RISC) m. RNA Translational Block Mechanism m. RNA Cleavage Mechanism Craig Mello University of Massachusetts Nobel Prize 2006
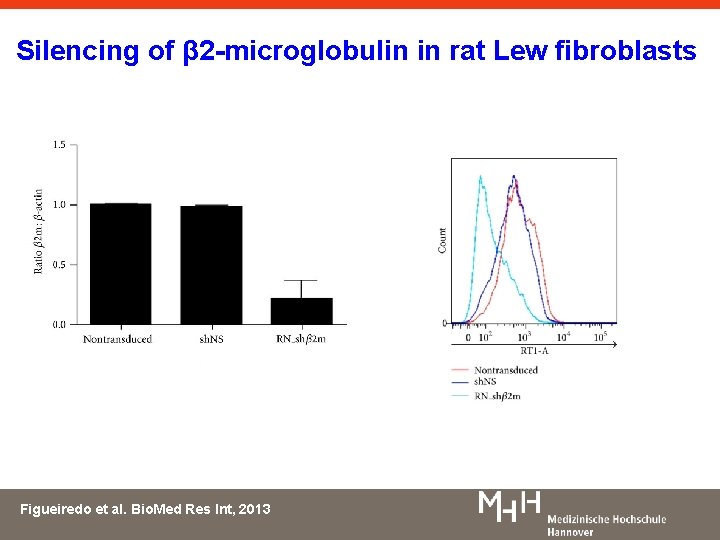
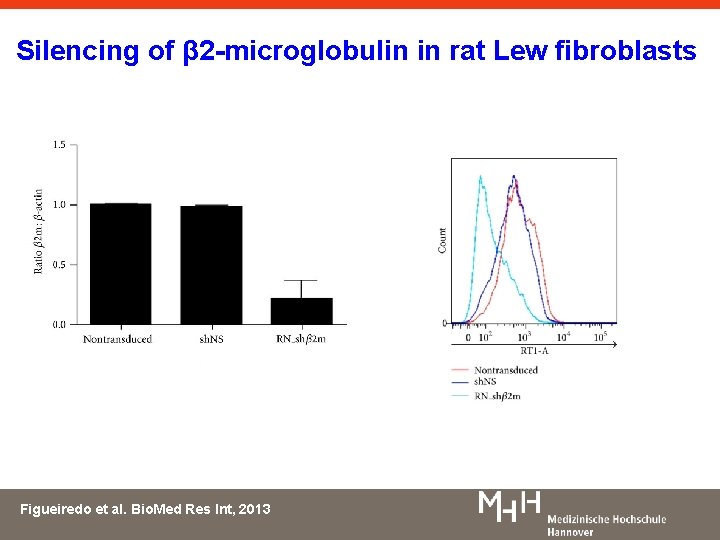
Silencing of β 2 -microglobulin in rat Lew fibroblasts Figueiredo et al. Bio. Med Res Int, 2013
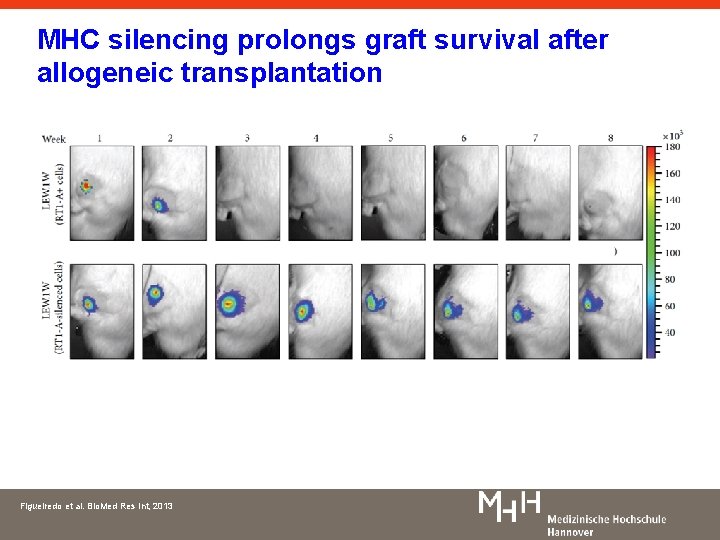
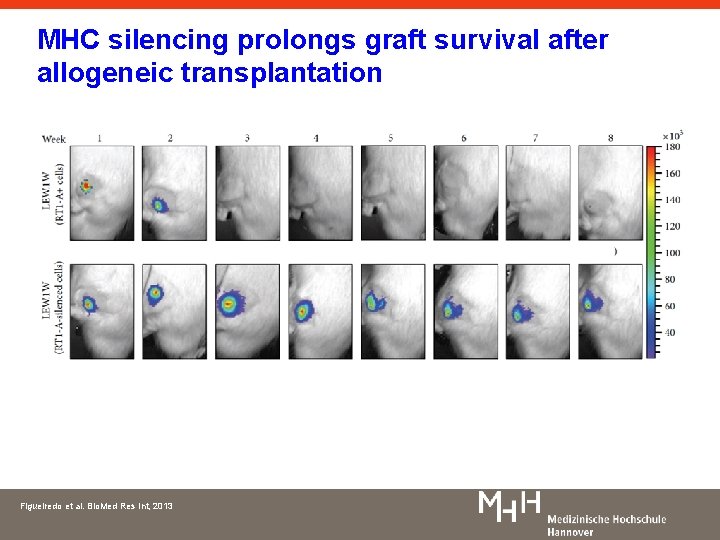
MHC silencing prolongs graft survival after allogeneic transplantation Figueiredo et al. Bio. Med Res Int, 2013
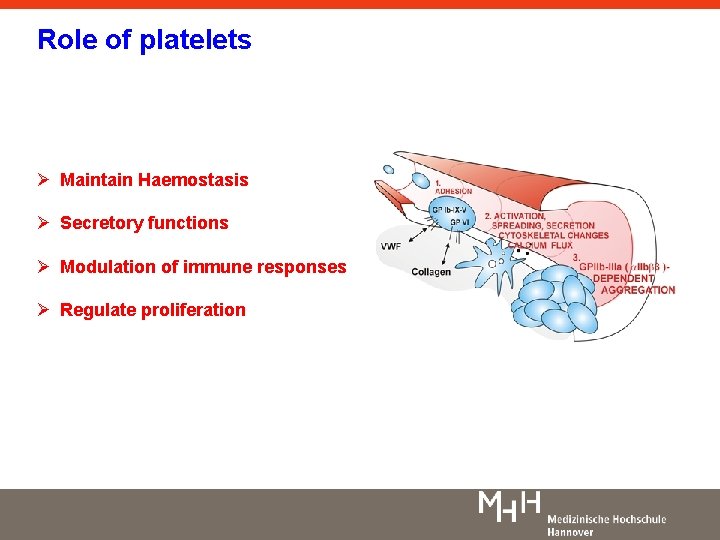
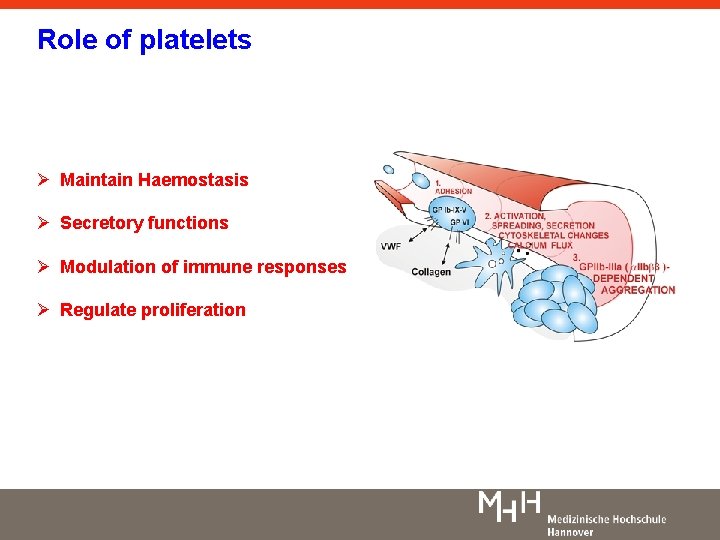
Role of platelets Ø Maintain Haemostasis Ø Secretory functions Ø Modulation of immune responses Ø Regulate proliferation
