General anesthetics This study material is recommended specifically

- Slides: 26
General anesthetics This study material is recommended specifically for practical courses from Pharmacology II for students of general medicine and stomatology. These brief notes could be used to prepare for the lesson and as a base for own notes during courses. Addititonal explanations and information are given in single lessons.
General anesthesia (GA) is artificialy induced reversible state, characterized by uncousciousness, analgesia and loss of vegetative and muscular reactions.
Requirements for GA • reversible loss of consciousness (uncousciousness alone is not sufficient to inhibit motoric and vegetative reflexes and induce analgesia) • • analgesia block of undesirable reflex reactions sufficient myorelaxation amnesia during the surgery
Stages of GA (when diethyl ether is used) 1. PREANESTETIC - without loss of consciousness, analgesia present 2. EXCITEMENT - uncousciousness, increase of vegetative reflexive activity, irregular breathing and heart rate, cardiovascular instability, spastic movements 3. SURGICAL - patient is ready for surgery 4. PARALYTIC - depression of brain stem due to anesthetic overdos.
Types of GA Combined GA intravenous + inhalational anesthetic Supplemented GA combination of GA with other drugs GA + opioids, anxiolytics Neuroleptanalgesia neuroleptics + opioids = strong sedation ad analgesia
Types of GA Neuroleptanestesia neuroleptanalgesia + i. v. anestetics + N 2 O + O 2 + short acting myorelaxants Ataranalgesia = analgosedation opiods + benzodiazepines diazepam + fentanyl Trankvanalgesia i. v. anesthetics + benzodiazepine ketamine + diazepam
General anesthetics • Inhalational liquid gaseous • Injectable barbiturates nonbarbiturates opiods benzodiazepines
Inhalational anesthetics Physical-chemical properties • gases • liquids (under atmospheric pressure liquids with boling point around 50°C, evporator – special instrumental equipment needed for use) • the equilibrium between drug concentration in inhaled air and blood is essential to reach optimal concentration of anesthetic in brain • different solubility in water, blood and lipids
Inhalational anesthetics Mode of action: depends on liposolubility nonspecific influence on ion channels in neuronal membranes MAC – minimal alveolar concentration, which is necessary to reach the surgical stage in a half of subjects
Inhalational anesthetics - liquids 1. Ethers diethyl ether today used rarely in humans (exposive, long excitation stage) advantage – can be administered without a special instrumentation because of low boiling point
Inhalational anesthetics - liquids 2. Halogenated hydrocarbons halothane fast onset and awaking weak analgesia biotransformartion up to 20% → hepatotoxicity AE: circulatory depression heart dysrhythmias when coadministered with catecholamines (increases myocardial senstivity) risk of malignant hyperthermia obsolete in developed countries
