General Pathology PATH 303 Lecture 11 q HAEMODYNAMIC
- Slides: 58
General Pathology (PATH 303) Lecture # 11 q HAEMODYNAMIC DISORDERS
HAEMODYNAMIC DISORDERS Normal blood circulation brings nutrients and oxygen to cells and tissues, removes wastes and maintains fluid balance in the body: Fluid homeostasis or fluid balance: Depending upon the species, sex and age of the animal 60% body weight is water, divided into intra and extracellular fluid compartments. Intracellular fluid – 40%, interstitial 15%, intravascular 5%. Common haemodynamic disorders are: hyperemia, congestion, haemorrhage, thrombosis, embolism, infarction, edema and shock.
Hyperemia and congestion: Both these terms indicate increased blood in the blood vessels of a tissue or organ. Hyperemia is an active process due to increased blood flow and arteriolar dilation whereas congestion is passive due to defective or incomplete venous drainage. Both the conditions maybe local or general; hyperemia is usually acute but congestion may be acute or chronic.
Hyperemia: An increased amount of blood in the arterial side of the vascular system. It is usually acute and may be general or local. i) General hyperemia: An increased amount of blood in the arterial system throughout the body. Causes: 1) Acute systemic diseases e. g. pasteurellosis (HS) and erysipelas. 2) Renal diseases.
Appearance: Macroscopic appearance: The affected tissues and organs are increased in size, warm and bright red. Arteries are distended with blood. Microscopic appearance: Arteries and capillaries are dilated and filled with blood.
ii) Acute local hyperemia: Increased amount of blood in the arterial system within a local area e. g. leg, stomach or lung etc. It is the most common type of hyperemia. Causes: Physiological: Lactating mammary gland, stomach and intestine after meal and in muscles during exercise. Pathological: The first stage of inflammation. Gross appearance: The affected part is swollen, warmer, heavier and bright red, blood vessels are distended with blood.
Microscopic appearance: The arteries contract after death and become empty. Therefore, acute hyperemia is difficult to observe in dead animals. It is seen as cardinal signs of inflammation. Significance: Hyperemia is beneficial in an area of inflammation because; It brings increased amounts of oxygen nutrients, leukocytes and antibodies. It dilutes the irritant (venom or toxin) It removes the waste products. Hyperemia disappears as soon as the cause is removed.
Passive congestion: Increased amount of blood in the veinous side of vascular system due to hindrance in the outflow of venous blood. It may be acute or chronic and local or general.
Acute general passive congestion: Increased amount of blood in the venous blood circulation. Causes: 1 - Degeneration and necrosis of myocardium 2 - Myocardial infarcts due to a thrombus or an embolus 3 - Acute pneumonia, capillaries in the lung are compressed and flow of blood is retarded. 4 - Hydropericardium or hemopericardium 5 - Hydrothorax or hemothorax.
Contd… Gross appearance: All organs are bluish red (cyanotic) due to increased venous blood. On incision, blood oozes out. Microscopic appearance: Veins and capillaries are distended and filled with blood.
Chronic general passive congestion: Increased amount of blood in the veinous side which persists for a long tissue, causing fibrosis and atrophy. Causes: Valvular stenosis and insufficiencies Heart failure due to myocardial necrosis or lesions in the conduction system Anomalies of heart e. g. persistent foramen ovale and septal defects Constrictive lesions of pericardium e. g. traumatic pericarditis. Some of the lung lesions causing general chronic congestion include: Pneumonia, emphysema and pneumoconeoses. In these conditions pulmonary capillaries are compressed, hindering the flow of blood through the lungs.
Pathogenesis: Chronic passive congestion causes long standing hypoxia and serious, harmful effects in tissues and organs including edema, necrosis, atrophy and fibrosis. As the veinous circulation slows down, capillary endothelial cells are deprived of oxygen and nutrients and undergo degeneration. This leads to leaking of fluid and proteins into the interstitial space (edema). According to the severity of congestion (stasis) the delicate parenchymal cells undergo necrosis or atrophy but more resistant cells like fibroblasts undergo hyperplasia (fibrosis). The gross and microscopic changes are pronounced in liver, lung and spleen.
Chronic passive congestion in lungs: Lungs are usually affected in the left-sided hearth failure, due to lesions, of bicuspid (mitral) value. Small numbers of RBCs escape from distended capillaries into the pulmonary alveoli. These are engulfed by alveolar macrophages which produce hemosiderin – called heart failure cells. The alveolar septae become thickened due to FCT proliferation and lungs become quite firm and brownish in colour – called brown induration of lungs.
