General Data l l l Name Age 11



- Slides: 37
General Data l l l Name: 林小弟 Age: 11 months Sex: male
Chief Complaints l l Intermittent fever for two days Sudden onset of barking cough, hoarseness, inspiratory stridor and vomiting in this morning.
Present Illness l l intermittent fever about 2 days Initially, he was taken to visit a GP and some medications were prescribed. Sudden onset of barking cough, hoarseness, running nose and vomiting attacked in this morning. His family took him to visit our PER for help and was admitted to our ward for a further investigation and management.
Past history l l l 5 Denied history of any other systemic disease Denied history of any other major operation ans trauma Denied history of allergy about known food or drugs
Personal history l l l 6 preterm 31 wks via C/S vaccination was given as schedule growth & development history: in normal range Contact history: His mother had URI symptoms Traveling history: nil
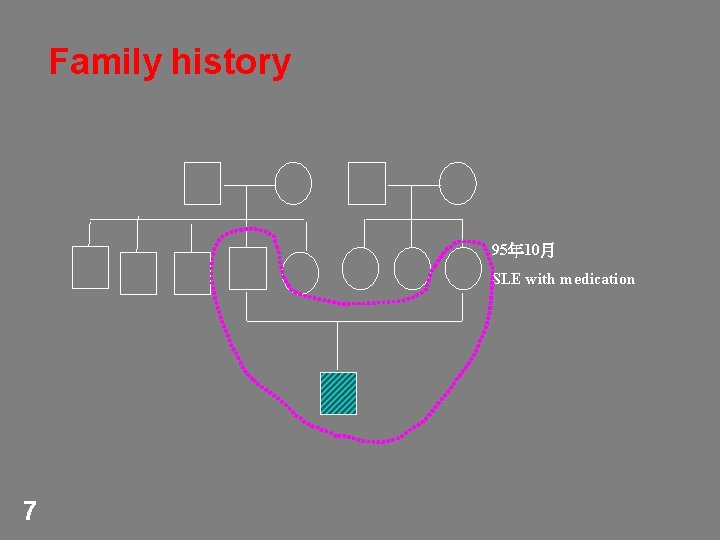
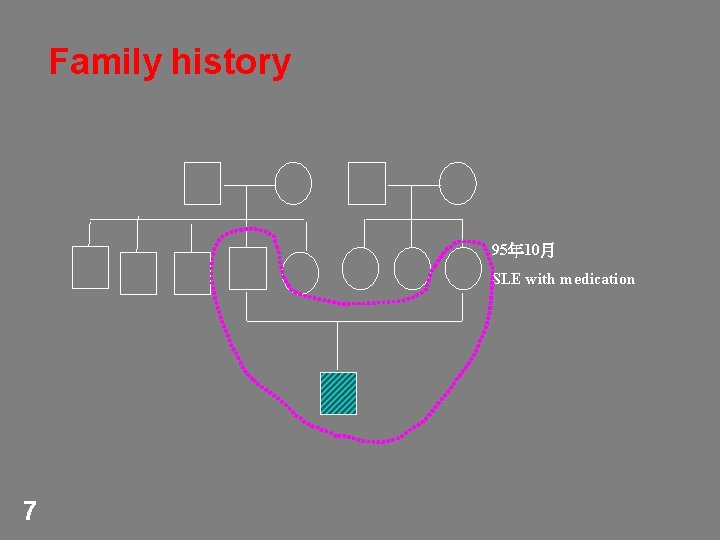
Family history 95年 10月 SLE with medication 7
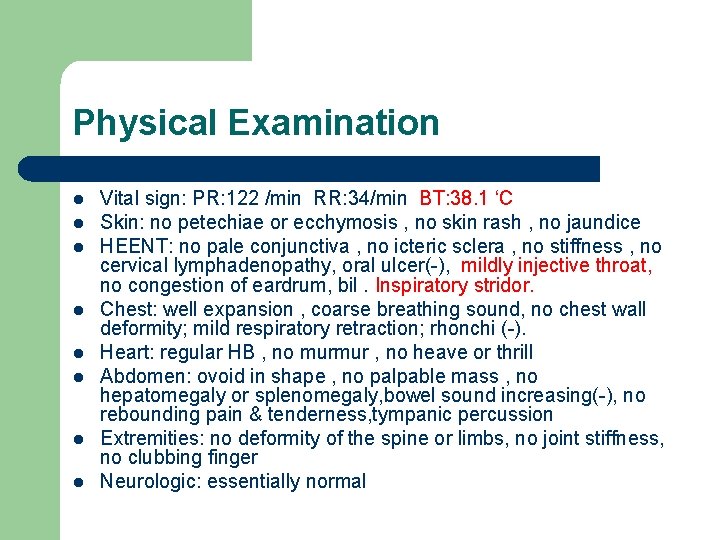
Physical Examination l l l l Vital sign: PR: 122 /min RR: 34/min BT: 38. 1 ‘C Skin: no petechiae or ecchymosis , no skin rash , no jaundice HEENT: no pale conjunctiva , no icteric sclera , no stiffness , no cervical lymphadenopathy, oral ulcer(-), mildly injective throat, no congestion of eardrum, bil. Inspiratory stridor. Chest: well expansion , coarse breathing sound, no chest wall deformity; mild respiratory retraction; rhonchi (-). Heart: regular HB , no murmur , no heave or thrill Abdomen: ovoid in shape , no palpable mass , no hepatomegaly or splenomegaly, bowel sound increasing(-), no rebounding pain & tenderness, tympanic percussion Extremities: no deformity of the spine or limbs, no joint stiffness, no clubbing finger Neurologic: essentially normal
