General Pathology Circulation Disorders II Manifestations Causes of

- Slides: 29
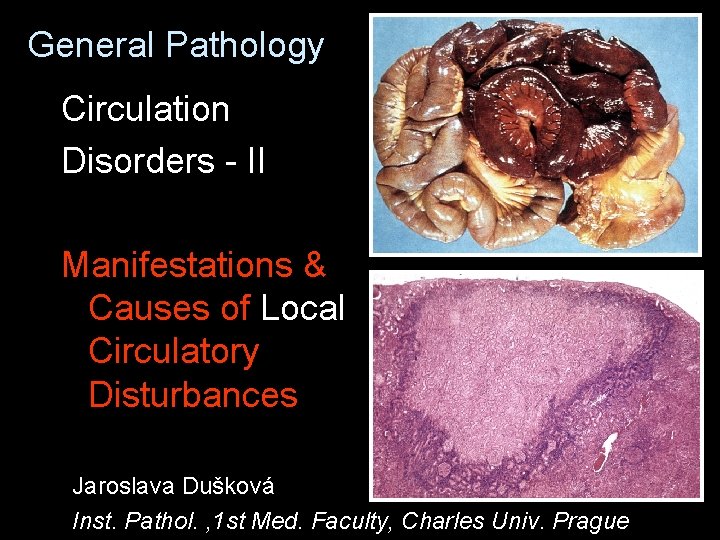
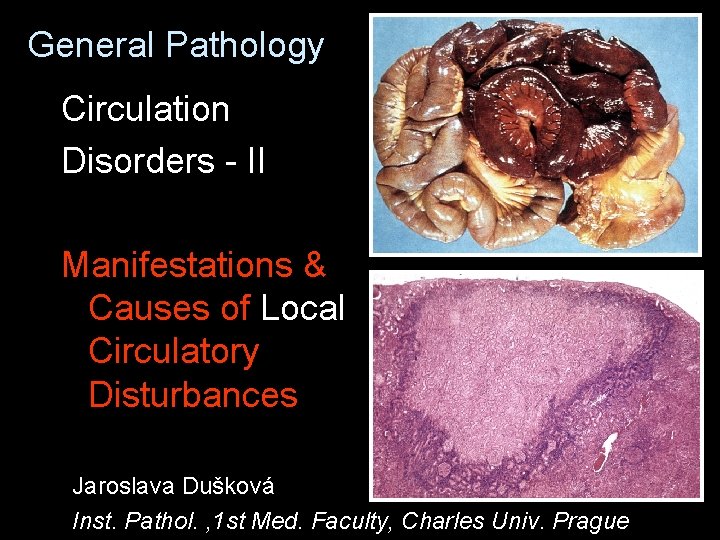
General Pathology Circulation Disorders - II Manifestations & Causes of Local Circulatory Disturbances Jaroslava Dušková Inst. Pathol. , 1 st Med. Faculty, Charles Univ. Prague
Manifestations of Local Circulatory Disturbances v local hyperemia v local anemia LOCAL ISCHEMIA
Manifestations of Local Circulatory Disturbances v local hyperemia – active – passive arterial (fluxe) capillary (peristatic) venous (stasis)