Inhalational anesthetics - liquids 3. Halogenated ethers isoflurane low biotransformation increase the efiicacy of myorelaxants unpleasant odour – disadvantage in pediatry desflurane, sevoflurane fast onset and awaking low biotransformation
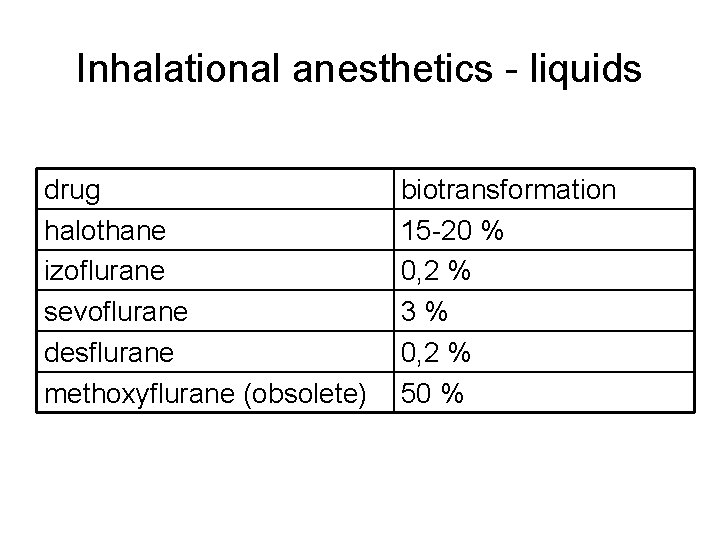
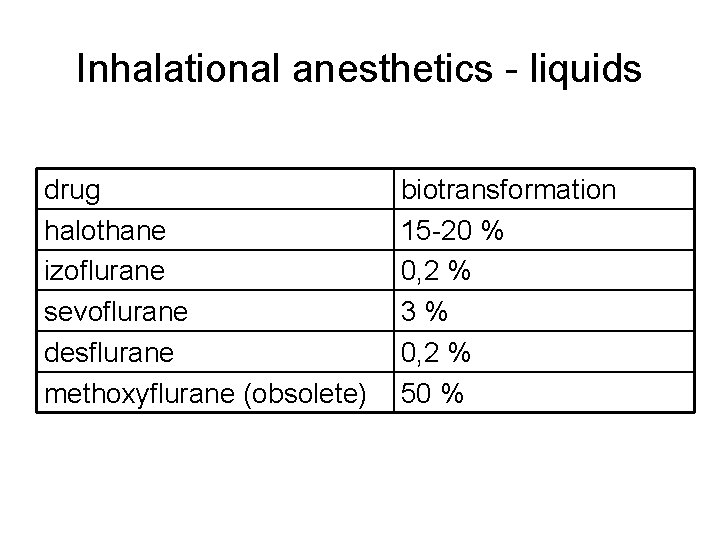
Inhalational anesthetics - liquids drug halothane izoflurane sevoflurane desflurane methoxyflurane (obsolete) biotransformation 15 -20 % 0, 2 % 3% 0, 2 % 50 %
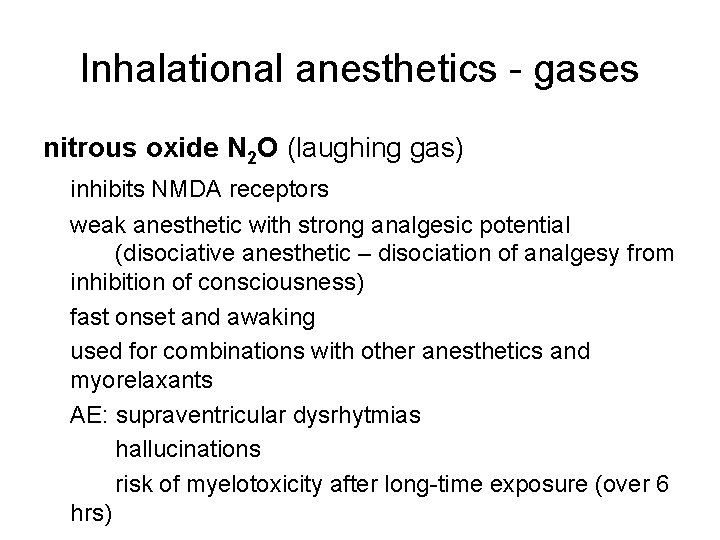
Inhalational anesthetics - gases nitrous oxide N 2 O (laughing gas) inhibits NMDA receptors weak anesthetic with strong analgesic potential (disociative anesthetic – disociation of analgesy from inhibition of consciousness) fast onset and awaking used for combinations with other anesthetics and myorelaxants AE: supraventricular dysrhytmias hallucinations risk of myelotoxicity after long-time exposure (over 6 hrs)
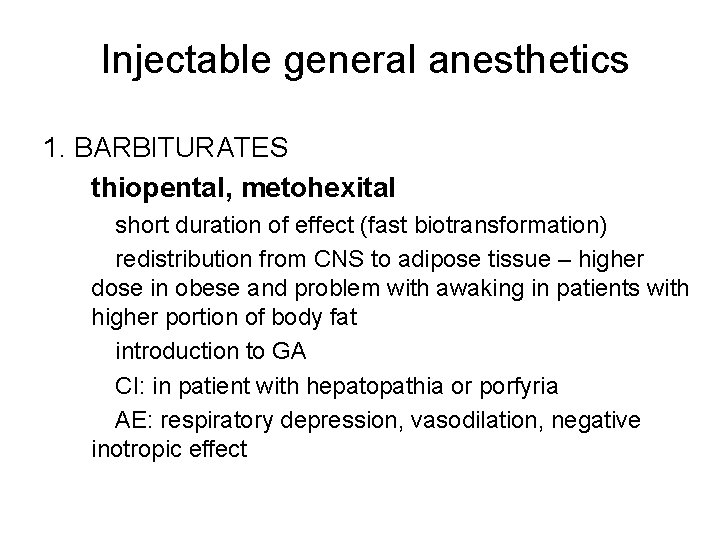
Injectable general anesthetics 1. BARBITURATES thiopental, metohexital short duration of effect (fast biotransformation) redistribution from CNS to adipose tissue – higher dose in obese and problem with awaking in patients with higher portion of body fat introduction to GA CI: in patient with hepatopathia or porfyria AE: respiratory depression, vasodilation, negative inotropic effect