Application of platelets in regenerative medicine Ø Treatment of thrombocytopenia Ø Wound healing Ø Tissue remodelling Ø Drug carriers
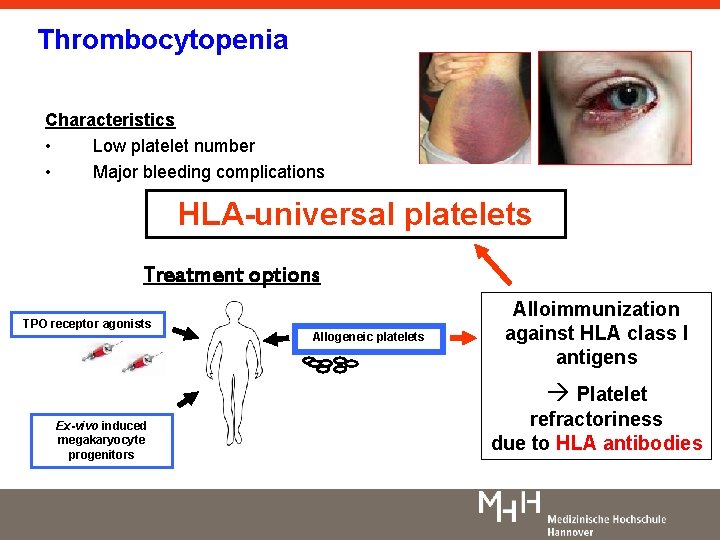
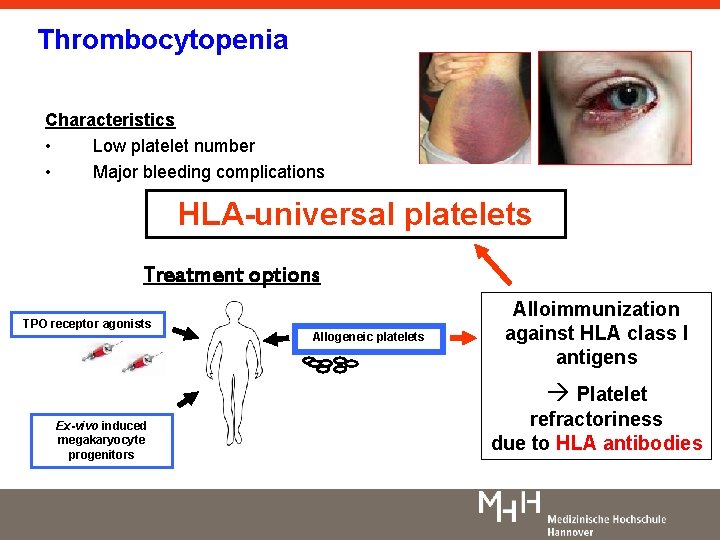
Thrombocytopenia Characteristics • Low platelet number • Major bleeding complications HLA-universal platelets Treatment options TPO receptor agonists Allogeneic platelets Alloimmunization against HLA class I antigens à Platelet Ex-vivo induced megakaryocyte progenitors refractoriness due to HLA antibodies
In vitro production of Platelets to treat platelet transfusion refractoriness
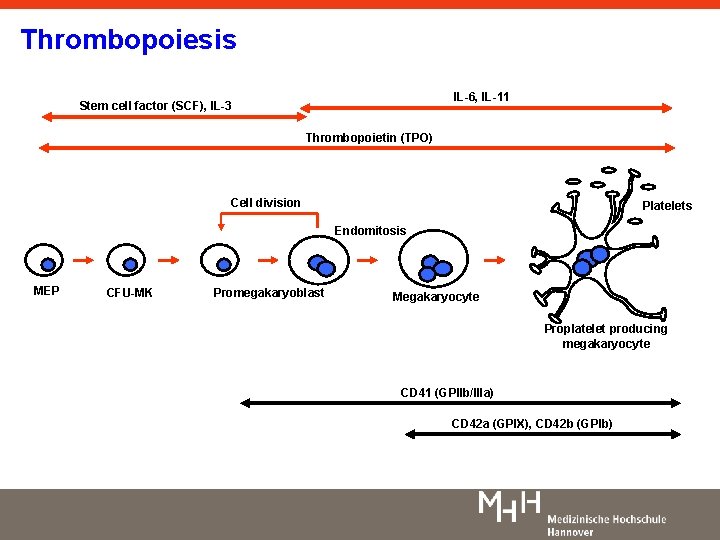
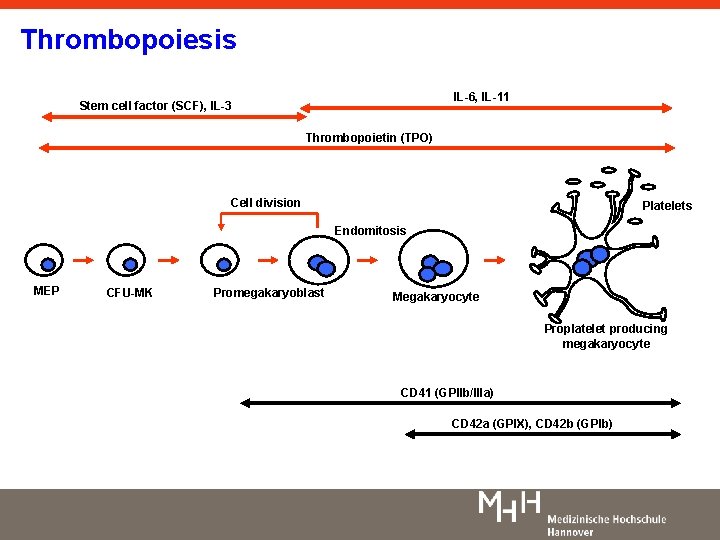
