General arrangement of ANS Each of the major


- Slides: 32
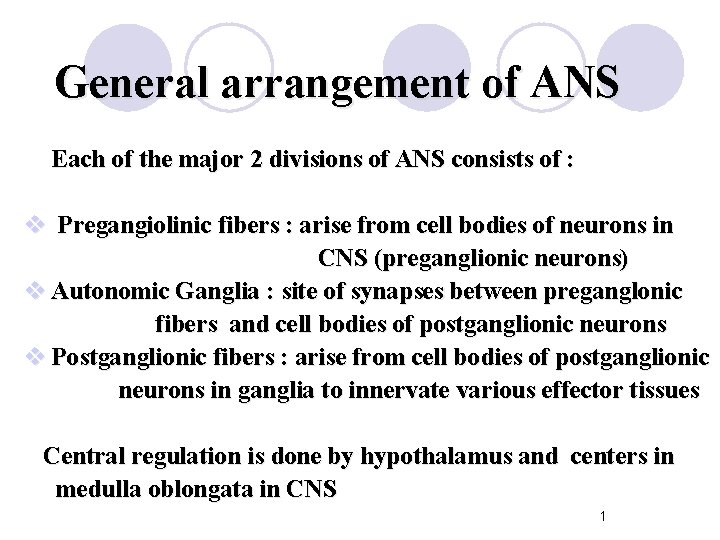
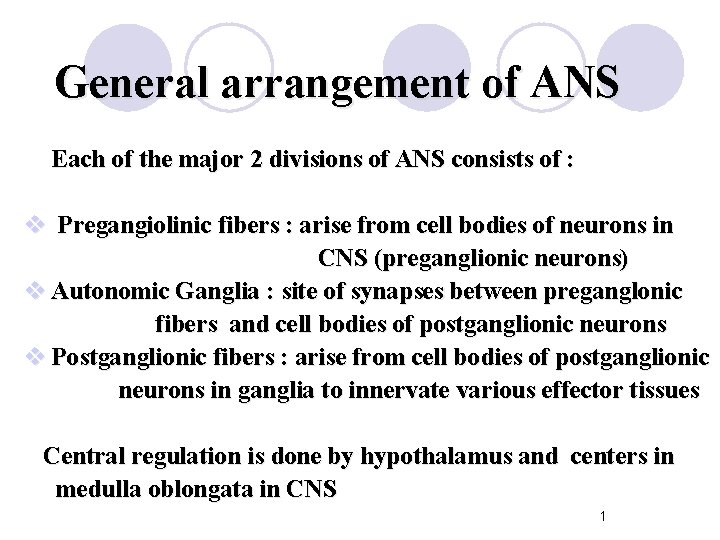
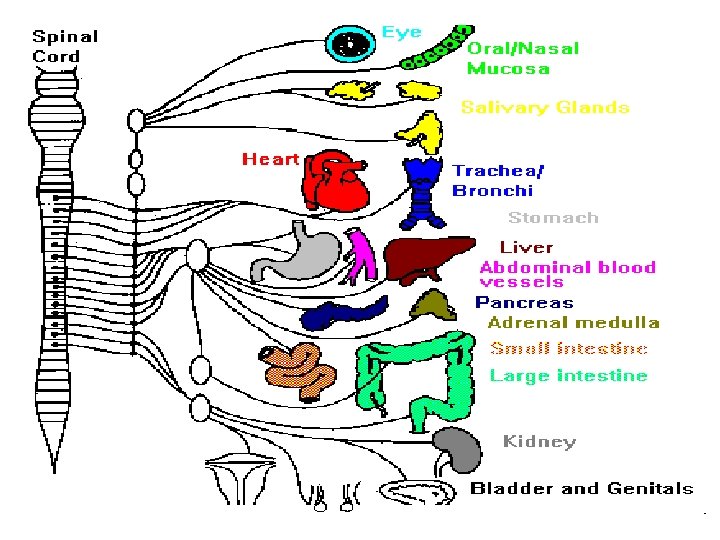
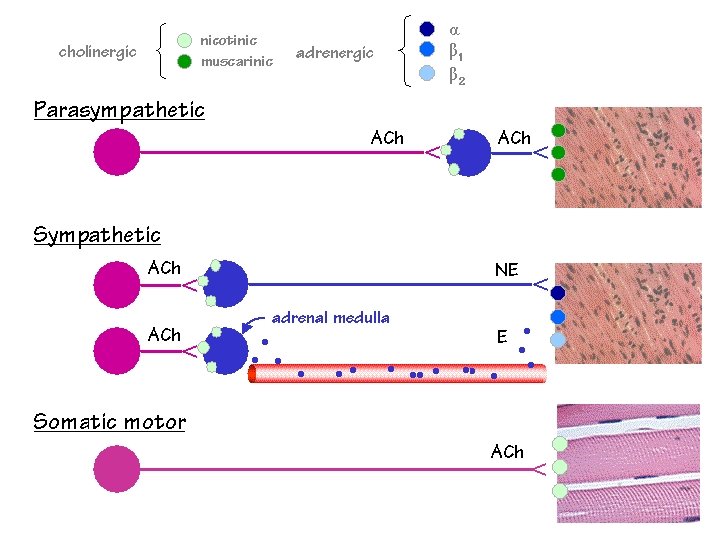
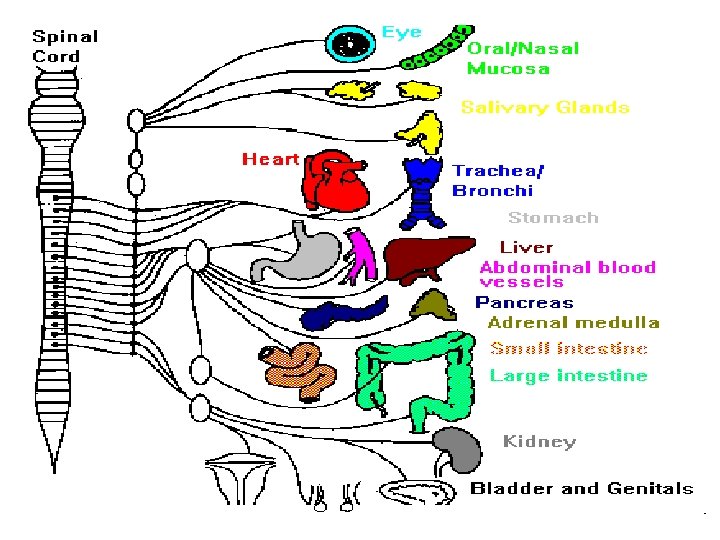
General arrangement of ANS Each of the major 2 divisions of ANS consists of : v Pregangiolinic fibers : arise from cell bodies of neurons in CNS (preganglionic neurons) v Autonomic Ganglia : site of synapses between preganglonic fibers and cell bodies of postganglionic neurons v Postganglionic fibers : arise from cell bodies of postganglionic neurons in ganglia to innervate various effector tissues Central regulation is done by hypothalamus and centers in medulla oblongata in CNS 1
2
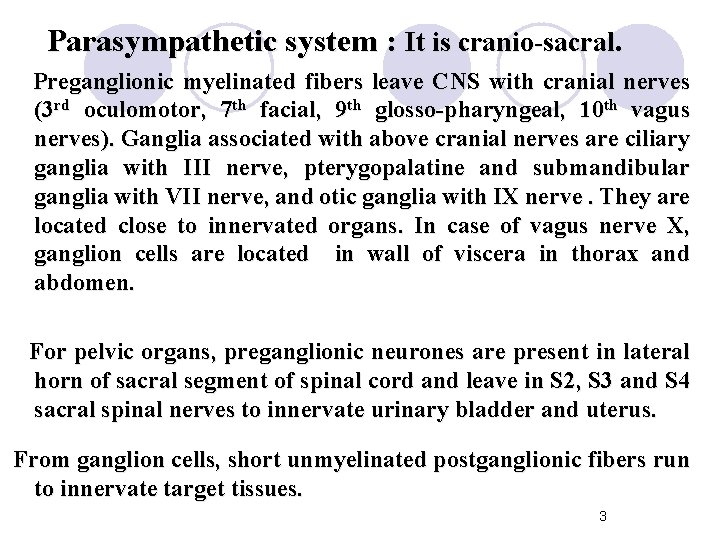
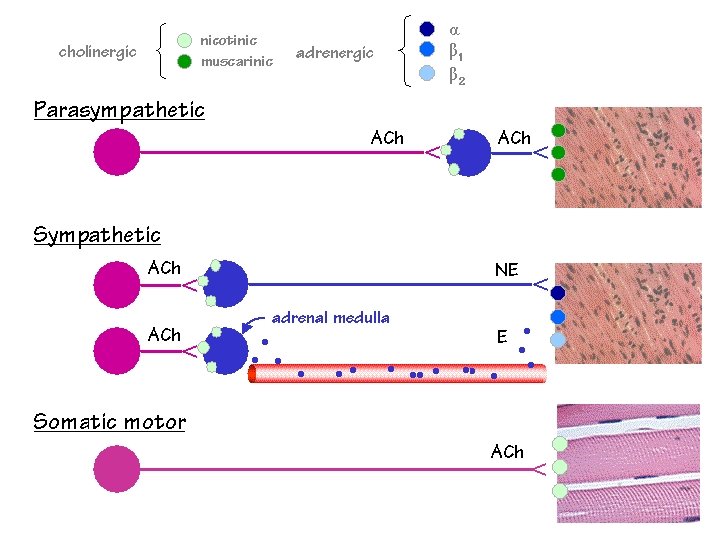
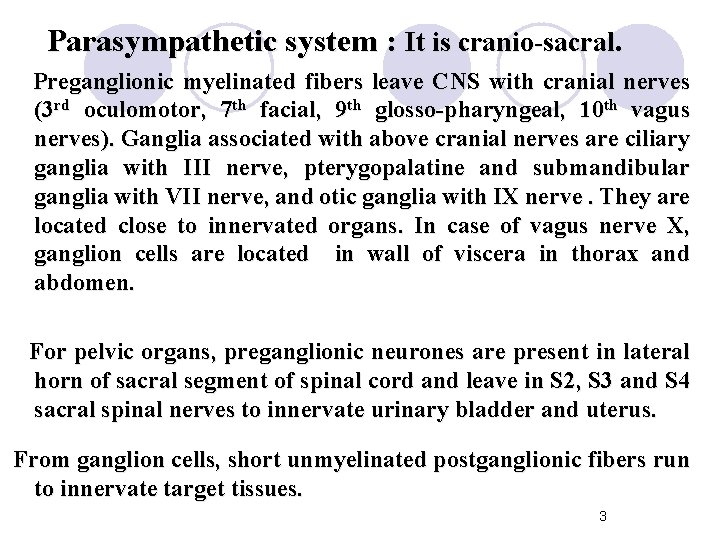
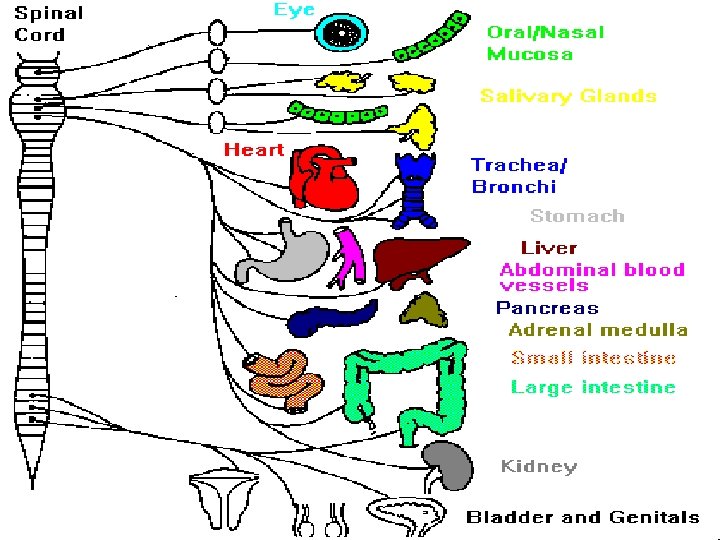
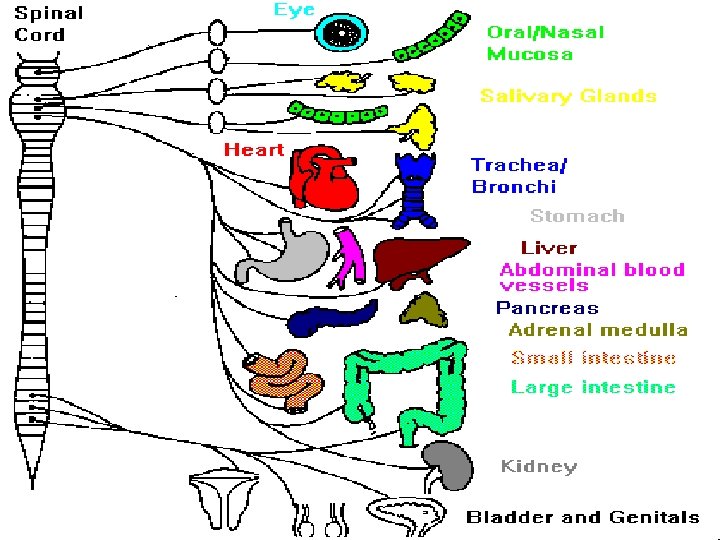
Parasympathetic system : It is cranio-sacral. Preganglionic myelinated fibers leave CNS with cranial nerves (3 rd oculomotor, 7 th facial, 9 th glosso-pharyngeal, 10 th vagus nerves). Ganglia associated with above cranial nerves are