Injectable general anesthetics 2. NONBARBITURATES ketamine Mof. A: NMDA receptor inhibition patients feel disociation from reality and own perception → disociative anesthesy introduction and short general anesthesy AE: ↑ BP and heart rate, hallucinations during awaking (prevention: combination with benzodiazepines) CI: hypertension, cardiac insufficiency, aterosclerosis, intracranial hypertension, glaucoma
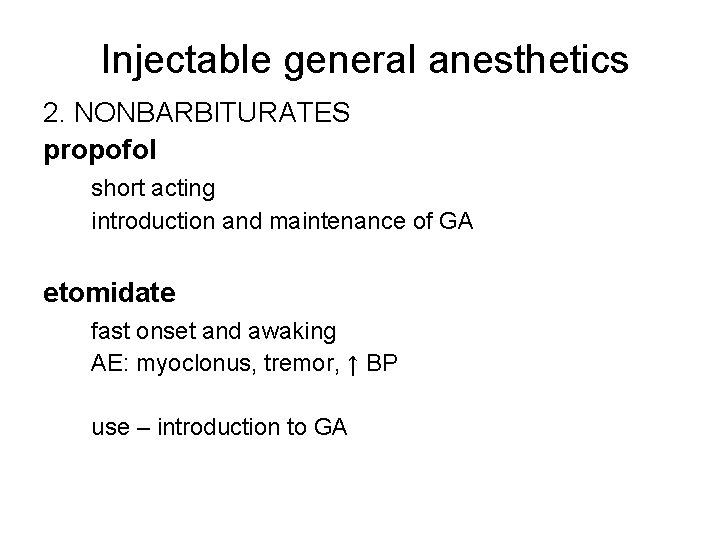
Injectable general anesthetics 2. NONBARBITURATES propofol short acting introduction and maintenance of GA etomidate fast onset and awaking AE: myoclonus, tremor, ↑ BP use – introduction to GA
Injectable general anesthetics 3. OPIOIDS fentanyl pethidin alfentanyl sufentanyl remifentanyl - see practicals from ANALGESICS
Injectable general anesthetics 4. BENZODIAZEPINES sensibilisation of GABA binding site on chloride channels midazolam premedication, introduction to GA depressive effect on respiration flunitrazepam
Process of GA 1. Premedication 2. Introduction to GA 3. Maintenance of GA 4. Awaking from GA
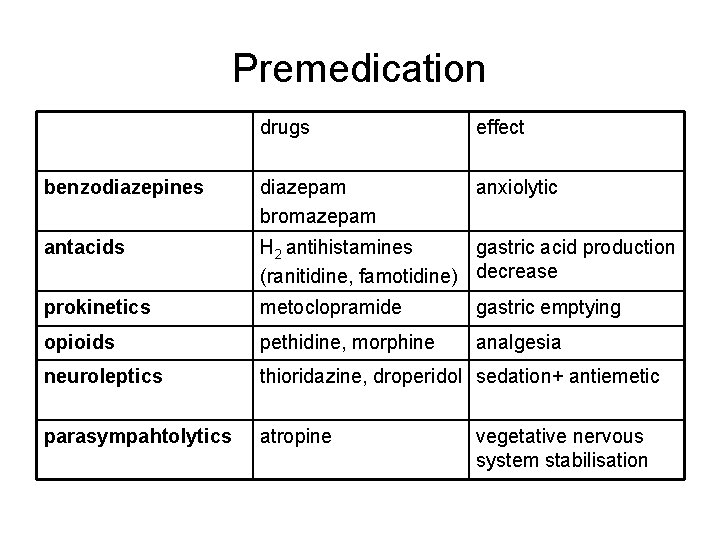
Premedication • to calm down the patinet • to prevent advers reactions of body • to prevent adverse reactions of anesthetics • to decerase the total amount of anesthetics • analgesy prior to surgery
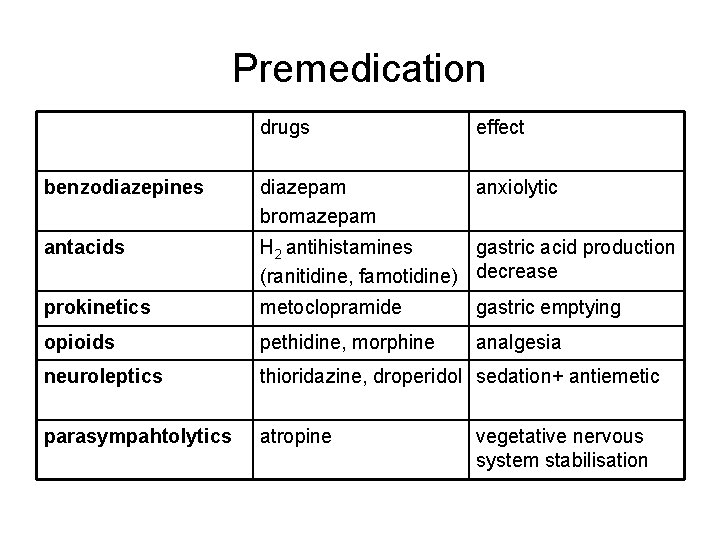