Thrombopoiesis IL-6, IL-11 Stem cell factor (SCF), IL-3 Thrombopoietin (TPO) Cell division Platelets Endomitosis MEP CFU-MK Promegakaryoblast Megakaryocyte Proplatelet producing megakaryocyte CD 41 (GPIIb/IIIa) CD 42 a (GPIX), CD 42 b (GPIb)
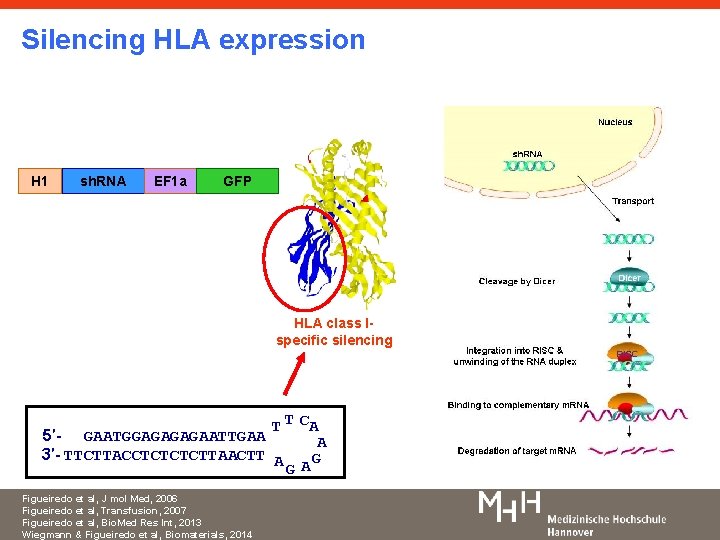
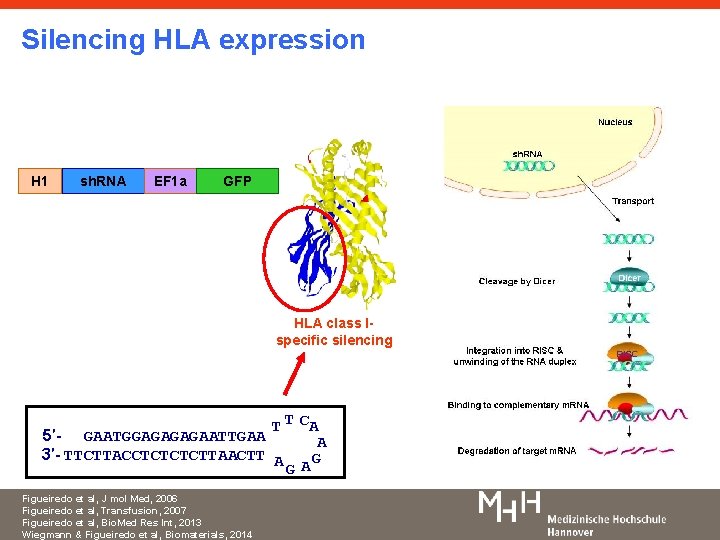
Silencing HLA expression H 1 sh. RNA EF 1 a GFP HLA class Ispecific silencing T T CA 5′- GAATGGAGAATTGAA A 3′- TTCTTACCTCTTAACTT A G GA Figueiredo et al, J mol Med, 2006 Figueiredo et al, Transfusion, 2007 Figueiredo et al, Bio. Med Res Int, 2013 Wiegmann & Figueiredo et al, Biomaterials, 2014
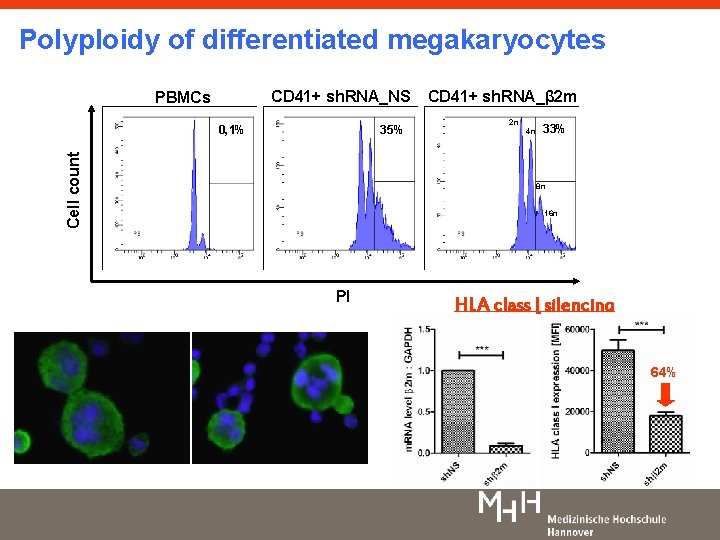
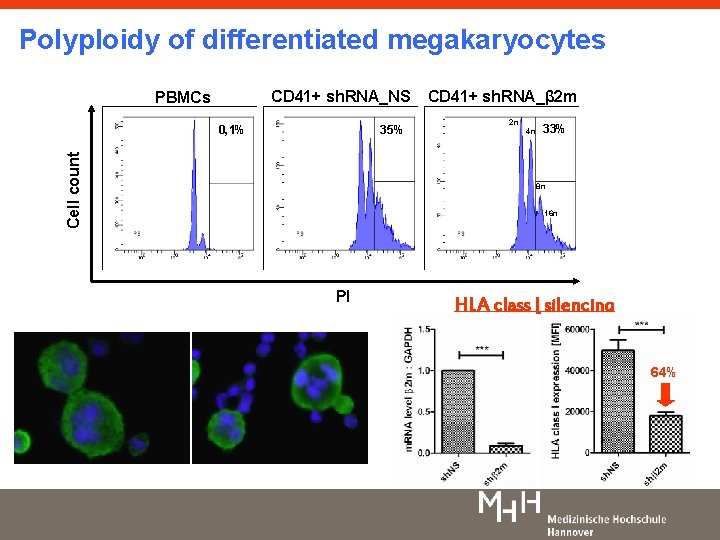
