GENERAL PRESENTER NOTES 1 This is an overview
- Slides: 35
GENERAL PRESENTER NOTES - 1 • This is an overview of pediatric neuropalliative care. • It is designed to be given by professionals with adult or pediatric palliative care or neurology training. • Consider using the case included in this talk or your own cases to increase interaction with audience. • A unique theme of this presentation is the different trajectories in pediatric palliative care that are presented in slides 13 -19. • After presenting the case and the slides that follow, a presenter might focus on assessment and communication skills that could be used at each point in the trajectory.
GENERAL PRESENTER NOTES - 2 • Throughout this presentation, we use the word parents, but really this refers to anyone taking care of the child. • Some of the communication strategies described in this module are covered in more depth in the "Communication and Delivering Difficult News" module. Depending on your audience, presenters might consider using some slides from that module in this module. • Pediatric pain management is a complex skill. This module is meant to introduce the topic. Further details are out of the scope of this module.
Pediatric Neuropalliative Care The EPEC-N™ Project Education in Palliative and End-of-Life Care – Neurology A collaboration with the International Neuropalliative Care Society
Objectives • Understand the types of conditions and demographics of children receiving pediatric palliative care (PPC) and highlight the need for pediatric neuropalliative care. • Recognize triggers for introduction of PPC and anticipate common barriers to the integration of PPC into the care of children with neurological disease. • Discuss the importance of language in PPC and highlight strategies for family engagement. • Review analgesic considerations for pediatrics.