Liver: Chronic passive congestion of liver is usually caused by right-sided hearth failure due to lesions of tricuspid valve or lesions in the lungs. The liver is increased in size and weight. The central veins and the surrounding sinusoids are distended, filled with blood and dark red in colour. The congested central areas are surrounding by pale hypoxic areas resembling a nutmeg (called nutmeg liver).
Microscopically: The central veins and surrounding sinusoids are distended with blood and the hepatocytes deprived of oxygen (hypoxia) undergo necrosis and atrophy whereas peripheral hepatocytes suffer less hypoxia and develop fatty change. If the animal survives for a considerable time, fibrosis develops around the central veins – called cardiac cirrhosis.
Local passive congestion: An increased amount of blood in the veins of an area e. g. tail, kidney, spleen, intestine etc. Causes: 1 - Compression of veins due to malposition of viscera such as torsion, intussusception 2 - External pressure from ligatures, tumours, cysts etc.
Appearance: Gross appearance: Veins are engorged with blood and endothelial cells of blood vessels undergo necrosis, haemorrhages and edema. In the digestive tract, putrefactive bacteria invade the dead tissues and cause gangrene. Microscopic appearance: The veins and capillaries are distended and filled with blood. Necrosis and suppurative inflammation maybe present.
Haemorrhage: 1. 2. Haemorrhage (extravasation) is escape of blood from a blood vessel. Two types are recognized: Haemorrhage by rhexis: There is rupture or break in a blood vessel. Haemorrhage by diapedesis: When there is no break in the vessel. RBCs leave one by one causing small haemorrhages.
Causes: 1 - Trauma caused by mechanical injuries like incision, lacerations, contusions and ruptures etc. 2 - Bacterial and viral infections: Toxins of different bacteria like Salmonella, Clostridium, Pasteurella, Streptococcus, especially in septicemias. 3 - Toxic chemical agents e. g. arsenic. 4 - Haemorrhagic diathesis – or bleeding disorders involving Vascular fragility – Vitamin C deficiency in G. pigs and monkeys. Reduced platelet numbers Defective platelet function Abnormalities in clotting factors 5 - Necrosis and destruction of vessel walls e. g. arteriosclerosis, aneurysms 6 - Neoplasms may attack blood vessels. But most neoplasms have tendency to bleed due to immature blood vessels.
Classification of haemorrhage according to source, size and location: Source: Cardiac, arterial, venous, capillary etc. Size: Petechiae are pinpoint, punctate, 1 -2 mm in diameter Echymotic (echymoses) – about 1 -2 cm in diameter Haematoma and haematocysts – accumulation of blood within a tissue or cyst. Suffusions are large, diffuse haemorrhages Linear haemorrhages appear as lines on the crests of mucosal folds in the intestine Agonal haemorrhages are petechiae and echymoses associated with death after struggling.
Location: Maybe perirenal, subcapsular, subcutaneous. Prefix “haemo” indicates haemorrhages as in haemopericardium, haemothorax. Bleeding from nose is epistaxis, from mouth haematemesis, haemoptysis is bleeding in sputum. Haematocele is bleeding in tunica vaginalis. Malena is passing of dark, digested blood in stool (upper digestive tract). Apoplexy is haemorrhage in brain.
Microscopic appearance: Recognized as RBCs outside blood vessels. Chronic haemorrhage is indicated by the presence hemosiderin as golden-brown, granular pigment. It gives Prussian blue reaction when stained with potassium ferrocyanide.
Significance: Significance depends upon volume, rate and site of haemorrhage. Loss of upto 20% of total volume usually has no clinical significance but a small haemorrhage in brain maybe fatal. Loss of a large volume of blood may cause hypovolemic shock. Haemorrhage in the pericardial sac and in the respiratory tract is also fatal.
General Pathology (PATH 303) Lecture # 12 q HAEMODYNAMIC DISORDERS
HAEMODYNAMIC DISORDERS Normal blood circulation brings nutrients and oxygen to cells and tissues, removes wastes and maintains fluid balance in the body: Fluid homeostasis or fluid balance: Depending upon the species, sex and age of the animal 60% body weight is water, divided into intra and extracellular fluid compartments. Intracellular fluid – 40%, interstitial 15%, intravascular 5%. Common haemodynamic disorders are: hyperemia, congestion, haemorrhage, thrombosis, embolism, infarction, edema and shock.