Polyploidy of differentiated megakaryocytes CD 41+ sh. RNA_NS PBMCs 35% Cell count 0, 1% CD 41+ sh. RNA_β 2 m 2 n 4 n 33% 8 n 16 n PI HLA class I silencing 64%
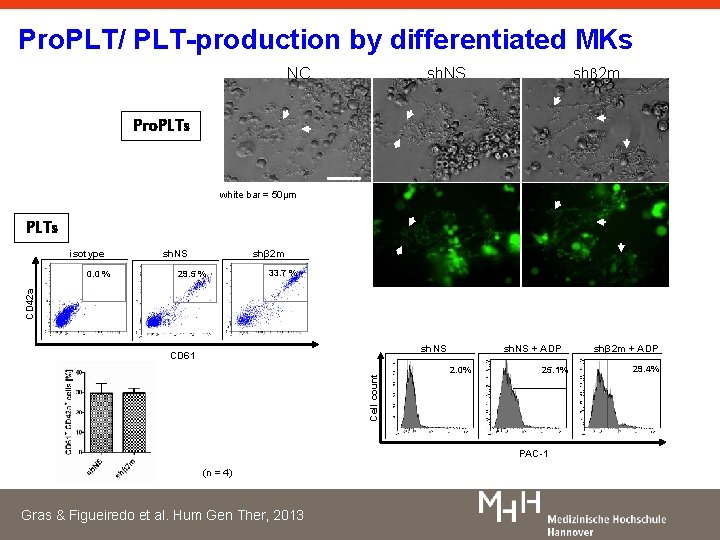
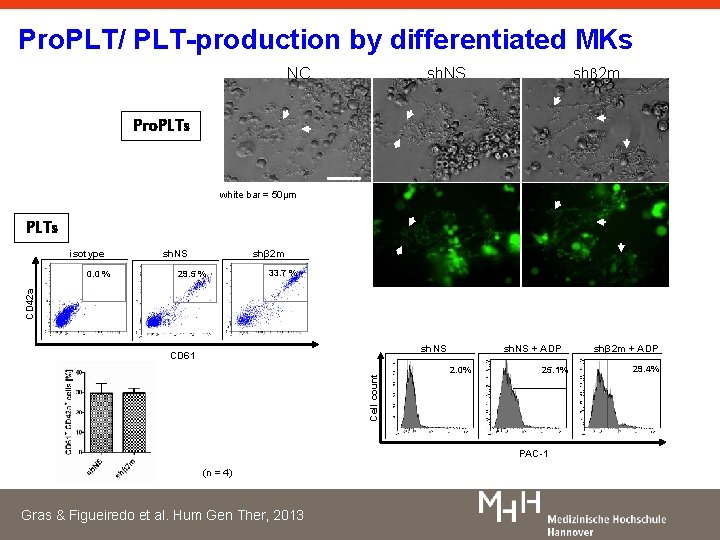
Pro. PLT/ PLT-production by differentiated MKs NC shβ 2 m sh. NS Pro. PLTs white bar = 50μm PLTs isotype 29. 5 % 33. 7 % CD 42 a 0. 0 % shβ 2 m sh. NS Cell count CD 61 sh. NS + ADP 2. 0% 25. 1% PAC-1 (n = 4) Gras & Figueiredo et al. Hum Gen Ther, 2013 shβ 2 m + ADP 29. 4%
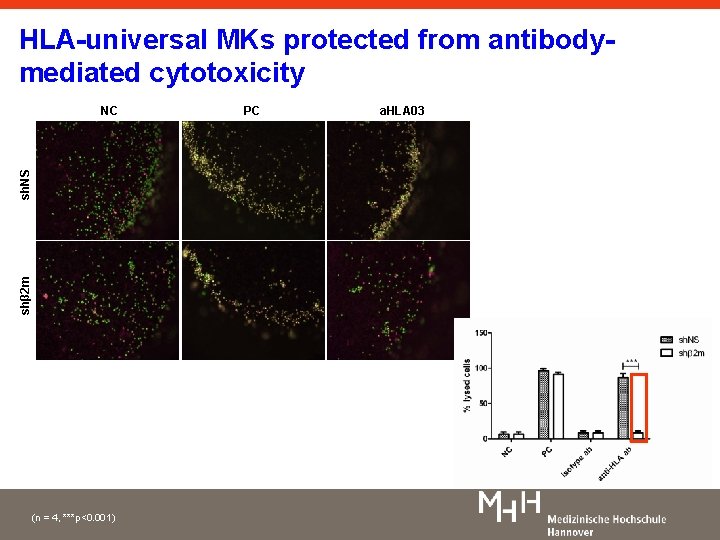
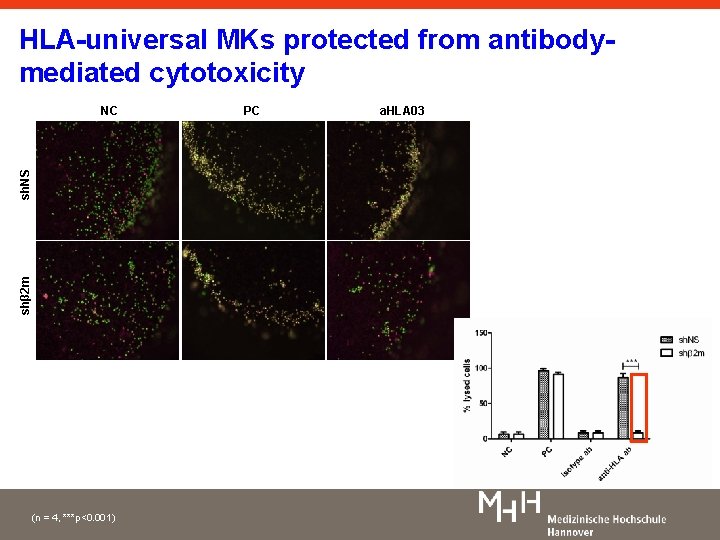
HLA-universal MKs protected from antibodymediated cytotoxicity shβ 2 m sh. NS NC (n = 4, ***p<0. 001) PC a. HLA 03