Clinical Case: Gail & Taylor Gail and Taylor just had a new baby daughter. After a normal pregnancy, Gail suffered a uterine rupture such that her daughter’s brain suffered hypoxemic insult for 30 minutes. When she was born, she was in cardiac arrest. The neonatal team initiated CPR and brought her to the neonatal intensive care unit (NICU), where she received therapeutic hypothermia for 3 days. During that time, she developed seizures and required multiple anticonvulsants. At 5 days old, she remains critically ill and intubated, and is not breathing over the ventilator. A brain MRI revealed changes consistent with severe hypoxic ischemic injury.
Clinical Case: Questions • How would you assess and discuss prognosis? • What decisions need to be made and when? • How can you engage parents in this process?
What is Pediatric Palliative Care? • Pediatric Palliative Care prevents, identifies, and treats suffering in children with serious illnesses, their families, and the teams that care for them. • It is appropriate at any stage of serious illness, and can be provided alongside disease-directed treatment.
What is Pediatric Palliative Care? • Major differences from adult palliative care include: • Recognition of death and disability as abnormal in childhood • Proxy decision making by parents • Emphasis on current quality of life and future potential rather than previously lived values
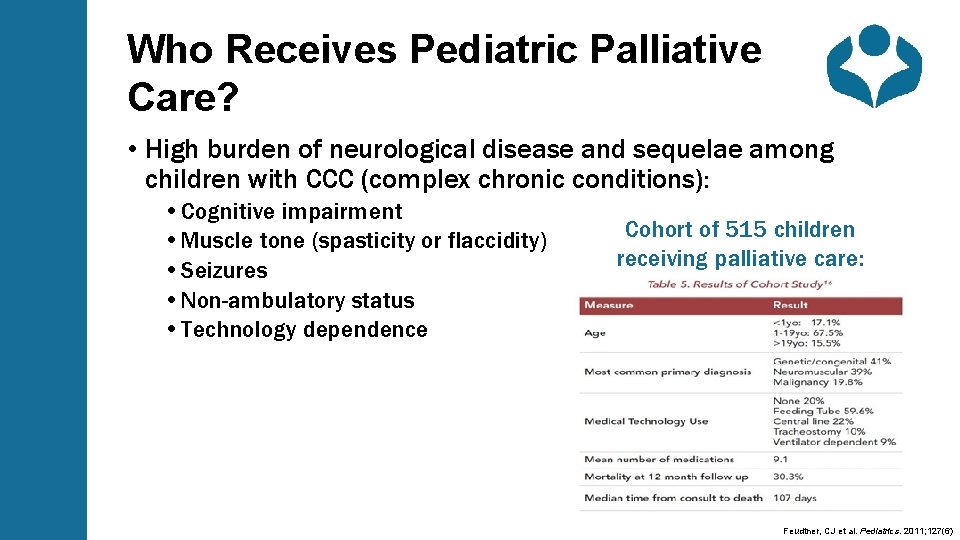
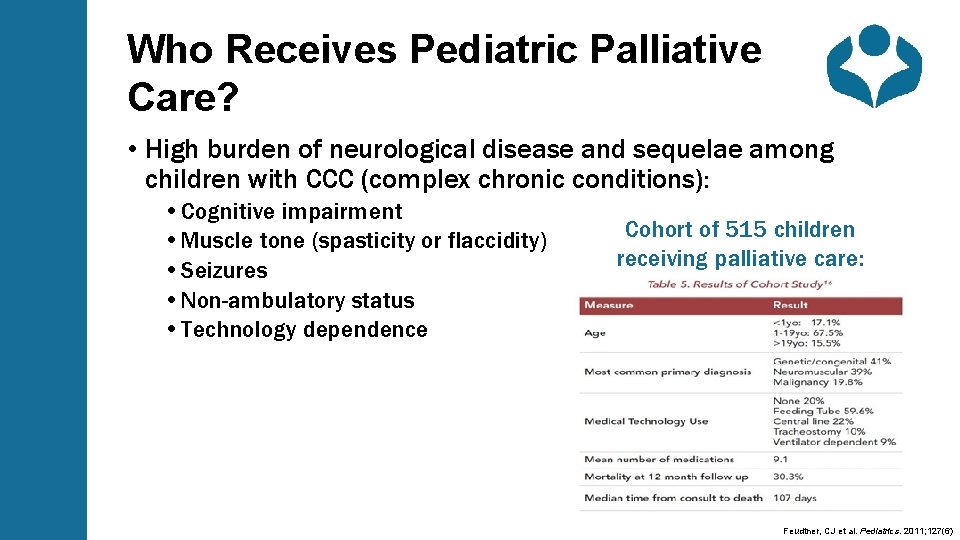
Who Receives Pediatric Palliative Care? • High burden of neurological disease and sequelae among children with CCC (complex chronic conditions): • Cognitive impairment • Muscle tone (spasticity or flaccidity) • Seizures • Non-ambulatory status • Technology dependence Cohort of 515 children receiving palliative care: Feudtner, CJ et al. Pediatrics. 2011; 127(6)
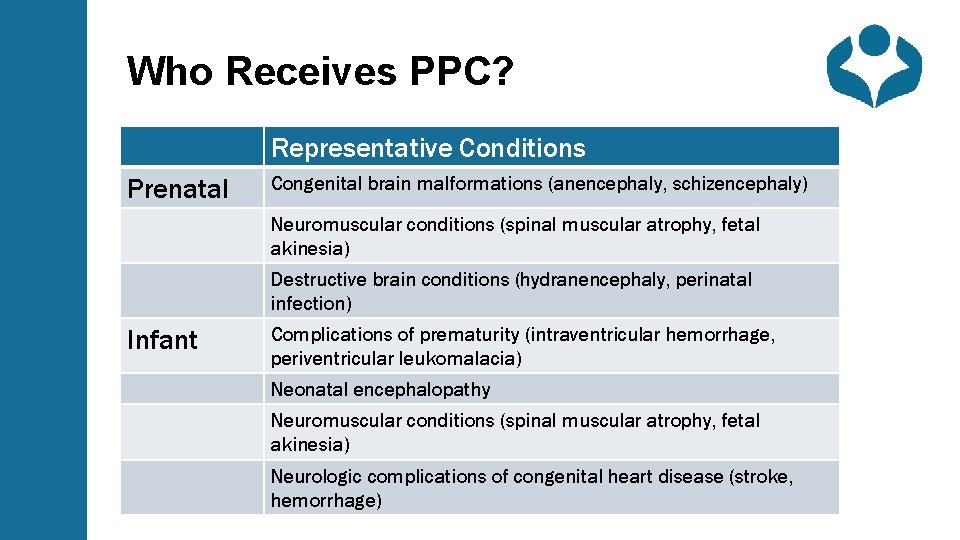
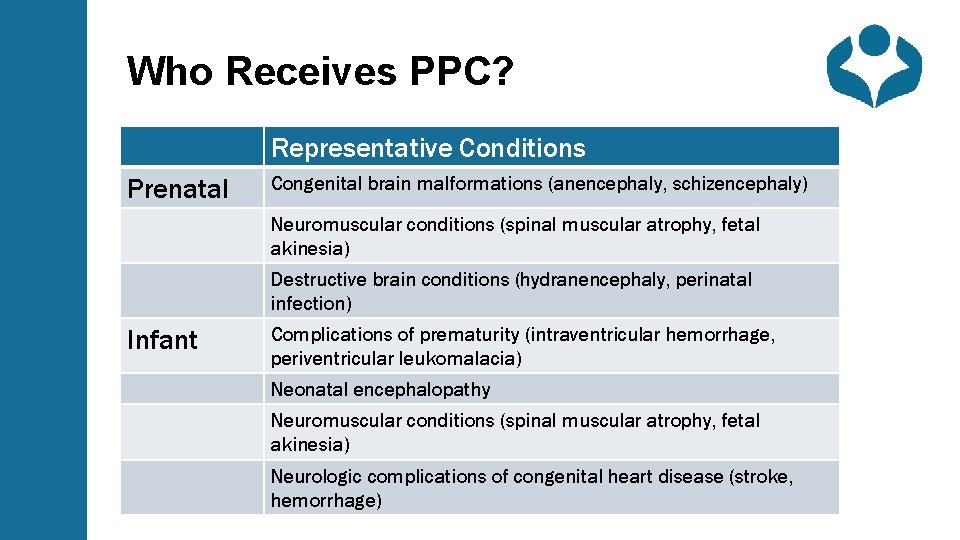