ciliary ganglia with III nerve, pterygopalatine and submandibular ganglia with VII nerve, and otic ganglia with IX nerve. They are located close to innervated organs. In case of vagus nerve X, ganglion cells are located in wall of viscera in thorax and abdomen. For pelvic organs, preganglionic neurones are present in lateral horn of sacral segment of spinal cord and leave in S 2, S 3 and S 4 sacral spinal nerves to innervate urinary bladder and uterus. From ganglion cells, short unmyelinated postganglionic fibers run to innervate target tissues. 3
4
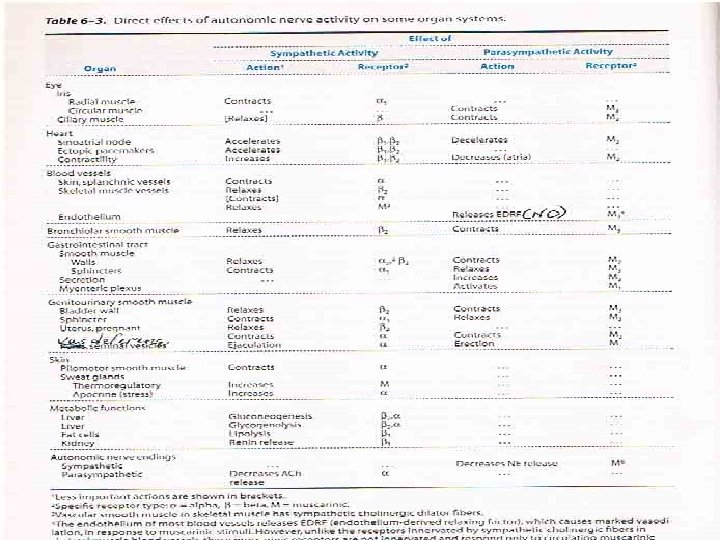
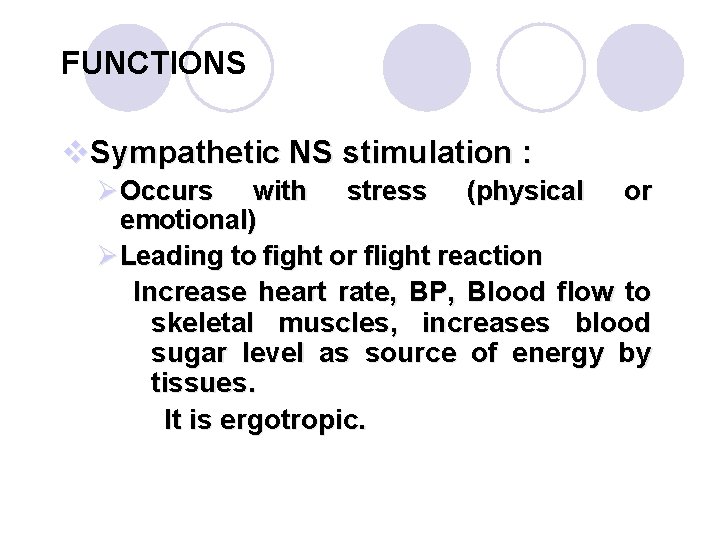
Functions v. Parasympathetic NS system stimulation: It predominates during rest or sleep. Parasympathetic NS slows the heart and regulates digestion, bladder and bowel function. It opposes sympathetic function in peripheral tissues. It is trophotropic. 5
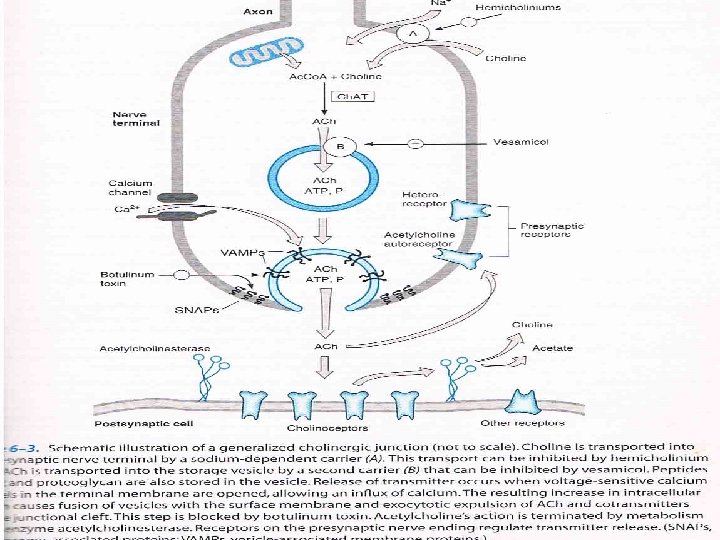
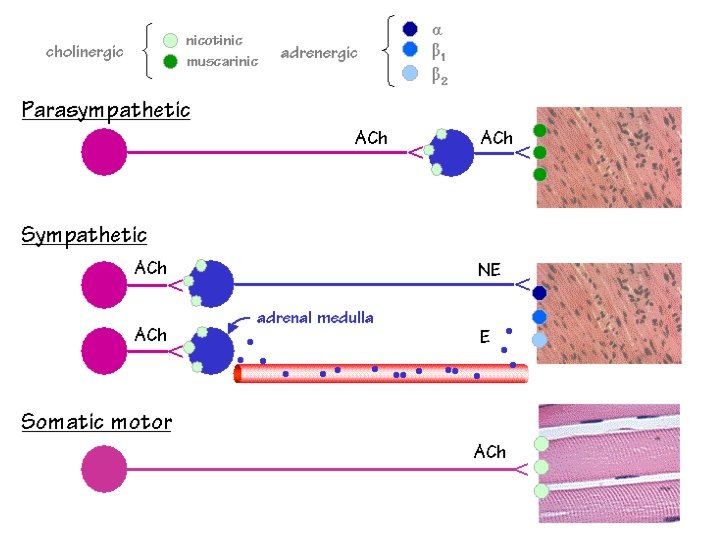
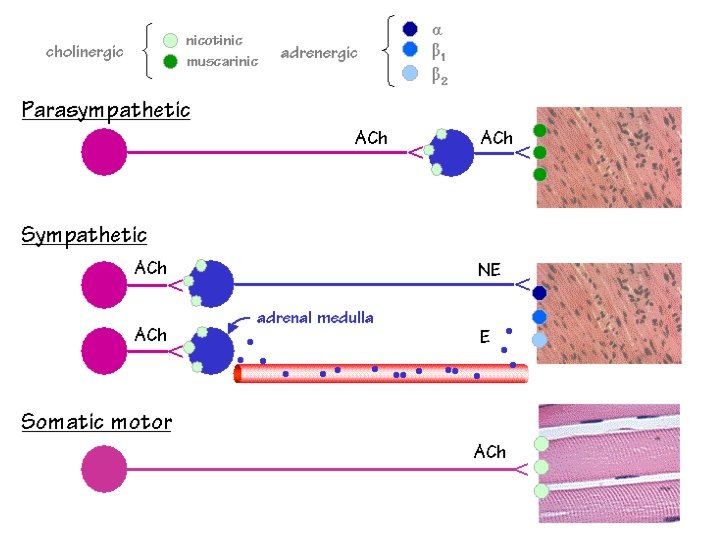
Cholinergic Transmission v. Acetylcholine ( Ach ) is the neurotransmitter v. Acts on cholinoceptors present in: Ø Autonomicganglia(sympathetic¶sympathetic ØNeuro-effector junction of parasympathetic post-ganglionic fibers ØAdrenal medulla ØSomatic NMJ (Neuro-muscular junction) endplates ØCNS 6