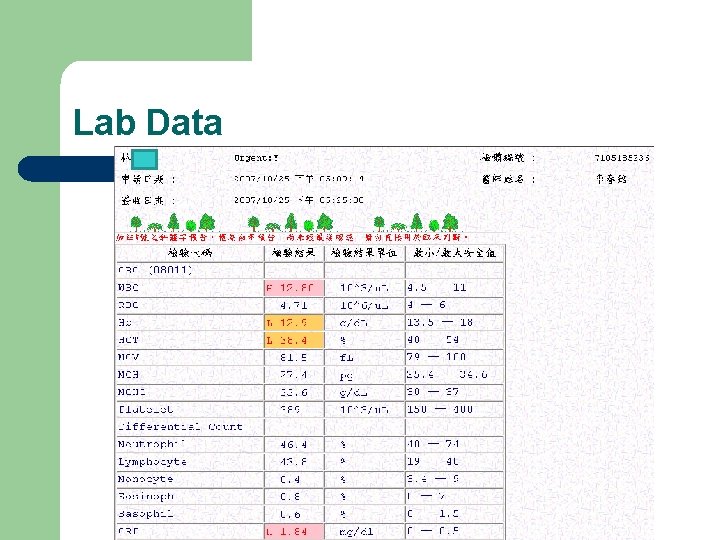
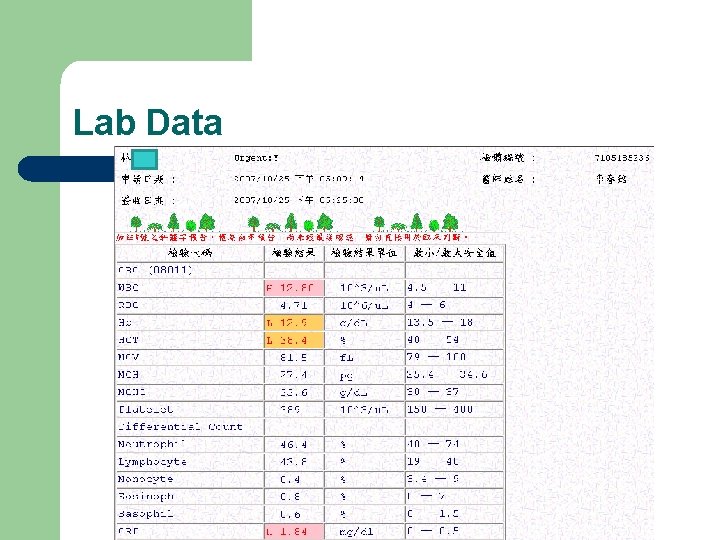
Lab Data
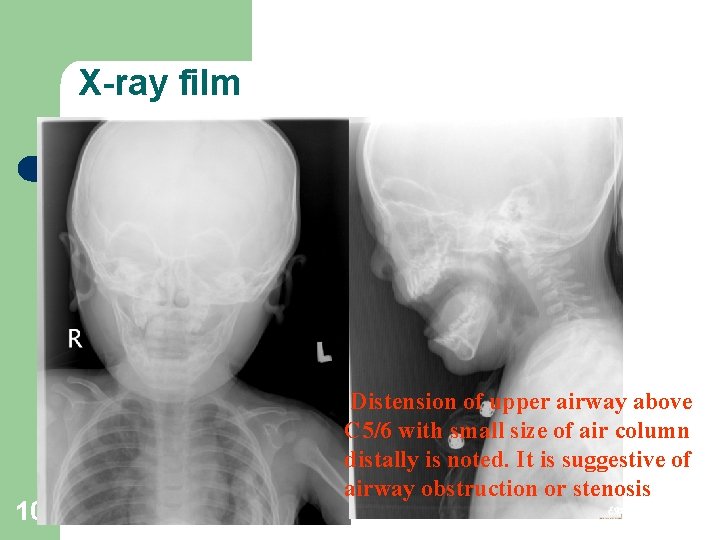
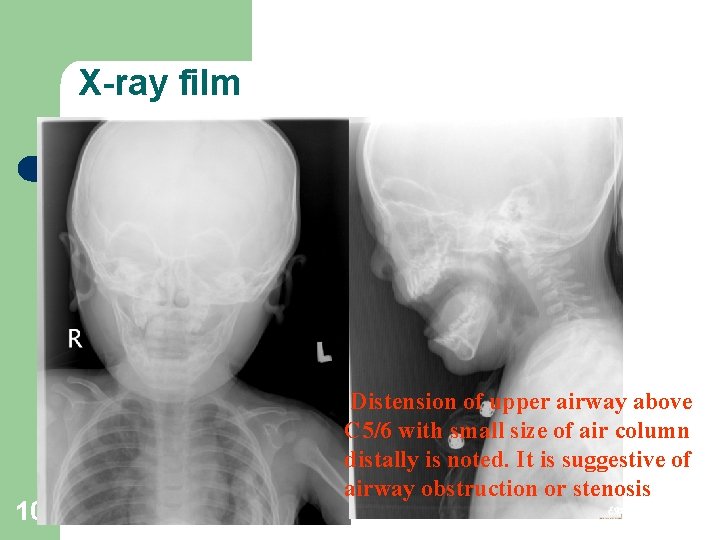
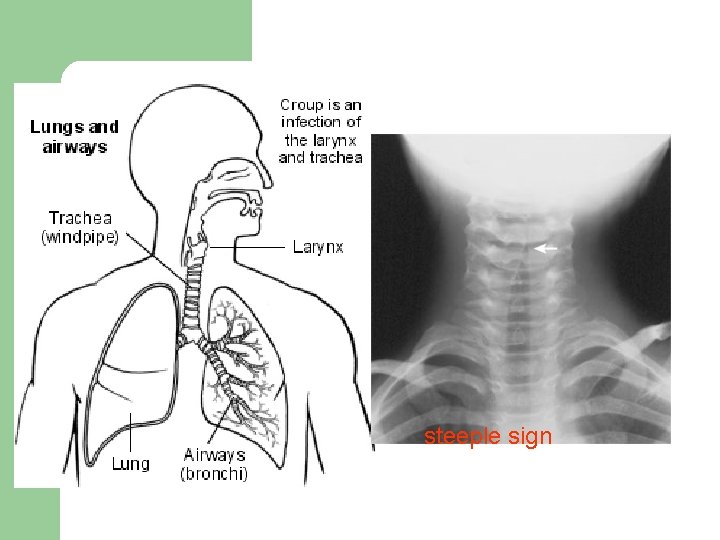
X-ray film 10 Distension of upper airway above C 5/6 with small size of air column distally is noted. It is suggestive of airway obstruction or stenosis

Impression l Croup

CROUP l 1 -4 day history of a coryzal illness(clear rhinorrhea, low-grade temperature, mild tachypnea) l Viral croup is the most common form of airway obstruction in children 6 mo to 5 ys-viral laryngotracheobronchitis
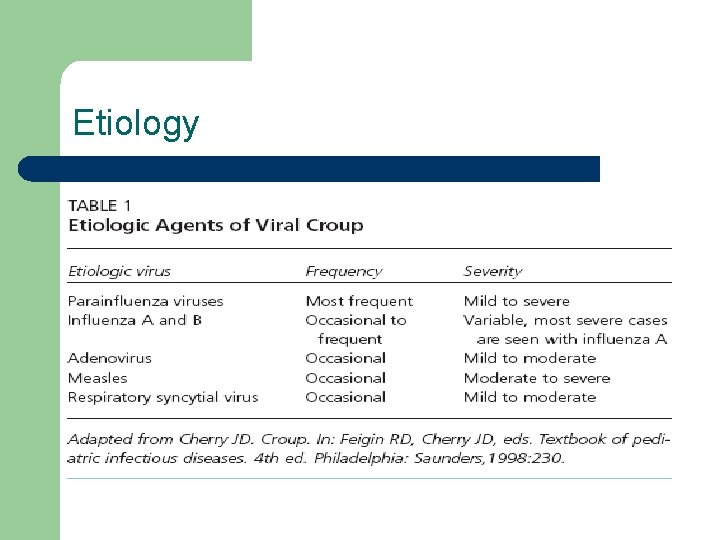
Viruses causing croup l l l most common are the parainfluenza 1 and 3 and respiratory syncytial viruses rhinovirus, adenovirus, measles virus and Mycoplasma pneumoniae parainfluenza viral infections typically in the autumn; respiratory syncytial virus mainly in the winter