Who Receives PPC? Representative Conditions Prenatal Congenital brain malformations (anencephaly, schizencephaly) Neuromuscular conditions (spinal muscular atrophy, fetal akinesia) Destructive brain conditions (hydranencephaly, perinatal infection) Infant Complications of prematurity (intraventricular hemorrhage, periventricular leukomalacia) Neonatal encephalopathy Neuromuscular conditions (spinal muscular atrophy, fetal akinesia) Neurologic complications of congenital heart disease (stroke, hemorrhage)
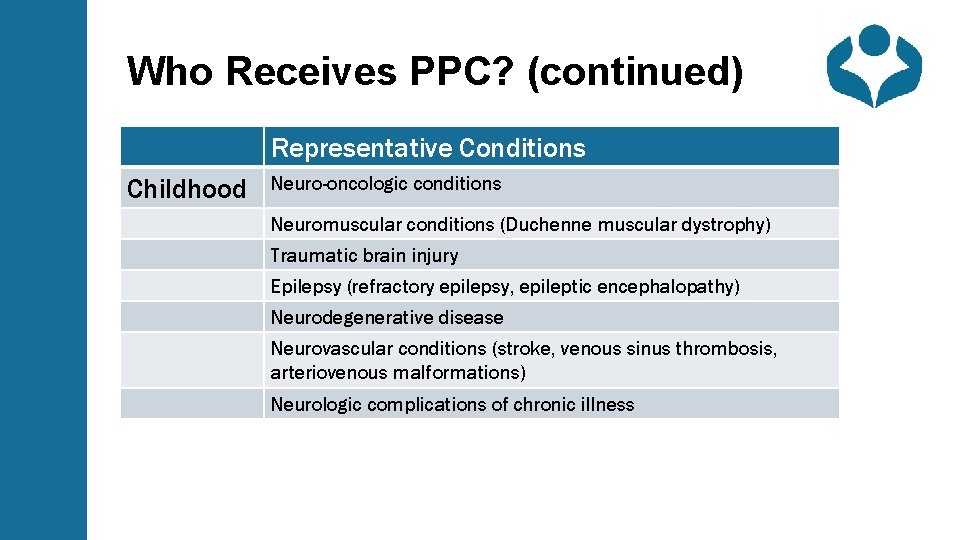
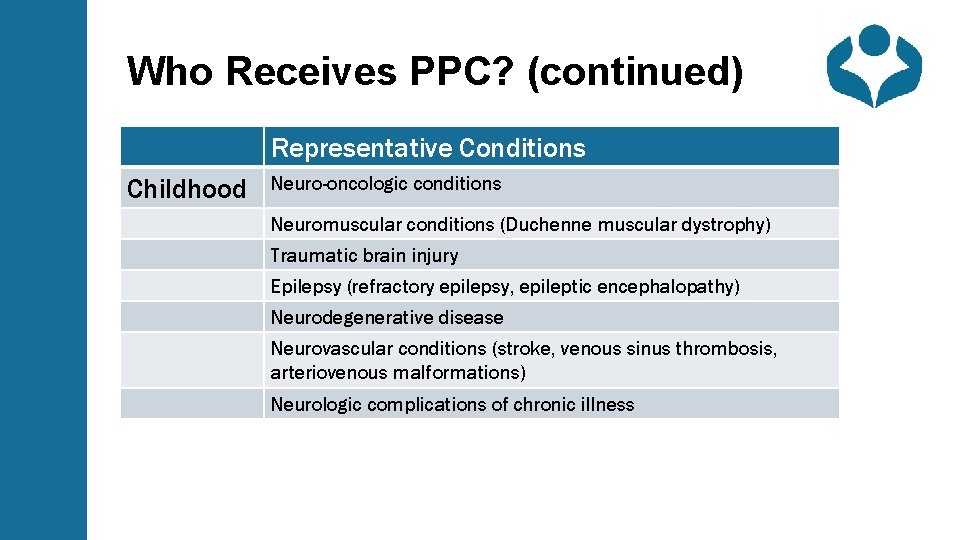
Who Receives PPC? (continued) Representative Conditions Childhood Neuro-oncologic conditions Neuromuscular conditions (Duchenne muscular dystrophy) Traumatic brain injury Epilepsy (refractory epilepsy, epileptic encephalopathy) Neurodegenerative disease Neurovascular conditions (stroke, venous sinus thrombosis, arteriovenous malformations) Neurologic complications of chronic illness
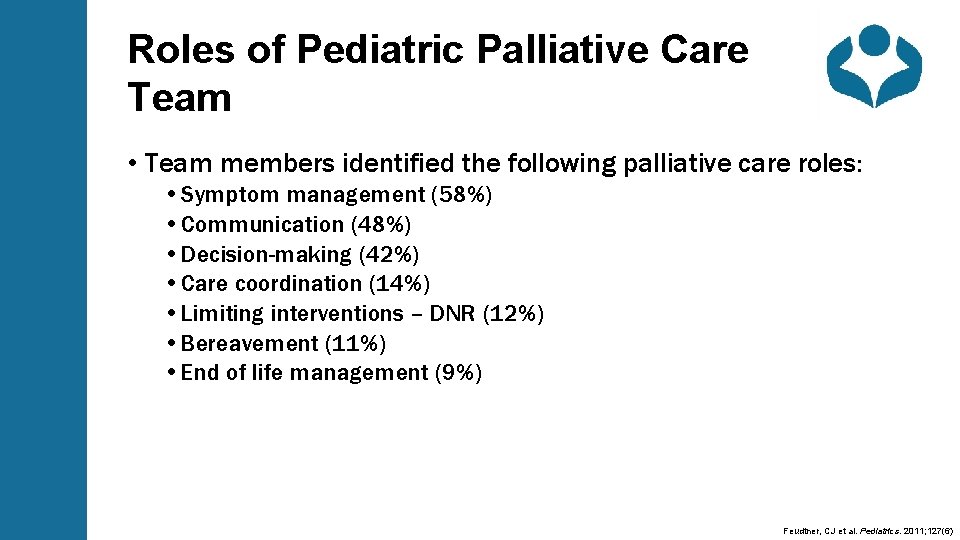
Roles of Pediatric Palliative Care Team • Team members identified the following palliative care roles: • Symptom management (58%) • Communication (48%) • Decision-making (42%) • Care coordination (14%) • Limiting interventions – DNR (12%) • Bereavement (11%) • End of life management (9%) Feudtner, CJ et al. Pediatrics. 2011; 127(6)
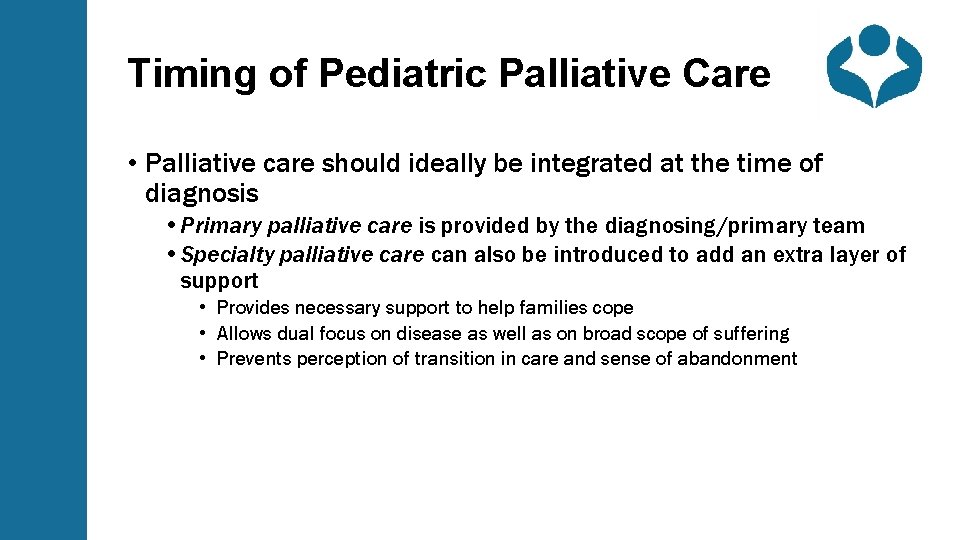
Timing of Pediatric Palliative Care • Palliative care should ideally be integrated at the time of diagnosis • Primary palliative care is provided by the diagnosing/primary team • Specialty palliative care can also be introduced to add an extra layer of support • Provides necessary support to help families cope • Allows dual focus on disease as well as on broad scope of suffering • Prevents perception of transition in care and sense of abandonment