Pathway of Acetylcholine Storage: Ø Ach is actively transported from cytoplasm into storage vesicles where it is protected from degradation Release : by exocytosis Binding : Ach binds to & activates cholinoceptors on post-synaptic tissues leading to various actions 7
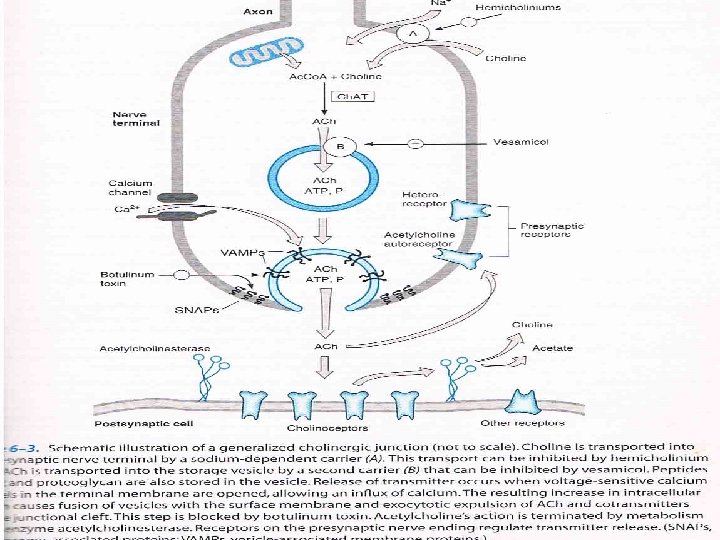
Inhibitors of Ach Pathway v Synthesis: ØHemicholinium v Storage: ØVesamicol v Release: ØBotulinum toxins (Botulism : food poisoning) v Binding of Ach to its receptors: anticholinergic 9 drugs
Cholinoceptors v. Muscarinic receptors v. Nicotinic receptors 10
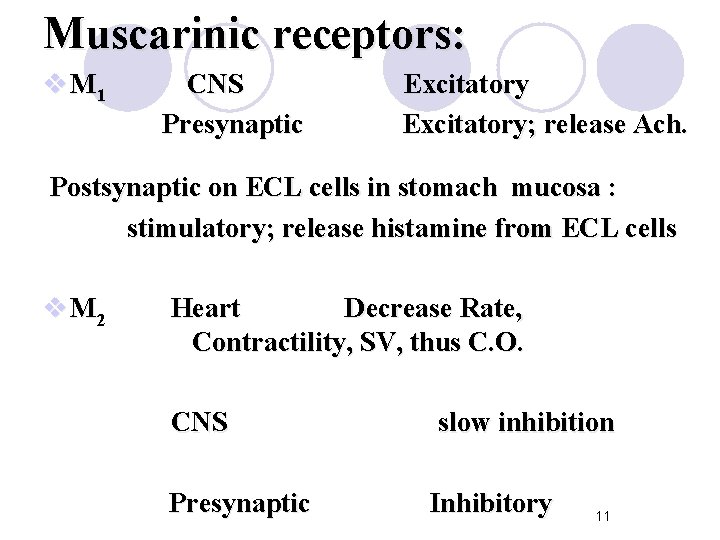
Muscarinic receptors: v M 1 CNS Presynaptic Excitatory; release Ach. Postsynaptic on ECL cells in stomach mucosa : stimulatory; release histamine from ECL cells v M 2 Heart Decrease Rate, Contractility, SV, thus C. O. CNS Presynaptic slow inhibition Inhibitory 11
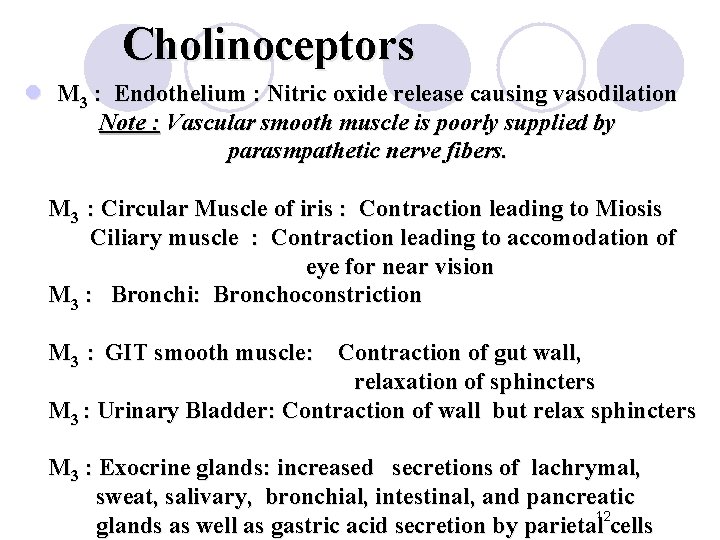
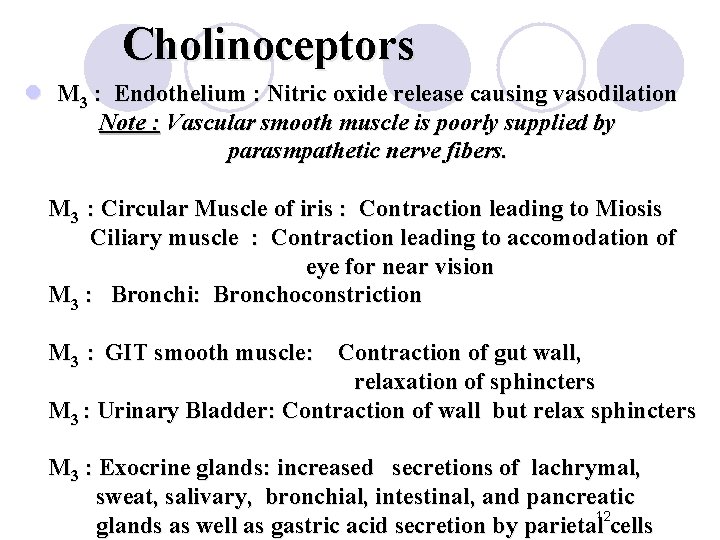