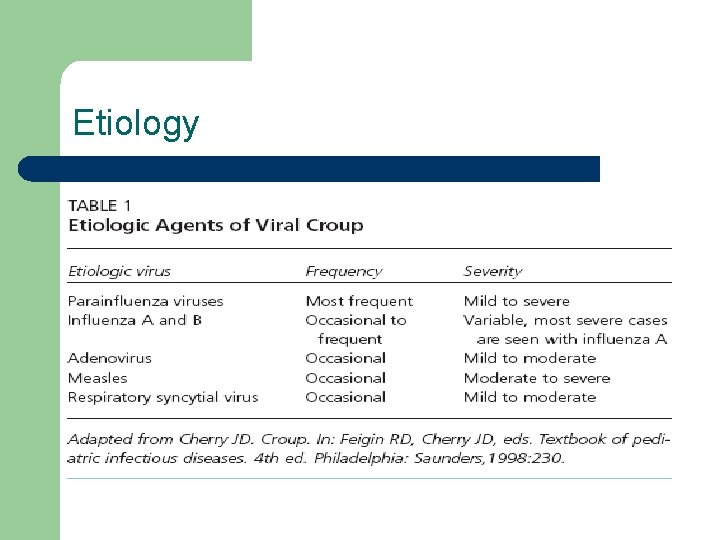
Etiology
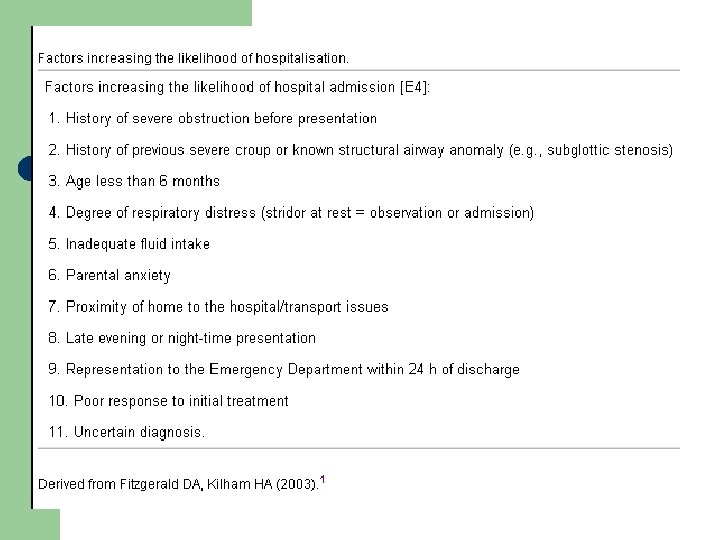
Epidemiology l l approximately 3% of children will have croup before the age of 6 years Data from the 1970 s suggested that up to 6% of young children with croup will require hospitalisation
Symptoms l l Noisy breathing (inspiratory stridor) - a high pitched sound Harsh, barking cough Hoarse voice Difficulty breathing - depending on the severity of the illness.
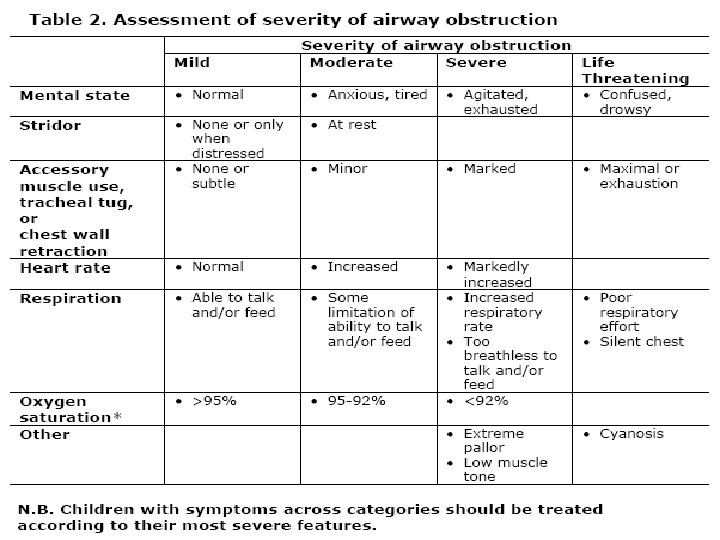
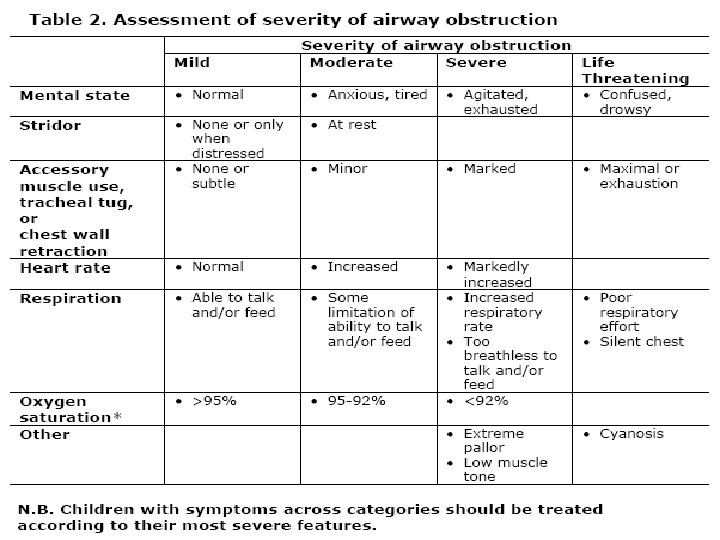
Serious signs l l l Breathing more quickly. Restlessness, anxiety and sweating. Continuous soft stridor (noisy breathing). Bluish tinge to the lips. ‘Caving in’ of the soft tissues of the neck and between the ribs when the child tries to breathe in.