Manifestations of Local Circulatory Disturbances v local anemia – slow development – vascular atrophy – fast development – dystrophy , necrosis
Ischemia – stratification of changes complete necrosis - central part v myomalacia v hyperemia v interstitial leucocyte infiltration – vital reaction v dystrophic steatosis (& glycogenosis) v healthy v
Causes of Local Circulatory Disturbances v local anemia stenosis to occlusion of artery v v lumen wall embolism atherosclerosis, thrombosis (spasmus, depositions, inflammations, tumours) combination of previous neighbourhood compression
Causes of Local Circulatory Disturbances v local hyperemia active w w passive w w w function inflammatory vasodilation (outflow blocade) lumen wall neighbourhood
Thrombosis Def. : intravital intravascular blood clotting Range: parietal obturative
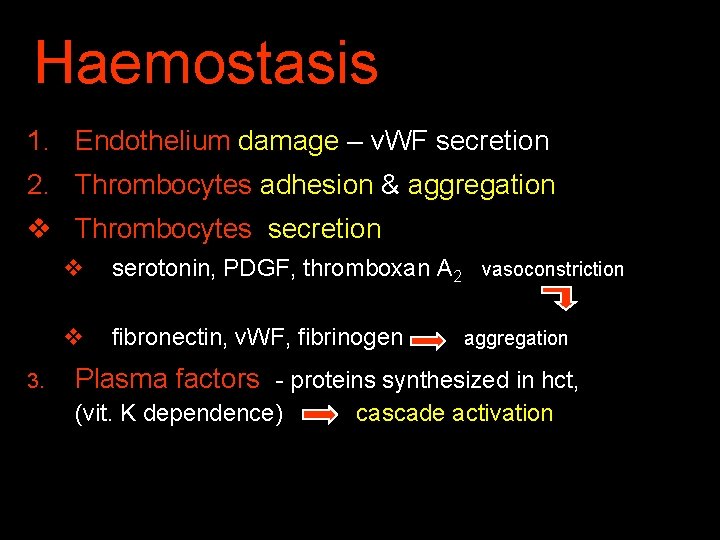
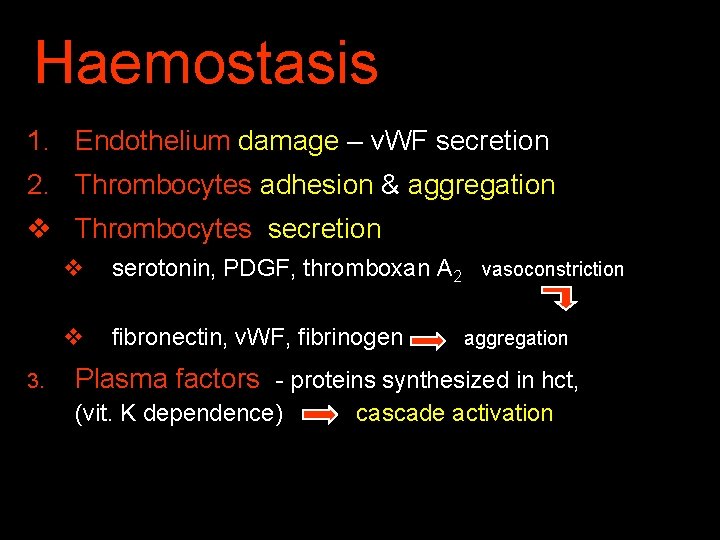
Haemostasis 1. Endothelium damage – v. WF secretion 2. Thrombocytes adhesion & aggregation v Thrombocytes secretion 3. v serotonin, PDGF, thromboxan A 2 vasoconstriction v fibronectin, v. WF, fibrinogen aggregation Plasma factors - proteins synthesized in hct, (vit. K dependence) cascade activation
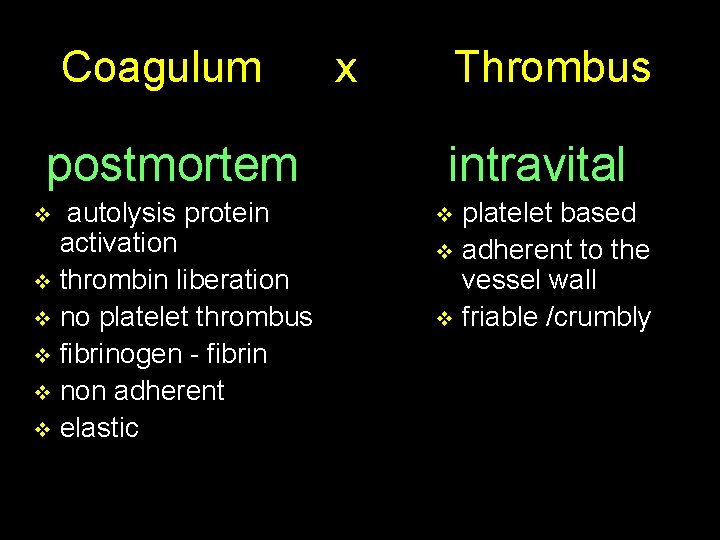
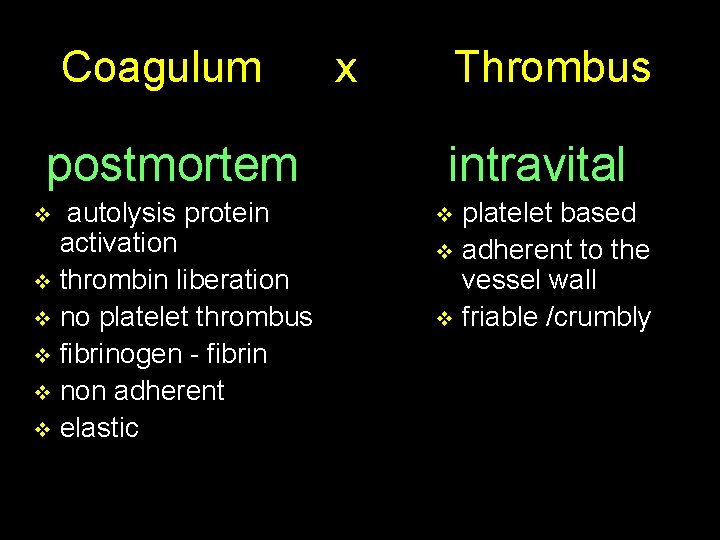