Hyperemia and congestion: Both these terms indicate increased blood in the blood vessels of a tissue or organ. Hyperemia is an active process due to increased blood flow and arteriolar dilation whereas congestion is passive due to defective or incomplete venous drainage. Both the conditions maybe local or general; hyperemia is usually acute but congestion may be acute or chronic.
Hyperemia: An increased amount of blood in the arterial side of the vascular system. It is usually acute and may be general or local. i) General hyperemia: An increased amount of blood in the arterial system throughout the body. Causes: 1) Acute systemic diseases e. g. pasteurellosis (HS) and erysipelas. 2) Renal diseases.
Appearance: Macroscopic appearance: The affected tissues and organs are increased in size, warm and bright red. Arteries are distended with blood. Microscopic appearance: Arteries and capillaries are dilated and filled with blood.
ii) Acute local hyperemia: Increased amount of blood in the arterial system within a local area e. g. leg, stomach or lung etc. It is the most common type of hyperemia. Causes: Physiological: Lactating mammary gland, stomach and intestine after meal and in muscles during exercise. Pathological: The first stage of inflammation. Gross appearance: The affected part is swollen, warmer, heavier and bright red, blood vessels are distended with blood.
Microscopic appearance: The arteries contract after death and become empty. Therefore, acute hyperemia is difficult to observe in dead animals. It is seen as cardinal signs of inflammation. Significance: Hyperemia is beneficial in an area of inflammation because; It brings increased amounts of oxygen nutrients, leukocytes and antibodies. It dilutes the irritant (venom or toxin) It removes the waste products. Hyperemia disappears as soon as the cause is removed.
Passive congestion: Increased amount of blood in the veinous side of vascular system due to hindrance in the outflow of venous blood. It may be acute or chronic and local or general.
Acute general passive congestion: Increased amount of blood in the venous blood circulation. Causes: 1 - Degeneration and necrosis of myocardium 2 - Myocardial infarcts due to a thrombus or an embolus 3 - Acute pneumonia, capillaries in the lung are compressed and flow of blood is retarded. 4 - Hydropericardium or hemopericardium 5 - Hydrothorax or hemothorax.
Contd… Gross appearance: All organs are bluish red (cyanotic) due to increased venous blood. On incision, blood oozes out. Microscopic appearance: Veins and capillaries are distended and filled with blood.
Chronic general passive congestion: Increased amount of blood in the veinous side which persists for a long tissue, causing fibrosis and atrophy. Causes: Valvular stenosis and insufficiencies Heart failure due to myocardial necrosis or lesions in the conduction system Anomalies of heart e. g. persistent foramen ovale and septal defects Constrictive lesions of pericardium e. g. traumatic pericarditis. Some of the lung lesions causing general chronic congestion include: Pneumonia, emphysema and pneumoconeoses. In these conditions pulmonary capillaries are compressed, hindering the flow of blood through the lungs.
Pathogenesis: Chronic passive congestion causes long standing hypoxia and serious, harmful effects in tissues and organs including edema, necrosis, atrophy and fibrosis. As the veinous circulation slows down, capillary endothelial cells are deprived of oxygen and nutrients and undergo degeneration. This leads to leaking of fluid and proteins into the interstitial space (edema). According to the severity of congestion (stasis) the delicate parenchymal cells undergo necrosis or atrophy but more resistant cells like fibroblasts undergo hyperplasia (fibrosis). The gross and microscopic changes are pronounced in liver, lung and spleen.
Chronic passive congestion in lungs: Lungs are usually affected in the left-sided hearth failure, due to lesions, of bicuspid (mitral) value. Small numbers of RBCs escape from distended capillaries into the pulmonary alveoli. These are engulfed by alveolar macrophages which produce hemosiderin – called heart failure cells. The alveolar septae become thickened due to FCT proliferation and lungs become quite firm and brownish in colour – called brown induration of lungs.
Liver: Chronic passive congestion of liver is usually caused by right-sided hearth failure due to lesions of tricuspid valve or lesions in the lungs. The liver is increased in size and weight. The central veins and the surrounding sinusoids are distended, filled with blood and dark red in colour. The congested central areas are surrounding by pale hypoxic areas resembling a nutmeg (called nutmeg liver).
Microscopically: The central veins and surrounding sinusoids are distended with blood and the hepatocytes deprived of oxygen (hypoxia) undergo necrosis and atrophy whereas peripheral hepatocytes suffer less hypoxia and develop fatty change. If the animal survives for a considerable time, fibrosis develops around the central veins – called cardiac cirrhosis.