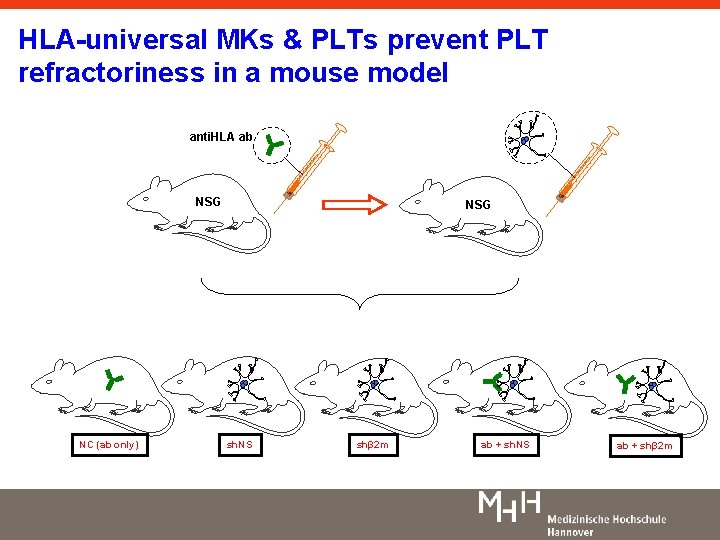
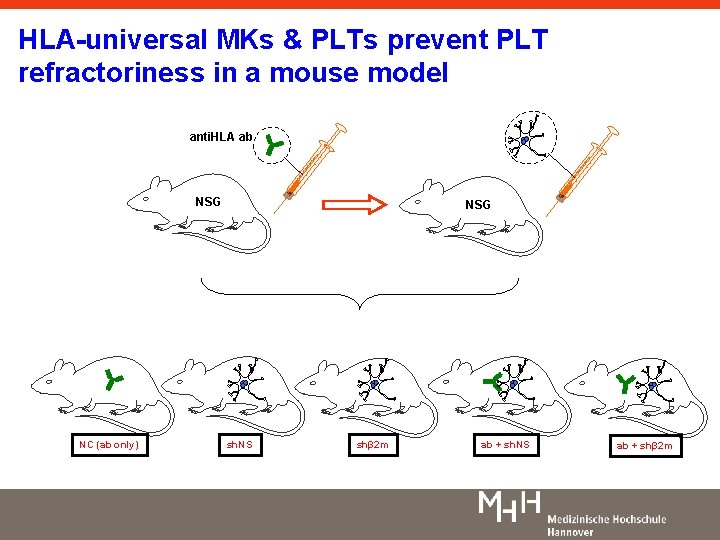
HLA-universal MKs & PLTs prevent PLT refractoriness in a mouse model anti. HLA ab NSG NC (ab only) NSG sh. NS shβ 2 m ab + sh. NS ab + shβ 2 m
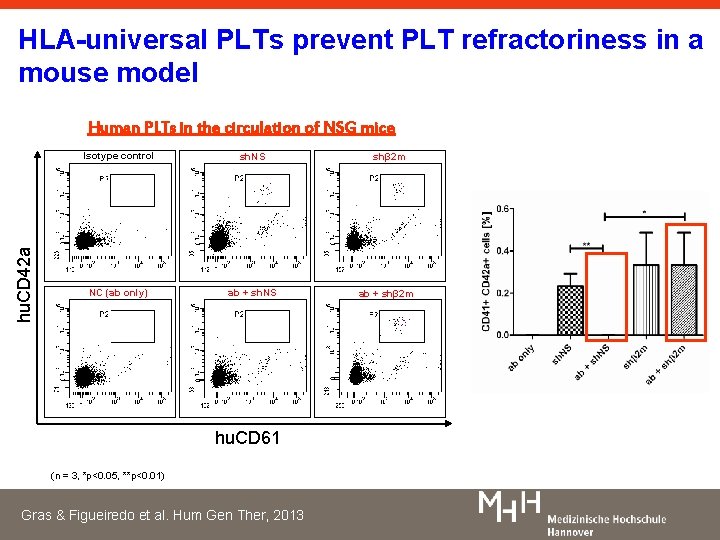
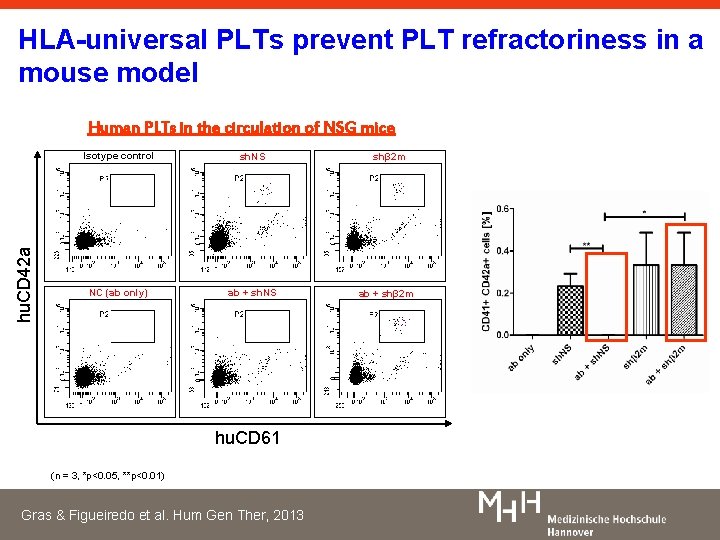
HLA-universal PLTs prevent PLT refractoriness in a mouse model hu. CD 42 a Human PLTs in the circulation of NSG mice Isotype control sh. NS shβ 2 m NC (ab only) ab + sh. NS ab + shβ 2 m hu. CD 61 (n = 3, *p<0. 05, **p<0. 01) Gras & Figueiredo et al. Hum Gen Ther, 2013
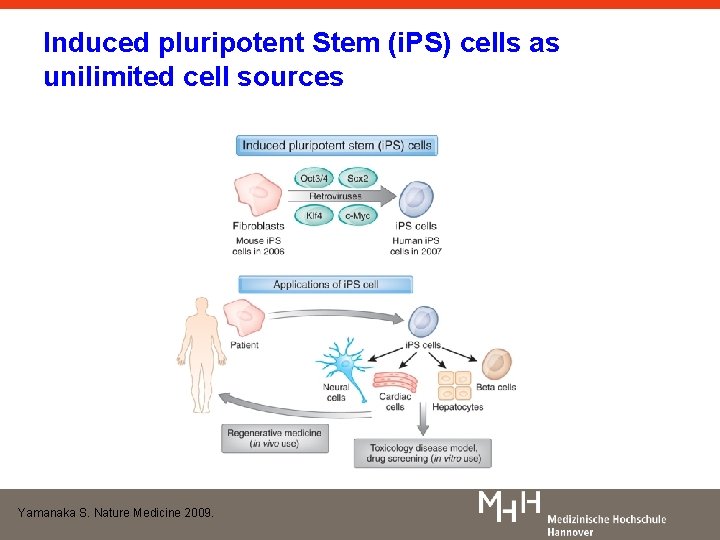
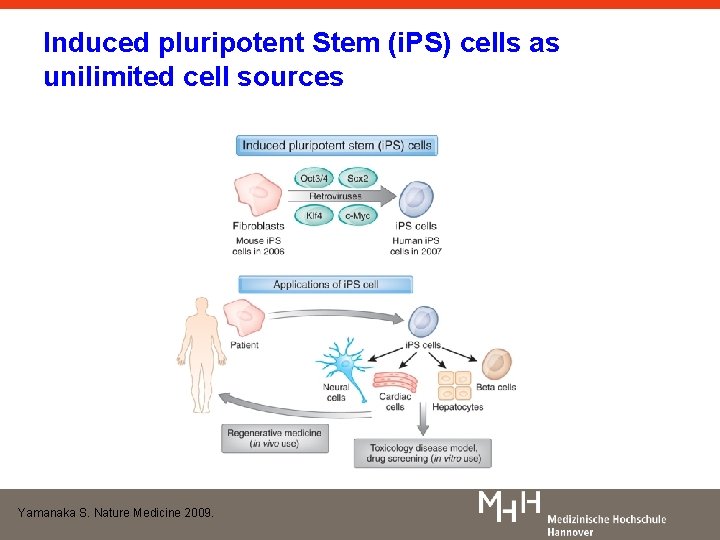
Induced pluripotent Stem (i. PS) cells as unilimited cell sources Yamanaka S. Nature Medicine 2009.