Language for Introducing Pediatric Palliative Care to Families • "PPC is the part of care for children with serious illness that focuses on: • Helping patients and families manage the symptoms and stress of serious illness • Providing an extra layer of psychosocial support • Spending time with patients and families to help them understand the disease and treatment options"
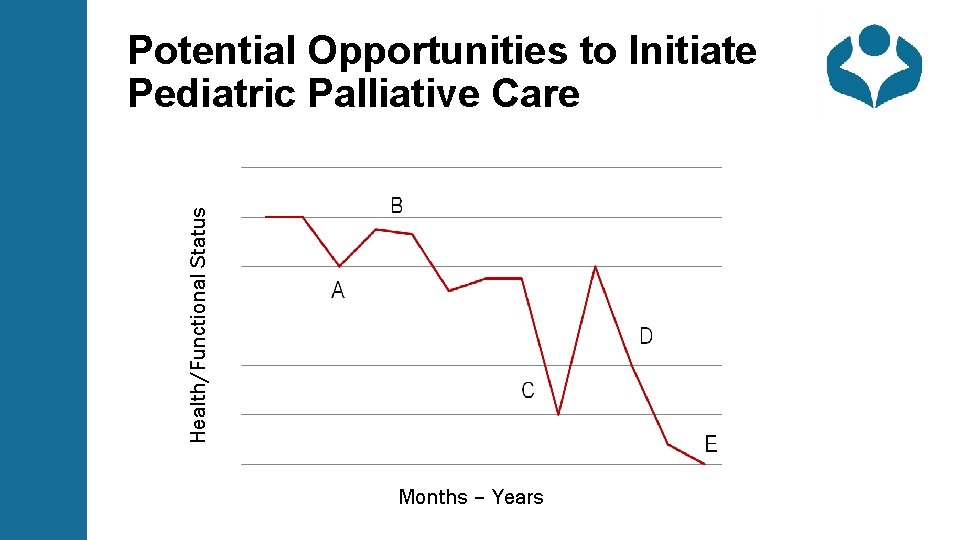
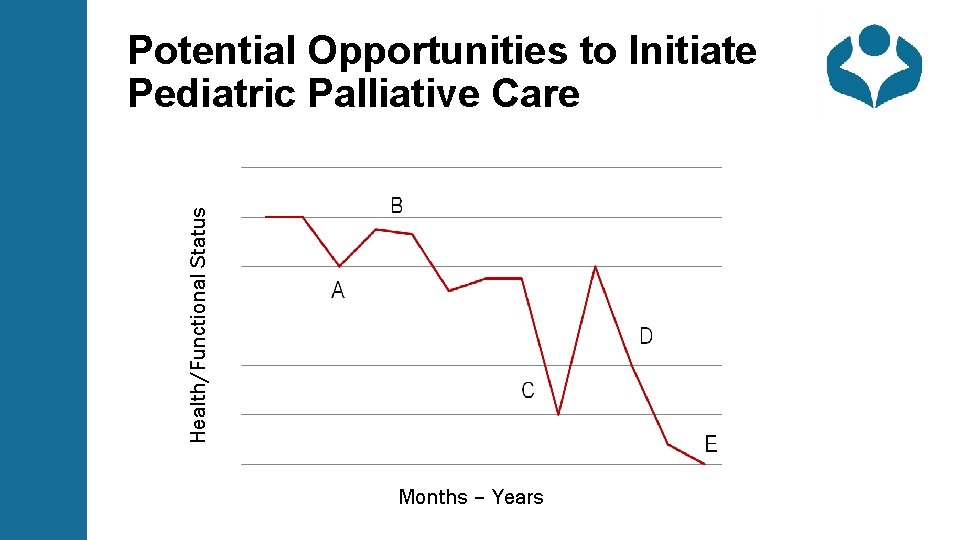
Health/Functional Status Potential Opportunities to Initiate Pediatric Palliative Care Months – Years
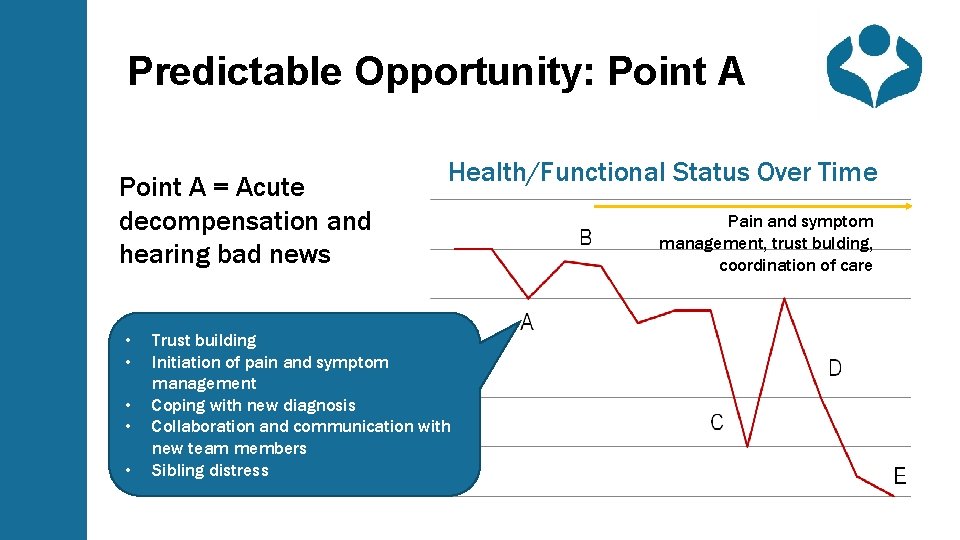
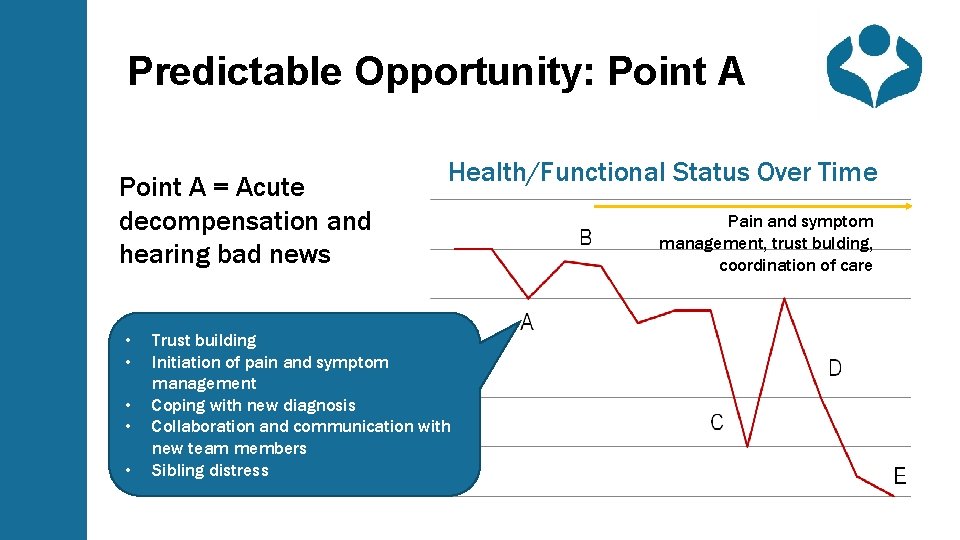
Predictable Opportunity: Point A = Acute decompensation and hearing bad news • • • Health/Functional Status Over Time Trust building Initiation of pain and symptom management Coping with new diagnosis Collaboration and communication with new team members Sibling distress Pain and symptom management, trust bulding, coordination of care
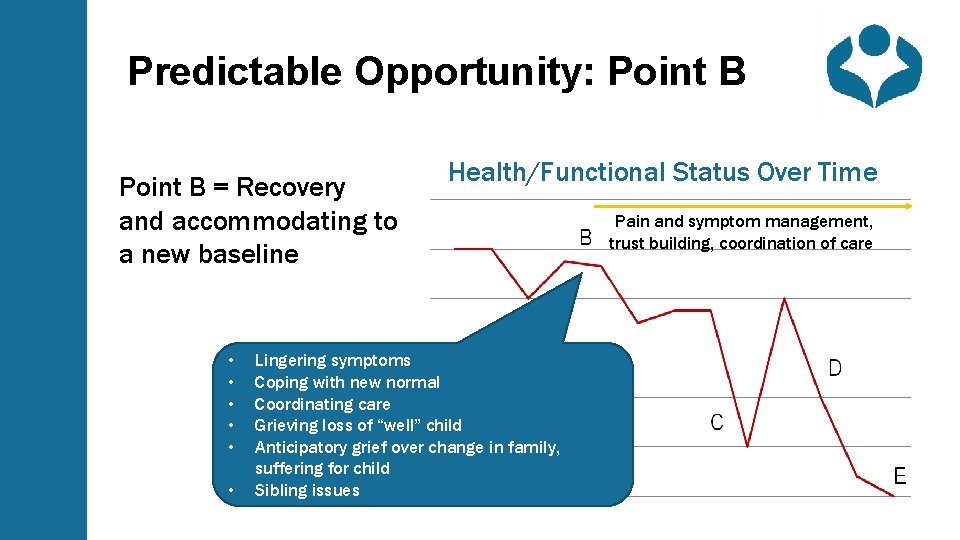
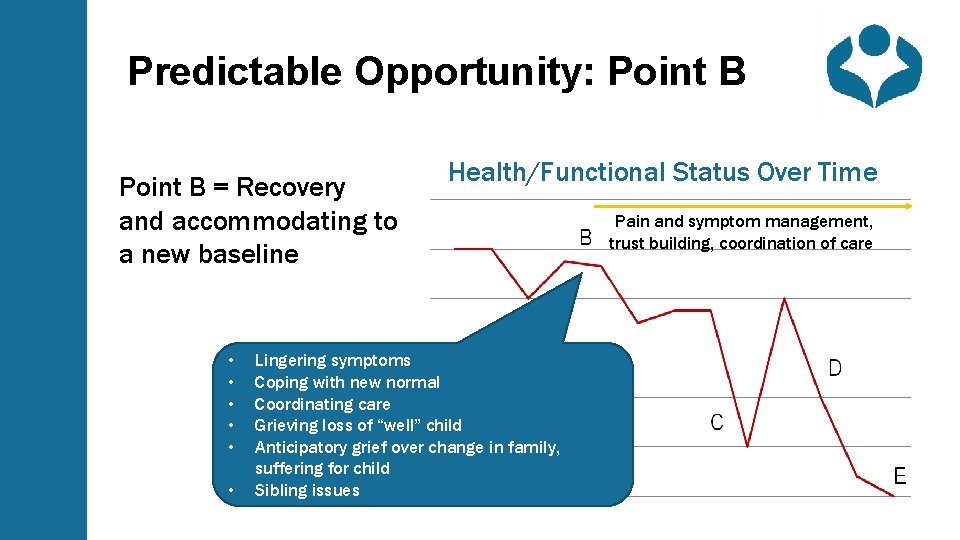
Predictable Opportunity: Point B = Recovery and accommodating to a new baseline • • • Health/Functional Status Over Time Lingering symptoms Coping with new normal Coordinating care Grieving loss of “well” child Anticipatory grief over change in family, suffering for child Sibling issues Pain and symptom management, trust building, coordination of care
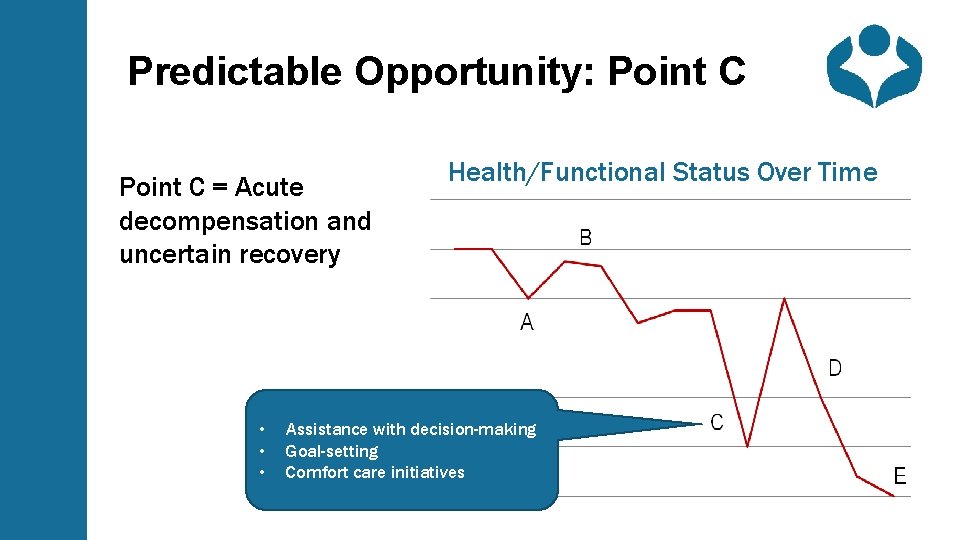
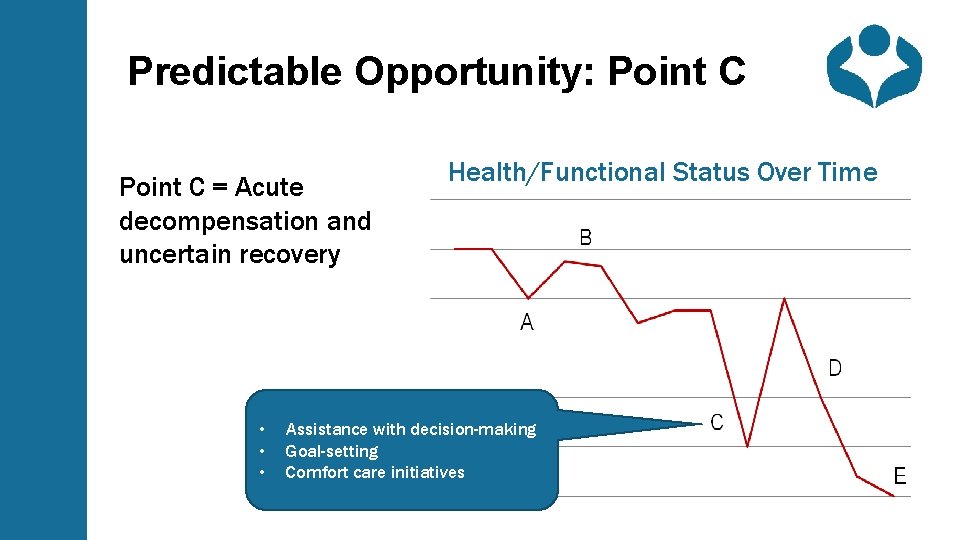
Predictable Opportunity: Point C = Acute decompensation and uncertain recovery • • • Health/Functional Status Over Time Assistance with decision-making Goal-setting Comfort care initiatives
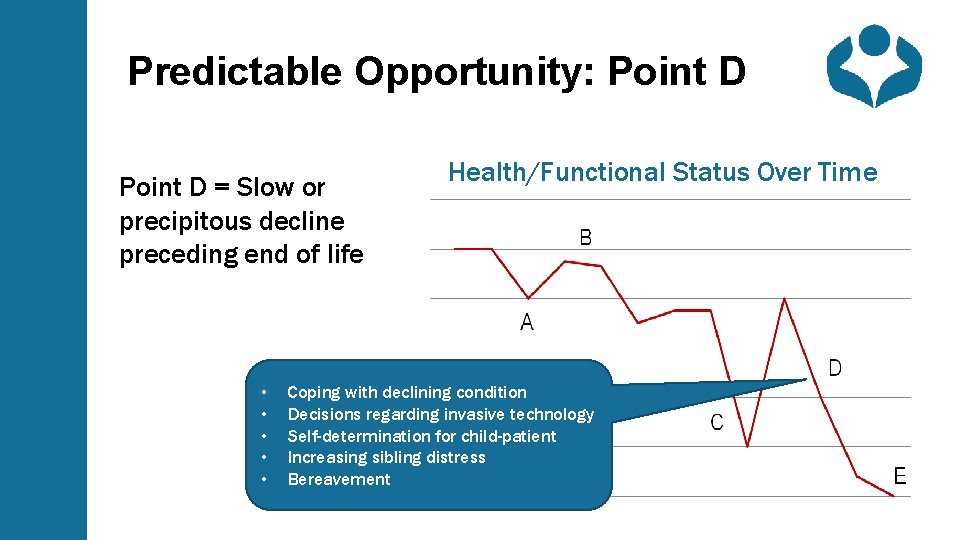
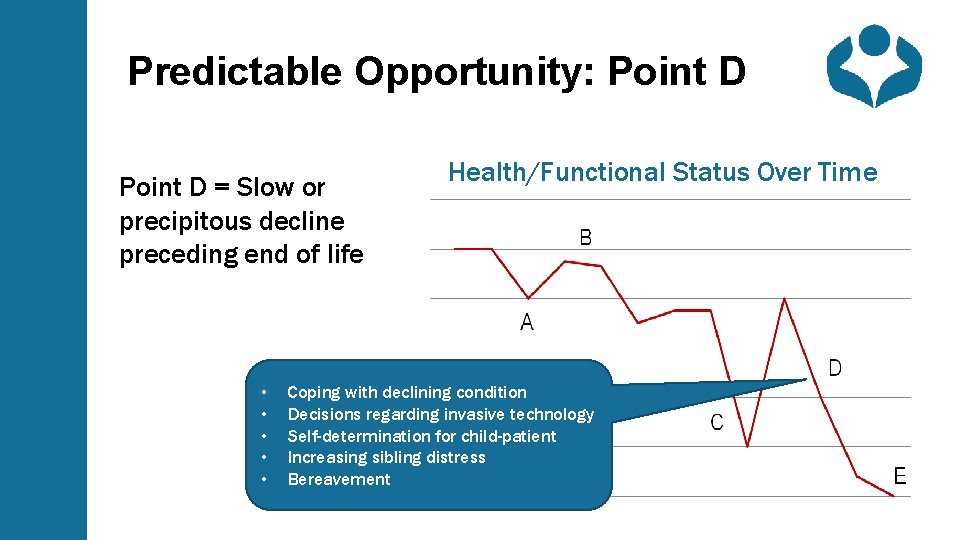
Predictable Opportunity: Point D = Slow or precipitous decline preceding end of life • • • Health/Functional Status Over Time Coping with declining condition Decisions regarding invasive technology Self-determination for child-patient Increasing sibling distress Bereavement