Cholinoceptors l M 3 : Endothelium : Nitric oxide release causing vasodilation Note : Vascular smooth muscle is poorly supplied by parasmpathetic nerve fibers. M 3 : Circular Muscle of iris : Contraction leading to Miosis Ciliary muscle : Contraction leading to accomodation of eye for near vision M 3 : Bronchi: Bronchoconstriction M 3 : GIT smooth muscle: Contraction of gut wall, relaxation of sphincters M 3 : Urinary Bladder: Contraction of wall but relax sphincters M 3 : Exocrine glands: increased secretions of lachrymal, sweat, salivary, bronchial, intestinal, and pancreatic glands as well as gastric acid secretion by parietal 12 cells
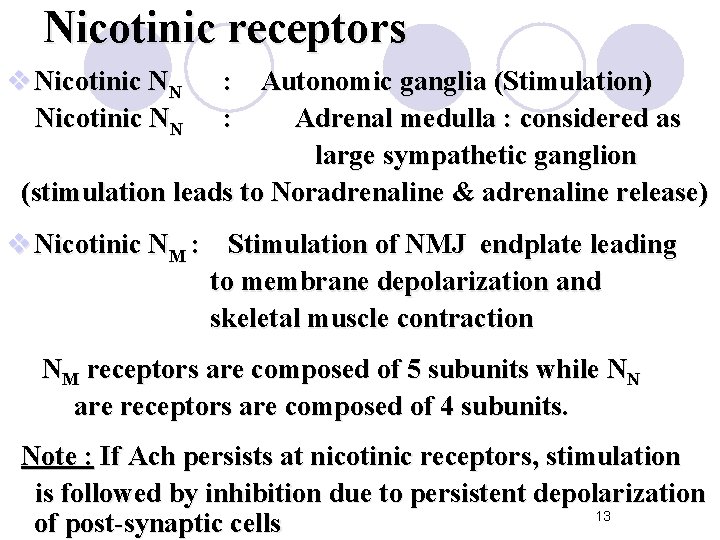
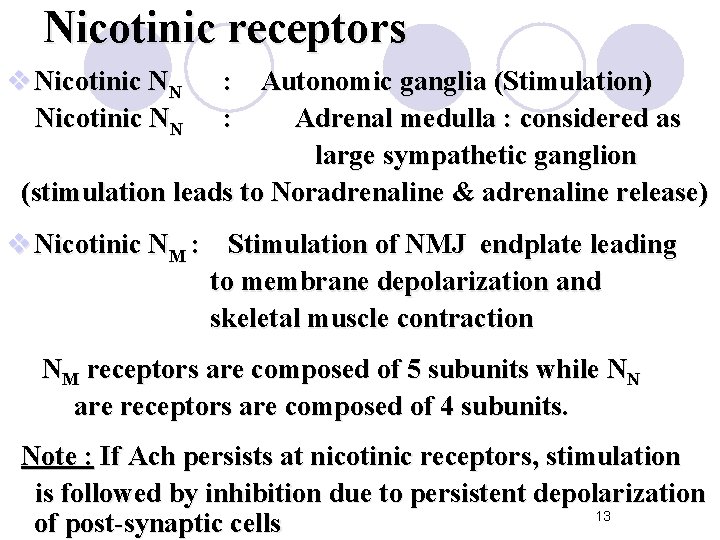
Nicotinic receptors v Nicotinic NN : Autonomic ganglia (Stimulation) : Adrenal medulla : considered as large sympathetic ganglion (stimulation leads to Noradrenaline & adrenaline release) v Nicotinic NM : Stimulation of NMJ endplate leading to membrane depolarization and skeletal muscle contraction NM receptors are composed of 5 subunits while NN are receptors are composed of 4 subunits. Note : If Ach persists at nicotinic receptors, stimulation is followed by inhibition due to persistent depolarization 13 of post-synaptic cells
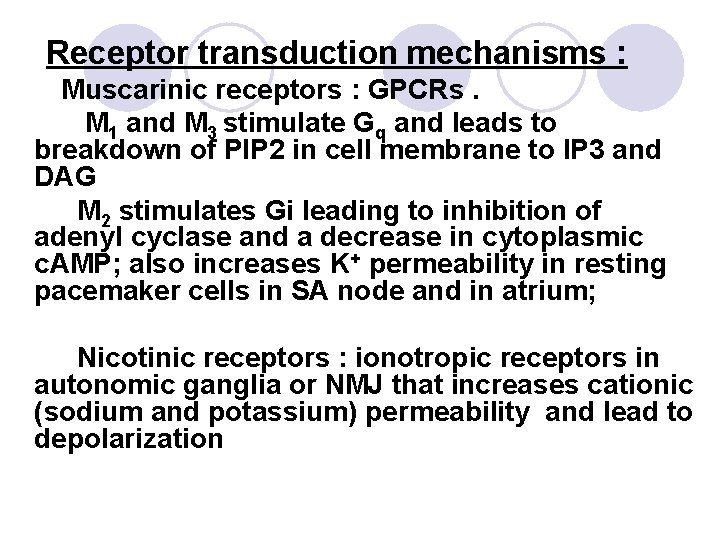