Coagulum postmortem autolysis protein activation v thrombin liberation v no platelet thrombus v fibrinogen - fibrin v non adherent v elastic v x Thrombus intravital platelet based v adherent to the vessel wall v friable /crumbly v
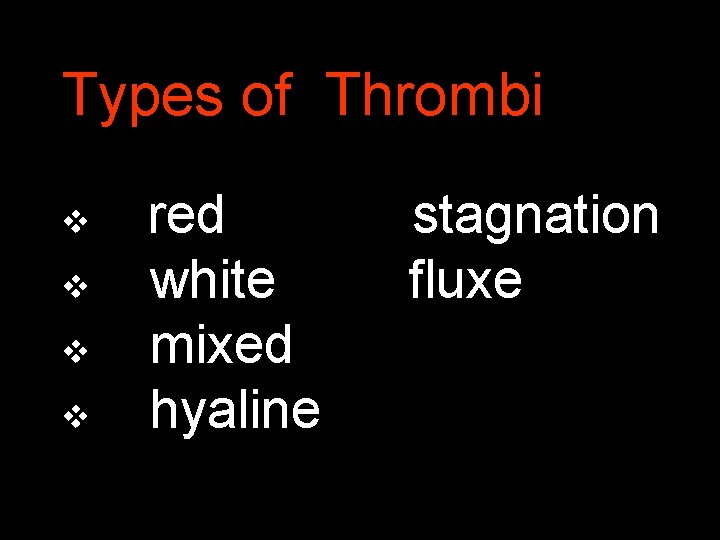
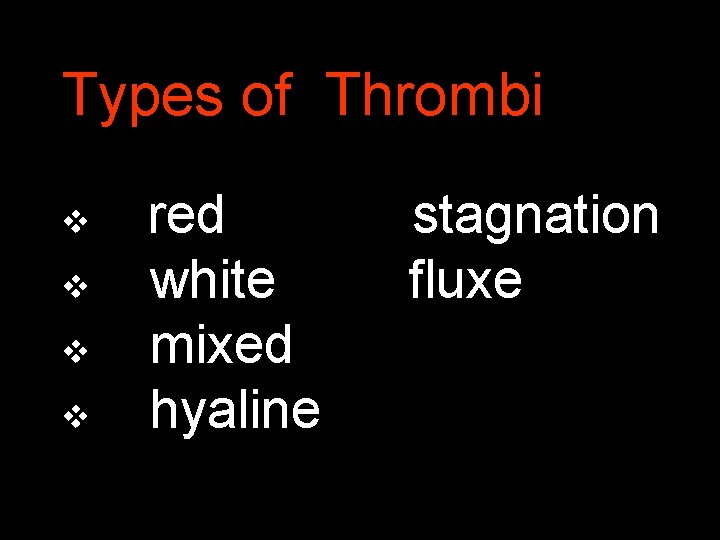
Types of Thrombi v v red white mixed hyaline stagnation fluxe
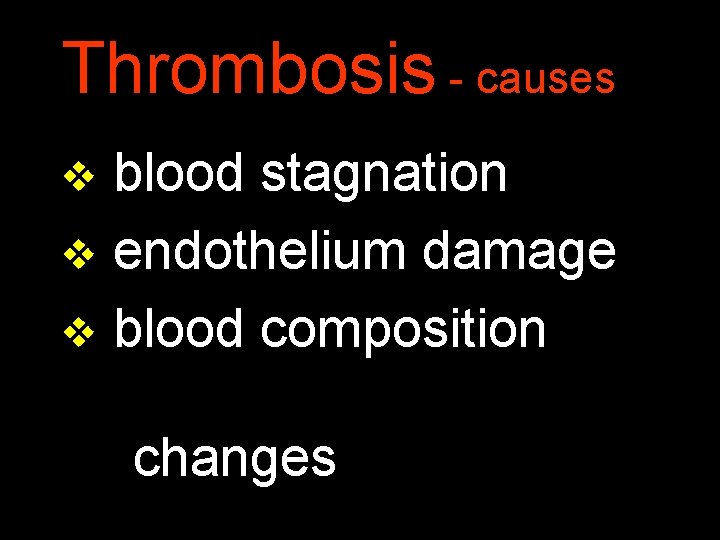
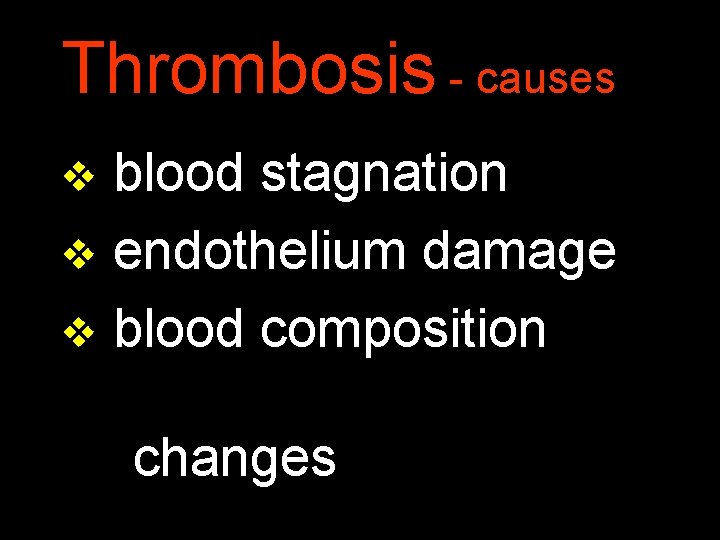
Thrombosis - causes blood stagnation v endothelium damage v blood composition v changes
Thrombosis - causes v blood stagnation – heart failure – vein insufficiency – local factors (compression) laminar flow disturbance