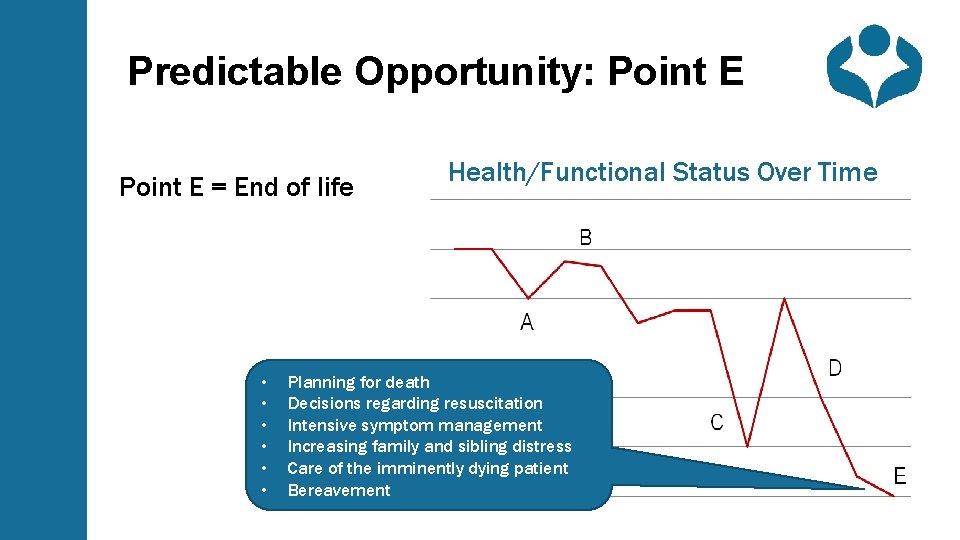
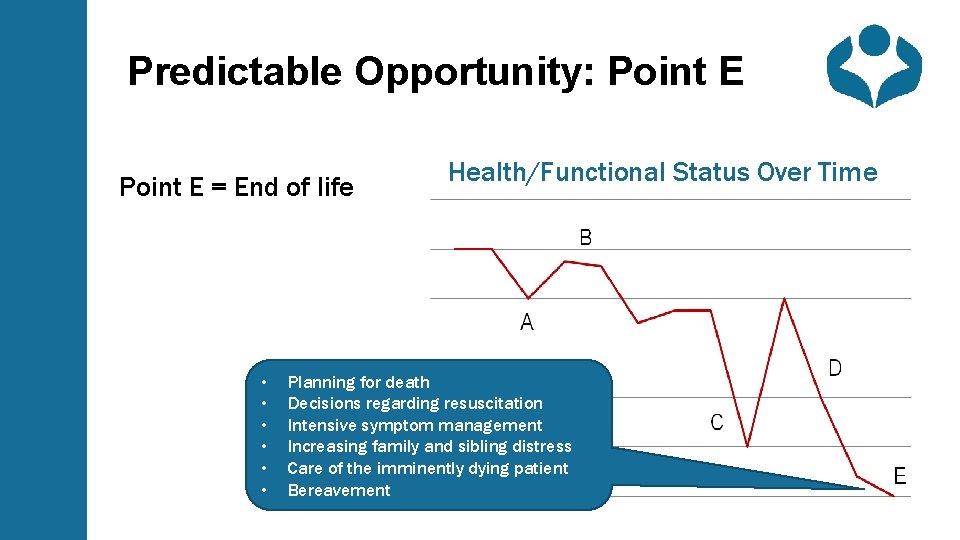
Predictable Opportunity: Point E = End of life • • • Health/Functional Status Over Time Planning for death Decisions regarding resuscitation Intensive symptom management Increasing family and sibling distress Care of the imminently dying patient Bereavement
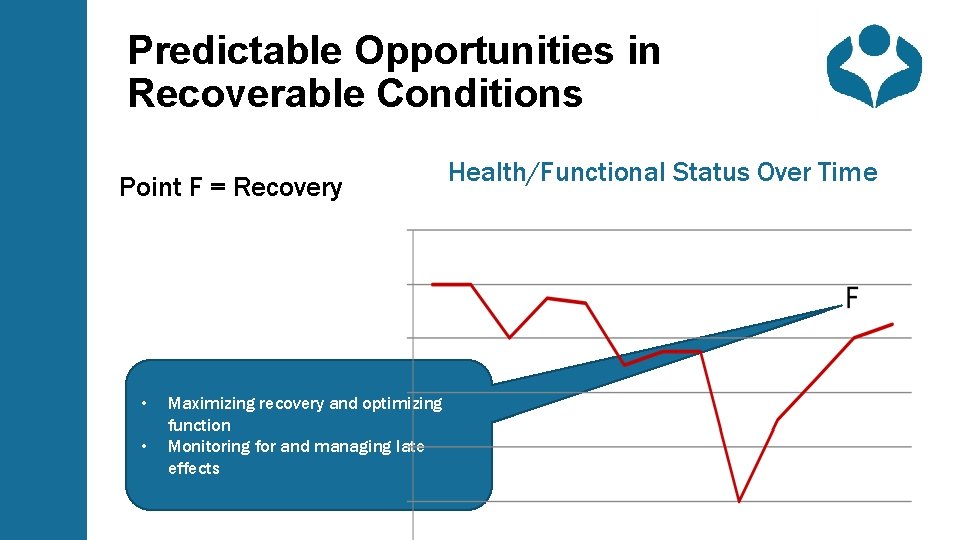
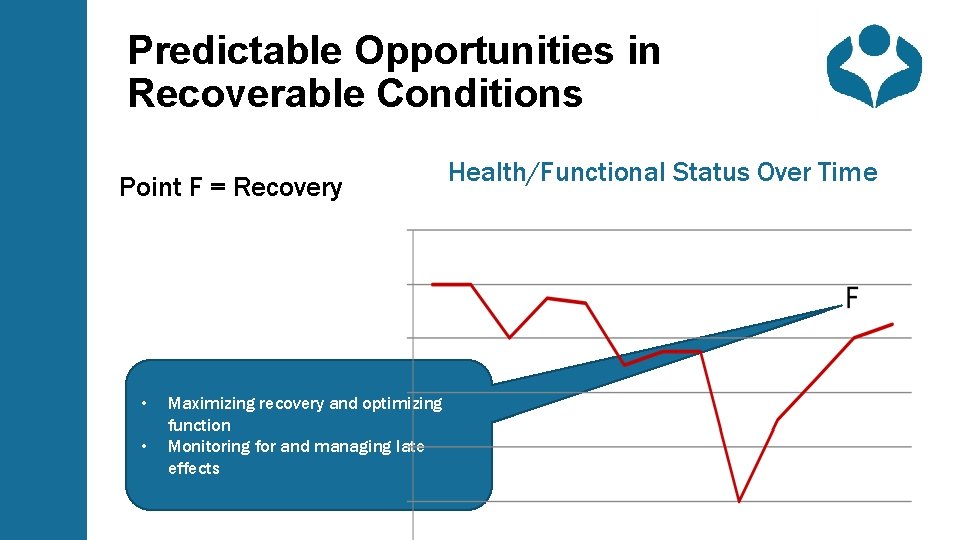
Predictable Opportunities in Recoverable Conditions Point F = Recovery • • Maximizing recovery and optimizing function Monitoring for and managing late effects Health/Functional Status Over Time
Prognostic Considerations - 1 • Most parents want prognostic information • Although many parents find prognostic information upsetting, they generally want to hear about it • PPC team can hold space for difficult emotions and help team adapt to informational needs of the parents • Prognosis can help to relieve uncertainty, which can help to form realistic hopes and support peace of mind • Prognostic information helps inform discussions • Information helps parents to prepare for the future and make decisions about care • Without realistic information about prognosis, parents tend to: • Choose aggressive therapies with low likelihood of benefit at the end of life • Experience regrets later about decisions made under false expectations
Prognostic Considerations - 2 • Prognostication in neurological disease is complex • Definitive biomarkers that accurately predict degree of future impairment are uncommon • Outcomes are mediated by neuronal plasticity, home environment, and early intervention. • Discussion of best case vs worst case vs most likely case of outcome is recommended to help communicate expectations in the setting of prognostic uncertainty