Clinical Course l l Viral croup typically is preceded by 12 to 72 hours of low-grade fever and coryza. As the illness progresses, hoarseness and the characteristic “croupy” or barking cough will develop. Other symptoms include dyspnea, hoarseness, stridor, and wheezing. Agitation and crying tend to aggravate symptoms, and children often prefer to sit up or be held upright.
Diagnosis l l The diagnosis of croup is clinical. There is very little research evidence on which to establish evidence-based recommendations for the diagnosis of croup. However, there is a consensus of opinion in the medical literature that a child presenting with abrupt onset of barking cough, inspiratory stridor and hoarseness is likely to have croup. The severity of these symptoms varies over time.
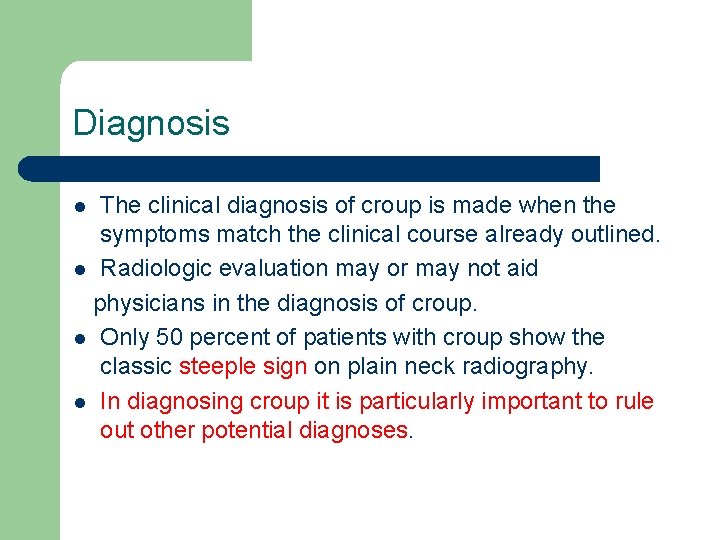
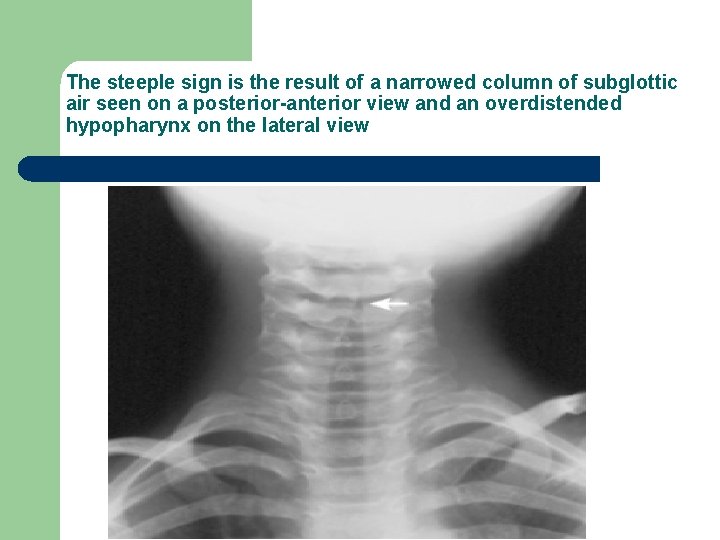
Diagnosis The clinical diagnosis of croup is made when the symptoms match the clinical course already outlined. l Radiologic evaluation may or may not aid physicians in the diagnosis of croup. l Only 50 percent of patients with croup show the classic steeple sign on plain neck radiography. l In diagnosing croup it is particularly important to rule out other potential diagnoses. l
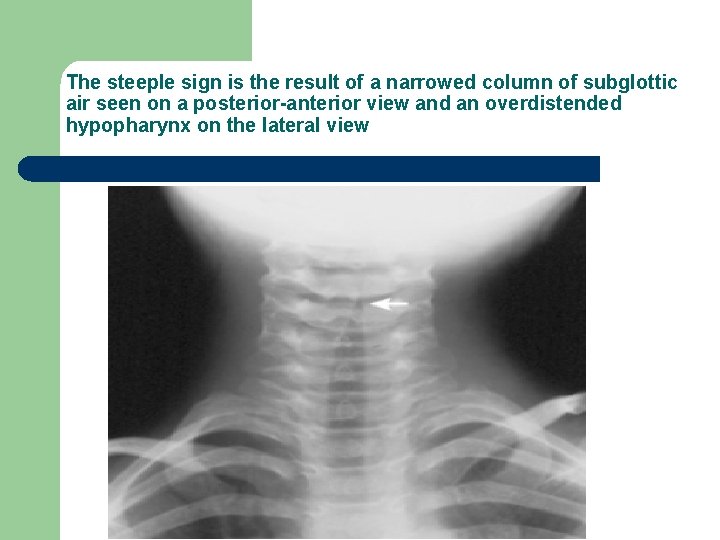
The steeple sign is the result of a narrowed column of subglottic air seen on a posterior-anterior view and an overdistended hypopharynx on the lateral view
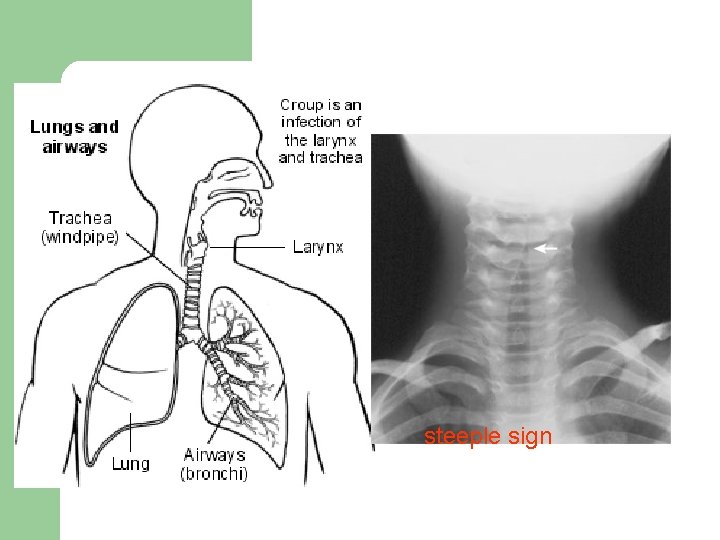