Thrombosis - causes v endothelium damage – atherosclerosis – inflammation – injury – hemodynamic stress – high cholesterol levels
Thrombosis - causes v blood composition changes – increased platelet number (over 400 000/mm 3) – thromboplastin liberation (e. g. following pancreas and lung surgery) – endotoxin - DIC – amniotic fluid embolism – contraceptives……
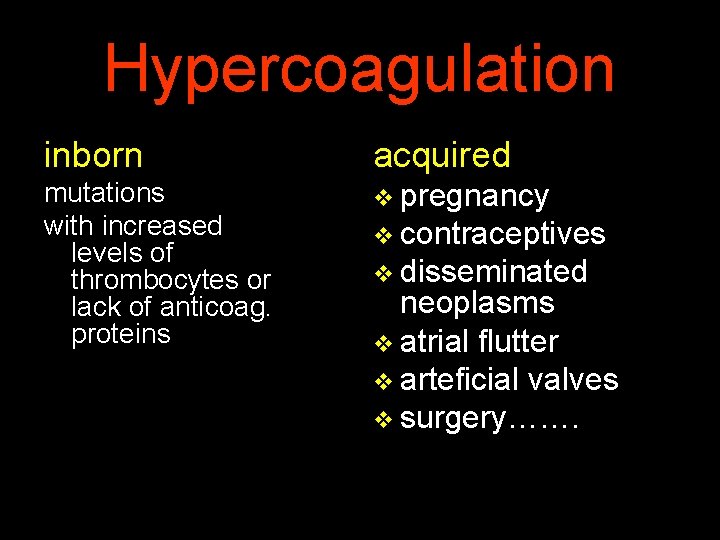
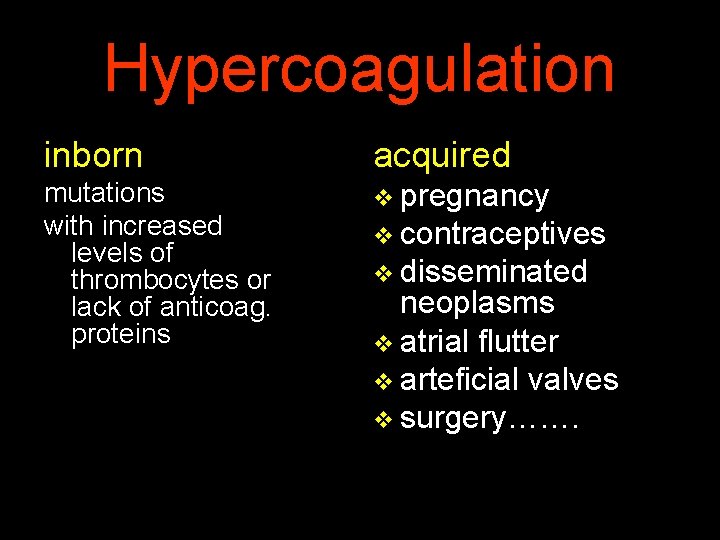
Hypercoagulation inborn acquired mutations with increased levels of thrombocytes or lack of anticoag. proteins v pregnancy v contraceptives v disseminated neoplasms v atrial flutter v arteficial valves v surgery…….