Prognostic Considerations - 3 • When communicating about prognosis, start by asking what the patient and family understand: • “As you think about this illness, what do you think is likely ahead? ” • “What have the other doctors told you about what to expect? ” • Then, ask what the patient and family want to know: • “Would it be helpful to talk about what this illness may mean for the future? ” • Depending on the age of the child, parents may need information about the level of impairment/disability expected in the future • Be prepared for patient/family to decline invitation
Discussing Resuscitation Status - 1 • Elicit understanding of prognosis • Use hypothetical circumstances to discern goals of care in light of understanding of prognosis • Make a recommendation regarding what good care would look like that is consistent with identified values
Discussing Resuscitation Status - 2 • Example: “As difficult as this is to say, in light of my understanding of your child’s medical condition, if his heart should stop, I believe that would mean that he has reached the natural end of his life. As such, I would recommend that he receive comfort measures and not treatment that would prolong his life artificially. Does that care plan seem reasonable to you? ”
Hope • Hopes can differ between parents and child • When parents' hopes are unattainable, clinicians can help them to shift the focus to realistic goals like avoidance of pain/suffering • Conflicting hopes can exist simultaneously • Parents can still have hope, even when death is imminent • Examples of how to discuss hope with parents • “In light of what we have been talking about, what are you hoping for? What are your worries? ” • “Though we are hoping that this next course of treatment will be helpful, it is also important to consider what outcomes are possible. ”