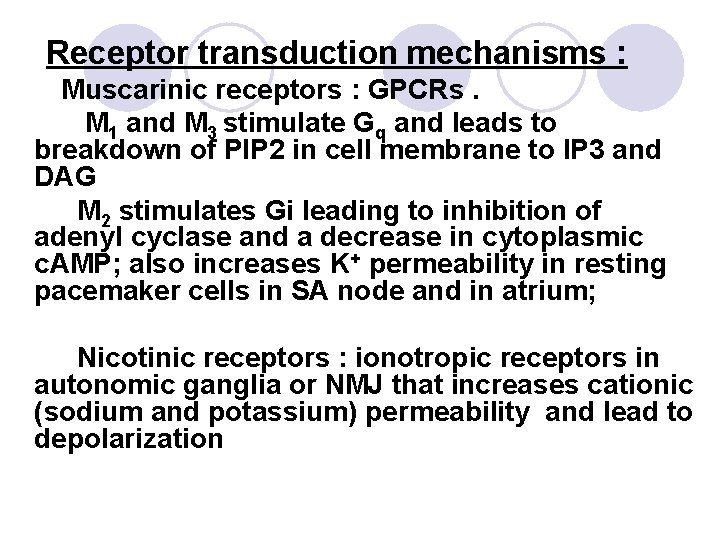
Receptor transduction mechanisms : Muscarinic receptors : GPCRs. M 1 and M 3 stimulate Gq and leads to breakdown of PIP 2 in cell membrane to IP 3 and DAG M 2 stimulates Gi leading to inhibition of adenyl cyclase and a decrease in cytoplasmic c. AMP; also increases K+ permeability in resting pacemaker cells in SA node and in atrium; Nicotinic receptors : ionotropic receptors in autonomic ganglia or NMJ that increases cationic (sodium and potassium) permeability and lead to depolarization
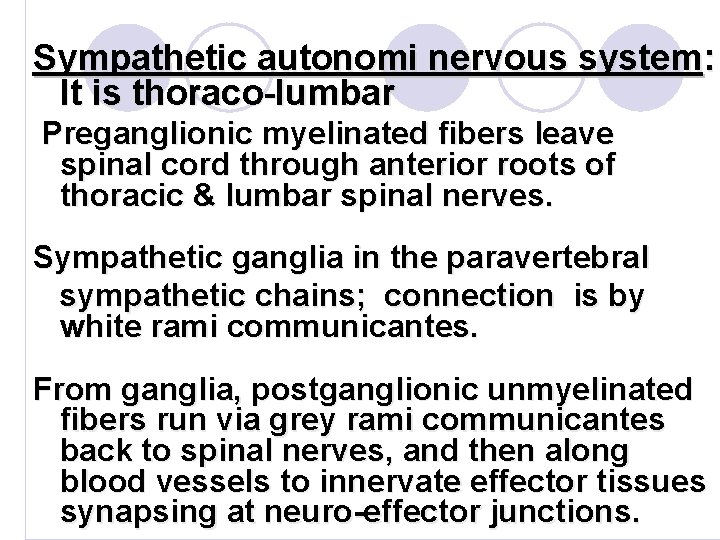
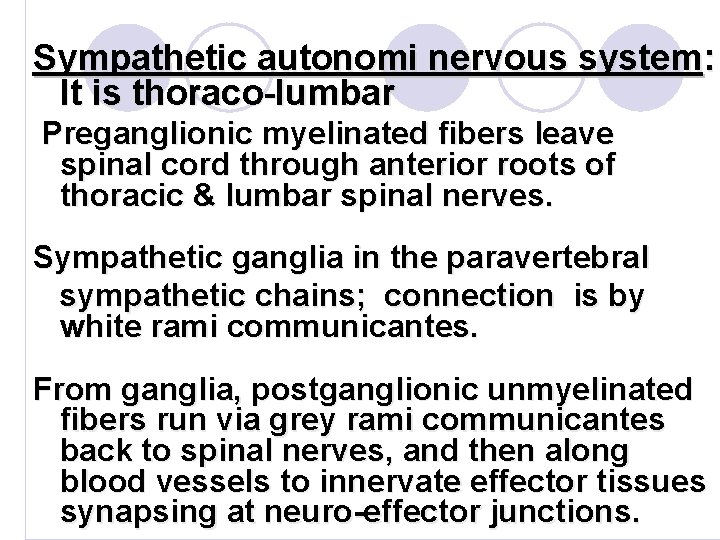
Sympathetic autonomi nervous system: It is thoraco-lumbar Preganglionic myelinated fibers leave spinal cord through anterior roots of thoracic & lumbar spinal nerves. Sympathetic ganglia in the paravertebral sympathetic chains; connection is by white rami communicantes. From ganglia, postganglionic unmyelinated fibers run via grey rami communicantes back to spinal nerves, and then along blood vessels to innervate effector tissues synapsing at neuro-effector junctions.