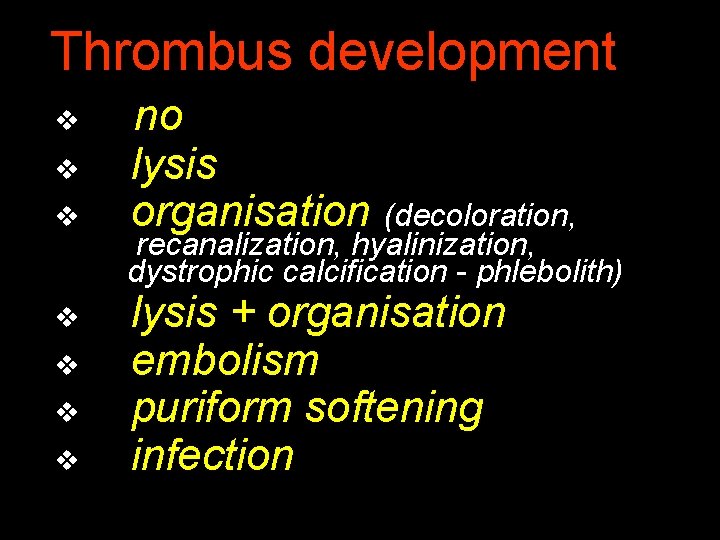
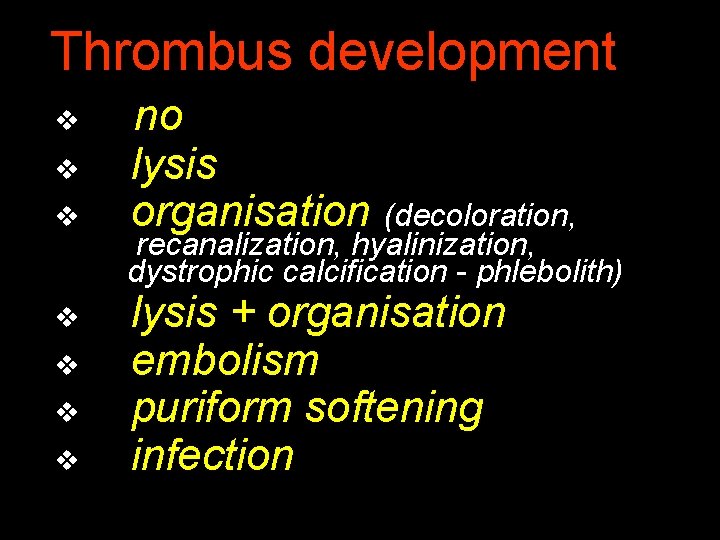
Thrombus development v v v v no lysis organisation (decoloration, recanalization, hyalinization, dystrophic calcification - phlebolith) lysis + organisation embolism puriform softening infection
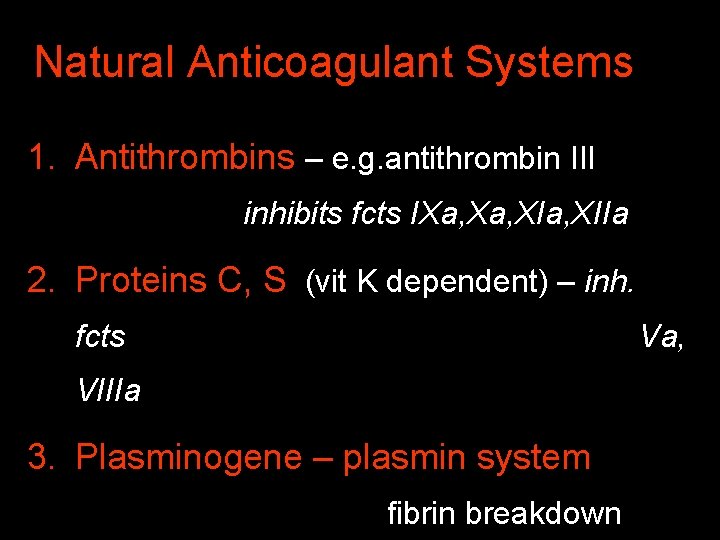
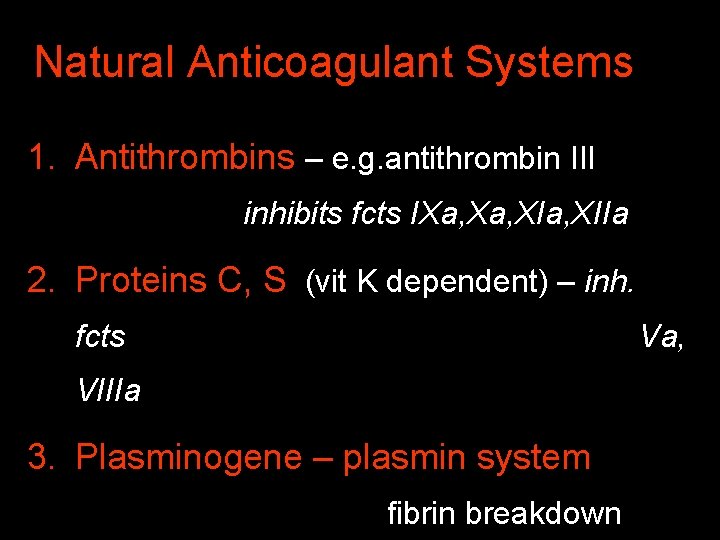
Natural Anticoagulant Systems 1. Antithrombins – e. g. antithrombin III inhibits fcts IXa, XIa, XIIa 2. Proteins C, S (vit K dependent) – inh. fcts Va, VIIIa 3. Plasminogene – plasmin system fibrin breakdown

Embolism Def. : transport of a compact particle in circulation with stopping in the place of anatomic narrowing
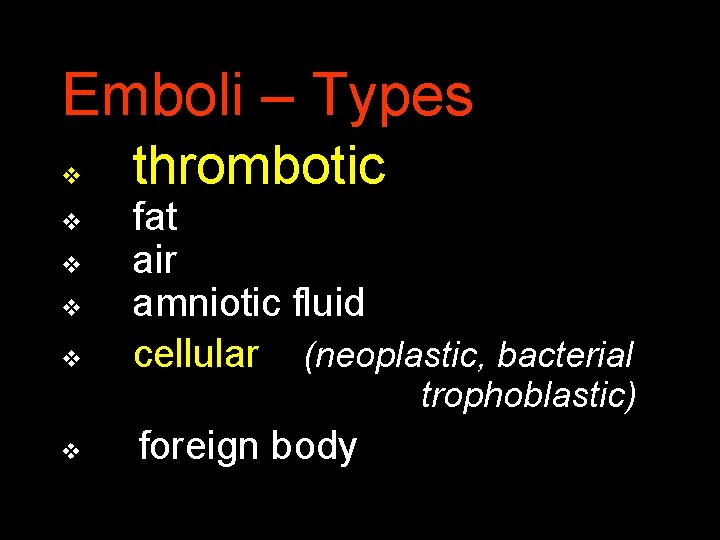
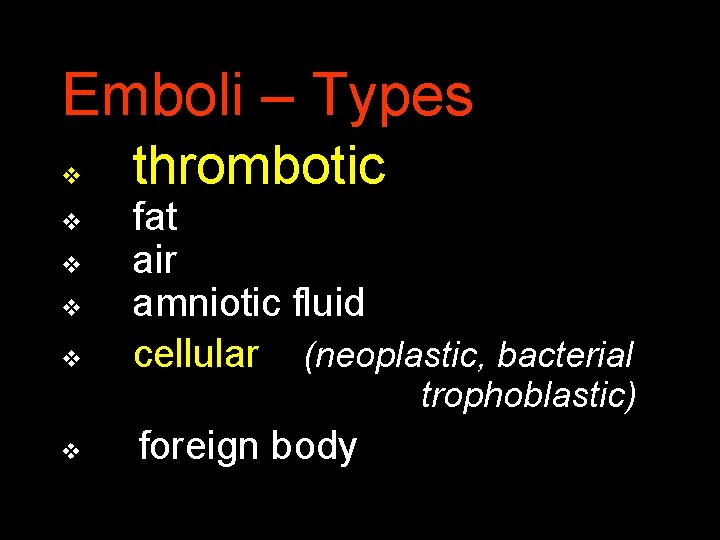