Local passive congestion: An increased amount of blood in the veins of an area e. g. tail, kidney, spleen, intestine etc. Causes: 1 - Compression of veins due to malposition of viscera such as torsion, intussusception 2 - External pressure from ligatures, tumours, cysts etc.
Appearance: Gross appearance: Veins are engorged with blood and endothelial cells of blood vessels undergo necrosis, haemorrhages and edema. In the digestive tract, putrefactive bacteria invade the dead tissues and cause gangrene. Microscopic appearance: The veins and capillaries are distended and filled with blood. Necrosis and suppurative inflammation maybe present.
Haemorrhage: 1. 2. Haemorrhage (extravasation) is escape of blood from a blood vessel. Two types are recognized: Haemorrhage by rhexis: There is rupture or break in a blood vessel. Haemorrhage by diapedesis: When there is no break in the vessel. RBCs leave one by one causing small haemorrhages.
Causes: 1 - Trauma caused by mechanical injuries like incision, lacerations, contusions and ruptures etc. 2 - Bacterial and viral infections: Toxins of different bacteria like Salmonella, Clostridium, Pasteurella, Streptococcus, especially in septicemias. 3 - Toxic chemical agents e. g. arsenic. 4 - Haemorrhagic diathesis – or bleeding disorders involving Vascular fragility – Vitamin C deficiency in G. pigs and monkeys. Reduced platelet numbers Defective platelet function Abnormalities in clotting factors 5 - Necrosis and destruction of vessel walls e. g. arteriosclerosis, aneurysms 6 - Neoplasms may attack blood vessels. But most neoplasms have tendency to bleed due to immature blood vessels.
Classification of haemorrhage according to source, size and location: Source: Cardiac, arterial, venous, capillary etc. Size: Petechiae are pinpoint, punctate, 1 -2 mm in diameter Echymotic (echymoses) – about 1 -2 cm in diameter Haematoma and haematocysts – accumulation of blood within a tissue or cyst. Suffusions are large, diffuse haemorrhages Linear haemorrhages appear as lines on the crests of mucosal folds in the intestine Agonal haemorrhages are petechiae and echymoses associated with death after struggling.
Location: Maybe perirenal, subcapsular, subcutaneous. Prefix “haemo” indicates haemorrhages as in haemopericardium, haemothorax. Bleeding from nose is epistaxis, from mouth haematemesis, haemoptysis is bleeding in sputum. Haematocele is bleeding in tunica vaginalis. Malena is passing of dark, digested blood in stool (upper digestive tract). Apoplexy is haemorrhage in brain.
Microscopic appearance: Recognized as RBCs outside blood vessels. Chronic haemorrhage is indicated by the presence hemosiderin as golden-brown, granular pigment. It gives Prussian blue reaction when stained with potassium ferrocyanide.
Significance: Significance depends upon volume, rate and site of haemorrhage. Loss of upto 20% of total volume usually has no clinical significance but a small haemorrhage in brain maybe fatal. Loss of a large volume of blood may cause hypovolemic shock. Haemorrhage in the pericardial sac and in the respiratory tract is also fatal.
Thrombosis “It is the formation a clotted mass within the cardiovascular system. The mass is called thrombus (plural thrombi)”.