FUNCTIONS v. Sympathetic NS stimulation : ØOccurs with stress (physical or emotional) ØLeading to fight or flight reaction Increase heart rate, BP, Blood flow to skeletal muscles, increases blood sugar level as source of energy by tissues. It is ergotropic.
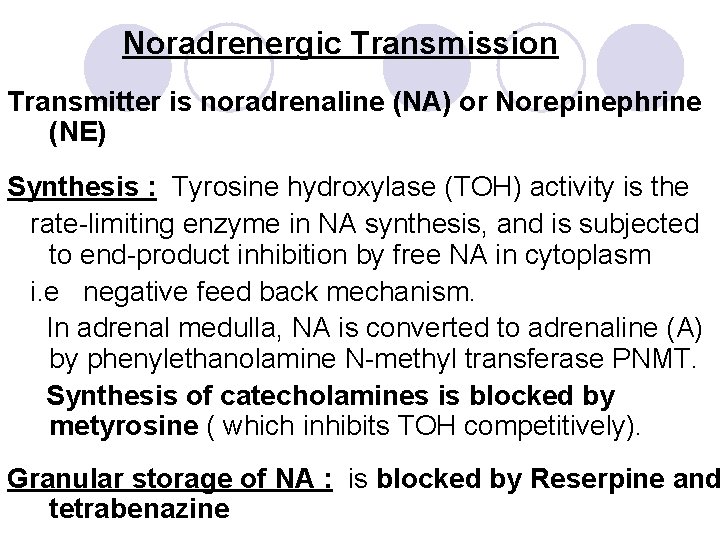
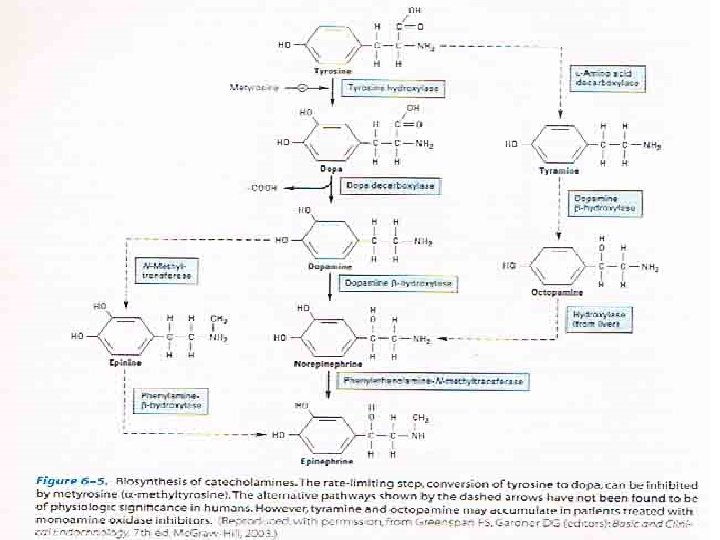
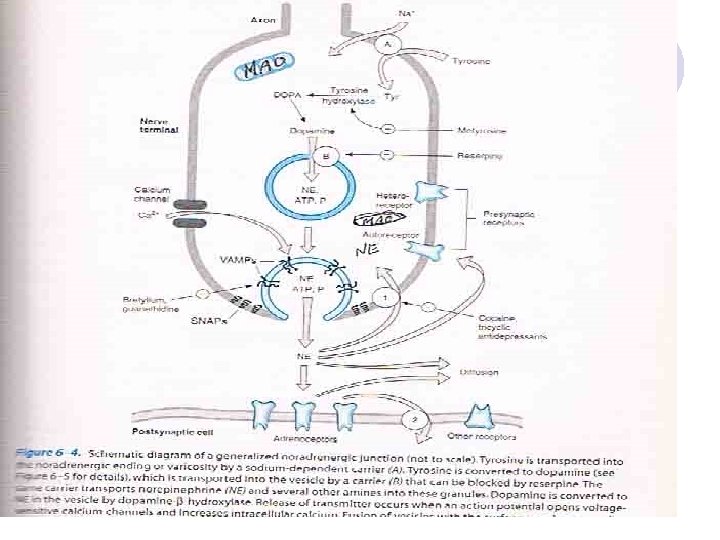
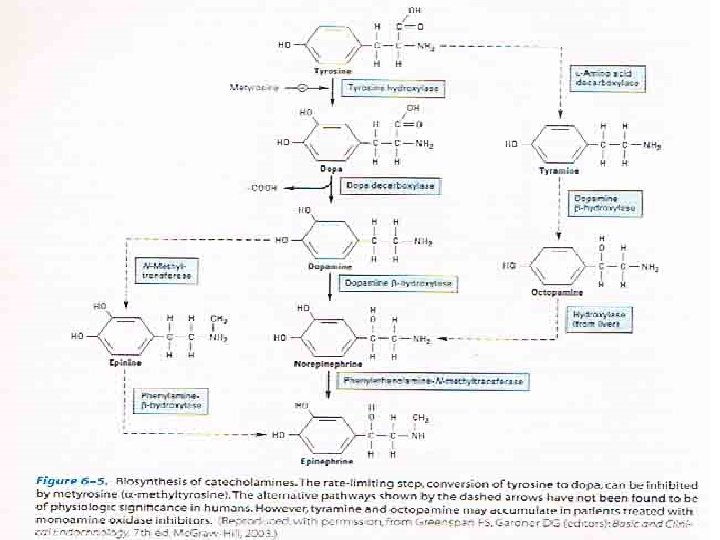
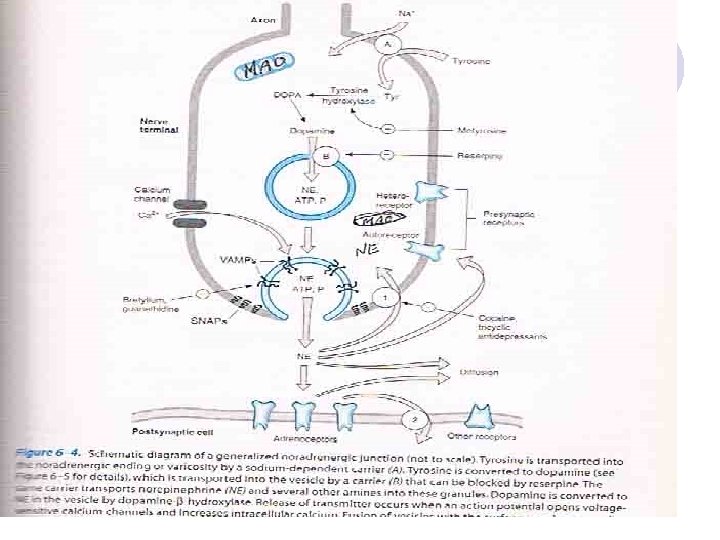
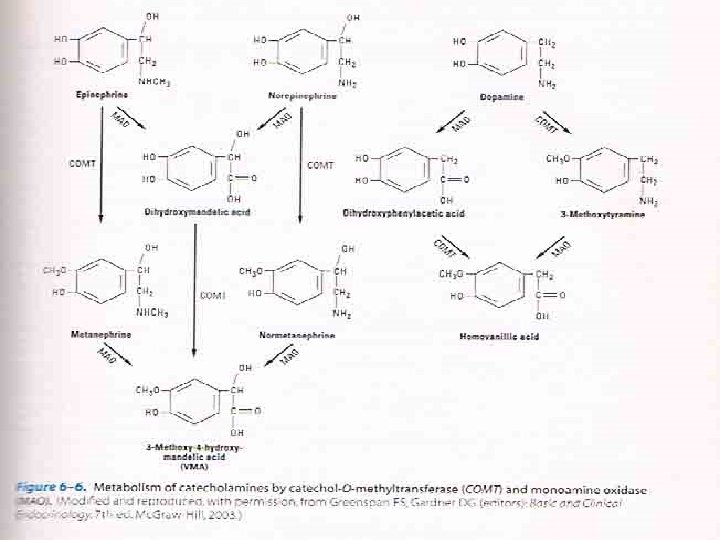
Noradrenergic Transmission Transmitter is noradrenaline (NA) or Norepinephrine (NE) Synthesis : Tyrosine hydroxylase (TOH) activity is the rate-limiting enzyme in NA synthesis, and is subjected to end-product inhibition by free NA in cytoplasm i. e negative feed back mechanism. In adrenal medulla, NA is converted to adrenaline (A) by phenylethanolamine N-methyl transferase PNMT. Synthesis of catecholamines is blocked by metyrosine ( which inhibits TOH competitively). Granular storage of NA : is blocked by Reserpine and tetrabenazine
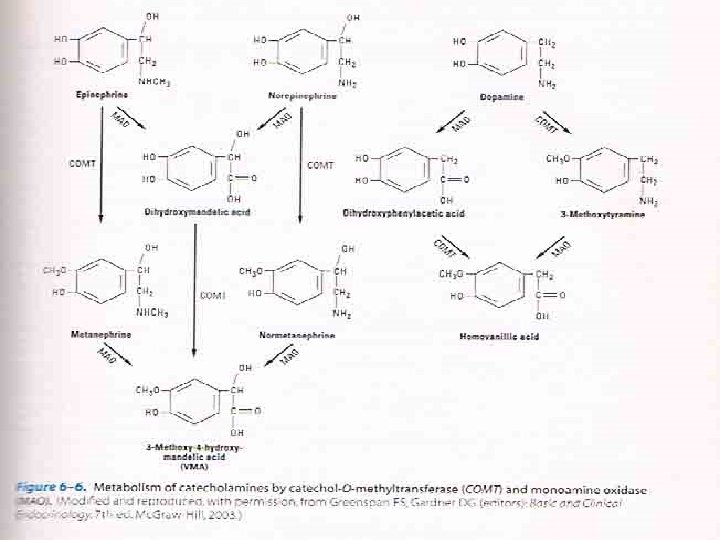
Release of NA from sympathetic nerve ending occurs by: 1. Exocytosis: in case of nerve impulses. It is blocked by bretylium and guanethidine 2. Displacement from storage granules: by indirect acting sympathomimetics