Premedication drugs effect benzodiazepines diazepam bromazepam anxiolytic antacids H 2 antihistamines gastric acid production (ranitidine, famotidine) decrease prokinetics metoclopramide gastric emptying opioids pethidine, morphine analgesia neuroleptics thioridazine, droperidol sedation+ antiemetic parasympahtolytics atropine vegetative nervous system stabilisation
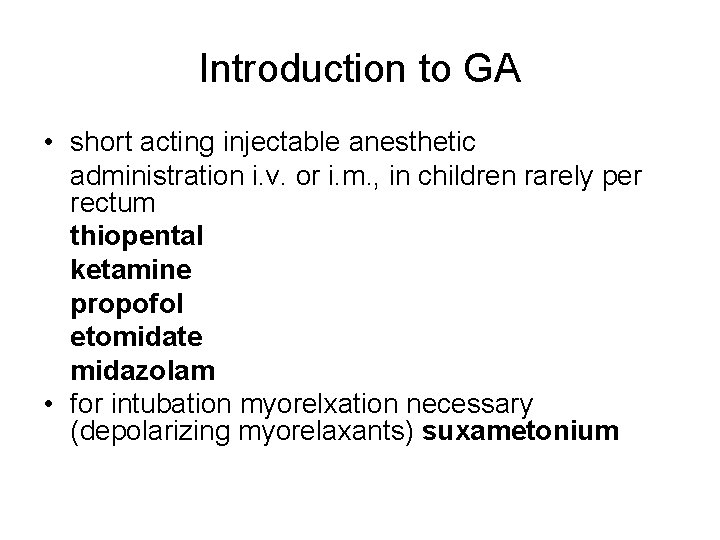
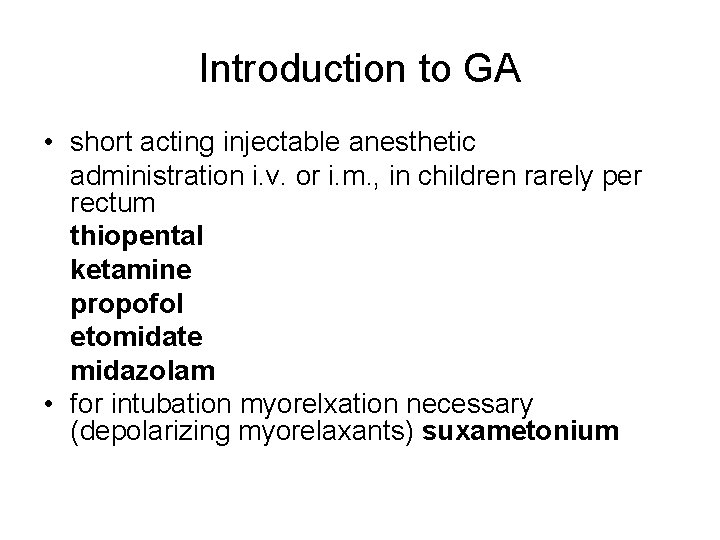
Introduction to GA • short acting injectable anesthetic administration i. v. or i. m. , in children rarely per rectum thiopental ketamine propofol etomidate midazolam • for intubation myorelxation necessary (depolarizing myorelaxants) suxametonium
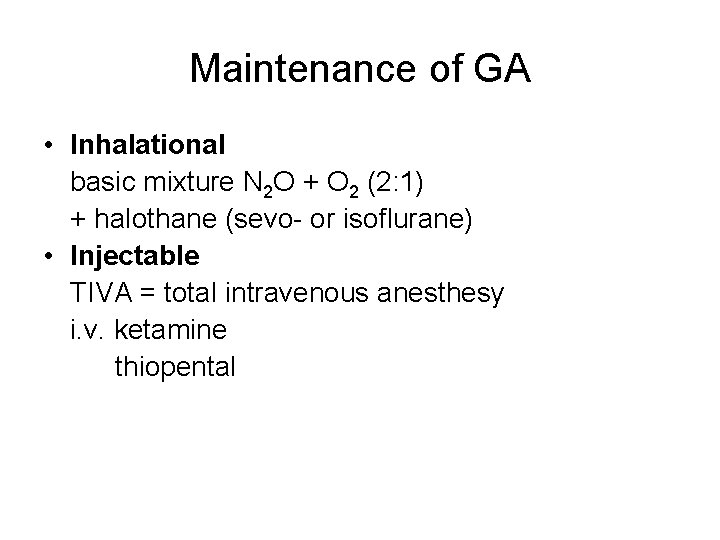
Maintenance of GA • Inhalational basic mixture N 2 O + O 2 (2: 1) + halothane (sevo- or isoflurane) • Injectable TIVA = total intravenous anesthesy i. v. ketamine thiopental
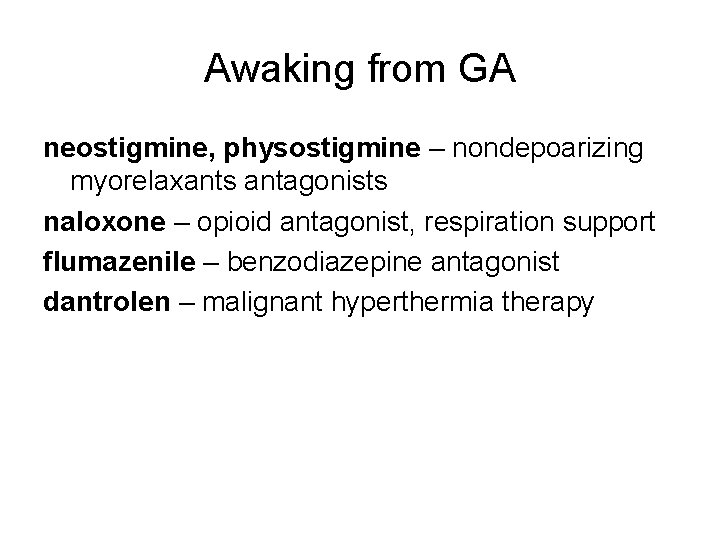
Awaking from GA neostigmine, physostigmine – nondepoarizing myorelaxants antagonists naloxone – opioid antagonist, respiration support flumazenile – benzodiazepine antagonist dantrolen – malignant hyperthermia therapy
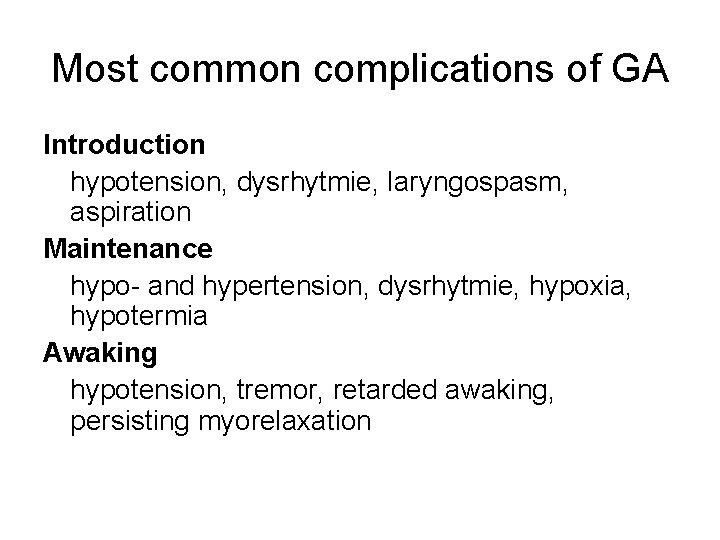
Most common complications of GA Introduction hypotension, dysrhytmie, laryngospasm, aspiration Maintenance hypo- and hypertension, dysrhytmie, hypoxia, hypotermia Awaking hypotension, tremor, retarded awaking, persisting myorelaxation