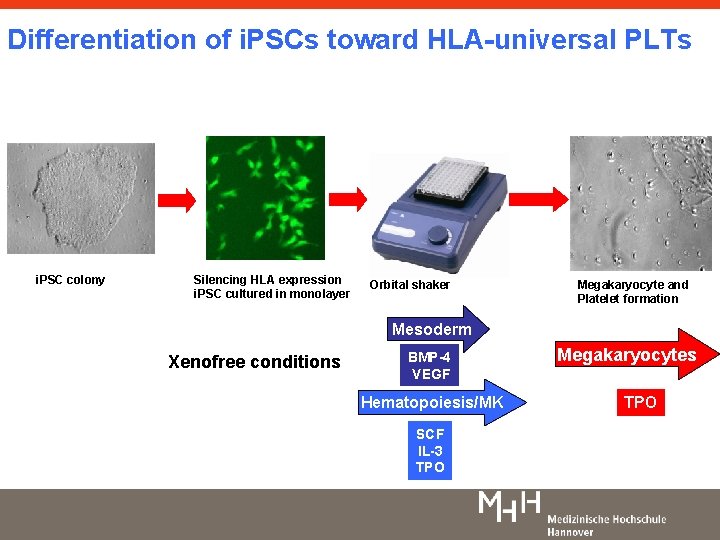
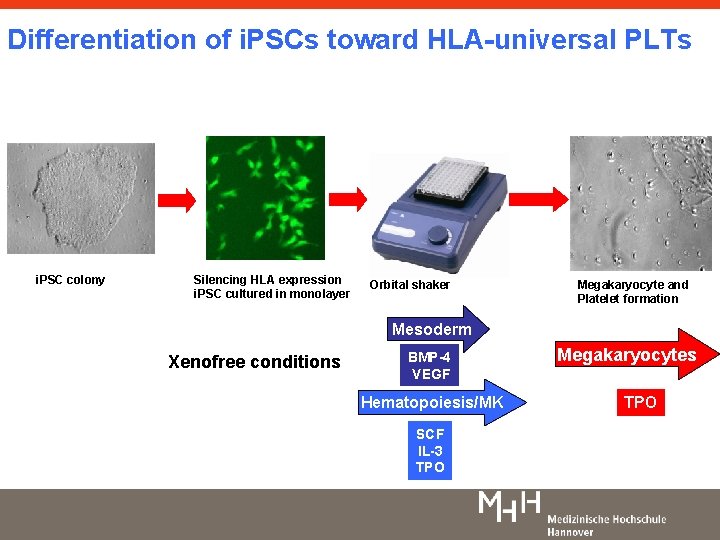
Differentiation of i. PSCs toward HLA-universal PLTs i. PSC colony Silencing HLA expression i. PSC cultured in monolayer Orbital shaker Megakaryocyte and Platelet formation Mesoderm Xenofree conditions BMP-4 VEGF Hematopoiesis/MK SCF IL-3 TPO Megakaryocytes TPO
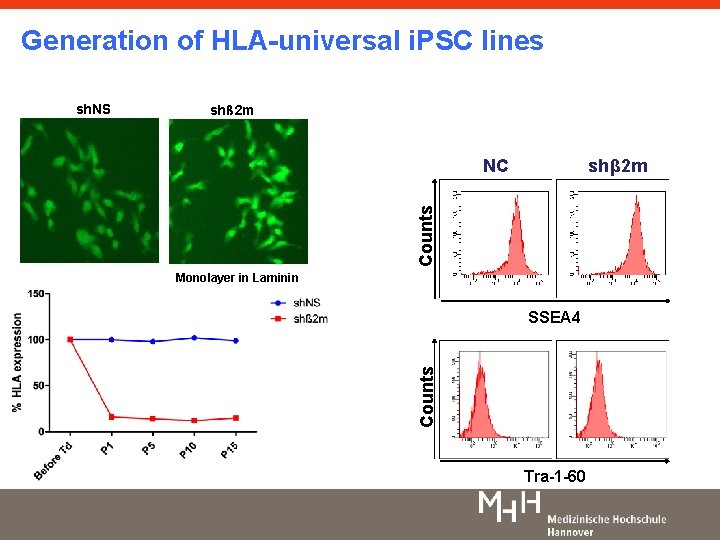
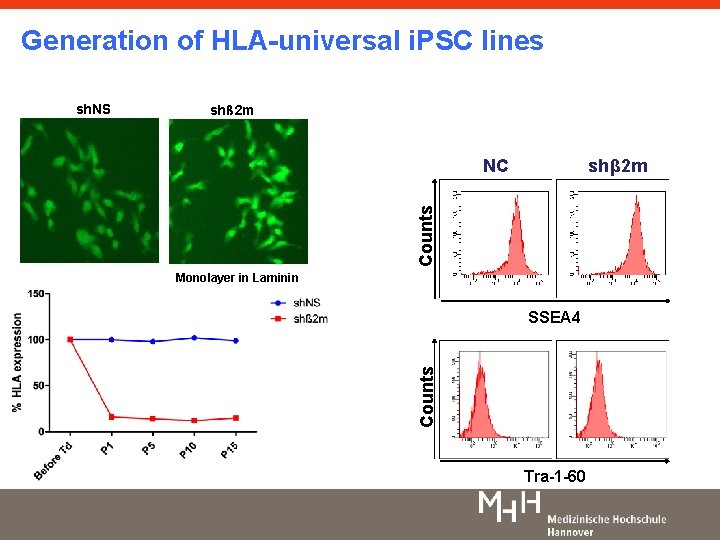
Generation of HLA-universal i. PSC lines shß 2 m shβ 2 m Counts NC Monolayer in Laminin SSEA 4 Counts sh. NS Tra-1 -60
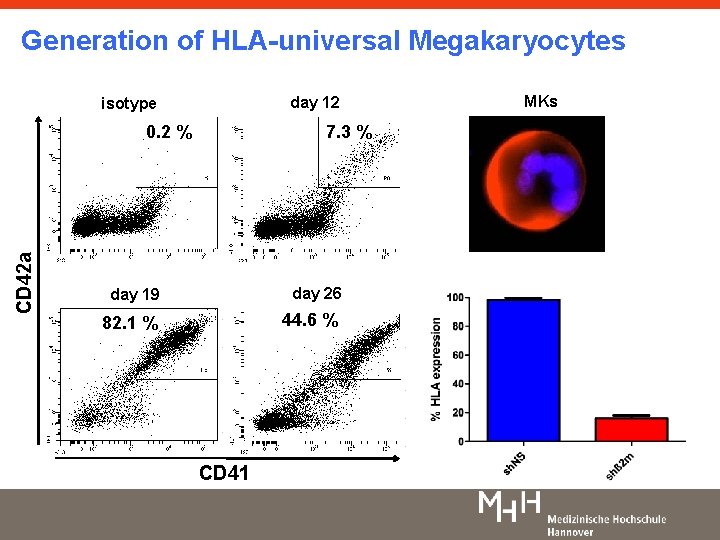
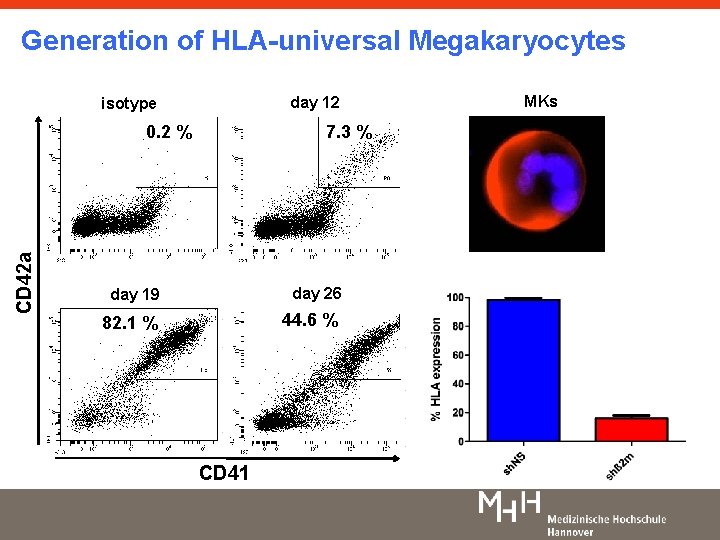