e. g. Amphetamine Termination of action of released NA: 1. Reuptake by sympathetic nerve ending: about 80%. - By active amine pump. This can be inhibited by tricyclic antidepressants, and by local anaesthetic cocaine. 2. Enzyme catabolism: MAO: found in mitochondria of sympathetic nerve endings, in intestine, liver & CNS. COMT: found in synapses and in plasma. End metabolite is Vanilylmandelic acid VMA: excreted in urine

Adrenergic Receptors : First proposed by Ahlquist in 1948 - Alpha : αlpha 1 ( A, B, D) , αlpha 2 (A, B, C) - Beta : B 1, B 2 , B 3 Transduction mechanisms : All are GPCRs alpha 1 : stimulates Gq leading to stimulation of PLC and increase in DAG and IP 3. alpha 2 : stimulates Gi leading to inhibition of adenyl cyclase and decrease in intracellular c. AMP Beta 1 & Beta 2 : both stimulate Gs leading to stimulation of adenyl cyclase and increase in intracellular c. AMP
Alpha receptors : αlpha 1 : on smooth muscle → contraction, in : Blood Vessels: vasoconstriction of arterioles and venules Skin & mucous membranes → pallor. Viscera e. g. kidney, uterus → ↓ blood flow. Skeletal muscle blood vesels → ↑ TPR (total peripheral resistance), ↑ DBP (diastolic BP).