Pain Management - 1 • Total pain is a composite of different types of pain: • Physical pain (somatic, visceral, neuropathic) • Psychological pain • Spiritual/existential pain • Social Pain • Non-physical pain symptoms may manifest as reports of worsened physical pain • Interdisciplinary team can help to address various aspects of non-physical pain
Pain Management - 2 • For physical pain, combine integrative modalities with pharmacological approaches • Touch (parental cuddle, massage) • Heat/cold • Biofeedback, relaxation exercises • Supportive counseling • Remember to consider neurologic etiologies of pain • Neuropathic pain • Sensitization • Anxiety can amplify pain
Pain Management - 3 • Opioids are widely used in PPC • General principles regarding opioids in PPC • Specific dosing considerations in neonates related to pharmacokinetics • Delayed maturation of hepatic enzyme systems, decreased GFR, decreased plasma proteins • Reluctance to schedule doses leads to inadequate analgesia • “PRN = patient receives nothing” • Alternative routes of administration are safe and well-tolerated • Sublingual, buccal, intranasal, transdermal, rectal • Analgesia can be balanced with sedation • Opioid rotation can reduce dose-limiting side effects
Pain Management - 4 • Clinician and parent fear of adverse effects of opioids may act as barriers to their appropriate use • Ileus/constipation • Over-sedation/respiratory depression • Addiction • Perception of giving up/hastening death (at end of life) • Proper management can address these fears
Clinician Well-being • Working with seriously ill and dying children and their families can be emotionally and spiritually challenging. • Particularly in neurology, children suffer from diseases that cause losses of meaningful abilities. • Teams must develop reliable strategies to support each other and allow for processing.