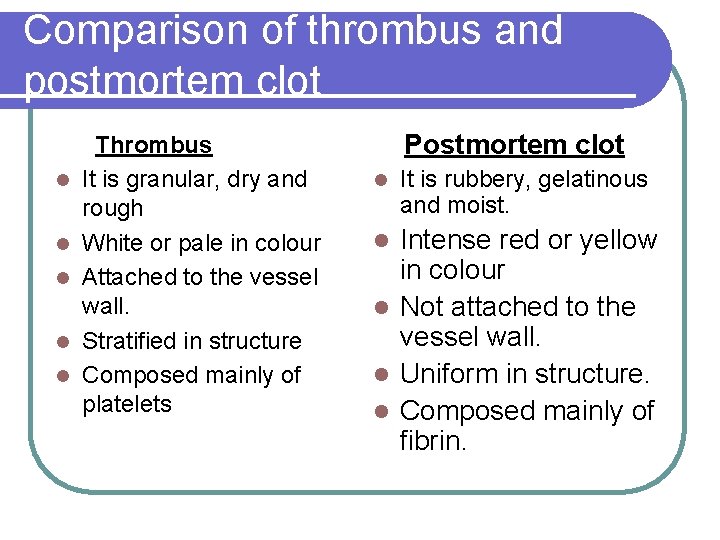
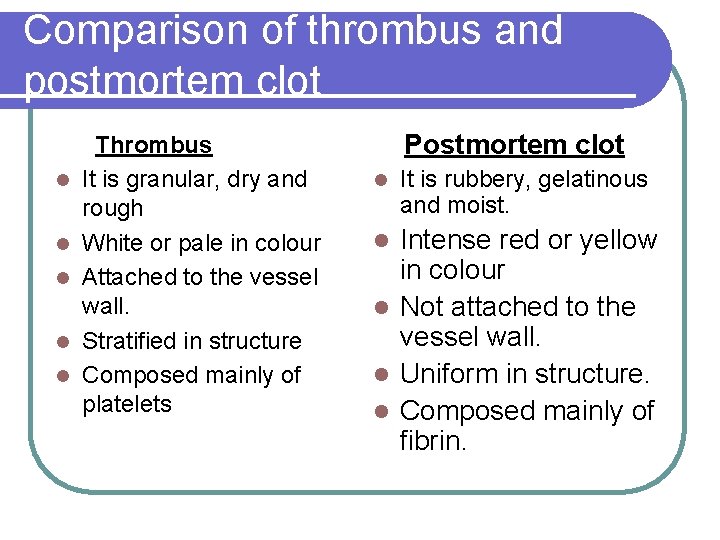
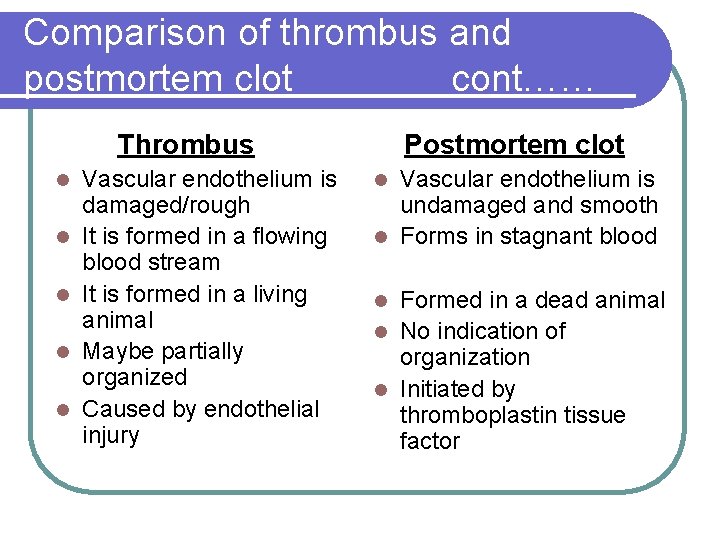
Comparison of thrombus and postmortem clot Thrombus It is granular, dry and rough White or pale in colour Attached to the vessel wall. Stratified in structure Composed mainly of platelets Postmortem clot It is rubbery, gelatinous and moist. Intense red or yellow in colour Not attached to the vessel wall. Uniform in structure. Composed mainly of fibrin.
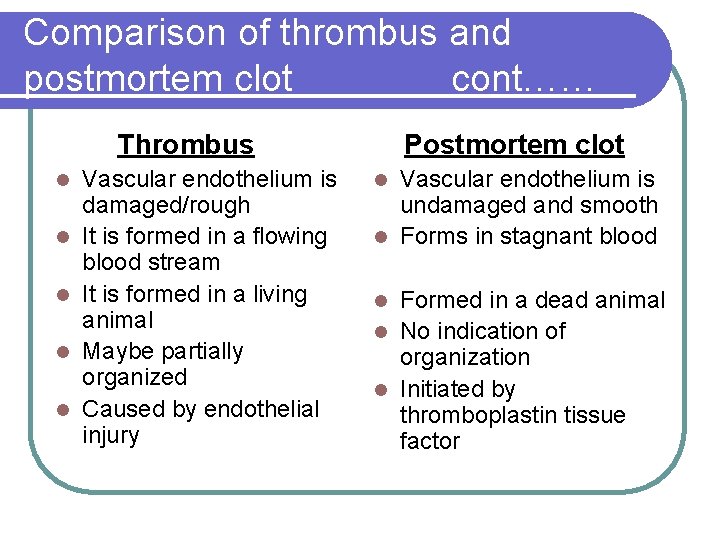
Comparison of thrombus and postmortem clot cont…… Thrombus Vascular endothelium is damaged/rough It is formed in a flowing blood stream It is formed in a living animal Maybe partially organized Caused by endothelial injury Postmortem clot Vascular endothelium is undamaged and smooth Forms in stagnant blood Formed in a dead animal No indication of organization Initiated by thromboplastin tissue factor
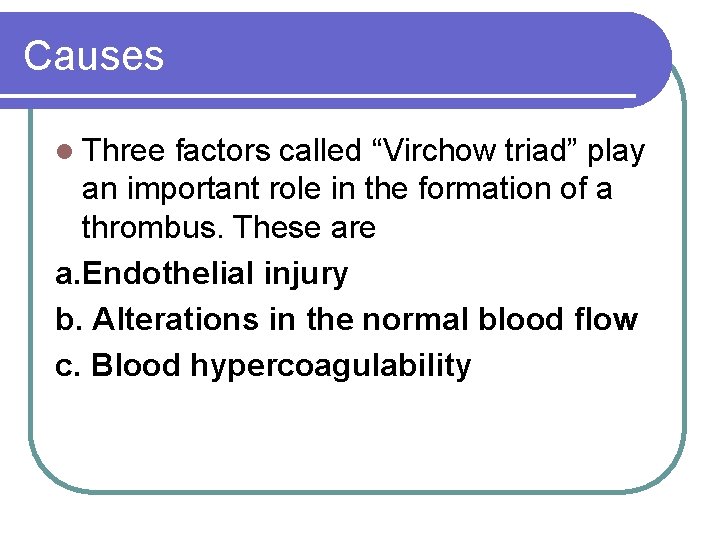
Causes Three factors called “Virchow triad” play an important role in the formation of a thrombus. These are a. Endothelial injury b. Alterations in the normal blood flow c. Blood hypercoagulability
a. Endothelial injury Damage to the endothelium and exposure of subendothelial extracellular matrix (ECM) is important for attachment and activation of platelets to vessel wall. Endothelial injury maybe caused by trauma, parasites, bacteria and arteriosclerosis etc.
b. Alterations in the normal blood flow In the fast or axial flow blood cells or platelets do not come in contact with endothelium. But in slow moving blood stream or laminar flow and stasis, blood cells and platelets come in contact with the endothelium and thrombus formation occurs. This is seen at bifurcation of arteries and in chronic passive congestion
c. Blood hypercoagulability Thrombosis is increased in extensive burns, cancer and suppurative diseases. This maybe due to increased levels of fibrinogen and prothrombin, increased number and stickiness of platelets or decreased levels of inhibitors like fibrinolysin etc.