Generation of HLA-universal Megakaryocytes day 12 isotype 7. 3 % CD 42 a 0. 2 % day 19 day 26 82. 1 % 44. 6 % CD 41 MKs
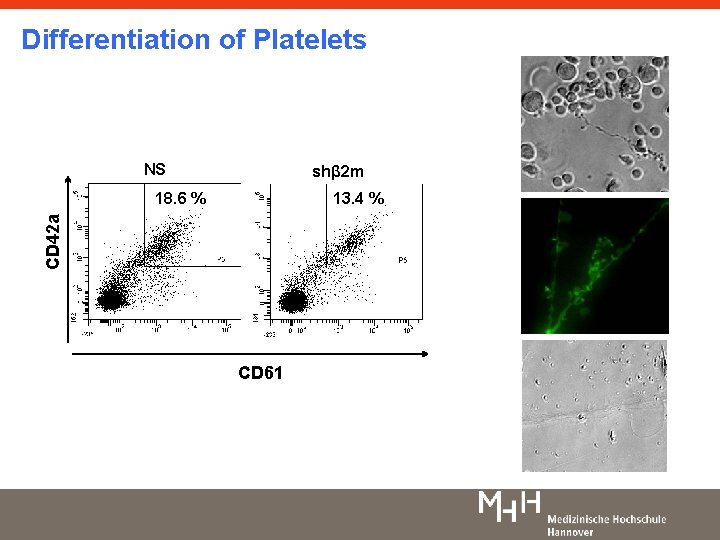
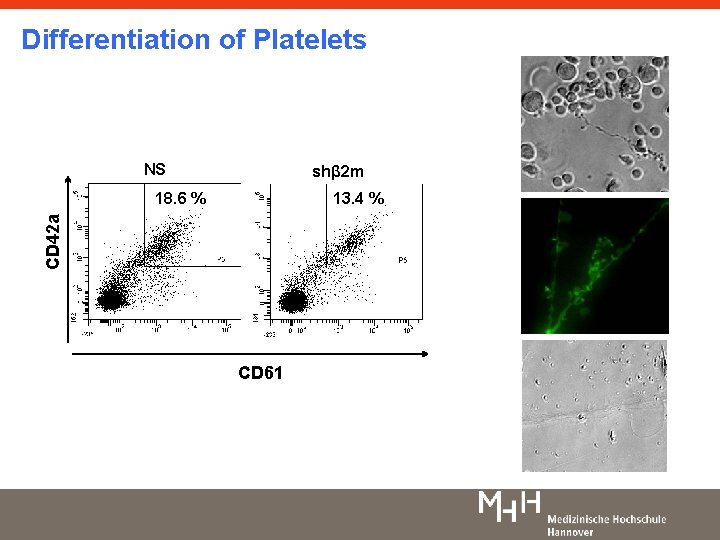
Differentiation of Platelets NS shβ 2 m 13. 4 % CD 42 a 18. 6 % CD 61
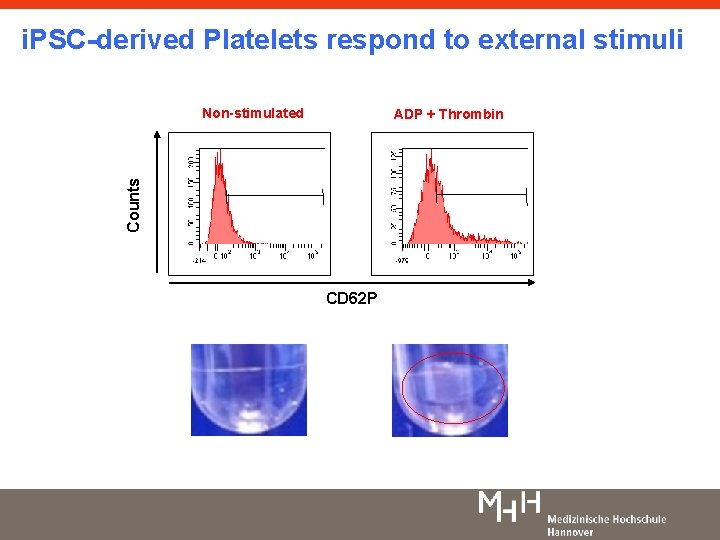
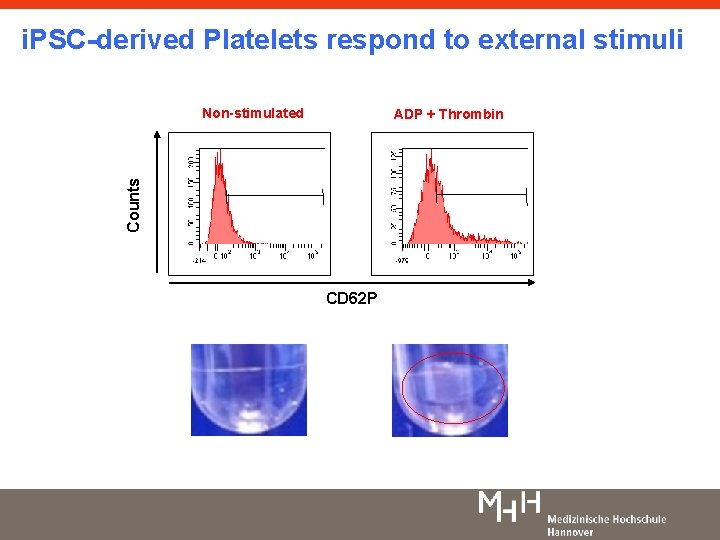
i. PSC-derived Platelets respond to external stimuli Non-stimulated Counts ADP + Thrombin CD 62 P
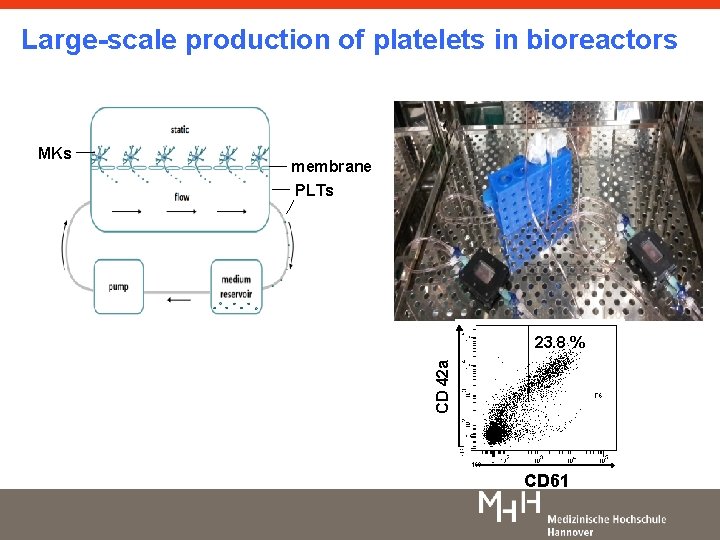
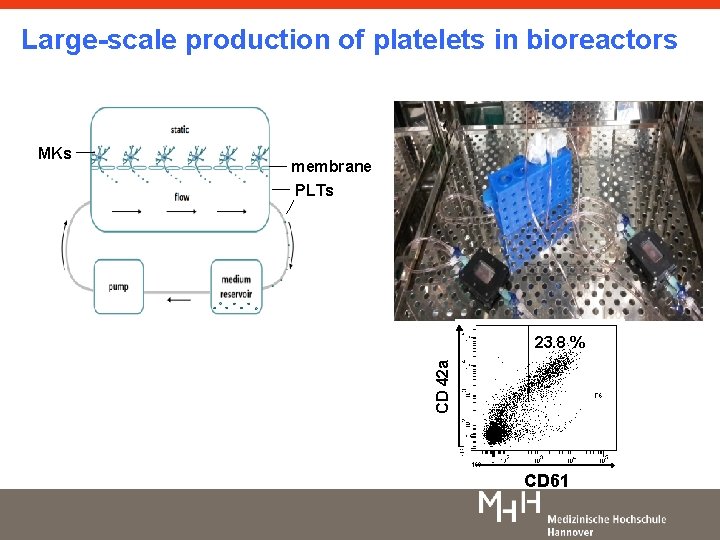
Large-scale production of platelets in bioreactors membrane PLTs 23. 8 % CD 42 a MKs CD 61
Summary • The generation of in vitro pharmed genetically modified platelets is feasible. • IPSC serve as an unlimited cell source for the large-scale production of platelets. • Universal platelets bring the concept of Universal cells one step closer to reality.

Acknowledgements Institute for Transfusion Medicine, Hannover Medical School, Germany. Rainer Blasczyk Dominca Ratuszny Laura Schlahsa Haijiao Zhang Ann-Kathrin Börger Stefanie Vahlsing Lilia Goudeva Helmholtz Center for Infection Research, Braunschweig, Germany Carlos Guzman Kai Schulze Institute of Experimental Hematology, Hannover Medical School, Hannover Thomas Moritz, Axel Schambach Nico Lachmann Mania Ackermann LEBAO, Hannover Medical School, Hannover Ulrich Martin Stefanie Wunderlich Lena Engels Stiftung für Transfusionsmedizin