steeple sign

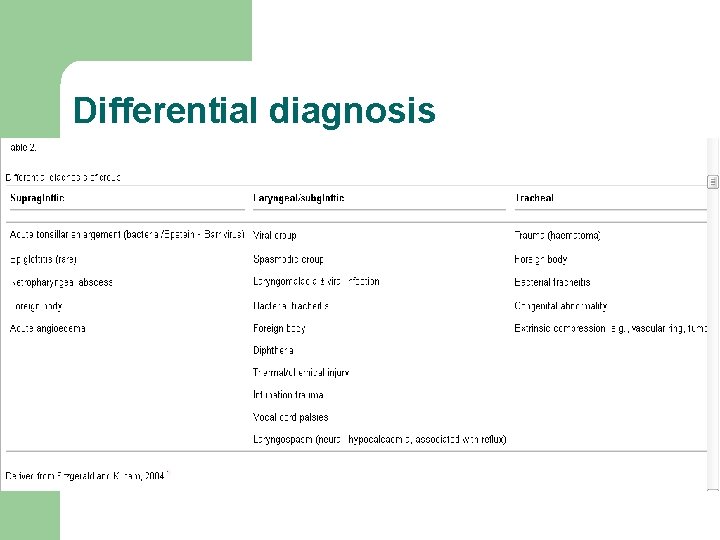
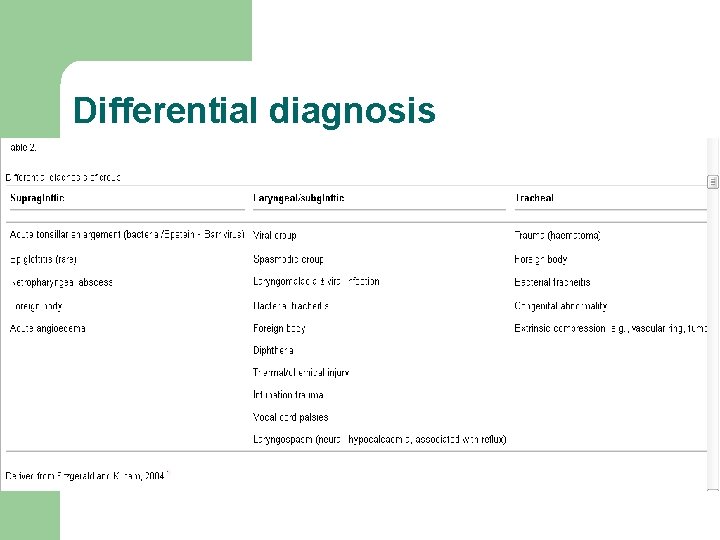
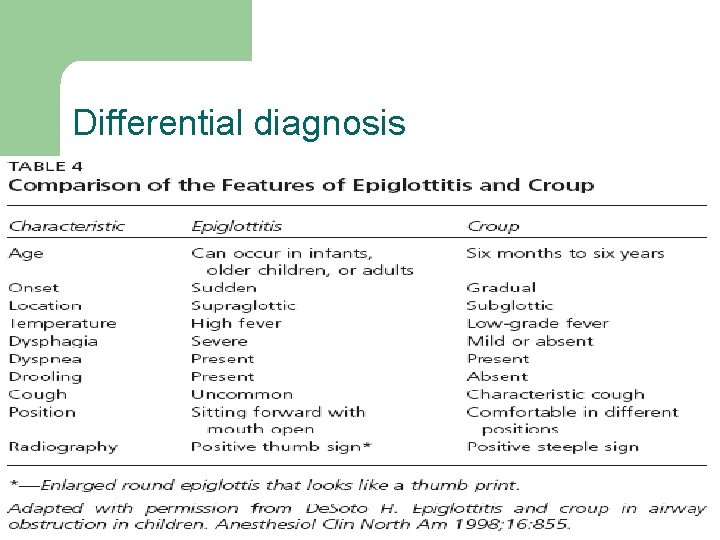
Differential diagnosis
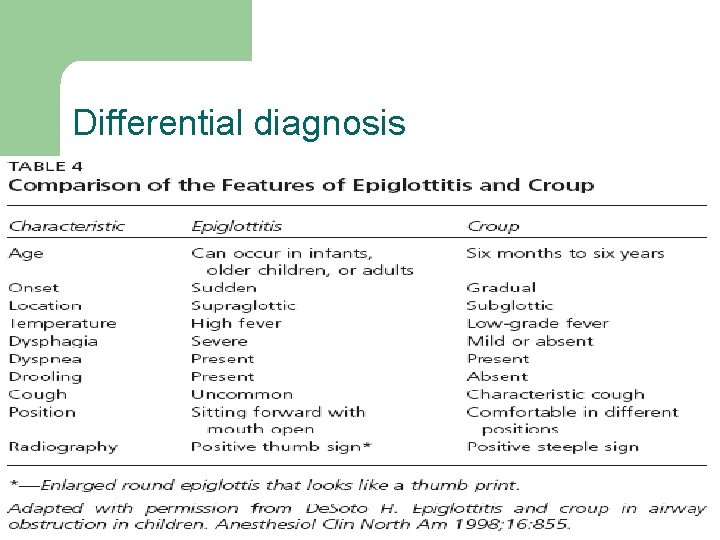
Differential diagnosis
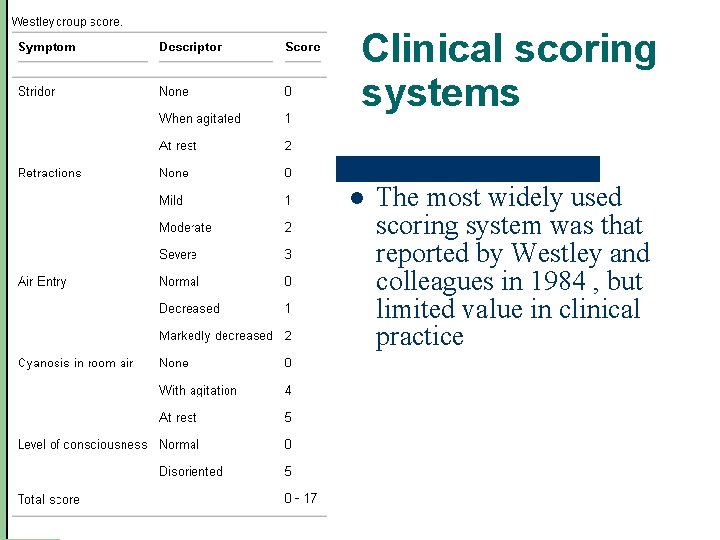
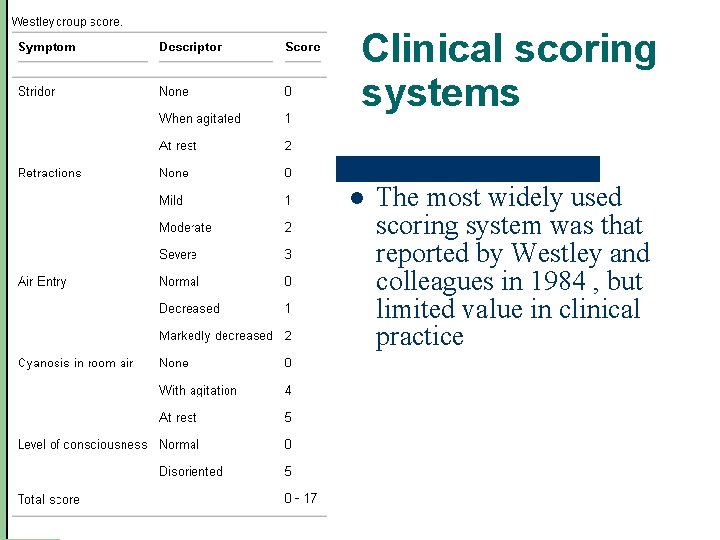
Clinical scoring systems l The most widely used scoring system was that reported by Westley and colleagues in 1984 , but limited value in clinical practice
Treatment l l l Mist therapy Corticosteroids Racemic epinephrine
Mist therapy l l Mucosal cooling, vasoconstriction, and lessened edema. In addition, cool mist moistens secretions, soothes inflamed mucosa, and decreases the viscosity of mucous secretions.