Emboli – Types v v v thrombotic fat air amniotic fluid cellular (neoplastic, bacterial trophoblastic) v foreign body
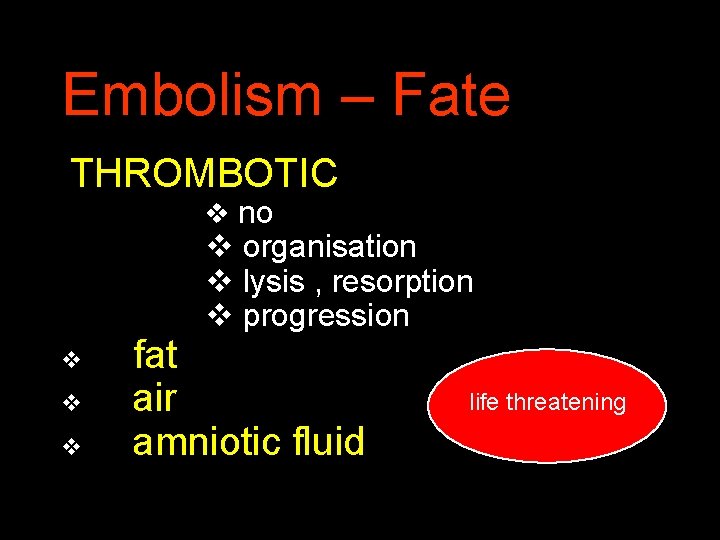
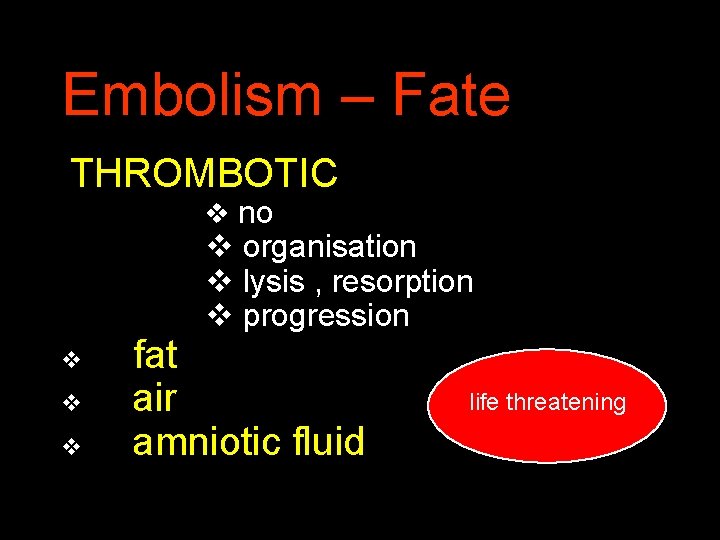
Embolism – Fate THROMBOTIC v no v organisation v lysis , resorption v progression v v v fat air amniotic fluid life threatening
Embolism – Fate CELLULAR v v lysis progression trophoblastic neoplastic METASTASES bacterial metastatic sepsis
Caisson Disease (Decompression thickness – gas microembolism) life threatening v divers v underwater construction workers v unpressurized aircraft in high altitudes
Factors Influencing Vessel Occlusion Result anatomy v time v tissue/organ sensitivity to hypoxy v functional status v general circulation status v MEDICAL INTERVENTION v
Haemorrhagia Def. : blood extravasation (and the presence of blood in the tissue)
Hemorrhage – Classification Localisation: – external – internal Source: – arterial – capillary – venous
Hemorrhage - pathogenesis Haemorrhagia – per rhexin (trauma – tear of the vessel wall) – per diabrosin (arosion – ulcus, neoplasm) – per diapedesin (increased vessel permeability- leakage)
Haemostasis 1. Endothelium damage – v. WF secretion 2. Thrombocytes adhesion & aggregation v Th secretion v serotonin, PDGF, thromboxan A 2 vasoconstriction v fibronectin, v. WF, fibrinogen 3. aggregation Plasma factors - proteins synthesized in hct, (vit. K dependence) activation cascade
Hemorrhagic Statuses Thrombocytopaties thrombocytopenia, thrombasthenia Coagulopaties hemofilia, hypoprothrombinemia, afibrinogenemia, Vasculopaties scurvy, m. Osler, m. Schönlein – Henoch