Summary • There a few a key differences between adult and pediatric palliative care • There are predictable opportunities along pediatric neurologic disease trajectories can benefit from palliative care involvement. • Prognostic considerations and discussions of hope are especially important in PPC • Opioids are widely used in PPC
Key References & Reading American Academy of Pediatrics statement on Palliative Care for Children https: //pediatrics. aappublications. org/content/106/2/351 Creutzfeldt CJ, Kluger BM, Holloway RG, eds. Neuropalliative Care: A guide to improving the lives of patients and families affected by neurologic disease. Cham, Switzerland: Springer; 2019. Friedrichsdorf, S, Remke, S, Hauser, J and Wolfe, J, eds, EPEC-Pediatrics. www. epec. net Friedrichsdorf SJ, Remke S, Hauser J, Foster L , Postier A, Kolste A, Wolfe J. Development of a Pediatric Palliative Care Curriculum and Dissemination Model: Education in Palliative and End-of-Life Care (EPEC) Pediatrics. J Pain Symptom Management 2019 Oct; 58(4): 707 -720. Feudtner C, Kang TI, Hexem KR, Friedrichsdorf SJ, Osenga K, Siden H, Friebert SE, Hays RM, Dussel V, Wolfe J. Pediatric palliative care patients: a prospective multicenter cohort study Pediatrics; 2011 Jun; 127(6): 1094 -101. Feudtner C. The breadth of hopes. N Engl J Med. 2009 Dec 10; 361(24): 2306 -7. Lemmon ME, Bross. Pediatric Neurology chapter. NINR Conversations Matter https: //www. ninr. nih. gov/newsandinformation/conversationsmatter/conversations-matter-newportal Pediatric Palliative Care at a Glance https: //www. ninr. nih. gov/sites/files/docs/NINR_508 c_Ata. Glance. pdf
For more information visit: www. EPEC. net or www. inpcs. org The information found in this module complements Chapter 10: Child Neurology, in Creutzfeldt CJ, Kluger BM, Holloway RG, eds. Neuropalliative Care: A guide to improving the lives of patients and families affected by neurologic disease. Cham, Switzerland: Springer; 2019.