Eye Conjunctival vessels Radial muscle of iris → mydriasis Skin Arector pilorum → goose skin Apocrine sweat glands in groin and axilla Viscera: Bladder neck → difficult urination. Uterus → contraction. So, avoid αlpha 1 agonists during pregnancy to prevent harm to fetus. Vas deferens → ejaculation - αlpha 1 receptors also present in salivary glands
αlpha 2 : - Mainly presynaptic: causing ↓ NA release from sympathetic nerve endings. - In some places, it is post-synaptic as in: Brain stem causing inhibition of vasomotor center (VMC) in medulla oblongata, so lowers BP. - pancreatic beta-cells causing ↓ insulin release. - Ciliary epithelium : if stimulated, they decrease formation of aqueous humor - Some B. V. to skeletal muscle : vasoconstriction - - on platelets causing aggregation

Beta receptors : Βeta 1 : a- Heart: ↑ Heart rate (tachycardia): due to ↑ SA node activity. ↑ AV node conduction occur ↑ Contractility of atria & ventricles → ↑ SV. ↑ C. O. occurs due to tachycardia and ↑ SV. As result, there is ↑ cardiac work & O 2 demand. Arrhythmias may occur due to ↑ in cardiac excitability, automaticity, and conductivity. In patients with coronary atherosclerosis, cardiac ischemia with angina may occur because sclerosed coronary arteries do not dilate enough to increas blood flow and O 2 supply to myocardium.
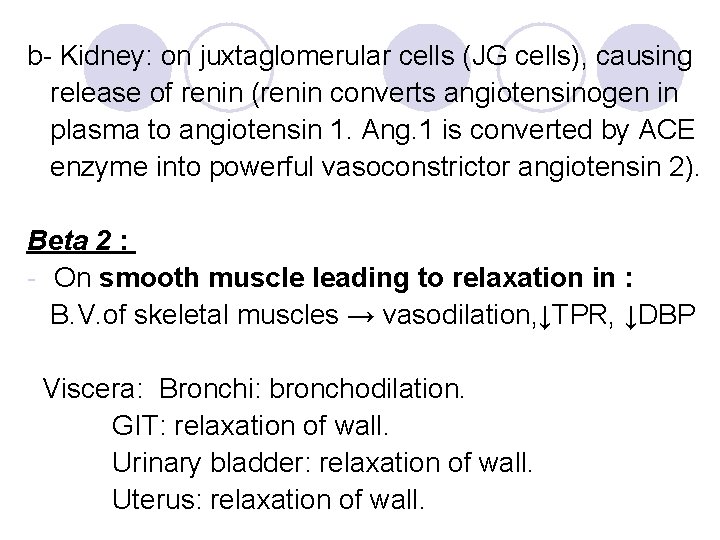
b- Kidney: on juxtaglomerular cells (JG cells), causing release of renin (renin converts angiotensinogen in plasma to angiotensin 1. Ang. 1 is converted by ACE enzyme into powerful vasoconstrictor angiotensin 2). Βeta 2 : - On smooth muscle leading to relaxation in : B. V. of skeletal muscles → vasodilation, ↓TPR, ↓DBP Viscera: Bronchi: bronchodilation. GIT: relaxation of wall. Urinary bladder: relaxation of wall. Uterus: relaxation of wall.
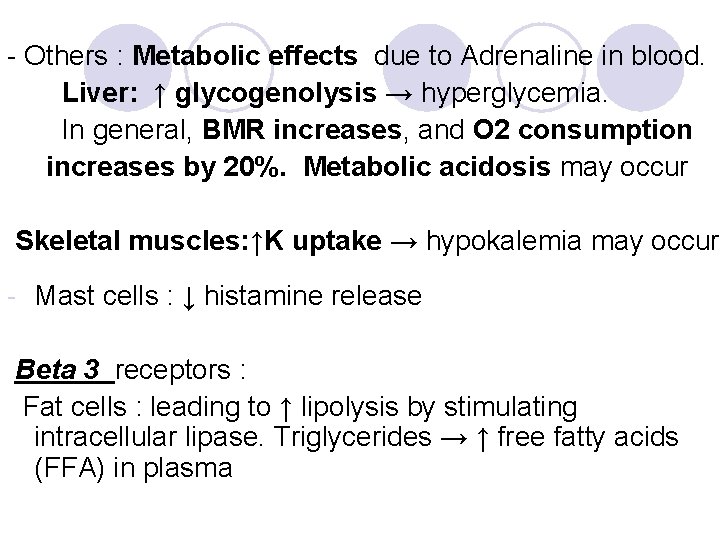
- Others : Metabolic effects due to Adrenaline in blood. Liver: ↑ glycogenolysis → hyperglycemia. In general, BMR increases, and O 2 consumption increases by 20%. Metabolic acidosis may occur Skeletal muscles: ↑K uptake → hypokalemia may occur - Mast cells : ↓ histamine release Βeta 3 receptors : Fat cells : leading to ↑ lipolysis by stimulating intracellular lipase. Triglycerides → ↑ free fatty acids (FFA) in plasma