STEROIDS l l Since the 1970 s, corticosteroid use for croup has been debated. More recently, results of a meta-analysis showed that treatment with glucocorticoids is effective in improving symptoms within 6 hours, for up to 12 hours, with significant improvement in croup scores, shorter hospital stays, and less use of epinephrine.
STEROIDS l In one study, investigators compared doses of 0. 15 mg per kg, 0. 3 mg per kg, and 0. 6 mg per kg and found no difference. l (International Journal of Pediatric Otorhinolaryngology (2007) 71, 473— 477 ---- A randomized comparison of dexamethasone 0. 15 mg/kg versus 0. 6 mg/kg for the treatment of moderate to severe croup) l These studies provide convincing evidence that oral dexamethasone is beneficial in the outpatient management of mild to moderate croup in the outpatient setting.
Racemic epinephrine l l l For decades, nebulized racemic epinephrine has been the standard treatment for patients with moderate to severe croup. In patients with croup, racemic epinephrine reduces bronchial and tracheal secretions and mucosal edema. Racemic epinephrine, a 1: 1 mixture of the dand l-isomers of epinephrine, is an alphaand beta-adrenergic receptor stimulator.
Racemic epinephrine l The routine dosage of racemic epinephrine is 0. 05 to 0. 1 m. L per kg per dose mixed with normal saline and delivered with humidified oxygen. l The l-isomer of epinephrine alone may be more available and is used by nebulization(5 m. L of 1: 1, 000 solution). Decreased inspiratory stridor and intercostal retractions are observed within 30 minutes of administering epinephrine, and the duration of action is about two hours. l
Racemic epinephrine l In the emergency department, children who have received nebulized epinephrine may be discharged if they have been observed for three to four hours and have no stridor at rest, normal air entry, good color, normal level of consciousness, and have received steroid therapy.
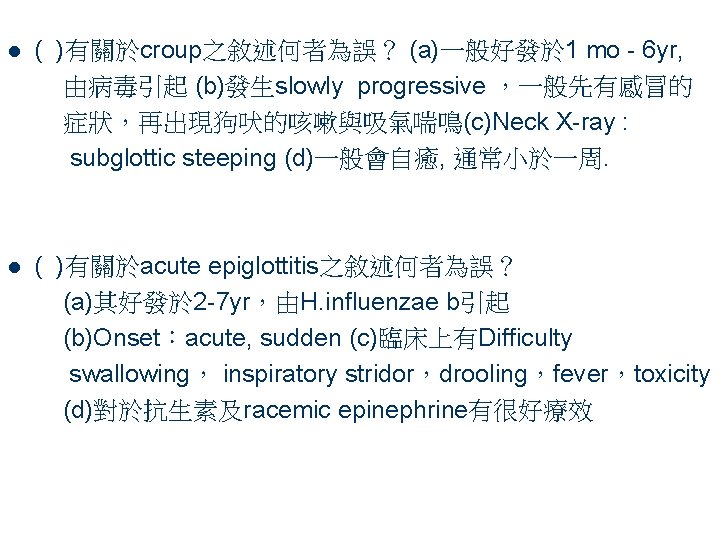
l ( )有關於croup之敘述何者為誤? (a)一般好發於 1 mo - 6 yr, 由病毒引起 (b)發生slowly progressive ,一般先有感冒的 症狀,再出現狗吠的咳嗽與吸氣喘鳴(c)Neck X-ray : subglottic steeping (d)一般會自癒, 通常小於一周. l ( )有關於acute epiglottitis之敘述何者為誤? (a)其好發於 2 -7 yr,由H. influenzae b引起 (b)Onset:acute, sudden (c)臨床上有Difficulty swallowing, inspiratory stridor,drooling,fever,toxicity (d)對於抗生素及racemic epinephrine有很好療效