Pathogenesis 1. 2. 3. 4. 5. Platelets become attached to the site of endothelial injury Platelets become activated, secrete ADP and synthesize thromboxane A 2 ADP stimulates formation of reversible (primary) homeostatic plug of platelets ATP, thrombin and thromboxane A 2 soon convert the primary plug into a large irreversible (secondary) plug. Deposition of fibrin stabilizes the thrombus and attaches it firmly to the site.
Classification of thrombi There are several types and systems for classification of thrombi. e. g. I. Classification according to the location in the circulatory system. Examples are cardiac, arterial, venous, capillary and lymphatic thrombi. ii. According to the location within the heart or blood vessels. Examples are mural (attached to the wall), valvular, lateral, occluding (attached to entire circumference), saddle thrombi (at the bifurcation of a blood vessel) and canalized thrombi (in which blood channels have formed)
Classification cont………. iii. Classification according to infectious agent e. g. septic (contain bacteria), parasites (e. g. S. vulgaris and Dirofilaria immitis), aseptic or bland thrombi. iv. Classification according to colour e. g. white or pale thrombi occur in the heart and large arteries and composed entirely of platelets. A red thrombus is composed of platelets, fibrin, RBC’s and leukocytes. A laminated or mixed thrombus consists of alternating layers of platelets and fibrin mixed with erythrocytes.
Fate of thrombi Thrombi end up in several ways e. g. a. Emboli formation by breaking up (dissolution). Most common type of emboli. b. Abcessation. Pyogenic bacteria when present cause abcessation. c. Organization and recanalization- can reestablish blood flow. d. Calcification- thrombi often undergo dystrophic calcification
Significance 1. 2. 3. 4. Thrombi play beneficial role in controlling hemorrhage. Harmful effects of thrombi depend upon the location, (organ) and size of blood vessel involved. In organs with abundant collateral circulation, thrombi have negligible effect. But in case of end arteries there maybe necrosis and infarction. The most harmful effect of thrombi is embolism. Other harmful effects include edema, atrophy and aneurysm etc.